Abstract
Background:
Non-medical prescription opioid (NMPO) use is a problem among young adults, yet young NMPO users are a diverse population that has been challenging to engage in overdose prevention and harm reduction programs.
Objectives:
This study compared the effectiveness and characteristics of persons recruited through two different sampling strategies to inform research and intervention efforts with young adult NMPO users.
Methods:
We analyzed data from the Rhode Island Young Adult Prescription Drug Study (RAPiDS), which enrolled persons aged 18 to 29 who reported past 30 day NMPO use. We compared the characteristics of two samples recruited simultaneously between February 2015 and February 2016. One sample was recruited using field-based strategies (e.g., respondent-driven sampling, transit ads), and a second from internet sources (e.g., online classifieds).
Results:
Among 198 eligible participants, the median age was 25 (IQR: 22, 27), 130 (65.7%) were male, 123 (63.1%) were white, and 150 (78.1%) resided in urban areas. A total of 79 (39.9%) were recruited using field-based strategies and 119 (60.1%) were recruited from internet sources. Internet-recruited persons were younger (median = 24 [IQR: 21, 27] vs. 26 [IQR: 23, 28] years) and likely to reside in rural areas (16.2% vs. 5.3%), although this finding was marginally significant. Field-recruited participants were more likely to have been homeless (36.7% vs. 17.7%), have been incarcerated (39.7% vs. 21.8%), and engage in daily NMPO use (34.6% vs. 14.5%).
Conclusions:
Multi-pronged outreach methods are needed to engage the spectrum of young adult NMPO users in prevention and harm reduction efforts.
Keywords: youth, young adults, prescription opioids, opioid-related disorders, sampling
Introduction
Non-medical prescription opioid (NMPO) use — defined as use without a prescription, intentional use as not directed by a physician, or use of one’s own prescription outside of prescribed parameters — is a continuing public health problem in the United States (National Institutes on Drug Abuse, 2011). Concomitant with a dramatic rise in the prescribing and sale of opioid pain relievers, the rate of NMPO-attributable fatal overdose quadrupled between 1999 and 2011 (Chen, Hedegaard, & Warner, 2014). In more recent years, the rate of opioid-attributable drug overdose death has continued to climb, increasing by 15.6% between 2014 and 2015 alone (Rudd, Seth, David, & Scholl, 2016). Substantial increases in the prevalence of NMPO abuse and dependence disorders have also been observed (McCabe, Cranford, & West, 2008), and the number of opioid-related emergency department visits increased from 89.1 per 100,000 in 2005 to 177.7 per 100,000 in 2014 (Weiss et al., 2016).
Young adults who use prescription opioids non-medically are at high risk of progression to opioid dependence (McCabe, West, Morales, Cranford, & Boyd, 2007), as well as transitions to heroin use and/or injection drug use (Carlson, Nahhas, Martins, & Daniulaityte, 2016; Cerdá, Santaella, Marshall, Kim, & Martins, 2015; Lankenau et al., 2012). One recent analysis of nationally representative US data found that the rate of past-year heroin use (37.5 per 1,000 population) was highest among 18 to 25 year olds who also reported past-year NMPO use (C. M. Jones, 2013). Evidence suggests that NMPO use is often part of polydrug use practices that involve alcohol, illicit drugs (e.g., cocaine), or other prescription drugs (e.g., benzodiazepines) (Daniulaityte, Falck, Wang, & Carlson, 2009; Sung, Richter, Vaughan, Johnson, & Thom, 2005), which further increases the risk of overdose, psychiatric comorbidity, and other adverse health outcomes (J. D. Jones, Mogali, & Comer, 2012).
Young adults who use prescription opioids non-medically represent a diverse, fragmented, and large population (Martins et al., 2015), which has proved difficult to engage in research and interventions (Daniulaityte, Falck, Li, Nahhas, & Carlson, 2012). For example, many young NMPO users, particularly infrequent users, obtain opioids primarily from friends and relatives and are thus outside of street-based networks traditionally reached by harm reduction and overdose prevention services (Frank et al., 2015; C. M. Jones, Paulozzi, & Mack, 2014). Ethno-epidemiological studies have confirmed that people who inject prescription opioids are not easily reached by existing interventions for people who inject illicit drugs, due to the distinct social and environmental context of NMPO use (Lankenau et al., 2012; Roy, Arruda, & Bourgois, 2011). Our prior work has identified different contexts of young adult NMPO use, such as polysubstance use in social contexts, or wide availability of prescription opioids for use in private contexts (e.g., alone in a home), including diversion of medications from friends and family members (Yedinak et al., 2016). Therefore, different recruitment methods may help to reach and identify a broader spectrum of young adults who use prescription opioids non-medically in these different contexts. For example, the recent HIV outbreak in Scott County, Indiana demonstrated significant transmission risk among a young, rural, predominately white population who inject prescription opioids, and who have broad access to opioid medications but extremely limited availability of opioid use disorder treatment and harm reduction programs (Strathdee & Beyrer, 2015). Thus, additional research is needed to determine more effective methods to identify and reach young adults who use prescription opioids non-medically. Such research may inform future efforts to engage young adult NMPO users in interventions to prevent transitions to injecting and to mitigate overdose risk.
Respondent-driven sampling (RDS) has been used successfully to reach hidden populations, including young people who inject drugs (Heckathorn, Semaan, Broadhead, & Hughes, 2002; Magnani, Sabin, Saidel, & Heckathorn, 2005). The method relies on drug users’ social networks to refer and recruit participants, and uses a post-stratification weighting procedure to account for the over-sampling of individuals from larger networks (Abdul-Quader et al., 2006). However, the method assumes the existence of a single underlying social network component, or the existence of “key” sub-network members that form ties across components (Johnston & Sabin, 2010). Given that many young adult NMPO users obtain prescription opioids from physicians or family members and are thus isolated from larger drug-using networks (McCabe, Cranford, Boyd, & Teter, 2007), traditional RDS (i.e., chain-based referral from a small number of “seeds”) may be ineffective. Only one study to date has used RDS to recruit young NMPO users (Daniulaityte et al., 2012). Recruitment was found to be less efficient than expected and the sample failed to achieve representativeness due to a lack of social connectedness in the target population, a high degree of homophily (i.e., the tendency for contact between people who share characteristics, such as age or race), and large differences in network sizes (Daniulaityte et al., 2012).
Internet-based sampling has been shown to be an effective method to access hidden populations of substance users (Miller & Sonderlund, 2010). Previous studies have shown that web-based methods (e.g., posting on drug user websites and forums) are an efficient, cost-effective way to recruit drug users (Duncan, White, & Nicholson, 2003; Miller, Johnston, McElwee, & Noble, 2007). Few studies have examined the use of drug user forums and other online venues to survey NMPO users, and the majority has focused on adult populations (Chiauzzi, Dasmahapatra, Lobo, & Barratt, 2013; Katz, Fernandez, Chang, Benoit, & Butler, 2008). Examples of internet sampling strategies of young adults who use drugs are limited, and are often specific to drugs such as tobacco, marijuana, and alcohol (Bauermeister et al., 2012; Gubner, Delucchi, & Ramo, 2016; Ramo & Prochaska, 2012), or are limited to cohorts of college students (Lord, Brevard, & Budman, 2011). One study that compared three different online strategies to recruit cannabis users found that multi-pronged recruitment campaigns with messages tailored to the population of interest are most effective (Temple & Brown, 2011). However, although the relativeness effectiveness of different online recruitment strategies (e.g., advertisements on mobile platforms, advertisements on traditional websites, social media) have been examined among populations including methamphetamine-using men who have sex with men (Wilkerson, Shenk, Grey, Rosser, & Noor, 2015), few studies have identified effective strategies to reach young adults who use prescription opioids non-medically. Furthermore, despite the fact that three-quarters of young adults in the US access social media websites (Ramo & Prochaska, 2012), very few studies have examined the use of social media venues (e.g., Facebook) to recruit young adult NMPO users. Finally, it remains unclear whether NMPO users recruited from the internet differ with respect to sociodemographic characteristics, drug use, and overdose risk profiles as compared to samples recruited using field-based and/or RDS methods.
In light of the abovementioned research priorities, a study of young adults who engage in NMPO use was initiated in Rhode Island. The state of Rhode Island was an ideal setting in which to conduct this study because it is among the states with the highest prevalence of NMPO use among young adults (Substance Abuse and Mental Health Services Administration (SAMSHA), 2013). Furthermore, Rhode Island is a small yet racially and ethnically diverse state with a combination of urban, suburban, and rural areas, permitting the characterization of NMPO use in multiple communities and subgroups.
Known as the Rhode Island Young Adult Prescription Drug Study (RAPiDS), this study aimed to evaluate and compare the effectiveness of two novel sampling methods (one field-based, one internet-based) to recruit young adult NMPO users. Given the high levels of internet literacy and social media use in young adult populations, we hypothesized that internet-based recruitment would be the more efficient and cost-effective method for recruiting young adult NMPO users. We also hypothesized that field-based recruitment would result in a sample with a higher prevalence of injecting history and overdose risk behaviors.
Materials and Methods
Formative Research
In the first phase of the study we conducted formative research, which included focus groups and one-on-one qualitative interviews with young adults who use prescription opioids non-medically. The objectives of the formative research were three-fold. First, we sought to gain preliminary knowledge about non-medical prescription drug use trends and patterns among young adults in Rhode Island as well as issues of public health interest (e.g., overdose). This information informed the development of the survey instrument and selection of the standardized screeners used as part of the instrument (e.g. AUDIT-C, CESD-10). Focus group members were also asked to comment on concerns regarding informed consent, confidentiality, and other factors that could influence participation in the research (e.g., location of the research site, most appropriate hours to conduct interviews). Second, focus group members and interviewed participants were asked to describe physical and online venues in which young adult NMPO users are known to congregate. Feedback from the focus groups was used to develop online ads that were youth-friendly, engaging, and thus more likely to recruit participants. Students and staff working for the research project created the final advertisements. Finally, the formative research was used to build rapport with the study population and identify RDS “seeds”. Young adults participating in the focus groups were asked if they were interested in acting as or referring potentially eligible “seeds” for the RDS phase of the study.
Formative research consisted of 13 individual interviews with members of the target population and 2 focus groups (n=14 total) with service providers who were familiar with NMPO use among young adults in Rhode Island. Participants who participated in the individual interviews were young adults who all reported NMPO use within the past six months. These youth were recruited using online classifieds, posters, and word-of-mouth. Service providers were recruited from organizations representing harm reduction programs, HIV prevention organizations, drug treatment centers, emergency medical services personnel, and youth advocacy organizations. All participants involved in the RAPiDS study, including those in the formative research, provided informed consent. All phases of the study were approved by the University Institutional Review Board. Detailed results of the formative research have been presented elsewhere (Yedinak et al., 2016).
Eligibility criteria, screening, and interviewing procedures
For subsequent phases of the study, eligibility criteria included: (1) currently residing in Rhode Island; (2) aged 18 to 29 years old; (3) speak and feel comfortable completing a survey in English; (4) report non-medical use of at least one prescription opioid painkiller in the past 30 days; and (5) able to provide informed consent. Non-medical use of at least one prescription opioid painkiller was defined as use without a prescription, or not as a doctor directed such as taking the drug at a different dose, frequency, or route than was prescribed. A trained research assistant screened all interested individuals over the phone. During the screening process, unique identifiers such as date of birth were recorded in a screening database to confirm the age criteria, and to verify first time enrollment in the study. If eligible, participants were then scheduled to complete an interviewer-administered survey in a public location of their choosing, or at the centrally located primary research site. Participants were asked to show a government issued photo ID to verify their name and date of birth prior to initiating the survey.
All interviews were conducted by professionally trained and supervised interviewers. We used computer-assisted personal interviewing (CAPI) to conduct participant interviews, which also included a computer-assisted self-interviewing (CASI) component for the collection of sensitive or potentially stigmatizing information (e.g., injection drug use). Surveys were conducted on laptop computers using DatStat Discovery™ data management architecture and Illume™ software, which allowed for direct and remote secure data entry. Interviews lasted approximately 60 minutes, including the review of study objectives and consenting procedures. Participants who completed the interview received $25 USD for their time.
Respondent-driven sampling and field-based recruitment
The respondent driven sampling (RDS) phase of the study was initiated in February 2015 through June 2015. To overcome previously observed challenges using RDS to recruit young adult NMPO users (Daniulaityte et al., 2012), we employed a combination of traditional field-based and RDS sampling procedures. All participants recruited during the RDS phase of the study were categorized as recruitment “seeds,” unless they were part of an RDS chain they were marked as “referred”. RDS “seeds” had to meet the same eligibility criteria as all other participants. To increase the diversity of RDS seeds, street outreach, public transit advertisements, and strategically placed study flyers were placed in locations around Rhode Island where young adults NMPO users may see them. Locations were selected based on feedback collected during the formative research.
After consent and administration of the survey, all seeds were asked to refer other young adults in their social networks with whom they had recently used prescription opioid non-medically. In lieu of paper coupons, seeds were provided with a code word that could be sent over text or e-mail to the seeds’ referrals. RDS seeds were instructed on the following eligibility requirements: (1) currently residing in Rhode Island; (2) aged 18 to 29 years old; and (3) report non-medical use of at least one prescription opioid painkiller. Full eligibility criteria details were not revealed to the seeds in order to avoid having ineligible people gain entry into the study, specifically the requirement of NMPO use in the past 30 days. Similar to other studies that have used RDS, we provided respondents who assisted with recruitment a small compensation for their referral efforts. Specifically, “seeds” were offered a $5 gift card for each eligible enrolled participant referral. Consistent with RDS methodology and to avoid biasing the sample with acquaintances of “super recruiters” (Salganik & Heckathorn, 2004), we capped enrollment at three eligible participants from each seed.
All screened individuals were asked how they heard about the project, and whether they received a code word from a friend, family member, or acquaintance. The code words were used to track recruitment chains. Interviewers were trained to identify situations in which the seed may be exerting exploitative influence over their referrals to enroll in the study.
Social network data were collected from all participants to assess the effectiveness of RDS and to conduct RDS analyses. Specifically, participants were asked to report how many people they knew who used prescription painkillers non-medically, and of these, how many were young adults, how many resided in Rhode Island, and finally, how many they had seen in the past week. Although these data were analyzed, an RDS sample analysis was not conducted due to the small number of successful referrals generated from the large number of seeds. Given the relative ineffectiveness of the RDS method, we terminated this recruitment approach in June of 2015, and RDS seeds were instead re-classified based on how they originally heard about the study for statistical analyses. After a two-week washout period, we began internet recruitment in August of 2015, and resumed field-based methods of recruitment (i.e., advertisements, flyers, word-of-mouth) in September of 2015 alongside the internet-based recruitment.
Internet-based recruitment
In addition to the methods described above, participants were also recruited using a multitude of internet-based strategies. Specifically, banner ads were purchased for sites and cellular phone apps that the study population was known to use (i.e., Google AdWords™, Facebook), based on information solicited during the formative research phase. Banner ads were purchased with a set daily budget and were limited to simple headlines (10 words or less) about the study that, if clicked, linked people to a social media account or website that included all relevant contact information for the study (Figure 1). Social media accounts (i.e., Snapchat, Tumblr, Bluelight.org, Erowid.org, Reddit, Facebook, Twitter), were created for additional online visibility. Activity on these accounts included daily announcements of study interview opportunities, postings to online forums and feeds, creating calendar events, and posting relevant online content such as educational materials and general information of interest to the study population. Finally, ads were placed on online classified websites (i.e., regional craigslist.org sites) several times each week, and included basic information about study interview opportunities and contact information. All individuals were screened and interviewed according to the procedures described above.
Figure 1:
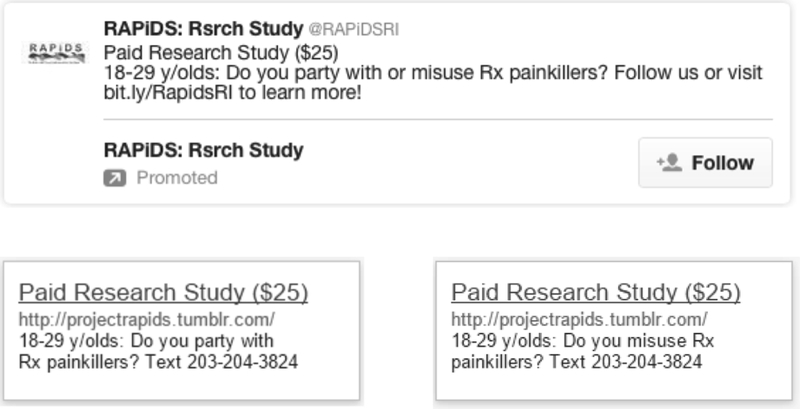
Sample banner advertisements
Measures
The primary outcome for this analysis was the method through which participants were successfully recruited. Specifically, during the screening procedure, all participants were asked to report how they first heard about the study. We categorized participants as having been recruited from either internet-based or field-based methods. Participants recruited during the RDS phase of the study but who first heard about the project through online sources were considered as internet-based recruits for all analyses. Participants recruited by an RDS seed were nested within the field-based sample for the subsequent analyses.
The RAPiDS survey instrument included measures related to sociodemographic characteristics, drug use behaviors, overdose experiences, health care utilization including addiction treatment services, and other covariates of interest. Sociodemographic characteristics assessed included: age (based on date of birth), sex at birth, race and ethnicity, sexual orientation, history of incarceration, and whether the participant had been homeless in the past six months. We also collected information on the participant’s self-reported zip code and/or town of current residence, which we used in geographic analyses (see below).
To increase the veracity of self-reported NMPO use, participants were asked to identify the opioids they had used from a modified version of the Substance Abuse and Mental Health Services Administration’s (SAMHSA’s) “pill card A” (Substance Abuse and Mental Health Services Administration (SAMHSA), 2008), which shows pictures of 21 different categories of opioid-based pain relievers. During the formative research phase (focus groups) previously discussed, the SAMHSA Pill Card A was modified for the study to include newer formulations of opioid-based pain relievers based on feedback from the study population (e.g. hydrocodone, roxicodone, oxymorphone). Referring to any drugs represented on these pill cards, we asked participants whether they had ever been prescribed an opioid, whether they use an opioid non-medically at least daily, whether their non-medical use usually occurred alone, and whether they had ever sniffed or snorted an opioid. By subtracting participants’ current age from the age at which participants first reported using prescription opioids non-medically, we calculated duration of NMPO use (in years). We also ascertained lifetime use of other illicit drugs, including cocaine, methamphetamine, and heroin. During the CASI portion of the interview, participants reported whether they had ever injected as well as the number of friends they knew who injected. Finally, we assessed lifetime history of overdose, including whether they had ever witnessed an overdose and whether they had ever overdosed themselves.
Statistical Analyses
Descriptive statistics were used to describe the overall study sample and to examine the social network characteristics of the participants recruited during the RDS phase of the study. Next, we used chi-square tests and Wilcoxon rank sum tests to compare the internet- and field-recruited samples. These analyses were conducted in SAS version 9.3 (SAS Institute Inc., Cary, NC), and all p-values are two-sided. Finally, we conducted geographic analyses using Tableau Desktop 9.3.0 (Tableau Software, Seattle, WA). Specifically, we mapped individuals based on their reported current zip code or town of residence, and categorized these areas as urban, suburban, or rural based on standard US census definitions and the Rhode Island land use survey (Rhode Island Department of Administration, 2000).
The cost effectiveness of the field-based and internet-based recruitment strategies were determined by calculating the total cost for each method (i.e., RDS costs, transit advertising, online advertising, and color poster printing), divided by the number of unique participants who contacted the study and the number of successfully completed surveys per recruitment method. Banner advertising metrics are often measured by “reach” (i.e. number of unique people shown the advertisement), “impressions” (i.e. number of times the banner ad was shown) and “click through rate” (i.e. the number of times people clicked on the banner ad) (Ramo & Prochaska, 2012); however, our results were driven almost exclusively by online classifieds and therefore these metrics were not included in the analysis. The average number of contacts per method was reported, which included text, voice, and email communications with a participant or an attempt at initiating communication, i.e. where a voicemail, email, or text message was sent. Communications about interviews and study participation were not conducted through social media messaging. The cost effectiveness calculations excluded research interviewer and student volunteer effort costs (including travel), which remained equivalent to approximately 1.0 FTE across the recruitment period.
Results
A total of 340 unique participants contacted the research study for the initial eligibility screening. Of these participants, 126 (37.1%) first heard about the study from field-based sources, 178 (52.4%) from internet-based sources, and another 36 (10.6%) participants contacted the study but did not disclose where they had heard about it (Figure 2). Of the 36 participants for whom recruitment source was unknown, only 2 (5.6%) were eligible and completed the survey (and were subsequently excluded from the following analyses). Of the 304 participants who contacted the study and for whom recruitment method was known, 230 (75.7%) screened eligible. Internet-based methods were responsible for 144 eligible participants and field based methods resulted in 86 eligible participants. As shown in Figure 2, a higher proportion of field-recruited eligible participants completed the survey (91.9%), compared to the internet-based sample (82.6%). The average number of contacts required per completed survey was higher for field-based methods (5.30 contacts per completed survey) versus internet-based methods (4.03 contacts per completed survey).
Figure 2:

Participant recruitment flowchart
Of the 198 eligible participants who completed the survey, the median age was 25 (interquartile range [IQR] = 22, 27) and 130 (65.7%) reported male sex at birth. The majority (62.1%) of the sample was white, 31 (15.7%) were of Black, African, Haitian, or of Cape Verdean descent, and 41 (20.7%) reported being of mixed race, bi-racial, or multi-racial ancestry. A total of 28 (14.1%) identified as Hispanic or Latino. The majority (86.3%) reported their sexual orientation as straight, and 26 identified as lesbian, gay, bisexual, or other (e.g., queer, questioning). Although participants resided throughout the state of Rhode Island (see Figure 3), approximately half (52.0%) reported living in the capital city of Providence, and 76% of all interviews were completed at the RAPiDS Study office in Providence.
Figure 3: Current place of residence reported by RAPiDS participants (n=193)*.

* Participants were mapped by zip code of current residence. A total of 62 participants who did not elect to provide a zip code were mapped based on reported city/town of residence. Seven participants elected not to report their zip code or city/town of residence and are not represented here.
Of the 94 persons recruited during the RDS phase of the study and for whom data on referrals were available, 77 “seeds” resulted in 15 recruitment chains, resulting in 17 total referrals. Thus, the majority of the recruitment chains consisted of only one seed and one referral. In analyzing the network data for these participants, we found that, while participants knew a median of 8 young adults who engaged in NMPO use (IQR: 3, 15), the median number they had seen in the past week was only 3 (IQR = 1, 7). For the subsequent analyses, the 77 RDS “seeds” were re-classified according to how they originally heard about the study, resulting in 21 field-based participants and 56 internet-based participants. All 17 RDS “seed” referrals were re-classified as the field-based source “word of mouth”.
A comparison of participant characteristics by recruitment method (internet- versus field-based) is shown in Table 1. Participants recruited using internet-based methods were younger and were more likely to currently reside in rural areas of the state, although this finding was marginally significant. In contrast, field-based methods results in a group who were more likely to have ever been incarcerated and were more likely to have ever experienced homelessness.
Table 1:
Factors associated with internet- versus field-based recruitment of young adults who use prescription opioids non-medically
| Characteristic | Overall n (%) n = 198 |
Internet-Based n (%) n = 119 |
Field-Based n (%) n = 79 |
p – value |
|---|---|---|---|---|
| Age (median, IQR) | 25 (22 – 27) | 24 (21 – 27) | 26 (23 – 28) | 0.002 |
| Sex at birth | 0.237 | |||
| Male | 130 (65.7) | 82 (68.9) | 48 (60.8) | |
| Female | 68 (34.3) | 37 (31.1) | 31 (39.2) | |
| Place of residence | 0.067 | |||
| Urban | 150 (78.1) | 86 (73.5) | 64 (85.3) | |
| Suburban | 19 (9.9) | 12 (10.3) | 7 (9.3) | |
| Rural | 23 (12.0) | 19 (16.2) | 4 (5.3) | |
| Race | 0.475 | |||
| White | 123 (63.1) | 71 (60.7) | 52 (66.6) | |
| Black | 31 (15.9) | 18 (15.4) | 13 (16.7) | |
| Mixed/other race | 41 (21.0) | 28 (23.9) | 13 (16.7) | |
| Ethnicity | 0.187 | |||
| Hispanic or Latino | 28 (14.1) | 20 (16.8) | 8 (10.1) | |
| Not Hispanic or Latino | 170 (85.6) | 99 (83.2) | 71 (89.9) | |
| Sexual orientation | 0.111 | |||
| Straight | 171 (86.8) | 107 (89.9) | 64 (82.1) | |
| LGBQ or other | 26 (13.2) | 12 (10.1) | 14 (17.9) | |
| Ever incarcerated | 57 (28.9) | 26 (21.8) | 31 (39.7) | 0.007 |
| Homeless† | 50 (25.3) | 21 (17.7) | 29 (36.7) | 0.003 |
| Ever prescribed an opioid | 120 (61.2) | 65 (55.1) | 55 (70.5) | 0.030 |
|
Duration of NMPO use (median, IQR in years) |
6 (3 – 9) | 5 (2 – 8) | 7 (4 – 10) | 0.002 |
| Daily NMPO use† | 44 (22.6) | 17 (14.5) | 27 (34.6) | 0.001 |
| Use NMPO alone† | 147 (75.0) | 93 (78.8) | 54 (69.2) | 0.129 |
| Number of young adult NMPO-using friends (median, IQR) | 9 (4 – 20) | 8 (4 – 15) | 9 (4 – 20) | 0.403 |
| Ever sniffed or snorted an opioid | 117 (59.7) | 62 (52.5) | 55 (70.5) | 0.012 |
| Ever used cocaine | 133 (67.2) | 70 (58.8) | 63 (79.7) | 0.002 |
| Ever used methamphetamine | 39 (19.7) | 15 (12.6) | 24 (30.4) | 0.002 |
| Ever used heroin | 85 (42.9) | 40 (33.6) | 45 (57.0) | 0.001 |
| Number of friends who inject | <0.001 | |||
| 0 | 88 (46.3) | 65 (54.6) | 23 (31.9) | |
| 1 | 26 (13.7) | 21 (17.7) | 5 (6.9) | |
| 2–5 | 50 (26.3) | 26 (21.9) | 24 (33.3) | |
| >5 | 26 (13.7) | 6 (5.0) | 20 (27.8) | |
| Ever injected | 59 (30.0) | 23 (19.3) | 36 (46.2) | <0.001 |
| Ever seen someone overdose | 102 (51.8) | 57 (47.9) | 45 (57.7) | 0.179 |
| Ever overdosed | 53 (26.8) | 29 (24.4) | 24 (30.4) | 0.350 |
Note: not all columns add to 100% due to rounding, and some percentages are over estimated due to missing values
refers to experiences/activities in the past 6 months
A trend emerged in which persons recruited using field-based methods had more extensive drug use profiles. For example, compared to internet-based recruitment, field-recruited participants were more likely to have ever been prescribed an opioid, engage in at least daily NMPO use, ever sniffed or snorted an opioid, and were more likely to report lifetime use of cocaine, methamphetamine and heroin (see Table 1). The field-recruited sample also had a longer median duration of NMPO use. Field-recruited participants were more likely to have ever injected, and had a greater number of persons in their social network who injected. However, the groups did not differ with respect to the number of NMPO-using young adults in their networks. Finally, the two groups were similar with regards to the proportion who reported ever witnessing an overdose and ever overdosing themselves.
The cost-effectiveness of each recruitment method is summarized in Table 2. Internet-based methods cost less overall and were more cost efficient ($7.24 per completed survey compared to $18.17 for the field-based method). Primary expenses for field-based recruitment methods included mileage for travel to community-based locations, color printing costs, and public transit advertising. Internet based expenses were limited to the online advertising costs.
Table 2:
Costs and cost efficiency by recruitment method
| Overall | Internet-Based | Field-Based | |
|---|---|---|---|
| Total Recruitment Costs | $2,297.45 | $861.70 | $1,435.75 |
| Per Unique Participant Screened (N = 340) | $6.76 | $4.84 | $11.39 |
| Per Completed Survey (N = 198) | $11.60 | $7.24 | $18.17 |
Of the 79 persons recruited through field-based methods, the majority (n=43, 54.4%) were referred to the study by word-of-mouth, 19 (24.1%) saw a flyer in the community, and 17 (21.5%) heard of the study from an advertisement on public transit. A limitation within internet-based recruitment was the social media advertising, which resulted in fewer successful surveys than anticipated. Despite a comprehensive online advertisement campaign on multiple websites (e.g., Facebook, Google) and drug use forums (e.g., bluelight.org, Reddit), these methods of internet-based recruitment resulted in just one completed survey.
Discussion
This is one of the first studies to compare the effectiveness and costs of internet- versus field-based recruitment methods to reach young adults who use prescription opioids non-medically. Both approaches were productive; however, the internet-based method was less costly and resulted in a younger and more geographically diverse sample. Comparing the sociodemographic and behavioral characteristics of the two samples, participants recruited using field-based methods had greater vulnerabilities (e.g., incarceration histories, homelessness), and more extensive NMPO and illicit drug use profiles. In contrast, internet-recruited participants were more likely to be experimental and/or less dependent users: they were younger, engaged in NMPO use less frequently, had shorter durations of NMPO use, and were less likely to have used an opioid by injection or insufflation. Collectively, these findings suggest that multi-faceted approaches are needed to identify, reach, and engage the diverse spectrum of young people who use prescription opioids non-medically.
This study also demonstrated that RDS was an ineffective method to recruit the target population. The small number of recruitment chains prevented an examination of homophily in our sample. However, many participants reported relatively small drug-using networks (and 75% of the sample used opioids alone), which may have limited the effectiveness of respondent-driven recruitment in this study. Nonetheless, we found that participants were willing to refer their close friends and sex partners without the need for RDS incentives, suggesting that traditional word-of-mouth is an effective strategy to engage small networks of NMPO users.
Although internet-based recruitment was more cost-efficient and resulted in a higher number of eligible participants, these individuals were less likely to complete the survey. Similar findings were observed in a study that compared field- and internet-based recruitment methods to enroll drug-using men who have sex with men (Parsons, Vial, Starks, & Golub, 2013). Future studies that employ online recruitment methods to engage young adult NMPO users should aim to collect multiple types of contact information to permit follow-up with these individuals, including for example Facebook usernames and Twitter handles. Nonetheless, the use of these approaches should aim to ensure and provide participant anonymity wherever possible. Finally, the internet-based recruitment results were driven almost exclusively by the online classifieds website Craigslist.org, a finding that deserves further investigation.
Despite differences in NMPO and illicit drug use behaviors, participants in both samples reported a high prevalence of prior overdose experiences (overall, 51.8% had ever seen someone overdose, and 26.8% had overdosed themselves). These findings underscore previous research demonstrating that overdose experiences are pervasive among young adult NMPO users (Frank et al., 2015). This is despite the fact that young opioid users are less likely to perceive themselves at high risk for overdose compared to older adults (Rowe, Santos, Behar, & Coffin, 2016). The results of our study suggest that overdose prevention education could be distributed to at-risk young adults through online media, particularly to those residing in rural areas where access to this information may otherwise be limited. Furthermore, given our finding that internet-recruited participants tended to be younger and have shorter NMPO use histories, online classifieds may represent effective venues in which to engage young adults in prevention interventions, interacting with youth before they become heavier users and/or develop opioid use disorders. Further research is needed to determine how to most appropriately leverage evolving technologies (including social media) to disseminate prevention, treatment, and harm reduction services to the large and diverse population of NMPO-using youth (Marshall, Green, Yedinak, & Hadland, 2016). However, the high prevalence of injection drug use among field-based participants suggests more traditional methods of harm reduction outreach (e.g. mobile syringe programs) should continue to be implemented and expanded.
This study has several limitations that must be noted. First, given that a sampling frame for the target population did not exist, we were unable to compare the internet- and field-recruited participants to a random sample. Nonetheless, this study demonstrates the degree to which recruitment design can influence the characteristics of a study sample, even with specific eligibility criteria. Second, the relatively small sample size limited more detailed comparisons, including whether the sociodemographics of each sample differed by geographic area. Finally, all measures were self-reported and thus may be susceptible to various reporting errors, including recall bias and socially desirable reporting. We attempted to mitigate these biases by employing visual aids (e.g., opioid pill cards) and mixed interviewer-administered and self-administered assessments methods.
Conclusions
In sum, this study demonstrated important differences in the demographics, behaviors, and NMPO use patterns among young adults recruited in the field versus those reached through online venues. Our results also suggest caution in the use of RDS to recruit young adult NMPO users, unless formative research can demonstrate large and interconnected drug-using networks in the target population. Internet-based approaches using online classifieds may be more effective at reaching a subset of the population who have less experience with NMPO use, but nonetheless are at high risk for overdose and thus may benefit from overdose prevention and education. Ultimately, the choice of recruitment strategy should be a function of both resource availability, and a clear understanding of the needs of the target population.
Acknowledgements
We would like to thank the study participants for their contribution to the research, as well as current and past RAPiDS researchers and staff. We would also like to acknowledge Max King for his research assistance.
Funding
The RAPiDS project is supported by the US National Institute on Drug Abuse (R03-DA037770). Brandon Marshall is supported by a Henry Merrit Wriston Fellowship from Brown University. Dr Hadland is supported by the Leadership Education in Adolescent Health Training Program T71 MC00009 (MCH/HRSA) and a National Research Service Award 1T32 HD075727 (NIH/NICHD). Dr. Green is supported by the Agency for Healthcare Research and Quality (R18 HS024021) and the Centers for Disease Control and Prevention (R21 CE002165).
List of Abbreviations
- NMPO
Non-Medical Prescription Opioid Use
- RAPIDS
Rhode Island Young Adult Prescription Drug Study
- RDS
Respondent-Driven Sampling
- CAPI
Computer-Assisted Personal Interviewing
- CASI
Computer-Assisted Self Interviewing
- SAMHSA
Substance Abuse and Mental Health Services Administration
Footnotes
Declarations
Ethics Approval and Consent to Participate
This study received approval from Brown University’s research ethics committee, IRB #1403001006. Participants voluntarily signed informed consent forms prior to completing a confidential survey.
Declaration of Interest
The authors report no conflicts of interest.
REFERENCES
- Abdul-Quader AS, Heckathorn DD, McKnight C, Bramson H, Nemeth C, Sabin K,. . . Des Jarlais DC. (2006). Effectiveness of respondent-driven sampling for recruiting drug users in New York City: findings from a pilot study. Journal of Urban Health, 83(3), 459–476. doi: 10.1007/s11524-006-9052-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Zimmerman MA, Johns MM, Glowacki P, Stoddard S, & Volz E (2012). Innovative Recruitment Using Online Networks: Lessons Learned From an Online Study of Alcohol and Other Drug Use Utilizing a Web-Based, Respondent-Driven Sampling (webRDS) Strategy. Journal of Studies on Alcohol and Drugs, 73(5), 834–838. doi: 10.15288/jsad.2012.73.834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson RG, Nahhas RW, Martins SS, & Daniulaityte R (2016). Predictors of transition to heroin use among initially non-opioid dependent illicit pharmaceutical opioid users: A natural history study. Drug and Alcohol Dependence, 160, 127–134. doi: 10.1016/j.drugalcdep.2015.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Santaella J, Marshall BDL, Kim JH, & Martins SS (2015). Nonmedical prescription opioid use in childhood and early adolescence predicts transitions to heroin use in young adulthood: A national study. Journal of Pediatrics, 167(3), 605–612. doi: 10.1016/j.jpeds.2015.04.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LH, Hedegaard H, & Warner M (2014). Drug-poisoning deaths involving opioid analgesics: United States, 1999–2011. Hyattsville, MD: National Center for Health Statistics; Retrieved from http://www.cdc.gov/nchs/data/databriefs/db166.pdf. [PubMed] [Google Scholar]
- Chiauzzi E, Dasmahapatra P, Lobo K, & Barratt MJ (2013). Participatory research with an online drug forum: a survey of user characteristics, information sharing, and harm reduction views. Substance Use and Misuse, 48(8), 661–670. doi: 10.3109/10826084.2013.800117 [DOI] [PubMed] [Google Scholar]
- Daniulaityte R, Falck R, Li L, Nahhas RW, & Carlson RG (2012). Respondent-driven sampling to recruit young adult non-medical users of pharmaceutical opioids: problems and solutions. Drug and Alcohol Dependence, 121(1–2), 23–29. doi: 10.1016/j.drugalcdep.2011.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniulaityte R, Falck RS, Wang J, & Carlson RG (2009). Illicit use of pharmaceutical opioids among young polydrug users in Ohio. Addictive Behaviors, 34(8), 649–653. doi: 10.1016/j.addbeh.2009.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DF, White JB, & Nicholson T (2003). Using Internet-based surveys to reach hidden populations: Case of nonabusive illicit drug users. American Journal of Health Behavior, 27(3), 208–218. [DOI] [PubMed] [Google Scholar]
- Frank D, Mateu-Gelabert P, Guarino H, Bennett A, Wendel T, Jessell L, & Teper A (2015). High risk and little knowledge: overdose experiences and knowledge among young adult nonmedical prescription opioid users. International Journal on Drug Policy, 26(1), 84–91. doi: 10.1016/j.drugpo.2014.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubner NR, Delucchi KL, & Ramo DE (2016). Associations between binge drinking frequency and tobacco use among young adults. Addict Behav, 60, 191–196. doi: 10.1016/j.addbeh.2016.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD, Semaan S, Broadhead RS, & Hughes JJ (2002). Extensions of respondent-driven sampling: A new approach to the study of injection drug users aged 18–25. AIDS and Behavior, 6(1), 55–67. [Google Scholar]
- Johnston LG, & Sabin K (2010). Sampling hard-to-reach populations with respondent driven sampling. Methodological Innovations Online, 5(2), 38–48. [Google Scholar]
- Jones CM (2013). Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers - United States, 2002–2004 and 2008–2010. Drug Alcohol Depend, 132(1–2), 95–100. doi: 10.1016/j.drugalcdep.2013.01.007 [DOI] [PubMed] [Google Scholar]
- Jones CM, Paulozzi LJ, & Mack KA (2014). Sources of prescription opioid pain relievers by frequency of past-year nonmedical use United States, 2008–2011. JAMA Internal Medicine, 174(5), 802–803. doi: 10.1001/jamainternmed.2013.12809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JD, Mogali S, & Comer SD (2012). Polydrug abuse: a review of opioid and benzodiazepine combination use. Drug and Alcohol Dependence, 125(1–2), 8–18. doi: 10.1016/j.drugalcdep.2012.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz N, Fernandez K, Chang A, Benoit C, & Butler SF (2008). Internet-based survey of nonmedical prescription opioid use in the United States. Clinical Journal of Pain, 24(6), 528–535. doi: 10.1097/AJP.0b013e318167a087 [DOI] [PubMed] [Google Scholar]
- Lankenau SE, Teti M, Silva K, Bloom JJ, Harocopos A, & Treese M (2012). Initiation into prescription opioid misuse amongst young injection drug users. International Journal on Drug Policy, 23(1), 37–44. doi: 10.1016/j.drugpo.2011.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord S, Brevard J, & Budman S (2011). Connecting to Young Adults: An Online Social Network Survey of Beliefs and Attitudes Associated With Prescription Opioid Misuse Among College Students. Subst Use Misuse, 46(1), 66–76. doi: 10.3109/10826084.2011.521371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnani R, Sabin K, Saidel T, & Heckathorn D (2005). Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS, 19(Suppl 2), S67–S72. [DOI] [PubMed] [Google Scholar]
- Marshall BD, Green TC, Yedinak JL, & Hadland SE (2016). Harm reduction for young people who use prescription opioids extra-medically: Obstacles and opportunities. Int J Drug Policy, 10.1016/j.drugpo.2016.01.022. doi: 10.1016/j.drugpo.2016.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Kim JH, Chen LY, Levin D, Keyes KM, Cerda M, & Storr CL (2015). Nonmedical prescription drug use among US young adults by educational attainment. Social Psychiatry and Psychiatric Epidemiology, 50(5), 713–724. doi: 10.1007/s00127-014-0980-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, Boyd CJ, & Teter CJ (2007). Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addictive Behaviors, 32(3), 562–575. doi: 10.1016/j.addbeh.2006.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, & West BT (2008). Trends in prescription drug abuse and dependence, co-occurrence with other substance use disorders, and treatment utilization: results from two national surveys. Addictive Behaviors, 33(10), 1297–1305. doi: 10.1016/j.addbeh.2008.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Morales M, Cranford JA, & Boyd CJ (2007). Does early onset of non-medical use of prescription drugs predict subsequent prescription drug abuse and dependence? Results from a national study. Addiction, 102(12), 1920–1930. doi: 10.1111/j.1360-0443.2007.02015.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller PG, Johnston J, McElwee PR, & Noble R (2007). A pilot study using the internet to study patterns of party drug use: processes, findings and limitations. Drug Alcohol Rev, 26(2), 169–174. doi: 10.1080/09595230601146629 [DOI] [PubMed] [Google Scholar]
- Miller PG, & Sonderlund AL (2010). Using the internet to research hidden populations of illicit drug users: a review. Addiction, 105(9), 1557–1567. doi: 10.1111/j.1360-0443.2010.02992.x [DOI] [PubMed] [Google Scholar]
- National Institutes on Drug Abuse. (2011). Prescription Drug Abuse: December 2011. Topics in Brief. Retrieved from http://www.drugabuse.gov/sites/default/files/prescription_1.pdf
- Parsons JT, Vial AC, Starks TJ, & Golub SA (2013). Recruiting drug using men who have sex with men in behavioral intervention trials: a comparison of internet and field-based strategies. AIDS and Behavior, 17(2), 688–699. doi: 10.1007/s10461-012-0231-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, & Prochaska JJ (2012). Broad reach and targeted recruitment using Facebook for an online survey of young adult substance use. Journal of Medical Internet Research, 14(1), e28. doi: 10.2196/jmir.1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhode Island Department of Administration. (2000). Rhode Island Land Use Trends and Analysis (Including Land use Surveys for the Period 1970–1995). Providence, RI Retrieved from http://www.planning.ri.gov/documents/tp/TP149.PDF.
- Rowe C, Santos GM, Behar E, & Coffin PO (2016). Correlates of overdose risk perception among illicit opioid users. Drug and Alcohol Dependence, 159, 234–239. doi: 10.1016/j.drugalcdep.2015.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy E, Arruda N, & Bourgois P (2011). The growing popularity of prescription opioid injection in downtown Montreal: new challenges for harm reduction. Substance Use and Misuse, 46(9), 1142–1150. doi: 10.3109/10826084.2011.552932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Seth P, David F, & Scholl L (2016). Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010–2015. MMWR: Morbidity and Mortality Weekly Report, 65(5051), 1445–1452. doi: 10.15585/mmwr.mm655051e1 [DOI] [PubMed] [Google Scholar]
- Salganik MJ, & Heckathorn DD (2004). Sampling and estimation in hidden populations using respondent-driven sampling. Sociological Methodology, 34(1), 193–239. [Google Scholar]
- Strathdee SA, & Beyrer C (2015). Threading the Needle—How to Stop the HIV Outbreak in Rural Indiana. New England Journal of Medicine, 373(5), 397–399. doi: 10.1056/NEJMp1507252 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2008). Results from the 2007 National Survey on Drug Use and Health: National Findings. Rockville, MD: SAMHSA. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMSHA). (2013). The NSDUH Report: State Estimates of Nonmedical Use of Prescription Pain Relievers. Rockville, MD: SAMSHA. [PubMed] [Google Scholar]
- Sung HE, Richter L, Vaughan R, Johnson PB, & Thom B (2005). Nonmedical use of prescription opioids among teenagers in the United States: trends and correlates. Journal of Adolescent Health, 37(1), 44–51. doi: 10.1016/j.jadohealth.2005.02.013 [DOI] [PubMed] [Google Scholar]
- Temple EC, & Brown RF (2011). A Comparison of Internet-Based Participant Recruitment Methods: Engaging the Hidden Population of Cannabis Users in Research. Journal of Research Practice, 7(2), D2. [Google Scholar]
- Weiss AJ, Elixhauser A, Barrett ML, Steiner CA, Bailey MK, & O’Malley L (2016). Opioid-Related Inpatient Stays and Emergency Department Visits by State, 2009–2014,. HCUP Statistical Brief #219. [Google Scholar]
- Wilkerson JM, Shenk JE, Grey JA, Rosser BRS, & Noor SW (2015). Recruitment strategies of methamphetamine-using men who have sex with men into an online survey. Journal of Substance Use, 20(1), 33–37. doi: 10.3109/14659891.2013.868936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yedinak JL, Kinnard EN, Hadland SE, Green TC, Clark MA, & Marshall BDL (2016). Social context and perspectives of non-medical prescription opioid use among young adults in Rhode Island: A qualitative study. The American Journal on Addictions, 25(8), 659–665. doi: 10.1111/ajad.12466 [DOI] [PMC free article] [PubMed] [Google Scholar]


