Abstract
Background:
State Medicaid programs in the United States provide services to children with special health care challenges through the Early Prevention, Screening, Diagnostic, and Treatment program. One element of the services provided is Medicaid Personal Care Services (PCS), which are intended to correct or ameliorate any functional impairments faced by a child or youth (C/Y) in the community. Previous research indicates that considerable variation in the allocation of PCS depends on the assessor. A case-mix model is developed that might make the distribution of such services more uniform and equitable.
Data:
The sample in this research includes 2708 C/Y aged 4 to 20 who were receiving PCS in Texas in 2008.
Results:
A case-mix model was developed that groups sample members into 33 categories based on the number of hours of PCS authorized by an assessor. The Pediatric Personal Care Allocation Model (PCAM) explains 27% of the variance in the allocation of PCS hours.
Discussion:
The implementation of the PCAM should provide guidance to assist in ensuring that C/Y facing similar functional challenges receive similar levels of PCS. However, implementation of any case-mix model is only a first step in moving to a prospective payment system for PCS.
Keywords: Medicaid, EPSDT, Case-Mix, Personal Care, Pediatrics
Background
In last half century in health policy in the United States, much of the conflict and resultant progress has involved the extension of various health services and health insurance programs to a variety of vulnerable populations. This extension of services began in the mid-1960s with the Great Society programs at the heart of President Lyndon Johnson’s domestic policy agenda. The highlights of this era of progress included the introduction of Medicare, an insurance program largely for older persons, and Medicaid, an insurance program for lower income families and individuals.1
As part of this movement, the US Congress passed legislation in 1967 establishing Medicaid’s Early Prevention, Screening, Diagnostic, and Treatment (EPSDT) program. In the fiscal year of 2015, almost 40 million children or youth received services through the EPSDT program. The program has 2 basic elements. The first element, which involves all program participants, focuses on prevention, screening, and diagnosis—in 2015, the program recorded almost 50 million screenings of participants.2
The second element involves providing all medically necessary services for Medicaid recipients fewer than 21 years of age who face chronic health challenges that demand more than the usual well-child screenings or services required by some short-lived, acute episode. Part of this second element of the EPSDT program is the focus of this effort.
As the Center for Medicare and Medicaid Services indicates,3
The Act provides for coverage of all medically necessary services . . . [that may] include physician and hospital services, private duty nursing, personal care services, home health and medical equipment and supplies, rehabilitative services, and vision, hearing, and dental services. Covered EPSDT services also include “any other medical care, and any other type of remedial care recognized under State law, [and] specified by the [US Department of Health and Human Services’] Secretary”. (p. 9)
Of interest in this research are personal care services (PCS) provided via the EPSDT program. These services are meant to “correct or ameliorate” the effect of any impairment or health challenge to a child or youth’s functional status. Services must be authorized by a medical professional and pre-approved by the responsible state agency. They may include assistance with any activities of daily living (ADLs—such as using the toilet, mobility, eating, or dressing) or any instrumental ADLs (IADLs—such as assistance with medications, meal preparation, laundry).4
Previous research with these data, which did not involve an attempt to create case-mix groups, used structural equation modeling. This research investigated caregivers’ reports of children’s impairment and case managers’ decisions concerning the number of hours of Medicaid PCS allocated to the children or youth (C/Y). Those results indicated that 29.4% of the variation in case managers’ decisions concerning the allocations personal care hours was explained by the client’s functional status, their age, and any behavior problems. However, supplementary analyses also indicated that 22% of the variance in PCS allocations was explained by the identity of the case manager. Such a strong influence of who performed the assessment on the hours allocated raises concerns about possible inequity in the allocation of PCS program resources. Similar C/Y may be receiving different service levels, based on the predilections of the persons assessing them.5
Such results imply a need for some more uniform structure for decision making concerning PCS hours, one that will assist in assuring that children or youth with the same needs receive the same level of program resources, no matter who the assessor might be. To assist in the development of a more uniform and effective allocation of PCS hours, this research presents a case-mix model for the allocation of PCS hours to children and youth with special health care challenges who are living in the community.
The basic purpose of any case-mix model is to assure that persons with similar care needs receive similar levels of program resources.6 While there is some evidence of case-mix modeling being used for allocating health services to children, acuity-based payment has long been in use in payment systems in a variety of health care sectors in the United States. Diagnosis-related groups are used for Medicare reimbursement in acute care.7 The Resource Utilization Groups’ (RUGs) case-mix model, now in their third incarnation (RUGIII), is used for nursing home payment in many states.8 The RUGIII model, Resource Utilization Groups III for Home Care (RUGIII/HC) is used, or under consideration, in a variety of state home care programs.9
What distinguishes this effort from these other efforts is that it presents a case-mix classification model specifically developed for use in the allocation of PCS services to children or youth living in the community and facing special health care challenges that result in functional impairment.
Methods
Data
In 2008, the Medicaid program administered by the Texas Health and Human Services Commission began assessing children in its EPSDT program with an early version of the interRAI PEDS HC assessment form.10,11 The instrument was used to assess the PCS needs of all C/Y in the program.
Assessment data were collected for 6 months by state case managers on a paper form and then entered into an electronic database. The database contained a total of 3068 assessments. Data were collected on 2780 children and youth (C/Y) from 4 to 20 years of age. Missing data reduced the number of C/Y included in this analysis to 2705, 97% of the 4 to 20 sample. Only the data for C/Y from 4 to 20 years old are used in this analysis.
A case manager employed by the Texas Department of State Health Services completed the assessment. The case managers were largely licensed social workers, with a few Registered Nurses among them. A home visit with the primary caregiver and the child was the setting in which the assessments were completed. The assessment was completed by observing the C/Y, querying the caregiver, and questioning the C/Y, if he or she could respond. Although these data were gathered during active program operations, they have proven their usefulness in many papers that have appeared in peer-reviewed journals.5,12–18
Measurement
Dependent variable
The dependent variable in this study is the hours of Medicaid PCS authorized by the Medicaid program assessor. Personal care services, provided by personal care assistants, include coding for different levels of assistance—setup, cueing, redirection, monitoring for safety, and hands-on assistance—with ADLs or with IADLs.
Independent variables
The PEDS HC assessment instrument contains items that generated information in a variety of domains relevant to the delivery of PCS, including the following:
Medical diagnoses and health conditions;
Indicators of cognitive function and memory;
Indicators of any psychiatric or behavioral health diagnoses or issues;
Treatments, therapies, health service use;
Measures of assistance provided with functional (ADL and IADL) challenges related to the C/Y’s conditions or diagnoses.
An extensive number of variables found useful in previous research on case-mix were used in the initial analyses. Bivariate analyses identified the variables useful in predicting hours of PCS for the sample and for building a case-mix model. Many diagnoses and conditions helped form the basic case-mix categories (see Table 1). Groups within these categories were based on at least 2 other variables. The precise definitions of these variables appear at the end of Table 1.
Table 1.
Definitions of Pediatric Personal Care Allocation Model categories and distributions of supplementary variables used to create groups within categories (N = 2725).
| Pediatric personal care allocation model categories | ||
|---|---|---|
| Categories | Percent of sample (n) | Defining factors |
| Extensive Challenges | 8.1% (n = 220) |
Any of list: chemotherapy, radiation therapy, dialysis, hospice care, restorative nursing, intravenous medications, intravenous feeding, or wound or skin lesion care |
| Special Challenges | 32.8% (n = 894) |
Any of list: nasopharyngeal suctioning, urinary catheter care, bedbound or chairfast, fall in last week, pain interferes with normal activities, or recurrent aspiration |
| Complex Challenges | 27.6% (n = 751) |
Any of list: anemia, cancer, cystic fibrosis, explicit terminal prognosis, metabolic disorder, any plegia, traumatic brain injury, an antibiotic resistant infection, contractures, hospital admission in last 30 days, an anxiety disorder, autistics disorder or other pervasive developmental disorder, schizophrenic, schizoaffective, or psychotic disorder, somatoform, eating or tic disorder |
| Cognitive Challenges | 12.3% (n = 335) |
None of the specific challenges listed above but at least moderately dependent in decision making or sometimes, rarely/never understood |
| Functional Challenges | 19.3% (n = 525) |
None of the specific challenges listed above but needs ADL assistance |
| Variables used to develop groups within categories | ||
| Variables | Distribution | Definition |
| Age Group Indicator | 1 = 4-8 2 = 9-15 3 = 16-20 |
Indicates child’s age at time of assessment |
| Functional Scale | 0-5 | Scale includes hands-on assistance provided in bed mobility, locomotion inside the home, transfer, and the need for a 2-person transfer, and the need for assistance in medication management (one point for each named function) |
| IADL Status Indicator | 0 or 1 | Indicates whether child or youth is totally dependent in any of 7 IADLs |
| Behavior Status Indicator | 0 or 1 | Indicates whether child or youth resisted ADL assistance, treatments or therapies, or engaged in self-injurious behavior in the last 7 days |
Abbreviations: ADL, activity of daily living; IADL, instrumental activity of daily living.
The only one of the supplementary indicators or scales used to develop groups that is not “normal fare” in case-mix modeling is age. Earlier research on case-mix for annual Medicaid home care expenditures with this population did not demand the inclusion of age.19 However, preliminary analyses of PCS hours for this modeling endeavor indicated a strong interaction between age and functional needs. The 3 age groups were defined by the grouping software.
Analysis strategy
The Pediatric Personal Care Allocation Model Development
The 5 general categories in the Pediatric Personal Care Allocation Model (PCAM) draw heavily on earlier work on case-mix modeling for nursing home residents8 and case-mix modeling for adult home care.9 It is, however, most heavily influenced by the case-mix modeling of home care expenditures for children in the EPSDT program, the Pediatric Expenditure Classification Model for Home Care (PECM).19
The PCAM divides C/Y receiving Medicaid PCS into 5 general categories of C/Y. These categories include Extensive Challenges, Special Challenges, Complex Challenges, Cognitive Challenges, and Functional Challenges. This nomenclature, these categories, and their definitions largely follow those of the PECM19 and the RUGs for Home Care model.9 The specific definition of each of these categories may differ from that in earlier models, depending on the average PCS hours related to specific items on the PEDS HC assessment in this sample.
The PCAM is a hierarchical model. After the categories were defined, all cases were evaluated to determine which participants fit in the Extensive Challenges category. All participants not selected for inclusion in the Extensive Challenges category were tested to determine whether they fit in the group with the next highest average PCS hours, the Special Challenges category. Then, all those cases that did not fit the requirement for the Special Challenges category were evaluated to determine whether they fit into the third category (Complex Challenges). This process continued until all those not in the 4 top categories were grouped into the final category, Functional Challenges, which has the lowest average PCS hours. This process places each sample member in the PCAM category that, given their characteristics, has the highest average PCS hours.
Within each of the 5 basic categories, as noted above, 4 sets of variables were considered when developing case-mix groups within these categories: age, functional (ADL/IADL) care provision, IADL care provision, and behavioral challenges.
Case-mix model development always involves attention both to the results provided by grouping software and to the researcher’s judgment. On a few occasions, the results from the grouping software are not reasonable. For example, the results might indicate that a small group of children with less functional impairment receive more hours of care than another small group composed of children with greater functional impairment. Such a result would be considered idiosyncratic and the split between these 2 groups suggested by the software would be ignored. The analyst’s judgment would take precedent over the software’s suggestions.
This means that different analyses of one database may—depending on starting assumptions, results, and the researcher judgment—yield different case-mix models.
Developing case-mix indices
Each group’s average number of PCS hours was used to calculate its case-mix index (CMI). The CMI was calculated by dividing each group’s average PCS hours by the average PCS hours for the group with the lowest average number of PCS hours. That means the lower bound of the CMIs is 1.00.
The use of CMIs creates the opportunity for states or programs that operate with different overall numbers of hours or average hours to use the PCAM. The basic assumption of this approach is that while average PCS hours may vary across settings or populations, the relative differences among groups (CMIs) will remain relatively constant. This assumption is common across a variety of case-mix modeling efforts with somewhat different dependent variables or populations.8,9,19
Evaluating the case-mix model
The percent of variance (adjusted R2) in PCS hours explained by the case-mix groups is the most basic standard for evaluating the usefulness of a case-mix model.
However, one can assess case-mix models in additional ways. Logistic regression models can be estimated to determine the degree to which a model correctly places children or youth in the lower quartile of allocated hours or the highest quartile of allocated hours. As a rule of thumb, the C-statistic generated by these models should be above 0.70.19 One can also compare the coefficient of variation (CV) for each group with that of the entire sample. A group’s CV should be smaller than the sample CV.
To test the robustness of case-mix models, researchers often build the model on one part of a database, and they then test the model on the remainder of the database. The desire for relatively stable hour estimates, the sample size, and the number of expected groups in the model leads to a different strategy in this effort. Model development involved the entire sample. The model’s robustness was tested by estimating the model’s explained variance in 10 randomly drawn 50% subsamples of the database.
Unfortunately, as this research presents the first published Medicaid pediatric PCS case-mix model, the PCAM’s usefulness cannot be directly compared with similar models. Such alternative models may be developed later, and at that time, their explanatory power, face validity, and robustness can be compared with that of the PCAM.
Statistical software
STATA 14 statistical software was used for data manipulation, descriptive and bivariate analyses, and multivariate analyses.20 XLSTAT 2015 was used to construct the case-mix groups within each category, based on XLSTAT’s implementation of Kass’ (1980) chi-square automatic interaction detection (CHAID) method.21,22 Some of the final splits, on IADLs or behaviors, in the groups developed using CHAID were based on testing mean differences using STATA.
Results
Extensive descriptive data concerning the sample can be found in the published research noted above.5,12,13,19 The information below, however, provides a glimpse at the status of children and youth included in the study sample:
Average age of the sample = 12.1 years of age;
Interquartile range = 8 to 17 years of age;
Men = 57.7%;
Totally dependent in bowel and bladder continence = 35.4%;
Totally dependent, due to conditions or impairments, in all 10 ADLs = 12.5%.
Information on which elements of the PEDS HC were used to populate each of the 5 major categories in the PCAM were defined (Extensive Challenges, Special Challenges, Complex Challenges, Cognitive Challenges, and Functional Challenges) appears in Table 1. That table also displays information on the supplemental variables used to define groups within each category.
As Table 1 indicates, 8% of study participants were included in the Extensive Challenges category, 33% were included in Special Challenges, almost 28% were included in Complex Challenges, just over 12% were included in Cognitive Challenges, and just over 19% were included in the Functional Challenges category.
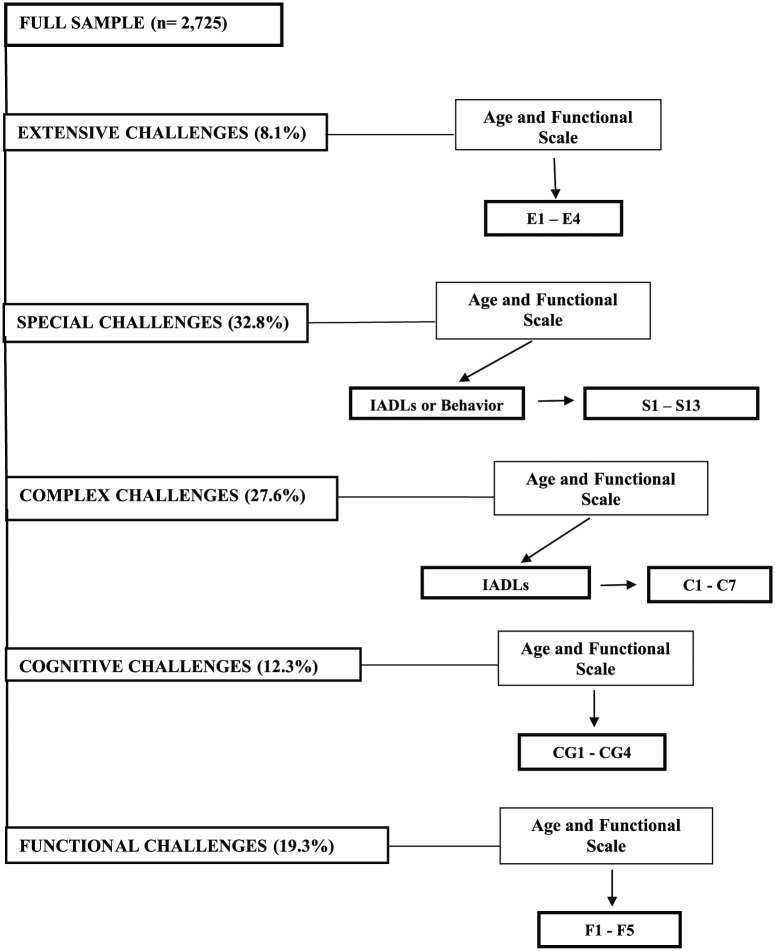
Figure 1 presents a visual summary of the PCAM in a somewhat abbreviated format. As that figure indicates, the groups within each category were first disaggregated based on a combination of the child’s age and functional status. For the Extensive Challenges, Cognitive Challenges, and Functional Challenges categories, no additional information was used to create groups within those categories. However, some of the initial (age and functional) groups in the Special Challenges category were further divided, based on the IADL status or behaviors exhibited by members of that group. In the Complex Challenges category, after forming groups based on age and functional status, only IADL status was used to further divide from some groups.
Figure 1.
Pediatric Personal Care Allocation Model (PCAM).
Table 2 presents the specifics of which characteristics of a child or youth placed them in 1 of the 33 groups. For example, members of group E4 contain children or youth under the age of 16 who score in the highest level (5) of the ADL scale, and it also contains children or youth 16 or older who score a 4 or 5 on the ADL scale. Children or youth more than 8 years of age who score roughly in the middle of the ADL scale (2, 3) and have at least 1 IADL in which they are totally dependent comprise group S7.
Table 2.
Defining 33 Pediatric Personal Care Allocation Model groupsa.
| Category | Group | Age | Functional scale | IADLs | Behavior |
|---|---|---|---|---|---|
| Extensive Challenges | |||||
| E1 | 1, 2, 3 | 0, 1 | — | — | |
| E2 | 1, 2, 3 | 2, 3 | — | — | |
| E3 | 1, 2 | 4 | — | — | |
| E4 | 1, 2 | 5 | — | — | |
| 3 | 4, 5 | — | — | ||
| Special Challenges | |||||
| S1 | 1 | 0, 1, 2 | 0 | — | |
| S2 | 1 | 0, 1, 2 | 1 | — | |
| S3 | 1 | 3, 4 | — | — | |
| S4 | 2, 3 | 0, 1 | 0 | — | |
| S5 | 2, 3 | 0, 1 | 1 | — | |
| S6 | 2, 3 | 2, 3 | 0 | 0 | |
| S7 | 2, 3 | 2, 3 | 1 | 0 | |
| S8 | 2, 3 | 2, 3 | — | 1 | |
| S9 | 2, 3 | 4 | — | 0 | |
| S10 | 2, 3 | 4 | — | 1 | |
| S11 | 1 | 5 | — | — | |
| S12 | 2, 3 | 5 | — | 0 | |
| S13 | 2, 3 | 5 | — | 1 | |
| Complex Challenges | |||||
| C1 | 1 | 0 | 0 | — | |
| C2 | 2 | 0 | 1 | — | |
| C3 | 1, 2 | 1 | 0 | — | |
| 3 | 0 | 0 | — | ||
| C4 | 1, 2 | 1 | 1 | — | |
| 3 | 0 | 1 | — | ||
| C5 | 1, 2 | 2, 3, 4, 5 | 0 | — | |
| 3 | 0, 1, 2 | 0 | — | ||
| C6 | 1, 2 | 2, 3, 4, 5 | 1 | — | |
| 3 | 0, 1, 2 | 1 | — | ||
| C7 | 3 | 3, 4, 5 | — | — | |
| Cognitive Challenges | |||||
| Cg1 | 1, 2 | 0 | — | — | |
| Cg2 | 1 | 1, 2, 3 | — | — | |
| 2 | 1 | — | — | ||
| Cg3 | 2 | 2, 3 | — | — | |
| 3 | 0, 1 | — | — | ||
| Cg4 | 1, 2 | 4, 5 | — | — | |
| 3 | 2, 3, 4, 5 | — | — | ||
| Functional Challenges | |||||
| F1 | 1 | 0 | — | — | |
| F2 | 1 | 1 | — | — | |
| 2 | 0, 1 | — | — | ||
| F3 | 1 | 2, 3, 4, 5 | — | — | |
| 2 | 2 | — | — | ||
| 3 | 0 | — | — | ||
| F4 | 2 | 3, 4, 5 | — | — | |
| 3 | 1 | — | — | ||
| F5 | 3 | 2, 3, 4, 5 | — | — | |
The functional scale ranges from 0 to 5; the age groups range from 1 to 3; the IADL and behavior indicators are binary, 0 or 1. The definition for each category in these variables appears in Table 1.
More detailed information on the 33 groups in the PCAM is presented in Table 3. The average CMIs among the 5 major categories are, as hoped, monotonic.
Table 3.
Thirty-three Pediatric Personal Care Allocation Model groups, case-mix indices, coefficients of variation, and group size.
| Category | Group | Mean, h | CMI | CV | N |
|---|---|---|---|---|---|
| Complete Sample | 25.55 | 1.89 | 0.59 | 2725 | |
| Extensive Challenges | 35.56 | 2.63 | 0.60 | 220 | |
| E1 | 25.58 | 1.89 | 0.46 | 38 | |
| E2 | 28.61 | 2.12 | 0.49 | 50 | |
| E3 | 32.06 | 2.37 | 0.65 | 41 | |
| E4 | 45.11 | 3.34 | 0.54 | 91 | |
| Special Challenges | 28.88 | 2.14 | 0.55 | 894 | |
| S1 | 18.95 | 1.40 | 0.54 | 61 | |
| S2 | 22.55 | 1.67 | 0.36 | 55 | |
| S3 | 26.33 | 1.95 | 0.44 | 129 | |
| S4 | 18.40 | 1.36 | 0.49 | 90 | |
| S5 | 24.78 | 1.84 | 0.43 | 117 | |
| S6 | 23.87 | 1.77 | 0.41 | 41 | |
| S7 | 31.20 | 2.31 | 0.43 | 75 | |
| S8 | 33.30 | 2.47 | 0.43 | 42 | |
| S9 | 28.34 | 2.84 | 0.50 | 135 | |
| S10 | 39.19 | 2.90 | 0.47 | 45 | |
| S11 | 26.69 | 1.98 | 0.45 | 22 | |
| S12 | 37.62 | 2.79 | 0.53 | 54 | |
| S13 | 42.61 | 3.16 | 0.61 | 28 | |
| Complex Challenges | 24.58 | 1.82 | 0.54 | 751 | |
| C1 | 18.30 | 1.36 | 0.50 | 163 | |
| C2 | 21.31 | 1.58 | 0.47 | 84 | |
| C3 | 19.37 | 1.43 | 0.58 | 58 | |
| C4 | 22.52 | 1.67 | 0.48 | 155 | |
| C5 | 26.19 | 1.94 | .048 | 69 | |
| C6 | 30.46 | 2.26 | 0.46 | 166 | |
| C7 | 39.41 | 2.92 | 0.43 | 56 | |
| Cognitive Challenges | 23.46 | 1.74 | 0.47 | 335 | |
| Cg1 | 17.97 | 1.33 | 0.48 | 99 | |
| Cg2 | 21.43 | 1.59 | 0.48 | 90 | |
| Cg3 | 26.47 | 1.96 | 0.39 | 80 | |
| Cg4 | 30.84 | 2.28 | 0.37 | 66 | |
| Functional Challenges | 18.43 | 1.37 | 0.53 | 525 | |
| 13.50 | 1.00 | 0.43 | 104 | ||
| 16.61 | 1.23 | 0.47 | 227 | ||
| 19.68 | 1.46 | 0.45 | 84 | ||
| 24.36 | 1.80 | 0.43 | 79 | ||
| 29.83 | 2.21 | 0.53 | 31 | ||
Abbreviations: CMI, case-mix index; CV, coefficient of variation.
Extensive Challenges = 2.63; Special Challenges = 2.14; Complex Challenges = 1.82; Cognitive Challenges = 1.74; and Functional Challenges = 0.49.
The highest CMI (2.34) applies to those 91 children or youth in Group E4 to whom an average of more than 45 hours of PCS was allocated. The lowest CMI applies to some of those who did not meet the definitions of Extensive Challenges, Special Challenges, Complex Challenges, or Cognitive Challenges. Group F1 had the lowest average number of hours (13.5) and was given, by definition, a CMI of 1.00.
As indicated, one also hopes that the CV for each group is lower than the CV for the entire sample. The CV for this sample was 0.59. Only 2 groups of the 33 groups (E3, CV = 0.65 and S13, CV = 0.61) exhibited a CV greater than 0.59. The lowest CV was observed for group S2 (.33). The number of children in each group varied considerably. The range in group size went from a minimum of 22 (S11) to a maximum of 163 children or youth (C1).
The usefulness of the PCAM can be at least partially ascertained by reviewing the degree to which the model’s 33 groups explain variance in home care expenditures for the children and youth in the sample. Table 4 presents the data from ordinary least squares (OLS) models using the 33 groups as independent variables. These groups explained 27% of the variance in PCS hours allocated.
Table 4.
Predicting personal care hours allocated using the 33 group pediatric PCAM.
| Dependent variable | Model | Adjusted R2 | |
|---|---|---|---|
| The Model’s Overall Explanatory Power | |||
| Annual Medicaid home care personal care hours | OLS: 33 PCAM groups | 0.27 | |
| Logged Medicaid home care personal care hours | OLS: 33 PCAM groups | 0.27 | |
| Explanatory Power of the Model with Sub-populations | |||
| Medical conditions only | OLS: 33 PCAM groups | 0.23 | 641 |
| Psychological or developmental health conditions only | OLS: 33 PCAM groups | 0.28 | 654 |
| Both medical and psychological or developmental conditions | OLS: 33 PCAM groups | 0.27 | 1414 |
| Intellectual or developmental disability | OLS: 33 PCAM groups | 0.24 | 1384 |
| How Well the Model Categories Predicts Upper and Lower Decile and Quartile Membership | |||
| Top 25% of home care personal care hours | Logistic regression: extensive special, complex, or cognitive challenges, ADL scale, IADL indicator, Behavior indicator | c = 0.76 Pseudo-R2 = 0.14 |
|
| Bottom 25% of home care personal care hours | Logistic regression: extensive special, complex, or cognitive challenges, ADL scale, IADL indicator, Behavior indicator | c = 0.71 Pseudo-R2 = 0.09 |
|
| The Robustness or External Validity of the Model | |||
| Annual Medicaid home care personal care hours (ten 50% random samples) | OLS: 33 PCAM groups | Mean adjusted R2 = 0.28 Range = 0.26-0.32 |
|
Abbreviations: ADL, activity of daily living; IADL, instrumental activity of daily living; OLS, ordinary least squares; PCAM, Pediatric Personal Care Allocation Model.
Table 4 also provides additional information about the PCAM model. It indicates that the explained variance using logged PCS hours does not differ from that found in the nonlogged data. This implies that the results were not a function of the effects of outliers. That table also indicates how well the PCAM did when tested with specific subpopulations among the C/Y receiving PCS. For those children with behavioral health challenges alone or those with a combination of medical and behavioral health issues, the model explained 27% and 28% of the variance in hours, respectively. The explained variance was slightly lower for those with medical challenges only (0.23) and for those with a diagnosis of an intellectual or developmental disability (0.24).
The logistic regression models estimated to determine whether the PCAM correctly places children or youth in the lowest quartile of allocated hours or the highest quartile of allocated hours resulted in C-statistics of more than 0.70, generally considering the minimum level of predictive power.15
Another test of the model is whether other impairments or conditions may be “missed” by the model. This possibility is tested by building a model with all 33 categories and then adding a variety of indicators to the model and looking at any change in explained variance. The results of these analyses indicate that when sex, the full age variable (4-20), or the presence of a diagnosis of an intellectual or developmental challenge is added to the model, the explained variance increased by less than 1%.
When one adds the full ADL scale (0-50) to the model, the explained variance increases by only 2%. Even when one adds each separate office that provides assessors to the sample into the model as dummy variables, even though this is a potentially potent source of inequity in allocation of hours, the explained variance increased by only 4%.
Such differences may seem relatively significant, until one looks at the actual effect on these factors on the accuracy of the models’ estimates of hours for the average child. The average error of the estimate (square root of the mean square error) for the basic model with the 33 groups was 3.58 hours; the average error of the estimate for the groups plus the extended ADL scale was 3.55 hours; the average error of the estimate for the groups plus office identifiers model was 3.54 hours.
As always, one must be concerned about the potential robustness of the model. This was done using the 33 PCAM groups to explain variance in hours in ten 50% random samples of the data used to develop the model. The average explained variance in the 10 models ranged from 26% to 32%, with a mean across the 10 trials of 28%.
Discussion
The half-century-old EPSDT program remains the most comprehensive health coverage available to children in lower income families in the United States. Much of EPSDT is focused on screening, but it is also the source of support and care for the tens of thousands of American children in lower income families who face serious health challenges. An important part of that package of services is the PCS program.
This research focused on the hours of PCS allocated to children with a wide variety of challenges. To help assure greater consistency and equity in the program, a case-mix model was developed that explained 27% of the variance in PCS hours allocated to children. The results indicate the model applied almost equally well to children facing different types of challenges. The results were also stable when retested with a series of 50% samples. They also indicated that there were no obvious or glaring errors in the construction of the groups; factors not included in the model were of relatively slight importance.
To compare the PCAM with other case-mix models, one must review the research on home care case-mix models that attempted to explain home care expenditures because of the lack of studies focusing on PCS for children. In a Michigan sample of older persons, the RUGIII/HC model explained 34% of the variance in total (formal and informal) home care expenditures.9 Using home care data from Canada, the RUGIII/HC model explained 21% of the variance in formal per diem home care costs.23 The Pediatric Expenditure Classification Model (PECM) explained 47% of the variance in total home care expenditures for the sample of children and youth used in this research.19
A variety of reasons may account for why the explained variance for the PCAM is somewhat lower than the level one sees in other home care models. However, one part of that difference may derive from the differential levels of variance one sees in expenditures, the focus of RUGIII/HC and the PECM versus PCS hours. For example, the CV for CMIs in the PECM sample was 1.49. In contrast, the CV for PCS hours is approximately 60% lower than that in the expenditure data used to develop the PECM. Where one observes less variance, one can expect OLS models to exhibit lower levels of explained variance.
Like other research, this effort has its obvious limitations. It focused on children in one program in one state. The modeling involved some decisions that called for the researcher’s judgment. Future research will allow one to pass judgment on the robustness of these results and those judgments.
Although an expensive part of Medicaid services, PCS for C/Y deal with only a small proportion of those C/Y who receive Medicaid services. In 2010 in Texas, EPSDT program recipients who received at least PCS constituted only 0.31% of the children or youth covered by Medicaid. For every 31 C/Y receiving EPSDT PCS services at home, another 9970 children in the Medicaid program who lived in those same communities had no need for long-term supports and services.
It must also always be remembered that a case-mix model is but the first step in implementing case-mix–based prospective payment. Implementation usually requires a phasing-in of the payment system in which payment for a specific group or CMI is surrounded by what is called a “corridor” (eg, ±1.5 hours).
This makes each group’s CMI the basis for a “presumptive” payment, but that payment can be allowed to move either up or down within the established corridors without any special justification. Even payment outside those corridors can be permitted with the submission of a justification provided by program staff.
Even in a more mature case-mix system, the presumptive number of hours should remain as a basic starting point. In many instances, it may be perfectly appropriate. Home care, however, creates a wide range of relatively idiosyncratic situations. So, the movement of payment within corridors in a specific instance, or even beyond them, may be required by some special circumstance in the home. For example, the family may have multiple children or youths who participate in the program, or the primary caregiver may have physical or behavioral health challenges of their own.
Finally, as noted earlier, case-mix modeling of care provision does not necessarily identify the optimal amount of care for each sample member. Case-mix is about distributing whatever care resources are being provided, not about identifying the correct amount of care needed by the recipient. Questions about the proper amount of care can only be answered by outcome studies.
Conclusions
Medicaid PCS are an important part of the array of services now provided to children living in the community with special health care needs. That PCS resources be allocated equitably constitutes an important policy issue. A case-mix model, such as the PCAM with a set of presumptive hours of PCS for members of this vulnerable population, might serve as a foundation on which a more equitable allocation process for PCS could be built.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: CDP is the sole contributor to all aspects of the paper.
References
- 1. Weissert W, Weissert C. Governing Health. 4th ed. Baltimore, MD: Johns Hopkins University Press; 2012. [Google Scholar]
- 2. https://www.medicaid.gov/medicaid/benefits/epsdt/index.html. FY 2015 Data Accessed September 12, 2016.
- 3. Centers for Medicare Medicaid Services. EPSDT: A Guide for States. Baltimore, MD: Centers for Medicare and Medicaid Services; 2014. [Google Scholar]
- 4.https://www.dshs.texas.gov/caseman/pcs.shtm. Accessed September 2, 2016.
- 5. Elliott TR, Phillips CD, Patnaik A, et al. Medicaid Personal Care Services and caregivers’ reports of children’s health: the dynamics of a relationship. Health Serv Res. 2011;46:1803–1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Phillips CD. Case-mix adjustment. In: Mullner R, ed. Encyclopedia of Health Services Research (Vol. 1). Thousand Oaks, CA: SAGE; 2009:129–132. [Google Scholar]
- 7. Fetter RB, Brand DA, Gamache D, eds. DRGs: Their Design and Development. Ann Arbor, MI: Health Administration Press; 1991. [Google Scholar]
- 8. Fries BE, Schneider DP, Foley WJ, Gavazzi M, Burke R, Cornelius E. Refining a case-mix measure for nursing homes: Resource Utilization Groups (RUG-III). Med Care. 1994;32:668–685. [DOI] [PubMed] [Google Scholar]
- 9. Bjorkgren M, Fries BE, Shugarman L. A RUG-III case-mix system for home care. Can J Aging. 2000;19:106–125. [Google Scholar]
- 10. Phillips CD, Hawes C, Morris JN, et al. interRAI Pediatric Home Care (PEDS-HC) Assessment Form and User’s Manual, Version 9.2. Washington, DC: interRAI; 2014. [Google Scholar]
- 11. Phillips CD, Hawes C. The interRAI Pediatric Home Care (PEDS HC) assessment: evaluating the long-term community-based services and supports for children facing special healthcare challenges. Health Serv Insights. 2015;8:17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fournier CJ, Davis MJ, Patnaik A, et al. Modeling caregivers’ perceptions of children’s need for formal care: physical function, intellectual disability, and behavior. Disabil Health J. 2010;3:213–221. [DOI] [PubMed] [Google Scholar]
- 13. Phillips CD, Patnaik A, Dyer JA, et al. Reliability and the measurement of activity limitations (ADLs) for children with special health care needs (CSHCN) living in the community. Disabil Rehabil. 2011;33:2013–2022. [DOI] [PubMed] [Google Scholar]
- 14. Patnaik A, Elliott TR, Moudouni DM, et al. Severity of children’s intellectual disabilities and Medicaid Personal Care Services. Rehabil Psychol. 2011;4:383–390. [DOI] [PubMed] [Google Scholar]
- 15. Phillips CD, Patnaik A, Moudouni DK, et al. Summarizing activity limitations in children with chronic illnesses living in the community: a measurement study using supplemented interRAI items. BMC Health Serv Res. 2012;12:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Miller TR, Elliott TR, McMaughan DM, et al. Personal care services provided to children with special health care needs (CSHCN) and their subsequent physician services. Disabil Health J. 2013;6:317–324. [DOI] [PubMed] [Google Scholar]
- 17. Adepoju L, Zhang Y, Phillips CD. Modeling the determinants of Medicaid home care payments for children with special health care needs: a structural equation model approach. Disabil Health J. 2014;7:426–432. [DOI] [PubMed] [Google Scholar]
- 18. Elliott TR, Patnaik A, Naiser E, et al. Medicaid Personal Care Services for children with intellectual disabilities: what assistance is provided? when is assistance provided. Intellect Dev Disabil. 2014;51:24–31. [DOI] [PubMed] [Google Scholar]
- 19. Phillips CD. The Pediatric Home Care Expenditure Classification model (P/ECM): a home care case-mix model for children facing special health care challenges. Health Serv Insights. 2015;8:35–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. STATA 14.2. College Station, TX: The Stata Corporation. [Google Scholar]
- 21. Addinsoft. XLSTAT; 1903. www.xlstat.com.
- 22. Kass GV. An exploratory technique for investigating large quantities of categorical data. J Roy Stat Soc C. 1980;29:119–127. [Google Scholar]
- 23. Poss JW, Hirdes JP, Fries BE, McKillop I, Chase M. Validation of Resource Utilization Groups, Version III for home care (RUG-III/HC): evidence from a Canadian home care jurisdiction. Med Care. 2008;46:380–387. [DOI] [PubMed] [Google Scholar]