Abstract
Purpose
Radiation therapy (RT) is a common treatment for benign diseases in Germany. Because the treatment concepts are inconsistent, we conducted this pattern-of-care study on behalf of the German Cooperative Group on Benign Diseases to evaluate treatment standards in Germany.
Methods and materials
Questionnaires were mailed to all radiation therapy facilities in Germany. We assessed the treatment equipment, annual number of patients, treatment indications, and, in particular, treatment strategies in patients with benign diseases in 2014.
Results
We evaluated questionnaires returned by 116 participating institutions, of which 41 were ambulatory health care centers, 28 were private institutions, 27 were community hospitals, and 20 were university hospitals. On average, 2 linac accelerators and 2 megavoltage units were available in each institution. In 2014, a total of 36,830 patients were treated for benign diseases: 16,989 for degenerative diseases (peritendinitis humeroscapularis n = 2691; epicondylitis humeri n = 3788; heel spur n = 10,510); 14,936 for osteoarthritis (coxarthrosis n = 2230; gonarthrosis n = 2623; omarthrosis n = 2691; rhizarthrosis n = 2440; polyarthrosis n = 2297; others n = 2655); 1563 for hyperproliferative diseases (morbus Dupuytren n = 960; morbus Ledderhose n = 441; keloids n = 139; pterygium of the conjunctiva n = 3; other hyperproliferative diseases n = 20); 2440 for functional disorders (gynecomastia n = 843; Graves' disease n = 205; lymphatic fistula n = 178; heterotopic ossification prophylaxis n = 1214); 859 for stereotactic RT in the central nervous system (arteriovenous malformation n = 53; meningioma n = 425; acoustic neuroma n = 201; pituitary adenoma n = 131; others n = 49), and 43 for rare indications (pigmented villonodular synovitis n = 20 or vertebral hemangioma n = 23). The mean whole dose was <10 Gy in the treatment of degenerative disorders, 25 Gy for hyperproliferative diseases, 15 Gy for functional disorders, and <50 Gy for stereotactic RT.
Conclusions
In 2014, RT had an important role in the treatment of benign diseases. Because treatment concepts are inherent, we recommend treatment based on the guidelines written by the German Cooperative Group on Benign Diseases.
Summary.
In the present analysis, we evaluate the standard of care in radiation therapy for benign diseases in Germany. The German Cooperative Group on Benign Diseases evaluated all German institutions via mailed questionnaires and analyzed data from 36,830 patients who were irradiated for benign disorders. The results demonstrate a wide acceptance of this treatment in Germany.
Alt-text: Unlabelled box
Introduction
In contrast to Germany, where radiation therapy (RT) is commonly used and well accepted in the treatment of benign diseases, its use is rarely applied in other countries, Anglo-American regions in particular. Several publications show the low acceptance and worldwide undulation of RT for benign diseases.1, 2
Nevertheless, many German publications reflect the significance of RT across the country,3, 4, 5 which is due primarily to the foundation of the German Cooperative Group on Benign Diseases (GCG-BD) in 1996 by the German Society for Radiation Oncology (DEGRO). This group was founded to train physicians in the treatment of benign diseases, coordinate scientific work and clinical trials, and improve experience within this entity.
The GCG-BD conducted many patterns-of-care studies (PCSs) to evaluate the standard of treatment.6, 7, 8, 9 In 2015, DEGRO published guidelines for radiotherapeutic treatment of nonmalignant disorders.10, 11, 12, 13 All of this underlines the value of RT for benign diseases in Germany, resulting from the work and annually organized scientific meetings of the GCG-BD. Seegenschmiedt et al conducted the first national PCS in 1994, 1995, and 1996 to evaluate technical equipment, treatment concepts, treatment indications, and numbers of patients.7
Although guidelines are available, treatment concepts are inconsistent. Therefore, we conducted this national PCS on behalf of the GCG-BD and DEGRO to evaluate the actual treatment standard in Germany and to compare the results with previous findings.
Methods and materials
In 2015, a questionnaire was mailed to all radiation therapy institutions in Germany, Austria, and Switzerland. After 8 weeks, the nonresponding centers were contacted via phone and mail. After another 8 weeks, the remaining centers were contacted again.
The questionnaire was used to collect the following information: 1) general information, 2) type and number of technical equipment, 3) number of patients, and 4) specific information. In a second part, data were collected to assess the following 5 subgroups of benign dysfunctions: a) degenerative, b) hyperproliferative, c) functional, d) stereotactic RT in the central nervous system (CNS), and e) rare indications. The values collected were the number of patients per disease category, single entity, single and total doses applied, fractions per week, total fractions, and number of treatment courses. The Kolmogorov-Smirnov, Shapiro-Wilk, and Kruskal-Wallis tests were applied using SPSS (version 24.0).
Results
General information and technical equipment
Of the 116 questionnaires that were returned by institutions (35%), 20 (17%) were from university hospitals, 27 (23%) from municipal hospitals, 28 (25%) from private institutions, and 41 (32%) from ambulatory health care centers (Figure 1). On average, 2 linac accelerators (range, 1-6) and 2 megavoltage units were available at each institution. Additionally, 27 institutions used orthovoltage units with a median age of 17 years (range, 1-52 years). In comparison, the linac accelerators had a median age of 5 years (range, 1-18 years).
Figure 1.
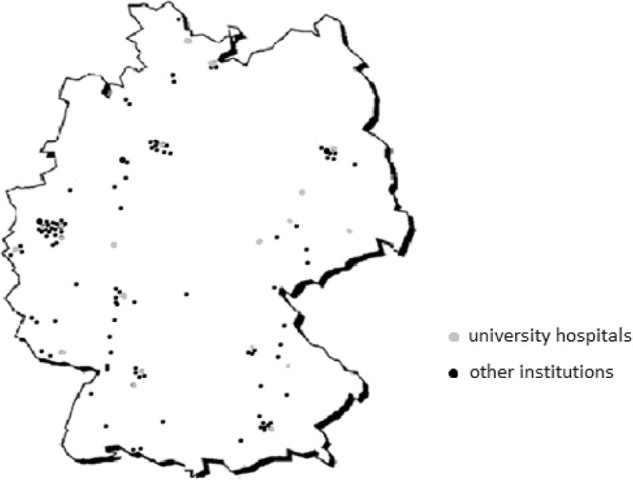
Participating centers in Germany.
Treatment indications and treatment concepts
In total, of the 53,932 patients receiving RT in 2014, 36,830 (68%) had benign diseases. Of those, 16,989 patients (46%) were treated for degenerative diseases, another 14,936 (40%) for osteoarthritis, 1563 (4%) for hyperproliferative diseases, and 2440 (7%) for functional disorders. Of the remainder, 859 (2%) received stereotactic RT of the CNS, and 43 patients were irradiated because of rare indications.
Degenerative diseases included peritendinitis humeroscapularis (n = 2691), epicondylitis humeri (n = 3788), and heel spur (n = 10,510). Osteoarthritis included coxarthrosis (n = 2230), gonarthrosis (n = 2623), omarthrosis (n = 2691), rhizarthrosis (n = 2440), polyarthrosis (n = 2297), and others (n = 2655). Hyperproliferative diseases included morbus Dupuytren (n = 960), morbus Ledderhose (n = 441), keloids (n = 139), pterygium of the conjunctiva (n = 3), and other hyperproliferative diseases (n = 20). Functional disorders included gynecomastia (n = 843), Graves' disease (n = 205), lymphatic fistula (n = 178), and heterotopic ossification prophylaxis (n = 1214). Stereotactic RT of the CNS included arteriovenous malformation (n = 53), meningioma (n = 425), acoustic neuroma (n = 201), pituitary adenoma (n = 131), and others (n = 49). Other rare indications were pigmented villonodular synovitis (n = 20) and vertebral hemangioma (n = 23).
Not all institutions revealed their treatment concepts in detail, but information from 80 institutions (68%) was available. The mean total dose was <10 Gy (range, 0.45-8 Gy) in the treatment of degenerative disorders, 25 Gy for hyperproliferative diseases (range, 8.75-30 Gy), 15 Gy for functional disorders (range, 2.1-40 Gy), and <50 Gy (range, 21-60 Gy) for stereotactic RT. Further details are shown in Table 1, Table 2.
Table 1.
Detailed information of treatment
| Disease category | University hospital | Community hospital | Medical practice | Ambulatory health care center | All institutions |
|---|---|---|---|---|---|
| Degenerative diseases | |||||
| Total institutions | n = 15 | n = 19 | n = 13 | n = 28 | n = 75 |
| Total patients | 4582 (13.5%) | 7692 (22.6%) | 6180 (18.1%) | 15,588 (45,8%) | 34,042 (100%) |
| Patients (mean ± SD) | 11 ± 536 | 250 ± 495 | 350 ± 417 | 245 ± 690 | 258 ± 572 |
| Range | 11-2102 | 5-692 | 37-1500 | 0-2818 | 0-2818 |
| Hyperproliferative diseases | |||||
| Total institutions | n = 15 | n = 17 | n = 12 | n = 24 | n = 68 |
| Total patients | 283 (22.5%) | 232 (18.4%) | 226 (18%) | 518 (41.1%) | 1259 (100%) |
| Patients (mean ± SD) | 5 ± 49 | 8 ± 14 | 17 ± 15 | 9 ± 42 | 8 ± 35 |
| Range | 0-194 | 0-46 | 1-51 | 0-206 | 0-206 |
| Functional diseases | |||||
| Total institutions | n = 16 | n = 20 | n = 14 | n = 22 | n = 72 |
| Total patients | 403 (16.9%) | 908 (38.1%) | 439 (18.4%) | 634 (26.6%) | 2384 (100%) |
| Patients (mean ± SD) | 21 ± 21 | 25 ± 68 | 15 ± 61 | 21 ± 23 | 20 ± 47 |
| Range | 3-90 | 2-314 | 2-241 | 0-75 | 0-314 |
| Stereotactic indications | |||||
| Total institutions | n = 15 | n = 12 | n = 9 | n = 21 | n = 57 |
| Total patients | 654 (77.9%) | 50 (6%) | 21 (2.5%) | 114 (13.6%) | 839 (100%) |
| Patients (mean ± SD) | 30 ± 61 | 2 ± 6 | 0 ± 6 | 0 ± 12 | 2 ± 36 |
| Range | 3-249 | 0-17 | 0-17 | 0-37 | 0-249 |
| Rare indications | |||||
| Total institutions | n = 11 | n = 10 | n = 12 | n = 20 | n = 53 |
| Total patients | 20 (40.8%) | 4 (8.2%) | 15 (30.6%) | 10 (20.4%) | 49 (100%) |
| Patients (mean ± SD) | 1 ± 3 | 0 ± 1 | 0 ± 3 | 0 ± 1 | 0 ± 2 |
| Range | 0-8 | 0-1 | 0-8 | 0-5 | 0-8 |
SD, standard deviation.
Table 2.
Dosage and fractionation
| Diagnosis | Single dose (Gy) | Total dose (Gy) | Fraction schedule |
|---|---|---|---|
| Degenerative diseases | |||
| Painful joints: insertion tendinitis | 0.45-1 | 2-8 | 2-4x/week |
| Painful joints: arthritis | 0.5-1 | 2-8 | 1-4x/week |
| Hyperproliferative diseases | |||
| M. Dupuytren | 2-7 | 15-30 | 3-10x/week |
| M. Ledderhose | 0.5-7 | 3-20 | 2-5x/week |
| Keloid | 1-7.5 | 7-20 | 2-5x/week |
| Pterygium | 5-10 | 8,75-20 | 1-2x/week |
| Functional diseases | |||
| Gynecomastia | 1.8-12 | 10-25 | 1-5x/week |
| Lymphatic fistula | 0.5-3 | 2,5-40 | 2-5x/week |
| Endocrine orbitopathia | 0.3-10 | 2,1-24 | 1-5x/week |
| Heterotopic ossification | 1-8 | 6-12 | 1-5x/week |
| Stereotactic indications | |||
| Ateriovenosis malformation | 1.8-22.5 | 12-54 | 1-5x/week |
| Menigioma | 1.8-18 | 14-60 | 1-5x/week |
| Acoustic neuroma | 2-15 | 14-60 | 1-5x/week |
| Pituitary adenoma | 1.5-25 | 13-54 | 1-5x/week |
Of the 80 institutions that provided details about specializations, 36 (45%) provided specialized consultation hours for benign diseases. Of the 69 institutions that provided details about clinical studies, 19 (27.5%) participated in them. Of the 64 institutions that provided details about publishing results, 10 (15.6%) publish their own results.
Discussion
This PCS shows the wide acceptance of RT for treatment of benign diseases across Germany. Benign indications account for more than one-third of all patients treated annually. The first PCS of RT for benign diseases was conducted by Seegenschmiedt et al in 1994 through 1996 and included 20,082 patients treated annually.7 The number of patients has nearly doubled within 20 years. This could be due to a number of reasons. First, Germany now has 340 active centers, compared with 152 in 1996. Because several studies have demonstrated the effectiveness of RT for benign diseases,3, 4, 5, 6, 7, 8, 9, 14, 15, 16, 17, 18, 19 RT is commonly used for several benign indications. In comparison with the first PCS, there is no change within the treatment concepts but rather a change in indications. Only 155 patients in the first PCS were treated because of meningioma, acoustic neuroma, or pituitary adenoma in contrast with the 757 patients in the present PCS.
There are retrospective data that encourage RT for degenerative diseases,6, 7, 20, 21 but unfortunately there are no prospective trials comparing RT with surgical treatment or the use of nonsteroidal anti-inflammatory drugs (NSAIDs) in this setting. One of the best-evaluated indications within randomized trials is the use of RT in heterotopic ossification prophylaxis.14, 15, 16, 17, 18 A risk–benefit ratio is available, and the 2 treatment options are perioperative RT and NSAIDs. Gregoritch et al and Knelles et al reported improved outcomes in hip function in contrast with no treatment and generally better outcomes for both RT and NSAIDs. Although RT shows treatment-related advantages in toxicity and patient compliance, NSAIDs are not as expensive and are more easily accessible.14, 15
Another indication with possible long-term follow-up data is RT for morbus Dupuytren. Nonradiotherapeutic treatment options are vitamins or steroids and surgical approaches. The efficacy of RT depends on the stage of disease. Betz et al studied patients with a median follow-up of 13 years and found avoidance of progression and improvement in 87% of patients in a stage with only nodules and chords and in 70% of patients with extension deficits.19
Another possible reason for widespread use of RT for benign diseases in German-speaking countries is that several studies and PCS of benign disorders conducted by the GCG-BD show the state of treatment and the possible indications, although major prospective trials remain to be seen6, 7, 9, 20, 21 to underline the effectiveness. Prospective randomized trials especially would further encourage the use of RT in benign diseases.
Because the performed PCS focused on special indications, this analysis calls into question the state of treatment in Germany. In comparison with the United States and other European countries, the use of RT for benign diseases is well accepted because of the available data, low side effects, and wide acceptance within the patient population. The contrast between eastern and western countries that was reported in the first PCS was not seen in the present analysis. There is also no difference between country and urban areas.
The participation of the centers varied between several PCS. Muecke et al obtained the best participation in their PCS on painful gonarthrosis:. Of 248 institutions, 238 (95.9%) completed their questionnaires.6 Seggenschmiedt et al received participation from 134 of 152 institutions (88%).7 Fewer questionnaires were completed for the study conducted by Micke et al in a PCS on painful heel spurs (101 returns) and on desmoid tumors (146 returns).9, 21 In comparison, we received 116 completed questionnaires, which is comparable to the number of questionnaires used in the first general PCS by Seegenschmiedt et al.7
Perhaps because of the wide distribution of centers, only a few chose to participate in the PCS questionnaires. In the past years, many private and therefore cost-oriented institutions were established, and their interest in research participation may be low. Only 19 institutions (5.5%) were interested in clinical studies and participated in studies, and only 10 institutions (2.9%) published their data. This is comparable to prior findings. In 1996, only 4% of participating centers participated in clinical studies.7
The high rate of patients (68%) who were treated for benign diseases among the patient populations we evaluated must be interpreted with care. On one hand, we received only 116 completed questionnaires, so there is a bias in the data. On the other hand, this could be a realistic number because 25% were private institutions and 32% were ambulatory health care centers that treat large numbers of patients with benign diseases.
Within the past few years, technical equipment has changed substantially. In 1996, 104 cobalt units were available, and 102 institutions had orthovoltage devices. We found no institutions treating with cobalt units, and only 27 centers used orthovoltage units. This reflects the high standard of treatment across Germany and possibly accounts for the wide acceptance of RT. Long-term toxicity and radiation-induced malignancies are feared and associated with old-fashioned equipment and the use of orthovoltage units. Another change due to the technological improvement in the past years is the increased number of patients treated for meningioma, acoustic neuroma, and pituitary adenoma.
Recently, because of the large amount of data available from clinical studies, PCS guidelines have been published by the GCG-BD on behalf of the DEGRO. They serve as a model in the treatment of benign diseases. In particular, when facing rare indications, treating physicians are encouraged to follow these guidelines. In addition, existing guidelines will encourage even more acceptance of RT in the treatment of benign diseases. Nevertheless, due to the heterogeneity of RT concepts, clinical studies should be encouraged to optimize treatment strategies and promote the responsible use of RT for patients with benign diseases.
Conclusions
This analysis underscores the widespread use of RT in the treatment of benign disorders in Germany. The large number of treated patients demonstrates the wide acceptance of this treatment option. Several published clinical studies, PCSs, and, in the last several years, consensus guidelines have helped establish this treatment. For benign diseases, RT continues to play an important treatment role.
Footnotes
Meeting information: Presented at the 58th Annual Meeting of the American Society for Therapeutic Radiology and Oncology in Boston, Massachusetts; September 25-28, 2016.
Conflicts of interest: None.
References
- 1.Order S., Donaldson S.S. 2nd ed. Springer; New York, NY: 1998. Radiotherapy of Benign Diseases. [Google Scholar]
- 2.Leer J., van Houtte P., Daelaar J. Indications and treatment schedules for irradiation of benign diseases: A survey. Radiother Oncol. 1998;48:249–257. doi: 10.1016/s0167-8140(98)00051-6. [DOI] [PubMed] [Google Scholar]
- 3.Heyd R., Micke O., Berger B. Radiation therapy in the treatment of pigmented villonodular synovitis (PVNS). Results of a national patterns of care study. Int J Radiat Oncol Biol Phys. 2010;78:199–204. doi: 10.1016/j.ijrobp.2009.07.1747. [DOI] [PubMed] [Google Scholar]
- 4.Kriz J., Eich H.T., Bruns F. Radiotherapy in Langerhans cell histiocytosis—a rare indication in a rare disease. Radiat Oncol. 2013;9:233. doi: 10.1186/1748-717X-8-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neu B., Sautter V., Momm F. Radiotherapy for prevention and therapy of gynecomastia due to antiandrogen treatment in prostate cancer patients: A patterns of care study. Strahlenther Onkol. 2011;187:771–777. doi: 10.1007/s00066-011-2283-x. [DOI] [PubMed] [Google Scholar]
- 6.Muecke R., Seegenschmiedt M.H., Heyd R. Radiotherapy in painful gonarthrosis. Results of a National Patterns of care study. Strahlenther Onkol. 2010;186:7–17. doi: 10.1007/s00066-009-1995-7. [DOI] [PubMed] [Google Scholar]
- 7.Seegenschmiedt M.H., Katalinic A., Makoski H. Radiation therapy for benign diseases: Patterns of care study in Germany. Int J Radiat Oncol Biol Phys. 2000;47:195–202. doi: 10.1016/s0360-3016(99)00537-4. [DOI] [PubMed] [Google Scholar]
- 8.Heyd R., Micke O., Surholt C. Radiation therapy for Gorham Stout Syndrome: Results of a national patterns of care study and literature review. Int J Radiat Oncol Biol Phys. 2011;81:179–185. doi: 10.1016/j.ijrobp.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Micke O., Seegenschmiedt M.H. Radiation therapy for aggressive fibromatosis (desmoid tumors): Results of a national patterns of care study. Int J Radiat Oncol Biol Phys. 2005;61:882–891. doi: 10.1016/j.ijrobp.2004.07.705. [DOI] [PubMed] [Google Scholar]
- 10.Reichl B., Block A., Schäfer U. DEGRO practical guidelines for radiotherapy of non-malignant disorders: Part I: Physical principles, radiobiological mechanisms, and radiogenic risk. Strahlenther Onkol. 2015;191:701–709. doi: 10.1007/s00066-015-0865-8. [DOI] [PubMed] [Google Scholar]
- 11.Ott O., Niewald M., Weitmann H. DEGRO guidelines for the radiotherapy of non-malignant disorders. Part II: Painful degenerative skeletal disorders. Strahlenther Onkol. 2015;191:1–6. doi: 10.1007/s00066-014-0757-3. [DOI] [PubMed] [Google Scholar]
- 12.Seegenschmiedt M.H., Micke O., Niewald M. DEGRO guidelines for the radiotherapy of non-malignant disorders: Part III: Hyperproliferative disorders. Strahlenther Onkol. 2015;191:541–548. doi: 10.1007/s00066-015-0818-2. [DOI] [PubMed] [Google Scholar]
- 13.Reinartz G., Eich H.T., Pohl F. DEGRO practical guidelines for the radiotherapy of non-malignant disorders—Part IV: Symptomatic functional disorders. Strahlenther Onkol. 2015;191:295–302. doi: 10.1007/s00066-014-0789-8. [DOI] [PubMed] [Google Scholar]
- 14.Gregoritch S.J., Chadha M., Pellegrini V.D., Rubin P., Kantorowitz D.A. Randomized trial comparing preoperative versus postoperative irradiation for prevention of heterotopic ossification following prosthetic total hip replacement: Preliminary results. Int J Radiat Oncol Biol Phys. 1994;30:55–62. doi: 10.1016/0360-3016(94)90519-3. [DOI] [PubMed] [Google Scholar]
- 15.Knelles D., Barthel T., Karrer A., Kraus U., Eulert J., Kolbl O. Prevention of heterotopic ossification after total hip replacement: A prospective, randomized study using acetylsalicyl acid, indomethacin and fractional or single dose irradiation. J Bone Joint Surg Br. 1997;79:596–602. doi: 10.1302/0301-620x.79b4.6829. [DOI] [PubMed] [Google Scholar]
- 16.Kolbl O., Knelles D., Barthel T., Raunecker F., Flentje M., Eulert J. Preoperative irradiation versus the use of nonsteroidal anti-inflammatory drugs for prevention of heterotopic ossification following total hip replacement: The results of a randomized trial. Int J Radiat Oncol Biol Phys. 1998;42:397–401. doi: 10.1016/s0360-3016(98)00204-1. [DOI] [PubMed] [Google Scholar]
- 17.Seegenschmiedt M.H., Martus P., Goldmann A.R., Wolfel R., Keilholz L., Sauer R. Preoperative versus postoperative radiotherapy for prevention of heterotopic ossification: First results of a randomized trial in high-risk patients. Int J Radiat Oncol Biol Phys. 1994;30:63–73. doi: 10.1016/0360-3016(94)90520-7. [DOI] [PubMed] [Google Scholar]
- 18.Seegenschmiedt M.H., Keilholz L., Martus P. Prevention of heterotopic ossification about the hip: Final results of two randomized trials in 410 patients using either preoperative or postoperative radiation therapy. Int J Radiat Oncol Biol Phys. 1997;39:161–171. doi: 10.1016/s0360-3016(97)00285-x. [DOI] [PubMed] [Google Scholar]
- 19.Betz N., Ott O.J., Adamietz B., Sauer R., Fietkau R., Keilholz L. Radiotherapy in early-stage Dupuytren's contracture. Long-term results after 13 years. Strahlenther Onkol. 2010;186:82–90. doi: 10.1007/s00066-010-2063-z. [DOI] [PubMed] [Google Scholar]
- 20.Micke O., Seegenschmiedt M.H. Consensus guidelines for radiation therapy of benign diseases: A multicentre approach in Germany. Int J Radiat Oncol Biol Phys. 2002;52:496–513. doi: 10.1016/s0360-3016(01)01814-4. [DOI] [PubMed] [Google Scholar]
- 21.Micke O., Seegenschmiedt M.H. Radiotherapy in painful heel spurs (plantar fasciitis) – results of a national patterns of care study. Int J Radiat Oncol Biol Phys. 2004;58:828–843. doi: 10.1016/S0360-3016(03)01620-1. [DOI] [PubMed] [Google Scholar]


