Abstract
Introduction
Despite a systematic increase in the coverage of patients with end-stage renal disease (ESRD) who have received dialytic therapies and transplantation over the past 2 decades, the Mexican health system currently still does not have a program to provide full coverage of ESRD. Our aim was to analyze mortality in patients with ESRD without health insurance.
Methods
This was a prospective cohort study of 850 patients with advanced chronic kidney disease (CKD). Risk factors associated with death were calculated using a Cox's proportional hazards model. We used the statistical package SPSS version 22.0 for data analysis.
Results
The mean age of patients was 44.8 ± 17.2 years old. At the time of hospital admission, 87.6% of the population did not have a social security program to cover the cost of renal replacement treatment, and 91.3% of families had an income below US$300 per month. During the 3 years of the study, 28.8% of the cohort patients were enrolled in 1 of Mexico's social security programs. The 3-year mortality rate was of 56.7% among patients without access to health insurance, in contrast to 38.2% of patients who had access to a social security program that provided access to renal replacement therapy (P < 0.001). Risk factor analysis revealed that not having health insurance increased mortality (risk ratio: 2.64, 95% confidence intervals: 1.84−3.79; P = 0.001).
Conclusion
Mexico needs a coordinated National Kidney Health and Treatment Program. A program of this nature should provide the basis for an appropriate educational and intervention strategy for early detection, prevention, and treatment of patients with advanced chronic kidney disease.
Keywords: chronic kidney disease, Mexico, mortality, survival analysis
Mexico has some of the highest incidence and prevalence rates of CKD in the world.1, 2 Data from the Institute of Health Metrics and Evaluation indicate diabetes mellitus and arterial hypertension as the principal causes of CKD, which has led to a significant increase in deaths associated with kidney disease in Mexico.2, 3, 4 Estimations have signaled that a significant increase in the incidence and prevalence of stage 5 CKD (according to the Kidney Disease: Improving Global Outcomes [KDIGO] guidelines) is to be expected in the medium term,5 which will likely increase the inequality and extreme poverty that exist in the country.6 Studies published by the National Institute of Public Health of Mexico show how CKD has increased disability-adjusted life years from 300% to 400%. This finding places CKD as the second and fourth leading cause of years of healthy life lost for men and women, respectively.7
As is the case in many countries, regular access to health care with financial protection is offered only to salaried workers and their families through social security mechanisms. The wealthier, formal private sectors receive care from the Mexican Institute for Social Security, and federal public workers receive care from the Institute for Social Security and Services for Civil Servants. The non-salaried population (self-employed workers, the underemployed, the unemployed, those out of the labor market permanently or temporarily, along with their families) typically access health services either through the Ministry of Health on a public assistance basis or through Seguro Popular.8, 9 However, patients assisted by either the Ministry of Health or Seguro Popular have free coverage for many diseases, except for CKD and renal replacement therapies (RRTs); thus, patients are required to pay for this type of treatment.
The General Hospital of Mexico Dr. Eduardo Liceaga is a public general hospital under the charge of the Ministry of Health. With >100 years of service and a central location in the heart of the country, this hospital receives uninsured patients with CKD from across the nation, many of whom require renal replacement treatment.10, 11, 12 The objective of the present study was to analyze the sociodemographic, clinical, and laboratory characteristics that could influence the mortality of CKD patients without social health insurance who were admitted to our institution.
Methods
Study Population
We included first-time patients admitted to the hospital with a diagnosis of KDIGO stage 5 CKD between August 1, 2012, and July 31, 2015. Our inclusion criteria were patients older than 18 years (because our hospital does not have pediatric nephrologists) with advanced CKD (stage 5 CKD based on the KDIGO guidelines) and who were not receiving RRT at the time of admission to the hospital. Patients with a diagnosis of acute kidney failure and patients with stage 3 or 4 CKD based on the KDIGO guidelines at the time of admission were excluded.
Study Variables
Selected patients were included in a prospective cohort study. Independent variables included age (in years), sex, etiology of CKD, comorbidities at admission to the hospital, time from diagnoses of kidney disease (in months), history of replacement therapy (if any), insurance status, schooling level, marital status, occupation, family income per month and registered by social work, economic provider for the household, and place of residence. Laboratory values at admission were also recorded, including hemoglobin (g/dl), serum sodium (mmol/l), potassium (mmol/l), bicarbonate (mmol/l), creatinine (mg/dl), and urea (mg/dl). The dependent variable at the end of the study was the clinical evaluation of the patient, which was dichotomized as living or deceased. All deaths that were recorded were confirmed through death certificates. A database was created and designed to follow patients and analyze the variables.
Patients entered the cohort at the moment of their first hospitalization and were followed up during outpatient visits. When patients failed to attend their follow-up visits, a team of 9 social workers made phone calls, and when required and possible, performed fieldwork by visiting patients’ homes to inquire about the current status of the patients.
Types of RRT
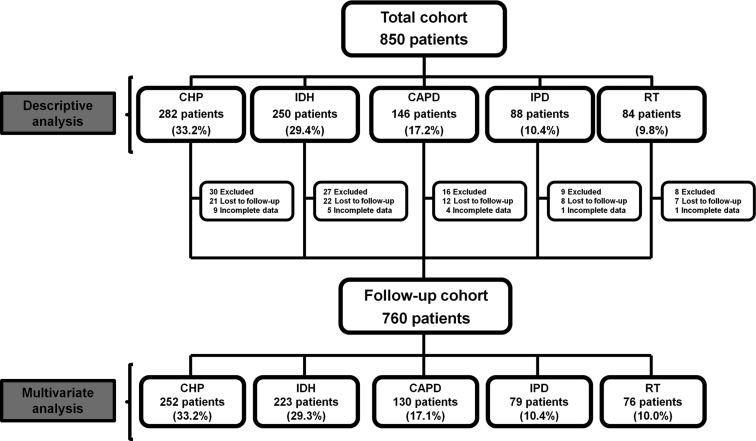
The following replacement therapies were performed and analyzed in this population: (i) patients in the chronic hemodialysis program (CHP) who underwent 2 to 3 hemodialysis sessions per week. CHPs were performed in our hospital or any other hemodialysis center; (ii) intermittent hemodialysis (IHD), which was a suboptimal treatment modality performed weekly, every 2 weeks, or even monthly, in our hospital or any hospital or at public or private institutions; (iii) continuous ambulatory peritoneal dialysis (CAPD), which traditionally consists of 4 dwells/day, with 2 to 3 l/dwell, with each remaining in the abdomen for 4 to 8 hours every day; the bags for dialysis replacement were obtained directly by the patient or by health insurance; (iv) intermittent peritoneal dialysis (IPD), which is a suboptimal treatment procedure performed in our hospital or any other public hospital. Usually, patients receiving IPD stay in-hospital for 3 days and are subjected to a 30 PD dwell using a dialysate of 1.5% glucose; subsequently, patients are discharged and readmitted every 15 or 30 days for subsequent IPD sessions; and (v) kidney transplantation, in which all cases analyzed were patients who initially underwent hemodialysis and subsequently underwent renal transplantation at our hospital during follow-up of the cohort, through a complex financing mechanism for surgery, and the coverage of induction and maintenance immunosuppression.11 Figure 1 shows a flowchart of the sample according to type of RRT.
Figure 1.
Trial profile showing a flowchart of patient numbers from initial screening to final analysis. The upper part shows the distribution of 850 patients who entered the cohort with the inclusion criteria. Ninety patients were excluded for multivariate analyses due to loss in follow-up (70 patients) or incomplete data (20 patients). The lower part presents the distribution of the 760 patients who completed the study until the end of the cohort (3 years). CAPD, continuous ambulatory peritoneal dialysis; CHP, chronic hemodialysis program; IHD, intermittent hemodialysis; IPD, intermittent peritoneal dialysis; RT, renal transplant.
Types of Social Health Insurance in Mexico
Patients were also registered according to their insurance status and whether they belonged to any of the social security insurance programs available in Mexico that provide full access to RRT or kidney transplantation.13 These programs include the Instituto Mexicano del Seguro Social, Instituto de Seguridad Social al Servicio de los Trabajadores del Estado, Petróleos Mexicanos, Secretaria de Marina, and the Secretaria de la Defensa Nacional. In addition, Mexico has a social security program called Seguro Popular (Popular Healthcare). This program is designed for patients without access to any of the previously mentioned social security programs and covers >250 conditions. In contrast to the other programs, Seguro Popular does not provide access to renal replacement treatment or transplantation (currently, it covers only renal transplantation patients younger than 18 years of age), which means that these treatments must be paid for by the patient.14
Sample Size
For the sample size calculation, we use the hazard ratio (HR) reported by Jurkovitz et al. for the risk of mortality according to presence of CKD and social security.15 The sample size was estimated using a z-test, for logistic regression and distribution of 1 tail, in the statistical package G*Power V.3.1.9.2 (Dusseldorf, Germany). An HR of 1.82 (95% confidence intervals [CI]: 1.56−2.12; Cohen's 0.33) was considered for mortality in the group with CKD without social security versus an HR of 1.68 (95% CI: 1.39−2.04; Cohen's 0.28) for the group without CKD with social security. Considering an α error of 0.05, a power of 95%, a critical value of z of 1.64, plus 10% for losses during follow-up, we obtained a minimum sample size of 180 patients.
Statistical Analysis
The results are expressed as the means ± SD or median (range) according to the distribution of variables. Comparisons between groups were performed by an analysis of variance or the Kruskal-Wallis test, also according to the distribution of variables. Initial survival analysis was performed using Kaplan-Meier curves, and a comparison between groups was performed with a log-rank test. Survival analysis for all patients was considered from the time they started replacement therapy until 3 years of follow-up. Cox’s proportional model was used to evaluate risk factors for death. An additional survival analysis was performed using Cox’s proportional model according to the subjects’ health insurance. The model was adjusted for each specified RRT (CHP, IDH, CAPD, IPD and renal transplantation), age (for each year), sex (male), diabetes status (yes), heart disease (yes), cancer (yes), education level (>6 years of schooling), income (>$300 per month), residence in a rural area (yes), access to health insurance programs, and laboratory results dichotomized by clinically significant cutpoints at hospital admission (serum potassium >7 mmol/l; serum bicarbonate <7 mmol/l; hemoglobin <6 g/dl; and urea >300 mg/dl). The starting point was considered the date of first hospital admission; patients were then followed until the last medical visit or death. All P values were 2-tailed, and we considered P < 0.05 to be statistically significant. All analyses were carried out using the statistical package SPSS (version 22.0; IBM Corp., Armonk, NY).
Results
CKD Predominated in Adults With Diabetes and Hypertension
Baseline characteristics of the population are presented in Table 1. The average age was 44.8 ± 17.2 years. A total of 850 patients who fulfilled the inclusion criteria were admitted during the study period. There were 424 men (49.9%) and 426 women (50.1%), and the main cause of CKD was diabetes mellitus (34.2%). At the time of hospitalization, the most common documented comorbidities were hypertension (in 82.4% of the participants), lipid disorders (62.1%), and diabetes mellitus (34.2%). Fifty-eight (6.8%) patients had a history of undergoing some form of RRT before being admitted to the hospital; 41 patients underwent a variable number of hemodialysis sessions (4.8%), and 17 patients had received PD (2%). The causes or clinical indications for each of these events are unknown. In addition, history of RRT did not reveal statistically significant differences according to social security status; however, the comparison of sociodemographic and clinical characteristics at hospital admission between patients with and without social security revealed differences in age, comorbidities, and economic income (Table 2).
Table 1.
Baseline characteristics of the study population
| Variables | Total (N = 850) | CHP (n = 282) | IDH (n = 250) | CAPD (n = 146) | IPD (n = 88) | RT (n = 840) | P value |
|---|---|---|---|---|---|---|---|
| Age, yr | 44.8 ± 17.2 | 45.7 ± 16.6 | 45.6 ± 17.9 | 45.3 ± 14.4 | 45.6 ± 17.9 | 37.6 ± 18.4 | 0.002a |
| Women | 426 (50.1) | 136 (48.2) | 129 (51.6) | 78 (53.4) | 39 (44.3) | 44 (52.4) | 0.625 |
| Etiology of ESRD | |||||||
| Diabetes mellitus | 291 (34.2) | 116 (41.1) | 77 (30.8) | 57 (39.0) | 29 (33.0) | 12 (14.3) | 0.001a |
| Hypertension | 120 (14.1) | 24 (8.5) | 46 (18.4) | 11 (7.5) | 16 (18.2) | 23 (27.4) | 0.001a |
| Glomerulopathies | 179 (21.1) | 51 (18.1) | 45 (18.0) | 39 (26.7) | 21 (23.9) | 19 (26.4) | 0.086 |
| APKD | 20 (2.4) | 15 (5.3) | 3 (1.2) | 1 (0.7) | 1 (1.1) | 0 (0) | 0.002a |
| Other | 34 (4.0) | 18 (6.4) | 6 (2.4) | 8 (5.5) | 2 (2.3) | 0 (0) | 0.028a |
| Unknown | 206 (24.2) | 58 (20.6) | 73 (29.2) | 30 (20.5) | 19 (21.6) | 26 (31.0) | 0.063 |
| Comorbidities | |||||||
| Diabetes mellitus | 291 (34.2) | 116 (58.9) | 77 (30.8) | 57 (39.0) | 29 (33.0) | 12 (14.3) | 0.001a |
| Hypertension | 700 (82.4) | 216 (76.6) | 208 (83.2) | 127 (87) | 74 (84.1) | 75 (89.3) | 0.020a |
| Heart disease | 31 (3.6) | 9 (3.2) | 10 (4.0) | 5 (3.4) | 3 (3.4) | 4 (4.8) | 0.965 |
| Lipid disorders | 528 (62.1) | 180 (63.8) | 149 (59.6) | 97 (66.4) | 57 (64.8) | 45 (53.6) | 0.283 |
| Autoimmune diseases | 168 (19.8) | 49 (17.4) | 44 (17.6) | 35 (24) | 18 (22.8) | 20 (23.8) | 0.316 |
| Liver disease | 16 (1.9) | 3 (1.1) | 6 (2.4) | 4 (2.7) | 2 (2.3) | 1 (1.2) | 0.770 |
| Cancer | 34 (4.0) | 18 (6.4) | 6 (2.4) | 8 (5.5) | 1 (1.3) | 0 (0) | 0.028a |
| Time since diagnosis of CKD, mo | 2.4 ± 6.5 | 2.1 ± 5.7 | 2.7 ± 6.7 | 1.15 ± 4.4 | 3.75 ± 9.8 | 3.6 ± 7.5 | 0.010a |
| History of RRT | |||||||
| Hemodialysis | 41 (4.8) | 15 (5.3) | 7 (2.8) | 13 (8.9) | 4 (4.5) | 2 (2.4) | 0.067 |
| Peritoneal dialysis | 17 (2.0) | 4 (1.4) | 2 (0.8) | 3 (2.1) | 7 (8.0) | 1 (1.2) | 0.001a |
| Social security coverage | 105 (12.4) | 25 (8.9) | 25 (17.1) | 27 (10.8) | 9 (10.2) | 19 (22.6) | 0.004a |
| Education | |||||||
| Illiterate | 74 (8.7) | 23 (8.2) | 6 (4.1) | 30 (12.0) | 11 (12.5) | 4 (4.8) | 0.031a |
| 1−6 yr | 356 (41.9) | 124 (44.0) | 62 (42.5) | 109 (43.6) | 38 (43.2) | 23 (27.4) | 0.086 |
| 7−9 yr | 286 (33.6) | 87 (30.9) | 54 (37.0) | 76 (30.4) | 28 (31.8) | 41 (48.8) | 0.020a |
| 9−12 yr | 104 (12.2) | 40 (14.2) | 20 (13.7) | 24 (9.6) | 7 (8.0) | 13 (15.5) | 0.265 |
| >12 yr | 29 (3.4) | 8 (2.8) | 4 (2.7) | 10 (4.0) | 4 (4.5) | 3 (3.6) | 0.896 |
| Marital status | |||||||
| Single | 297 (34.9) | 83 (29.4) | 47 (32.2) | 104 (41.6) | 23 (26.1) | 40 (47.6) | 0.001a |
| Married | 435 (51.2) | 166 (58.9) | 73 (50.0) | 114 (45.6) | 49 (55.7) | 33 (39.3) | 0.004a |
| Widowed | 55 (6.5) | 8 (2.8) | 13 (8.9) | 17 (6.8) | 8 (9.1) | 9 (10.7) | 0.025a |
| Divorced | 63 (7.4) | 25 (8.9) | 13 (8.9) | 15 (6.0) | 8 (9.1) | 2 (2.4) | 0.238 |
| Occupation | |||||||
| Unemployed | 390 (45.9) | 128 (45.4) | 74 (50.7) | 99 (39.6) | 45 (51.1) | 44 (52.4) | 0.101 |
| Merchant | 49 (5.8) | 14 (5.0) | 10 (6.8) | 20 (8.0) | 2 (2.3) | 3 (3.6) | 0.226 |
| Manual laborer | 32 (3.8) | 16 (5.7) | 3 (2.1) | 8 (3.2) | 2 (2.3) | 3 (3.6) | 0.311 |
| Field worker | 55 (11.8) | 15 (9.6) | 7 (9.7) | 11 (7.3) | 16 (35.6) | 6 (14.6) | 0.001a |
| Student | 32 (3.9) | 12 (4.5) | 4 (2.8) | 16 (6.6) | 0 (0) | 3 (3.6) | 0.016a |
| Housewife | 275 (33.6) | 95 (35.7) | 45 (31.5) | 86 (35.5) | 22 (25.6) | 27 (33.3) | 0.448 |
| Other | 17 (2.0) | 2 (0.7) | 3 (2.1) | 10 (4.0) | 1 (1.1) | 1 (1.2) | 0.087 |
| Monthly income | |||||||
| <$100 | 194 (22.8) | 70 (24.8) | 30 (20.5) | 54 (21.6) | 29 (33.0) | 11 (13.1) | 0.027a |
| Between $100 and $300 | 582 (68.5) | 202 (71.6) | 101 (69.2) | 168 (67.2) | 52 (59.1) | 59 (70.2) | 0.265 |
| >$300 | 74 (8.7) | 10 (3.5) | 15 (10.3) | 28 (11.2) | 7 (8.0) | 14 (16.7) | 0.001a |
| Principal economic provider | 339 (39.9) | 120 (42.6) | 69 (47.3) | 98 (39.2) | 29 (33.0) | 23 (27.4) | 0.022a |
| Area of residence | |||||||
| Urban areas | 687 (80.8) | 231 (81.9) | 120 (82.2) | 196 (78.4) | 66 (75) | 74 (88.1) | 0.190 |
| Rural areas | 163 (19.2) | 51 (18.1) | 26 (17.8) | 54 (21.6) | 22 (25.0) | 10 (11.9) |
APKD, adult polycystic kidney disease; CAPD, continuous ambulatory peritoneal dialysis; CHP, chronic hemodialysis program; CKD, chronic kidney disease; ESRD, end-stage kidney disease; IHD, intermittent hemodialysis; IPD, intermittent peritoneal dialysis; RRT, renal replacement therapy RT, renal transplant.
Data are n (%) or mean ± SD.
P < 0.05 indicates statistical significance.
Table 2.
Baseline comparisons between patients with and without social security
| Variable | Without social insurance (n = 745) | With social insurance (n = 105) | P value |
|---|---|---|---|
| Age, yr | 44.1 ± 16.9 | 49.0 ± 17.6 | 0.007a |
| Women | 397 (50.6) | 49 (46.7) | 0.451 |
| Etiology of ESRD | |||
| Diabetes mellitus | 238 (31.9) | 49 (46.7) | 0.001a |
| Hypertension | 102 (13.7) | 18 (17.1) | 0.342 |
| Glomerulopathies | 157 (21.1) | 22 (21) | 0.977 |
| APKD | 16 (2.1) | 4 (3.8) | 0.293 |
| Others | 34 (4.6) | 0 (0) | 0.025a |
| Unknown | 198 (26.6) | 8 (7.6) | 0.001a |
| Comorbidities (%) | |||
| Diabetes mellitus | 238 (31.9) | 53 (50.5) | 0.001a |
| Hypertension | 622 (83.5) | 78 (74.3) | 0.021a |
| Heart disease | 22 (3) | 9 (8.6) | 0.001a |
| Lipid disorders | 449 (60.3) | 79 (75.2) | 0.003a |
| Autoimmune diseases | 147 (19.7) | 21 (20) | 0.949 |
| Liver disease | 13 (1.7) | 3 (2.9) | 0.433 |
| Cancer | 34 (4.6) | 0 (0) | 0.025a |
| Time since diagnosis of CKD, mo | 2.42 ± 6.6 | 2.56 ± 6.5 | 0.832 |
| History of RRT | |||
| Hemodialysis | 37 (5) | 4 (3.8) | 0.605 |
| Peritoneal dialysis | 15 (2) | 2 (1.9) | 0.941 |
| Monthly income | |||
| <$100 | 177 (23.8) | 17 (16.2) | 0.084 |
| Between $100 and $300 | 509 (68.3) | 73 (69.5) | 0.804 |
| > $300 | 59 (7.9) | 15 (14.3) | 0.030a |
| Laboratory values | |||
| Hemoglobin, g/dl | 6.2 (3.2−9.9) | 6.0 (4.2−8.9) | 0.087 |
| Serum urea, mg/dl | 306.5 (100−1,799) | 317.1 (157−744) | 0.534 |
| Serum creatinine, mg/dl | 11.6 (1.8−40.1) | 12.1 (1.9−24.8) | 0.510 |
| CKD-EPI, ml/min per 1.73 m2 | 5.6 (0.9−12.7) | 6.0 (1.2−15.2) | 0.221 |
| Serum potassium, mmol/l | 7.3 (5.6−14.1) | 7.2 (5.6−9.1) | 0.242 |
| Serum bicarbonate, mmol/l | 7.45 (1.1−18.1) | 8.1 (2.6−16.1) | 0.051 |
APKD, adult polycystic kidney disease; CKD, chronic kidney disease; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; ESRD, end-stage kidney disease; RRT, renal replacement therapy RT, renal transplant.
Data are n (%), mean ± SD, or median (range).
P < 0.05 indicates statistical significance.
Poor Patients and Those With Low Levels of Education Predominated the Cohort
Figure 2 shows that the participants in the study were primarily from central and southern Mexican states. In terms of education level, 8.7% of the study population was illiterate, and only 3.4% had >12 years of schooling; 51.2% of the participants were married, and 45.9% were unemployed. During interviews with social workers, 68.5% of the population declared their income as being between $100 and $300 per month, and 22.8% declared their income to be below $100 per month. The principal economic provider of the family was the patient in 39.9% of cases. Regarding their living situation, 80.8% of the patients lived in urban areas with access to public services and utilities (potable water, electricity, and sewage system), whereas the rest (19.2%) lived in rural areas with limited access to communication networks and public services. Sociodemographic characteristics are shown in Table 1.
Figure 2.

Map of Mexico. The principal Mexican states from which participants originated are shown on this map. The states in red, including the Distrito Federal and Estado de Mexico, had 65% of the patients who participated in the cohort. The states in blue, including Oaxaca, Michoacan, Puebla, Hidalgo, and Queretaro, were home to 20% of the participants. Veracruz, Guerrero, and Guanajuato, from which 12% of the population originated, are green, and Baja California, Tlaxcala, Morelos, San Luis Potosí, and Jalisco, from which 3% of the population originated, are yellow.
Inequalities in Access to RRTs in Mexico
The 850 studied patients were distributed into the following groups: 282 (33.2%) began treatment in CHP, 250 (29.4%) received IHD, 146 (17.2%) received CAPD, 88 (10.4%) underwent IPD, and 84 (9.8%) were admitted to a kidney transplantation program and managed to receive a graft after a variable period of time in RRT (range: 3−6 months). Among the patients, 32 (4.21%) died during their first hospitalization; those patients were in the IHD group. Upon hospital intake, 745 patients (87.6%) did not have any insurance plan that provided access to RRT. However, during follow-up, 16.4% of patients were enrolled in a social security institution throughout the study (140 patients), which added to the 12.4% (105 patients) who already had social security and resulted in 28.9% of patients (245 patients) who had complete access to social security programs that offered RRT. The remaining patients in the cohort were treated in health programs that required them to pay partially or completely for hemodialysis or PD, with prices depending on the type of institution, and for some patients, their economic ability to pay.
An analysis based on social security status revealed significant differences regarding RRT (Table 3). Patients with social security had a higher frequency of renal transplantations and admissions to CAPD programs. In contrast, patients without social security entered long-term hemodialysis programs and underwent intermittent therapies significantly more frequently.
Table 3.
Renal replacement therapy according to final insurance status
| Type of substitution therapy | Without health insurance (n = 604) | With health insurance (n = 245) | P value |
|---|---|---|---|
| Renal transplant | 16 (2.6) | 68 (27.8) | 0.001a |
| Chronic hemodialysis program | 219 (36.3) | 62 (25.3) | 0.003a |
| Continuous ambulatory peritoneal dialysis | 58 (9.6) | 88 (35.9) | 0.001a |
| Intermittent hemodialysis | 238 (39.4) | 12 (4.9) | 0.001a |
| Intermittent peritoneal dialysis | 73 (12.1) | 15 (6.1) | 0.009a |
Data are n (%).
P < 0.05 indicates statistical significance.
Predominance of Patients With Extremely Advanced CKD and Late Commencement of RRT
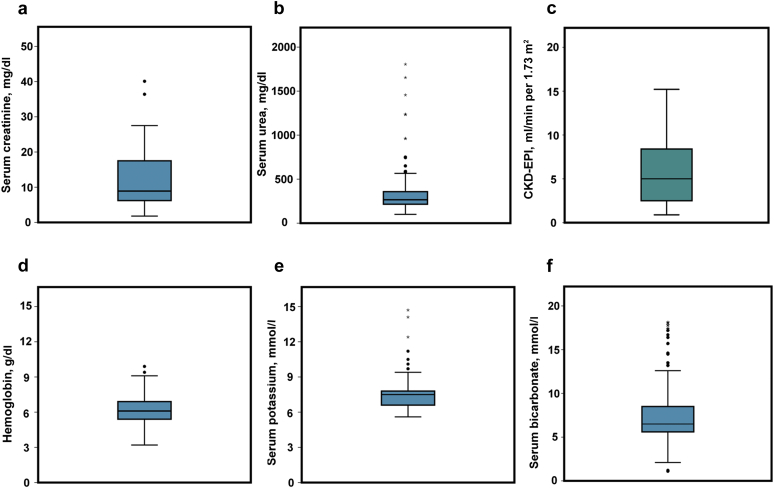
All patients in the cohort had indications for placement of temporal vascular access and the commencement of hemodialysis. Figure 3a to 3f shows laboratory values obtained upon hospital admission. One hundred twenty-one patients (14.2%) were admitted with extreme levels of azotemia (levels of urea >500 mg/dl). The median serum creatinine level was 11.7 mg/dl (range: 1.8−40.1 mg/dl), the median urea level was 307.8 mg/dl (range: 100−1799 mg/dl), and the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) was 5.8 ml/min per 1.73 m2 (range: 0.9−15.2 ml/min per 1.73 m2). The median hemoglobin value was 6.2 g/dl (range: 3.2−9.9 g/dl), and 602 patients (70.8%) required blood transfusions during their hospital stay (range: 1−9 transfusions of erythrocyte concentrates). Upon admission, the median serum potassium level was 7.35 mmol/l (range: 5.6−14.1 mmol/l), and the serum bicarbonate level was 7.53 mmol/l (range: 1.1−18.1 mmol/l). On average, patients in this first hospitalization underwent 3 hemodialysis sessions (range: 2−10) during their hospital stay. From a clinical viewpoint, the principal indication for commencing RRT was a combination of a uremic syndrome associated with hyperkalemia, metabolic acidosis, and acute pulmonary edema (85.3%). A comparison of laboratory findings between patients with and without social security at the time of admission to the hospital did not show significant differences (see Table 2).
Figure 3.
Laboratory results reported upon admittance to the hospital for patients with chronic kidney disease (CKD). The median level of serum creatinine was 11.7 mg/dl (range: 1.8−40.1 mg/dl) (a). The median level of serum urea was 307.8 mg/dl (range: 100–1799 mg/dl) (b). Median Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) was 5.8 ml/min per 1.73 m2 (range: 0.9–15.2 ml/min per 1.73 m2) (c). The median hemoglobin level was 6.2 g/dl (range: 3.2–9.9 g/dl) (d). The median serum potassium level was 7.35 mmol/l (range: 5.6–14.1 mmol/l) (e). The median bicarbonate level was 7.53 mmol/l (range: 1.1–18.1 mmol/l) (f).
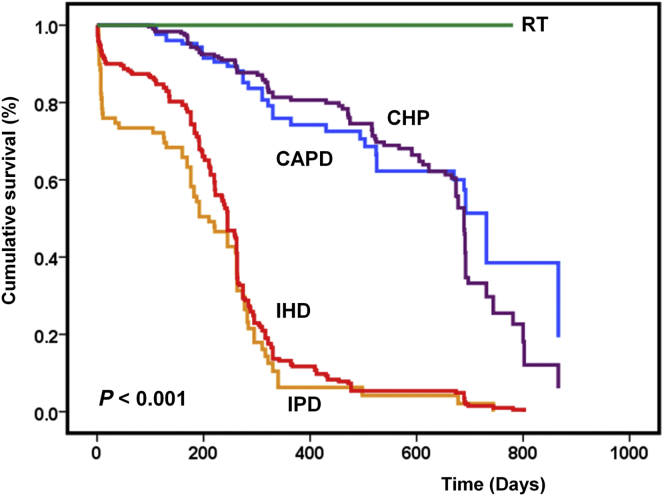
Mortality in CKD Patients According to Treatment Modality
For this analysis, only 760 patients were considered because 90 patients were excluded due to loss in follow-up (70 patients) or incomplete data (20 patients). The results of a survival analysis performed according to the type of RRT are shown in Figure 4. Global survival was 45.8% at the end of the follow-up (3 years). According to the type of RRT, mean survival was 100% for those who received a kidney transplant: 61.9% for patients on CHP; 72.5% for patients on CAPD; 8.2% for patients on IHD; and 11.4% for patients on IPD (P < 0.001). Full financial coverage for medical treatment was observed in 81.9% of renal transplantation patients, 78.1% of patients on CHP, and 58.8% of patients on CAPD. In contrast, patients on IPD received coverage in only 10.2% of cases, and those who received IHD received coverage in only 10.8% of cases. There were no deaths in transplantation patients during the study period. However, the analysis of survival graft according to social security and donor type did not reveal differences (P = 0.774 and P = 0.106, respectively).
Figure 4.
Kaplan-Meier analysis for patients with chronic kidney disease. The graphs show patients who underwent kidney transplantation (green line), patients who continued in the chronic hemodialysis program (CHP) (purple line), patients who migrated to continue ambulatory peritoneal dialysis (CAPD) (blue line), patients on intermittent hemodialysis (IHD) (red line), and patients on intermittent peritoneal dialysis (IPD) (orange line). The survival of the entire population (760 patients) was 45.8% in the final analysis. According to the type of replacement therapy, the average survival rates were 100%, 61.9%, 72.5%, 8.2%, and 11.4% for patients who underwent a kidney transplantation, CHP, CAPD, IHD, and IDP, respectively (P < 0.001). RT, renal transplant.
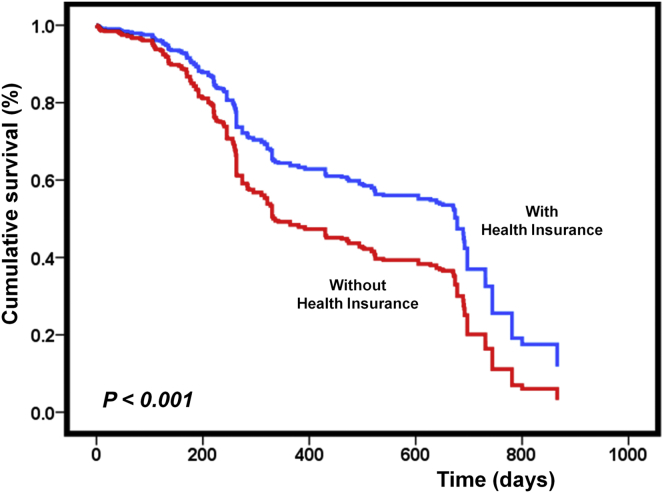
Lack of Access to RRT in Health Coverage Is the Main Risk Factor for Mortality in Patients With CKD in Mexico
As presented in the previous section, we analyzed possible risk factors based on the complete information of 760 patients. Univariate analysis showed that age (RR: 1.15; 95% CI: 1.01−1.30; P = 0.001), a relatively low level of serum bicarbonate (RR: 1.33; 95% CI: 1.00−1.77; P = 0.029), IHD (RR: 6.29; 95% CI: 4.41−8.98; P = 0.001), IPD (RR: 3.18; 95% CI: 1.91−5.27; P = 0.001), and lack of access to health insurance programs (RR: 7.51; 95% CI: 5.12−11.0; P = 0.001) were associated with mortality in patients with CKD. Alternatively, patients with income levels above $300 per month (RR: 0.79; 95% CI: 0.65−0.98; P = 0.030), relatively high levels of education (>6 years of schooling) (RR: 0.82; 95% CI: 0.72−0.95; P = 0.005), and patients who underwent renal transplantation (RR: 0.39; 95% CI: 0.30−0.51; P = 0.001) had significantly lower risks of dying from CKD. Multivariate analysis showed that age, diabetes mellitus, cancer, renal transplantation, IHD, and IPD were independent factors that increased mortality, whereas not having access to health insurance was associated with an independent risk factor of death (RR: 2.64; 95% CI: 1.84−3.79; P = 0.001). Table 4 summarizes the analysis of factors associated with mortality in CKD patients. Alternatively, Figure 5 shows survival analysis using Cox’s proportional model according to health insurance. We observed a mortality rate of 56.7% in patients without health insurance versus a mortality rate of 38.2% in patients with access to a social security program and access to RRT.
Table 4.
Analysis of possible risk factors associated with mortality
| Risk factors | Univariate analysis |
Multivariate analysis |
||||
|---|---|---|---|---|---|---|
| RR | 95% CI | P value | HR | 95% CI | P value | |
| Age (for each year) | 1.15 | 1.01−1.30 | 0.001a | 1.01 | 1.00−1.02 | 0.001a |
| Male (yes) | 1.01 | 0.76−1.35 | 0.477 | 0.98 | 0.85−1.12 | 0.798 |
| Education (>6 yr of schooling) | 0.82 | 0.72−0.95 | 0.005a | 0.87 | 0.60−1.14 | 0.106 |
| Income (>$300 per month) | 0.79 | 0.65−0.98 | 0.030a | 0.70 | 0.48−1.02 | 0.708 |
| Residence in rural area (yes) | 1.06 | 0.79−1.52 | 0.400 | 1.14 | 0.87−1.49 | 0.332 |
| Diabetes (yes) | 1.40 | 1.12−1.76 | 0.003a | 1.29 | 1.09−1.50 | 0.012a |
| Heart disease (yes) | 1.28 | 0.80−2.06 | 0.168 | 1.15 | 0.42−1.88 | 0.709 |
| Liver disease (yes) | 0.70 | 0.24−2.00 | 0.347 | 0.73 | 0.19−1.28 | 0.186 |
| Cancer (yes) | 1.76 | 1.03−2.99 | 0.001a | 1.36 | 1.16−1.57 | 0.011a |
| Hemoglobin (<6 g/dl) | 0.93 | 0.81−1.07 | 0.181 | 1.08 | 0.87−1.33 | 0.459 |
| Serum potassium (>7 mEq/dl) | 0.96 | 0.72−1.28 | 0.425 | 0.85 | 0.56−1.22 | 0.148 |
| Urea (>300 mg/dl) | 1.08 | 0.81−1.44 | 0.324 | 0.91 | 0.73−1.12 | 0.363 |
| Serum bicarbonate (<7 mEq/dl) | 1.33 | 1.00−1.77 | 0.029a | 1.26 | 0.84−1.87 | 0.252 |
| Renal transplant (yes) | 0.39 | 0.30−0.51 | 0.001a | 0.50 | 0.29−0.88 | 0.016a |
| Chronic hemodialysis programme (yes) | 0.57 | 0.46−0.71 | 0.001a | 1.02 | 0.62−1.68 | 0.926 |
| Continuous ambulatory peritoneal dialysis (yes) | 0.35 | 0.24−0.51 | 0.001a | 0.91 | 0.53−1.55 | 0.735 |
| Intermittent hemodialysis (yes) | 6.29 | 4.41−8.98 | 0.001a | 4.30 | 2.65−6.96 | 0.001a |
| Intermittent peritoneal dialysis (yes) | 3.18 | 1.91−5.27 | 0.001a | 1.97 | 1.13−3.44 | 0.001a |
| Health insurance (No) | 7.51 | 5.12−11.0 | 0.001a | 2.64 | 1.84−3.79 | 0.001a |
CI, confidence interval; HR, hazard ratio; RR, risk ratio.
P < 0.05 indicates statistical significance.
Figure 5.
Cox proportional model of patients with chronic kidney disease according to health insurance. The graph shows patients who were able to obtain coverage through a health insurance program (blue line) and patients without health insurance (red line). The mortality at the end of the study was 38.2% for patients with social security and 56.7% for patients without social security (P < 0.001). The model was adjusted for each renal replacement therapy (chronic hemodialysis program, intermittent hemodialysis, continuous ambulatory peritoneal dialysis, intermittent peritoneal dialysis, and renal transplant), age (for each year), sex (male), diabetes status (yes), heart disease (yes), cancer (yes), education level (>6 years of schooling), income (>$300 per month), residence in rural area (yes), access to health insurance programs, and laboratories dichotomized by clinically significant cutpoints at the moment of hospital admission (serum potassium >7 mmol/l, serum bicarbonate <7 mmol/l, hemoglobin <6 g/dl, and urea >300 mg/dl).
Discussion
The results of the present study showed that, in addition to known variables, such as age, diabetes mellitus, and the presence of a malignancy, socioeconomic factors, as expected, had a profoundly negative effect on advanced CKD survival in our population. Our findings showed the diagnosis of advanced CKD in adult patients in the fourth decade of life, and also identified diabetes and hypertension as the main causes of CKD. Although most new cases of type 2 diabetes mellitus occurred in older adults, the greatest relative increase in type 2 diabetes mellitus was observed in patients in their second decade of life.16 Increasing numbers of youth-onset type 2 diabetes mellitus will also influence the incidence of diabetic kidney disease, because CKD may be more prevalent or develop more rapidly in those who develop type 2 diabetes mellitus during early adulthood or adolescence.17, 18
Demographic characteristics showed a population with low economic and educational levels. Other studies showed the impact of social disadvantage in moderate to severe CKD, with higher rates of cardiovascular events and mortality.19 In Mexico, the prevalence of obesity among children and adolescents increased significantly. During the last 2.5 decades, obesity shifted toward groups in lower socioeconomic levels, which showed the impact of obesity on the development of diabetes and subsequent CKD.20 A message of World Kidney Day 2015 revealed the increased burden of CKD in disadvantaged populations with low socioeconomic status and poor access to care, which contributed to health care disparities and exacerbated the negative effects of genetic or biological predisposition.21
We also found inequities in access to RRT in our country. Since 2005, reports revealed differences in access to RRT in Jalisco, a western state of Mexico.22 In Mexico, many patients did not receive RRT despite presenting with CKD.23 Examining commonalities across pathways to adequate health care revealed major failings in the Mexican system.24 Patients with CKD without financial coverage must face the high costs of replacement therapy. Therefore, most of these patients received suboptimal forms of RRT through intermittent sessions that were linked to their ability to pay and that were often triggered by extreme symptoms as “survival procedures.” These systemic problems served to reproduce and deepen health inequalities. In our health system, the costs of RRT are borne by the patients themselves, who are usually from low socio-economic strata.24 Recognizing the preceding factors will be important in the planning of a new national renal health policy. Likewise, our results revealed a predominance of patients with advanced CKD and late commencement of RRT that allowed us to theorize late referrals to nephrologists. Early referral to nephrologists is a key point for preventing the progression to end-stage kidney disease. Studies showed reduced mortality for patients with CKD who were referred early to nephrologists.25 Our results revealed late referral of patients with CKD to nephrologists. This trend could be caused by the fact that most patients entered the hospital in critical condition. Due to late referral, it was difficult to channel patients with CKD to kidney transplantation programs, fistula first programs, or CAPD training. Establishing an adequate network of early referral of patients with CKD in Mexico could help to reduce the incidence and prevalence of CKD in addition to the potential costs that RRT would entail. Our hospital is a referral center for CKD patients, as evidenced by the fact that the majority of the patients who participated in the cohort came from states outside of Mexico City. However, once a patient is stabilized as an inpatient in the hospital, they are given instructions to return to their place of residence to seek a hospital or medical institution that might provide adequate access to some type of long-term RRT. Because many of these individuals are uninsured, and there is no universal coverage for ESRD treatment, many patients returned intermittently to our hospital because private replacement treatment was unaffordable in their place of residence. When they returned, we again offered transient relief in many instances, providing a few hemodialysis sessions; ultimately, however, most of these patients died in their place of residence, without appropriate medical care. A large number of our patients had social security insurance; however, they did not receive initial RRT through their programs because many social security programs in Mexico have protocols according to which patients with CKD must first undergo PD. For this reason, patients who did not accept PD as a first-choice RRT came to our hospital seeking a second opinion or to begin hemodialysis sessions.
In contrast, most of the patients did not have social security that guaranteed adequate coverage of substitution therapy (87.6%). However, patients who underwent IHD and IPD (39.7%) frequently abandoned dialysis because of economic limitations to pay for hemodialysis sessions. Regarding kidney transplantations, graft survival did not show differences according to social security. This result was observed possibly because in our hospital, transplant patients without social security receive support from foundations or nongovernmental programs, and a high percentage of the expenses associated with the transplantation are absorbed by the hospital itself.11
In 2007, García-García et al. published an article that presented data on poor patients with CKD in Guadalajara, located in the state of Jalisco in western Mexico.13 In the article, the authors documented late referrals to nephrologists and a high mortality rate in poor patients with CKD, a situation highlighted as a pressing issue. Nearly 10 years later, the incidence and prevalence of CKD in our country has unfortunately increased dramatically, and mortality rates continue to climb.7
For countries such as Mexico, with significant heterogeneity in terms of human development (education, health, and other services), there is an urgent need to formulate and implement programs and strategies that are tailored according to regional needs but that also provide a comprehensive approach to kidney disease.26 Recently, the International Society of Nephrology called for all members of the World Health Organization to recognize CKD as a nontransmissible disease that requires public health policies for its opportune detection and treatment.27
In 2003, the Mexican government implemented a pilot program called Salud para Todos (“Health for All”). This program expanded to become the Social Health Protection System (commonly referred to as Seguro Popular or Popular Health Insurance).27 Within the Seguro Popular program, there is a subprogram called the Fund for Protection against Catastrophic Costs (FPGC in Spanish), which offers complete coverage for high-cost, high-specialty diseases (e.g., cervical cancer, breast cancer, and malignant hematological diseases in children). The purpose of this fund is to provide medical coverage for the included diseases and to avoid economic expenditures by patients and their families that could put their economy at risk. The general objective of Seguro Popular is to achieve universal health coverage in Mexico.8, 28, 29, 30, 31, 32
Although there have been significant efforts within the past 2 decades to increase the coverage of patients with ESRD within the social security program in Mexico and a permanent increase in patients on dialysis (from approximately 130 patients per 1 million inhabitants in 1993 to approximately 850 patients per 1 million at present), this benefit has not been extended to all Mexicans within the expanded health programs that have been created as part of the Seguro Popular. Unfortunately, Seguro Popular still does not provide coverage to patients with CKD. We therefore believe that the careful formulation and establishment of a National Program for Kidney Health are currently required. This program should be centred on 4 essential axes:
-
•
Establishment of early detection as well as primary and secondary prevention programs for CKD. The main causes of CKD in our country are diabetes mellitus, primary systemic hypertension, and obesity.33, 34 The Ministry of Health has already promoted a national policy for a healthier diet, including a reduced intake of dietary salt, refined sugars, carbohydrates and fats, and has also established health promotion and care programs, such as the National Strategy for the Prevention and Control of Overweight, Obesity, and Diabetes.35 However, these programs and initiatives, as they are, have proven to be insufficient to control and prevent the incidence of CKD.36
-
•
Improve the education of specialists in nephrology, as well as technicians and nurses with appropriate training in the field. With approximately 1000 certified nephrologists, Mexico has a ratio of 9 nephrologists per 1 million inhabitants.37 This figure is clearly insufficient, considering an incidence of 466.5 and a prevalence of >1400 per 1 million inhabitants.1
-
•
Creation of an appropriate infrastructure, both physical and human, to guarantee stepwise universal coverage of CKD and all renal replacement treatment modalities to all patients through Seguro Popular.
-
•
Creation of a national registry of patients who need renal replacement treatment (dialysis). This registry would allow us to better understand the growth of this condition and to provide better treatment options to those requiring renal replacement treatments.
In 2013, the Health Commission of the Mexican Congress began analyzing a proposal that would incorporate CKD (both end-stage and non−end-stage) into Seguro Popular. For this consideration, the commission recommended assigning sufficient resources in the Federal Expenditures Budget of 2014 to the coverage of CKD.38 Unfortunately, at present, uninsured patients or patients under Seguro Popular with CKD remain without access to renal replacement treatment. Data recently published by Obrador et al. showed that Mexico’s 6.3% of health expenditures, as a proportion of gross domestic product, was significantly lower than what other Latin American countries invest in health care. Our present perceptual health expenditure may be insufficient to guarantee the resources that the nation needs to develop a national kidney health program and other required health programs.39 Finally, because a large number of patients did not have a clear etiology of ESRD, we can hypothesize the possibility of facing different pathologies, among them, Mesoamerican nephropathy. Nevertheless, our study design did not allow for such a conclusion.
Our results showed a complicated situation to access RRT that patients with CKD have in our country. However, these results had some limitations that should be considered; for example, usually our hospital receives patients with low economic resources. It is recognized that economic status is typically related to prognosis in patients with CKD. In conclusion, our results revealed that there are inequalities in access to RRT in Mexico. These inequalities lead to higher mortality in patients who do not have health insurance. For this reason a program with full coverage for renal replacement treatment, including kidney transplantation, would be highly desirable and could serve as a goal to achieve a better and more egalitarian health system. A program of this nature cannot be created from a simple decree and would require the careful development of a national program, which would need to be constructed progressively in all areas.
Disclosure
All the authors declared no competing interests.
Acknowledgments
We would like to express our gratitude to Ma. Lugarda Cervantes Molina, Head of the Department of Social Work at the General Hospital of Mexico Dr. Eduardo Liceaga, and to Berenice Ortega Ibáñez, Ana Karen Guarda Ayala, Xóchitl Juárez Dávalos, Jessica Alejandra Pacheco Bernabé, Lucero Jiménez Ochoa, Magaly Wuendoly Ruiz Hernández, and Denise Valeria Castro Jiménez, all social work students performing an internship as part of CETIS 51 (Centro de Educación Técnica en Trabajo Social). We would also like to thank Victor Martinez Suarez for helping with proofreading.
References
- 1.Jha V., Garcia-Garcia G., Iseki K. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:260–372. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 2.Institute for Health Metrics and Evaluation. Mexico. University of Washington, Seattle, WA. Available at: http://www.healthdata.org/mexico (accessed on August 30, 2016).
- 3.Gómez-Dantés H., Fullman N., Lamadrid-Figueroa H. Dissonant health transition in the states of Mexico, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2016;388:2386–2402. doi: 10.1016/S0140-6736(16)31773-1. [DOI] [PubMed] [Google Scholar]
- 4.Alegre-Díaz J., Herrington W., López-Cervantes M. Diabetes and cause-specific mortality in Mexico City. N Engl J Med. 2016;375:1961–1971. doi: 10.1056/NEJMoa1605368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Obrador G.T., García-García G., Villa A.R. Prevalence of chronic kidney disease in the Kidney Early Evaluation Program (KEEP) México and comparison with KEEP US. Kidney Int Suppl. 2010;(116):S2–S8. doi: 10.1038/ki.2009.540. [DOI] [PubMed] [Google Scholar]
- 6.Franco-Marina F., Tirado-Gómez L.L., Estrada A.V. An indirect estimation of current and future inequalities in the frequency of end stage renal disease in Mexico. Salud Publica Mex. 2011;53 Suppl 4:506–515. doi: 10.1590/s0036-36342011001000015. [DOI] [PubMed] [Google Scholar]
- 7.Lozano R., Gómez-Dantés H., Garrido-Latorre F. Burden of disease, injuries, risk factors and challenges for the health system in Mexico. Salud Publica Mex. 2013;55:580–594. [PubMed] [Google Scholar]
- 8.Knaul F.M., González-Pier E., Gómez-Dantés O. The quest for universal health coverage: achieving social protection for all in Mexico. Lancet. 2012;380:1259–1279. doi: 10.1016/S0140-6736(12)61068-X. [DOI] [PubMed] [Google Scholar]
- 9.Frenk J., Knaul F., Gómez-Dantés O., González-Pier E. Ministry of Health; Mexico City: 2004. Fair Financing and Universal Protection: The Structural Reform of the Mexican Health System. [Google Scholar]
- 10.Navarro-Reynoso F. Hospital General de México 107 Anniversary. Rev Med Hosp Gen Méx. 2012;75:73e5. [Google Scholar]
- 11.Rossano A., Valdez-Ortiz R., Garcia L. Reproducible model to perform kidney transplantation in a low-resource population. Transplant Proc. 2014;46:3032–3038. doi: 10.1016/j.transproceed.2014.07.028. [DOI] [PubMed] [Google Scholar]
- 12.López-Cervantes M., Rojas-Russell M.E., Tirado-Gómez L.L. Facultad de Medicina, Universidad Nacional Autónoma de México; México, City: 2009. Enfermedad renal crónica y su atención mediante tratamiento sustitutivo en México. [Google Scholar]
- 13.Garcia-Garcia G., Briseño-Rentería G., Luquín-Arellan V.H. Survival among patients with kidney failure in Jalisco, Mexico. J Am Soc Nephrol. 2007;18:1922–1927. doi: 10.1681/ASN.2006121388. [DOI] [PubMed] [Google Scholar]
- 14.Durán-Arenas L., Avila-Palomares P.D., Zendejas-Villanueva R. Direct cost analysis of hemodialysis units. Salud Publica Mex. 2011;53 Suppl 4:516–524. doi: 10.1590/s0036-36342011001000016. [DOI] [PubMed] [Google Scholar]
- 15.Jurkovitz C.T., Li S., Norris K.C., KEEP Investigators Association between lack of health insurance and risk of death and ESRD: results from the Kidney Early Evaluation Program (KEEP) Am J Kidney Dis. 2013;61(4 Suppl 2):S24–S32. doi: 10.1053/j.ajkd.2012.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D'Adamo E., Caprio S. Type 2 diabetes in youth: epidemiology and pathophysiology. Diabetes Care. 2011;34 Suppl 2:S161–S165. doi: 10.2337/dc11-s212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pinhas-Hamiel O., Zeitler P. Acute and chronic complications of type 2 diabetes mellitus in children and adolescents. Lancet. 2007;369:1823–1831. doi: 10.1016/S0140-6736(07)60821-6. [DOI] [PubMed] [Google Scholar]
- 18.Thomas M.C., Cooper M.E., Zimmet P. Changing epidemiology of type 2 diabetes mellitus and associated chronic kidney disease. Nat Rev Nephrol. 2016;12:73–81. doi: 10.1038/nrneph.2015.173. [DOI] [PubMed] [Google Scholar]
- 19.Morton R.L., Schlackow I., Mihaylova B. The impact of social disadvantage in moderate-to-severe chronic kidney disease: an equity-focused systematic review. Nephrol Dial Transplant. 2016;31:46–56. doi: 10.1093/ndt/gfu394. [DOI] [PubMed] [Google Scholar]
- 20.Hernández-Cordero S., Cuevas-Nasu L., Morán-Ruán M.C. Overweight and obesity in Mexican children and adolescents during the last 25 years. J Am Nutr Diabetes. 2017;7:e257. doi: 10.1038/nutd.2016.52. erratum J Am Nutr Diabetes. 2017;7:e280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garcia-Garcia G., Jha V., World Kidney Day Steering Committee CKD in disadvantaged populations. Kidney Int. 2015;87:251–253. doi: 10.1038/ki.2014.369. [DOI] [PubMed] [Google Scholar]
- 22.Garcia-Garcia G., Monteon-Ramos J.F., Garcia-Bejarano H. Renal replacement therapy among disadvantaged populations in Mexico: a report from the Jalisco Dialysis and Transplant Registry (REDTJAL) Kidney Int Suppl. 2005:S58–S61. doi: 10.1111/j.1523-1755.2005.09710.x. [DOI] [PubMed] [Google Scholar]
- 23.Cueto-Manzano A.M., Rojas-Campos E. Status of renal replacement therapy and peritoneal dialysis in Mexico. Perit Dial Int. 2007;27:142–148. [PubMed] [Google Scholar]
- 24.Kierans C., Padilla-Altamira C., Garcia-Garcia G. When health systems are barriers to health care: challenges faced by uninsured Mexican kidney patients. PLoS One. 2013;8:e54380. doi: 10.1371/journal.pone.0054380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smart N.A., Dieberg G., Ladhani M., Titus T. Early referral to specialist nephrology services for preventing the progression to end-stage kidney disease. Cochrane Database Syst Rev. 2014;18:CD007333. doi: 10.1002/14651858.CD007333.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Correa-Rotter R. Renal replacement therapy in the developing world: are we on the right track, or should there be a new paradigm? J Am Soc Nephrol. 2007;18:1635–1636. doi: 10.1681/ASN.2007040447. [DOI] [PubMed] [Google Scholar]
- 27.Feehally J. Health burden of kidney disease recognized by UN. Nat Rev Nephrol. 2012;8:12–13. doi: 10.1038/nrneph.2011.191. [DOI] [PubMed] [Google Scholar]
- 28.Chertorivski Woldenberg S., García Junco D., López Aranda V.H. Catalogo Universal de Servicios de Salud, CAUSES 2012. Ciudad de México: Secretaria de Salubridad y Asistencia. Talleres Gráficos de la Nación. 2012 [Google Scholar]
- 29.Frenk J., Gómez-Dantés O., Knaul F.M. The democratization of health in Mexico: financial innovations for universal coverage. Bull World Health Organ. 2009;87:542–548. doi: 10.2471/BLT.08.053199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Urquieta-Salomón J.E., Villarreal H.J. Evolution of health coverage in Mexico: evidence of progress and challenges in the Mexican health system. Health Policy Plan. 2016;31:28–36. doi: 10.1093/heapol/czv015. [DOI] [PubMed] [Google Scholar]
- 31.Servan-Mori E., Heredia-Pi I., Montañez-Hernandez J. Access to medicines by Seguro Popular beneficiaries: pending tasks towards universal health coverage. PLoS One. 2015;10:e0136823. doi: 10.1371/journal.pone.0136823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laurell A.C. The Mexican popular health insurance: myths and realities. Int J Health Serv. 2015;45:105–125. doi: 10.2190/HS.45.1.h. [DOI] [PubMed] [Google Scholar]
- 33.Arredondo A., Cuadra S.M., Duarte M.B. Challenges of the epidemiological and economic burdens associated with hypertension in middle-income countries: evidence from Mexico. BMC Public Health. 2015;15:1106. doi: 10.1186/s12889-015-2430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meza R., Barrientos-Gutierrez T., Rojas-Martinez R. Burden of type 2 diabetes in Mexico: past, current and future prevalence and incidence rates. Prev Med. 2015;81:445–450. doi: 10.1016/j.ypmed.2015.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gobierno de la República, Estados Unidos Mexicanos. Estrategia Nacional para la prevención y el control del sobrepeso, obesidad y la diabetes. Available at: http://promocion.salud.gob.mx/dgps/descargas1/estrategia/Estrategia_con_portada.pdf. Accessed November 15, 2015.
- 36.Di Bonaventura M.D., Le Lay A., Fournier J., Kull K. The burden of obesity in Mexico: prevalence, comorbidities, and associations with quality of life, resource utilization and productivity. Value Health. 2015;18:A843. [Google Scholar]
- 37.Consejo Mexicano de Nefrología. Nefrólogos Certificados en México. Available at: http://consejomexicanodenefrologia.org/nefrologos-con-certificacion-vigente/. Accessed November 15, 2015.
- 38.Dictamen de la Comisión de Salud de la Comisión de Salud de la LXII Legislatura de la Cámara de Senadores del Honorable Congreso de la Unión. Available at: http://sil.gobernacion.gob.mx/Archivos/Documentos/2014/10/asun_3162493_20141023_1413473621.pdf. Accessed November 15, 2015.
- 39.Obrador G.T., Rubilar X., Agazzi E., Estefan J. The challenge of providing renal replacement therapy in developing countries: the Latin American perspective. Am J Kidney Dis. 2016;67:499–506. doi: 10.1053/j.ajkd.2015.08.033. [DOI] [PubMed] [Google Scholar]