Abstract
Purpose
Patients with gastroesophageal reflux disease without esophagitis show varying responses to proton pump inhibitors (PPIs). The aim of this study was to objectively evaluate the effect of a new PPI, ilaprazole, on patients with heartburn but without reflux esophagitis.
Materials and Methods
This prospective study was performed on 20 patients with heartburn but without reflux esophagitis. All patients underwent upper endoscopy and 24-hr combined multichannel intraluminal impedance and pH esophageal monitoring (MII-pH). They were then treated with ilaprazole (20 mg) once daily for 4 weeks. The GerdQ questionnaire, histologic findings, and inflammatory biomarkers were used for assessment before and after ilaprazole.
Results
Among the 20 patients, 13 (65%) showed GerdQ score ≥8. Based on MII-pH results, patients were classified as true nonerosive reflux disease (n=2), hypersensitive esophagus (n=10), and functional heartburn (n=8). After treatment, patients showed a statistically significant improvement in GerdQ score (p<0.001). Among histopathologic findings, basal cell hyperplasia, papillary elongation, and infiltration of intraepithelial T lymphocytes improved significantly (p=0.008, p=0.021, and p=0.008; respectively). Expression of TNF-α, IL-8, TRPV1, and MCP-1 decreased marginally after treatment (p=0.049, p=0.046, p=0.045, and p=0.042; respectively).
Conclusion
Daily ilaprazole (20 mg) is efficacious in improving symptom scores, histopathologic findings, and inflammatory biomarkers in patients with heartburn but no reflux esophagitis.
Keywords: Heartburn, reflux esophagitis, proton pump inhibitors, ilaprazole
INTRODUCTION
Gastroesophageal reflux disease (GERD) is a chronic condition that develops when gastric contents flow into the esophagus and cause troublesome symptoms, such as heartburn and/or acid regurgitation.1 The severity of GERD does not necessarily indicate actual injury to the esophagus. GERD without reflux esophagitis is more common than erosive esophagitis and is sometimes called non-erosive reflux disease (NERD). NERD seems to differ from reflux esophagitis in relation to pathophysiology and clinical characteristics; moreover, it is known to exhibit a lower response rate to proton pump inhibitors (PPIs) than erosive esophagitis.2 However, recent investigations insisted that responses to PPI in NERD are equal to those in erosive gastritis.3
Patients with GERD without reflux esophagitis show varying characteristics. Savarino, et al.4 sub-classified patients into three subtypes based on findings of pH esophageal monitoring: 1) true NERD, with abnormal distal esophageal acid exposure time (AET); 2) hypersensitive esophagus, defined as normal distal esophageal AET and positive symptom association for either acid and/or non-acid reflux; and 3) functional heartburn with normal distal esophageal AET and negative symptom association for acid and nonacid reflux.
PPIs are the most effective drugs for the treatment of GERD. Many PPIs have been developed and widely used for the management of acid-related diseases, such as peptic ulcers and GERD. PPIs are highly recommended for the management of NERD and are thought to provide symptomatic improvement. 5 Ilaprazole is the latest PPI and is almost equivalent to omeprazole for control of gastric acid secretion.6 It is considered to improve symptoms. It has a prolonged half-life, compared to other PPIs, and shows powerful dose-dependent inhibition of symptoms. Its safety is similar to that of omeprazole.7 Although a few studies have been published on the efficacy of ilaprazole for treatment of acid-related diseases,6,8,9 studies on the efficacy of ilaprazole for NERD are lacking.
Herein, we prospectively investigated the efficacy of ilaprazole for treatment of patients with heartburn but without reflux esophagitis, as assessed by 24-hr combined multichannel intraluminal impedance and pH esophageal monitoring (MII-pH) using standardized histologic criteria and inflammatory biomarkers.
MATERIALS AND METHODS
Patients
Eligible patients included adults who had heartburn lasting for more than 6 months and occurring at least twice weekly and who were treated at Severance Hospital, Korea between July 2014 and August 2015. Patients were between the ages of 20 and 80 years. They showed no erosion at the gastroesophageal junction in esophagogastroduodenoscopy. Potential study participants were screened and enrolled by a research coordinator. Written informed consent was obtained from each patient before enrollment. The study protocol was approved by the Yonsei University College of Medicine Ethics Committee (Institutional Review Board Number: 4-2014-0110) and was registered at ClinicalTrials.gov (NCT02666976).
Study design
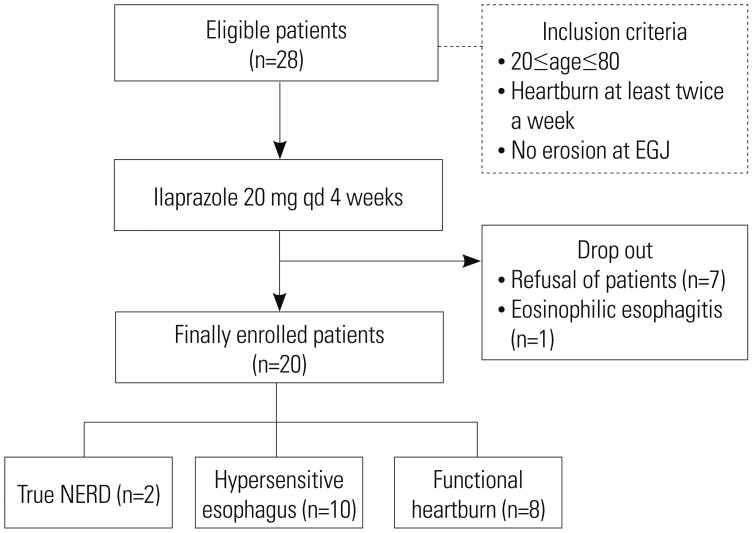
This study was undertaken as a single-center, open-label, single-arm, prospective study to objectively evaluate the efficacy of ilaprazole (Noltec®; IL-YANG Pharmaceutical Co., Ltd., Seoul, Korea) for GERD. The study design is shown in Fig. 1. The intra-esophageal pressure of all subjects was tested, and they underwent MII-pH. The results of MII-pH were used to classify patients into three groups: a true NERD group, a hypersensitive esophagus group, and functional heartburn group. Patients completed GerdQ questionnaires regarding their symptoms. They were treated with ilaprazole (20 mg) once daily for 4 weeks. After treatment, all subjects completed esophagogastroduodenoscopy and the GerdQ questionnaire again. Other substances that could influence the relief of symptoms related to acid secretion were not permitted during the study. We aimed to enroll 37 patients; however, the study was concluded prematurely owing to the difficulty of subject enrollment and the prolonged study period.
Fig. 1. Study design. NERD, non-erosive reflux disease; EGJ, esophagogastric junction.
Endoscopy and sampling for inflammatory and histologic evaluation
The gastroesophageal junction was defined as the most proximal extent of the gastric folds during endoscopy. Before and after treatment, three tissue samples for histologic evaluation and three tissue samples for inflammatory biomarker evaluation were obtained from 3 cm above the gastroesophageal junction, respectively. Fresh tissues for biomarker evaluation were maintained at −80℃ until measurement of messenger RNA (mRNA). Total mRNA was extracted according to the manufacturer's instructions using TRIzol reagent (Invitrogen Life Technologies, Carlsbad, CA, USA). For complementary DNA synthesis, total RNA was reverse transcribed using SuperScript™ II (Invitrogen) following the manufacturer's protocol. Quantitative polymerase chain reaction (qPCR) was performed using iQ SYBR Green Supermix (Applied Biosystems Inc., Carlsbad, CA, USA) and conducted on a Roche Light Cycler480 Real-Time PCR System (Idaho Technology Inc., Salt Lake City, UT, USA). The target sequences for qPCR were as follows: tumor necrosis factor-alpha (TNF-α) (F-5′CAGCCTCTTCTCCTTCCTGAT3′; R-5′GCCAGAGGGCTGATTAGAGA3′), interleukin 8 (IL-8) (F-5′GCAGCCTTCCTGATTTCTGCAGCTC3′; R-5′ACTTCTCCACAACCCTCTGCACCCA3′), interleukin- 1 beta (IL-1β) (F-5′CCAGCTACGAATCTCGGACCACC3′; R-5′TTAGGAAGACACAAATTGCATGGTGAAGTCAGT3′), transient receptor potential vanilloid 1 (TRPV1) (F-5′GAGTTTCAGGCAGACACTGGAA3′; R-5′CTATCTCGAGCACTTGCCTCTCT3′), monocyte chemoattractant protein-1 (MCP-1) (F-5′GATCTCAGTGCAGAGGCTCG3′; R-5′TGCTTGTCCAGGTGGTCCAT3′), glyceraldehyde 3-phosphate dehydrogenase (GAPDH) (F-5′CCGGGAAACTGTGGCGTGATGG3′; R-5′AGGTGGAGGAGTGGGTGTCGCTGTT3′). GAPDH was used as an endogenous control, and the Ct value was normalized to GAPDH using the 2−ΔΔCt method. Only reliable quantitative real-time PCR (qRT-PCR) data points were used for analysis.
Histopathologic evaluation
Histologic findings included basal cell hyperplasia, papillary elongation, dilated intercellular spaces (DIS), intraepithelial eosinophils, and intraepithelial T lymphocytes. All specimens were assessed by a single histologist (H.K.). To classify the severity of the histologic findings, we used the histologic criteria and severity score (score range, 0–2) set by the Esohisto project.10,11
Manometric study
We used an eight-channel, water-perfused esophageal manometry catheter (MUI Scientific Company, Mississauga, ON, Canada) and a water-perfused, low-compliance perfusion system (Synetics Medical Co., Stockholm, Sweden). The manometric analysis was performed before the MII-pH study. During the esophageal manometry study, we evaluated variable parameters, such as the resting lower esophageal sphincter (LES) pressure, the length of LES, the amplitude of pressure waves, and the duration of pressure waves.
24-hr combined multichannel intraluminal impedance and pH esophageal monitoring
MII-pH was performed before treatment using an ambulatory multichannel intraluminal impedance and pH monitoring system (Sleuth; Sandhill Scientific, Inc., Highland Ranch, CO, USA). The DeMeester score, distal esophageal AET, total number of reflux episodes, symptom association probability (SAP), and the symptom index (SI) were determined. The distal esophageal AET was defined as the total time with a pH <4, divided by the total monitoring time. A percent time <4.2% with pH <4 over 24 hours was referred to as normal. Pathologic acid reflux was defined as a distal esophageal acid exposure percent time >4.2%.4
The SAP was calculated for acid and nonacid reflux using a custom-made Excel macro function. The SAP was considered to be positive at ≥95%.12 The SI was calculated using the Bioview analysis software (Sandhill Scientific, Inc.). It was defined as the number of symptoms associated with reflux divided by the total number of symptoms. The SI was considered to be positive when ≥50%.13 We defined a positive symptom association for reflux as either a positive SAP or a positive SI.
Outcome measures
Our aim was to demonstrate the efficacy of ilaprazole for GERD without reflux esophagitis. To assess the improvement of symptoms, all patients completed the GerdQ questionnaire before and after taking ilaprazole. The questionnaire is composed of six items and can be used as a diagnostic tool for GERD. It has also been used as a tool for evaluating PPI responses in GERD patients.14 We classified 20 patients as either those in whom GERD was well-controlled with PPI therapy (responders) or those in whom it was not well-controlled with PPI therapy (partial responders). Responders were defined as patients who reported 0 days of having heartburn (question 1), regurgitation (question 2), sleep disturbance (question 5), or over-the-counter acid suppressive medication use (question 6) during the preceding week. We defined partial responsiveness in PPI users as more than 1 day of experiencing any one of heartburn, regurgitation, sleep disturbances, and additional medications, as reported in the GerdQ.15 Our secondary endpoint included changes in histological findings and inflammatory biomarkers on tissue analysis after treatment.
Statistical analysis
Calculations were performed using SPSS statistical software, version 18.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as means±standard deviation, and discrete variables are expressed as numbers and percentages. The baseline characteristics of the patients in the three groups were compared using the chi-squared test or Fisher's exact test, one-way ANOVA, and the Kruskal-Wallis test. Paired comparisons of parameters before and after taking ilaprazole were performed using a paired t-test or a Wilcoxon signed-rank test. Results are presented as odds ratios, 95% confidence intervals, and p values. p≤0.05 was considered statistically significant. Using a significance level of 5% and a statistical power of 90% with a two-sided test, a sample size of 37 patients was required for our treatment group, assuming a 30% drop-out rate.
RESULTS
The patient's characteristics and marker of histology and inflammation before treatment
Twenty-eight individuals participated in our study. Of these subjects, 8 patients were excluded from the study; 7 patients discontinued due to improvement of symptoms or unexpected patient refusal, and 1 patient was diagnosed with eosinophilic esophagitis based on their histological results (Fig. 1). The mean age of the 20 patients was 59.5±9.4 years, and the patients included 16 females and 4 males (80% and 20%, respectively; ratio=4:1). All 20 patients had previous history of PPI use, and 14 patients (70%) responded to PPI. The mean GerdQ score before treatment was 11.1±2.1. Thirteen patients (65%) had a GerdQ score of 8 or more at baseline. There were eight responders and 12 partial responders after taking ilaprazole.
The baseline clinical characteristics and parameters of MII-pH are presented in Table 1. Eight patients (40%) were classified as having functional heartburn. The remaining patients were defined with true NERD (n=2, 10%) and a hypersensitive esophagus (n=10, 50%). The hypersensitive esophagus group comprised five with an acid-sensitive esophagus and five with a weak acid-sensitive esophagus. The proportion of patients with a GerdQ score 8 or more was significantly higher in the true NERD (100%) and hypersensitive esophagus (70%) groups, compared to functional heartburn group (50%) (p<0.001). Among the findings of MII-pH analysis, baseline AET was significantly higher in patients with true NERD than those with hypertensive esophagus and functional heartburn (p<0.001). No differences in manometric parameters were observed among subtypes.
Table 1. The Baseline Characteristics and Results of MII-pH.
| Characteristics | True NERD | Hypersensitive esophagus | Functional heartburn | Total | p value |
|---|---|---|---|---|---|
| Mean age (yr) | 69.0±12.7 | 59.2±10.7 | 57.4±6.1 | 59.5±9.4 | 0.307 |
| Male (%) | 1 (50.0) | 2 (20.0) | 1 (12.5) | 4 (20.0) | 0.740 |
| GerdQ score | 11.0±1.4 | 11.1±1.9 | 11.1±2.6 | 11.1±2.1 | 0.997 |
| GerdQ≥8 | 2/2 | 7/10 | 4/8 | 13/20 | <0.001 |
| Responder/partial responder | 0/2 | 5/5 | 3/5 | 8/12 | 0.413 |
| MII-pH parameters | |||||
| Acid exposure time (%) | 10.0±4.5 | 1.1±1.2 | 0.5±0.7 | 1.7±3.2 | <0.001 |
| Total number of reflux episodes | 49.0±46.2 | 32.0±15.3 | 42.4±33.7 | 37.8±26.1 | 0.601 |
| Acid reflux (%) | 37.5±34.6 | 14.9±12.1 | 13.3±8.3 | 16.5±14.5 | 0.088 |
| Length of abdominal LES (cm) | 3.5±2.1 | 3.4±1.0 | 2.4±0.7 | 3.0±1.1 | 0.100 |
| LES pressure (mm Hg) | 19.4±4.7 | 14.5±5.0 | 13.0±2.7 | 14.4±4.4 | 0.196 |
| Amplitude pressure waves (mm Hg) | 98.4±42.3 | 70.6±21.7 | 70.6±20.9 | 73.4±23.5 | 0.299 |
| Duration pressure waves (sec) | 4.1±0.2 | 3.4±0.6 | 3.5±0.3 | 3.5±0.5 | 0.208 |
NERD, non-erosive reflux disease; MII-pH, multichannel intraluminal impedance and pH esophageal monitoring; LES, lower esophageal sphincter.
No differences in TNF-α, IL-8, IL-1β, TRPV1, and MCP-1 among subtypes (Table 2). Among the pre-treatment histological findings, there was no difference among the subgroups, except in infiltration of intraepithelial T lymphocytes, which was higher in the hypersensitive esophagus group than in the functional heartburn group (p=0.03). The DIS and infiltration of intraepithelial eosinophils were more clustered to scores 0 to 1, compared to other histologic findings.
Table 2. Inflammatory and Histologic Findings at Baseline.
| Parameters | True NERD | Hypersensitive esophagus | Functional heartburn | Total | p value |
|---|---|---|---|---|---|
| Inflammatory markers | |||||
| TNF-α* | 0.66±0. 61 | 0.24±4.77 | 3.53±4.39 | 2.61±4.39 | 0.742 |
| IL-8* | 2.50±0.40 | 4.45±6.94 | 6.73±11.09 | 5.09±8.19 | 0.783 |
| IL-1β* | 0.27±0.15 | 0.34±0.12 | 0.38±0.23 | 0.35±0.17 | 0.724 |
| TRPV1* | 0.24±0.14 | 0.63±0.89 | 1.02±0.90 | 0.74±0.85 | 0.475 |
| MCP-1* | 9.19±3.17 | 15.09±9.70 | 19.62±12.88 | 16.00±10.55 | 0.477 |
| Histologic markers (score/number)† | |||||
| Basal cell hyperplasia | 2/2 | 9/10 | 10/8 | 0.656 | |
| Papillary elongation | 2/2 | 8/10 | 6/8 | 0.098 | |
| DIS | 0/2 | 19/10 | 4/8 | 0.391 | |
| Eosinophils | 0/2 | 10/10 | 0/10 | 0.348 | |
| T lymphocytes | 3/2 | 14/10 | 9/10 | 0.030 |
NERD, non-erosive reflux disease; TNF-α, tumor necrosis factor-alpha; IL-8, interleukin 8; IL-1β, interleukin-1 beta; TRPV1, transient receptor potential vanilloid 1; MCP-1, monocyte chemoattractant protein-1; qRT-PCR, quantitative real time polymerase chain reaction; GAPDH, glyceraldehyde 3-phosphate dehydrogenase; DIS, dilated intercellular spaces.
*TNF-α, IL-8, IL-1β, TRPV1, and MCP-1 were measured by qRT-PCR. GAPDH was used as the endogenous control. The Ct values of TNF-α, IL-8, TRPV1, and MCP-1 were normalized to GAPDH using the 2−ΔΔCt method. Fold-change in TNF-α, IL-8, TRPV1, and MCP-1 compared to GAPDH was amplified by 104-fold for convenience. Some samples were not sufficient to perform qRT-PCR, and only reliable qRT-PCR data points were used for analysis (TNF-α: 16; IL-8: 18; IL-1β: 19; TRPV1: 18; MCP-1:14). †Histologic marker represented as the sum of score/number of patients in each subgroup. Histologic findings include basal cell hyperplasia, papillary elongation, DIS, intraepithelial eosinophils, and intraepithelial T lymphocytes.
Efficacy of ilaprazole on GerdQ, histology, and inflammatory cytokines
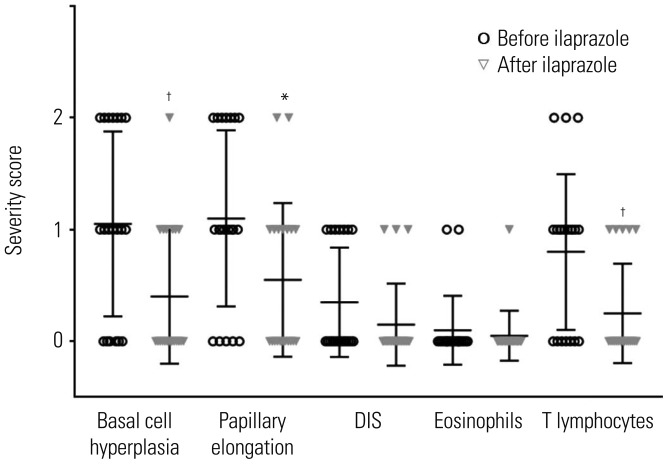
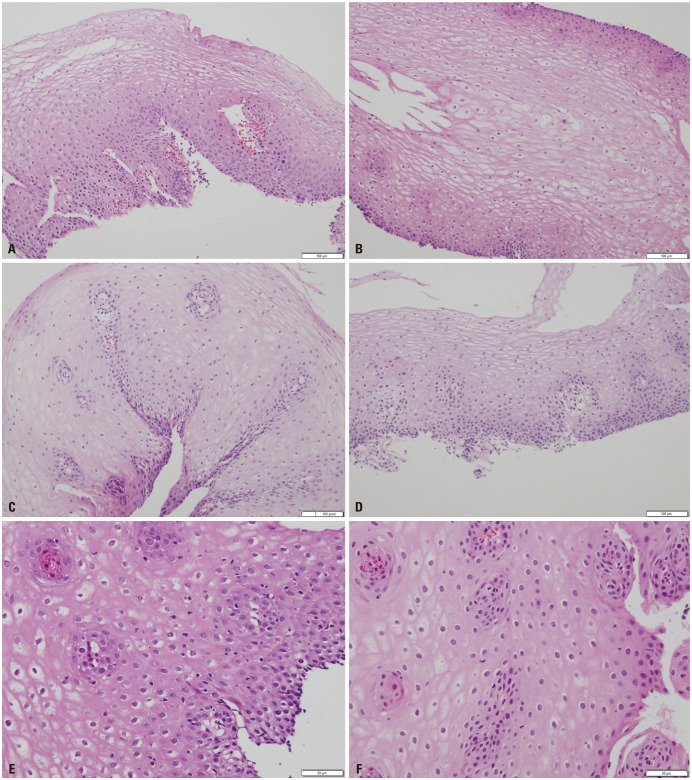
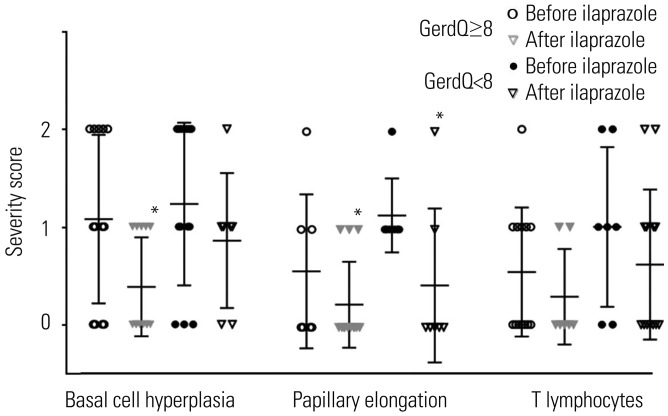
The histopathologic findings revealed decreases in scores for all parameters after ilaprazole treatment. Some findings, such as basal cell hyperplasia, papillary elongation, and infiltration of intraepithelial T lymphocytes, were improved significantly (p=0.008, p=0.021, p=0.008; respectively) (Fig. 2). Improvement of basal cell hyperplasia, papillary elongation, and infiltration of intraepithelial T lymphocytes were clearly demonstrated with hematoxylin and eosin (H&E) staining (Fig. 3).
Fig. 2. Histologic findings before and after treatment: basal cell hyperplasia (p=0.008); papillary elongation (p=0.021); DIS (p=0.391); infiltration of intraepithelial eosinophils (p=0.348); infiltration of intraepithelial T lymphocytes (p=0.008). *p<0.05, †p<0.01. DIS, dilated intercellular spaces; eosinophils, infiltration of intraepithelial eosinophils; T lymphocytes, infiltration of intraepithelial T lymphocytes.
Fig. 3. Representative cases showing changes in histologic findings after treatment with ilaprazole. Several histologic findings showed improvement following treatment. The thickness of the basal layer changed from 40% (H&E, ×100) (A) to 10% (H&E, ×100) (B). The length of papillae changed from 80% (H&E, ×100) (C) to 40% (H&E, ×100) (D) of the total epithelial thickness. Infiltration of T lymphocytes changed from 16/high power field (H&E, ×200) (E) to 4/high power field (H&E, ×200) (F). H&E, hematoxylin and eosin.
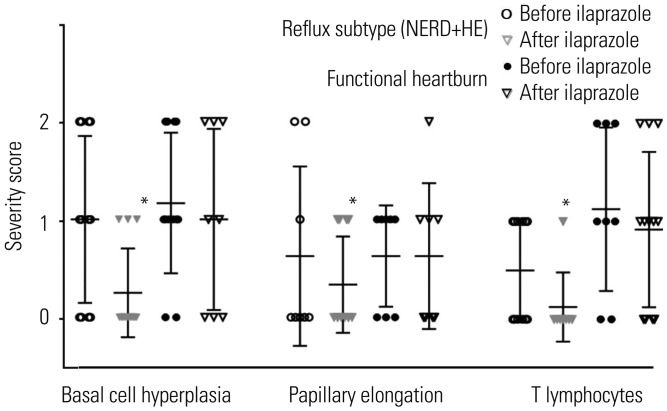
When we analyzed three histologic findings between refluxrelated subtype (true NERD+hypersensitive esophagus group) and functional heartburn, the degrees of basal cell hyperplasia, papillary elongation, and infiltration of intraepithelial T lymphocytes were reduced significantly in reflux-related subtype (p=0.034, p=0.023, and p=0.034, respectively) (Fig. 4). In patients with heartburn, none of the three findings showed any difference before and after treatment. Next, we analyzed the histologic responses between patients with GerdQ ≥8 and GerdQ <8 (Fig. 5). Similarly, the degrees of basal cell hyperplasia and papillary elongation were reduced significantly patients with GerdQ ≥8 (p=0.043, and p=0.048; respectively).
Fig. 4. Histologic responses between reflux-related subtype (true NERD+hypersensitivity group) and proton pump inhibitor-responsive functional heartburn groups. The degrees of basal cell hyperplasia (p=0.034), papillary elongation (p=0.023), and infiltration of intraepithelial T lymphocytes (p=0.034) were reduced significantly in the reflux-related group. *p<0.05. T lymphocytes, infiltration of intraepithelial T lymphocytes. NERD, nonerosive reflux disease; HE, hypersensitive esophagus.
Fig. 5. Histologic responses between patients with GerdQ ≥8 and GerdQ <8. The degrees of basal cell hyperplasia (p=0.043) and papillary elongation (p=0.048) were reduced significantly patients with GerdQ ≥8. The papillary elongation was reduced significantly in patients with GerdQ <8 (p=0.038). *p<0.05. T lymphocytes, infiltration of intraepithelial T lymphocytes.
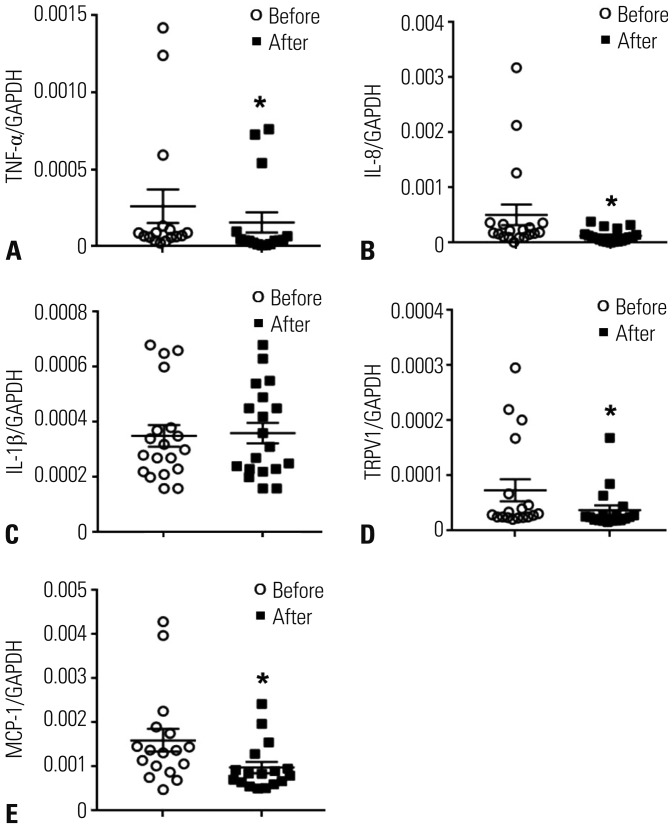
Among the inflammatory cytokines examined, expression of TNF-α (p=0.049), IL-8 (p=0.046), TRPV1 (p=0.045), and MCP1 (p=0.042) were decreased significantly after treatment with ilaprazole (Fig. 6). However, IL-1β did not change after treatment.
Fig. 6. Inflammatory biomarkers before and after treatment. (A) TNF-α, (B) IL-8, (C) IL-1β, (D) TRPV1, and (E) MCP-1 were measured by qRT-PCR. GAPDH was used as the endogenous control. The Ct values of TNF-α, IL-8, TRPV1, and MCP-1 were normalized to GAPDH using the 2−ΔΔCt method. Some samples were not sufficient to perform qRT-PCR, and only reliable qRT-PCR data points were used for analysis (TNF-α: 16; IL-8: 18; IL-1β: 19; TRPV1: 18; MCP-1: 14). *p<0.05. TNF-α, tumor necrosis factor-alpha; IL-8, interleukin 8; IL-1β, interleukin-1 beta; TRPV1, transient receptor potential vanilloid 1; MCP-1, monocyte chemoattractant protein-1; qRT-PCR, quantitative real time polymerase chain reaction; GAPDH, glyceraldehyde 3-phosphate dehydrogenase.
After treatment, the patients' GerdQ scores were significantly reduced (11.1±2.1 and 3.2±3.0, p<0.001). There were eight responders (44%) and 12 partial responders. There was no difference in the proportion of respondents according to the subtype of GerdQ score and MII-pH results.
DISCUSSION
This is the first prospective study to show the effect of ilaprazole on patients with GERD without reflux esophagitis, using not only subjective measures, such as GerdQ scores, but also objective methods, including standardized histologic parameters and inflammatory markers. Ilaprazole significantly improved histologic findings, including basal cell hyperplasia, papillary elongation, and infiltration of intraepithelial T lymphocytes. This histologic improvement was specifically observed only in reflux-subtypes, compared to functional heartburn.
We attempted to measure symptoms objectively, using the GerdQ questionnaire as a symptom rating scale. A GerdQ score of 8 has been determined to be an appropriate cutoff value in a Japanese population.16 In this study, 65% of patients showed GerdQ ≥8. After treatment with ilaprazole, 18 of 20 patients showed a GerdQ score <8. Among them, 12 patients were classified as partial responders. Considering that the number of individuals with functional heartburn was not small in this study, the response rate to ilaprazole is relatively high. We hypothesize that the patients in the functional heartburn group might have been primarily composed of PPI responders in this study; this could have induced the high rate of responses to ilaprazole observed among the functional heartburn group in our study.
In our study, we adapted the MII-pH to subdivide the patients into three groups. The proportion of patients with true NERD/hypersensitive esophagus/functional heartburn was 10%/50%/40%. The ratio of patients with functional heartburn correlated well with a previous report, although the number of patients with true NERD was somewhat lower than in previous studies.17,18,19
Recently, microscopic changes in GERD have received attention as diagnostic and monitoring tools. Pathologic reflux in the esophagus results in injury to epithelial cells of the mucosa. It can lead to promotion of cell turnover and basal cell hyperplasia. Hyperemia of the capillaries presents as papillary elongation.20 Infiltration of lymphocytes appears to be more frequent than infiltration with eosinophilic or neutrophilic granulocytes.21 A previous study showed significant histopathological differences between NERD and functional heartburn.22 According to our data, only infiltration of intraepithelial T cells differed between the two. This discrepancy with previous reports might be caused by the small sample size, as we could only include two cases of true NERD in this study. We tried to resolve this issue over the course of the study, but had difficulty in enrolling patients and eventually had to terminate it early.
Basal cell hyperplasia, papillary elongation, and infiltration of T lymphocytes were improved after treatment in all patients in this study. All of these histologic markers have been recognized as evidence of reflux disease.23 As studied earlier, whether histologic changes revert to normal can be used to judge the efficacy of PPIs, such as esomezole.24 Ilaprazole also improved these microscopic findings in the present study. Herein, we found that histologic improvement is generally seen only in patients with a reflux subtype or GERD ≥8 score. These results show that ilaprazole is involved in the pathophysiologic process by reflux.
Among histologic changes, DIS is known as an early marker of tissue injury in GERD and NERD.25 A previous study demonstrated that DIS is well correlated with AET of the distal esophagus in NERD and that patients with abnormal AET are more likely to show DIS than those with normal AET.26 In our study, DIS did not change after ilaprazole. These results suggest that DIS is a good indicator of acid reflux, although our study included too few patients with true NERD, suggesting that its impact was markedly reduced. In fact, the basal score of DIS and infiltration of eosinophil were almost clustered to scores of 0 to 1 before treatment. For this reason, DIS and infiltration of eosinophil were not good indicators of treatment responses in our study. In this study, DIS was measured by H&E staining, not by electron microscopy. This fact may be a factor in reducing the importance of DIS.
Recent studies have demonstrated that some immune mechefanisms are mediated by specific cytokines or chemokines in GERD.27 IL-8 is a neutrophil chemotactic factor that plays a crucial role in inducing inflammation and is a representative chemokine in the pathogenesis of NERD.28 IL-1β also appears to play an important role therein, including inflammation and fibrosis, and is known to be related to NERD.29 TNF-α induced transcription of oncogenes, such as c-myc, and its epithelial expression was increased in the progress of Barrett's esophagus to adenocarcinoma. IL-1β and TNF-α may be related to the Barrett's esophagus-dysplasia-carcinoma sequence.27 MCP-1 attracts monocytes and lymphocytes and was higher in patients with reflux esophagitis than healthy controls.27
TRPV1 has been implicated in the mechanism of acid-induced inflammation in GERD.30 These markers were tested for use as tools in determining the efficacy of drugs in treating NERD. The expression of IL-8, IL-1β, and MCP-1 was decreased by treatment with PPIs, such as lansoprazole.31,32,33 In our study, all inflammatory biomarkers except IL-1β decreased after taking ilaprazole, with moderate amplitudes.
This study has some limitations. First, the number of subjects was small because the study was ended due to poor enrollment. However, the subgroup proportions were similar to those reported in studies of large populations. This means there will be less bias, even though the number of patients with true NERD was only two. Second, we had no control group. To improve confidence, a comparison study between the efficacy of ilaprazole and that of other PPIs is required. Third, we did not consider the placebo effect of ilaprazole itself in our results. Ilaprazole is expected to show a placebo effect on symptomatic responses, similar to other PPIs.34 To complement these facts, we introduced a highly objective method, including histological exams and use of biomarkers, in order to exclude a possible placebo effect. Fourth, we only had a single pathologist interpret the histologic findings.
Despite these limitations, we showed that ilaprazole is effective in treatment of GERD patients without esophagitis in terms of symptoms, histology, and inflammation. Further study with a larger number of patients with NERD, however, is needed to validate our findings.
ACKNOWLEDGEMENTS
This study was supported and funded by the IL-YANG Pharmaceutical Co., Ltd.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710–717. doi: 10.1136/gut.2004.051821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dent J. Microscopic esophageal mucosal injury in nonerosive reflux disease. Clin Gastroenterol Hepatol. 2007;5:4–16. doi: 10.1016/j.cgh.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 3.Savarino E, Zentilin P, Savarino V. NERD: an umbrella term including heterogeneous subpopulations. Nat Rev Gastroenterol Hepatol. 2013;10:371–380. doi: 10.1038/nrgastro.2013.50. [DOI] [PubMed] [Google Scholar]
- 4.Savarino E, Zentilin P, Tutuian R, Pohl D, Casa DD, Frazzoni M, et al. The role of nonacid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103:2685–2693. doi: 10.1111/j.1572-0241.2008.02119.x. [DOI] [PubMed] [Google Scholar]
- 5.Dean BB, Gano AD, Jr, Knight K, Ofman JJ, Fass R. Effectiveness of proton pump inhibitors in nonerosive reflux disease. Clin Gastroenterol Hepatol. 2004;2:656–664. doi: 10.1016/s1542-3565(04)00288-5. [DOI] [PubMed] [Google Scholar]
- 6.Ji XQ, Du JF, Chen G, Chen G, Yu B. Efficacy of ilaprazole in the treatment of duodenal ulcers: a meta-analysis. World J Gastroenterol. 2014;20:5119–5123. doi: 10.3748/wjg.v20.i17.5119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Periclou AP, Goldwater R, Lee SM, Park DW, Kim DY, Cho KD, et al. A comparative pharmacodynamic study of IY-81149 versus omeprazole in patients with gastroesophageal reflux disease. Clin Pharmacol Ther. 2000;68:304–311. doi: 10.1067/mcp.2000.109155. [DOI] [PubMed] [Google Scholar]
- 8.de Bortoli N, Martinucci I, Giacchino M, Blandizzi C, Marchi S, Savarino V, et al. The pharmacokinetics of ilaprazole for gastroesophageal reflux treatment. Expert Opin Drug Metab Toxicol. 2013;9:1361–1369. doi: 10.1517/17425255.2013.813018. [DOI] [PubMed] [Google Scholar]
- 9.Du YQ, Guo WY, Zou DW, Zhan XB, Li Z, Hu JH, et al. Acid inhibition effect of ilaprazole on Helicobacter pylori-negative healthy volunteers: an open randomized cross-over study. J Dig Dis. 2012;13:113–119. doi: 10.1111/j.1751-2980.2011.00557.x. [DOI] [PubMed] [Google Scholar]
- 10.Fiocca R, Mastracci L, Riddell R, Takubo K, Vieth M, Yerian L, et al. Development of consensus guidelines for the histologic recognition of microscopic esophagitis in patients with gastroesophageal reflux disease: the Esohisto project. Hum Pathol. 2010;41:223–231. doi: 10.1016/j.humpath.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 11.Yerian L, Fiocca R, Mastracci L, Riddell R, Vieth M, Sharma P, et al. Refinement and reproducibility of histologic criteria for the assessment of microscopic lesions in patients with gastroesophageal reflux disease: the Esohisto Project. Dig Dis Sci. 2011;56:2656–2665. doi: 10.1007/s10620-011-1624-z. [DOI] [PubMed] [Google Scholar]
- 12.Weusten BL, Roelofs JM, Akkermans LM, Van Berge-Henegouwen GP, Smout AJ. The symptom-association probability: an improved method for symptom analysis of 24-hour esophageal pH data. Gastroenterology. 1994;107:1741–1745. doi: 10.1016/0016-5085(94)90815-x. [DOI] [PubMed] [Google Scholar]
- 13.Ward BW, Wu WC, Richter JE, Lui KW, Castell DO. Ambulatory 24-hour esophageal pH monitoring. Technology searching for a clinical application. J Clin Gastroenterol. 1986;8(Suppl 1):59–67. doi: 10.1097/00004836-198606001-00009. [DOI] [PubMed] [Google Scholar]
- 14.Tielemans MM, van Oijen MG. Online follow-up of individuals with gastroesophageal reflux disease using a patient-reported outcomes instrument: results of an observational study. BMC Gastroenterol. 2013;13:144. doi: 10.1186/1471-230X-13-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tielemans MM, Jansen JB, van Oijen MG. Open access capture of patients with gastroesophageal reflux disease using an online patient-reported outcomes instrument. Interact J Med Res. 2012;1:e7. doi: 10.2196/ijmr.2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suzuki H, Matsuzaki J, Okada S, Hirata K, Fukuhara S, Hibi T. Validation of the GerdQ questionnaire for the management of gastrooesophageal reflux disease in Japan. United European Gastroenterol J. 2013;1:175–183. doi: 10.1177/2050640613485238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quigley EM. Non-erosive reflux disease, functional heartburn and gastroesophageal reflux disease; insights into pathophysiology and clinical presentation. Chin J Dig Dis. 2006;7:186–190. doi: 10.1111/j.1443-9573.2006.00266.x. [DOI] [PubMed] [Google Scholar]
- 18.Savarino E, Zentilin P, Tutuian R, Pohl D, Gemignani L, Malesci A, et al. Impedance-pH reflux patterns can differentiate non-erosive reflux disease from functional heartburn patients. J Gastroenterol. 2012;47:159–168. doi: 10.1007/s00535-011-0480-0. [DOI] [PubMed] [Google Scholar]
- 19.Long JD, Orlando RC. Nonerosive reflux disease: a pathophysiologic perspective. Curr Gastroenterol Rep. 2008;10:200–207. doi: 10.1007/s11894-008-0044-5. [DOI] [PubMed] [Google Scholar]
- 20.Stolte M, Vieth M, Schmitz JM, Alexandridis T, Seifert E. Effects of long-term treatment with proton pump inhibitors in gastro-oesophageal reflux disease on the histological findings in the lower oesophagus. Scand J Gastroenterol. 2000;35:1125–1130. doi: 10.1080/003655200750056574. [DOI] [PubMed] [Google Scholar]
- 21.Vieth M, Peitz U, Labenz J, Kulig M, Nauclér E, Jaspersen D, et al. What parameters are relevant for the histological diagnosis of gastroesophageal reflux disease without Barrett's mucosa? Dig Dis. 2004;22:196–201. doi: 10.1159/000080319. [DOI] [PubMed] [Google Scholar]
- 22.Kandulski A, Jechorek D, Caro C, Weigt J, Wex T, Mönkemüller K, et al. Histomorphological differentiation of non-erosive reflux disease and functional heartburn in patients with PPI-refractory heartburn. Aliment Pharmacol Ther. 2013;38:643–651. doi: 10.1111/apt.12428. [DOI] [PubMed] [Google Scholar]
- 23.Funch-Jensen P, Kock K, Christensen LA, Fallingborg J, Kjaergaard JJ, Andersen SP, et al. Microscopic appearance of the esophageal mucosa in a consecutive series of patients submitted to upper endoscopy. Correlation with gastroesophageal reflux symptoms and macroscopic findings. Scand J Gastroenterol. 1986;21:65–69. doi: 10.3109/00365528609034624. [DOI] [PubMed] [Google Scholar]
- 24.Kiesslich R, Kanzler S, Vieth M, Moehler M, Neidig J, Thanka Nadar BJ, et al. Minimal change esophagitis: prospective comparison of endoscopic and histological markers between patients with non-erosive reflux disease and normal controls using magnifying endoscopy. Dig Dis. 2004;22:221–227. doi: 10.1159/000080323. [DOI] [PubMed] [Google Scholar]
- 25.Farré R, Fornari F, Blondeau K, Vieth M, De Vos R, Bisschops R, et al. Acid and weakly acidic solutions impair mucosal integrity of distal exposed and proximal non-exposed human oesophagus. Gut. 2010;59:164–169. doi: 10.1136/gut.2009.194191. [DOI] [PubMed] [Google Scholar]
- 26.Caviglia R, Ribolsi M, Maggiano N, Gabbrielli AM, Emerenziani S, Guarino MP, et al. Dilated intercellular spaces of esophageal epithelium in nonerosive reflux disease patients with physiological esophageal acid exposure. Am J Gastroenterol. 2005;100:543–548. doi: 10.1111/j.1572-0241.2005.40978.x. [DOI] [PubMed] [Google Scholar]
- 27.Isomoto H, Nishi Y, Kanazawa Y, Shikuwa S, Mizuta Y, Inoue K, et al. Immune and inflammatory responses in GERD and lansoprazole. J Clin Biochem Nutr. 2007;41:84–91. doi: 10.3164/jcbn.2007012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Isomoto H, Saenko VA, Kanazawa Y, Nishi Y, Ohtsuru A, Inoue K, et al. Enhanced expression of interleukin-8 and activation of nuclear factor kappa-B in endoscopy-negative gastroesophageal reflux disease. Am J Gastroenterol. 2004;99:589–597. doi: 10.1111/j.1572-0241.2004.04110.x. [DOI] [PubMed] [Google Scholar]
- 29.Mönkemüller K, Wex T, Kuester D, Fry LC, Peitz U, Beyer M, et al. Interleukin-1beta and interleukin-8 expression correlate with the histomorphological changes in esophageal mucosa of patients with erosive and non-erosive reflux disease. Digestion. 2009;79:186–195. doi: 10.1159/000211714. [DOI] [PubMed] [Google Scholar]
- 30.Shieh KR, Yi CH, Liu TT, Tseng HL, Ho HC, Hsieh HT, et al. Evidence for neurotrophic factors associating with TRPV1 gene expression in the inflamed human esophagus. Neurogastroenterol Motil. 2010;22:971–977.:e252. doi: 10.1111/j.1365-2982.2010.01530.x. [DOI] [PubMed] [Google Scholar]
- 31.Isomoto H, Wang A, Mizuta Y, Akazawa Y, Ohba K, Omagari K, et al. Elevated levels of chemokines in esophageal mucosa of patients with reflux esophagitis. Am J Gastroenterol. 2003;98:551–556. doi: 10.1111/j.1572-0241.2003.07303.x. [DOI] [PubMed] [Google Scholar]
- 32.Isomoto H, Nishi Y, Wang A, Takeshima F, Omagari K, Mizuta Y, et al. Mucosal concentrations of proinflammatory cytokines and chemokines at gastric cardia: implication of Helicobacter pylori infection and gastroesophageal reflux. Am J Gastroenterol. 2004;99:1063–1068. doi: 10.1111/j.1572-0241.2004.30847.x. [DOI] [PubMed] [Google Scholar]
- 33.Yoshida N, Uchiyama K, Kuroda M, Sakuma K, Kokura S, Ichikawa H, et al. Interleukin-8 expression in the esophageal mucosa of patients with gastroesophageal reflux disease. Scand J Gastroenterol. 2004;39:816–822. doi: 10.1080/00365520410006729. [DOI] [PubMed] [Google Scholar]
- 34.Noordzij JP, Khidr A, Evans BA, Desper E, Mittal RK, Reibel JF, et al. Evaluation of omeprazole in the treatment of reflux laryngitis: a prospective, placebo-controlled, randomized, double-blind study. Laryngoscope. 2001;111:2147–2151. doi: 10.1097/00005537-200112000-00013. [DOI] [PubMed] [Google Scholar]