Abstract
The aim of this study is to assess the incidence of post traumatic BPPV and evaluate its treatment outcomes in mild and moderate traumatic head injury patients. The study population consisted of 128 patients (89 male:39 female) who were admitted with head and neck injury (Motor Vehicle Accident, Blow to the head, Fall from Height, Whiplash injury) as inpatients in Department of Neurosurgery in Tertiary care hospital in Kerala during a 2 month period from 1st April 2014 to 31st May 2014. The age range was 10–70 years and mean 39.8 with standard deviation 15.5. All cases were evaluated and serially followed up to a period of 6 months in Department of Otorhinolaryngology. In our study, the number of patients with mild injuries (Glasgow coma scale 13–15) were 108 and moderate injury (Glasgow coma scale 9–12) were 20. We found out that post traumatic BPPV was found to be 17% of the traumatic brain injury patients. All patients were treated with particle re-positioning maneuvers and were followed up for a period of 6 months. Recurrence were reported in 9 (40.9%) patients. In these patients re positioning maneuvers were repeated.
Keywords: Benign paroxysmal positional vertigo (BPPV), Traumatic brain injury (TBI), Dix–Hallpike maneuver, Epleys maneuver
Introduction
Traumatic brain injuries (TBI) are becoming increasingly more common in modern society. Dizziness is a common sequelae of traumatic head injury. Owing to the increased frequency of dizziness associated with head and neck injury, it is important for the otolaryngologists to understand the diagnosis and treatment of giddiness associated with head and neck trauma.
The common causes of Head and Neck injury are motor vehicle accidents, fall from height, and blow to the head and/or neck or whiplash injury [1, 2]. Road traffic accidents are major health problems in this new age. India accounts for 10% of the road crash fatalities worldwide [3]. Despite being a small state with just three per cent of India’s total population, Kerala accounts for 12 per cent of the road accidents in the country.
Traumatic brain injury (TBI) is the commonest cause of death and disability in young people. Onset of vertigo can appear immediately or few days after trauma. Patients often avoid positions triggering symptoms. Symptoms may resolve by its own in some patients but there is always a chance for recurrence.
Benign Paroxysmal Positional Vertigo (BPPV) was coined by Dix and Hallpike in 1952 and it is one of the most common peripheral vestibular disorders. Traumatic BPPV accounts for 8.5–20% of all BPPV cases [4, 5]. Benign Paroxysmal Positional Vertigo is a disorder characterized by brief attacks of vertigo, with associated nystagmus, precipitated by certain changes in head position with respect to gravity. Each episode of vertigo typically lasts for 10–20 s. The vertigo is intense and may occasionally be associated with nausea and/or vomiting.
Sometimes vertigo may be the single symptom after TBI disturbing social as well as routine activities of the patient resulting in immense loss of man power as well as economic resources.
Materials and Methods
A prospective observational clinical study was conducted from 1st April 2014 to 31st May 2014 at the Department of Neurosurgery and Department of Otorhinolaryngology in a tertiary care hospital in Kerala after prior clearance from the Institute ethics committee and in accordance with the ethical standards. Follow up of each case was done in the 1st month, 3rd month and 6th month.
In this study among 128 consenting adults, 89 were males and 39, females. These patients were followed up for a period of 6 months. Information regarding the mechanism of injury, level of consciousness, Glasgow coma scale (GCS) scores and vital signs were noted. GCS is a neurological scale comprising eye, verbal and motor response in-order to assess the conscious state of a person for initial and further assessment. Categorical descriptions of the mechanism of injury such as motor vehicle accident, fall from height, blow to the head/neck, whiplash injury were recorded. Recording of mechanism of injury, time and type of vehicle was done. Information regarding whether the patient was having vertigo or seizures at the time of admission and whether the patient underwent any surgical procedure during hospital stay were also noted.
Thorough history, physical and ENT examinations were carried out meticulously in all patients reporting with vertigo. Tests to rule out other causes of peripheral vertigo and central causes were done with help of imaging studies, videonystamography and audiogram. The Dix Hallpike maneuver, considered to be the gold standard for diagnosis of posterior canal BPPV [6, 7] was performed in all patients. Supine head rolling tests were done to find out cases of horizontal canal BPPV [4, 8, 9]. Optic fixation that reduces severity of nystagmus was overcome by using frenzels glasses (glasses with strong prisms for lenses, that remove the ability of the eyes to focus an object) thereby increasing the sensitivity of the Hallpike maneuver. Previous history of vertigo was ruled out (e.g. Degenerating disorders, thyroid disorders, episodic ataxia, CNS tumors, previous history of migraine, otological causes, known cases of Meniere’s disease). Central causes of vertigo were also excluded from the study. Patients with severe TBI (GCS less than 9) were also excluded from study. All patients were followed up after 1, 3 and 6 months. The modality of treatments were Epleys maneuver, Semonts maneuver and prolonged bed rest. Vestibular sedatives were given as an initial treatment in those patients in whom particle re-positioning maneuver were contraindicated. In cases of bilateral BPPV, the right side was tackled first after which re-assessment was done and treated accordingly. If there was recurrence of symptoms, the re-positioning maneuvers were repeated according to which semicircular canal was affected.
Statistical Analysis
It is a prospective observational study. The data obtained were categorical. Descriptive studies, graphs and contingency tables of the data are presented.
Observation and Results
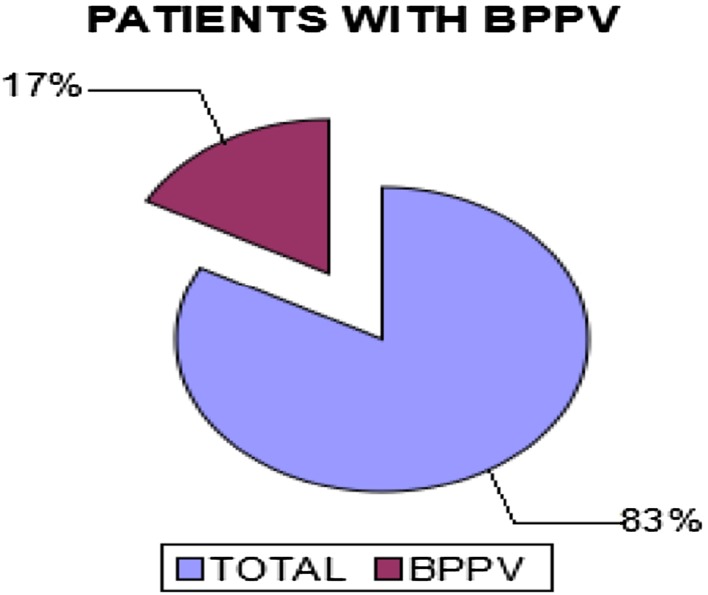
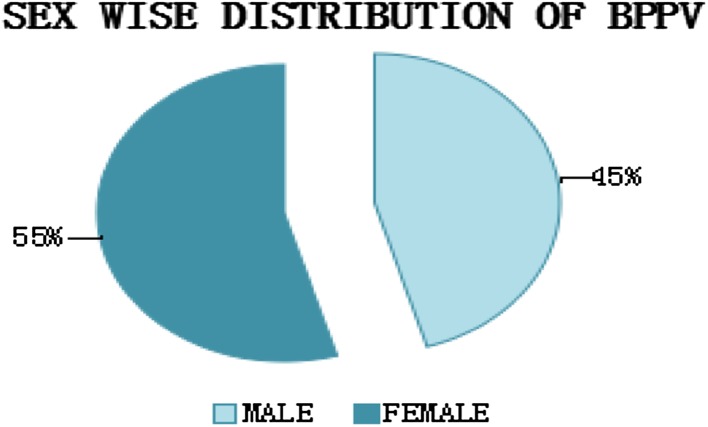
A total of 128 patients were included in the study. Of these 128 patients, 22 patients (17%) were diagnosed with BPPV (Fig. 1). Among 128 patients 89 were male and 39 female in the age group 10–70 years. Among the 22 patients diagnosed with BPPV, 10 (45.5%) were males and 12 (54.5%) were females (Fig. 2).
Fig. 1.
Pie diagram showing the incidence of BPPV in traumatic brain injury
Fig. 2.
Pie diagram illustrating the sex wise distribution of BPPV
In our study, the 2 commonest mechanisms for head trauma were
Road traffic accidents (RTA)
Fall from height.
RTA outnumbered fall from height, and among RTA, two wheeler accidents were most common (41.4%) (Table 1) Patients with in age range of 41–50 were highest in number followed by age range of 21–30 years.
Table 1.
Incidence of traumatic BPPV according to mechanism of injury
| Mechanism of injury | % total patients | % of traumatic BPPV |
|---|---|---|
| RTA (2 wheelers) | 41.4 | 45.45 |
| RTA (pedestrians) | 10.9 | 22.7 |
| RTA (others vehicles) | 27.3 | 9 |
| Fall from height | 20.3 | 22.7 |
All patients with mild and moderate head injury were included in the study. Number of patients with mild injuries were 108 and moderate injury were 20.
All cases were evaluated on admission and followed up. Patients with peripheral vertigo were evaluated in detail and causes for each were diagnosed with all possible investigations that were available in our hospital. Of the 22 patients with BPPV, 18 (81.8%) cases were posterior canal BPPV and 4 (18.2%) cases were horizontal canal BPPV (Fig. 3). Two (9%) patients had bilateral BPPV, while 13 (59.1%) had symptoms towards the right side and 7 (31.8%) had symptoms towards left side. Those patients fit for particle re positioning maneuvers were given treatment and in some patients if contraindicated, they were immediately treated with vestibular sedatives. Recurrence were reported in 9 (40.9%) patients (Table 2) In these patients re-positioning maneuvers’ were repeated.
Fig. 3.
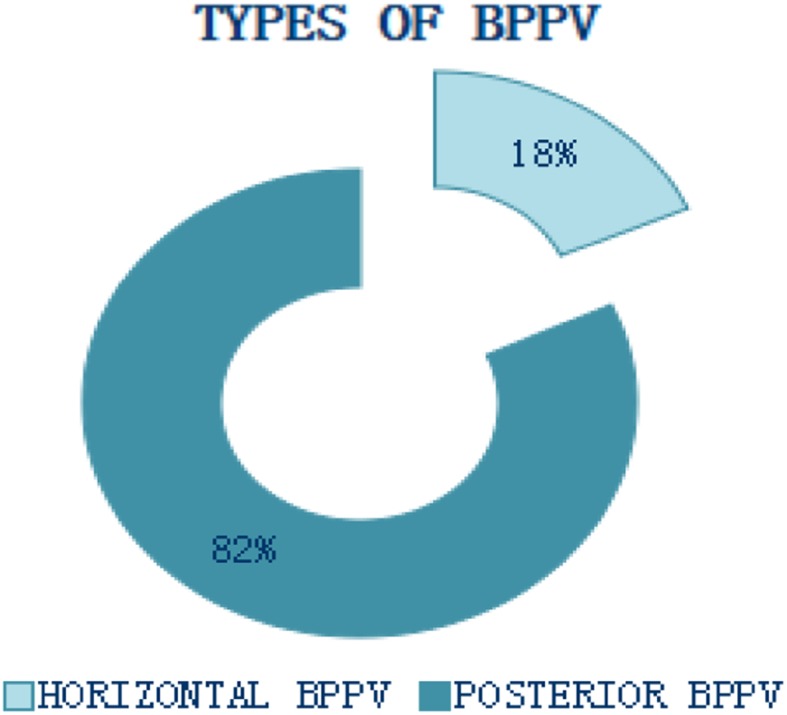
Pie diagram showing the types of BPPV
Table 2.
Clinical features of post traumatic benign paroxysmal positional vertigo
| Patient no. | Sex/age | Cause of injury | Imaging study | Type of BPPV | Laterality/side | Recurrence |
|---|---|---|---|---|---|---|
| 1 | 44/F | RTA | N/L | P-BPPV | B/L | 0 |
| 2 | 46/F | RTA | N/L | P-BPPV | R | 0 |
| 3 | 37/F | RTA | Cerebral concussion | P-BPPV | L | 1 |
| 4 | 24/F | RTA | N/L | P-BPPV | R | 1 |
| 5 | 53/M | RTA | B/L squamous temporal bone # | P-BPPV | L | 0 |
| 6 | 69/F | FALL | N/L | P-BPPV | R | 1 |
| 7 | 60/M | RTA | N/L | P-BPPV | R | 0 |
| 8 | 24/F | RTA | Rt parietal bone # SAH | P-BPPV | L | 0 |
| 9 | 70/M | FALL | N/L | P-BPPV | R | 0 |
| 10 | 30/F | RTA | N/L | P-BPPV | R | 1 |
| 11 | 53/F | FALL | N/L | P-BPPV | L | 0 |
| 12 | 44/F | RTA | EDH | H-BPPV | L | 0 |
| 13 | 64/M | FALL | N/L | P-BPPV | R | 0 |
| 14 | 34/M | RTA | N/L | P-BPPV | R | 0 |
| 15 | 70/M | FALL | SDH | H-BPPV | R | 1 |
| 16 | 49/M | RTA | N/L | P-BPPV | B/L | 0 |
| 17 | 30/F | RTA | Rt temporal bone # | P-BPPV | R | 2 |
| 18 | 43/F | RTA | N/L | P-BPPV | L | 1 |
| 19 | 45/F | RTA | SDH | P-BPPV | R | 0 |
| 20 | 61/M | RTA | Frontal bone # | P-BPPV | L | 1 |
| 21 | 57/M | RTA | N/L | H-BPPV | R | 0 |
| 22 | 32/M | RTA | N/L | H-BPPV | R | 0 |
RTA road traffic accidents, # fracture, EDH extra dural hematoma, SDH subdural hematoma, P-BPPV posterior canal BPPV, H-BPPV horizontal canal BPPV, B/L bilateral, R right, L left
Discussion
A total of 128 patients of mild and moderate head injury (GCS 9–15) were included in the study. There were 89 males and 39 females. The age range was 10–70 years and mean 39.8 with standard deviation 15.5. In our study, of the 128 patients, road traffic accidents (80%) outnumbered those patients with fall (20%). In the study by Guharaj, Epidemiology of traumatic brain injuries: Indian scenario [10] road traffic injuries were the leading cause (60%) of traumatic brain injury followed by falls (20–25%) and violence (10%). Benign paroxysmal positional vertigo should always be considered in those patients with head trauma whose primary complaint is positional vertigo. Griffiths [11] in his study reported the incidence of post traumatic dizziness and imbalance to be 24 and 83% respectively. The most frequent causes of vertigo is following blunt head trauma or whiplash injury [12]. It may present only few days or weeks after head injury and may be bilateral. The late onset of symptomatology can be explained by [13]
Slow degeneration of otolith organ after labyrinthine concussion.
The settling of dislodged otoconia in the utricular cavity before entering the semicircular canal.
The time needed for several pieces of otoconia to form a clot (canalolith) to become causative factor.
Of the 128 patients in our study, 22 patients (17%) were diagnosed with BPPV. Head traumas lead to separation of otoconial debris from the macula and possible sedimentation inside one of the semi-circular canals. Shifting of these particles, due to movement of head and neck, produces an endolymphatic stream which stimulates the ampullar receptors resulting in typical BPPV symptomatology [2]. The pathognomonic clinical sign is postural nystagmus evoked by diagnostic maneuvers. Motin et al. [13] found that, 10 of 20 patients (50%) with severe TBI complained of vertigo elicited by positional changes and were diagnosed as having BPPV. Similarly in the study conducted by Davies and Luxon [14], 25 of 100 patients with dizziness after head trauma were confirmed to have BPPV by a positive Dix–Hallpike test. Ahn et al. [15], in his study on 192 consecutive patients with TBI, 45 patients (23%) who complained of positional vertigo were diagnosed with BPPV.
The majority (69.5%) of the patients in our study were males. Men are more likely to be involved in RTA and in cases of work related injury like fall from height. But incidence of BPPV, in this study was more in females (54.5%). This female prevalence is in conformity with the literature, the Quebec Task Force in particular and a paper by Spitzer et al. [16] whose study on auditory symptoms after blunt head trauma, stated that prevailing trauma mechanisms affected the young women more because of less adequate muscular resistance against the sudden impact.
In the previous study by Ahn et al. [15], the incidence of Horizontal canal BPPV versus Posterior canal BPPV was found to be 1:2.2 and bilateral BPPV at 3.13%. In our study the incidence of horizontal canal BPPV vs posterior canal BPPV is 1:4.5 and bilateral BPPV in 9%. Regarding bilaterality, previous studies [1, 5] have shown that bilateral BPPV accounted for 14.3–19% of the post traumatic BPPV cases.
Our results demonstrated that regardless of the degree of head trauma, the type of post-traumatic dizziness can guide patient outcome and treatment. Those individuals with BPPV are treated by Epley‘s maneuver and Barbeque maneuver depending on the semicircular canal affected. Post procedure restriction of movement was advised for 48 h. All patients were compliant to the treatment. Paroxysmal positional nystagmus was seen with Dix–Hallpike positioning test and was treated with canalith re positioning maneuvers like Epleys or Semont’s liberatory maneuver. In our study, recurrences were reported in 9 patients (40.9%). While recurrence rate reported in the study done by Gordon et al. [1], was 57%, another study by Nunez et al. [17], found the recurrence rate at 26.8%. In the former, the study found that traumatic BPPV required repeated re positioning compared to those with non-traumatic BPPV.
Conclusion
Patients with post traumatic dizziness are a challenging group of individuals. Often, due to cognitive deficits like post traumatic stress disorders, the management of vertiginous symptoms are often ignored. During the period of convalescence, these patients may not manifest any neurological deficits. But the vertigo can be severe enough to affect their daily routine, work, social life resulting in loss of man hours and economic resources. In short, the quality of life is severely hampered.
Accurate diagnosis and timely management helps to ameliorate the symptoms of post-traumatic vertigo. Establishing a diagnosis of BPPV is beneficial since it is treated by relatively simple physical maneuvers without need for additional investigations or drug therapy. The prognosis of this syndrome in proper hands is excellent.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
G. R. Haripriya, Email: itsgrhari@gmail.com
Preethy Mary, Email: preethymarycharles@gmail.com.
Mathew Dominic, Email: mathewmdkent@gmail.com.
Rashmi Goyal, Email: drrashmi03@gmail.com.
Ambily Sahadevan, Email: ambily.sahadevan@gmail.com.
References
- 1.Gordon CR, Levite R, Joffe V, et al. Is post-traumatic benign paroxysmal positional vertigo different from the idiopathic form. Arch Neurol. 2004;61:1590–1593. doi: 10.1001/archneur.61.10.1590. [DOI] [PubMed] [Google Scholar]
- 2.Katsarkas A. Benign paroxysmal positional vertigo (BPPV): idiopathic versus post-traumatic. Acta Otolaryngol (Stockh) 1999;119:745–749. doi: 10.1080/00016489950180360. [DOI] [PubMed] [Google Scholar]
- 3.Mohan D. Road traffic accidents and injuries in India: time for action. Nat Med J India. 2004;17(2):63–66. [PubMed] [Google Scholar]
- 4.Baloh RW, Honrubia V, Jacobson K. Benign positional vertigo: clinical and oculographic features in 240 cases. Neurology. 1987;37(3):371–378. doi: 10.1212/WNL.37.3.371. [DOI] [PubMed] [Google Scholar]
- 5.Katsarkas A, Kirkham TH. Paroxysmal positional vertigo—a study of 255 cases. J Otolaryngol. 1978;7:320–330. [PubMed] [Google Scholar]
- 6.Dix MR, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Proc R Soc Med. 1952;45:341–354. doi: 10.1177/003591575204500604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV) CMAJ. 2003;169:681–693. [PMC free article] [PubMed] [Google Scholar]
- 8.White JA, Coale KD, Catalano PJ, et al. Diagnosis and management of lateral semicircular canal benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2005;133(2):278–284. doi: 10.1016/j.otohns.2005.03.080. [DOI] [PubMed] [Google Scholar]
- 9.Escher A, Ruffieux C, Maire R. Efficacy of the barbecue manoeuvre in benign paroxysmal vertigo of the horizontal canal. Eur Arch Otorhinolaryngol. 2007;264:1239–1241. doi: 10.1007/s00405-007-0337-6. [DOI] [PubMed] [Google Scholar]
- 10.Guharaj G. Epidemiology of traumatic brain injuries: Indian scenario. Neurol Res. 2002;24:24–28. doi: 10.1179/016164102101199503. [DOI] [PubMed] [Google Scholar]
- 11.Griffiths MV. The incidence of auditory vestibular concussion following minor head injury. J Laryngol Otol. 1979;93:253–265. doi: 10.1017/S0022215100086990. [DOI] [PubMed] [Google Scholar]
- 12.Brain Injury.com. Brain Injury association of America 2015. http://www.braininjury.com/injured.shtml. Accessed 5 May 2017
- 13.Motin M, Keren O, Groswasser Z, et al. Benign paroxysmal positional vertigo as the cause of dizziness in patients after severe traumatic brain injury: diagnosis and treatment. Brain Inj. 2005;19:693–697. doi: 10.1080/02699050400013600. [DOI] [PubMed] [Google Scholar]
- 14.Davies RA, Luxon LM. Dizziness following head injury: a neuro-otological study. J Neurol. 1995;242:222–230. doi: 10.1007/BF00919595. [DOI] [PubMed] [Google Scholar]
- 15.Ahn SK, Jeon SY, Kim JP, et al. Clinical characteristics and treatment of benign paroxysmal positional vertigo after traumatic brain injury. J Trauma. 2011;70(2):442–446. doi: 10.1097/TA.0b013e3181d0c3d9. [DOI] [PubMed] [Google Scholar]
- 16.Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining whiplash and its management. Spine (Phila Pa 1976) 1995;20(8 Suppl):1S–73S. [PubMed] [Google Scholar]
- 17.Nunez RA, Cass SP, Furman JM. Short- and long-term outcomes of canalith repositioning for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2000;122:647–652. doi: 10.1016/S0194-5998(00)70190-2. [DOI] [PubMed] [Google Scholar]