Abstract
A rare case of adenoid cystic carcinoma arising from the sphenoid sinus causing lateral rectus palsy is presented here. Adenoid cystic carcinoma of the paranasal sinuses is an aggressive neoplasm which needs early diagnosis and treatment. Ideal treatment paradigm for paranasal sinus tumors is yet to be established. A combination of surgery and radiotherapy offers a better disease control and survival.
Keywords: Adenoid cystic carcinoma, Perineural invasion, Paranasal sinus, Nasal cavity
Introduction
Adenoid cystic carcinoma (ACC) of the sinonasal tract is a rare malignant tumor that accounts for fewer than 1% of all head and neck malignancies and 10% of all salivary gland neoplasms [1, 2]. ACC also known as “Cylindroma” is a tumor characterized by perineural spread [3]. Perineural spread of head and neck tumors commonly occurs along the branches of the trigeminal and facial nerves [2]. Hence it is very essential to rule out perineural spread to prevent treatment failure. ACC is known to recur with delayed development of distant metastasis [4]. Distant metastasis of ACC may be more common than regional lymph node metastasis, often leading to the death of the patient [5].
However, ACC of the paranasal sinuses represents a pathology with distinct clinical implications as they present late and their proximity to vital structures like orbit, dura, brain and cranial nerves makes complete reaction impossible, with positive surgical margins [6]. ACC of paranasal sinuses pose therapeutic and surgical challenges with regard to execution of surgical excision and post-operative radiation in view of recurrence. We present a rare case of adenoid cystic carcinoma arising from the sphenoid sinus that presented with headache and left lateral rectus palsy (Figs. 1, 2, 3, 4).
Fig. 1.

Left eye lateral rectus palsy
Fig. 2.
Heterogenous enhancing mass filling the sphenoid sinus with subtle bony erosions noted along the left lateral wall of the sphenoid sinus
Fig. 3.

Reddish friable mass filling the left sphenoid sinus and polypoidal mucosa involving the right sphenoid sinus
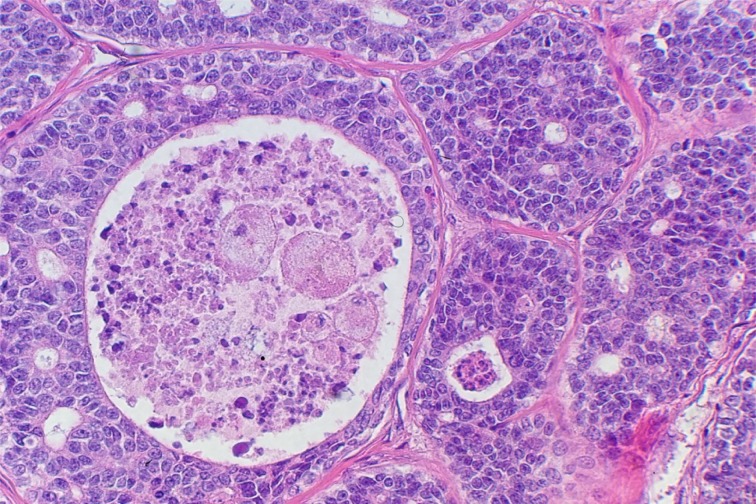
Fig. 4.
Tumor composed of basaloid epithelial cells forming sharply demarcated cell nests separated by fibrous septae (cribriform pattern)
Case Report
A 36-year-old male presented to the neurology out-patient department with complaints of headache and double vision in the left eye of 4 months duration. A diagnosis of left lateral rectus palsy for evaluation was made. On further evaluation MRI scan of the brain with contrast showed ill defined heterogenous enhancing mass lesion completely filling the left sphenoid sinus, with minimal enhancement of the adjacent dura around the sphenoid sinus, cavernous sinus and also the nasopharynx. The case was referred to the ENT department for sphenoid mass evaluation. A CT scan of the PNS was done which showed a heterogenous enhancing mass filling the sphenoid sinus with subtle bony erosions noted along the left lateral wall of the sphenoid sinus. A provisional diagnosis of chronic fungal sinusitis was made.
The patient was posted for endoscopic sinus surgery under general anesthesia. Per-operatively reddish friable lesion was seen arising from the left lateral wall of the sphenoid sinus and lateral recess. Polypoidal changes in the right sphenoid were seen. Posterior septectomy with midline wide sphenoidotomy with clearance of disease was made. A differential diagnosis of malignancy or pseudotumor was made. KOH mount and fungal cultures done were negative.
The histopathological sections showed fragments of tissue bits lined by respiratory epithelium with an infiltrative tumor composed of basaloid epithelial cells forming sharply demarcated cell nests separated by fibrous septae (cribriform pattern). The nests contained multiple extracellular cystic spaces containing eosinophilic PAS positive material. These features were suggestive of ACC. Further immunohistochemistry showed tumor cells to be positive in Bcl2 and negative for CD117 and Anti-S100 protein. The diagnosis of ACC was confirmed and the patient was referred for radiation therapy.
Discussion
ACC of the paranasal sinus or nasal cavity is a rare neoplasm with aggressive behaviour and a high incidence of both local recurrence and distant metastasis [4]. Leafstedt et al. [7] in a review from Roswell Park Cancer Institute described sinonasal ACC to have the poorest prognosis. Paranasal sinus tumors are known to have positive surgical margins due to proximity to vital structures like the orbit, dura, brain and cranial nerves. Our patient had an isolated sphenoid sinus lesion with a bony breach making complete clearance almost impossible. Moreover, perineural spread which is unpredictable makes clearance with negative surgical margins even more difficult. Howard and Lund have reported histologic evidence of an embolic pattern of perineural spread in paranasal ACC [8]. Hence studies have concluded that positive margins are a marker of more aggressive disease. Relationship between perineural invasion and distant metastasis is still controversial. Mendenhall et al. [9] in their multivariate analysis stated that perineural invasion was a prognostic factor for development of distant metastasis.
ACC has 3 recognised histopathological patterns tubular, cribriform and solid. The cribriform is the most common and solid variant least common subtype. Sometimes one can see all the three subtypes in a single specimen as polymorphism is common in ACC [5]. Our patient had a cribriform pattern which is the most common type. Managing patients with positive margins is challenging. ACC is considered to be a radiosensitive tumor but not radiocurable tumor [7]. Post operative radiation delays rather prevents local recurrence [1]. The optimal therapy for ACC of paranasal sinuses is still not established. Management depends on multiple factors like the site and location of the lesion, lymphatic nodal status, cell type, degree of differentiation and bony involvement. Primary treatment is surgery in combination with radiotherapy. Chemotherapy for ACC has shown limited role and often considered for palliation.
ACC of minor salivary glands has a worse prognosis than those of major salivary glands [5]. Certain markers are implicated in the prognosis which include DNA ploidy, Ki-67 antigen expression, S-Phase value and nucleolar organising regions [10]. The present case was a rare of its kind in presentation with headache and lateral rectus palsy. A high index of suspicion is essential while planning surgery. Studies have shown that ACC frequently develops delayed distant metastasis and needs long term follow up. Bone metastasis is said to be associated with worse prognosis than pulmonary metastasis [4].
Conclusion
ACC of the paranasal sinuses is very rare tumor which presents late and needs high index of suspicion. Early diagnosis and management is the key to minimize treatment failures and morbidity involved. Due to its rarity, there are some arguments over the clinical and histological factors that affect the survival of patients with ACC of the paranasal sinuses. Further studies are essential of the role of adjuvant treatment with radiation and chemotherapy, and quality of life in these patients needs addressal. Long term follow up is essential to check locoregional and distant metastasis.
References
- 1.Wiseman SM, Popat SR, Rigual NR, Hicks WL, Orner JB, Wein RO, McGary CT, Loree TR. Adenoid cystic carcinoma of the paranasal sinuses or nasal cavity: a 40-year review of 35 cases. Ear Nose Throat J. 2002;81(8):510–514. [PubMed] [Google Scholar]
- 2.Shimamoto H, Chindasombatjaroen J, Kakimoto N, Kishino M, Murakami S, Furukawa S. Perineural spread of adenoid cystic carcinoma in the oral and maxillofacial regions: evaluation with contrast-enhanced CT and MRI. Dentomaxillofac Radiol. 2012;41(2):143–151. doi: 10.1259/dmfr/21825064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanna E, Vural E, Prokopakis E, Carrau R, Snyderman C, Weissman J. The sensitivity and specificity of high-resolution imaging in evaluating perineural spread of adenoid cystic carcinoma to the skull base. Arch Otolaryngol Head Neck Surg. 2007;133:541–545. doi: 10.1001/archotol.133.6.541. [DOI] [PubMed] [Google Scholar]
- 4.Sung MW, Kim KH, Kim JW, Min YG, Seong WJ, Roh JL, Lee SJ, Kwon TK, Park SW. Clinicopathologic predictors and impact of distant metastasis from adenoid cystic carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg. 2003;129:1193–1197. doi: 10.1001/archotol.129.11.1193. [DOI] [PubMed] [Google Scholar]
- 5.Pinakapani R, Chaitanya NC, Lavanya R, Yarram S, Boringi M, Waghray S. Adenoid cystic carcinoma of the head and neck—literature review. Qual Prim Care. 2015;23(5):309–314. [Google Scholar]
- 6.Mendenhall WM, Morris CG, Amdur RJ, Werning JW, Hinerman RW, Villaret DB. Radiotherapy alone or combined with surgery for adenoid cystic carcinoma of the head and neck. Head Neck. 2004;26(2):154–162. doi: 10.1002/hed.10380. [DOI] [PubMed] [Google Scholar]
- 7.Leafstedt SW, Gaeta JF, Sako K, Marchetta FC, Shedd DP. Adenoid cystic carcinoma of major and minor salivary glands. Am J Surg. 1971;122:756–762. doi: 10.1016/0002-9610(71)90440-5. [DOI] [PubMed] [Google Scholar]
- 8.Howard DJ, Lund VJ. Reflextions on the management of adenoid cystic carcinoma of nasal cavity and paranasal sinuses. Otolaryngol Head Neck Surg. 1985;93:338–341. doi: 10.1177/019459988509300309. [DOI] [PubMed] [Google Scholar]
- 9.Mendenhall WM, Morris CG, Amdur RJ, Werning JW, Hinerman RW, Villaret DB. Radiotherapy alone or combined with surgery for adenoid cystic carcinoma of the head and neck. Head Neck. 2004;26:154–162. doi: 10.1002/hed.10380. [DOI] [PubMed] [Google Scholar]
- 10.Fordice J, Kershaw C, El-Naggar A, Goepfert H. Adenoid cystic carcinoma of the head and neck: predictors of morbidity and mortality. Arch Otolaryngol Head Neck Surg. 1999;125(2):149–152. doi: 10.1001/archotol.125.2.149. [DOI] [PubMed] [Google Scholar]