Abstract
Background and purpose
Although case reports have long identified a temporal association between cocaine use and ischemic stroke, few epidemiological studies have examined the association of cocaine use with ischemic stroke in young adults, by timing, route and frequency of use.
Methods
A population-based case-control study design with 1,090 cases and 1,154 controls was used to investigate the relationship of cocaine use and young-onset ischemic stroke. Stroke cases were between the ages of 15 and 49. Logistic regression analysis was used to evaluate the association between cocaine use and ischemic stroke with and without adjustment for potential confounders.
Results
Ever use of cocaine was not associated with stroke with 28% of cases and 26% of controls reporting ever use. In contrast, acute cocaine use in the prior 24 hours was strongly associated with increased risk of stroke (age-sex-race adjusted OR = 6.4, 95% CI=2.2 - 18.6). Among acute users, the smoking route had an adjusted odds ratio of 7.9 (95% CI=1.8 – 35.0), while the inhalation route had an adjusted odds ratio of 3.5 (95% CI=0.7 – 16.9). After additional adjustment for current alcohol, smoking use and hypertension, the odds ratio for acute cocaine use by any route was 5.7 (95% CI =1.7, 19.7). Of the 26 patients with cocaine use within 24 hours of their stroke, 14 reported use within 6 hours of their event.
Conclusion
Our data are consistent with a causal association between acute cocaine use and risk of early-onset ischemic stroke.
Keywords: stroke, cocaine, young adult
INTRODUCTION
Cocaine is one of the most commonly abused drugs in the United States. Population-based data from the Greater Cincinnati and Northern Kentucky region indicate a threefold increase in cocaine use among young adults with stroke between 1993 and 20051. Case reports and case series2 have long suggested a link between acute cocaine use and ischemic stroke (IS) in young adults. These clinical observations have strong biological plausibility due to cocaine’s effects on the cardiovascular system. Nevertheless, few epidemiological studies have evaluated the effect of cocaine on IS risk3–8. While most3–5, but not all reports6, 7 have supported an association between cocaine use and IS, limitations of prior research include grouping ischemic and hemorrhagic stroke3, 6, lack of data on time of last cocaine use4–6 or route of use3, 5, 6, and small numbers of cases3, 4, 6, 7. The goal of this report is to determine the association between cocaine use and risk of IS, with particular attention to the effects of timing and route of cocaine use, in a large population-based case-control study.
METHODS
Study Population
The Stroke Prevention in Young Adults Study was designed as a population-based case–control study of young onset ischemic stroke. During 3 study periods between 1992 and 2008, cases with a first-ever ischemic stroke ages 15 to 49 years were identified by discharge surveillance from 59 nonfederal acute care hospitals in the greater Baltimore/Washington, DC area and by direct referral from regional neurologists. In the initial study period, only women were recruited, the upper age limit was 44 years, and controls were in a 2:1 ratio to cases and were frequency-matched to cases by age, sex, region of residence. Women were recruited in the second study period and men in the third study period. In the last two study periods, the upper age limit was 49 years, and controls were in a 1:1 ratio to cases and were additionally matched for race. Details of the study design have been previously described.8
Assessment of cocaine use and other stroke risk factors
To assess the use of illicit drug use, participants were asked to recall whether, prior to the reference date, they had ever used drugs, pills or medications for non-medical or recreational reasons or to “get high”. The name(s), route(s) and timing(s) of drug use were also collected. The reference date was defined as the date of stroke onset for cases and for controls, the date of interview (initial study period) or the day of week that the stroke occurred in the matched case (last two study periods). Participants were shown cards with the names, routes of use and duration of use of various illicit drugs. In order to minimize potential discomfort associated with disclosing sensitive information, participants indicated their responses using codes printed on the cards rather than naming the drug or route of use directly. In addition, participants were informed that their responses were protected by a Federal Confidentiality Certificate. A copy of the questionnaire on drug use is provided in the Supplementary Materials. Acute cocaine use was defined as use of cocaine within 24 hours prior to the reference date, and current cocaine use was defined as cocaine use within one month (including those reporting cocaine use within 24 hours) prior to the reference date.
Information on traditional stroke risk factors (e.g. history of hypertension, diabetes, current smoking status and alcohol consumption) and demographic variables (e.g. age, gender, and race) was collected by self-report through a standardized face-to-face interview. Current smoking status was defined as use within one month prior to the stroke or, for controls, prior to the reference date. Current alcohol consumption was defined as having a drink of wine, beer or hard liquor in the year prior to the stroke or, for controls, prior to the reference date.
The study was approved by the University of Maryland at Baltimore Institutional Review Board and all participants gave informed consent.
Statistical analyses
Statistical analyses were performed using the Statistical Analysis System Software package (version 9.3; SAS Institute, Inc., Cary, N.C.). Cases and controls were compared for differences in means using t-tests (for continuous variables) or differences in proportions by χ2 tests (for categorical variables) to obtain the unadjusted two-sided P-values. Logistic regression with case/control status as the outcome and study characteristics as predictors was used to obtain the age-, sex- and ethnicity-adjusted p-values.
Assessment of the association between cocaine use and IS was performed using a logistic regression model with case/control status as outcome and cocaine variable as the predictor after adjusting for the effect of age, gender, ethnicity and/or other stroke risk factors. The odds ratio (OR) of cocaine use (e.g. ever, 1–30 days, or within 24 hours) was estimated by comparing to those who had never used cocaine previously (reference group).
Kappa was calculated to estimate the agreement between self-reported current cocaine use and the results of toxicology screening from the medical record among a subset of 373 cases.
RESULTS
Study characteristics
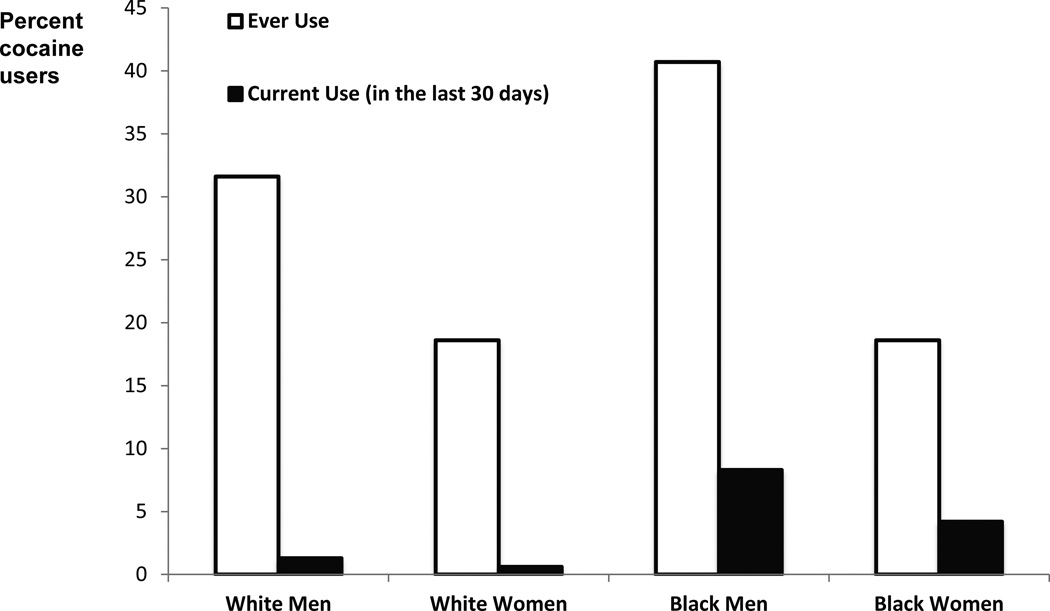
A total of 1,101 adjudicated first-ever IS cases and 1,154 stroke-free controls, aged 15–49 years old, were recruited in the study. This report is based on the 1,090 cases and 1,152 controls for whom cocaine information was available. Table 1 summarizes the characteristics of the study participants. The mean age was 41 years for cases and 39 years for controls. Self-reported race was primarily white or black. Cases were more likely than controls to report having a history of hypertension and diabetes and being current smokers but less likely to be current alcohol users. There was no statistical difference of self-reported history of ever use of cocaine between cases and controls (28% versus 26%, p=0.95). Figure 1 shows rates of ever use and current use of cocaine among controls, stratified by race and gender. Males had higher rates of use than females and African-Americans had higher rates of use than whites.
Table 1.
Characteristics of cases and controls
| Cases (n=1,090) |
Controls (n=1,152) |
p-value* | |
|---|---|---|---|
| Age, mean (standard deviation) | 40.9 (7.0) | 38.6 (7.4) | <0.001† |
| Male, n (%) | 584 (53.6) | 537 (46.6) | 0.001† |
| Self-reported race, n (%) | |||
| White | 544 (50) | 656 (57) | 0.003† |
| Black | 490 (45) | 441 (38) | |
| Others | 56 (5) | 55 (5) | |
| History of diabetes, n (%) | 186 (17.1) | 53 (4.6) | <0.001 |
| History of hypertension, n (%) | 455 (41.7) | 208 (18.1) | <0.001 |
| Current Smokers, n (%) | 492 (45.1) | 337 (29.3) | <0.001 |
| Current alcohol users, n (%) | 659 (60.5) | 764 (66.3) | 0.005 |
| History of cocaine use | |||
| Never | 784 (71.9) | 856 (74.3) | 0.95 |
| Ever | 306 (28.1) | 296 (25.7) |
Unadjusted p-values for age, gender and ethnicity; for other variables, P-values were adjusted for age, gender and race.
The age, gender and race disparity between cases and controls is due to the fact that the initial study period had a younger age limit, recruited only women, did not match for race, and had a 1:2 case:control ratio.
Figure 1.
Prevalence of self-reported cocaine use among controls by gender and ethnicity*
*Percentage of self-reported cocaine use was estimated based on control samples only; current cocaine users include those who reported cocaine use within 24 hours and 1–30 days.
Cocaine use and risk of IS
Table 2 shows the association between cocaine use and IS, stratified by timing and route of intake, adjusted for age, gender and ethnicity. Compared to those who had never used cocaine, individuals reporting acute cocaine use within last 24 hours had a 6.4-fold (95% CI 2.2–18.6) increase in the odds of ischemic stroke. The sample sizes of the cocaine use groups by different routes were small, particularly for intravenous use. However, among the acute users, those who indicated smoking as the route of administration showed the strongest association with IS (OR=7.9, 95% CI 1.8–35.0). Among cases with acute use of cocaine within 24 hours prior to stroke onset, the median frequency of cocaine use in the past year was 7 times per week, higher than the median frequency among all cases (1.2 times per week). After excluding acute cocaine users, those who reported frequent use of cocaine (more than once per week) in the past year remained significantly associated with an increased risk of IS, although the estimated effect was markedly reduced (OR=1.9, 95% CI 1.1–3.3). The association between acute cocaine use and risk of IS remained statistically significant after additionally adjusting for the effect of smoking, alcohol consumption, and hypertension (OR=5.7, 95% CI 1.7–19.7).
Table 2.
Association between cocaine use and ischemic stroke, by timing and route of intake.
| Cocaine Use | Cases (n=1090) |
Controls (n=1,152) |
Adjusted OR* (95% CI) |
P- value* |
|---|---|---|---|---|
| Timing of last cocaine use† | ||||
| Never users | 784 | 856 | 1.0 (reference) | |
| Years ago | 205 | 235 | 0.9 (0.7, 1.1) | 0.14 |
| Months ago | 36 | 27 | 1.2 (0.7, 2.1) | 0.42 |
| 1–30 days | 39 | 30 | 1.1 (0.7, 1.9) | 0.65 |
| Within 24 hours (acute users) | 26 | 4 | 6.4 (2.2, 18.6) | <0.001 |
| Route of cocaine use | ||||
| Never users | 784 | 856 | 1.0 (reference) | |
| Smoke | 134 | 102 | 1.2 (0.9, 1.6) | 0.22 |
| Inhale | 204 | 225 | 0.9 (0.7, 1.1) | 0.24 |
| Inject | 22 | 15 | 1.3 (0.7, 2.6) | 0.40 |
| Route of cocaine use among acute users (within 24 hours) |
||||
| Never | 784 | 856 | 1.0 (reference) | |
| Smoke | 16 | 2 | 7.9 (1.8, 35.0) | 0.006 |
| Inhale | 8 | 2 | 3.5 (0.7, 16.9) | 0.11 |
| Inject | 2 | 0 | NA | NA |
| Frequency of intake in the past year† | ||||
| Median (times per week) | 1.23 | 0.47 | ||
| Infrequent users, % | 36 (3.3) | 38 (3.3) | 0.9 (0.6, 1.5) | 0.81 |
| Frequent users, % | 65 (6.0) | 23 (2.0) | 2.61 (1.60, 4.27) | <0.001 |
| Frequency of intake in the past year, excluding acute users‡ |
||||
| Median (times per week) | 1.00 | 0.47 | ||
| Infrequent users, % | 31 (2.9) | 37 (3.2) | 0.8 (0.5, 1.4) | 0.47 |
| Frequent users, % | 44 (4.1) | 20 (1.7) | 1.9 (1.1, 3.3) | 0.02 |
OR (and p-value) was adjusted for age, gender and ethnicity. All analyses were calculated using individuals who had never used cocaine as reference group.
Mutually exclusive categories;
Infrequent users were defined as once/week or less; frequent users were defined as cocaine use more than once/week.
The odds ratio for acute cocaine use was higher for the initial study period where the reference date for controls was the date of the interview (% of acute users cases vs. controls: 5.2% vs. 0%; OR=19.1, Fisher’s exact P<0.001) than that for the last two study periods (% of acute users in cases vs. controls: 2.6% vs. 0.7%; OR = 3.6, P=0.02) where reference date for controls was the same day of the week as the stroke occurrence of the matched case. Restricting the analysis to the last two study periods and adjusting for age, gender and race, the association between acute cocaine use and risk of IS remained statistically significant (OR=3.3, 95% CI=1.1–10.1). Additional adjustment for current smoking, alcohol consumption and hypertension did not reduce the point estimate for the association but further widened the confidence interval with the loss of statistical significance (OR=3.5, 95% CI=0.9–12.6).
Table 3 shows the agreement between self-reported cocaine use within 30 days and toxicology results among a subset of cases. A total of 373 stroke cases underwent toxicology screening at the time of hospital admission and, of these, 46 (12.3%) tested positive for cocaine use. The Kappa value between self-reported acute cocaine use and results from toxicology screening was 0.65 (S.E. 0.06), indicating moderate agreement between the two approaches.
Table 3.
Agreement between self-reported cocaine use and toxicology results among cases
| Self-reported cocaine use within 30 days | ||||
|---|---|---|---|---|
| Yes | No | Total | ||
| Toxicology result | Positive | 34 | 12 | 46 |
| Negative | 18 | 309 | 327 | |
| Total | 52 | 321 | 373 | |
Clinical characteristics of 26 stroke patients with acute cocaine use
Supplemental Table I summarizes the demographic characteristics, risk factors, and information on the cocaine exposure for the 26 IS stroke cases with self-reported acute cocaine use, grouped by probable stroke mechanism. Fifteen cases were female and 21 were black, with a mean age of 39.8 years. Stroke risk factors were present in all patients, including tobacco use, hypertension, hyperlipidemia, diabetes and MI. A history of tobacco use was reported in 25 cases and 24 cases were current smokers. Twelve patients also reported concurrent use of other illicit drug within 24 hours prior to stroke onset, including marijuana and heroin, but none of them reported using other vasoactive drugs. Probable stroke mechanism was determined based on clinical data without consideration of cocaine exposure. Of the 26 cases, 7 had a strong cardiac source of embolism, 3 were cryptogenic strokes in multiple vascular territories, 9 were cryptogenic strokes in a single vascular territory, 6 were lacunar strokes, and 1 was a carotid dissection. The 7 cases with a strong cardiac source of embolism included 3 with poor ventricular function, 2 with endocarditis, 1 with acute myocardial infarction, and 1 with a mobile aortic mass.
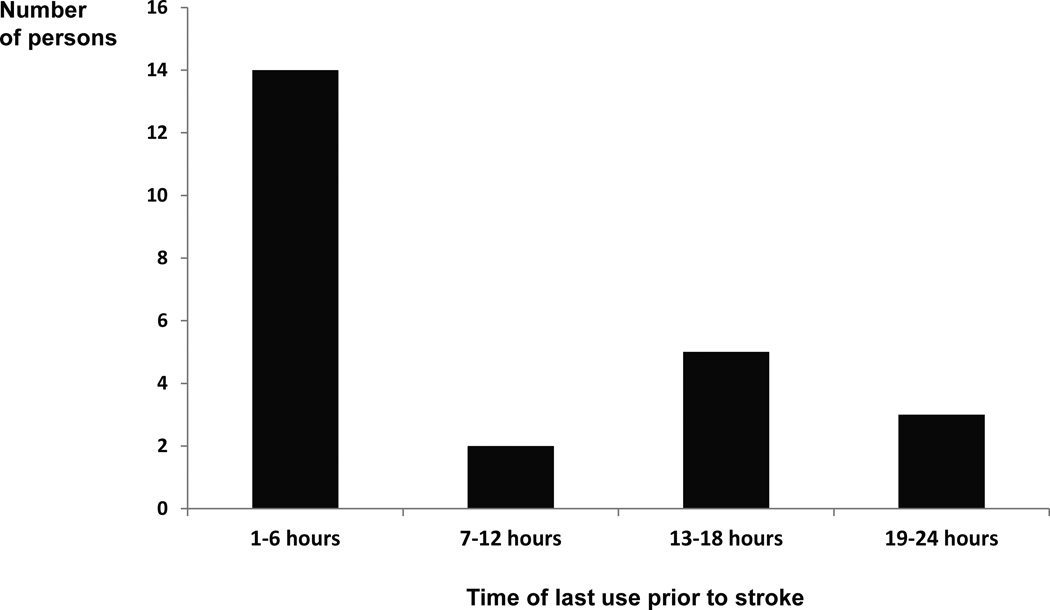
Figure 2 summarizes results from the Supplemental Table I by showing the timing of last cocaine use for the 24 patients who reported use within 24 hours (2 cases without specific timing, in hours, were excluded). Fourteen (54%) of these 26 stroke patients reported cocaine use within 6 hours prior to the onset of stroke.
Figure 2.
Timing of last cocaine use for the 24 stroke patients with self-reported acute cocaine use*
*Two stroke cases who reported acute cocaine use without specific timing (in hours) of last use were excluded from the graph
DISCUSSION
Our study, including more than 1,000 adjudicated young stroke cases, is one of the largest case-control studies to date examining the association of cocaine use and risk of ischemic stroke in young adults. Compared to those who had never used cocaine, those who reported acute cocaine use prior to the study reference time had a 5.7-fold increase in the odds of stroke after adjusting for other stroke risk factors. Furthermore, among the 26 stroke patients with acute cocaine use, the majority reported cocaine use within 6 hours prior to stroke onset and the most commonly used route of drug utilization was smoking (“crack”). In contrast to acute use, use of cocaine months or years ago was not associated with increased risk of stroke.
Cocaine has multiple effects that could predispose to ischemic stroke9. At lower cocaine doses, enhanced sympathetic activity due to inhibition of catecholamine reuptake at sympathetic nerve terminals predominates, leading to hypertension and vasoconstriction. At higher doses, cocaine blocks sodium and potassium channels, leading to depressed myocardial contractility and ventricular arrhythmias. Cocaine also induces a prothrombotic state9. Prior case series10,11 of ischemic stroke among cocaine users of all ages that found atherosclerosis or small vessel disease to be the predominant etiology. In contrast, we found cardiogenic etiologies or cryptogenic nonlacunar stroke to be the most common ischemic stroke types. This is not surprising since cardiogenic or cryptogenic nonlacunar stroke is also the most common etiology in general among young-onset ischemic stroke in the Baltimore-Washington region 12.
In one of the earliest studies, Kaku et al reported an adjusted odds ratio of 49.4 (95% CI 6.4–379.0) for illicit drug abuse and stroke risk based on a chart review study of 214 matched young adult case-control pairs from San Francisco General Hospital3. However, the analysis included illicit drugs other than cocaine, and aggregated intracerebral and subarachnoid hemorrhage with ischemic stroke. Petitti et al reported an adjusted odds ratio of 13.9 (95%CI 2.8–69.4) for cocaine use in the week before the index date in 347 cases of ischemic or hemorrhagic stroke and 1,021 controls within the Kaiser Permanente Medical Care Program of California4. Adjusted odds ratios were similar for cocaine as a paste or powder and smoked cocaine. The authors did report the odds ratio for use of either cocaine and/or amphetamine as 9.6 (95% CI 2.7–33.5) for hemorrhagic stroke and 4.5 (95% CI 0.9–21.6) for ischemic stroke. However, they did not report the specific association of cocaine use with ischemic stroke. Qureshi et al reported that crack cocaine use, either at any time or acute use, was not associated with stroke or cerebral infarction among a small sample of 144 cases and 147 controls from Grady Memorial Hospital in Atlanta7. However, this discordant result may be due to several reasons: the cocaine exposure was based on chart review, a high percentage of cases and controls had missing information on cocaine use, and the controls were hospitalized patients who may not have been representative of the non-stroke population since they had a higher prevalence of smoking and diabetes than the cases. Other studies of cocaine and stroke risk were based on administrative datasets and lacked information on the timing of cocaine use in relationship to the index stroke5–6.
Nevertheless, there are also limitations to our study. Although our study is substantially larger than previous reports, the sample size, specifically the number of cases and controls with cocaine exposure within 24 hours, was too small to address the possibility of residual confounding with measured risk factors. While we did control for current smoking in past month and any alcohol intake in past year, we were not able to control for amount of use of these substances. This is particularly important for smoking, which is known to have a graded association with risk of stroke in young adults13. The very high prevalence of cocaine use in both cases and controls but a low absolute risk of stroke suggests the possibility that other factors may be necessary to potentiate the risk of cocaine. However, again due to sample size limitations, we were not able to examine the interaction of cocaine use with other vascular risk factors.
The most important limitation of our study relates to information bias between cases and controls regarding self-report of cocaine use. First, in the initial study period, controls were asked to recall drug use in the 24 hours prior to the study visit, and they may have been less likely to take drugs shortly before the study interview. The reference time for the cases was always the time of the stroke. This potential bias was addressed in the last two recruitment periods where controls were asked to recall drug use 24 hours prior to a reference date that is matched to the day of the week of stroke onset of the matched index case. For example, if the control was interviewed on a Wednesday and was matched to a case whose event occurred on a Saturday, the reference date for the control was the previous Saturday. When restricting our analyses to the last two study periods, we still see a significant, albeit smaller, association between cocaine use and stroke risk in the unadjusted model. Point estimates for the association were similar after adjusting for demographic and risk factors, although the fully adjusted model failed to achieve statistical significance. Second, study participants also may have been reluctant to share information regarding illegal drug activity. To maximize truthfulness of responses, we used the “card” approach for obtaining the sensitive information about illicit drug use and also informed subjects of the Federal Confidentiality Certificate, which means that no person, organization or legal entity can acquire information obtained during the interview. There was substantial, but not perfect, agreement between self-report and toxicology screen results in the subset of cases that had this testing for clinical care. While we do not have similar data for our control participants, the most persuasive argument against information bias is the fact that self-report of cocaine use at any time in the past and even in the prior 1–30 days was virtually identical among cases and controls. Cocaine use was associated with stroke only when exposure occurred in the most biologically relevant time period.
In summary, our data provides the strongest evidence to date that acute cocaine use within 24 hours is associated with ischemic stroke in young adults. Since cocaine use may be a contributory factor in stroke risk, probing for recent cocaine use and obtaining a toxicology screen should be considered in the evaluation of stroke in young adults.
Supplementary Material
Acknowledgments
Sources of funding: This work was supported by the Department of Veterans Affairs, the Centers for Disease Control and Prevention, and the National Institutes of Health (R01 NS45012). Dr. Cheng was supported by Department of Veterans Affairs (Career Development Award 1IK2BX001823). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
This paper is dedicated to Michael A. Sloan MD, MS, whose ideas and writings on drug abuse and stroke contributed greatly to this project.
Footnotes
Online Data Supplement:
Supplemental Table I - Clinical characteristics of 26 IS patients with symptoms occurring within 24 hours of cocaine use. Grouped by probable stroke mechanism
Illicit Drug Use Questionnaire
Disclosures. None
REFERENCES
- 1.de los Ríos F, Kleindorfer DO, Khoury J, Broderick JP, Moomaw CJ, Adeoye O, et al. Trends in substance abuse preceding stroke among young adults: a population-based study. Stroke. 2012;43:3179–3183. doi: 10.1161/STROKEAHA.112.667808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levine SR, Brust JCM, Futrell N, Ho K-L, Blake D, Millikan CH, et al. Cerebrovascular complications of the use of the crack form of alkaloidal cocaine. New England Journal of Medicine. 1990;323:699–704. doi: 10.1056/NEJM199009133231102. [DOI] [PubMed] [Google Scholar]
- 3.Kaku DA, Lowenstein DH. Emergence of recreational drug abuse as a major risk factor for stroke in young adults. Annals of Internal Medicine. 1990;113:821–827. doi: 10.7326/0003-4819-113-11-821. [DOI] [PubMed] [Google Scholar]
- 4.Petitti DB, Sidney S, Quesenberry C, Bernstein A. Stroke and cocaine or amphetamine use. Epidemiology. 1998;9:596–600. [PubMed] [Google Scholar]
- 5.Westover AN, McBride S, Haley RW. Stroke in young adults who abuse amphetamines or cocaine: A population-based study of hospitalized patients. Archives of General Psychiatry. 2007;64:495–502. doi: 10.1001/archpsyc.64.4.495. [DOI] [PubMed] [Google Scholar]
- 6.Qureshi AI, Suri MFK, Guterman LR, Hopkins LN. Cocaine use and the likelihood of nonfatal myocardial infarction and stroke: Data from the third national health and nutrition examination survey. Circulation. 2001;103:502–506. doi: 10.1161/01.cir.103.4.502. [DOI] [PubMed] [Google Scholar]
- 7.Qureshi AI, Akbar MS, Czander E, Safdar K, Janssen RS, Frankel MR. Crack cocaine use and stroke in young patients. Neurology. 1997;48:341–345. doi: 10.1212/wnl.48.2.341. [DOI] [PubMed] [Google Scholar]
- 8.Hamedani AG, Cole JW, Cheng Y, Sparks MJ, O’Connell JR, Stine OC, et al. Factor V Leiden and ischemic stroke risk: the Genetics of EarlyOnset Stroke (GEOS) study. J Stroke Cerebrovasc Dis. 2013;22:419–423. doi: 10.1016/j.jstrokecerebrovasdis.2011.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwartz BG, Rezkallal S, Kloner RA. Cardiovascular effects of cocaine. Circulation. 2010;122:2558–2569. doi: 10.1161/CIRCULATIONAHA.110.940569. [DOI] [PubMed] [Google Scholar]
- 10.Toosi S, Hess CP, Hills NK, Josephson SA. Neurovascular complications of cocaine use at a tertiary stroke center. Journal of Stroke and Cerebrovascular Diseases. 2010;19:273–278. doi: 10.1016/j.jstrokecerebrovasdis.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Bhattacharya P, Taraman S, Shakar L, Chaturvedi S, Madhavan R. Clinical profiles, complications, and disability in cocaine-related ischemic stroke. Journal of Stroke and Cerebrovascular Diseases. 2011;20:443–449. doi: 10.1016/j.jstrokecerebrovasdis.2010.02.017. [DOI] [PubMed] [Google Scholar]
- 12.Sloan MA, Kittner SJ, Feeser BR, Gardner J, Epstein A, Wozniak MA, et al. Illicit drug-associated ischemic stroke in the Baltimore-Washington Young Stroke Study. Neurology. 1998;50:1688–1693. doi: 10.1212/wnl.50.6.1688. [DOI] [PubMed] [Google Scholar]
- 13.Bhat VM, 1, Cole JW, Sorkin JD, Wozniak MA, Malarcher AM, Giles WH, Stern BJ, Kittner SJ. Dose-response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke. 2008;39:2439–2443. doi: 10.1161/STROKEAHA.107.510073. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.