Abstract
Massive weight loss (MWL) brachioplasty is frequently requested for the improvement of the appearance and function of arms. Despite its diffusion, this procedure can be associated with significant complications. Liposuction-assisted brachioplasty (LAB) preserves the vascular, nervous, and lymphatic network and reduces the incidence of postoperative complications. This retrospective cohort study is aimed at analyzing two different modalities of arm contouring after MWL by evaluating the outcomes and complications. Of 31 patients (all females, average age 43.5 years), 20 were managed with standard brachioplasty represented by a swallowtail scar and monobloc resection and 11 with brachioplasty combined with aggressive liposuction. Evaluated parameters included age, body mass index, method of weight loss, and complications rate. No statistical analysis was used. Major postoperative complications (reoperation, bleeding, or thromboembolism) were not reported in both groups. The incidence of minor complications (wound separation, wound infection, and seroma) was globally 42%; the incidence of complications was significantly lower in the LAB group (9% vs. 60%). The incidence of hypertrophic scarring or keloid was higher in the control group (55% vs. 18%). Most patients were satisfied after surgery: in the LAB group, 81.8% of the patients expressed a high degree of satisfaction and 18.2% a good degree of satisfaction after 4 months of follow-up. In our experience, the LAB should be preferred in MWL patients because it has a lower rate of complications and a faster recovery than the standard technique. Proper execution requires considerable technical skill and experience.
Keywords: Body contouring, brachioplasty, liposuction, postbariatric surgery
INTRODUCTION
The growing popularity of bariatric surgery was determined by the increase in the massive weight loss (MWL) population. MWL produces various body deformities, therefore the increasing demand for body contouring surgery.[1,2]
In a number of cases, problems of skin excess and ptosis in the arms, abdomen, hips, and thighs that can be significant enough to cause functional impairments, skin inflammation, and infections as well as considerable psychological discomfort have been reported.[3,4,5] The arms are often the first body area to be treated because of the most visible and compromising global body harmony. Although brachioplasty is widespread, the risk of postoperative complications such as hematomas, lymphedema, or skin sensitivity disorders still remains high because the surgical area has vascular, nerve, and lymphatic structures.[6,7,8,9,10]
Thorek[11] was the first author to describe brachioplasty as a surgical procedure to improve arm shape; over the years, many other surgeons have been looking for techniques to correct skin deformity, achieve good aesthetic results, and at the same time reduce the incidence of postoperative complications.[12,13,14,15,16,17]
Since the introduction by Illouz in 1980,[18] liposuction has been frequently combined with body contouring techniques. Liposuction can be used in the arm either alone in the case of mild skin laxity and ptosis or in conjunction with surgical resection.[19] In the latter case, it is used to refine arm contouring.
Our experience with 11 patients who were operated for arm deformity after MWL with liposuction-assisted brachioplasty (LAB) is presented. The results of this study are compared with those obtained by using the traditional approach and the outcomes and complications recorded in the last 8 years are evaluated.
MATERIALS AND METHODS
In this retrospective review, 31 patients (age range 22–66 years) underwent medial arm contouring after MWL (December 2009–April 2017). Traditional brachioplasty technique with a swallowtail scar and monobloc resection of the skin excess was performed in 20 patients (control group) whereas the LAB was performed in 11 patients (study group). The average follow-up was 44 months (range 4–120 months).
Surgical technique
Standard brachioplasty
Preoperative markings are made with the patient standing in an upright position. A straight line is drawn in the bicipital groove from the medial condyle of the elbow to the axillary dome. This line indicates approximately the final scar location as well as the approximate axis of the ellipse of resection. The width of the ellipse, which is usually between 4 and 6cm, is estimated with pinch test. At the axilla, we mark two ellipses so that the final scar has a swallowtail design [Figure 1A].
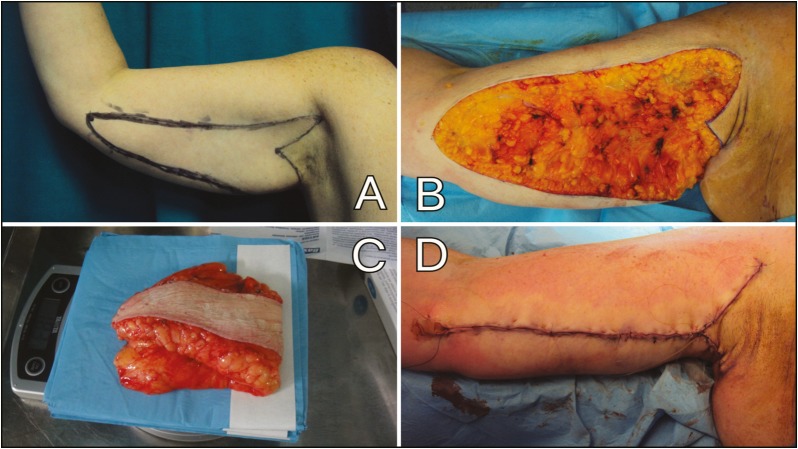
Figure 1.
(A) Preoperative markings of standard brachioplasty. (B) Ellipse was removed en bloc. (C) Excised skin. (D) Final appearance of the arm
All patients receive general anesthesia and are positioned supine on the surgical table with arms abducted at 90°; we wrap the lower limbs as a preventive measure from thromboembolic risk. Two grams of cefazolin is infused intravenously before the incision. We start the procedure with an infusion of Klein solution (1mg epinephrine/L saline solution + 3 naropin 7.5mg/mL) in the resection area. After skin incision, the ellipse is removed en bloc, leaving some fat over the fascia to preserve the superficial lymphatic network [Figure 1B,C].
We usually anchor the dermis of the upper and lower skin flap to brachial fascia with absorbable sutures. This leads to less tension on the scar and to more lasting results over time. We put a drain for each arm treated and then, we complete the planned suture of the subcutaneous tissue, subdermal tissue, and skin with absorbable suture Monocryl® 3-0 and 4-0 [Figure 1D]. A compressive dressing is then applied.
Liposuction-assisted brachioplasty
The patient is drawn in a vertical position with arms raised and abducted at 90°, and forearms supinated in order to expose the medial bicipital groove [Figure 2A].
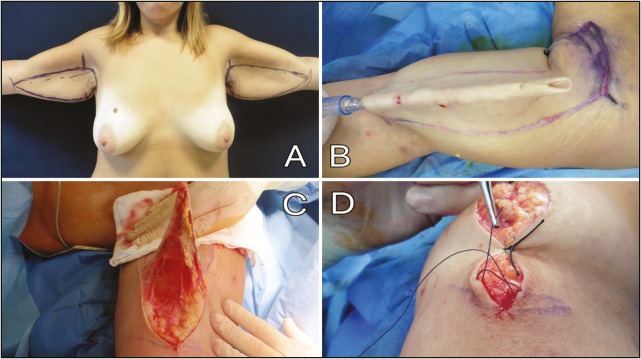
Figure 2.
(A) Preoperative markings of liposuction-assisted brachioplasty. (B) Medial arm liposuction. (C) Skin layer resection. (D) Single running intradermal suture in Vicryl 2/0
First we draw a vertical line from the anterior axillary dome to the posterior one. Then we draw the distal end of the skin fold and mark a horizontal line from this point up to the axilla: this line must be parallel to the upper profile of the arm and perpendicular to the vertical axillary line. The resection’s width in the axilla is estimated with the pinch test. Then we find the inferior line by lifting the skin upward and marking a straight line from the axilla to the end of the skin fold. We repeated the same procedure for the upper resection line pulling the skin downward. It is important to draw straight lines in order to have linear scars that are easy to hide under the clothes. At the end we draw the resection area in the axilla and in the lateral chest wall.
Markings were different depending on the amount of the excess skin:
Mild excess: we mark a small triangle oriented in the same direction of the main scar [Figure 2A].
Moderate excess: we mark a larger ellipse that is perpendicular to the brachial scar. Triangle’s width is estimated by pinch test.
Severe excess: we use the same markings of the moderate excess adding a further ellipse parallel to the inframammary fold and perpendicular to the lateral thoracic ellipse.
The patient wears antithrombotic stockings or elastic wraps throughout the duration of the surgery as a preventive measure from thromboembolic risk. All patients receive general anesthesia and are positioned supine on the surgical table with arms abducted at 90°. Two grams of cefazolin is infused intravenously before the incision.
We infiltrated the resection area with 1mg of epinephrine/L saline solution. The infiltration–aspiration ratio is 1:1. Then we infiltrate the incision lines with 1.5mg epinephrine/L saline solution.
After a period of about 15–20min from the infiltration, we perform the liposuction in the area of skin resection using three holes and 3-, 4-, 5-mm diameter cannulas. We remove all the fat between the skin and the arm muscle fascia so at the end of liposuction the skin is just 2 or 3mm thick [Figure 2B]. If necessary, we perform a “standard” liposuction (final thickness of the skin: 1–1.5cm) in the other parts of the arm.
After liposuction we put some silk suture and check if the ellipse is wide enough and if we are able to close: very often because of tissue mobilization thanks to liposuction it is necessary to widen the ellipse. In that case, we change the position of the inferior line to prevent the scar from moving forward. Also if we had to modify the lateral thoracic ellipse, we change the position of the posterior line to avoid any distortion or lateral displacement of the breast. When we are satisfied with the drawing, we incise the ellipse. The incision will be bloodless due to the previous infiltration: in this way, we proceed faster because there is no need to coagulate the dermis and the wound heals better and faster. Then we remove the excess skin at a very superficial level, just under the dermis: it is important to keep the coagulator oriented toward the skin to not damage the underlying connective network [Figure 2C].
In the axilla, beside the skin we also remove sweat glands in order to reduce local moisture and ensure better wound healing. Usually we do not put drains. Then, we perform the suture with a single running intradermal suture in Vicryl 2/0. There are no external stitches: on one side the suture is blocked passing the needle two times in the same point [Figure 2D]; on the other one we continue the suture with four passages in the opposite direction. Unlike what we perform in the standard technique and in the other body districts, after the LAB, we do not use any compressive garments to reduce the risk of compartmental syndrome. Follow-up examinations are conducted every 5 days for the first 15 days and then at 1 month, 3 months, 6 months, and 1 year after surgery [Figures 3 and 4.
Figure 3.

(A) Anterior view of a 38-year-old woman who underwent liposuction-assisted brachioplasty after gastric bypass and weight loss of 54kg. (B) Six months postoperatively. Skin excess had been removed and the arm contour was aesthetically pleasing
Figure 4.

(A) Anterior views of a 29-year-old woman who underwent liposuction-assisted brachioplasty after sleeve gastrectomy and weight loss of 59kg. (B) Six months postoperatively. Note the location and the quality of the scar
RESULTS
Patients’ mean weight at the time of surgery was 75.4kg, with an average BMI of 26.67. The mean weight loss was 56.42kg (average delta-BMI: 19.56). The mean time of surgery was 2.6h in both groups whereas the mean time of postoperative hospitalization was significantly lower in the LAB group (2.3 vs. 3.2 days, P < 0.001). This results in lower hospitalization costs and early patient resumption of normal activity. The mean amount of tissue removed was 256.63g in the LAB group and 397.8g in the standard technique group.
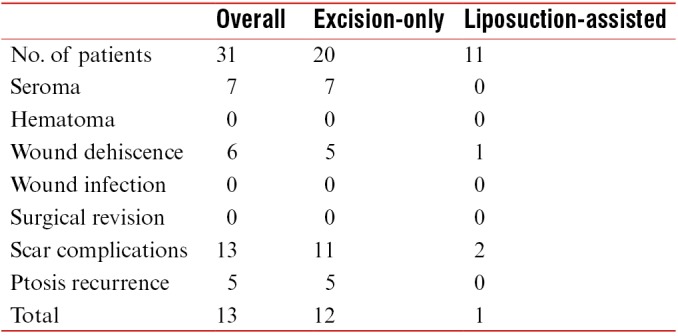
Major postoperative complications such as re-treatment, bleeding, or thrombo-embolism were not observed in the two groups. The incidence of minor complications (wound separation, wound infection, and seroma) was globally 42%; the incidence of complications was significantly lower in the LAB group (9% vs. 60%, P < 0.01). In the LAB group, only one patient (smoker) had problems of wound healing after surgery; in the control group, seven patients (35%) had seroma and five patients (25%) had wound separation. The incidence of hypertrophic scarring or keloid was higher in the second group (55% vs. 18%). Five patients (20%) of the control group experienced a recurrence of skin ptosis, whereas none of the LAB group had such problems.
Smoke was found to be a preoperative risk factor for complications (OR: 7, P < 0.05). Age, amount of weight loss, surgery duration, and amount of tissue removed were found to be higher in patients who experienced complications.
Most patients were satisfied after surgery: in the standard technique group, 50% of the patients expressed a high degree of satisfaction, 25% a good degree, 5% a sufficient degree, and 25% an insufficient degree because of bad scars. In the LAB group, 81.8% of the patients expressed a high degree of satisfaction and 18.2% a good degree of satisfaction; no patient was dissatisfied. Patients’ data are reported [Tables 1–4].
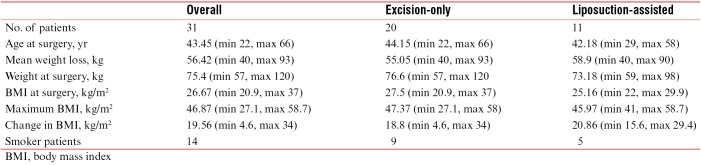
Table 1.
Demographic data
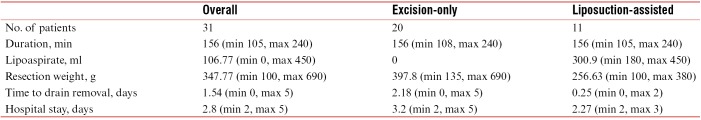
Table 4.
Patients’ satisfaction
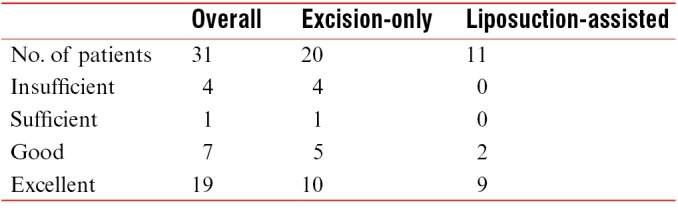
Table 2.
Surgical data
Table 3.
Complications
DISCUSSION
Brachioplasty is a surgical procedure used to treat lipodystrophy and ptosis caused by MWL after bariatric surgery. Despite its diffusion, this procedure is full of pitfalls because nerves, blood vessels, and lymphatics of the arm are located just beneath the area of resection so complications such as hematoma, seroma, or paresthesia are common.[6,7,8,9,10] One of the main problems is scar location and quality.
Strauch et al. proposed to place the scar in the posterior part of the arm where lymphatic vessels are fewer,[20] but in this way the risk of damaging the subcutaneous posterior branch of the medial cutaneous antebrachial nerve is higher.[10] Furthermore, authors who prefer the medial arm scar argue that posterior scars are more difficult to hide from behind and tend more easily to become hypertrophic.[21,22]
For this reason, we prefer to locate the final scar in the medial arm that is easier to hide even if it increases the risk of injuring subcutaneous branches of sensory nerves and superficial lymphatics of the limb. To avoid this, we have modified the standard technique including liposuction of the area of resection.
In ex-obese patients, the arms present two types of problems: excess volume, due to residual fat after bariatric surgery and MWL, and excess skin.[33] LAB resolves the first problem with liposuction, and the second one with surgical resection. In fact, liposuction reduces the volume of the medial arm but does not increase complication rate, because it does not damage the perforator vessels,[23,24] the microcirculation, that allows fluid, molecular, gas, cellular exchange,[25] and of lymphatic vessels.[26]
Brachioplasty combined with liposuction was already described by Pascal and Le Louarn in 2005.[27] Recently, two studies evaluated the safety of these combined procedures. Gusenoff et al.[28] stated that brachioplasty could be safe if combined with other procedures, and Bossert et al.[9] found that the complication rate of the patient who underwent brachioplasty with medial scar alone was the same as that of the patient who underwent brachioplasty and liposuction of the posterior arm (outside the brachioplasty excision site). In our study, we found that the incidence of complications was significantly lower in the LAB group than in the standard technique group (9% vs. 60%, P < 0.01).
Aly[29] sustained that combination of liposuction and brachioplasty could not be safe because tissue edema makes it more difficult to correctly estimate the amount of tissue to be removed: so there is a higher risk of over- or under-resection. We avoided this because after liposuction and before the incision of the skin we check the adequacy and the accuracy of the drawings and if necessary we enlarge or reduce the resection ellipse width.
Furthermore, even among proponents of the combined procedure, there is no consensus about where to suction the arm, if under the resection area,[27,30] in the adjacent tissues,[31,32] or circumferentially. In our study, we chose to perform the suction of the excision site; in this way, the anatomical planes are easier to identify and the resection can be made very superficially, just under the dermis, preserving blood vessels, lymphatics, and nerves of the medial arm. Conversely, with the monobloc resection performed using the standard technique, these structures remain within tissues resected and complications such as seroma, bleeding, or hematoma are more likely to happen. This is also the reason why in the standard technique we used to put drains that we removed after 3 or 4 days, whereas no drain was put in the LAB group; and without drains there was no wound infection, the comfort of the patient was higher, and the duration of hospitalization was shorter.
We found that patients who smoked had more complications from both procedures; so we encourage to avoid smoking for at least 1 month before surgery. Furthermore, special care should be taken with older patients, with patients who have lost more than 50kg, and when surgery duration is longer than 3h.
The combination of these two procedures could elongate surgery time and the risk of complications for various reasons such as prolonged anesthesia, hypothermia, or surgeon fatigue. In our study, the mean surgery time was similar in the two groups. In fact, liposuction did not take long because the area to be treated was usually small, so the total duration of the surgery was not longer than the mean duration of a standard brachioplasty; on the other hand, the lower morbidity of the procedure reduced the mean time of hospitalization and allowed patients to return to their work earlier.
Finally, the aesthetic result was satisfactory for all patients but the patients who underwent LAB were particularly pleased with the absence of drains and external sutures and also with the reduction in axillary sweating, often disabling in obese patients.
CONCLUSIONS
Brachioplasty is a surgical procedure associated with high morbidity due to the density of important anatomical structures in a narrow space and at a superficial level. LAB, thanks to a selective and multimodal approach to arm deformity, preserves vascular, nervous, and lymphatic network and reduces the incidence of postoperative complications. The encouraging results of LAB and patient satisfaction have led the authors to abandon the traditional technique.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cosmetic Surgery National Data Bank Statistics. Aesthet Surg J. 2016;13:1–29. doi: 10.1093/asj/36.Supplement_1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Society of Plastic Surgeons. [Accessed June 19, 2015] Plastic Surgery Trends [ASPS website] 2015. Jun 1, [Last accessed on 2015 May 14]. Available from: http://www.plasticsurgery.org/news/2015/massive-weight-lossfuels-surge-in-plastic-surgery.html .
- 3.Koller M, Schubhart S, Hintringer T. Quality of life and body image after circumferential body lifting of the lower trunk: A prospective clinical trial. Obes Surg. 2013;13:561–6. doi: 10.1007/s11695-012-0849-z. [DOI] [PubMed] [Google Scholar]
- 4.Modarressi A, Balagué N, Huber O, Chilcott M, Pittet-Cuénod B. Plastic surgery after gastric bypass improves long-term quality of life. Obes Surg. 2013;13:24–30. doi: 10.1007/s11695-012-0735-8. [DOI] [PubMed] [Google Scholar]
- 5.van der Beek ES, Geenen R, de Heer FA, van der Molen AB, van Ramshorst B. Quality of life long-term after body contouring surgery following bariatric surgery: Sustained improvement after 7 years. Plast Reconstr Surg. 2012;13:1133–9. doi: 10.1097/PRS.0b013e318267d51d. [DOI] [PubMed] [Google Scholar]
- 6.Teimourian B, Malekzadeh S. Rejuvenation of the upper arm. Plast Reconstr Surg. 1998;13:545–51. doi: 10.1097/00006534-199808000-00041. [DOI] [PubMed] [Google Scholar]
- 7.Symbas JD, Losken A. An outcome analysis of brachioplasty techniques following massive weight loss. Ann Plast Surg. 2010;13:588–91. doi: 10.1097/SAP.0b013e3181c6cde8. [DOI] [PubMed] [Google Scholar]
- 8.Zomerlei TA, Neaman KC, Armstrong SD, Aitken ME, Cullen WT, Ford RD, et al. Brachioplasty outcomes: A review of a multipractice cohort. Plast Reconstr Surg. 2013;13:883–9. doi: 10.1097/PRS.0b013e3182827726. [DOI] [PubMed] [Google Scholar]
- 9.Bossert RP, Dreifuss S, Coon D, Wollstein A, Clavijo-Alvarez J, Gusenoff JA, et al. Liposuction of the arm concurrent with brachioplasty in the massive weight loss patient: Is it safe? Plast Reconstr Surg. 2013;13:357–65. doi: 10.1097/PRS.0b013e3182789de9. [DOI] [PubMed] [Google Scholar]
- 10.Knoetgen J, 3rd, Moran SL. Long-term outcomes and complications associated with brachioplasty: A retrospective review and cadaveric study. Plast Reconstr Surg. 2006;13:2219–23. doi: 10.1097/01.prs.0000218707.95410.47. [DOI] [PubMed] [Google Scholar]
- 11.Thorek M. Esthetic surgery of pendulous breast, abdomen and arms in the female. Ill Med J. 1930;13:48–57. [Google Scholar]
- 12.Baroudi R. Dermolipectomy of the upper arm. Clin Plast Surg. 1975;13:485–9. [Google Scholar]
- 13.Borges AF. W-plastic dermolipectomy to correct “bat-wing” deformity. Ann Plast Surg. 1982;13:498–501. [PubMed] [Google Scholar]
- 14.Juri J, Juri C, Elías JC. Arm dermolipectomy with a quadrangular flap and “T” closure. Plast Reconstr Surg. 1979;13:521–5. doi: 10.1097/00006534-197910000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Goddio AS. A new technique for brachioplasty. Plast Reconstr Surg. 1989;13:85–91. doi: 10.1097/00006534-198907000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Lockwood T. Brachioplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;13:912–20. doi: 10.1097/00006534-199509001-00022. [DOI] [PubMed] [Google Scholar]
- 17.Lillis PJ. Liposuction of the arms. Dermatol Clin. 1999;13:783–97. doi: 10.1016/s0733-8635(05)70127-3. [DOI] [PubMed] [Google Scholar]
- 18.Illouz YG. Study of subcutaneous fat. Aesthetic Plast Surg. 1990;13:165–77. doi: 10.1007/BF01578345. [DOI] [PubMed] [Google Scholar]
- 19.Song AY, Jean RD, Hurwitz DJ, Fernstrom MH, Scott JA, Rubin JP. A classification of contour deformities after bariatric weight loss: The Pittsburgh rating scale. Plast Reconstr Surg. 2005;13:1535. doi: 10.1097/01.prs.0000182606.92069.13. [DOI] [PubMed] [Google Scholar]
- 20.Strauch B, Greenspun D, Levine J, Baum T. A technique of brachioplasty. Plast Reconstr Surg. 2004;13:1044–8; discussion 1049. doi: 10.1097/01.prs.0000105648.54174.11. [DOI] [PubMed] [Google Scholar]
- 21.Vogt PA, Baroudi R. Brachioplasty and brachial suction assisted lipectomy. In: Cohen M, editor. Mastery of Plastic and Reconstructive Surgery. 1st ed. Boston, MA: Little Brown & Co; 1994. pp. 2219–36. [Google Scholar]
- 22.Hurwitz DJ, Holland SW. The L brachioplasty: an innovative approach to correct excess tissue of the upper arm, axilla, and lateral chest. Plast Reconstr Surg. 2006;13:403. doi: 10.1097/01.prs.0000200800.81548.37. [DOI] [PubMed] [Google Scholar]
- 23.Graf R, de Araujo LR, Rippel R, Neto LG, Pace DT, Cruz GA. Lipoabdominoplasty: Liposuction with reduced undermining and traditional abdominal skin flap resection. Aesthetic Plast Surg. 2006;13:1–8. doi: 10.1007/s00266-004-0084-7. [DOI] [PubMed] [Google Scholar]
- 24.Salgarello M, Barone-Adesi L, Cina A, Farallo E. The effect of liposuction on inferior epigastric perforator vessels: A prospective study with color doppler sonography. Ann Plast Surg. 2005;13:346–51. doi: 10.1097/01.sap.0000179168.69667.43. [DOI] [PubMed] [Google Scholar]
- 25.Bertheuil N, Chaput B, Berger-Müller S, Ménard C, Mourcin F, Watier E, et al. Liposuction preserves the morphological integrity of the microvascular network: Flow cytometry and confocal microscopy evidence in a controlled study. Aesthet Surg J. 2016;13:609–18. doi: 10.1093/asj/sjv209. https://doi.org/10.1093/asj/sjv209 . [DOI] [PubMed] [Google Scholar]
- 26.Haddad Filho D, Kafejian-Haddad AP, Alonso N, Perez Mdel C, Castiglione M, Fukutaki MF, et al. Lymphoscintigraphic appraisal of the lower limbs after liposuction. Aesthet Surg J. 2009;13:396–9. doi: 10.1016/j.asj.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 27.Pascal JF, Le Louarn C. Brachioplasty. Aesthetic Plast Surg. 2005;13:423–9; discussion 430. doi: 10.1007/s00266-005-0058-4. [DOI] [PubMed] [Google Scholar]
- 28.Gusenoff JA, Coon D, Rubin JP. Brachioplasty and concomitant procedures after massive weight loss: A statistical analysis from a prospective registry. Plast Reconstr Surg. 2008;13:595–603. doi: 10.1097/PRS.0b013e31817d54a9. [DOI] [PubMed] [Google Scholar]
- 29.Aly A. Discussion: liposuction of the arm concurrent with brachioplasty in the massive weight loss patient: Is it safe? Plast Reconstr Surg. 2013;13:366–7. doi: 10.1097/PRS.0b013e318278d70e. [DOI] [PubMed] [Google Scholar]
- 30.de Runz A, Colson T, Minetti C, Brix M, Pujo J, Gisquet H, et al. Liposuction-assisted medial brachioplasty after massive weight loss: An efficient procedure with a high functional benefit. Plast Reconstr Surg. 2015;13:74e–84e. doi: 10.1097/PRS.0000000000000845. [DOI] [PubMed] [Google Scholar]
- 31.D’Ettorre M, Bracaglia R, Gentileschi S, Tambasco D. S-shaped brachioplasty: An effective technique to correct excess skin and fat of the upper arm. Plast Reconstr Surg. 2013;13:675e–6e. doi: 10.1097/PRS.0b013e31829fe259. [DOI] [PubMed] [Google Scholar]
- 32.Bracaglia R, D’Ettorre M, Gentileschi S, Mingrone G, Tambasco D. “Kris knife” brachioplasty after bariatric surgery and massive weight loss. Aesthetic Plast Surg. 2013;13:640–2. doi: 10.1007/s00266-013-0101-9. [DOI] [PubMed] [Google Scholar]
- 33.Labardi L, Gentile P, Gigliotti S, Marianetti M, Colicchia GM, Pascali M, et al. Medial thighplasty: Horizontal and vertical procedures after massive weight loss. J Cutan Aesthet Surg. 2012;13:20–5. doi: 10.4103/0974-2077.94330. [DOI] [PMC free article] [PubMed] [Google Scholar]