Abstract
Background:
Neurological rehabilitation service in developing countries like India is a great challenge in view of limited resources and manpower. Currently, neurological rehabilitation with a multidisciplinary team is limited to a few major cities in the country. Tele-neurorehabilitation (TNR) is considered as an alternative and innovative approach in health care. It connects the needy patients with the health-care providers with minimum inconvenience and yields cost-effective health care.
Aim:
The aim of this study was to study the socioclinical parameters, feasibility, and utility of TNR services in India.
Methodology:
A retrospective file review of TNR consultations provided through Telemedicine Center at a quaternary hospital-based research center in south India between August 2012 and January 2016.
Results:
A total of 37 consultations were provided to the patients belonging to four districts of Karnataka. The mean age of the patients was 34.7 (±19.5) years, 23 (62.1%) were aged between 19 and 60 years, and 31 (83.8%) were male. Thirty-one patients (83.8%) had central nervous system-related disorders such as stroke, cerebral palsy, and tubercular meningitis with sequelae or neuromuscular disorders such as Guillain–Barre Syndrome and Duchenne muscular dystrophy. Twelve patients (32.4%) were advised to consult higher centers in the vicinity, and the rest was referred to the district hospital.
Conclusion:
The findings suggest that TNR services are feasible, effective, and less resource intensive in delivering quality telemedicine care in India. More clinical studies are required to elucidate its full utility at different levels and in different parts of the country.
KEYWORDS: Collaborative care, feasibility, neurorehabilitation, telemedicine
INTRODUCTION
Tele-rehabilitation is defined as “Providing rehabilitation services to patients at their location using information and communication technologies.”[1] Tele-rehabilitation is considered as an alternative and innovative approach to health care, which has been made possible with rapid advancement in technological and rehabilitation methods in the recent years. The current technological approach provides a wide range of services such as teleconsultation, tele-multimodal care, telehealth care, tele-home-based care, tele-technology-aided rehabilitation including robotics, telemonitoring, e-health, and cognitive rehabilitation to name a few.[2,3,4,5,6,7,8,9] All of these modalities can be considered as subfields of tele-rehabilitation and would fall under the rubric of telemedicine. In the last decade or so, the utility of tele-rehabilitation services and the programs has seen an upsurge worldwide. It may be attributed to several factors such as growing attention among researchers and service providers, development and upgradation of advanced technology, funding resource, feasibility of services, and acceptability of services by consumers/end users.[5,10,11] Tele-neurorehabilitation (TNR) serves to needy patients, who are unable to access health-care facility due to long distance, immobility, cost, nonavailability of the expert clinician in their geographical area, etc.[1,11,12] This, in turn, reduces health cost burden for the patient and the society, as has been suggested by many studies in the past.[3,5,6] Telemedicine services encompass a variety of services such as patient consultation, education and training of families and professionals in the area, follow-up of the patients, and monitoring of tele-services.[4,5,6,8,13,14] Recent reviews on clinical effectiveness and applications of technology in delivering effective tele-rehabilitation service and alternative interventions are limited.[13,15,16] Hence, there is a need for more trials and comprehensive studies on same issue.
India is facing huge challenges in the health sector due to a paradigm shift in disease burden. One of the major issues is increasing incidence of noncommunicable disorders (NCDs).[17] Among the NCDs, several neurological disorders are associated with limited therapeutic options, and lack of specific treatment further contributes to the disease burden, mortality, morbidity, and disability. Neurorehabilitation is considered as an integral component of neurology services, because of the morbidity and disability occurring due to neurological disorder. Providing neurorehabilitation service in developing country like India is a great challenge in view of limited resources and manpower, which are limited to a few tertiary/quaternary institutes and corporate sector in the major cities. There are very limited data from India on the role of telemedicine in neurological rehabilitation. One of such studies with 22 patients suggested that tele-rehabilitation in the form of home-based geriatric care is feasible and acceptable by clients.[18] With the interventions based on telemedicine consultation, 70% of the patients showed significant improvement in balance at the end of intervention as compared to baseline.[18,19]
Telemedicine Center in our institute has been providing TNR service since 2010 to all district hospitals of Karnataka in collaboration with the Department of Health and Family Welfare, Government of Karnataka through Karnataka State Wide Area Network (KSWAN).[20] The aim of the present study was to observe the socioclinical parameters of the patients who were provided tele-rehabilitation services. We also wanted to observe the feasibility and utility of these services provided for over 4 years in our center.
METHODOLOGY
The TNR services are provided through hub and spoke model (HSM) of telemedicine using electronic health record (HER)-based video conference mode, enabled for the synchronous mode with a collaborative care model in our institute. Clinicians from the district hospital, who desire to have these consultations contacted through their telemedicine technicians and provided basic socioclinical details of patients who in turn entered in EHR of KSWAN network.[20] These technicians would then fix up an appointment based on the availability of clinicians, experts, patients, and telemedicine service. In a collaborative care model patients are seen/discussed with respective district hospitals in live, real-time video conference mode (in the hub and spoke as well as a synchronous model of telemedicine) for an average of about 15–20 min. At the end of the consultations, treatment and prescription to the patients would be provided by a district hospital doctors.
For the study purpose, data were collected from the file of tele-neurorehabilitation consultations and tele-register. Data were analyzed using descriptive statistical methods using Statistical Package for the Social Sciences (SPSS) version 20 (IBM, Chicago, IL, USA). This study was approved by the Institutional Internal Ethics Committee.
RESULTS
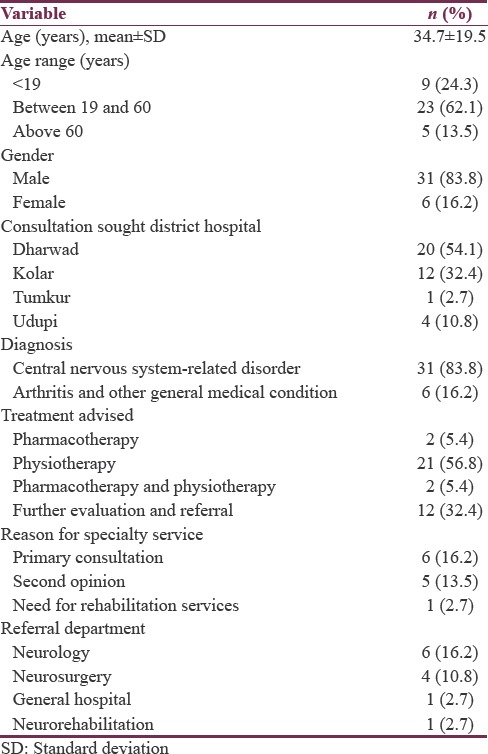
A total of 37 TNR consultations were provided between August 2012 and January 2016. Patients from four districts of Karnataka had sought the consultation. Table 1 shows the sociodemographic and clinical profile details of patients. Thirty-one (83.8%) patients were male and the mean age was 34.7 (±19.5) years and 23 (62.1%) were aged between 19 and 60 years. Thirty-one patients (83.8%) had central nervous system-related disorders such as stroke, cerebral palsy, tubercular meningitis, intervertebral disc prolapse (IVDP), tuberculosis of the spine, spinal astrocytoma with sequelae, and low backache or neuromuscular disorders such as Duchene muscular dystrophy and Guillain–Barre syndrome. Twenty-one (56.8%) patients were advised physiotherapy. Out of 12 (32.4%) requiring specialist referral along with pharmacotherapy, six required neurology and four required neurosurgery consultations. Four (10.8%) patients reported back after a fortnight for follow-up.
Table 1.
Sociodemographic and clinical profile of patients who availed tele-neurorehabilitation service (n=37)
DISCUSSION
Overall, HSM of telemedicine (where teleconsultations are provided using EHR-based video conference mode enabled for the synchronous mode) was found technically and operationally feasible in a developing country like India. We used collaborative care model where patients are seen/discussed with respective district hospitals clinician in live, real-time video conference mode on average for about 15–20 min. Overall, we have rehabilitation specialist clinicians at our center, who provide consultation and make appropriate referral whenever required, to the clinician at the district hospital. Availability of technicians ensures further support in the operation and resource feasibility of the model.
There is a large treatment gap in neurorehabilitation service in the country in view of limited resources and manpower. The biggest advantage of this model is reducing treatment gap by providing health service at the doorstep, especially to unreached needy patients. This model eventually reduces health cost burden and reduces health and time gap to reach experts in the field. Telemedicine makes universalization of health services accessible to patients in their vicinity. It also helps in providing consultation services, education and training to the patients’ families, and follow-up and monitoring of teleservices. It is considered as an alternative model in health care, which addresses and minimizes the barriers of distance, time, and cost and in turn promotes quality of life of the patients in their environment such as home, community, and workplace.
Even though this model was started in liaison with all district hospitals of Karnataka, only four (13.3%) districts have utilized the services so far, which suggests a communication gap and scope for improvement for effective collaboration and multidisciplinary approach in delivering quality service to unreachable patients. Patients, who were provided consultations in the study, were suffering from neurological disorders ranging from acute to chronic illnesses such as cerebral palsy, stroke, low backache, spinal cord injury, Guillain–Barre syndrome, IVDP, and tuberculosis of the spine. Patients with similar illness profile requiring TNR and inpatient neurorehabilitation have been reported worldwide and in India by some studies in the recent past.[15,21,22]
Another disappointing observation in the present study was 12 patients who were referred for Neurology and Neurosurgery consultation in other hospitals, which could have been done in our institute, which boasts to have one of the best Neurology and Neurosurgery departments in the country. It can be attributed to lack of coordination in cross-consultation in telemedicine services within the institute.
The present study provides data on TNR service in India. Poor follow-up was observed in the study. This can be attributed to multiple factors such as inadequate focus on our part, clinicians in the district hospital taking care of follow-up of the referred cases and patients not reporting back to us and drop out from district hospital health services and patients seeking treatment elsewhere.
There are multiple challenges and potential barriers to TNR practice, the primary concerns being privacy and confidentiality while providing teleservice. There is limited research on tele-rehabilitation with respect to policy issues, licensure, privacy, confidentiality, and cross-cultural acceptance of services.[23] Government support is needed for strengthening TNR services through logistics, surveillance, and service delivery. The researchers should also focus on capacity building for a strong interdisciplinary workplace through multisectorial approach for better service delivery.[24]
Strengths and limitations
This study provides a data on TNR outpatient consultation and academic training service from India. However, the study has limitations such as small sample size and outpatient consultation only. Another limitation is small number of district hospitals in the entire state utilizing tele-rehabilitation services.
Implication
With effective collaboration with district hospitals’ clinicians/staff, specialists at the tertiary/quaternary care center and telemedicine department can help in treatment and rehabilitation of needy population and universalize health into all sectors. The prospective research in this area on the effectiveness of conventional models, economic, cost-effectiveness, legal implication on care, and acceptability of model by patients, caregiver, and professionals is desirable and is the need of the hour.
CONCLUSION
This file review findings and 4-year experience indicate that TNR services are feasible, effective, and less resource intensive in delivering quality telemedicine care in a developing country like India. More clinical studies are required to elucidate its full utility at different levels and in different parts of the country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Brennan DM, Mawson S, Brownsell S. Telerehabilitation: Enabling the remote delivery of healthcare, rehabilitation, and self management. Stud Health Technol Inform. 2009;145:231–48. [PubMed] [Google Scholar]
- 2.Larson EB, Feigon M, Gagliardo P, Dvorkin AY. Virtual reality and cognitive rehabilitation: A review of current outcome research. NeuroRehabilitation. 2014;34:759–72. doi: 10.3233/NRE-141078. [DOI] [PubMed] [Google Scholar]
- 3.Koh GC, Yen SC, Tay A, Cheong A, Ng YS, De Silva DA, et al. Singapore tele-technology aided rehabilitation in stroke (STARS) trial: Protocol of a randomized clinical trial on tele-rehabilitation for stroke patients. BMC Neurol. 2015;15:161. doi: 10.1186/s12883-015-0420-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jagos H, David V, Haller M, Kotzian S, Hofmann M, Schlossarek S, et al. A framework for (Tele-) monitoring of the rehabilitation progress in stroke patients: EHealth 2015 special issue. Appl Clin Inform. 2015;6:757–68. doi: 10.4338/ACI-2015-03-RA-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giordano A, Bonometti GP, Vanoglio F, Paneroni M, Bernocchi P, Comini L, et al. Feasibility and cost-effectiveness of a multidisciplinary home-telehealth intervention programme to reduce falls among elderly discharged from hospital: Study protocol for a randomized controlled trial. BMC Geriatr. 2016;16:209. doi: 10.1186/s12877-016-0378-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Luca R, Bramanti A, De Cola MC, Trifiletti A, Tomasello P, Torrisi M, et al. Tele-health-care in the elderly living in nursing home: The first Sicilian multimodal approach. Aging Clin Exp Res. 2016;28:753–9. doi: 10.1007/s40520-015-0463-8. [DOI] [PubMed] [Google Scholar]
- 7.Sharifi M, Behzadipour S, Salarieh H, Tavakoli M. Cooperative modalities in robotic tele-rehabilitation using nonlinear bilateral impedance control. Control Eng Pract. 2017;67:52–63. [Google Scholar]
- 8.Kizony R, Weiss PL, Harel S, Feldman Y, Obuhov A, Zeilig G, et al. Tele-rehabilitation service delivery journey from prototype to robust in-home use. Disabil Rehabil. 2017;39:1532–40. doi: 10.1080/09638288.2016.1250827. [DOI] [PubMed] [Google Scholar]
- 9.Díaz I, Catalan JM, Badesa FJ, Justo X, Lledo LD, Ugartemendia A, et al. Development of a robotic device for post-stroke home tele-rehabilitation. Adv Mech Eng. 2018;4:5–8.1687814017752302. [Google Scholar]
- 10.Mountain G, Wilson S, Eccleston C, Mawson S, Hammerton J, Ware T, et al. Developing and testing a telerehabilitation system for people following stroke: Issues of usability. J Eng Des. 2010;21:223–36. [Google Scholar]
- 11.Gerber CN, Kunz B, van Hedel HJ. Preparing a neuropediatric upper limb exergame rehabilitation system for home-use: A feasibility study. J Neuroeng Rehabil. 2016;13:33. doi: 10.1186/s12984-016-0141-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cary MP, Jr, Spencer M, Carroll A, Hand DH, Amis K, Karan E, et al. Benefits and challenges of delivering tele-rehabilitation services to rural veterans. Home Healthc Now. 2016;34:440–6. doi: 10.1097/NHH.0000000000000441. [DOI] [PubMed] [Google Scholar]
- 13.Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31:427–47. doi: 10.1080/09638280802062553. [DOI] [PubMed] [Google Scholar]
- 14.Ponte S, Gabrielli S, Jonsdottir J, Morando M, Dellepiane S. Monitoring game-based motor rehabilitation of patients at home for better plans of care and quality of life. Conf Proc IEEE Eng Med Biol Soc. 2015;2015:3941–4. doi: 10.1109/EMBC.2015.7319256. [DOI] [PubMed] [Google Scholar]
- 15.Rogante M, Grigioni M, Cordella D, Giacomozzi C. Ten years of telerehabilitation: A literature overview of technologies and clinical applications. NeuroRehabilitation. 2010;27:287–304. doi: 10.3233/NRE-2010-0612. [DOI] [PubMed] [Google Scholar]
- 16.Hailey D, Roine R, Ohinmaa A, Dennett L. Evidence of benefit from telerehabilitation in routine care: A systematic review. J Telemed Telecare. 2011;17:281–7. doi: 10.1258/jtt.2011.101208. [DOI] [PubMed] [Google Scholar]
- 17.Srinath Reddy K, Shah B, Varghese C, Ramadoss A. Responding to the threat of chronic diseases in India. Lancet. 2005;366:1744–9. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- 18.Gourie-Devi M. Organization of neurology services in India: Unmet needs and the way forward. Neurol India. 2008;56:4–12. doi: 10.4103/0028-3886.39304. [DOI] [PubMed] [Google Scholar]
- 19.Tyagi N, Aikat R, Pratap J. Tele-rehabilitation as an adjunct service for geri care: Reaching the unreached. Int J Sci Res. 2015;4:332–4. [Google Scholar]
- 20.Karnataka State Wide Area Network (KSWAN) [Last accessed on 2018 Feb 20]. Available from: http://www.ktkswan.gov.in/services.php .
- 21.Seelman KD, Hartman LM. Telerehabilitation: Policy issues and research tools. Int J Telerehabil. 2009;1:47–58. doi: 10.5195/ijt.2009.6013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nirmala BP, Janardhana N, Shari TM. Profile of patients availing neurological rehabilitation services in a super specialty tertiary care hospital. Indian J Neurosci. 2017;3:134–8. [Google Scholar]
- 23.McCue M, Fairman A, Pramuka M. Enhancing quality of life through telerehabilitation. Phys Med Rehabil Clin N Am. 2010;21:195–205. doi: 10.1016/j.pmr.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Khan F, Amatya B, Mannan H, Rathore FA. Neurorehabilitation in developing countries: Challenges and the way forward. Phys Med Rehabil Int. 2015;2:1–13. [Google Scholar]


