Abstract
Objective:
Despite rising rates of obesity among patients with HIV, the potential role for weight loss surgery in this population remains less clear. The primary aim of this study was to evaluate the role of bariatric surgery on relevant clinical outcomes among hospitalized obese patients with HIV.
Design:
Retrospective analysis using the United States Nationwide Inpatient Sample database from 2004 to 2014. Using Poisson regression, adjusted incidence risk ratios (IRR) were derived for clinical outcomes in patients with prior-bariatric surgery compared to those without bariatric surgery.
Subjects:
Patients with discharge co-diagnoses of morbid obesity and HIV.
Intervention:
Bariatric surgery.
Main Outcome Measures:
Primary outcome was in-hospital mortality. Secondary outcomes included renal failure, urinary tract infection, malnutrition, sepsis, pneumonia, respiratory failure, thromboembolic events, gastrointestinal strictures, micronutrient deficiency, length of stay, and hospitalization costs.
Results:
Among 7,803 patients with discharge diagnoses of HIV and morbid obesity, 346 patients (4.4%) had bariatric surgery. The proportion of bariatric surgery in obese patients with HIV initially declined by −0.10% per year from 2004 to 2009 (Ptrend<0.05), then increased at an annual rate of +0.33% from 2012 to 2014 (Ptrend<0.05). On multivariable analysis, bariatric surgery did not influence mortality (P=0.98). Bariatric surgery was associated with decreased risk for renal failure, respiratory failure, and sepsis (all P<0.001). However, bariatric surgery increased the risk for post-operative strictures (IRR 2.5; 95% CI, 1.5–4.5; P=0.001).
Conclusions:
Though initially underutilized, bariatric surgery in morbidly obese HIV patients is increasing and appears to be safe and effective in significantly reducing life-threatening morbidity.
Keywords: HIV, AIDS, Obesity, Bariatric Surgery, Weight loss
INTRODUCTION
As of 2014, there were an estimated 1.1 million individuals in the United States living with human immunodeficiency virus (HIV) infection.1 In 2015 alone, despite a 9% decrease in the number of new diagnoses, approximately 39,500 people were diagnosed with HIV. With the introduction of more available and effective antiviral treatments, the last 30 years have ushered in a monumental shift in the management of HIV/Acquired immunodeficiency syndrome (AIDS) – moving from an acute to a chronic illness.2 However, treatment with combined anti-retroviral therapy has been associated with weight gain and multiple metabolic problems such as dyslipidemia, lipodystrophy, insulin resistance, and increased risk of vascular disease.3–5
With this paradigm shift to a chronic disease model, under-nutrition in these HIV patients has become less prevalent in the Western world with growing rates of obesity and metabolic syndrome increasing similar to the general population. According to a recent National Health and Nutrition Examination Survey (NHANES), obesity among HIV positive patients is common, affecting 2 in 5 HIV-infected women and 1 in 5 HIV-infected men.6 While there is evidence to suggest that mild-to-moderate obesity in HIV-infected individuals is associated with better HIV-related survival, other studies have shown that adipose tissue may be a reservoir of HIV shedding, which has implications for viral persistence.7,8
Although dietary modification and exercise regimens can promote weight loss, a vast majority of patients are unable to achieve and maintain the necessary amount of weight loss related to meaningful clinical improvement.9 With the potential association between HIV, morbid obesity, and metabolic syndrome coupled with the concern for viral persistence, studies have suggested a potential role for bariatric surgery. However, concerns persist regarding the absorption and efficacy of antiretroviral therapies post-bariatric surgery. While studies have evaluated bariatric surgery in this unique patient population and found the procedure to be safe and effective, there remains a paucity of data regarding the impact of bariatric surgery on outcomes of patients with HIV.8,10
The aim of this study was to examine the impact of bariatric surgery on clinical outcomes in morbidly obese hospitalized patients with HIV. We hypothesized that bariatric surgery would be associated with better outcomes.
METHODS
Data Source and Study Population:
The study sample originated from the Nationwide Inpatient Sample database, which includes hospitalized patients in the United States during the 2004 to 2014 period. This registry is part of the Healthcare Cost and Utilization Project, sponsored by the Agency for Healthcare Research and Quality.11 The Nationwide Inpatient Sample is a database of hospital inpatient stays derived from billing data submitted by hospitals to statewide data organizations across the United States. Inpatient data includes clinical and resource use information typically available from discharge abstracts. Each discharge is coded with a principal diagnosis for that specific hospitalization in addition to the potential for 14 secondary diagnoses and 15 associated procedures. The Nationwide Inpatient Sample is the largest United States inpatient care database, encompassing hospitals from a total of 46 states, which serve 97% of the United States population.
Inclusion and Exclusion Criteria:
Patients were included if they had a primary or secondary diagnosis of HIV and morbid obesity. These conditions were identified using the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) codes. HIV was defined based upon ICD-9-CM code 042, 043, 044, V08, and 079.53 as previously validated.12 Morbid obesity was defined by ICD-9-CM codes 278.01, V85.35, V85.36, V85.37, V85.37, V85.38, V85.39, V85.40, V85.41, V85.42, V85.43, V85.44, and V85.45 in accordance with prior studies.13,14
Ascertainment of bariatric surgery
Among the included patients with morbid obesity and HIV, hospitalizations with a history of prior-bariatric surgery (Roux-en-Y, gastric band, and sleeve gastrectomy) were identified using the following ICD-9-CM codes: laparoscopic or open Roux-en-Y gastric bypass (ICD-9-CM 44.31, 44.38, and 43.39), laparoscopic adjustable gastric band (ICD-9-CM 44.95), and laparoscopic sleeve gastrectomy (ICD-9-CM 43.82).13,14
Covariates and Statistical Analysis
Demographic and clinical characteristics were compared between patients with and without a history of bariatric surgery. The covariates included demographic data (age, gender, and race/ethnicity), as well as characteristics related to metabolic syndrome and HIV-related outcomes. Hospitalization data such as day of admission (weekday or weekend), route of admission, mean length of hospital stay, hospitalization charges, and primary payer source were also included. Details on the covariates are highlighted in Appendix 1. Categorical variables were presented as counts and proportions, and differences tested using Pearson’s Chi-square test. Continuous variables were presented as mean (standard deviation), and differences between groups were tested using the t-test. The age-adjusted mortality rate was calculated for each year of study by summing the product of age-specific mortality rates by the age-specific weights. For population trends, the total number of cases were standardized per 100,000 based upon total population derived from the United States census data for the specific year (2004 to 2014).15 The weights used in the age adjustment of the data were the proportion of the year 2000 standard United States population within each age group.16
Secular trends in mortality rates were assessed using linear Poisson regression models. The models were used to investigate the effect of the period of diagnosis (independent variable) on the in-hospital mortality rate (dependent variable), while controlling for other variables (i.e. adjusting for age, sex, race, income, insurance status, type of admission, and modified Elixhauser comorbidity index including: diabetes, hypertension, hyperlipidemia, coronary artery disease, and Polycystic ovarian syndrome). Risk estimates and 95% confidence intervals (CI’s) were calculated for all independent variables in the final model. Poisson regression with robust (Huber–White) standard errors was also used to determine incident risk ratios (IRR) for predictors of in-hospital mortality. Prior to our analysis, we tested the Poisson models for over-dispersion using a Pearson goodness- of-fit test. Models were not over dispersed; thus, Poisson regression was then used to determine incident risk ratios (IRR) for clinical outcomes in patients with prior-bariatric surgery compared to those without bariatric surgery.
All the analyses accounted for clustering and sampling weights. The Healthcare Cost and Utilization Project Nationwide Inpatient Sample has a 2-stage cluster design incorporating clustering at the hospital level and discharge level. The weighting of discharges is based on the hospital type and volume of discharges relative to the sampling region. Analyses were performed using Stata version 13.0 (Stata Corp LP, College Station, TX). All p values were based on 2-sided tests and were considered statistically significant at P value < 0.05. According to the data user agreement, any individual table cell counts of 10 or fewer cannot be presented to preserve patient confidentiality. In such instances, data are suppressed and labeled as IS, information suppressed.
RESULTS
Demographic and Patients Characteristics
A total of 7,803 patients with discharge diagnoses of morbid obesity and HIV were included in our study, of which 346 (4.4%) had prior-bariatric surgery. The baseline demographic and hospitalization characteristics of patients by bariatric surgery status are presented in Table 1. Morbidly obese HIV patients with prior weight loss surgery were younger as compared to patients without bariatric surgery (mean age of 42.9 ± 8.6 versus 45.5 ± 10.7 years, respectively; P<0.001). A majority of included morbidly obese HIV patients, both with or without bariatric surgery, were female though a higher percentage of women did not undergo bariatric surgery (P<0.001). Patients with obesity and HIV with or without a history of bariatric surgery were not significantly different in comorbidities including coronary artery disease (P=0.58) and polycystic ovarian syndrome (P=0.42). However, obese HIV patients with a history of bariatric surgery were more likely to have a documented history of hypertension (P<0.001) and hyperlipidemia (P<0.001).
Table 1.
Characteristics of Hospitalized Patients with Morbid Obesity and HIV
| Variable | Bariatric Surgery (N=346; 4.4%) | No Bariatric Surgery (N=7457; 95.6%) | P Value |
|---|---|---|---|
| Demographic Characteristics | |||
| Age (years)* | 42.9 (8.6) | 45.5 (10.7) | <0.001 |
| Gender | <0.001 | ||
| Male Gender | 37.9 | 30.6 | |
| Female Gender | 62.1 | 69.4 | |
| Race /Ethnicity | <0.001 | ||
| White | 36.8 | 22.7 | |
| Black | 44.3 | 63.7 | |
| Hispanic | 14.2 | 9.7 | |
| Other | 4.7 | 3.9 | |
| Hypertension | 52.0 | 42.0 | <0.001 |
| Coronary Artery Disease | IS | 1.5 | 0.58 |
| Hyperlipidemia | 22.5 | 17.6 | <0.001 |
| PCOS | IS | 0.2 | 0.42 |
| Hospital Related Characteristics | |||
| Elective admission | 90.4 | 36.8 | <0.001 |
| Weekend Admission | IS | 21.7 | <0.001 |
| Primary Payer Source | <0.001 | ||
| Private Insurance | 35.1 | 36.8 | |
| Medicaid | 26.7 | 40.2 | |
| Medicare | 36.5 | 15.7 | |
| Other Payment Source | 1.7 | 4.7 | |
| Self-Pay | IS | 0.8 | |
| No Charge | IS | 1.8 | |
Data are counts (percentage)
Mean (SD)
PCOS= Polycystic Ovarian Syndrome; NOTE. According to the data user agreement, any individual table cell counts of 10 or fewer cannot be presented to preserve patient confidentiality. In such instances, data are suppressed. IS, information suppressed.
Trends in Obesity and Bariatric Surgery Use
Trends of obesity among HIV patients as adjusted for the proportion of discharges demonstrated an annual percent change of +0.12% from 2004 to 2014. The overall number of bariatric surgeries in morbidly obese HIV patients increased approximately 6.3 times the previous number of procedures performed from 2004 (n=12) to 2014 (n=76) – Table 2. Trends in overall bariatric surgery as adjusted for the proportion of discharges with bariatric surgery demonstrated an annual percent change of −0.10% from 2004 to 2009 (Ptrend<0.05) and then increased at an annual rate of +0.33% from 2012 to 2014 (Ptrend<0.05) – Figure 1.
Table 2.
Trends in Bariatric Surgery Among Patients with Morbid Obesity and HIV
| Year | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bariatric Surgery | 12 | 12 | 14 | 15 | 22 | 25 | 35 | 40 | 45 | 50 | 76 | 346 |
| No Bariatric Surgery | 248 | 249 | 318 | 356 | 459 | 583 | 721 | 1150 | 1009 | 1125 | 1239 | 7457 |
| Total No. of Patients | 260 | 261 | 332 | 371 | 481 | 608 | 756 | 1190 | 1054 | 1175 | 1315 | 7803 |
NOTE. According to the data user agreement, any individual table cell counts of 10 or fewer cannot be presented to preserve patient confidentiality. In such instances, data are suppressed. IS, information suppressed.
Figure 1.
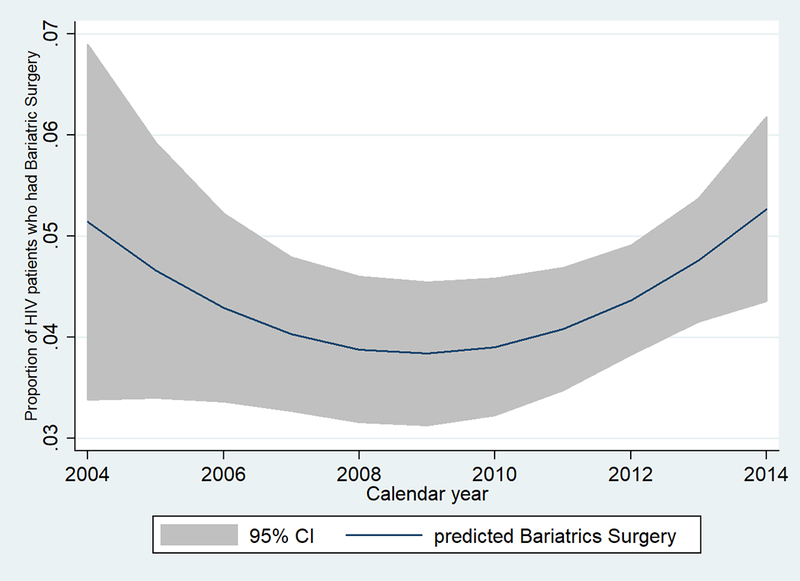
Proportion of Discharges in Patients with HIV and Bariatric Surgery, 2004 – 2014.
Clinical Outcomes
On multivariate analysis, patients without history of a surgical weight loss procedure were found to have no significant in-hospital mortality difference when compared to those that underwent a bariatric procedure (P=0.98) – Table 3. Renal failure (P<0.001), sepsis (P<0.001), and respiratory failure (P<0.001) were significantly lower among obese patients with HIV and a history of bariatric surgery. Gastrointestinal strictures were significantly higher in obese HIV patients with a history of prior bariatric surgery (IRR 2.5; 95% CI, 1.5–4.5; P=0.001). In comparison to patients without weight loss surgery, obese patients with HIV and bariatric surgery demonstrated higher hospitalization costs ($45206 ± 31198 versus $42908 ± 69791; P<0.001), but shorter length of hospital stay (2.3 ± 1.8 days versus 5.8 ± 7.5 days; P<0.001) – Table 3.
Table 3.
Multivariable Regression Analysis for Outcomes with Prior Bariatric Surgery versus No Bariatric Surgery in Patients with Morbid Obesity and HIV
| Outcome | Bariatric Surgery (%) | No Bariatric Surgery (%) | P Value | IRR* (95% CI) | P Value |
|---|---|---|---|---|---|
| Overall | |||||
| Renal Failure | 0.3 | 11.6 | <0.001 | 0.05(0.01–0.39)- | 0.004 |
| Malnutrition | 0.3 | 1.7 | 0.04 | 0.25(0.03–1.9) | 0.18 |
| Pneumonia | 2.0 | 10.0 | <0.001 | 0.60(0.27–1.33) | 0.21 |
| Sepsis | 0.6 | 5.9 | <0.001 | 0.23(0.05–0.96) | 0.04 |
| Respiratory failure | 0.6 | 7.4 | <0.001 | 0.17(0.04–0.71) | 0.02 |
| UTI | IS | 7.4 | <0.001 | # | 0.98 |
| Pancreatitis | 0.3 | 1.5 | 0.07 | - | - |
| Surgical | |||||
| Wound Infection | IS | 1.1 | 0.05 | - | - |
| Hemorrhage | 0.6 | 0.4 | 0.65 | - | - |
| Obstruction | IS | 0.5 | 0.19 | - | - |
| Strictures | 7.2 | 1.0 | <0.001 | 2.5(1.5–4.5) | 0.001 |
| Fistula | 0.3 | 0.1 | 0.21 | - | - |
| Nutritional | |||||
| Anemia | 2.3 | 3.6 | 0.22 | - | - |
| Thiamine deficiency | 0.6 | 0.1 | 0.002 | 3.7(0.37–37.7) | 0.26 |
| Zinc Deficiency | 0.3 | 0.9 | 0.23 | - | - |
| LOS, Costs, Mortality | |||||
| LOS | 2.3(1.8) | 5.8(7.5) | <0.001 | 0.43(0.39–0.46) | <0.001 |
| Total Costs | 45206(31198) | 42908 (69791) | <0.001 | 1.01 (1.012–1.013) | <0.001 |
| Mortality | IS | 1.4 | 0.03 | # | 0.98 |
CI = Confidence interval; UTI= Urinary Tract Infection; LOS= Length of Stay
IRR = Incident risk ratios adjusted for age, sex, race, income, insurance status, type of admission, modified Elixhauser comorbidity index including: diabetes, hypertension, hyperlipidemia, coronary artery disease, and obstructive sleep apnea.
NOTE. According to the data user agreement, any individual table cell counts of 10 or fewer cannot be presented to preserve patient confidentiality. In such instances, #data are suppressed. IS, information suppressed.
DISCUSSION
In this study, we utilized a large United States inpatient database to evaluate trends in bariatric surgery and related clinical outcomes in a hospitalized population of 7,803 morbidly obese patients with HIV. In spite of the rising trends of obesity in this patient population as a result of improved anti-viral therapy and a transition to a chronic disease model, only a 4.4% of morbidly obese patients with HIV had prior bariatric surgery. Bariatric surgery was not associated with a decrease in in-hospital mortality rate among morbidly obese patients with HIV; however, weight loss surgery was associated with lower rates of renal failure, respiratory failure, and sepsis.
Mechanisms of Obesity and HIV: A Clinical Paradox
For many years, lean body mass was the characteristic body habitus for an HIV-infected individual.3 However, with advances in anti-retroviral therapy leading to increased life-span and over-all survival, HIV infected patients have become susceptible to developing chronic medical problems and metabolic syndrome including obesity, diabetes, insulin resistance, and coronary artery disease.17–21 With an increased prevalence of obesity and metabolic syndrome, cardiovascular disease is quickly becoming one of the most important causes of mortality in HIV-infected patients, superseding opportunistic infections.19–22 While the most likely contributing factor for weight gain in the HIV population is the decrease in HIV-related morbidity, additional factors including successful immune recovery as well as health improvement overall may reduce weight loss and even promote weight gain.3–5 Furthermore, an another major element to explain weight gain and predispose towards obesity is medication associated lipodystrophy resulting from the long-term use of highly active anti-retroviral therapy, particularly the protease inhibitors and nucleoside agents. 3–5,23 Moreover, obesity itself may have a directly negative effect on the HIV host.17,24–28 Therefore, for patients with HIV and morbid obesity, weight management programs and weight loss strategies, including bariatric surgery may be important components of HIV care.23
HIV and Bariatric Associated Weight Loss
Currently, bariatric surgery provides the highest level of excess weight loss as compared to other presently available methods, achieving approximately 62% with gastric bypass, 41% with laparoscopic adjustable gastric banding, and 66% with laparoscopic sleeve gastrectomy.29–34 While bariatric surgery may have unintended side effects including the alteration of pharmacodynamics and pharmacokinetics of orally administered anti-retroviral drugs, weight loss surgery has an excellent safety and success rate.29,30,35–38 As a result, the total number of weight loss procedures have increased globally and in the United States in the past decade.39,40 However, despite a total increase in number of procedures, the proportion of morbidly obese HIV patients with bariatric surgery declined from 2004 to 2009 in our study sample. This observation may be due to initial reluctance among surgeons to surgically treat these patients as a result of prior reports of complications associated with weight reduction surgery, particularly regarding the change in pharmacokinetics of anti-retroviral therapies post-bariatric surgery.38 Yet, an encouraging and positive aspect of our analyses is the finding rising trends of bariatric surgery after 2010 in this select population, suggesting a sense of confidence among physicians and patients regarding these weight loss procedures.
Safety of Bariatric Surgery
While case series and case reports have reported safety of bariatric surgery in morbidly obese patients with HIV, these reports are limited by their small sample size.14,41–46
Our study is consistent with these prior reports in further supporting the role of bariatric surgery for obese HIV patients finding no difference in mortality. We are unable to rule out the influence of bariatric surgery in long-term mortality in these patients for which studies with longer duration of follow-up will be beneficial. However, our data aligns with previous literature that suggests that morbidly obese patients with HIV and prior bariatric surgery have lower rates of complications (i.e., renal failure, respiratory failure, and sepsis).47,48 Currently available data is inadequate to explain the exact mechanism by which bariatric surgery may lead to these positive outcomes; however, decreased chronic inflammation and improvement in overall health of these patients may improve outcomes post-weight loss procedures.
Our data contradicts previous findings of micronutrient deficiency by demonstrating that bariatric surgery in obese HIV patients was not associated with any of these micronutrient deficiencies.49 Furthermore, obese patients with HIV and prior weight loss surgery were associated with a shorter hospital stay but higher costs of hospitalizations. Overall, this suggests that bariatric surgery is beneficial for these patients and supports the need to promote bariatric procedures in effort to improve anti-retro viral effectiveness, reduce complications, and decrease overall healthcare utilization. One major complication encountered among HIV patients with obesity that underwent bariatric surgery in our study is the high rates of post-operative strictures. Strictures have been reported as complications of prior bariatric surgery and are one of the primary indications of revision surgery.41 This increased rate of strictures in this group may suggest a need for vigilance during the post-operative period and may guide physicians for a closer follow-up of patients after bariatric surgery for early diagnosis and management of this potential complication.
Clinical Implications and Future Directions
Our data suggest that bariatric surgery does not affect mortality in morbidly obese patients but may be associated with mitigation of life-threatening complications such as respiratory failure, renal failure, and sepsis. Bariatric surgery did, however, demonstrate an increased risk of gastrointestinal stricture in HIV patients which suggests a need for caution during the post-operative period. These results are of utmost clinical significance particularly for a disease like HIV which has long been associated with opportunistic infections and sepsis. Though introduction of antiretroviral therapy and subsequent immune recovery has lowered the rates of infection among these patients, our findings suggest that prior bariatric surgery may have a role in further lowering the rates of infection and multi-organ failure in morbidly obese patients with HIV.
Strengths and Limitations
Our study has limitations intrinsic to its retrospective and observational design. Also, we are only able to assess in-hospital outcomes and information on long-term outcomes upon discharge is not available in this inpatient database. Patients with HIV and morbid obesity and other covariates in our cohort were identified solely based on ICD-9-CM codes, thus may introduce bias to our study as a result of coding errors. While previous studies have validated these codes for the HIV, morbid obesity, and bariatric surgery populations, we are unable to determine the temporal sequence in the occurrence of HIV and the bariatric surgery procedure.12–14 There is additionally the possibility of residual confounding as some important covariates (i.e., percent excess weight loss, body mass index [BMI], CD4 count, and viral load) were not available in the database. As NIS does not provide information on laboratory values and pharmacotherapy, we do not have information on CD4 count, viral load, and type of anti-retroviral therapy limiting our ability to gauge the virologic and immunologic response to bariatric surgery. We are also unable to extract information to determine the roles of other methods of weight management such as lifestyle modifications and pharmacotherapies in this patient population. Due to small sample size of obese patients with HIV that underwent bariatric surgery, we were also unable to stratify and compare trends and outcomes between malabsorptive and restrictive type of bariatric surgery.
Despite these limitations, our study has several strengths and novel salient findings. To the best of our knowledge, this study is the largest and first ever study evaluating these trends and outcomes of bariatric surgery over a period of 10 years for morbidly obese patients with HIV. Our study includes the largest number of patients from a nationwide population-based sample including several racial/ethnic groups. This minimizes the possible biases that may be seen in single-center studies and provides strong data to generalize our observations to clinical practice in the United States. Our data and trends of obesity among HIV-infected individuals is supported by previous studies which demonstrate the global epidemic of obesity has not spared this selected population. The number of morbidly obese patients with HIV steadily rose over the study period similarly to previous studies.6,23 Furthermore, we have included a vast array of relevant outcomes (i.e., renal failure, respiratory failure, sepsis, surgical, and malabsorptive complications), which would reliably indicate a response to bariatric surgery above and beyond percent weight loss and change in BMI.
CONCLUSION
In conclusion, there is a shifting phenotype among HIV patients with a transition from lean body mass and under-nourished presentation to one of weight gain, giving rise to chronic medical comorbidities including metabolic syndrome and predisposition to morbid obesity. Therefore, weight management strategies are critical for this increasingly common population of HIV patients. Bariatric surgery appears to be associated with decreased complications and better outcomes among individuals with morbid obesity and HIV. We are hopeful that our results will motivate both the HIV community and physicians to consider bariatric surgery as a safe and effective treatment option for those patients with morbid obesity. Future studies are needed which will stratify the outcomes of these weight loss surgeries based on their mechanism of action (i.e., restrictive, malabsorptive, or both) to delineate if one type of procedure is recommended over another. Additionally, studies with a larger population designed to investigate the virologic and immunologic response secondary to these procedures are required.
Supplementary Material
Acknowledgements
All authors approved of the final version of the manuscript.
Financial Support: Supported by NIH 5 T32 DK 7356–37 (BN)
Footnotes
Potential Conflicts of Interest: The authors have no conflicts to disclose.
Author Contributions:
Study concept and design – McCarty T, Sharma P and Njei B, Paper preparation – McCarty T, and Sharma P, Statistical analysis – Njei B, Critical revisions – McCarty TR, Njei B, Ngu J, O’Donnell M
REFERENCES
- 1.HIV Basic Statistics. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/statistics.html. Accessed September 19, 2017.
- 2.Fee E, Fox DM. Introduction: the contemporary historiography of AIDS In: Fee E, Fox DM, eds. AIDS: the making of a chronic disease. Berkeley: University of California; 1992:1–19. [Google Scholar]
- 3.Shikuma CM, Zackin R, Sattler F, et al. Changes in weight and lean body mass during highly active antiretroviral therapy. Clin Infect Dis 2004;39:1223–30. [DOI] [PubMed] [Google Scholar]
- 4.Montessori V, Press N, Harris M, Akagi L, Montaner JS. Adverse effects of antiretroviral therapy for HIV infection. CMAJ 2004;170:229–38. [PMC free article] [PubMed] [Google Scholar]
- 5.Henry K, Melroe H, Huebsch J, et al. Severe premature coronary artery disease with protease inhibitors. Lancet 1998;351:1328. [DOI] [PubMed] [Google Scholar]
- 6.Thompson-Paul AM, Wei SC, Mattson CL, et al. Obesity Among HIV-Infected Adults Receiving Medical Care in the United States: Data From the Cross-Sectional Medical Monitoring Project and National Health and Nutrition Examination Survey. Medicine (Baltimore) 2015;94:e1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shor-Posner G, Campa A, Zhang G, et al. When obesity is desirable: a longitudinal study of the Miami HIV-1-infected drug abusers (MIDAS) cohort. J Acquir Immune Defic Syndr 2000;23:81–8. [DOI] [PubMed] [Google Scholar]
- 8.Panko N, Dunford G, Lutfi R. HIV Infection Is Not a Contraindication to Laparoscopic Sleeve Gastrectomy for Morbid Obesity. Obes Surg 2018;28:464–8. [DOI] [PubMed] [Google Scholar]
- 9.Dudekula A, Rachakonda V, Shaik B, Behari J. Weight loss in nonalcoholic Fatty liver disease patients in an ambulatory care setting is largely unsuccessful but correlates with frequency of clinic visits. PLoS One 2014;9:e111808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kassir R, Huart E, Tiffet O, et al. Feasibility of Bariatric Surgery in the HIV-Infected Patients. Obes Surg 2017;27:818–9. [DOI] [PubMed] [Google Scholar]
- 11.Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality (AHRQ): Advancing Excellence in Health Care. https://www.ahrq.gov/research/data/hcup/index.html. Accessed January 6, 2018.
- 12.Mehta K, Im A, Rahman F, Wang H, Veldkamp P. Epidemiology and Outcomes of Hematopoietic Stem Cell Transplant in HIV (+) Patients from 1998 to 2012: A Nationwide Analysis. Clin Infect Dis 2018. [DOI] [PubMed] [Google Scholar]
- 13.McCarty TR, Echouffo-Tcheugui JB, Lange A, Haque L, Njei B. Impact of bariatric surgery on outcomes of patients with nonalcoholic fatty liver disease: a nationwide inpatient sample analysis, 2004–2012. Surg Obes Relat Dis 2018;14:74–80. [DOI] [PubMed] [Google Scholar]
- 14.Sharma P, McCarty TR, Njei B. Impact of Bariatric Surgery on Outcomes of Patients with Inflammatory Bowel Disease: a Nationwide Inpatient Sample Analysis, 2004–2014. Obes Surg 2017. [DOI] [PubMed] [Google Scholar]
- 15.Population Estimates. United States Census Bureau. https://www.census.gov/popest/data/intercensal/national/nat2010.html. Accessed February 11, 2018.
- 16.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. National vital statistics report: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 1998;47:1-16, 2 . [PubMed] [Google Scholar]
- 17.Crum-Cianflone N, Tejidor R, Medina S, Barahona I, Ganesan A. Obesity among patients with HIV: the latest epidemic. AIDS Patient Care STDS 2008;22:925–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palella FJ Jr., Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med 1998;338:853–60. [DOI] [PubMed] [Google Scholar]
- 19.Enanoria WT, Ng C, Saha SR, Colford JM Jr., Treatment outcomes after highly active antiretroviral therapy: a meta-analysis of randomised controlled trials. Lancet Infect Dis 2004;4:414–25. [DOI] [PubMed] [Google Scholar]
- 20.Sharma G, Strong AT, Boules M, et al. Comparative Outcomes of Bariatric Surgery in Patients With and Without Human Immunodeficiency Virus. Obes Surg 2017. [DOI] [PubMed] [Google Scholar]
- 21.Keithley JK, Duloy AM, Swanson B, Zeller JM. HIV infection and obesity: a review of the evidence. J Assoc Nurses AIDS Care 2009;20:260–74. [DOI] [PubMed] [Google Scholar]
- 22.Barbaro G Highly active antiretroviral therapy-associated metabolic syndrome: pathogenesis and cardiovascular risk. Am J Ther 2006;13:248–60. [DOI] [PubMed] [Google Scholar]
- 23.Crum-Cianflone N, Roediger MP, Eberly L, et al. Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PLoS One 2010;5:e10106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wellen KE, Hotamisligil GS. Inflammation, stress, and diabetes. J Clin Invest 2005;115:1111–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bahceci M, Gokalp D, Bahceci S, Tuzcu A, Atmaca S, Arikan S. The correlation between adiposity and adiponectin, tumor necrosis factor alpha, interleukin-6 and high sensitivity C-reactive protein levels. Is adipocyte size associated with inflammation in adults? J Endocrinol Invest 2007;30:210–4. [DOI] [PubMed] [Google Scholar]
- 26.Ford ES. Body mass index, diabetes, and C-reactive protein among U.S. adults. Diabetes Care 1999;22:1971–7. [DOI] [PubMed] [Google Scholar]
- 27.Tanaka S, Isoda F, Ishihara Y, Kimura M, Yamakawa T. T lymphopaenia in relation to body mass index and TNF-alpha in human obesity: adequate weight reduction can be corrective. Clin Endocrinol (Oxf) 2001;54:347–54. [PubMed] [Google Scholar]
- 28.Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-reactive protein levels in overweight and obese adults. JAMA 1999;282:2131–5. [DOI] [PubMed] [Google Scholar]
- 29.Colquitt JL, Picot J, Loveman E, Clegg AJ. Surgery for obesity. Cochrane Database Syst Rev 2009:CD003641. [DOI] [PubMed] [Google Scholar]
- 30.Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007;357:741–52. [DOI] [PubMed] [Google Scholar]
- 31.Khan S, Rock K, Baskara A, Qu W, Nazzal M, Ortiz J. Trends in bariatric surgery from 2008 to 2012. Am J Surg 2016;211:1041–6. [DOI] [PubMed] [Google Scholar]
- 32.Phillips E, Ponce J, Cunneen SA, et al. Safety and effectiveness of Realize adjustable gastric band: 3-year prospective study in the United States. Surg Obes Relat Dis 2009;5:588–97. [DOI] [PubMed] [Google Scholar]
- 33.Fischer L, Hildebrandt C, Bruckner T, et al. Excessive weight loss after sleeve gastrectomy: a systematic review. Obes Surg 2012;22:721–31. [DOI] [PubMed] [Google Scholar]
- 34.O’Brien PE, McPhail T, Chaston TB, Dixon JB. Systematic review of medium-term weight loss after bariatric operations. Obes Surg 2006;16:1032–40. [DOI] [PubMed] [Google Scholar]
- 35.Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA 2005;294:1909–17. [DOI] [PubMed] [Google Scholar]
- 36.Miller AD, Smith KM. Medication and nutrient administration considerations after bariatric surgery. Am J Health Syst Pharm 2006;63:1852–7. [DOI] [PubMed] [Google Scholar]
- 37.Smith A, Henriksen B, Cohen A. Pharmacokinetic considerations in Roux-en-Y gastric bypass patients. Am J Health Syst Pharm 2011;68:2241–7. [DOI] [PubMed] [Google Scholar]
- 38.MacBrayne CE, Blum JD, Kiser JJ. Tenofovir, emtricitabine, and darunavir/ritonavir pharmacokinetics in an HIV-infected patient after Roux-en-Y gastric bypass surgery. Ann Pharmacother 2014;48:816–9. [DOI] [PubMed] [Google Scholar]
- 39.Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric Surgery Worldwide 2013. Obes Surg 2015;25:1822–32. [DOI] [PubMed] [Google Scholar]
- 40.Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg 2013;23:427–36. [DOI] [PubMed] [Google Scholar]
- 41.Flancbaum L, Drake V, Colarusso T, Belsley S. Initial experience with bariatric surgery in asymptomatic human immunodeficiency virus-infected patients. Surg Obes Relat Dis 2005;1:73–6. [DOI] [PubMed] [Google Scholar]
- 42.Fazylov R, Soto E, Merola S. Laparoscopic gastric bypass surgery in human immunodeficiency virus-infected patients. Surg Obes Relat Dis 2007;3:637–9. [DOI] [PubMed] [Google Scholar]
- 43.Fysekidis M, Cohen R, Bekheit M, et al. Sleeve gastrectomy is a safe and efficient procedure in HIV patients with morbid obesity: a case series with results in weight loss, comorbidity evolution, CD4 count, and viral load. Obes Surg 2015;25:229–33. [DOI] [PubMed] [Google Scholar]
- 44.Selke H, Norris S, Osterholzer D, Fife KH, DeRose B, Gupta SK. Bariatric surgery outcomes in HIV-infected subjects: a case series. AIDS Patient Care STDS 2010;24:545–50. [DOI] [PubMed] [Google Scholar]
- 45.Zivich S, Cauterucci M, Allen S, Vetter M, Vinnard C. Long-term virologic outcomes following bariatric surgery in patients with HIV. Obes Res Clin Pract 2015;9:633–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alfa-Wali M, Seechurn S, Ayodeji O, et al. Outcomes of bariatric surgery in human immunodeficiency virus positive individuals: a single center experience. Minerva Chir 2016;71:233–8. [PubMed] [Google Scholar]
- 47.Chang AR, Grams ME, Navaneethan SD. Bariatric Surgery and Kidney-Related Outcomes. Kidney Int Rep 2017;2:261–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seghieri M, Vitolo E, Giannini L, et al. Determinants of glomerular filtration rate following bariatric surgery in individuals with severe, otherwise uncomplicated, obesity: an observational, prospective study. Acta Diabetol 2017;54:593–8. [DOI] [PubMed] [Google Scholar]
- 49.Ma IT, Madura JA 2nd. Gastrointestinal Complications After Bariatric Surgery. Gastroenterol Hepatol (N Y) 2015;11:526–35. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


