Abstract
Nerve injury is often associated with limited axonal regeneration and thus leads to delayed or incomplete axonal reinnervation. As a consequence of slow nerve regeneration, target muscle function is often insufficient and leads to a lifelong burden. Recently, the diagnosis of nerve injuries has been improved and likewise surgical reconstruction has undergone significant developments. However, the problem of slow nerve regeneration has not been solved. In a recent meta-analysis, we have shown that the application of low-intensity ultrasound promotes nerve regeneration experimentally and thereby can improve functional outcomes. Here we want to demonstrate the experimental effect of low intensity ultrasound on nerve regeneration, the current state of investigations and its possible future clinical applications.
Keywords: peripheral nerve injuries, nerve regeneration, reinnervation, experimental studies, low-intensity ultrasound, adjunct treatment, nerve reconstruction, nerve surgery, axonal injury
Introduction
As nerve surgery has leaped into the 21st century and provided many novel treatment options, it is still unable to successfully restore impaired function in a significant number of patients. Scientific studies have provided us with the necessary knowledge to understand the pathophysiology of nerve injury and adjust diagnosis and treatment accordingly. Thereby, we are now able to precisely identify nerve injuries using nerve conduction studies, sonography and most recently MR-neurography (a modern technology to image nerves using specific magnetic resonance imaging (MRI)-sequences). Likewise, treatment strategies have improved by identifying the necessity of tension-free reconstruction as propagated by Millesi (1984) or the ability to bypass long regeneration-distances using nerve transfers (Brown and Mackinnon, 2008; Colbert and Mackinnon, 2008).
The key issue in treating peripheral nerve injuries remains the inability to instantly reconnect severed axons to the distal stump and the slow or incomplete nerve regeneration after surgical reconstruction. As a consequence of long regeneration-distances or incomplete regeneration, target muscles undergo fibrotic degeneration. Proximal nerve lesions, where the distance-to-target exceeds the capacity for nerve regeneration (1 mm per day) in the time-frame for potential reinnervation (18 months), are therefore often associated with considerable functional disability in the mostly young and previously healthy patients.
For the reconstruction of nerve injuries, numerous surgical strategies have been developed to approach different injury scenarios. Uncomplicated distal nerve injuries can be treated with tension-free repair and autologous nerve grafts if necessary, which yields a significant chance for sufficient recovery. For this purpose, several donor nerves exist with acceptable donor morbidity while providing sufficient length and diameter for most reconstructions. In proximal injuries, as for example high radial nerve injuries or brachial plexus injuries, primary repair may often lead to unsuccessful recovery, necessitating the need for distal nerve transfers to provide reinnervation of muscle targets before fibrotic degeneration occurs. Therefore, many nerve injuries with traditionally poor outcomes have nowadays significantly better treatment options, to provide patients with motor function. However, as nerve transfers following proximal nerve injury necessitate the use of donor nerves, an additional sacrifice of healthy motor function is required, whereas the regenerative capacity of the original axon population remains unexploited. Therefore, whenever a tension-free nerve coaptation is possible, the primary repair remains the gold standard procedure in reconstructive nerve surgery, although the distance-to-target remains a limiting factor, especially in high-level nerve injuries.
All strategies, primary repairs, autologous nerve transplantation and nerve transfers have little chance to restore the original motor unit pattern of the reinnervated muscle, due to decreased numbers of reinnervating axons. The neuromuscular unit is able to compensate for this loss of innervation to some extent, as the lower number of regenerating axons reinnervates larger muscle units (territories of muscle fibers) to minimize the loss in force production. However, clinical experience shows that patients are rarely able to perform extremity function with the same dexterity and maximum force as before. As of today, we are thus merely able to provide acceptable solutions, especially compared to results without reconstructive surgery.
Currently, there is no surgical solution at hand to accelerate nerve regeneration and few promising surgical developments in sight. Therefore, adopting alternative solutions to supplement current nerve surgery concepts, may provide an additional boost to improve nerve regeneration. For this purpose, one potential approach is to improve nerve regeneration following surgery by the application of external stimulation, such as low-intensity ultrasound. These are devices used for self-guided therapy that are easy to apply and have shown to improve tissue regeneration in various applications. However, the use of ultrasound in nerve injury has not been investigated systematically in humans. We have, therefore, recently performed a meta-analysis on the available literature regarding its pre-clinical, positive experimental effects on nerve regeneration, which have however not been shown for shock wave treatment (Daeschler et al., 2018). In this perspective, we illustrate the potential benefit of additional ultrasound treatment for peripheral nerve reconstruction.
Ultrasound
Ultrasound is sound waves with frequencies above the human ear’s auditory spectrum. Its use has been investigated in numerous medical applications as supporting treatment for bone and cartilage healing. Previous investigations have shown that relatively low ultrasound intensities can stimulate tissue regeneration clinically and experimentally by the transmission of mechanical energy to target tissues (Hannemann et al., 2014). It is therefore used in the treatment of acute bone fractures and delayed fracture healing and has been shown to significantly promote the regeneration of ligaments, articular cartilage in intervertebral discs and acute fractures (Hannemann et al., 2014). Here, ultrasound waves induce mechanical motion of molecules in periodically alternating phases of compression and rarefaction and thereby stimulate tissue regeneration due to the transmission of mechanical energy (Hannemann et al., 2014). Furthermore, microscale turbulences are induced in inter- and intra-cellular fluids due to the nearby vibrating structures stimulated by ultrasound. This phenomenon has been termed the acoustic streaming effect and is believed to affect both diffusion rates of transmembrane channels and cellular membrane permeability. This subsequently allows better perfusion and transfusion of regenerative molecules (Dinno et al., 1989).
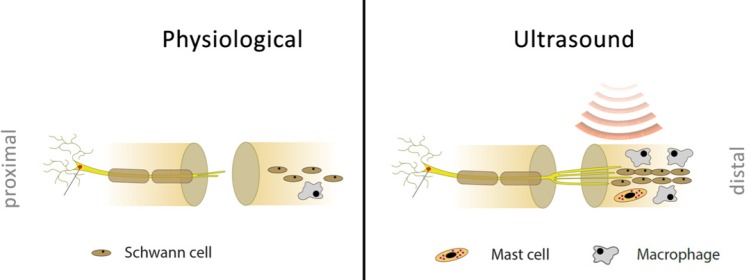
After nerve injury, a pathophysiological process takes place distal to the injury side called Wallerian degeneration. Here, the axons distal to the injury are removed and intact proximal axons grow distally to possibly reinnervate targets. A crucial role during this regeneration process is conducted by Schwann cells, which encase axons and are responsible together with Ranvier nodes for saltatory conduction in healthy nerves. During the initial injury phase, they recruit macrophages to the nerve, which phagocytose the cellular debris after axonal breakdown (Reichert et al., 1994). If the severed nerve is surgically reconnected, subsequent axonal regeneration and re-myelination distal to the injury side can take place. In this situation, the initial injury phase is followed by a proliferative phase, where Schwann cells guide the regeneration of axons and provide trophic support to the regenerating axons. Ultrasound may accelerate these physiological processes and therefore potentially stimulate peripheral nerve regeneration, as has been suggested by experimental studies. During the initial injury phase, external stimulation using ultrasound was found to increase the activity and number of Schwann cells and thereby the inflammatory phase in the absence of negative side effects (Raso et al., 2005; Zhang et al., 2009; Chen et al., 2010; Jahromy et al., 2013). Therefore, the process of removing the axonal debris and the consecutive start of the proliferative phase is potentially accelerated (Figure 1).
Figure 1.
Potential effects of external stimulation.
Left: Physiological regeneration of a nerve; right: regeneration of an ultrasound treated nerve including increased Schwann cell proliferation and activation, accelerated axonal regrowth, enhanced sprouting, and modulated early inflammatory response due to macrophage activation and mast cell degranulation.
The use of ultrasound after nerve repair has not been systematically explored in clinical studies, and its effect in patients remains unclear. We therefore recently analyzed the available experimental, pre-clinical literature in a systematic meta-analysis according to the PRISMA guidelines (Daeschler et al., 2018). Our findings suggest that supplemental ultrasound treatment at the side of injury improves functional regeneration in nerve injury models. Interestingly, the positive effects were evident throughout the regeneration phase, from early after injury to the end of the observation period in axonotmetic injury (nerve injury limited to axonal disconnection) and autograft repairs. A possible explanation for the improved regeneration can be derived from electromyographic studies, which suggest earlier reinnervation of the target muscles by accelerated axonal regeneration. Likewise, histomorphological analyses show that nerves exhibited a higher number of large calibre axons, a higher nerve fiber density and overall thicker myelin sheaths and possibly as a result significantly faster nerve conduction velocities. Previous works found increased expression of nerve growth factor (NGF) and ciliary neurotrophic factor (CNTF) in ultrasound treated nerves (Chen et al., 2010; Jahromy et al., 2013). These enhanced neurotrophin levels have been postulated to be involved in the beneficial effects of ultrasound therapy following nerve surgery. In accordance with the observed ultrasound effects, NGF is known to promote axonal branching (Streppel et al., 2002) and Schwann cell migration into the nerve gap (Whitworth et al., 1996). Moreover, CNTF has been shown to activate signal cascades that up-regulate the synthesis of axonal growth cone components in injured neurons (Kirsch et al., 2003; Wang et al., 2009). These signal cascades have been proven to be implicated in the promotion of the axonal outgrowth following nerve lesion (Qiu et al., 2005; Wu et al., 2007). Additionally, previous studies indicated a strong pro-survival effect for CNTF in severely injured motor neurons (Sendtner et al., 1990; Lang et al., 2005). These effects may contribute to the increased number of myelinated axons found in ultrasound treated nerves. However, future research is needed to further specify the neurobiological events during ultrasound therapy.
For the optimal application intensity, we found 200–500 mW/cm2 to improve nerve regeneration, but 200–300 mW/cm² to be superior in some functional and histological analyses (Mourad et al., 2001; Jahromy et al., 2013; Jiang et al., 2016).
Overall, this suggests that ultrasound stimulates the acceleration of the injury phase by faster debris removal as well as the proliferative phase by improving the release of growth factors. In experimental models, this leads to faster reinnervation of target muscles and consequently less fibrotic degeneration.
Application
Based on the promising findings of our meta-analysis and from known beneficial effects in other indications, we suggest testing ultrasound clinically in nerve injuries after surgical reconstruction. For this purpose, the adequate translation of ultrasound application in experimental models with different size properties or current clinical indications with only local application will be a key aspect for success. Typically, ultrasound therapy is self-applied one or multiple times a day with a small handheld applicator attached to a larger device serving as the base unit. There have been no reports of side effects and the application is not painful. The applicator’s size varies and subsequently the area of ultrasound application to the body surface. In experimental models, this is typically unproblematic, as the anatomy is comparably smaller and a sufficient application over the entire nerve is easy to achieve. In humans, application of the transducer over the entire nerve is not possible simultaneously. Therefore, the pathophysiology of the nerve injury must be considered for the optimal application. In the injury phase, debris is removed in the entire segment distal to the nerve injury, and therefore positive effects of ultrasound treatment could be expected in this distal segment. For this purpose, the transducer could be applied in the course of the nerve multiple times a day after the patient was instructed in the nerve’s anatomy. During the proliferative phase, axons regenerate distally to their target organ and so does the site of regeneration, where the ultrasound needs to be applied. As most patients with severe nerve injury undergo physiotherapy to keep passive motion intact, the physiotherapist or hand therapist could identify the site of nerve regeneration regularly using the Hoffmann-Tinel sign and instruct the patient to apply the ultrasound device in this location. This would ensure a reliable ultrasound application and establish a therapy monitoring. In general, it is to be expected that the self-application of the device provides good results, as an excellent compliance rate of 91% was reported for fracture delayed union treatment (Schofer et al., 2010). Additionally, to the monitoring by therapists, the currently available US food and drug administration (FDA) approved devices have integrated analyses software to allow clinical supervision of outpatient treatment and scientific evaluation (Figure 2).
Figure 2.
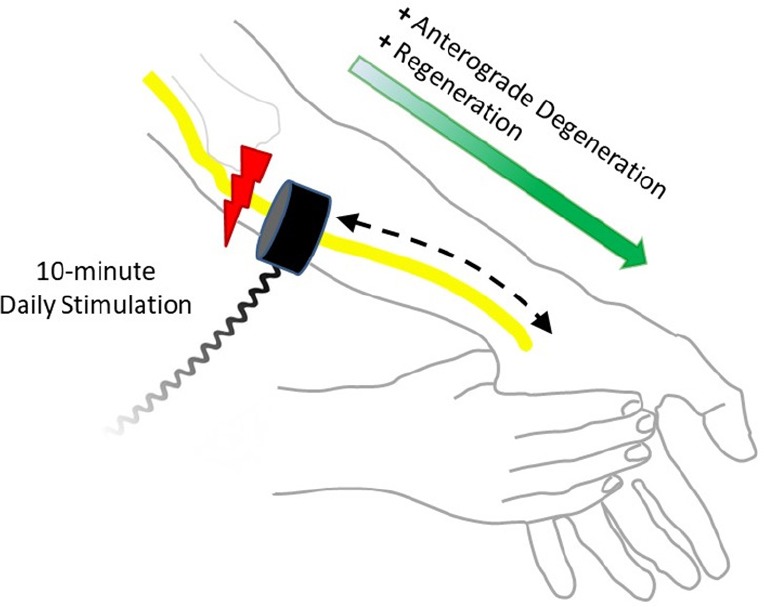
Application of ultrasound to nerve injuries.
An exemplary ulnar nerve injury is shown on the left arm. Distal to the nerve injury, first Wallerian degeneration takes place and subsequent regeneration after successful nerve reconstruction. To support both the injury and proliferative phase, the ultrasound transducer is applied in the course of the nerve, from the injury site to the distal muscle targets for 10 minutes a day.
Conclusion and Outlook
Recent developments in nerve surgery have provided patient-specific solutions to achieve better reconstructive treatment strategies. Thereby, we aim to defeat slow nerve regeneration. This task could potentially be augmented by supplemental treatments following nerve surgery. Based on our recent meta-analysis, we suggest that there is significant evidence to systematically explore ultrasound clinically in humans as an adjunct therapy following nerve surgery. It is to hope that this may further improve our results. We are currently preparing a clinical trial to investigate low-intensity ultrasound in nerve injuries and invite others to participate or conduct studies on their own.
Additional file: Open peer review report 1 (90.8KB, pdf) .
Footnotes
Conflicts of interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be considered as a potential conflict of interest.
Financial support: None.
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewer: Vance P. Lemmon, University of Miami, USA.
References
- Brown JM, Mackinnon SE. Nerve transfers in the forearm and hand. Hand Clin. 2008;24:319–340. doi: 10.1016/j.hcl.2008.08.002. v. [DOI] [PubMed] [Google Scholar]
- Chen WZ, Qiao H, Zhou W, Wu J, Wang ZB. Upgraded nerve growth factor expression induced by low-intensity continuous-wave ultrasound accelerates regeneration of neurotometicly injured sciatic nerve in rats. Ultrasound Med Biol. 2010;36:1109–1117. doi: 10.1016/j.ultrasmedbio.2010.04.014. [DOI] [PubMed] [Google Scholar]
- Colbert SH, Mackinnon SE. Nerve transfers for brachial plexus reconstruction. Hand Clin. 2008;24:341–361. doi: 10.1016/j.hcl.2008.07.001. v. [DOI] [PubMed] [Google Scholar]
- Daeschler SC, Harhaus L, Schoenle P, Boecker A, Kneser U, Bergmeister KD. Ultrasound and shock-wave stimulation to promote axonal regeneration following nerve surgery: a systematic review and meta-analysis of preclinical studies. Sci Rep. 2018;8:3168. doi: 10.1038/s41598-018-21540-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinno MA, Dyson M, Young SR, Mortimer AJ, Hart J, Crum LA. The significance of membrane changes in the safe and effective use of therapeutic and diagnostic ultrasound. Phys Med Biol. 1989;34:1543–1552. doi: 10.1088/0031-9155/34/11/003. [DOI] [PubMed] [Google Scholar]
- Hannemann PF, Mommers EH, Schots JP, Brink PR, Poeze M. The effects of low-intensity pulsed ultrasound and pulsed electromagnetic fields bone growth stimulation in acute fractures: a systematic review and meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg. 2014;134:1093–1106. doi: 10.1007/s00402-014-2014-8. [DOI] [PubMed] [Google Scholar]
- Jahromy FZ, Behnam H, Mansoori K, Rahimi AA, Edalat R, Mobarake JI. The effect of ultrasound on the expression of CNTF gene, a possible cause of ultrasound influence on the rate of injured peripheral nerve regeneration. Australas Phys Eng Sci Med. 2013;36:323–329. doi: 10.1007/s13246-013-0216-y. [DOI] [PubMed] [Google Scholar]
- Jiang WL, Wang YX, Tang J, Peng J, Wang Y, Guo QY, Guo ZY, Li P, Xiao B, Zhang JX. Low-intensity pulsed ultrasound treatment improved the rate of autograft peripheral nerve regeneration in rat. Sci Rep. 2016;6:22773. doi: 10.1038/srep22773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirsch M, Terheggen U, Hofmann HD. Ciliary neurotrophic factor is an early lesion-induced retrograde signal for axotomized facial motoneurons. Mol Cell Neurosci. 2003;24:130–138. doi: 10.1016/s1044-7431(03)00130-1. [DOI] [PubMed] [Google Scholar]
- Lang EM, Asan E, Plesnila N, Hofmann GO, Sendtner M. Motoneuron survival after C7 nerve root avulsion and replantation in the adult rabbit: effects of local ciliary neurotrophic factor and brain-derived neurotrophic factor application. Plast Reconstr Surg. 2005;115:2042–2050. doi: 10.1097/01.prs.0000163328.51271.dd. [DOI] [PubMed] [Google Scholar]
- Millesi H. Nerve grafting. Clinics in plastic surgery. 1984;11:105–113. [PubMed] [Google Scholar]
- Mourad PD, Lazar DA, Curra FP, Mohr BC, Andrus KC, Avellino AM, McNutt LD, Crum LA, Kliot M. Ultrasound accelerates functional recovery after peripheral nerve damage. Neurosurgery. 2001;48:1136–1141. doi: 10.1097/00006123-200105000-00035. [DOI] [PubMed] [Google Scholar]
- Qiu J, Cafferty WB, McMahon SB, Thompson SW. Conditioning injury-induced spinal axon regeneration requires signal transducer and activator of transcription 3 activation. J Neurosci. 2005;25:1645–1653. doi: 10.1523/JNEUROSCI.3269-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raso VV, Barbieri CH, Mazzer N, Fasan VS. Can therapeutic ultrasound influence the regeneration of peripheral nerves? J Neurosci Methods. 2005;142:185–192. doi: 10.1016/j.jneumeth.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Reichert F, Saada A, Rotshenker S. Peripheral nerve injury induces Schwann cells to express two macrophage phenotypes: phagocytosis and the galactose-specific lectin MAC-2. J Neurosci. 1994;14:3231–3245. doi: 10.1523/JNEUROSCI.14-05-03231.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofer MD, Block JE, Aigner J, Schmelz A. Improved healing response in delayed unions of the tibia with low-intensity pulsed ultrasound: results of a randomized sham-controlled trial. BMC Musculoskelet Disord. 2010;11:229. doi: 10.1186/1471-2474-11-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sendtner M, Kreutzberg GW, Thoenen H. Ciliary neurotrophic factor prevents the degeneration of motor neurons after axotomy. Nature. 1990;345:440–441. doi: 10.1038/345440a0. [DOI] [PubMed] [Google Scholar]
- Streppel M, Azzolin N, Dohm S, Guntinas-Lichius O, Haas C, Grothe C, Wevers A, Neiss WF, Angelov DN. Focal application of neutralizing antibodies to soluble neurotrophic factors reduces collateral axonal branching after peripheral nerve lesion. Eur J Neurosci. 2002;15:1327–1342. doi: 10.1046/j.1460-9568.2002.01971.x. [DOI] [PubMed] [Google Scholar]
- Wang L, Lee HK, Seo IA, Shin YK, Lee KY, Park HT. Cell type-specific STAT3 activation by gp130-related cytokines in the peripheral nerves. Neuroreport. 2009;20:663–668. doi: 10.1097/WNR.0b013e32832a09f8. [DOI] [PubMed] [Google Scholar]
- Whitworth IH, Brown RA, Dore CJ, Anand P, Green CJ, Terenghi G. Nerve growth factor enhances nerve regeneration through fibronectin grafts. J Hand Surg Br. 1996;21:514–522. doi: 10.1016/s0266-7681(96)80058-1. [DOI] [PubMed] [Google Scholar]
- Wu D, Zhang Y, Bo X, Huang W, Xiao F, Zhang X, Miao T, Magoulas C, Subang MC, Richardson PM. Actions of neuropoietic cytokines and cyclic AMP in regenerative conditioning of rat primary sensory neurons. Exp Neurol. 2007;204:66–76. doi: 10.1016/j.expneurol.2006.09.017. [DOI] [PubMed] [Google Scholar]
- Zhang H, Lin X, Wan H, Li JH, Li JM. Effect of low-intensity pulsed ultrasound on the expression of neurotrophin-3 and brain-derived neurotrophic factor in cultured Schwann cells. Microsurgery. 2009;29:479–485. doi: 10.1002/micr.20644. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.