Abstract
Purpose
An accurate understanding of the anatomy, identification and preservation of facial nerve is critical in performing successful functional parotidectomies. The current literature is replete with inconsistencies of various landmarks when used alone for identification of facial nerve trunk (FNT). The purpose of the paper is to introduce a new anatomical triangle, Borle's triangle (BT) for safer and reliable operative identification of FNT during parotodectomies.
Patients and methods
Between Aug 2014 and Dec 2017, twelve patients who reported with unilateral disease of the parotid gland with intact facial nerve function who underwent superficial or complete parotidecomies were included in the study. BT was conceptualized by intersection of three imaginary lines drawn along anatomical structures and forming a triangle comprising of angles a, b and c.
Results
Introperatively, BT helped reliably identify the FNT and its branches successfully in all the cases. The mean distance of FNT from angle b was found to be 12.18 ± 1.7 mm. Transient neurological deficits with one or more branches were seen in four cases whilst, one case had transient deficit with all the five peripheral branches. All of them spontaneously resolved completely by the end of three months post operatively.
Conclusions
When used in isolation, substantial variations exist in distances measured from anatomic landmarks to the main FNT in the literature. The BT utilizes three commonly used anatomical landmarks. It predictably helps in proper anatomic orientation, identification and preservation of FNT and branches with ease in parotidectomies.
Keywords: Borle's triangle, Facial nerve trunk, Parotidectomies, Anterograde dissection
1. Introduction
The facial nerve along its extracranial course, passes through the glandular substance of the parotid gland (PG) and hence vulnerable to injuries during parotidectomies. A comprehensive knowledge of its anatomy and meticulous dissection are the keys for identification of facial nerve trunk (FNT) and its branches which are crucial in preventing permanent functional impairment and medico-legal implications. During parotidectomies, the two classical approaches in identifying the FNT described are the conventional antegrade and retrograde dissection. To aid in early operative identification of FNT, various soft tissue and bony landmarks have been proposed. Frequently used anatomical landmarks are the tragal pointer (TP),1 the tympanomastoid suture,2 the posterior belly of digastric, (PBD)3 the styloid process, (SP)4 and retromandibular vein.5 Though these have been extensively discussed in literature, however, it lacks convincing evidence of establishing superiority of an individual landmark when compared to others.6
The consistency of soft tissue landmarks are influenced by age, previous surgery, intrinsic scarring and the extent of the existing pathology.7 Bony landmarks have been considered as the most reliable anatomical guides owing to their rigid and consistent location.8 However, recently variability and discrepancy between the two sexes while using some of the bony landmarks have been reported.9,10
This marked ambiguity and controversy amongst surgeons regarding the operative accuracy and precision of these bony and soft tissue landmarks led the senior author propose an anatomical triangle for ease of identification of FNT during parotid surgeries. The aim of the present paper was to introduce a new anatomical triangle using the some of the commonly used landmarks for safe, easy and reliable way of identifying FNT.
2. Patients and method
The present study included 12 patients with unilateral PG pathology that underwent unilateral superficial parotidectomies for benign and malignant pathologies affecting parotid glands by the same surgical team during Aug 2014 to Dec 2017 at our institute. All procedures performed in the study were in accordance with the ethical standards of the institution and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Institutional ethical committee clearance was obtained for this study. Detailed written informed consent conveying all possible complications with emphasis on facial nerve palsy was obtained from the patient. Preoperatively, all patients were evaluated by 1.5 T contrast Magnetic Resonance Imaging (MRI) for the extent of the disease. Fine needle aspiration cytology (FNAC) was carried out to ascertain the diagnosis. 10 patients were diagnosed with benign salivary gland tumors (5 pleomorphic adenomas, 3 Warthin's tumour, 1 case each of oncocytoma, and chronic nonspecific sialadenitis of the PG), whilst the disease in the remaining two cases were found to be malignant in nature (1 case each of Muco epidermoid carcinoma and Carcinoma ex pleomorphic adenoma).
2.1. Method
Under general anesthesia, in supine position, with adequate extension at neck the subject's head was turned to the opposite direction. Following standard preparation of the surgical site with a suitable antimicrobial solution, the surgical site was accessed using Modified Blair's lazy S incision. A skin flap was raised in a sub platysmal plane in the cervical region and along the superficial musculo aponeurotic (SMAS) layer over the PG to expose the parotid capsule in the preauricular area. Dissection in the same plane was continued to expose the PG anteriorly and the anterior border of the sternocleidomastoid muscle (SCM) posteriorly. At all point of time, care was exercised to avoid perforation of skin flap.
The anterior border of the SCM was used to identify the tail of the PG. Sharp dissection was continued to separate the tail of the PG off the SCM and also from the cartilaginous external auditory canal. The greater auricular nerve coursing superficially on surface of the SCM was identified and divided as close to the PG as possible in an effort to preserve the posterior branch which if required may serve as a potential nerve graft if needed. The superficial lobe of the gland was gently retracted medially and the blunt dissection was accomplished at the posterior border of the gland. The skeletonized anterior border of SCM was retracted laterally to expose the PBD muscle which was then visualized.
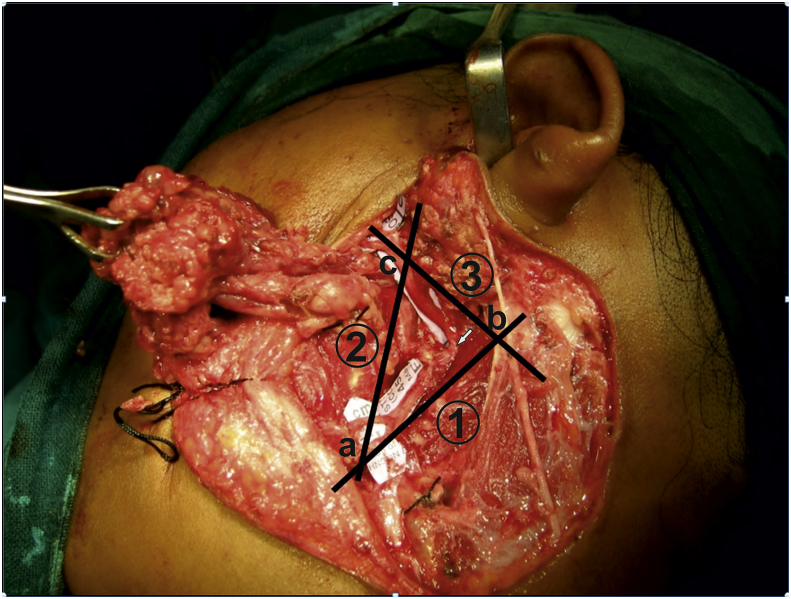
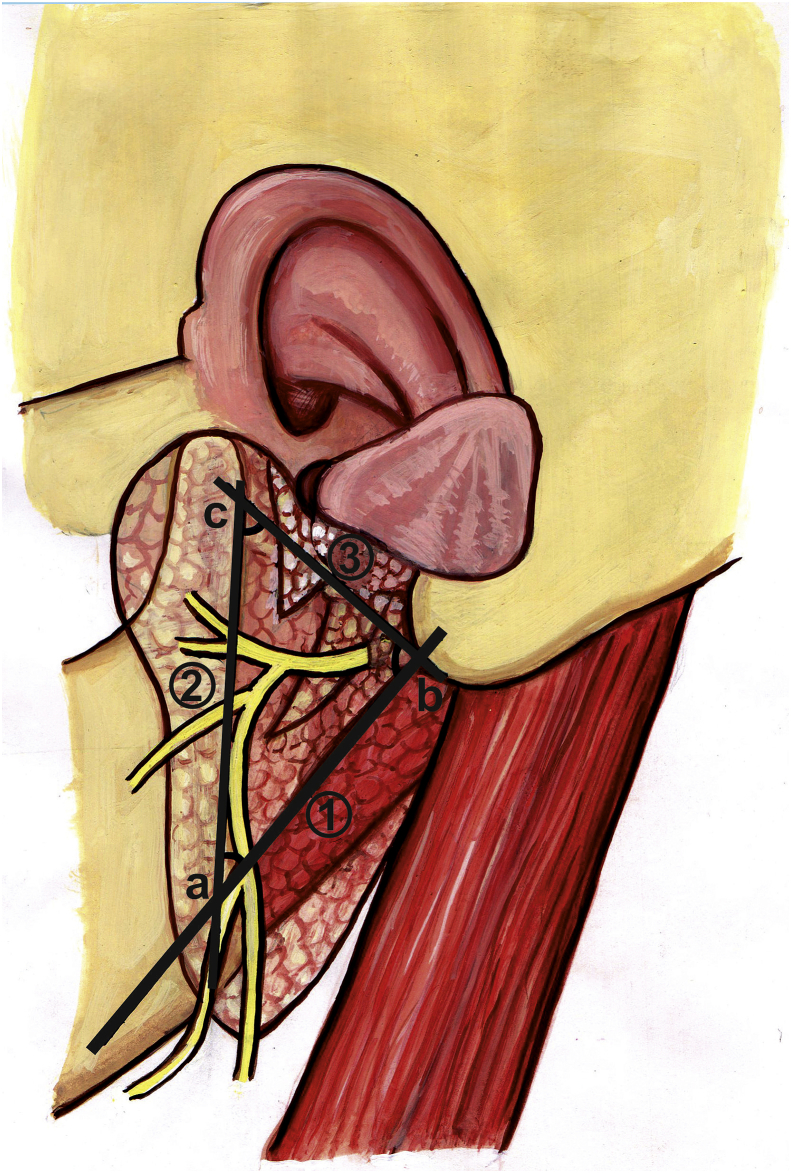
2.2. Outlining of Borle's triangle
A first line was marked with the ink starting from the tip of the mastoid process, running along the superior border of the PBD. Posterior border of the ramus of the mandible was then palpated and second line was drawn along the posterior border of the ramus. These two lines intersect with each other anteriorly, forming the apex of the triangle (angle a). The base of the triangle is marked by drawing the third line starting from the tip of the mastoid process, (angle b) running anteriorly, till it joins the second drawn line along the posterior border of the ramus (angle c). The FNT is often found within this triangle just above the angle b formed by the 1st and the 3rd line if gentle and blunt dissection is carried out at this point (Fig. 1, Fig. 2). The facial nerve is seen as white and glistening structure. The mean distance of FNT from the angle b was 12.18 ± 2 mm within a range of 9–15 mm. The use of tragal pointer helps in locating the FNT during the dissection. The dissection was carried out in an antegrade manner following the FNT to reach the pes anserinus. Thereafter, using bipolar cautery and blunt dissection, the cervicofacial and temporofacial divisions were exposed and the ‘pes anserinus’ dissected while bluntly lifting off the superficial lobe of the PG from the nerve branches. In total parotidectomy cases, after delivering the superficial lobe, the FNT along with the nerve branches were gently lifted up and the deep lobe of the PG was dissected and removed. After achieving hemostasis, a closed circuit suction drain was secured and layer wise closure done with 3-0 vicryl and subcuticular suturing of the skin with 3-0 prolene. Pressure dressing was applied over the surgical area and parenteral antibiotics and analgesics were instituted.
Fig. 1.
Outlining of Borle's Triangle for identification of facial nerve trunk.
Fig. 2.
Diagrammatic presentation of Borle's Triangle.
2.3. Follow up
All the patients were followed up closely during the hospital stay postoperatively for nerve injuries and wound-associated complications and consequently at 1 and 3 weeks and subsequently every month until the sixth month postoperatively. For evaluation of integrity of facial nerve, five standard facial expressions were requested to be performed: eyebrow raise, gentle eye closure, tight eye closure, nose wrinkle, and maximal smile. The neurological deficits of the facial nerve were graded according to House and Brackmann facial nerve grading system (HBI) for facial nerve grading system.11 These observations were recorded by an independent examiner postoperatively during hospital stay and subsequently during each hospital visit as per the defined study protocol.
3. Results and observations
The demographics, diagnosis, procedures performed and complications of all patients are tabulated in Table 1. There were 9 male and 3 female patients. Mean age of the patients was 41.6 ± 2.42 years. All the surgical wounds healed uneventfully. Post-operatively, complications of superficial parotidectomies included transient neurologic deficit (Grade III) of the marginal mandibular nerve in 1 case and of the temporal nerve in 2 cases. All the three cases of transient nerve deficit responded well to injectable corticosteroids immediate post operatively followed by oral steroid therapy of Methyl Prednisolone 20 mg (appropriate tapering dosages) with Methylcobalamine 1500 μgm. The transient nerve palsies in all the three cases of superficial parotidectomy resolved completely in 6 weeks duration.
Table 1.
Patients' demographic and clinical data
| Patient no | Age Yrs |
Sex | Diagnosis | Type of parotidectomy | Distance of FNT from angle B | Complications |
|---|---|---|---|---|---|---|
| 1 | 41 | M | Pleomorphic adenoma | Superficial parotidectomy | 13.6 | Marginal Mandibular nerve deficit |
| 2 | 39 | M | Pleomorphic adenoma | Superficial parotidectomy | 12.4 | NIL |
| 3 | 43 | F | Warthins tumour | Superficial parotidectomy | 12.0 | NIL |
| 4 | 40 | M | Pleomorphic adenoma | Superficial parotidectomy | 9.2 | Temporal nerve deficit |
| 5 | 44 | M | Carcinoma expleomorphic adenoma | Total parotidectomy | 14.4 | Marginal Mandibular and Buccal nerve deficit |
| 6 | 46 | M | Oncocytoma | Superficial parotidectomy | 10.4 | NIL |
| 7 | 39 | F | Pleomorphic adenoma | Superficial parotidectomy | 13.0 | NIL |
| 8 | 45 | M | Mucoepidermoid Carcinoma | Total parotidectomy | 10.6 | Nerve deficit with all the branches |
| 9 | 42 | F | Chronic sialadenitis | Superficial parotidectomy | 11.4 | Temporal nerve deficit |
| 10 | 40 | M | Warthins tumour | Superficial parotidectomy | 15.0 | NIL |
| 11 | 39 | M | Pleomorphic adenoma | Superficial parotidectomy | 13.6 | NIL |
| 12 | 42 | M | Warthins tumour | Superficial parotidectomy | 10.6 | NIL |
Amongst the two total parotidectomy cases, 1 case had transient nerve deficit of the buccal and marginal mandibular nerve while one case demonstrated weakness with all the branches of facial nerve (Grade IV). The patients were administered the same drug regimen protocol and exhibited complete functional recovery in averagely 8 weeks. We did not experience any Frey's syndrome or salivary fistula post operatively in any of the operated cases.
4. Discussion
The location and identification of certain anatomic structures are the basic tenet employed in any surgical procedure. Intraoperatively, surgeons rely on the use of certain anatomical landmarks for identifying the location of vital structures. PG surgery presents a special challenge to the maxillofacial surgeons, because majority of tumors indicated for removal are benign and hence, the treating surgeons and patients anticipate an uneventful, complete recovery of facial nerve function post surgically. Facial nerve injury during parotidectomy is a much feared complication having daunting repercussions on the patients' quality of life. A detailed understanding of the operative anatomical landmarks during surgery and a meticulous surgical exploration can help safeguarding the FNT and branches. The present study aims to exhibit easily identifiable anatomical landmarks providing a safer and more predictable route to dissecting the FNT and its branches with minimal post op morbidity.
Janes (1940)1 has been credited for the first known attempt for early intraoperative exposure of FNT by antegrade dissection, and, since then numerous authors have advocated various landmarks for intraoperative identification of FNT. Traditionally, antegrade dissection has been the technique of choice for intraoperative identification of FNT. The retrograde technique is highly technique sensitive and can result in injury to the peripheral branches while locating them. The retrograde dissection was lost to favour because of diverse branching patterns in particularly observed distal to pes anserinus and variability of relationship of peripheral branches deeper to the venous structures However, retrograde dissection is the technique of choice in cases of revision surgeries and large tumors obstructing FNT.12
Almost all of the existing landmarks described in the literature have been evaluated as individual (single) landmarks or in comparison with others for locating and identification of FNT. When evaluated individually, both, whether bony or soft tissue, exhibit variations and some minor inherent limitations. The commonly used landmarks are the TP, the TMS, and the superior part of PBD.
TP advocated by Conley,4 is the frequently referred landmark for intraoperative identification of FNT. The mean of differences in measurements between TP and FNT ranged from 13.6 ± 11.0 mm.6 This wide difference in linear distance makes the surgery more challenging, more time consuming and complex for surgeons. It was observed that the direction of the cartilaginous tip of lacks uniform interpretations especially by trainee surgeons. It soon fell out of favour in view it being cartilageous, mobile and blunt with irregular tip.1 The TMS is the other most commonly evaluated landmark along with TP. The FNT from TMS was measured in the mean range of 3.79 ± 2.92 mm in various studies.6 It has some advantages like, it is easy to locate, because of its invariable position and it further leads to the stylomastoid foramen. However, it has some disadvantages like, need of additional dissection inferiorly and the need of stripping the periosteum for its exposure. Furthermore, that its accessibility is obscured by robust tendon of sternocleidomastoid muscle traversing across to the lateral part of mastoid. This cumulatively adds to the complexity of the procedure.
Another frequently used landmark is the superior border of PBD. FNT was found to lie within a distance of 4.8–12.8 mm of PBD with a mean distance of 8.79 ± 3.99 mm in various studies.6 Its advantages include, being easily identifiable by the virtue of it lying superficial to FNT, but by virtue of it being a mobile tissue it is vulnerable to degree of retraction.9 The SP is another consistent landmark to identify FNT. The mean length of SP from FNT was found to be 9.8 mm ± 0 mm.6 However, the FNT may lie plane deeper to facial nerve making vulnerable to damage while dissection. In certain clinical situations, its length may be variable, such as elongation in eagles syndrome, or small or absent in some proportion of cases.4 Furthermore, in few instances the exposure of the SP could be impeded by the tumour mass itself. The above mentioned landmarks however cannot be underestimated as they form the basis of our proposed triangle.
The dexterous effort to explore the FNT in supra-fascial parotidectomy is anatomically driven and is rewarded by a deeper than expected dissection. The triangle described herein should further re-enforce the effort to persevere the search of FNT. In the exhibited technique, we utilized three superficial, easily identifiable landmarks to outline a triangle (Borle's triangle) for ease of identification of FNT namely, the inferior tip of the mastoid process, the superior border of PBD and posterior border of ramus of mandible which are rarely found to be involved in the parotid disease. The proposed triangle is outlined by joining these three anatomical landmarks with imaginary lines. These structures are easily identifiable, stable, not usually involved by the disease process and invariably exposed during dissections in parotid surgery.
BT is a modification of anatomic triangles described earlier. 13,14 The clinical utility of this triangle has been substantiated clinically in a series of 12 cases exhibited in the present series. Utilizing the aforementioned landmarks we could easily identify and locate the FNT in all the cases. We believe that implementation of such anatomical orientation could aid in safer navigation around FNT and its branches in parotidectomies. The main advantage of our approach lies in the ease with which the proposed landmarks aid in reliably locating the FNT. Our technique has a definite learning curve albeit small, can be an indispensable tool at the disposal of trainee or under experienced surgeons and can be potentially used as tutoring technique. The limitation of the present paper is that it lacks comparison with other commonly used landmarks for identification of FNT.
5. Conclusions
The proposed anatomical landmarks in our study aid in reliable identification of FNT with ease and reliability. It can be of help to trainees, under experienced surgeons and can be applied to surgeries in and around PG.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for- profit sectors.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jobcr.2018.08.004.
Contributor Information
Rajiv M. Borle, Email: Borleregistrardmims@gmail.com.
Anendd Jadhav, Email: anendd.j@gmail.com.
Nitin Bhola, Email: drnitinbhola@gmail.com.
Pawan Hingnikar, Email: pawan.hingnikar@gmail.com.
Prafulla Gaikwad, Email: drprafullagaikwad@yahoo.com.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Beahrs O.H. The surgical anatomy and technique of parotidectomy. Surg Clin North Am. 1977;57:477. doi: 10.1016/s0039-6109(16)41230-2. [DOI] [PubMed] [Google Scholar]
- 2.Conley J. Search for and identification of the facial nerve. Laryngoscope. 1978;88:172. [PubMed] [Google Scholar]
- 3.Reid A.P. Surgical approach to the parotid gland. Ear Nose Throat J. 1989;68:151. [PubMed] [Google Scholar]
- 4.Conley J. Thieme; 1975. Salivary Glands and the Facial Nerve. George Stuttgart. [Google Scholar]
- 5.Kopuz C., Ilgi S., Yavuz S., Onderoglu S. Morphology of the retromandibular vein in relation to the facial nerve in the parotid gland. Acta Anat (Basel). 1995;152:66–68. doi: 10.1159/000147685. [DOI] [PubMed] [Google Scholar]
- 6.Ji Y.D., Donoff R.B., Peacock Z.S., Carlson E.R. Surgical landmarks to locating the main trunk of the facial nerve in parotid surgery: a systematic review. J Oral Maxillofac Surg. 2018 Feb;76(2):438–443. doi: 10.1016/j.joms.2017.06.039. [DOI] [PubMed] [Google Scholar]
- 7.Greyling L.M., Glanvill R., Boon J.M. Bony landmarks as an aid for intraoperative facial nerve identification. Clin Anat. 2007 Oct;20(7):739–744. doi: 10.1002/ca.20508. [DOI] [PubMed] [Google Scholar]
- 8.Nishida M., Matsuura H. A landmark for facial nerve identification during parotid surgery. J Oral Maxillofac Surg. 1993;51:451–453. doi: 10.1016/s0278-2391(10)80368-4. [DOI] [PubMed] [Google Scholar]
- 9.Pather N., Osman M. Landmarks of the facial nerve: implications for parotidectomy. Surg Radiol Anat. 2006;28:170. doi: 10.1007/s00276-005-0070-z. [DOI] [PubMed] [Google Scholar]
- 10.Rea P.M., McGarry G., Shaw-Dunn J. The precision of four commonly used surgical landmarks for locating the facial nerve in anterograde parotidectomy in humans. Ann Anat. 2010;192:27. doi: 10.1016/j.aanat.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 11.House J.W., Brackmann D.E. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93:146–147. doi: 10.1177/019459988509300202. [DOI] [PubMed] [Google Scholar]
- 12.Witt R.L., Weinstein G.S., Rejto L.K. Tympanomastoid suture and digastric muscle in cadaver and live parotidectomy. Laryngoscope. 2005;115:574. doi: 10.1097/01.mlg.0000161343.85009.4c. [DOI] [PubMed] [Google Scholar]
- 13.Carlson G.W. The salivary glands. Embryology, anatomy, and surgical applications. Surg Clin North Am. 2000 Feb;80(1):261–273. doi: 10.1016/s0039-6109(05)70405-9. [DOI] [PubMed] [Google Scholar]
- 14.Pereira J.A., Merí A., Potau J.M., Prats-Galino A., Sancho J.J., Sitges-Serra A. ASimple method for safe identification of the facial nerve using palpable landmarks. Arch Surg. 2004;139(7):745–747. doi: 10.1001/archsurg.139.7.745. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.