Abstract
Background
The prevalence of obesity and type 2 diabetes continues to increase. These conditions disproportionately affect minorities and are associated with poor nutrition early in life. Current food-consumption patterns can inform pending dietary guidelines for infants and toddlers.
Objective
The aim of this study was to describe infant feeding, complementary feeding, and food and beverage consumption patterns of 0- to 23.9-mo-olds in the general population.
Methods
The Feeding Infants and Toddlers Study 2016 is a cross-sectional survey of caregivers of children aged <4 y. Dietary data were collected from a national random sample by using a 24-h dietary recall (n = 3235). The percentage of children consuming foods from >400 food groups was calculated. Differences in the percentage consuming between Hispanic, non-Hispanic white, and non-Hispanic black children aged 0–23.9 mo were evaluated with the use of ORs and 95% CIs.
Results
Eighty-three percent of 0- to 23.9-mo-olds (n = 2635) were ever breastfed, 34% of 0- to 3.9-mo-olds (n = 305) and 15% of 4- to 5.9-mo-olds (n = 295) were exclusively breastfed, and 24% of 12- to 14.9-mo-olds (n = 412) consumed breast milk on the day of the recall. Complementary foods were more likely to be introduced before 4 mo in formula-fed infants (27%) than in infants who did not consume formula (5%). Half of 4- to 5.9-mo-olds consumed iron-fortified infant cereal, but few consumed iron-rich meats. Among toddlers (12–23.9 mo; n = 1133), >20% consumed no servings of fruit or vegetables on the day of the recall, approximately half consumed 100% fruit juice, and one-quarter to one-third consumed a sugar-sweetened beverage (SSB).
Conclusions
Breastfeeding initiation and duration have improved, but exclusivity remains low. Low consumption of iron-rich foods, fruit, and vegetables and lack of variety in vegetable consumption are problems. Efforts to reduce the consumption of SSBs and 100% fruit juice are warranted in early childhood.
Keywords: Feeding Infants and Toddlers Study, FITS 2016, food intakes, breastfeeding, eating habits, young children, disparities
Introduction
Approximately 8% of US infants <2 y old have high weight relative to recumbent length (1), and 14% of 2- to 5-y-olds are obese (2). Obesity at age 5 y is a strong predictor of obesity in early adolescence (3). Breastfeeding is associated with a lower risk of later development of overweight, obesity, and type 2 diabetes (4, 5); however, some studies have questioned the association between breastfeeding and lower risk of other health outcomes, such as cholesterol and blood pressure (4, 6). The relation between age of introduction of complementary foods, however, and later development of overweight and obesity is not consistent (5). The identification of the foods and dietary behaviors that may contribute to excess caloric
intake can offer insights into dietary strategies to prevent obesity and other poor health outcomes. In addition, previous studies have shown that low-income and some minority populations are disproportionately affected by these poor health outcomes (7–12). Consequently, an exploratory consideration of potential racial/ethnic differences in dietary intake may help to guide further research and policy discussions to support more vulnerable populations.
The American Academy of Pediatrics (AAP) has provided comprehensive recommendations for early feeding practices for children <2 y old. Optimal breastfeeding behaviors recommended by the AAP include exclusive breastfeeding for the first 6 mo of life and continued breastfeeding until ≥12 mo (9). Breastfeeding reduces the risks of sudden infant death syndrome, infectious diseases, asthma, obesity, and type 2 diabetes (13–18), all of which disproportionately affect minority children (12, 19–21). Model estimates of the excess disease cases, deaths, and costs attributable to suboptimal breastfeeding are substantial for both mothers and infants in the United States. For example, estimates are that optimal breastfeeding could prevent >700 child deaths in the United States annually (22). National breastfeeding rates remain low, particularly the rate of exclusive breastfeeding in the first 6 mo of life (23). Furthermore, low-income minority women, especially non-Hispanic black (NHB) mothers, breastfeed at lower rates than their non-Hispanic white (NHW) counterparts (24, 25).
The AAP Committee on Nutrition recommends the introduction of complementary foods between 4 and 6 mo of age (26, 27). At this age, breast milk alone is typically no longer sufficient to meet an infant's nutritional requirements without the introduction of other foods and liquids (complementary foods). The introduction of complementary foods represents a critical transition from the largely milk-based infant diet to a diet primarily based on the foods eaten by the rest of the family by the time the child is 18–24 mo old (28). The choice of complementary foods may affect intakes of essential nutrients that older infants and toddlers may underconsume, such as iron and vitamin D, as well as nutrients that are often consumed to excess, such as sodium. Small studies have reported that complementary feeding practices are more likely to depart from the AAP recommendations for minority children (29), but only limited nationally representative data are available to adequately quantify these differences (30).
Despite the links between early nutrition and health outcomes, national data on early feeding practices are largely absent from the literature. Furthermore, the Dietary Guidelines for Americans, first issued in 1980, have not yet covered children aged 0–24 mo (the so-called “Birth to 24” or “B-24” age group). However, the first B-24 recommendations are expected to be released in the 2020–2025 Dietary Guidelines for Americans (31).
The Feeding Infants and Toddlers Study (FITS) is a unique survey that provides national estimates of early feeding behaviors, including breastfeeding and introduction of complementary foods, which can inform the development of dietary guidelines for the B-24 age group. Previous FITS studies reported that the prevalence of children who were “ever breastfed” was 76% ± 1.1% (mean ± SE) in 2002 and modestly higher in 2008 (80% ± 1.5%). Those studies also report that infant cereal was introduced between 4 and 6 mo for only 65% of infants in 2002 and 50% in 2008 (32). The consumption of fruit and vegetables was substantially lower than recommendations in previous studies as well, with 15–30% of infants and toddlers >6 mo old consuming no fruit and 25–30% consuming no vegetables on the day of the survey in both the FITS 2002 and 2008 (32).
The aim herein is to provide a cross-sectional description of the breastfeeding practices, the use of human-milk substitutes, and complementary feeding behaviors among 0- to 23.9-mo-olds from the FITS 2016. In addition, exploratory analyses were performed to identify potentially important racial/ethnic differences. These results can inform the development of US dietary guidelines for children aged <2 y and lead to recommendations to optimize both breastfeeding and complementary feeding practices among the general population and, potentially, minorities. In addition, these findings can be used to indicate avenues for future research, such as the development of hypotheses to explore in the analysis of FITS 2002, 2008, and 2016 to compare trends over time.
Methods
FITS survey methods
A detailed report of the FITS 2016 design and methodology is reported elsewhere in this supplement issue (33). Briefly, the FITS 2016 is a national cross-sectional survey designed to collect data on the food and beverage intake, using the 24-h recall method, among children <4 y old living in the 50 states and Washington, DC. This method enables subsequent estimation of food and nutrient intakes on the day of the survey. Details of the questionnaire development and testing, sampling, and data collection methodology largely replicate the methods used in previous FITS surveys conducted in 2008 and 2002 (34, 35), with some updates to the food classification scheme. The questionnaires from 2008 were used in 2016 with minor modifications and the addition of some new data items (none of which are reflected in this article). The sample for FITS 2016 was identified through stratified random sampling from 4 sampling frames to obtain target sample sizes in cells defined by 12 age groups. In addition, a secondary objective of the target sample frames was to obtain adequate cell sizes within each of the 12 age groups of children participating in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Sampling weights were calculated to account for the probability of household selection and then adjusted for nonresponse and incomplete coverage by calibration to reflect the US population <4 y old. This article focuses on food consumption patterns of 0- to 23.9-mo-olds (n = 2635). Supplemental Table 1 shows the unweighted demographic details on the sample compared with the US population.
Data collection
The full survey instrument comprised a screener questionnaire to identify eligible participants, a recruitment questionnaire consisting of sociodemographic and lifestyle questions (e.g., physical activity, television viewing, and sleep habits), a feeding-practices questionnaire (e.g., breastfeeding practices, introduction of complementary foods), and one 24-h dietary recall (n = 3235). A random subsample of 25% (n = 799) of the total sampled population provided a second 24-h dietary recall to estimate within-person variance. The instrument was reviewed and approved by the institutional review boards of RTI International, the University of Minnesota Nutrition Coordinating Center, and the Docking Institute of Public Affairs, Fort Hays State University.
The dietary recall interviews were conducted by telephone and administered by certified interviewers using multiple-pass 24-h recall methodology and the Nutrition Data System for Research (NDSR, version 2015: University of Minnesota, Minneapolis, Minnesota). Interviews were conducted with the parent or caregiver primarily responsible for feeding the child, and a form was provided to assist the parent in collecting dietary recall data from daycare centers and other caregivers where the child may have spent part of the day. Only 13% of meals reported were consumed when the child was not with the respondent for part of the 24-h recall period.
Data analysis
All foods and beverages reported in the 24-h dietary recalls were assigned to food groups developed for the study. These were based on the food-grouping system previously developed for FITS 2008 (35), but updated in 2016 to align with food groups from the USDA's What We Eat in America survey (36) and to account for foods and beverages consumed by infants and young children. Estimation of breast-milk volumes replicated the methods used in previous FITS surveys: for infants <12 mo, these were based on defined amounts by age, adjusted for the total volume of other milks consumed during the recall day; for children aged ≥12 mo, these were based on volume per feeding (35). The estimated percentage of children consuming specific foods or food groups was calculated on the basis of a single 24-h dietary recall, which has been confirmed elsewhere as appropriate for estimation at the population level (37). SAS software (version 9.3; SAS Institute) and SAS-callable SUDAAN software (release 11; RTI International) were used to incorporate sample weights and produce point estimates and SEs that reflect the US population of children aged birth to 47.9 mo.
If there were ≥30 consumers and nonconsumers in each of the 3 largest race/ethnicity groups (Hispanic, NHW, NHB), we performed exploratory analyses (i.e., we did not start with a specific hypothesis) to assess whether consumption patterns differed between race/ethnicity groups. We highlight occurrences where the difference in the percentage consuming a given food between 1 race/ethnicity group (the comparison group) and the other 2 groups is large and the 95% CI for the OR for the comparison group compared with the other 2 groups does not contain the null value of 1.
Results
In this section, the results are presented first in relation to the general population, followed by selected findings according to racial/ethnic differences. Findings for the percentage of the general population (i.e., regardless of racial/ethnic group) consuming are presented for selected food groups in 3-mo intervals for infants aged <6 mo, and in 6-mo intervals for infants aged ≥6 mo and toddlers. The interested reader may find additional results for the general population in 3-mo intervals for infants >6 mo old and toddlers in Supplemental Table 2, and results for more food groups, and by race/ethnicity, in Supplemental Table 3 for infants (aged 0–11.9 mo) and in Supplemental Table 4 for toddlers.
Breastfeeding and breastfeeding alternatives
On the basis of responses to the feeding-practices questionnaire, which asked about practices not limited to the day of the recall, ∼85% of 0- to 11.9-mo-olds were ever breastfed (Supplemental Table 1). Nearly 60% of 0- to 3.9-mo-olds were currently breastfeeding at the time of the survey, as well as almost half of 4- to 5.9- and 6- to 8.9-mo-olds and more than one-third of 9- to 11.9-mo-olds (Figure 1, Table 1). The prevalence of exclusive breastfeeding was much lower than that of current breastfeeding: 34% of 0- to 3.9-mo-olds and 15% of 4- to 5.9-mo-olds and <5% of 6- to 8.9-mo-olds and 9- to 11.9-mo-olds were exclusively breastfed (Figure 1). Findings from the 24-h recall showed that results for the percentage consuming breast milk on the day of the recall were very similar to the percentage currently breastfeeding from the feeding-practices questionnaire: 58% of 0- to 3.9-mo-olds consumed breast milk on the day of the recall, as well as 44% of 4- to 5.9- and 6- to 8.9-mo-olds, 34% of 9- to 11.9-mo-olds, and nearly one-quarter of 12- to 14.9-mo-olds; by 21–23.9 mo, <5% were consuming breast milk (Table 2).
FIGURE 1.
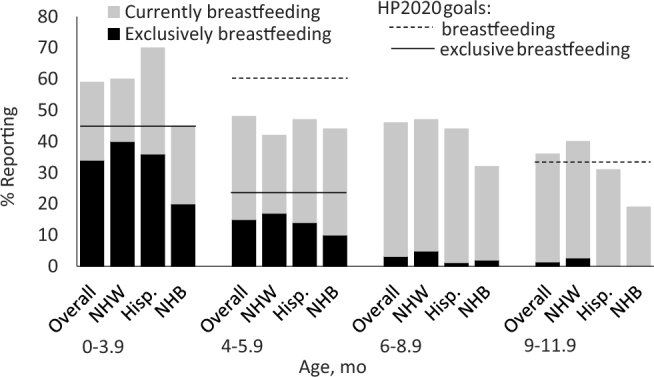
Current and exclusive breastfeeding rates by race and ethnicity, from FITS 2016 feeding practices questionnaire. Lines represent HP 2020 goals (38) for exclusive breastfeeding at ages 3 (0–3.9-mo columns) and 6 (4–5.9-mo columns; solid line) mo and for any breastfeeding at ages 6 (4–5.9-mo columns; dashed line) and 12 (9–11.9-mo columns) mo. No HP 2020 goals are set for breastfeeding at age 9 mo. See Table 1 for sample sizes. FITS, Feeding Infants and Toddlers Study; Hisp., Hispanic; HP, Healthy People; NHB, non-Hispanic black; NHW, non-Hispanic white.
TABLE 1.
Sample sizes by race/ethnicity for infants aged 0–11.9 mo1
| Sample size, n | ||||
|---|---|---|---|---|
| Child's age, mo | Overall | NHW | Hispanic | NHB |
| 0–3.9 | 305 | 198 | 49 | 38 |
| 4–5.9 | 294 | 191 | 47 | 38 |
| 6–8.9 | 465 | 318 | 62 | 62 |
| 9–11.9 | 430 | 294 | 63 | 51 |
TABLE 2.
Consumption of breast milk, infant formula, and cow milk during a single 24-h dietary recall: general population, children aged 0–23.9 mo1
| Child's age, mo | ||||||||
|---|---|---|---|---|---|---|---|---|
| Food group | 0–3.9 (n = 305) | 4–5.9 (n = 295) | 6–8.9 (n = 468) | 9–11.9 (n = 434) | 12–14.9 (n = 412) | 15–17.9 (n = 308) | 18–20.9 (n = 251) | 21–23.9 (n = 162) |
| Breast milk | 58 | 44 | 44 | 34 | 24 | 12 | 5.5 | 4.7 |
| Infant formula | 59 | 69 | 67 | 63 | 12 | 3.1 | 1.6 | 0.5 |
| Any cow milk2 | 1.8 | 2.0 | 3.7 | 17 | 78 | 84 | 83 | 86 |
| Whole | 1.4 | 1.2 | 1.5 | 10 | 67 | 71 | 71 | 58 |
| Reduced-fat | 0 | 0.7 | 1.4 | 5.6 | 11 | 10 | 13 | 23 |
| Low-fat | 0.4 | 0 | 0.8 | 1.5 | 3.2 | 3.3 | 3.5 | 9.0 |
| Nonfat | 0 | 0.2 | 0 | 0.2 | 1.7 | 2.4 | 3.6 | 2.5 |
Values are mean percentages of children (regardless of race/ethnicity) consuming the food category during a single 24-h recall.
Includes all fat levels, as well as flavored, unflavored, or powdered.
Approximately two-thirds of infants (aged <12 mo) consumed infant formula on the day of the survey (Table 2). The percentage consuming was much lower among toddlers, with only 12% of 12- to 14.9-mo-olds and <4% of 15- to 23.9-mo-olds consuming formula. Less than 4% of 0- to 8.9-mo-olds but 17% of 9- to 11.9-mo-olds consumed cow milk (Table 2). Among toddlers, cow milk was consumed by 78–86%, with most consuming whole milk (58–71%), some consuming reduced-fat milk (10–23%), and few consuming low-fat or nonfat milk (<4% except for 12- to 23.9-mo-olds who consumed low-fat milk, 9%) (Table 2).
Introduction of complementary foods (infants aged 0–5.9 mo)
Seventeen percent of 0- to 3.9-mo-olds and 73% of 4- to 5.9-mo-olds consumed a complementary food on the day of the recall, and those who consumed any formula (regardless of whether they also consumed breast milk) were more likely to consume complementary foods than those who consumed no formula (i.e., exclusively breastfed) (Table 3). Few 0- to 3.9-mo-olds who consumed no formula consumed any complementary foods (5%), but 27% of 0- to 3.9-mo-olds receiving formula consumed complementary foods. The same pattern was observed for 4- to 5.9-mo-olds: 85% of infants receiving formula consumed complementary foods compared with 51% of infants not consuming any formula. However, 4- to 5.9-mo-olds receiving formula were less likely to consume potentially non–age-appropriate complementary foods (e.g., bread rolls, pretzels, hot dogs; foods that may be less nutrient dense, contain fewer developmentally important nutrients, or have a texture that is not developmentally appropriate for infants, unlike infant cereal and home-made or commercial puréed foods) compared with those consuming no formula (3.8% compared with 14%, respectively) (Table 3).
TABLE 3.
Consumption of complementary foods during a single dietary recall by breastfeeding status among children aged 0–5.9 mo1
| Children consuming, % | ||||||
|---|---|---|---|---|---|---|
| Age 0–3.9 mo | Age 4–5.9 mo | |||||
| Type of complementary foods | Overall (n = 305) | Consumed no formula (n = 139) | Consumed any formula2 (n = 162) | Overall (n = 295) | Consumed no formula (n = 100) | Consumed any formula2 (n = 192) |
| No complementary foods | 83 | 95 | 73 | 27 | 49 | 15 |
| Any complementary foods | 17 | 5 | 27 | 73 | 51 | 85 |
| Infant cereal only3 | 5.7 | 2.3 | 8.7 | 13 | 5.9 | 17 |
| Puréed baby foods4 | 6.4 | 0.8 | 11 | 53 | 31 | 64 |
| Other food or beverage5 | 4.6 | 1.8 | 6.9 | 7.3 | 14 | 3.8 |
Values are mean percentages of children consuming the complementary food category during a single 24-h recall.
Includes children who consumed both formula and breast milk as well as children who consumed formula and no breast milk.
Includes any kind of infant cereal, regardless of grain (i.e., rice, oat, quinoa, wheat, multigrain, or unknown grain).
Includes any puréed fruit, vegetable, or meat, whether commercial jarred baby food or homemade puréed fresh foods; child may also consume infant cereal in addition to these but does not consume other (not puréed) foods.
Includes any food that is not infant cereal or commercial or homemade puréed baby food.
Among 4- to 5.9-mo-olds, regardless of whether they received formula, the most commonly consumed complementary food was iron-fortified infant cereal (50%); few other grains were consumed (Figure 2). Baby-food fruits (excluding 100% juice) and baby-food vegetables, respectively, were the second and third most commonly consumed complementary foods in this age group (29% and 27%). Approximately 5% of 4- to 5.9-mo-olds consumed 100% fruit juice. Few 4- to 5.9-mo-olds consumed meats (many of which, such as beef, are iron rich) and other nondairy protein foods (4.3%); the most-commonly consumed sources of protein were other (nonmeat) foods (2.3%), whereas baby-food meats were the least consumed (1.1%) (Table 4). However, 6.7% consumed some type of dessert, sweet, or sweetened beverage.
FIGURE 2.
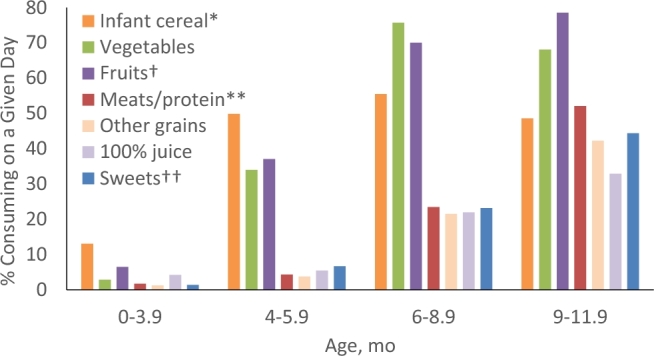
Percentages of infants consuming complementary foods by age, from FITS 2016 24-h dietary recall. *May include other grains; **excludes cheese and yogurt; †excludes fruit juice; ††includes sugar-sweetened beverages. See Table 1 for sample sizes. FITS, Feeding Infants and Toddlers Study.
TABLE 4.
Consumption of complementary foods during a single 24-h dietary recall: general population, children 0–23.9 mo1
| Child's age, mo | |||||
|---|---|---|---|---|---|
| Food group | 0–3.9 (n = 305) | 4–5.9 (n = 295) | 6–11.9 (n = 902) | 12–17.9 (n = 720) | 18–23.9 (n = 413) |
| Any grain products | 14 | 54 | 84 | 94 | 96 |
| Infant cereal2 | 13 | 50 | 52 | 16 | 5.3 |
| Family cereal3 | 0.6 | 1.1 | 20 | 50 | 58 |
| Baby finger foods4 | 1.1 | 4.4 | 33 | 16 | 5.7 |
| Any fruit5 | 6.5 | 37 | 74 | 75 | 79 |
| Any 100% fruit juice6 | 4.2 | 5.5 | 27 | 45 | 55 |
| Any vegetable7 | 2.9 | 34 | 72 | 73 | 71 |
| Baby-food vegetables8 | 1.5 | 27 | 45 | 8.7 | 2.5 |
| Vegetables (not baby food)9 | 0.9 | 7.6 | 29 | 58 | 60 |
| White potatoes10 | 0.7 | 2.7 | 15 | 33 | 32 |
| Any meat/other protein food11 | 1.7 | 4.3 | 41 | 88 | 91 |
| Baby-food meats | 0.2 | 1.1 | 4.2 | 0.9 | 0.6 |
| Meats (not baby food) | 1.1 | 1.3 | 26 | 68 | 72 |
| Other protein sources12 | 0.8 | 2.3 | 26 | 68 | 75 |
| Any sweets/sugar-sweetened beverage13 | 1.4 | 6.7 | 34 | 73 | 80 |
| Sugar-sweetened beverages | 0.1 | 2.3 | 8.5 | 27 | 31 |
| Savory snacks14 | 0.4 | 0.7 | 77 | 17 | 20 |
Values are mean percentages of children (regardless of race/ethnicity) consuming the food category during a single 24-h recall.
Includes any kind of baby-food cereal, regardless of grain (i.e., rice, oat, quinoa, wheat, multigrain, or unknown grain).
Includes any ready-to-eat or hot cereal that is not infant cereal.
Includes pretzels, crackers, rice cakes, and baby-food puffs.
Includes commercial and homemade puréed baby-food fruit and non–baby-food fruit; excludes 100% fruit juice.
Includes any 100% fruit juice regardless of whether it is specifically labeled for babies or not. Beverages that are <100% fruit juice are included in sugar-sweetened beverages.
Includes dark-green, orange, red, starchy, and other vegetables, whether baby food or not, as well as white potatoes.
Includes commercial and homemade puréed baby-food vegetables.
Includes non–baby-food dark-green, orange, red, starchy, and other vegetables; excludes baby food and white potatoes.
Includes fried potatoes, mashed potatoes and mixtures, and baked potatoes.
Includes meats and nonmeat sources of protein, including cheese and yogurt.
Includes dried beans and legumes; eggs; vegetarian meat substitutes; nuts, nut butters, and seeds; cheese; and yogurt.
Includes cakes, pies, chocolate/sweet cookies, bars, brownies, sweet rolls, doughnuts, muffins, and quick breads; frozen desserts, syrups, and sugar; as well as sugar-sweetened beverages.
Includes chips, corn chips, popcorn, snack mix, and puffs (non–baby food).
Consumption patterns of older infants (aged 6–11.9 mo)
Among 6- to 11.9-mo-olds, 84% consumed a grain-based food (Table 4), with iron-fortified infant cereal being the most common (52%), followed by grain-based baby finger foods (33%) and family (i.e., noninfant) cereal (20%). Approximately three-quarters consumed a serving of fruit (74%) or vegetables (72%). The most commonly consumed fruits (excluding 100% fruit juice) before 12 mo were apples, bananas, and pears; and the most commonly consumed vegetables were sweet potatoes, green beans, carrots, squash, and mashed potatoes/other potato mixtures (data not shown). Approximately 27% of 6- to 11.9-mo-olds consumed 100% fruit juice. Among 6- to 11.9-mo-olds, 41% consumed a meat or other protein, but <5% consumed baby-food meats. Nonbaby-food meats and other proteins were about equally likely to be consumed (26%). One-third of 6- to 11.9-mo-olds consumed sweets, including sugar-sweetened beverages (SSBs) (Table 4).
Consumption patterns of toddlers (aged 12–23.9 mo)
Most toddlers consumed some grain products (>90%), and approximately half consumed family (i.e., not infant) cereal (Table 4). For younger toddlers (aged 12–17.9 mo), more consumed unsweetened cereal than presweetened cereal (30% compared with 23%), but older toddlers (aged 18–23.9 mo) were equally likely to consume presweetened and unsweetened cereal (29% and 27%, respectively; Supplemental Table 4). After cereal, the most-commonly consumed grain-based foods among toddlers were bread, crackers, and rice and pasta (Supplemental Table 4).
Approximately three-quarters of toddlers consumed a fruit on the day of the survey, and a similar percentage consumed a vegetable (Table 4); however, if white potatoes are excluded, only ∼60% consumed a vegetable. Most fruits consumed were fresh fruits (Supplemental Table 4). The most-commonly consumed category of vegetables was white potatoes (∼33%), followed by red and orange vegetables (25%), other starchy vegetables (∼15%), dark-green vegetables (∼12%), and other vegetables (<3%) (Supplemental Table 4). Nearly half of 12- to 17.9-mo-olds and just over half of 18- to 23.9-mo-olds consumed 100% fruit juice (Table 4). The AAP (39) has recently recommended that children aged 1–3 y consume no more than 4 ounces (118 mL) of 100% fruit juice/d, but nearly one-quarter of 12- to 14.9-mo-olds and nearly half of 21- to 23.9-mo-olds exceeded this recommendation on the day of the recall (Table 5). At the time of the survey, the AAP recommendation was no more than 6 ounces (177 mL), and 14% of 12- to 14.9-mo-olds and 32% of 21- to 23.9-mo-olds exceeded that amount (Table 5).
TABLE 5.
Consumption of 100% fruit juice in excess of 2017 AAP-recommended amount of 4 ounces (118 mL) or 2001 AAP-recommended amount of 4–6 ounces (118–177 mL)/d in children aged 12–23.9 mo1
| Child's age, mo | ||||
|---|---|---|---|---|
| Amount consumed | 12–14.9 (n = 412) | 15–17.9 (n = 308) | 18–20.9 (n = 251) | 21–23.9 (n = 162) |
| >4 ounces (>118 mL) | 23 ± 2.9 | 31 ± 3.6 | 40 ± 4.0 | 46 ± 4.7 |
| >6 ounces (>177 mL) | 14 ± 2.2 | 23 ± 3.3 | 29 ± 3.8 | 32 ± 4.6 |
Values are mean ± SE percentages of children consuming more than the 2017 AAP-recommended 4 ounces (118 mL) of juice/d (39) or the 2001 AAP recommendation (40) [reaffirmed in 2006 (41) and in place at the time of the survey] of 4–6 ounces (118–177 mL)/d, during a single 24-h recall. AAP, American Academy of Pediatrics.
Approximately two-thirds of toddlers consumed meats, and about the same percentage consumed nonmeat protein foods (Table 4). The most-commonly consumed meat among both younger and older toddlers was chicken or turkey (39% of 12- to 17.9-mo-olds and 42% of 18- to 23.9-mo-olds), but cured meats were also consumed by more than one-quarter of toddlers (Supplemental Table 4). Beef lagged farther behind at just over 10%. The most commonly consumed nonmeat protein foods consumed by toddlers were cheese, eggs, yogurt, and nuts and nut butters (Supplemental Table 4).
Approximately three-quarters of toddlers consumed sweets and SSBs (Table 4). The most-commonly consumed solid sweets (i.e., not an SSB) were sweet bakery items (27% of 12- to 17.9-mo-olds and 36% of 18- to 23.9-mo-olds) and sugars, syrups, preserves, and jellies (22% of 12- to 17.9-mo-olds and 30% of 18- to 23.9-mo-olds; Supplemental Table 4). One-quarter to one-third of toddlers consumed an SSB on the day of the survey (27% of 12- to 17.9-mo-olds and 31% of 18- to 23.9-mo-olds; Table 4).
Notable differences by race/ethnicity
Infants (aged 0–11.9 mo)
Throughout the first year, NHB children were less likely than NHW and Hispanic infants to consume breast milk on the day of the recall (43% compared with 53–59%—OR: 0.63; 95% CI: 0.36, 1.12 for ages 0–5.9 mo; 22% compared with 36–42%—OR: 0.43; 95% CI: 0.26, 0.71 for ages 6–11.9 mo; Table 6). NHB 0- to 3.9-mo-olds and 4- to 5.9-mo-olds also had the lowest rates of exclusive breastfeeding (20% and 10%, respectively; Figure 1). Several notable differences by race and ethnicity were observed for specific grain products: NHB 6- to 11.9-mo-olds were much more likely than their NHW and Hispanic counterparts to consume baby-food puffs (14% compared with 27%; OR: 0.43; 95% CI: 0.24, 0.77) and ready-to-eat cereal (5% compared with 13–16%; OR: 0.33; 95% CI: 0.14, 0.77) (Table 6). Few other notable differences by race/ethnicity were observed for infants.
TABLE 6.
Consumption of selected foods during a single 24-h dietary recall, by race/ethnicity, in children aged 0–23.9 mo1
| Consumers,2 % | |||||
|---|---|---|---|---|---|
| Food group | Hispanic | NHW | NHB | Comparison group3 | OR (95% CI)4 |
| Age 0–5.9 mo | |||||
| n | 96 | 389 | 76 | — | — |
| Breast milk | 59 | 53 | 43 | NHB | 0.63 (0.36, 1.12) |
| Age 6–11.9 mo | |||||
| n | 125 | 612 | 113 | — | — |
| Breast milk | 36 | 42 | 22 | NHB | 0.43 (0.26, 0.71) |
| RTE cereal5 | 16 | 13 | 5.3 | NHB | 0.33 (0.14, 0.77) |
| Baby-food puffs | 27 | 27 | 14 | NHB | 0.43 (0.24, 0.77) |
| Age 12–23.9 mo | |||||
| n | 161 | 770 | 150 | — | — |
| Breast milk | 11 | 13 | 5 | NHB | 0.36 (0.18, 0.72) |
| Sugar-sweetened beverages | 28 | 25 | 45 | NHB | 2.31 (1.50, 3.57) |
| White potatoes6 | 28 | 30 | 46 | NHB | 2.03 (1.25, 3.30) |
| Cheese | 34 | 43 | 27 | NHB | 0.55 (0.35, 0.89) |
| Rice and pasta | 35 | 20 | 25 | Hispanic | 1.88 (1.06, 3.32) |
| Dried beans, peas, legumes | 14 | 9 | 8 | Hispanic | 1.84 (1.06, 3.20) |
| Eggs and egg dishes | 30 | 21 | 24 | Hispanic | 1.74 (1.14, 2.64) |
| Sweet bakery7 | 22 | 36 | 37 | Hispanic | 0.51 (0.31, 0.82) |
| Any fruit8 | 70 | 78 | 63 | NHW | 1.72 (1.20, 2.48) |
| Orange and red vegetables | 20 | 26 | 15 | NHW | 1.59 (1.08, 2.32) |
| Any 100% juice9 | 55 | 37 | 56 | NHW | 0.48 (0.35, 0.67) |
NHB, non-Hispanic black; NHW, non-Hispanic white; RTE, ready-to-eat.
Values are mean percentages of children consuming the food category during a single 24-h recall unless otherwise indicated.
The comparison group was the group with the highest or lowest percentage consuming among the 3 groups that was also the most different from the value of the middle group. For example, for dried beans, peas, and legumes, the group with the highest percentage consuming is Hispanic and the lowest is NHB; we chose Hispanic for the comparison group because the middle value (9%, NHW) is much closer to the value for NHB (8%) than the value for Hispanic (14%).
Values are ORs for the percentage consuming in the comparison group compared with the percentage consuming for the other 2 groups, and the 95% CI around the OR.
Includes any RTE cereal that is not infant cereal.
Includes fried potatoes, mashed potatoes and mixtures, and baked potatoes.
Includes cakes, pies, chocolate/sweet cookies, bars, brownies, sweet rolls, doughnuts, muffins, and quick breads.
Includes any fruit whether baby food or not; excludes 100% fruit juice.
Includes any 100% fruit juice regardless of whether it is specifically labeled for babies or not. Beverages that are <100% fruit juice are included in sugar-sweetened beverages.
Toddlers (aged 12–23.9 mo)
Beyond the first year, NHB toddlers continue to be less likely than NHW and Hispanic toddlers to consume breast milk (5% compared with 11–13%; OR: 0.36; 95% CI: 0.18, 0.72). In addition, NHB toddlers were more likely to consume SSBs (45% compared with 25–28%; OR: 2.31; 95% CI: 1.50, 3.57) and white potatoes (46% compared with 28–30%: OR: 2.03; 95% CI: 1.25, 3.30) than NHW and Hispanic toddlers and less likely to consume cheese (27% compared with 34–43%: OR: 0.55; 95% CI: 0.35, 0.89). Hispanic toddlers were almost twice as likely to consume rice and pasta (35% compared with 20–25%; OR: 1.88; 95% CI: 1.06, 3.32), eggs (30% compared with 21–24%; OR: 1.74; 95% CI: 1.14, 2.64), and dried beans and legumes (14% compared with 8–9%; OR: 1.84; 95% CI: 1.06, 3.20) than non-Hispanic toddlers (Table 6) and less likely to consume sweet bakery items (22% compared with 36–37%; OR: 0.51; 95% CI: 0.31, 0.82). NHW toddlers were more likely to consume fruit than NHB and Hispanic toddlers (78% compared with 63–70%; OR: 1.72; 95% CI: 1.20, 2.48) and red and orange vegetables (26% compared with 15–20%; OR: 1.59; 95% CI: 1.08, 2.32) and less likely to consume 100% fruit juice (37% compared with 55–56%; OR: 0.48; 95% CI: 0.35, 0.67). No notable differences were seen in the percentage of toddlers consuming any meats by race and ethnicity.
Discussion
The large sample of children <24 mo old studied in FITS 2016 provides the best current estimates of infant and toddler food and nutrient intake and allows us to make some comparisons by race and ethnicity. Several positive findings suggest that policy and public health initiatives may be changing infant and toddler feeding practices to better align with early-feeding recommendations. However, there is some evidence that these improvements have not been consistent. To put the results of FITS 2016 in context, we have compared our results with previously published data from past FITS surveys and other relevant studies in the following discussion. The comparisons to previous FITS surveys are not a statistically rigorous trend analysis in that they do not account for changes in food-group organization (which has evolved with each study iteration) or control for changes in the demographic characteristics of the US population over time.
Breastfeeding
There appears to have been a trend for both the initiation and duration of breastfeeding to have increased in the total population over the 3 FITS surveys. In 2016, 83% of 4- to 23.9-mo-olds were ever breastfed, compared with 80% in FITS 2008 and 76% in 2002 (32). The percentage of infants currently breastfed was also modestly higher than in 2008 for 4- to 5.9-mo-olds (42% in 2008, 48% in 2016) and 6- to 8.9-mo-olds (37% in 2008, 46% in 2016), and remained similar for 9- to 11.9-mo-olds (37% in 2008, 36% in 2016) (32). In addition, in FITS 2016, 2 of the Healthy People 2020 goals for breastfeeding (38) were met in the total population: the percentage of mothers initiating breastfeeding (Healthy People goal is 81.9%; result from FITS 2016 is 83%) and continuing to breastfeed at 12 mo (Healthy People goal is 34.1%; result from FITS 2016 is 36%). This success may be attributable to changing norms and cultural shifts in preferences to prolong nursing, as well as interventions intended to promote increased breastfeeding, such as the Baby Friendly Hospital Initiative (42). For example, 21% of US births in 2016 occurred in Baby Friendly facilities, compared with 3% in 2007.
Despite these gains, the prevalence and duration of exclusive breastfeeding still fall short of Healthy People 2020 goals (38) and AAP recommendations for exclusive breastfeeding until ∼6 mo and continued breastfeeding until ∼1 y (9). In addition, notable differences in breastfeeding behavior still exist by race and ethnicity. Although more infants overall continued to breastfeed in later infancy than in 2008, the prevalence was lower among minorities. Across all age categories, the prevalence of breastfeeding among NHB mothers was lower than the prevalence of breastfeeding among the total population. The prevalence of exclusive breastfeeding up to 6 mo was appreciably lower for NHB infants than for NHW and Hispanic infants. As such, the progress in overall breastfeeding initiation and the moderate success in extending breastfeeding duration mask important racial/ethnic differences and emphasizes the need to address these disparities. Previous research has shown that ∼60% of women stop breastfeeding earlier than they would like (43). Known barriers to breastfeeding include lack of family, peer, and health provider support; lack of social/cultural acceptance; inadequate knowledge; preference to bottle feed; difficulties around initiation (e.g., latching problems, breast discomfort); and the need to return to work (24, 44). Mothers who returned to work within 6 wk postpartum were 3 times as likely to stop breastfeeding before the recommended 6 mo, after adjusting for race, income, and education (45). Inequities in paid parental leave may further contribute to the breastfeeding disparity seen among low-income and racial minority groups (46).
Complementary foods
FITS 2016 also provides evidence of success in complementary feeding practices, such as timing of introduction of complementary foods, while signaling the need for improvement in others, such as low consumption of iron-rich foods, fruits, and vegetables and excess consumption of 100% fruit juice and SSBs.
Age of introduction of complementary foods
Similar to findings from NHANES 2009–2012 (47), the prevalence of the early introduction of complementary foods continues to decline, with only 17% infants <4 mo old being introduced to foods other than breast milk or formula in 2016. However, the introduction of complementary foods before 4 mo of age was considerably higher among infants who consumed any formula than among those who consumed no formula. The age of introduction of complementary foods and its association with overweight and obesity in later childhood remains equivocal, with only a few studies showing that early introduction before 4 mo of age may be associated with a higher BMI, whereas the majority of studies failed to show a relation between the age of introduction of complementary foods and later adiposity in childhood (5, 48, 49).
Consumption of iron-rich foods
Sixteen percent of 1- to 2-y-olds were reported in 2010 to be iron deficient (50), and evidence from longitudinal studies highlights some of the long-term cognitive impairments associated with iron deficiency in early childhood (51). Iron deficiency is caused by multiple factors, including insufficient intake, genetic factors affecting iron metabolism, and excessive losses. Both globally and in the United States, iron deficiency is common in young children (52). The AAP recommends that full-term infants who are partially or exclusively breastfed receive ∼1 mg Fe ⋅ kg−1 ⋅ d−1 starting at 4 to 6 mo, in the form of a liquid iron supplement, until iron-rich foods like iron-fortified infant cereal and iron-rich meats are introduced (50). In FITS 2008, 12% of 6- to 11.9-mo-olds consumed less than the Estimated Average Requirement for iron, an increase from 7% in FITS 2002 (53). Elsewhere in this supplement issue, FITS 2016 data show that figure has increased to 18% (52). In addition, among 6- to 11.9-mo-olds, only 15% consumed any type of supplement and <5% consumed iron supplements specifically (52). Iron-fortified infant cereal is often thought of as the first solid food introduced to infants. However, the consumption of iron-fortified infant cereal declined since 2008: 55% of 6- to 8.9-mo-olds in 2016 (Supplemental Table 2) compared with 82% and 79% in 2002 and 2008, respectively (32). This decline was not compensated for by the consumption of iron-rich puréed baby-food meats, which was also low and peaked at 5% among 6- to 8.9-mo-olds (Supplemental Table 2).
Another compounding contributor to iron deficiency in this age group is the early introduction and consumption of cow milk, which has been associated with gastrointestinal blood loss in infants from conditions such as food protein–induced allergic proctocolitis and cow-milk protein allergy (54, 55). The AAP recommends that parents avoid the introduction of cow milk before 12 mo (56). The prevalence of cow-milk consumption earlier than 12 mo remained at ∼17% of 9- to 11.9-mo-olds compared with FITS 2008 (32); however, those infants consuming cow milk tended to consume large quantities. These observations highlight the need for the continued education of caregivers about the avoidance of cow milk in the first year of life and the need for efforts to educate parents and caregivers of the sources and importance of iron in their child's diet.
Fruits, 100% fruit juice, and vegetables
Fruit and vegetable consumption for infants <9 mo old continued to increase or remain level. In FITS 2016, 70% of 6- to 8.9-mo-olds and 79% of 9- to 11.9-mo-olds consumed any fruit (Supplemental Table 2) compared with 65% and 81% in FITS 2008 (32), and 76% of 6- to 8.9-mo-olds and 78% of 9- to 11.9-mo-olds consumed any vegetable (Supplemental Table 2) compared with 63% and 72% in FITS 2008 (32). For toddlers, ∼80% consumed a fruit [a decrease somewhat from 85–90% in 2008 (32)] and ∼70% consumed a vegetable [about the same as in 2008 (32)]. Nonetheless, as with findings in NHANES (47) and FITS 2008 (32), the amount and variety of fruit and vegetable consumption remained far below recommendations in many older infants, and fell even shorter in toddlers. The AAP recommends offering a fruit or vegetable at every meal and snack after 6 mo (57). However, >20% of 12- to 23.9-mo-olds did not consume a single serving of fruit on the day of recall, and 30% did not consume any vegetable servings.
Several areas for improvement were noted with regard to types of fruits and vegetables consumed among 12- to 23.9-mo-olds. Although toddlers were about as likely to consume a serving of vegetable (71–74%; Supplemental Table 2) as a serving of fruit (71–81%), only ∼60% consumed a vegetable other than white potatoes, and approximately one-third consumed white potatoes.
Current studies have linked the consumption of fruits and vegetables to a decreased risk of several chronic diseases and obesity (15, 58–69), and early feeding preferences may persist throughout the life span (70). Innovative approaches to introduce and sustain the consumption of a variety of fruits and vegetables should be a high priority, not just for infant feeding but also for families.
In 2017, the AAP updated its position on fruit juice and recommended delaying the introduction of juice until 12 mo and limiting the maximum amount of juice for young toddlers to no more than 4 ounces (118 mL) of 100% fruit juice/d (58, 71, 72). However, at the time of the survey, the previous recommendation from the AAP allowed for no more than 4–6 ounces (118–177 mL) daily starting in late infancy. A recent meta-analysis concluded that the consumption of 100% fruit juice was associated with a small amount of excess weight gain in childhood (58). We found that infants and toddlers were somewhat less likely to consume 100% fruit juice in 2016 than in FITS 2008 (32), with the greatest decrease between 6 and 12 mo [e.g., for 6- to 11.9-mo-olds, the percentage consuming 100% juice fell from 31–41% in 2008 (32) to 22–33% in 2016; Supplemental Table 2]. However, one-third of 9- to 11.9-mo-olds still drank 100% fruit juice (Supplemental Table 2), which is not consistent with the most recent AAP recommendations to delay the introduction of fruit juice until 12 mo (39). Furthermore, nearly one-quarter of the youngest toddlers (12–14.9 mo) were consuming more than the new recommended maximum amount of 4 ounces (118 mL) of 100% fruit juice/d, and 14% were consuming more than the previously recommended maximum amount of 6 ounces (177 mL) (40). Nearly half of toddlers aged 21–23.9 mo were consuming >4 ounces (118 mL) and nearly one-third were consuming >6 ounces (177 mL)/d.
SSBs
The consumption of SSBs has increased for some age groups and decreased for others since 2008. In 2016, few younger infants (<6 mo) consumed SSBs, but among 9- to 11.9-mo-olds, the percentage consuming increased from 11% in 2008 (32) to 14% in 2016 (Supplemental Table 2) and doubled—from 14% in 2008 (32) to 28% in 2016 (Supplemental Table 2)—for 12- to 14.9-mo-olds. Peak consumption in 2016 was in 18- to 20.9-mo-olds (33% consuming an average of 106 kcal/consumer; Supplemental Table 2). Clearly, there is an opportunity to further delay the introduction of SSBs and to reduce consumption in late infancy and toddlerhood. There were racial/ethnic disparities in the consumption of SSBs: NHB toddlers were more likely to consume SSBs than NHW and Hispanic toddlers. Sugary drinks should be avoided because they contribute calories but few nutrients and may decrease the child's appetite for more nutritious foods. Moreover, the consumption of high-caloric-density foods and beverages in early childhood significantly increases the likelihood of consumption of these products later in childhood, increases the risk of dental caries, and may contribute to the prevalence of early childhood obesity (15, 60, 62, 63).
Study strengths and limitations
Data from the FITS 2016 can make an important contribution to early-childhood nutrition. The study provides population-level data and builds on previous FITS studies, which, in turn, can help us to monitor the diets of very young children in the United States. It can allow us to compare feeding practices to national recommendations and also contribute to new dietary guidelines for the population aged from birth to 2 y.
A potential limitation of the FITS 2016 study applies to all cross-sectional studies that use self-reported 24-h recall data, because they are subject to reporting bias and errors in remembering what and how much was consumed. Some of the race/ethnicity differences in food-consumption patterns that we found may be due to household economic and education status, access to food (related to geographic location; i.e., food deserts), and other social determinants rather than, or in addition to, race/ethnicity. Previous research has yielded conflicting conclusions about the role of race/ethnicity on breastfeeding. One study found that maternal education had a greater effect on breastfeeding incidence than race/ethnicity (73), whereas another reported that, even after accounting for socioeconomic status, NHBs were consistently less likely to breastfeed than were NHWs (74, 75). The analysis of differences between racial/ethnic groups was exploratory, because previous FITS studies did not present results by race/ethnicity, and we did not have any specific hypotheses we were testing. However, the race/ethnicity differences we report are largely consistent with the limited data available in the literature (47) and suggest that although national data are useful for documenting trends, it is critical that they take into account race/ethnicity during study design, data collection, and analysis. Future analyses are planned and include examining racial/ethnic differences in the FITS 2002 and 2008 surveys (informed by the results reported here) and conducting in-depth trend analyses.
Opportunities for future research
The most recent data from the FITS appear to indicate that we have found some improvements in breastfeeding practices and early introduction of complementary foods; however, several areas of concern remain. These include exclusive breastfeeding; timing of introduction of complementary foods, particularly in formula-fed infants; low consumption of iron-rich foods; early introduction of cow milk; inadequate quantity and variety of fruits and vegetables consumed; and early introduction and consumption of SSBs and 100% fruit juice in the first year of life. In addition, the racial/ethnic disparities in feeding practices highlighted herein may herald disparities in obesity and metabolic disorders later in life (22, 24, 76–78).
Factors that account for the departure from the feeding practices recommended by the AAP remain uncertain. The design of FITS 2016 and the substantial data collection necessary to describe patterns of food consumption limit somewhat our ability to measure and understand the underlying attitudes, beliefs, socioeconomic, and potential environmental factors that led to these patterns. Associated lifestyle factors that may influence consumption patterns will be explored in subsequent publications. Although dietary counseling by primary care providers is a part of routine care, the quality and effectiveness of such counseling may need to be strengthened to be inclusive of cultural preferences, practices, and access to nutritious and affordable foods. To our knowledge, the frequency, quality, and efficacy with which counseling routinely addresses practices such as avoiding the early introduction of solids or cow milk have not been carefully examined (79). Furthermore, we are not aware of any studies that have effectively addressed the substantial intake of high-caloric-density foods that may lead to the development of early obesity. FITS 2016 offers many opportunities to fill further data gaps in relation to the feeding of infants and toddlers. Future exploration of the meal, snack, and beverage patterns in this age group is planned, and it is hoped will shed light on potential obesogenic dietary patterns. In addition, examining food sources of nutrients could provide more insights into how foods selected by caregivers contribute to nutrient intakes, and allow for exploration of differences by race and ethnicity, WIC status, or socioeconomic status. Ongoing surveillance of early-childhood food and beverage consumption that accounts for race and ethnicity is needed to identify feeding patterns that may lead to future health problems early enough to intervene and change behaviors.
Across race and ethnicity, our results are largely consistent with the limited data available in the literature (47) and underline the need for focused education and policy changes to decrease some of the disparities observed in feeding practices and dietary intakes. Whether the differences in food-consumption patterns reflect cultural preferences, choices directed by access to food or food insecurity, or other social justice issues remains uncertain. These differences could also be due to household economic and education status rather than race and ethnicity. Our observations point to the need to tailor education and feeding guidance to specific racial and ethnic groups.
Conclusions
FITS 2016 provides the most recent cross-sectional estimates of food and beverage consumption for young children in the United States. The sample size of FITS permits exploration of racial/ethnic comparisons that have not previously been described, and although initial findings with regard to differences by race/ethnicity herein are exploratory, our data may set the stage for further research and provide important insights into guidance and interventions that are still needed in order to improve diets.
Supplementary Material
Acknowledgments
The study upon which the data presented here is based was a collaborative effort of many organizations and individuals, which are listed in the acknowledgments to the companion Methods and Study Design article (33). In addition, we acknowledge Johanna Dwyer (Tufts University and the NIH, Office of Dietary Supplements) and Virginia A Stallings (Children's Hospital of Philadelphia) for their guidance on current issues in evaluating food consumption. The authors’ responsibilities were as follows—ASA, DJC, and EFJ: designed the research; DJC: performed the statistical analysis; AAR, WHD, ACL, RC, ASA, and EFJ: analyzed or interpreted the data and wrote the manuscript; AAR: had primary responsibility for the final content; and all authors: read and approved the final manuscript.
Notes
Published in a supplement to The Journal of Nutrition. Select contents of this supplement were presented at the Experimental Biology 2017 conference in a session titled, “Informing B-24 Dietary Guidelines: Findings from the New Feeding Infants and Toddlers Study 2016,” held in Chicago, IL, April 22, 2017. Supplement Coordinators were William Dietz, Milken School of Public Health at the George Washington University and Andrea S Anater, RTI International. The FITS research was funded by Nestlé Research (Lausanne, Switzerland) through a contract with RTI International and its subcontractor, the University of Minnesota. Dr. Dietz is a compensated consultant to RTI on this project. The article contents are the responsibility of the authors and do not necessarily represent the opinions or recommendations of Nestlé. Publication costs for this supplement were defrayed in part by the payment of page charges. This publication must therefore be hereby marked “advertisement” in accordance with 18 USC section 1734 solely to indicate this fact. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of The Journal of Nutrition.
Supported by Nestlé Research, Lausanne, Switzerland.
Supplemental Tables 1–4 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn/.
Author disclosures: AAR, DJC, ACL, ASA, no conflicts of interest. EFJ is employed by Nestlé Research (funding source); RC is employed by Nestlé Nutrition. WHD has served on the Weight Watchers Scientific Advisory Committee and has received grant support from Bridgespan for analyses of NHANES.
Abbreviations used:
- AAP
American Academy of Pediatrics
- B-24
birth to 24 mo
- FITS
Feeding Infants and Toddlers Study
- NHB
non-Hispanic black
- NHW
non-Hispanic white
- SSB
sugar-sweetened beverage
References
- 1. Ogden C, Carroll M, Kit B, Flegal K. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311(8):806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ogden C, Carroll M, Lawman H, Fryar C, Kruszon-Moran D, Kit B, Flegal K. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016;315(21):2292–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cunningham S, Kramer M, Narayan K. Incidence of childhood obesity in the United States. N Engl J Med 2014;370(5):403–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Horta B, Loret de Mola C, Victora C. Long‐term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta‐analysis. Acta Paediatr 2015;104(S467):30–7. [DOI] [PubMed] [Google Scholar]
- 5. Patro-Gołąb B, Zalewski M, Kołodziej M, Kouwenhoven S, Poston L, Godfrey K, Koletzko B, van Goudoever J, Szajewska H. Nutritional interventions or exposures in infants and children aged up to 3 years and their effects on subsequent risk of overweight, obesity and body fat: a systematic review of systematic reviews. Obes Rev 2016;17(12):1245–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan L, Freedman D, Sharma A, Castellanos-Brown K, Park S, Smith R, Blanck H. Trends in obesity among participants aged 2–4 years in the Special Supplemental Nutrition Program for Women, Infants, and Children—United States, 2000–2014. MMWR Morb Mortal Wkly Rep 2016;65(45):1256–60. [DOI] [PubMed] [Google Scholar]
- 7. Isong IA, Rao SR, Bind M-A, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics 2018;141(1):e20170865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thompson A, Bentley M. The critical period of infant feeding for the development of early disparities in obesity. Soc Sci Med 2013;97:288–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. American Academy of Pediatrics, Section on Breastfeeding Policy statement: breastfeeding and the use of human milk. Pediatrics 2012;129(3):e827–41. [DOI] [PubMed] [Google Scholar]
- 10. Rendall M, Weden M, Fernandes M, Vaynman I. Hispanic and black US children's paths to high adolescent obesity prevalence. Pediatr Obes 2012;7:423–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Skinner A, Skelton J. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatr 2014;168(6):561–6. [DOI] [PubMed] [Google Scholar]
- 12. Wang Y, Beydoun M. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28. [DOI] [PubMed] [Google Scholar]
- 13. Dewey K, Heinig M, Nommsen-Rivers L. Differences in morbidity between breast-fed and formula-fed infants. J Pediatr 1995;126:696–70. [DOI] [PubMed] [Google Scholar]
- 14. Gartner L, Morton J, Lawrence R, Naylor A, O'Hare D, Schanler R, Eidelman A. Breastfeeding and the use of human milk. Pediatrics 2005;115(2):496–506. [DOI] [PubMed] [Google Scholar]
- 15. Pan L, Li R, Park S, Galuska D, Sherry B, Freedman D. A longitudinal analysis of sugar-sweetened beverage intake in infancy and obesity at 6 years. Pediatrics 2014;134(Suppl 1):S29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Slusser W. Breastfeeding and maternal and infant health outcomes in developed countries. AAP Grand Rounds 2007;18(2):15–6. [Google Scholar]
- 17. Hauck F, Thompson J, Tanabe K, Moon R, Vennemann M. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics 2011;128:103–10. [DOI] [PubMed] [Google Scholar]
- 18. Li R, Dee D, Li C-M, Hoffman H, Grummer-Strawn L. Breastfeeding and risk of infections at 6 years. Pediatrics 2014;134(Suppl 1):S13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Moorman J, Zahran H, Truman B, Molla M. Current asthma prevalence—United States, 2006–200 8. MMWR Suppl 2011;60:84–6. [PubMed] [Google Scholar]
- 20. Kitsantas P, Gaffney K. Racial/ethnic disparities in infant mortality. J Perinat Med 2010;38:87–94. [DOI] [PubMed] [Google Scholar]
- 21. Freedman D. Obesity—United States, 1988–2008. MMWR Suppl 2011;60:73–7. [PubMed] [Google Scholar]
- 22. Bartick M, Jegier B, Green B, Schwarz E, Reinhold A, Stuebe A. Disparities in breastfeeding: impact on maternal and child health outcomes and costs. J Pediatr 2017;181:49–55. [DOI] [PubMed] [Google Scholar]
- 23. CDC Breastfeeding Report card: progressing toward national breastfeeding goals, United States 2016. Atlanta (GA): CDC; 2016. [Google Scholar]
- 24. Jones K, Power M, Queenan J, Schulkin J. Racial and ethnic disparities in breastfeeding. Breastfeed Med 2015;10:186–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sparks P. Racial/ethnic differences in breastfeeding duration among WIC-eligible families. Womens Health Issues 2011;21:374–82. [DOI] [PubMed] [Google Scholar]
- 26. Holt K, Wooldridge N, Story M, Sofka D. Bright Futures nutrition. 3rd ed.Elk Grove Village; (IL): American Academy of Pediatrics; 2011. [Google Scholar]
- 27. American Academy of Pediatrics, Committee on Nutrition Complementary Feeding. In: Kleinman R, and Greer F, editors. Pediatric nutrition handbook. 6th ed Elk Grove Village (IL): American Academy of Pediatrics; 2009, 123–140. [Google Scholar]
- 28. WHO Global strategy for infant and young child feeding. Geneva (Switzerland): WHO; 2003. [Google Scholar]
- 29. Kuo A, Inkelas M, Slusser W, Maidenberg M, Halfon N. Introduction of solid food to young infants. Matern Child Health J 2011;15(8):1185–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fein S, Labiner-Wolfe J, Shealy K, Li R, Chen J, Grummer-Strawn L. Infant Feeding Practices Study II: study methods. Pediatrics 2008;122(Suppl 2):S28–35. [DOI] [PubMed] [Google Scholar]
- 31. Raiten D, Raghavan R, Porter A, Obbagy J, Spahn J. Executive summary: evaluating the evidence base to support the inclusion of infants and children from birth to 24 mo of age in the Dietary Guidelines for Americans—“the B-24 Project”. Am J Clin Nutr 2014;99(Suppl):663S–91S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Siega-Riz AM, Deming DM, Reidy KC, Fox MK, Condon E, Briefel RR. Food consumption patterns of infants and toddlers: where are we now? J Am Diet Assoc 2010;110(12):S38–51. [DOI] [PubMed] [Google Scholar]
- 33. Anater AS, Catellier DJ, Levine BA, Krotki KP, Jacquier EF, Eldridge AL, Bronstein KE, Harnack LJ, Lorenzana Peasley JM, Lutes AC. The Feeding Infants and Toddlers Study (FITS) 2016: study design and methods. J Nutr 2018;148:1516S–24S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Devaney B, Kalb L, Briefel R, Zavitsky-Novak T, Clusen N, Ziegler P. Feeding Infants and Toddlers Study: overview of the study design. J Am Diet Assoc 2004;104:8–13. [DOI] [PubMed] [Google Scholar]
- 35. Briefel RR, Kalb LM, Condon E, Deming DM, Clusen NA, Fox MK, Harnack L, Gemmill E, Stevens M, Reidy KC. The Feeding Infants and Toddlers Study 2008: study design and methods. J Am Diet Assoc 2010;110(12 Suppl):S16–26. [DOI] [PubMed] [Google Scholar]
- 36. Rhodes D, Adler M, Clemens J, Moshfegh A. What We Eat in America food categories and changes between survey cycles. J Food Comp Anal 2017;64:107–11. [Google Scholar]
- 37. Institute of Medicine, Food and Nutrition Board Dietary Reference Intakes: applications in dietary assessment. Washington (DC): National Academies Press; 2000. [PubMed] [Google Scholar]
- 38. US Department of Health and Human Services Healthy People 2020: Maternal, Infant, and Child Health Objectives MICH-21.1 through 21.5: Office of Disease Prevention and Health Promotion; 2010[updated 2012; cited 2018 Mar 26]. Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/Maternal-Infant-and-Child-Health/objectives. [Google Scholar]
- 39. American Academy of Pediatrics Where we stand: fruit juice 2017 [updated May 22, 2017; cited 2017 Jun 1]. Available from: https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Where-We-Stand-Fruit-Juice.aspx. [Google Scholar]
- 40. American Academy of Pediatrics, Committee on Nutrition The use and misuse of fruit juice in pediatrics. Pediatrics 2001;107(5):1210–3. [DOI] [PubMed] [Google Scholar]
- 41. American Academy of Pediatrics AAP publications retired or reaffirmed, October 2006. Pediatrics 2007;119(2):405. [Google Scholar]
- 42. Munn A, Newman S, Mueller M, Phillips S, Taylor S. The impact in the United States of the baby-friendly hospital initiative on early infant health and breastfeeding outcomes. Breastfeed Med 2016;11(5):222–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Odom E, Li R, Scanlon K, Perrine C, Grummer-Strawn L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics 2013;131(3):e726–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gross TT, Powell R, Anderson AK, Hall J, Davis M, Hilyard K. WIC peer counselors' perceptions of breastfeeding in African American women with lower incomes. J Hum Lact 2015;31(1):99–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Guendelman S, Kosa J, Pearl M, Graham S, Goodman J, Kharrazi M. Juggling work and breastfeeding: effects of maternity leave and occupational characteristics. Pediatrics 2009;123(1):e38–46. [DOI] [PubMed] [Google Scholar]
- 46. Ogbuanu C, Glover S, Probst J, Liu J, Hussey J. The effect of maternity leave length and time of return to work on breastfeeding. Pediatrics 2011;127(6):e1414–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Miles G, Siega-Riz AM. Trends in food and beverage consumption among infants and toddlers: 2005–2012. Pediatrics 2017;139(6):e20163290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Burdette HL, Whitaker RC, Hall WC, Daniels SR. Breastfeeding, introduction of complementary foods, and adiposity at 5 y of age. Am J Clin Nutr 2006;83(3):550–8. [DOI] [PubMed] [Google Scholar]
- 49. Pierce J, Taylor M, Langley-Evans S. Timing of the introduction of complementary feeding and risk of childhood obesity: a systematic review. Int J Obes 2013;37:1295–306. [DOI] [PubMed] [Google Scholar]
- 50. Baker R, Greer F. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0-3 years of age). Pediatrics 2010;126(5):1040–50. [DOI] [PubMed] [Google Scholar]
- 51. Lozoff B, Castillo M, Clark K, Smith J, Sturza J. Iron supplementation in infancy contributes to more adaptive behavior at 10 years of age. J Nutr 2014;144(6):838–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Bailey RL, Catellier DJ, Jun S, Dwyer JT, Jacquier EF, Anater AS, Eldridge AL. Total usual nutrient intakes of US children (under 48 months): findings from the Feeding Infants and Toddlers Study (FITS) 2016. J Nutr 2018;148:1557S–66S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Butte NF, Fox MK, Briefel RR, Siega-Riz AM, Dwyer JT, Deming DM, Reidy KC. Nutrient intakes of US infants, toddlers, and preschoolers meet or exceed Dietary Reference Intakes. J Am Diet Assoc 2010;110(12):S27–37. [DOI] [PubMed] [Google Scholar]
- 54. Nowak-Węgrzyn A, Katz Y, Mehr S, Koletzko S. Non-IgE-mediated gastrointestinal food allergy. J Allergy Clin Immunol 2015;135(5):1114–24. [DOI] [PubMed] [Google Scholar]
- 55. Ziegler E. Consumption of cow's milk as a cause of iron deficiency in infants and todd. Nutr Rev 2011;69(s1):S37–42. [DOI] [PubMed] [Google Scholar]
- 56. American Academy of Pediatrics, Committee on Nutrition The use of whole cow's milk in infancy. Pediatrics 1992;89(6):1105–9. [PubMed] [Google Scholar]
- 57. American Academy of Pediatrics About HALF: Healthy Active Living for Families (HALF) program 2012 [updated not specified; cited 2018 Apr 3]. Available from: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/HALF-Implementation-Guide/Pages/About-HALF.aspx. [Google Scholar]
- 58. Auerbach B, Wolf F, Hikida A, Vallila-Buchman P, Littman A, Thompson D, Louden D, Taber D, Krieger J. Fruit juice and change in BMI: A meta-analysis. Pediatrics 2017;139(4):e20162454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Dietz W. Childhood weight affects adult morbidity and mortality. J Nutr 1998;128(Suppl):411S–4S. [DOI] [PubMed] [Google Scholar]
- 60. Ebbeling C, Feldman H, Chomitz V, Antonelli TA, Gortmaker SL, Osganian SK, Ludwig DS. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med 2012;367(15):1407–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Institute of Medicine Early childhood obesity prevention policies: consensus report. National Academies Press, Washington DC: 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ludwig D, Peterson K, Gortmaker S. Relation between consumption of sugar sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet 2001;357(9255):505–8. [DOI] [PubMed] [Google Scholar]
- 63. Park S, Pan L, Sherry B, Li R. The association of sugar-sweetened beverage intake during infancy with sugar-sweetened beverage intake at 6 years of age. Pediatrics 2014;134(Suppl 1):S56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Pocock M, Trivedi D, Wills W, Bunn F, Magnusson J. Parental perceptions regarding healthy behaviours for preventing overweight and obesity in young children: a systematic review of qualitative studies. Obes Rev 2010;11(5):338–53. [DOI] [PubMed] [Google Scholar]
- 65. He F, Nowson C, Lucas M, MacGregor G. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens 2007;21(9):717–28. [DOI] [PubMed] [Google Scholar]
- 66. He F, Nowson C, MacGregor G. Fruit and vegetable consumption and stroke: meta-analysis of cohort studies. Lancet 2006;367(9507):320–6. [DOI] [PubMed] [Google Scholar]
- 67. Hodder R, Stacey F, O'Brien K, Wyse R, Clinton-McHarg T, Tzelepis F, James E, Bartlem K, Nathan N, Sutherland R et al. Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database Syst Rev 2018;1:CD008552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wu L, Sun D, He Y. Fruit and vegetables consumption and incident hypertension: dose-response meta-analysis of prospective cohort studies. J Hum Hypertens 2016;30(10):573–80. [DOI] [PubMed] [Google Scholar]
- 69. Zhan J, Liu Y, Cai L, Xu F, Xie T, He Q. Fruit and vegetable consumption and risk of cardiovascular disease: a meta-analysis of prospective cohort studies. Crit Rev Food Sci Nutr 2017;57(8):1650–63. [DOI] [PubMed] [Google Scholar]
- 70. Birch L, Savage J, Ventura A. Influences on the development of children's eating behaviours: from infancy to adolescence. Can J Diet Pract Res 2007;68(1):s1. [PMC free article] [PubMed] [Google Scholar]
- 71. Abrams S, Daniels S. Fruit juice and child health. Pediatrics 2017;139(4):e20170041. [DOI] [PubMed] [Google Scholar]
- 72. Heyman M, Abrams S. Fruit juice in infants, children, and adolescents: current recommendations. Pediatrics 2017;139(6):e20170967. [DOI] [PubMed] [Google Scholar]
- 73. Kurinij N, Shiono P, Rhoads G. Breastfeeding incidence and duration in black and white women. Pediatrics 1988;81:365–71. [PubMed] [Google Scholar]
- 74. Li R, Grummer-Strawn L. Racial and ethnic disparities in breastfeeding among United States infants: Third National Health and Nutrition Examination Survey, 1988–1994. Birth 2002;29(4):251–7. [DOI] [PubMed] [Google Scholar]
- 75. Rassin D, Richardson C, Baranowski T, Nader PR, Guenther N, Bee DE, Brown JP. Incidence of breastfeeding in a low socioeconomic group of mothers in the United States: ethnic patterns. Pediatrics 1984;73(2):132–7. [PubMed] [Google Scholar]
- 76. American Cancer Society Breast cancer facts & figures, 2009–2010. American Cancer Society, Atlanta GA: 2010. [Google Scholar]
- 77. Arenz S, Rückerl R, Koletzko B, von Kries R. Breast-feeding and childhood obesity—a systematic review. Int J Obes 2004;28(10):1247–56. [DOI] [PubMed] [Google Scholar]
- 78. Fejerman L, Stern M, John E, Torres-Mejía G, Hines L, Wolff R, Baumgartner K, Giuliano A, Ziv E, Pérez-Stable E et al. Interaction between common breast cancer susceptibility variants, genetic ancestry, and nongenetic risk factors in Hispanic women. Cancer Epidemiol Biomarkers Prev 2015;24(11):1731–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Daniels S, Hassink S. The role of the pediatrician in primary prevention of obesity. Pediatrics 2015;136(1):e275–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


