Abstract
Suicide is a major public health issue in Canada. The quality of health care services, in addition to other individual and population factors, has been shown to affect suicide rates. In publicly managed care systems, such as systems in Canada and the United Kingdom, the quality of health care is manifested at the individual, program and system levels. Suicide audits are used to assess health care services in relation to the deaths by suicide at individual level and when aggregated at the program and system levels.
Large health administrative databases comprise another data source used to inform population-based decisions at the system, program and individual levels regarding mental health services that may affect the risk of suicide. This status report paper describes a project we are conducting at the Institut national de santé publique du Québec (INSPQ) with the Quebec Integrated Chronic Disease Surveillance System (QICDSS) in collaboration with colleagues from Wales (United Kingdom) and the Norwegian Institute of Public Health.
This study describes the development of quality of care indicators at three levels and the corresponding statistical analysis strategies designed. We propose 13 quality of care indicators, including system-level and several population-level determinants, primary care treatment, specialist care, the balance between care sectors, emergency room utilization, and mental health and addiction budgets, that may be drawn from a chronic disease surveillance system.
Keywords: suicide, services, mental health care, large health administrative databases
Highlights
The quality of health care services affects suicide rates.
Health administrative databases may inform population-based decisions at three levels (individual, program, and system) by indicating service gaps. Addressing these gaps may improve strategies for suicide prevention.
Thirteen quality of mental health care indicators are proposed based on data from health administrative databases in Quebec; these data are available from the Quebec Integrated Chronic Disease Surveillance System.
The proposed indicators and determinants encompass primary care and specialist care, emergency room utilization, mental health and addiction budgets, unemployment rates and socioeconomic deprivation, among other factors.
Our approach is reproducible in other Canadian provinces.
Introduction
Suicide mortality is a major public health issue. Several studies show that this phenomenon is associated with the quality of health care services,1 as well as mental disorders, particularly depression.1,2 Surveillance plays an essential role in containing the burden of chronic diseases;3 however, prevention strategies to reduce suicide risk remain a challenge.4 To contribute to the prevention and potential reduction of suicide mortality, this status report paper establishes and delineates the development of quality of mental health care indicators using large health administrative databases. We describe how the use of these databases may be maximized in the Canadian context using the Quebec Integrated Chronic Disease Surveillance System (QICDSS) as a case study.
Conceptual framework of the untapped potential of linked health administrative databases for identifying suicide prevention avenues
From a public health perspective, there are four primary determinants of health status: i) genetics; ii) the environment; iii) lifestyle; and iv) healthcare services.5 These determinants also apply to suicide risk.6 The relevant information required to analyze mental health care in relation to suicide mortality is available from suicide audits7 and health administrative databases. Tansella and Thornicroft8 first proposed this type of conceptual framework using the latter, which included service data and patient-based information. These investigators applied the classic Donabedian’s medical services quality model9 to create a two-dimensional matrix: a temporal axis of the input-processes-outcomes and a geographical axis of the system-programindividual levels. In their model, suicide rates are outcomes at the system and program levels, and the suicide risk at the individual level. Budgets represent input at the system and program levels; the balance between primary and specialist services is a process indicator at the system and program levels; and the quality of follow- up after the detection of depression in primary care or after an admission for a suicide attempt is a process indicator at all levels. Other terminology has been used to refer to the program level, such as the Meso-level by Contandriopoulos, et al.,10 who also drew their approach from the seminal work of Donabedian.9
Table 1 presents our adaptation of the Tansella and Thornicroft8 model using the untapped potential of the large linked health administrative databases of the QICDSS to investigate quality of mental health care as a determinant of suicide.
Table 1. The three levels of the quality of mental health care services model.
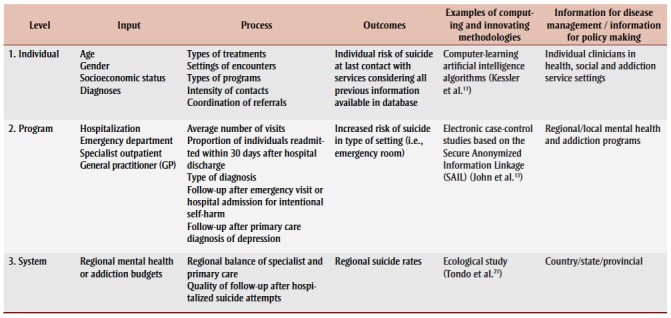 |
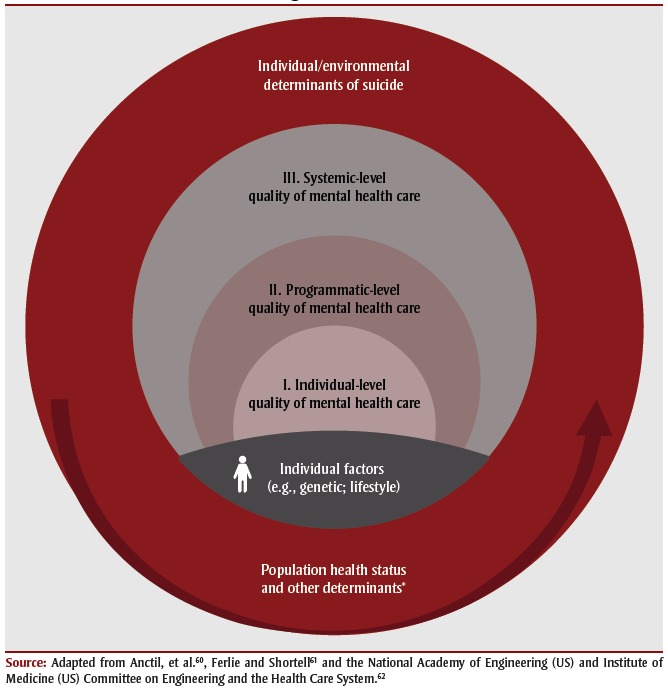
Each level presented in Table 1 refers to a representation of our conceptual framework of a three-level mental health care system, as shown in Figure 1. This system includes the individual, programmatic and systemic levels embedded within environmental determinants of suicide, population health status and other determinants.
Figure 1. Conceptual framework linking health care and determinants of suicide.
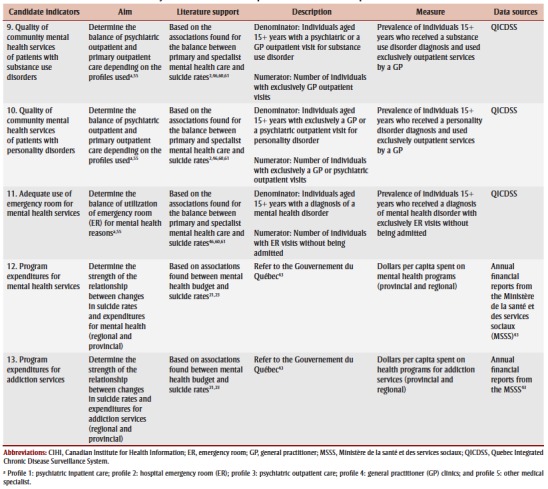
Risk factors at the individual level indicated in Table 1 may be used to conduct analyses that would produce algorithms of trajectories associated with a higher risk of suicide. These algorithms, thus, become indicators of the quality of care at the individual level within the available databases. The algorithms are complex to interpret, as demonstrated with the same databases as recent QICDSS trials in cardiovascular diseases.11,12 A set of largely used indicators of quality of care, such as those presented in the literature or Table 2, is considered in establishing the validity of the individual level-defined algorithms, such as audits that informed at the individual level or aggregated for the validity at the program and system levels. Established indicators of the quality of mental health care may be obtained from the literature at the programmatic and system levels, with potential candidates from the QICDSS proposed in Table 2. At the programmatic level, a casecontrol design between individuals who died by suicide and individuals who did not may be explored. These indicator outcomes should be worse among suicide cases in the year preceding their death than in non-cases with similar mental disorder diagnoses after controlling for other covariates.13 Finally, the system-level analysis suggested in Table 1 may employ identified risk factors from the two previous levels as indicators of the quality of mental health care, considering other risk factors as co-variates, if available, in the various linked health databases, and applicable at this level for the dependent variable of regional or provincial/state suicide rates.
Table 2. List of the candidate indicators at the programmatic and system levels supported by the health services and public health literature or practices.
|
Furthermore, suicide is believed to result from the interaction of different factors, including genetics14 and lifestyle/social factors,15,16 as illustrated in the other risk factors in Figure 1; several mental illnesses have genetic influences.17 However, there is no possibility, at this time, to measure genetic risk factors with linked health administrative databases. To accomplish this task, in the future, a reliable test may be discovered and recorded in the electronic medical records available for research.18,19
A brief history of the major initiatives
Previous courses of action have provided important information at each level identified in Figure 1. For example, aggregated individual suicide audits have demonstrated that acting on services may help prevent suicide, as reported by regions following the recommendations outlined in the National Confidential Inquiry into Suicide and Homicide by People with Mental Illness in England and Wales.20
Large health administrative databases may provide information relatively promptly for decisions at the system and program levels, whereas the value at the individual level remains experimental. There are reports regarding the examples identified in Table 1. For example, Kessler, et al.11 addressed individual-level factors and developed an actuarial risk algorithm to predict suicide in the 12 months following inpatient treatment of US Army soldiers for psychiatric disorders using data from the Historical Administrative Data System(HADS) of the Army Study to Assess Risk and Resilience in Service members (Army STARRS). Furthermore, this study relied on machine learning. The findings suggested that the strongest predictors included sociodemographic factors, criminal offenses, prior suicidality, aspects of prior psychiatric inpatient and outpatient treatment, and disorders diagnosed during the focal hospitalization. Similar experimental endeavors have been undertaken with Quebec’s linked health administrative databases by Najjar12 and a project underway in Wales, UK by co-authors John, et al.
At the program level, John, et al.13 developed a general population-based study of suicide mortality and mental health using routinely collected administrative databases and proposed a case-control design. The services provided were shown to determine the quality of care and define the program determinants of suicide mortality (i.e., general hospital admission; emergency department contact for selfharm and other indications including psychiatric admission and primary care contact in the year prior to probable suicide).
Finally, a system-level ecological study of suicide rates and assessment of mental health services was conducted by Tondo, et al.21 in the 50 US states. Their study indicated that a higher population density of psychiatrists and physicians and increased levels of federal aid for mental health were associated with lower suicide rates.22 Leff, et al.23 demonstrated that efficient mental health services predicted suicide reduction in a sample of publicly managed US facilities. The conceptualization and findings of these studies further substantiated the richness of the information available in administrative health databases used internationally. As suggested by While, et al.,20 the provision of mental health services may affect suicide rates in clinical populations, and investigations of these services in relation to suicide may help inform future suicide prevention efforts and improve safety for patients receiving mental health care.
Among the environmental and social determinants of suicide, in international and Canadian studies, the unemployment rate has been associated with suicide mortality. 24-28 Seminal work by Durkheim, the founder of modern sociology, at the end of the 19th century demonstrated that suicide rates are higher in socially and materially deprived areas, where the social capital for support and opportunities is lower.6
Large health administrative databases are available in Canada; however, there are few national and provincial studies that utilize them. Research in Alberta29 using a health services administrative database indicated that approximately 90% of individuals who die by suicide utilized a health service in the year prior to their death, and the majority visited a general practitioner (GP). Moreover, approximately 60% of these individuals had an emergency room (ER) visit, whereas only 39% of their peers had ER visit in the UK and Wales, as reported by Gairin, et al.30 At the national level, the Canadian Medical Association Journal (CMAJ) recently supported the value of large linked health administrative databases for suicide studies. However, it acknowledged the methodological and analytical challenges noted by Patrick,31 Quan and Williamson32 and the international research groups of Benchimol, et al.33 and Nicholls, et al.34 The main challenges raised were missing data and, for non-random missing data, variables that created incomplete or inadequate reporting of research based on routinely collected data.33
Delimitation of a conceptual framework in the Canadian context: health care services and suicide risk using big data
The creation and growth of national surveillance systems in Canada and their impact on chronic disease and injury prevention have been reviewed,35 with a primary focus on chronic physical conditions. Our conceptual framework considers health care services, particularly mental illness care to analyze suicide mortality and the possibility of obtaining a better understanding and prevention. Based on this conceptual framework, we will independently test each quality of care indicator (13 indicators). Our general hypothesis is that programs and systems that follow literature guidelines in terms of the quality of mental health care are less likely to present higher suicide rates than programs that do not follow guidelines (Table 2).
In Canada, one example of using mental health care service records from large linked health administrative databases is the QICDSS, from the province of Quebec. Our study was produced in collaboration with colleagues from Wales, UK13 and the Norwegian Institute of Public Health, and it may accelerate and validate gaps in the publicly managed care system regarding suicide.
QICDSS
The QICDSS was created by the Institut national de santé publique du Québec (INSPQ), which is a public health expertise and reference center that extracts data from five linked health administrative databases. The QICDSS includes all data from all individuals who suffer from one or more chronic diseases, including mental disorders. All mental disorder ICD codes are included, except for dementia. All cases of suicide reported by the coroner in the province of Quebec, whether individuals received a mental disorder diagnosis in the previous year or years, will be investigated.
The QICDSS includes, for all cases, the utilization of all services (hospitalization; emergency room; outpatient specialist; and general practitioners). The QICDSS has been updated annually since 1996.3 Blais, et al.3 assessed the essential features and strengths of the QICDSS and determined that it meets all basic requirements of a public health surveillance system.
Underreporting of mental health problems is often called into question; thus, databases and case definitions require validation before being used for epidemiological purposes36-39. Therefore, regarding the data quality of the QICDSS, it has been determined that psychiatrists and pediatricians entered the ICD-9 code in billing files in 95% of cases, and an internal medicine diagnosis code was indicated in 94% of claims.37,40 The literature indicates that diagnoses from recorded medical records fully correspond to the entries in administrative databases for other diseases in Quebec, as well as for other provinces.37,40In addition, Dodds, et al.41 reported that administrative health databases can clearly identify children with autism. In this context, the official data are considered largely reliable. To complement the data in the QICDSS, the determinants listed in Table 3 are provided by a provincial-level statistics organization42 and a government ministry.43
Table 3. List of environmental determinants.
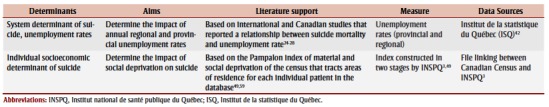 |
Candidate indicators
Table 2 summarizes each of the 13 quality of mental health care candidate indicators produced using the QICDSS and other data sources to specifically cover the determinants presented in our conceptual framework (Figure 1) and at the programmatic and system levels (Table 1).
Our 13 quality of care indicators are based on a literature review of health services research and practices from epidemiological studies. The indicators of receiving four or more visits for mental health in one year44 following a primary care physician first diagnosis of depression or substance abuse are drawn from US epidemiological studies that defined the quality of depression care or from guidelines for US family physicians for substance- abuse care at the primary care level. The 30-day readmission rate indicator of the quality of specialist care is based on the Canadian Institute of Health Information (CIHI),45 whereas the balance of specialist and primary care is based on countries with similar socioeconomic profiles and a publicly funded managed care system as Canada.46
Interpretation of the indicators proposed in Table 2 all point to a positive relationship with decreased suicide rates, excluding indicator 4, which is the 30-day readmission rate indicator from the CIHI original definition.45 For example, more expenditures on mental health and addiction services per capita would represent an indicator of the capacity to provide effective and timely services, whereas the two environmental determinants of a lower unemployment rate and a better social and material deprivation index would be expected to be associated with lower programmatic- and regional/provincial/statelevel suicide rates and variations. Other variables may be selected,* since the variables retained are the primary control variables included in analyses in the literature. Overall, by testing the 13 candidate indicators previously described, our aim is to determine the strength of the relationship between the changes in suicide rates and the program or system-level indicators of increased quality of mental health care at the provincial level and in each regional health territory, with consideration of the timeframe allowed for observation by the available linked health administrative databases.
Our work includes patient-centered information to capture the quality of primary care; however, some data are not recorded, such as family history and child abuse, specific treatments, and non-profit organization activities. In particular, the application of specific evidence-based treatments, such as anti-depressant medication and psychotherapy, are not currently available in the QICDSS; however, this information may be available in the future in Quebec or other jurisdictions. Nevertheless, as previously indicated, linking new health databases, such as medication or electronic medical records, may increase the potential determinants considered; however, these databases suffer from missing data or incomplete coverage of the population of interest.47 Moreover, primary care improvements in the late 1990s may have reduced suicide rates, and thus, it is difficult to estimate their effect. However, this remains important to note.48
Next steps: empirical testing of our theoretical framework
The next phase of the project focusses on conducting an empirical analysis to test our theoretical framework. Several statistical models will be tested to explore the relationship between changes in suicide rates and each individual, program and system level indicators of the 13 candidate indicators. The analyses will be performed at the provincial and regional levels. Two models will be considered: 1) a proportional hazard regression model (Cox regression) to investigate the associations between each of the 13 indicators and suicide; and 2) an ecological analysis to assess the association between the two environmental determinants, presented in Table 3, and suicide rates. There will be one model for each indicator – separately. The dependent variables for each Cox regression model will be suicide outcomes, and the exposure variables will be the 13 indicators. Because the indicators may change in value over the course of observation, the Cox regression is an appropriate model to account for timedependent variables.
The individual-level candidate indicators, covariates such as gender, age, comorbidity, and deprivation index,49 are available and will be integrated into the Cox regression models. Comorbidity will be adjusted at the individual level. Comorbidity refers to the physical conditions described in the Elixhauser comorbidity index.50 However, mental conditions, such as mood disorders, depression, substance abuse, personality disorders, psychoses and anxiety, will not be included because they are included in the proposed indicators. Furthermore, the Elixhauser index covers more diseases than the QICDSS. The latter covers chronic conditions that have a validated case definition using health administrative data. Some diseases, such as cancer and liver diseases, that are part of the Elixhauser Index, do not have a validated case definition using linked health administrative databases.
For candidate indicators at the regional level, mental health expenditures and the unemployment rate will also be included in the models. The ecological models will be linear models adjusted at the regional level for the unemployment rate and at the dissemination area-level for the socioeconomic deprivation index.
Ethics in the Canadian context: respecting access to documents held by public bodies and the protection of personal information
Ethical and legal issues in suicide research and the legal status of suicide have been reviewed in the literature,51,52 which highlights concerns regarding the context of common ethical perspectives, the acceptability of suicidal behaviors, and the obligations and limitations in intervening to prevent suicides. Specifically, in this study on suicide and mental health services, legitimate issues of confidentiality arise from the use of administrative databases.
The preliminary work of recording the various chronic diseases in a large database was completed by the INSPQ following authorization from the Commission d’accès à l’information du Québec (CAI). The INSPQ operates with strict access procedures and within secured zones. Only authorized programmers can directly access and extract data from the anonymized QICDSS databases. Other analysts and experts can access the unit for specific projects, and only aggregate results may be reported.3 Greater access and collaboration with academic institutes may help accelerate the use of and resolve the difficulty in computing the information. The QICDSS sends aggregate data to the Canadian Chronic Disease Surveillance System (CCDSS) of the Public Health Agency of Canada (PHAC), which has produced two interactive reports on overal mental disorders and anxio-depressive disorders by province.53,54
National chronic disease surveillance: actions for suicide and issues for public health
Suicide is a complex phenomenon. The use of a large public health administrative database may provide further opportunities to identify gaps in care and promotion that may be integrated to inform decisionmakers as they develop population-based programs. The quality of care indicators defined in this paper support the national, regional and local activities of health advocates throughout Quebec using a web public health portal (InfoCentre). A substantial advantage of our approach is that it may be reproduced in other provinces and may be examined at the national level in Canada because the indicators may be readily obtained from provincial/territorial health administrative databases. All cases of an individual citizen dying by suicide are recorded by a coroner or the medical examiner system. This is the responsibility of each individual Canadian province and territory, and there is no overarching federal authority.55 Other countries with similar health care systems and access to large health administrative databases, such as the United Kingdom,13 have begun to examine the associations of mental health care services with suicide and how the innovative use of these data sources may improve prevention strategies. Moreover, a national registry database in Norway has been incorporated by the Norwegian Public Health Institute as part of the effort to monitor mental health and suicidal behaviour.56
Therefore, health administrative databases represent a substantive complement to suicide audits and other data sources by identifying opportunities for intervention services that may improve the prevention of suicide. With approximately 4000 deaths by suicide57 each year in Canada, our study will likely provide useful information for PHAC, Quebec (INSPQ) and other provinces.
For example, population levels of alcohol consumption or access to firearms.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Authors’ contributions and statement
AL, ER, and LT designed and conceptualized the work. LT, AL, ER, JL, EP, LR, AJ, AR, and KL, contributed to the analytical plan, and LR, LT, ER, and JL assessed the suggested statistical modeling for empirical testing. LT drafted the manuscript, and LT, ER, AL, JL EP, LR, AJ, AR, and KL edited and critically reviewed the manuscript. All authors approved the final manuscript for submission.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
References
- Blair-West GW, Mellsop GW, Annan ML, et al. Down-rating lifetime suicide risk in major depression. Acta Psychiatrica Scandinavica. 1997;95((3)):259–63. doi: 10.1111/j.1600-0447.1997.tb09629.x. [DOI] [PubMed] [Google Scholar]
- Cavanagh JT, Carson AJ, Sharpe M, et al, et al. Psychological autopsy studies of suicide: a systematic review. Psychological Medicine. 2003;33((3)):395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- Blais C, Jean S, Sirois C, et al, et al. Quebec Integrated Chronic Disease Surveillance System (QICDSS), an innovative approach. Chronic Dis Inj Can. 2014;34((4)):226–35. [PubMed] [Google Scholar]
- Suicide prevention framework (Internet) Government of Canada. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/suicide-prevention-framework.html. [Google Scholar]
- Bernard P, Lemay M, zina M, et al. Perspectives de recherche en santé des populations au moyen de données complexes. Institut national de Santé publique du Québec. :1–71. [Google Scholar]
- Lesage A, St-Laurent D, et al, et al. (Suicide prevention from a public health perspective) Lesage A, St-Laurent D, Gagné M, et al. 2012;37((2)):239–55. doi: 10.7202/1014954ar. [DOI] [PubMed] [Google Scholar]
- Lesage A, Seguin M, Guy A, et al, et al. Systematic services audit of consecutive suicides in New Brunswick: the case for coordinating specialist mental health and addiction services. Can J Psychiatry. 2008;53((10)):671–78. doi: 10.1177/070674370805301006. [DOI] [PubMed] [Google Scholar]
- Tansella M, Thornicroft G, et al. A conceptual framework for mental health services: the matrix model. Psychol Med. 1998;28((03)):503–08. doi: 10.1017/s0033291796005880. [DOI] [PubMed] [Google Scholar]
- Donabedian A, et al. The quality of care: how can it be assessed. JAMA. 1988;260((12)):1743–48. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Contandriopoulos AP, Champagne F, et al, et al. L’évaluation dans le domaine de la santé : concepts et méthodes. Contandriopoulos AP, Champagne F, Denis J-L, et al. 2000:517–39. [PubMed] [Google Scholar]
- Kessler RC, Warner CH, Ivany C, et al, et al. Predicting suicides after psychiatric hospitalization in US Army soldiers: the Army Study to Assess Risk and Resilience in Service members (Army STARRS) JAMA Psychiatry. 2015;72((1)):49–57. doi: 10.1001/jamapsychiatry.2014.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najjar A, Reinharz D, Girouard C, et al. A two-step approach for mining patient treatment pathways in administrative healthcare databases. Artif Intell Med. 2018:34–48. doi: 10.1016/j.artmed.2018.03.004. [DOI] [PubMed] [Google Scholar]
- John A, Dennis M, Kosnes L, et al, et al. Suicide Information Database-Cymru: a protocol for a population-based, routinely collected data linkage study to explore risks and patterns of healthcare contact prior to suicide to identify opportunities for intervention. BMJ Open. 2014;4((11)):e006780–48. doi: 10.1136/bmjopen-2014-006780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brezo J, Klempan T, Turecki G, North Am, et al. The genetics of suicide: a critical review of molecular studies. Psychiatr Clin North Am. 2008;31((2)):179–203. doi: 10.1016/j.psc.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Evans E, Hawton K, Rodham K, et al. Suicidal phenomena and abuse in adolescents: a review of epidemiological studies. Child Abuse Negl. 2005:45–58. doi: 10.1016/j.chiabu.2004.06.014. [DOI] [PubMed] [Google Scholar]
- Afifi TO, Taillieu T, Zamorski MA, et al, et al. Association of child abuse exposure with suicidal ideation, suicide plans, and suicide attempts in military personnel and the general population in Canada. JAMA Psychiatry. 2016;73((3)):229–38. doi: 10.1001/jamapsychiatry.2015.2732. [DOI] [PubMed] [Google Scholar]
- Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381((9875)):1371–9. doi: 10.1016/S0140-6736(12)62129-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman N, Halas G, Peeler W, et al, et al. From patient care to research: a validation study examining the factors contributing to data quality in a primary care electronic medical record database. BMC Fam Pract. 2015:11–9. doi: 10.1186/s12875-015-0223-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vezyridis P, Timmons S, et al. Evolution of primary care databases in UK: a scientometric analysis of research output. BMJ Open. 2016;6((10)):e012785–9. doi: 10.1136/bmjopen-2016-012785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- While D, Bickley H, Roscoe A, et al, et al. Implementation of mental health service recommendations in England and Wales and suicide rates, 1997–2006: a cross-sectional and before-and-after observational study. Lancet. 2012;379((9820)):a cross–sectional and before. doi: 10.1016/S0140-6736(11)61712-1. [DOI] [PubMed] [Google Scholar]
- Tondo L, Albert MJ, Baldessarini RJ, et al. Suicide rates in relation to health care access in the United States: an ecological study. J Clin Psychiatry. 2006:517–23. doi: 10.4088/jcp.v67n0402. [DOI] [PubMed] [Google Scholar]
- Rutledge R, Fakhry SM, Baker CC, et al, et al. A population-based study of the association of medical manpower with county trauma death rates in the United States. Ann Surg. 1994:547–63. doi: 10.1097/00000658-199405000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leff HS, McPartland JC, Banks S, et al, et al. Service quality as measured by service fit and mortality among public mental health system service recipients. Ment Health Serv Res. 2004;6((2)):93–107. doi: 10.1023/b:mhsr.0000024353.30425.ab. [DOI] [PubMed] [Google Scholar]
- Thibodeau L, Lachaud J, et al. Impact of economic fluctuations on suicide mortality in Canada (1926-2008): testing the Durkheim, Ginsberg and Henry and Short Theories. Death Stud. 2016;40((5)):testing the Durkheim, Ginsberg and Henry and Short Theories–107. doi: 10.1080/07481187.2015.1133727. [DOI] [PubMed] [Google Scholar]
- Ahlburg DA, Schapiro MO, et al. Socioeconomic ramifications of changing cohort size: an analysis of U.S. Demography. 1984;21((1)):97–108. [PubMed] [Google Scholar]
- Morrell S, Taylor R, Quine S, et al, et al. Suicide and unemployment in Australia 1907-1990. Suicide and unemployment in Australia 1907-1990. Soc Sci Med. 1993;36((6)):749–56. doi: 10.1016/0277-9536(93)90035-3. [DOI] [PubMed] [Google Scholar]
- Stack S, et al. Suicide: a 15-year review of the sociological literature. Suicide Life Threat Behav. 2000;30((2)):145–62. [PubMed] [Google Scholar]
- Yang B, Lester D, Yang CH, et al. Sociological and economic theories of suicide: a comparison of the U.S.A. Soc Sci Med. 1992;34((3)):333–4. doi: 10.1016/0277-9536(92)90275-u. [DOI] [PubMed] [Google Scholar]
- Morrison KB, Laing L, et al. Adults’ use of health services in the year before death by suicide in Alberta. Health Rep. 2011;22((3)):15–22. [PubMed] [Google Scholar]
- Gairin I, House A, Owens D, et al. Attendance at the accident and emergency department in the year before suicide: retrospective study. Br J Psychiatry. 2003:28–33. doi: 10.1192/bjp.183.1.28. [DOI] [PubMed] [Google Scholar]
- Patrick K, et al. Harnessing big data for health. CMAJ. 2016;188((8)):555–33. doi: 10.1503/cmaj.160410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quan H, Williamson T, et al. Guiding the reporting of studies that use routinely collected health data. CMAJ. 2016:559–60. doi: 10.1503/cmaj.151470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benchimol EI, Smeeth L, Guttmann A, et al, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLOS Med. 2015;12((10)):e1001885–60. doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholls SG, Quach P, Elm E, et al, et al. The REporting of Studies Conducted Using Observational Routinely-Collected Health Data (RECORD) statement: methods for arriving at consensus and developing reporting guidelines. PLOS ONE. 2015;10((5)):e0125620–60. doi: 10.1371/journal.pone.0125620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi BC, Wigle DT, Johansen H, et al, et al. Status report – Retracing the history of the early development of national chronic disease surveillance in Canada and the major role of the Laboratory Centre for Disease Control (LCDC) from 1972 to 2000. Choi BC, Wigle DT, Johansen H, et al. 2015;35((2)):35–44. doi: 10.24095/hpcdp.35.2.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hux JE, Ivis F, Flintoft V, et al, et al. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;25((3)):512–6. doi: 10.2337/diacare.25.3.512. [DOI] [PubMed] [Google Scholar]
- Jean S, Candas B, Belzile E, et al, et al. Algorithms can be used to identify fragility fracture cases in physician-claims databases. Osteoporos Int. 2012;23((2)):483–501. doi: 10.1007/s00198-011-1559-4. [DOI] [PubMed] [Google Scholar]
- Lambert L, Blais C, Hamel D, et al, et al. Evaluation of care and surveillance of cardiovascular disease: can we trust medico-administrative hospital data. Can J Cardiol. 2012;28((2)):162–8. doi: 10.1016/j.cjca.2011.10.005. [DOI] [PubMed] [Google Scholar]
- John A, McGregor J, Fone D, et al, et al. Case-finding for common mental disorders of anxiety and depression in primary care: an external validation of routinely collected data. BMC Med Inform Dec Mak. 2016:35–8. doi: 10.1186/s12911-016-0274-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouhoummane N, et al. Impact du diabète sur la mortalité à la suite d'une hospitalisation pour un premier infarctus aigu du myocarde au Québec. Université Laval. 2010 [Google Scholar]
- Dodds L, Spencer A, Shea S, et al, et al. Validity of autism diagnoses using administrative health data. Chronic Dis Can. 2009;29((3)):102–7. [PMC free article] [PubMed] [Google Scholar]
- Enquête sur la population active, 2012, adaptée par l'Institut de la statistique du Québec, 2016. Institut de la statistique du Québec. Available from: http://www.bdso.gouv.qc.ca/pls/ken/ken214_tabl_detl.page_detl?p_iden_tran=REERCZFKHN1573377857748,O%60uH&p_lang=1&p_id_raprt=1186. [Google Scholar]
- Rapport financier des établissements (AS-471 (M30)): Service de l'administration des banques de données; 2016 (updated 2015-01-28; cited 2016 Apr) Service de l'administration des banques de données. Available from: http://publications.msss.gouv.qc.ca/msss/document-001663/ [Google Scholar]
- Wang PS, Berglund P, Kessler RC, et al. Recent care of common mental disorders in the United States: prevalence and conformance with evidence-based recommendations. J Gen Intern Med. 2000;15((5)):284–92. doi: 10.1046/j.1525-1497.2000.9908044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CIHI. Ottawa(ON): 2013. A performance measurement framework for the Canadian health system. Available from: https://secure.cihi.ca/free_products/HSP_Framework_Technical_Report_EN.pdf. [Google Scholar]
- Pirkola S, Sund R, Sailas E, Wahlbeck K, et al. Community mental-health services and suicide rate in Finland: a nationwide small-area analysis. Lancet. 2009;373((9658)):147–153. doi: 10.1016/S0140-6736(08)61848-6. [DOI] [PubMed] [Google Scholar]
- The world health report 2000 - health systems: improving performance. World Health Organization. 2000 Available from: http://www.who.int/whr/2000/en/whr00_en.pdf?ua=1. [PubMed] [Google Scholar]
- Hutchison B, Strumpf E, et al, Milbank Q, et al. Primary health care in Canada: systems in motion. Milbank Q. 2011;89((2)):256–88. doi: 10.1111/j.1468-0009.2011.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pampalon R, Hamel D, Gamache P, et al, et al. A deprivation index for health planning in Canada. Chronic Dis Can. 2009;29((4)):178–91. [PubMed] [Google Scholar]
- University of Manitoba. Winnipeg(MB): Concept: Elixhauser Comorbidity Index (Internet) Available from: http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?conceptID=1436. [Google Scholar]
- Mishara BL, Weisstub DN, et al. The legal status of suicide: a global review. Int J Law Psychiatry. 2016:54–74. doi: 10.1016/j.ijlp.2015.08.032. [DOI] [PubMed] [Google Scholar]
- Mishara BL, Weisstub DN, et al. Ethical and legal issues in suicide research. Int J Law Psychiatry. 2005;28((1)):23–41. doi: 10.1016/j.ijlp.2004.12.006. [DOI] [PubMed] [Google Scholar]
- Lesage A, Emond VR, et al. Surveillance of mental disorders in Quebec: prevalence, mortality and service utilization profile. Lesage A, Emond VR [Google Scholar]
- Public Health Agency of Canada. Ottawa(ON): 2016. Report from the Canadian Chronic Disease Surveillance System: mood and anxiety disorders in Canada, 2016. [Google Scholar]
- Routhier D, Leduc N, Lesage AD, Benigeri M, et al. Service utilization by hospitalized suicide attempters with schizophrenia or depression in Montreal. Psychiatr Serv. 2012;63((4)):364–9. doi: 10.1176/appi.ps.201000405. [DOI] [PubMed] [Google Scholar]
- Reneflot A, et al. Presentation of the Norwegian Institute of Public Health: suicide research and prevention. Reneflot A [Google Scholar]
- Statistics Canada. Ottawa(ON): Table 102-0552 - Deaths and mortality rate, by selected grouped causes and sex, Canada, provinces and territories, annual, CANSIM 2016 (Internet) Available from: http://www5.statcan.gc.ca/cansim/a26. [Google Scholar]
- British Psychological Society & The Royal College of Psychiatrists. Leicester(UK): 2011. Alcohol-use disorders: diagnosis, assessment and management of harmful drinking and alcohol dependence. [PubMed] [Google Scholar]
- Pampalon R, Raymond G, et al. A deprivation index for health and welfare planning in Quebec. Chronic Dis Can. 2000;21((3)):104–13. [PubMed] [Google Scholar]
- Anctil H, Jobin L, Pigeon M, et al. La santéet ses déterminants : mieux comprendre pour mieux agir. Anctil H, Jobin L, Pigeon M. 2012 Available from: http://publications.msss.gouv.qc.ca/msss/fichiers/2011/11-202-06.pdf. [Google Scholar]
- Ferlie EB, Shortell SM, Milbank Q, et al. Improving the quality of health care in United Kingdom and the United States: a framework change. Milbank Q. 2001:281–315–13. doi: 10.1111/1468-0009.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid PP, Compton WD, Grossman JH, et al. National Academies Press (US) Washington(DC): 2005. A framework for a systems approach to health care delivery. [PubMed] [Google Scholar]


