Abstract
Three-dimensional printing (3DP) is one of the latest tools in the armamentarium of the modern spine surgeon. The yearning to be more precise and reliable whilst operating on the spine has led to an interest in this technology which has claimed to achieve these goals. 3D printing has been used pre-operatively for surgical planning and for resident or patient education. It has also found its way to the operation theatre where it is used to fabricate customized surgical tools or patient-specific implants. Several authors have highlighted significant benefits when 3D printing is used for specific indications in spine surgery. Novel applications of this technology in spine surgery have also been described and though still in a nascent stage, these are important for this technology to sustain itself in the future. However, major limitations have also come to light with this technology in use. This article seeks to review the current status and applications of 3D printing in spinal surgery and its major drawbacks while briefly describing the essentials of the technology. It is imperative that the modern spine surgeon knows about this important innovation and when and how it can be applied to improve surgical outcomes.
Keywords: Additive manufacturing, Patient-specific implants, Rapid prototyping, Spine surgery, Three-dimensional printing
1. Introduction
Surgical practice has evolved over the last few decades to become less invasive, more precise and safer without compromising on the surgical time. From the use of minimally invasive techniques to the use of navigation, from the development of safer approaches to the use of hi-tech simulators in surgical training – new innovations have continuously enhanced and empowered the modern surgeon. The past few years have seen tremendous advances in medical imaging and bioengineering, which together have fathered a new child in the form of three dimensional printing (3DP) – the latest innovation in modern surgical practice. The dramatic evolution of medical imaging has seen it become less invasive and more informative at the same time. High-resolution three-dimensional image data can be acquired in a very short time. This data can be processed by various softwares to enable three-dimensional visualization and multi-planar reformation, which serve as a template for its eventual use in 3DP.
Arguably, the sectors most influenced by the advent of 3DP technology have been cranial and spine surgery. Apart from dealing with degenerative spine conditions, spine surgeons need to engage in complex surgical procedures to treat various congenital and idiopathic spinal deformities. The anatomy of the spine and its close relation to vital neurovascular structures makes it unique and poses inherent surgical challenges when dealing with complex deformities or spinal tumours. Any technique which aids in surgical planning and improves the procedural accuracy in such situations would certainly be welcome.
3DP is essentially a manufacturing method in which objects are made by fusing or depositing materials—such as metal, plastic, powders, ceramics, liquids, or even living cells—in layers to create a 3D object. This process has also been referred to as rapid prototyping (RP), additive manufacturing (AM) or solid free-form technology (SFF).1 The purpose of this review is to familiarize the reader with the technology of 3DP, discuss its varied applications in spine surgery, outline its limitations and shed light on the future directions of this technology in spine surgery.
2. Three dimensional printing: a brief background
Charles Hull is credited with the first use of the 3DP technology (which he called ‘stereolithography’) in the early 1980s.2 Hull, who possesses a bachelor's degree in engineering physics, later went on to establish the company 3D Systems which developed the world's first 3D printer calling it a ‘stereolithography apparatus’.1 Inspite of technological advances since then, the essential principles of 3DP have largely remained the same. In the early stage of design, a digital 3D model is ‘sliced’ into two-dimensional (2D) sections akin to the axial sections of computerized tomography (CT) or magnetic resonance imaging (MRI) data. Each ‘slice’ is then physically re-created by a 3D printer, with a chosen material being laid down layer by layer – culminating into a single solid model, once enough of these ‘slices’ have been created and fused together. There are three commonly used methods of adding the material in layers3:
-
i)
Fused deposition modelling (FDM) is where layers are made by depositing a heat-softened polymer by a computer controlled extrusion nozzle. Most economical consumer printers use this technique.
-
ii)
Selective laser sintering (SLS) involves a focussed energy source (such as an electron beam or a laser) acting upon a fine powder bed of varied materials which may include nylon, titanium and stainless steel. The shape of a 2D slice is traced out, and the geometry of each layer is created. Simultaneous melting and fusing of these areas is then done.
-
iii)
Stereolithography (SLA) uses a light curable resin, on which an optical light energy source works. Chosen areas on the surface of the liquid are solidified. Gradual descent of the floor of the fluid container increases the depth of material. Successive layers of resin are cured on top of each other as the model grows and achieves its final form.
While FDM 3D printers are fast and economical, SLS and SLA printers are the benchmark in medical applications of 3DP technology.4 In addition to being more accurate, they also allow the use of materials which can withstand common sterilization procedures used prior to surgery whereas FDM printers typically use materials with a low melting point. However, on the downside, they require significant training and technical knowledge prior to use.
3. Applications in spine surgery
In a recent systematic literature review, the three largest medical literature databases were screened for case series in English language describing the use of 3DP in surgical applications. A substantial 7.46% of the total papers on the use of 3DP for any surgical domain were dedicated to its applications in spine surgery.5 D'Urso et al. were the first to describe the use of 3DP in spine surgery in their paper on spinal biomodelling in 1999.6 Currently, the application of 3DP in spine surgery can be broadly categorized into three areas: i) use of 3D printed anatomical models for training or pre-operative surgical planning ii) creation of patient-specific surgical instruments such as pedicle screw drill-guides or jigs and iii) printing of customized implants tailor-made to the surgeon's needs. It is interesting that while most papers in the earlier half of the previous decade elaborated the use of 3DP for creating models for pre-operative surgical planning – in the last 5 years, these have given way to case reports and publications involving the use of 3D printed instruments or implants. This change from a more simple and straightforward application to a more nuanced and technically specific application is suggestive of how 3DP technology has progressed by leaps and bounds. We briefly outline the use of 3DP in each of the three areas of focus enlisted above.
3.1. Pre-operative planning using anatomical models
Spine surgeons dealing with scoliosis are familiar with many of the inherent problems of these complex deformities encountered intra-operatively. Vertebral rotation, absent or dysmorphic pedicles and segmentation anomalies are all components of scoliotic spines and distort the anatomical landmarks for pedicle insertion. Current imaging modalities like CT scans or MRI have often been found to be inadequate. 3D printed anatomical models provide the ‘fourth’ dimension of tactile feedback to the surgeons which can help them anticipate the technical challenges that may be encountered intra-operatively. Almost as a testament to the popular adage – ‘the more you sweat in practice, the less you bleed in war’ - surgeons can practically carry out the entire surgical procedure and make a note of the technical challenges and the improvisations needed, before the actual surgery takes place.
Various authors have published their experience with these anatomical models for complex spine surgery. Izatt et al.7 used a detailed biomodel utility survey and discovered from the surgeons' feedback that there was better visualization of anatomical details on the biomodel as compared to other imaging modalities in 65% of cases which were a mix of spinal deformity and tumour patients. Mizutani et al.8 also reported positively in their experience with full-scale 3D models of rheumatoid cervical spines. Mao et al.9 used computer-designed polystyrene models in 16 cases of complex severe spinal deformity and claimed to have more accurate morphological information from the models. In another retrospective study, the authors reported that the use of 3D printed models for surgical planning in thoracic scoliosis surgery resulted in shorter operative times and lesser blood loss, but had no effect on the complication rate, the screw misplacement rate or the length of hospital stay.10 These findings were echoed by Li et al.11 in a study, wherein they assessed the effectiveness of 3-D printing technology in revision lumbar discectomy cases. Xiao12 and Kim,13 in separate papers, have also highlighted the application of 3DP in assisting surgical resection of bone tumours. More recently, the use of 3DP has also been reported in the field of minimally invasive spine surgery (MISS) although there are limitations to its widespread implementation.14 Zhao et al. have reported on the use of 3D biomodelling-assisted MISS to deal with 13 cases of thoracic ossification of ligamentum flavum. Biomodels of the patients' spinal anatomy were used to determine the angle of insertion of the percutaneous tubular retractors, and also to guide the surgeon towards the location and size of the bony spaces.15
Another useful application of 3D printed anatomical models is in resident training and patient education.16 A tangible and concrete representation of the pathoanatomy can act as a valuable aid in explaining the patient regarding his/her condition and what the proposed surgical procedure intends to achieve. As much as 25% higher patient informed consent scores were obtained when a biomodel was used in comparison to pre-operative image demonstration to explain and educate the patient regarding the nature of the condition and the treatment offered.17 3D printed models can be used in lieu of cadavers for training and education of residents. Such models are free of several concerns surrounding cadavers which include lack of availability, health and safety issues and other medicolegal or ethical hassles. These models can also be easily customized to better simulate surgical challenges such as those seen with complex spinal deformities.18
3.2. Surgical tools and guides
Pedicle screws are universally the most frequently used fixation technique in spinal surgery. The close proximity of neural structures makes pedicle screw insertion a dangerous proposition though in the hands of most experienced surgeons, the rate of neurological complications is extremely low. However, inserting pedicle screws in the cervical spine or in a scoliotic deformity, particularly in paediatric patients, is certainly more challenging and prone to pedicle wall breeches/perforations. Most surgeons still use a fluoroscopy-guided free-hand technique – however, this technique is less accurate and carries a much greater risk of radiation exposure for the surgeon. Computer-assisted navigation is another innovation used worldwide for pedicle screw insertion in these ‘difficult’ situations. However navigation equipment comes with its own baggage of limitations – it is expensive to procure and maintain, needs a substantial learning curve, needs additional trained personnel with technical know-how and increases the operative time due to bone registration requirements.19 3D printed screw guides serve as a low-cost, accurate and simple alternative to both these techniques. The creation of anatomy-based guides requires the prior creation of a 3D model of each target vertebra. The guide template is then reverse-engineered to exactly reciprocate the posterior elements of the vertebra where it can sit perfectly when applied during surgery. The screw insertion points and trajectories are validated in the lab pre-operatively and the same are used for screw insertion during surgery.
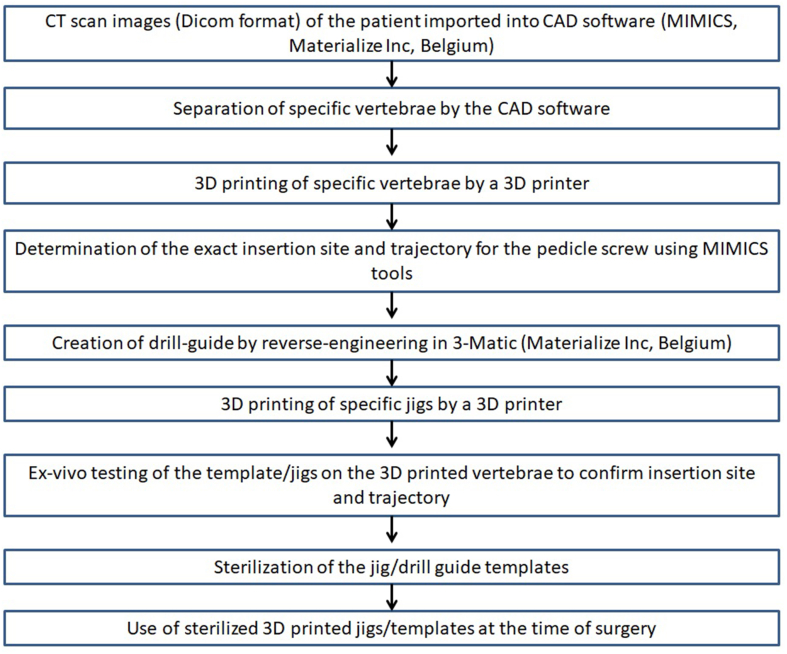
Various authors, including ourselves, have described the use of 3D printed screw guides for inserting screws in cervical spine20,21,22 complex spinal deformity such as scoliosis23,24 and in revision surgeries where anatomical landmarks are more likely to be distorted.25 A number of benefits of using these 3D printed guides have been described such as decreased operative time, lesser blood loss, greater accuracy, lower screw misplacement rate, simplicity of use, decreased radiation exposure and relative cost-effectiveness compared to the other techniques.20,21,22,24,25 Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6 are illustrative of how the 3DP technology is used to fabricate patient-specific pedicle screw drill guides. The process of preparation of a patient-specific drill-guide template for inserting pedicle screws in the authors' own institute in shown in a flowchart (Fig. 7). A preference of titanium templates over their plastic counterparts has been advocated - with the argument that when in contact with high-speed drills or other surgical equipment, the plastic would likely produce debris which can collect in the wound and be a potential source of infection.26 The titanium templates have the added advantage of being stronger and more rigid, which makes them more accurate and reliable. However, these advantages come at a substantial cost because the titanium templates are costly compared to plastic.
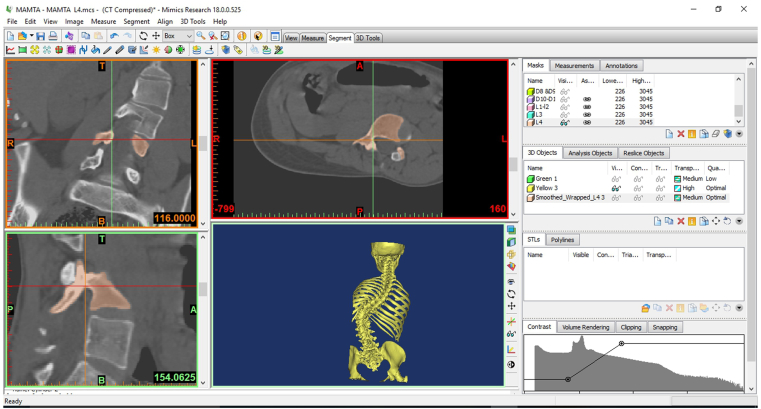
Fig. 1.
Import of images and creation of a digital 3D model. Individual vertebrae are subsequently separated.
Fig. 2.
Marking the insertion points and trajectories of each individual vertebrae on the software.
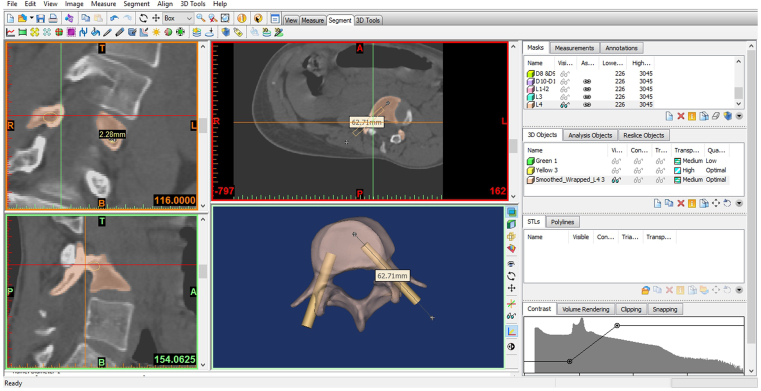
Fig. 3.
Creation of a reciprocal vertebral guide template for inserting screws.
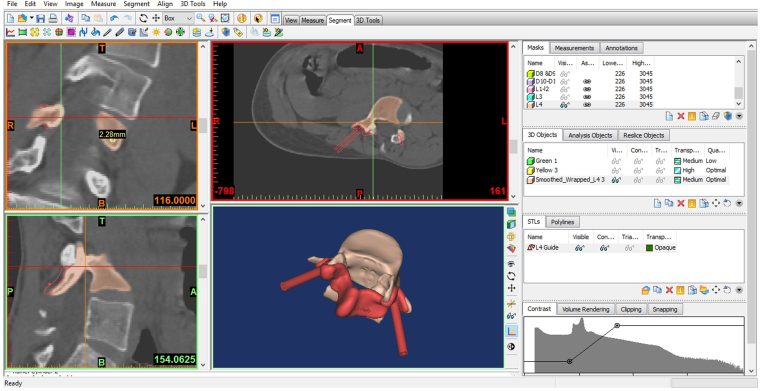
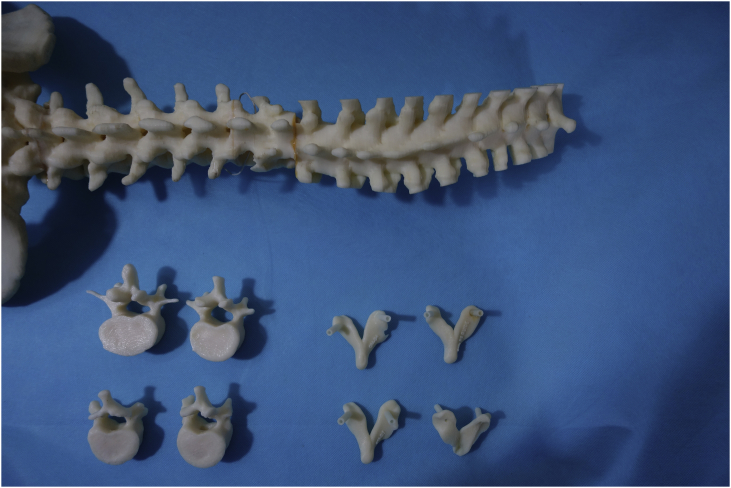
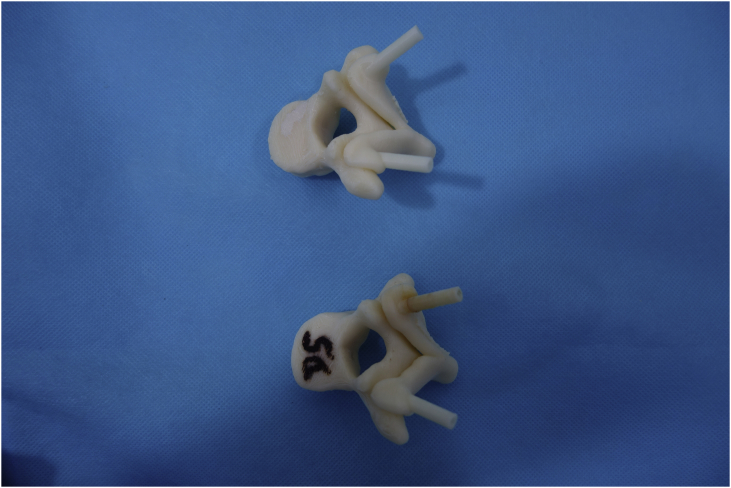
Fig. 4.
Individual 3D printed vertebrae and their corresponding guide templates.
Fig. 5.
Jigs and 3D printed vertebrae assembled ex-vivo to check and validate the insertion point and trajectory.
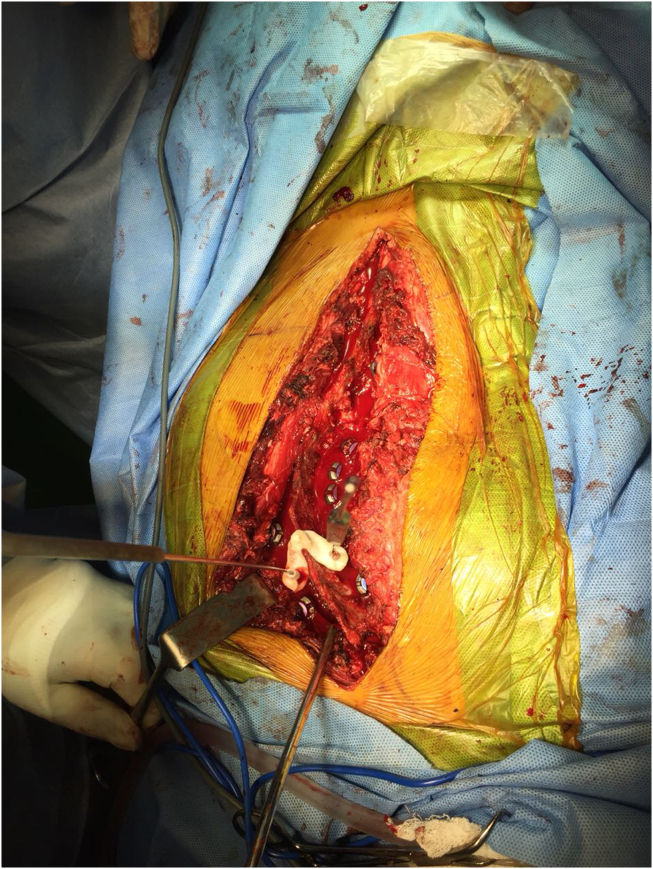
Fig. 6.
Drilling pedicle screw trajectory using a 3D printed jig during surgery.
Fig. 7.
Flowchart denoting the process/methodology of creating a 3D printed drill-guide template to aid pedicle screw insertion using 3DP technology.
Apart from its application in creation of 3D printed pedicle screw guide templates, 3DP has also been used in a cadaveric study to make drill guide templates for trough preparation in expansive open-door cervical laminoplasty.27 It has been claimed that a rapid prototyping drill template could guide the surgeon towards appropriate trough position and bone removal in this procedure.
3.3. Customized implants
3DP has also been used to manufacture customized, patient-specific implants that are left in the patient's body at the end of the surgery. These are used in highly complex surgeries in anatomically distinct and unique regions, where a customized implant will provide a perfect fit and hence, more even loads and superior osseo-integration. The most common application of these customized implants has been in spine tumour surgery where these are used to fill in for the resected portion of the spine with most studies reporting positive outcomes.28,29,30 Though rarely reported, such customized 3D printed implants have also found to be useful in other conditions. Phan used a customized 3D printed implant for C1/C2 fusion is a 65 year old female with severe facet arthropathy.31 More recently, the use of 3D printed vertebral body replacement (VBR) has been reported for cervical spondylotic myelopathy.32 After undergoing anterior cervical corpectomy and decompression, 3D printed customized VBRs made of polyethyletherketone (PEEK) were implanted in 6 patients with degenerative cervical spine disease. Another popular application of 3DP is in designing interbody cages, where incorporation of both a porosity and surface roughness akin to natural bone has been associated with bone growth activity.33 The incremental expansion of 3DP has touched spinal braces as well. As the braces can be completely customized based on the patient specific body and shape as well as their corrective requirements, these braces are proving to be more efficient, comfortable and acceptable for the patient.34
3.4. Novel applications
Many other uses of 3DP in spine surgery have been proposed which are still in a nascent investigative stage and have not yet found clinical application. Artificial intervertebral discs based on tissue-engineered biodegradable scaffolds have been created which aims to replicate the viscoelastic nature of the disc.35,36 If these early reports of experimental success can be translated to clinical use, it would indeed revolutionize the treatment of degenerative disc disease. Tissue-engineering is also being investigated for regenerating soft tissues by delivering suitable matrix tissue and living cells using the 3DP technology.37 3D printed drug delivery systems are being investigated which can allow creation of implantable drug-delivery devices with complex drug release profiles. Many novel dosage forms, such as: microcapsules, nanosuspensions, hyaluronan-based synthetic extracellular matrices, mesoporous bioactive glass scaffolds, antibiotic printed micropatterns and multilayered drug delivery devices have been synthesized using 3D printers.38 A Chinese group has successfully tested a novel drug delivery system for use in spinal tuberculosis in a laboratory setting. Anti-tubercular drugs were mixed with Poly-DL-lactide (PDLLA) and nano-hydroxyapatite (nHA) and a unique porous 3D scaffold was created using 3DP technology. Such a scaffold may be used individually or in combination with titanium mesh during reconstruction of defects in spinal stabilization surgery in spinal tuberculosis.39
4. Pitfalls and concerns
It is not difficult to envisage that 3DP has its own share of pitfalls and concerns when you consider the fact that inspite of being such a promising technology; it can hardly claim to be universally adopted. We summarize below the major limitations of this technology reported in literature:
-
•
The time required to plan and create the 3D model has been viewed as a deterrent in many studies. Only the 3D printing process itself, including creation of the CAD model on the software, typically takes between 10 and 12 h. This renders the 3DP technology impractical to use in emergency cases and in hospitals with high output and turnover.40 Although 3DP leads to a substantial increase in pre-operative time consumption, it actually leads to a decrease in the intra-operative time. It has been surmised in one of the reviews on 3D spine systems that 10 min saved in the operating room is monetarily equivalent to about 1 h spent in pre-operative preparation.40
-
•
Costs of having a 3D printing facility are considerable for any hospital, let alone one where complex spine cases are rarely operated. The costs include purchase of a computer-aided designing (CAD) software, camera, purchase and maintenance of a 3D printer and other ancillary expenses. Depending on the set-up, rough estimates of INR 10000–40000 have been reported per patient.41 Even in western countries, where healthcare expenses are covered by insurance companies – these additional costs are usually not covered under insurance, making this technology cost-prohibitive for the patient. Usually, a trained professional with expertise in using the CAD software is also required.
-
•
Inability to simultaneously simulate both bone and soft tissue by a single material is a major drawback of 3D printed anatomical models which is particularly relevant if these are to be preferred over cadavers for resident training. Multimaterial 3D printers have now been described which can greatly improve the training experience.42 Intra-operatively soft tissues have to be stripped off the posterior elements to enable a tight fit of the screw guide template.24
-
•
Currently, the United States Food and Drug Administration (FDA) has been approving 3D printed implants or surgical tools on a case-by-case basis and as such these do not enjoy any blanket clearance from the regulatory authority. Thus, the quality of the biomaterial used to manufacture 3D printed tools or implants is still questionable. In the United Kingdom, the National Institute for Health and Care Excellence (NICE) have also yet to determine their stance on 3DP technology. Data regarding the long-term safety of 3D printed implants is unavailable as these are in use only since the last decade.
5. Conclusion
-
•
3D printing technology is an exciting innovation with key applications in spinal surgery
-
•
Use of anatomical models for pre-operative planning and resident or patient education, fabricating surgical tools such as screw guides and creation of customized implants are some of the applications of 3DP technology in spinal surgery reported in literature
-
•
Long production times and high costs incurred along with the limited nature of its applications in spinal surgery has prevented 3DP technology from being widely used
-
•
Breakthrough developments in bioengineering to make the technology more affordable, faster and more accessible are needed to ensure the growth and expansion of 3DP technology in the future
-
•
Presently, the use of 3DP technology is limited exclusively to a niche of complex surgeries like paediatric spinal deformities, revision surgeries and spinal tumour surgeries with anatomically challenging reconstructions needed after tumour excision. The technology has scarce use or application in routine spine care.
Conflicts of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Bhavuk Garg, Email: drbhavukgarg@gmail.com.
Nishank Mehta, Email: mehta.nishank@gmail.com.
References
- 1.Gross B.C., Erkal J.L., Lockwood S.Y., Chen C., Spence D.M. ACS Publications; 2014. Evaluation of 3D Printing and its Potential Impact on Biotechnology and the Chemical Sciences. [DOI] [PubMed] [Google Scholar]
- 2.Hull C., Feygin M., Baron Y. Rapid prototyping: current technology and future potential. Rapid Prototyp J. 1995;1(1):11–19. [Google Scholar]
- 3.Malik H.H., Darwood A.R., Shaunak S. Three-dimensional printing in surgery: a review of current surgical applications. J Surg Res. 2015;199(2):512–522. doi: 10.1016/j.jss.2015.06.051. [DOI] [PubMed] [Google Scholar]
- 4.Liu Y., Xu L., Zhu H., Liu S.S.-Y. Technical procedures for template-guided surgery for mandibular reconstruction based on digital design and manufacturing. Biomed Eng Online. 2014;13(1):63. doi: 10.1186/1475-925X-13-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tack P., Victor J., Gemmel P., Annemans L. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016;15(1):115. doi: 10.1186/s12938-016-0236-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Urso P.S., Askin G., Earwaker J.S. Spinal Biomodeling. Spine. 1999;24(12):1247. doi: 10.1097/00007632-199906150-00013. [DOI] [PubMed] [Google Scholar]
- 7.Izatt M.T., Thorpe P.L.P.J., Thompson R.G. The use of physical biomodelling in complex spinal surgery. Eur Spine J. 2007;16(9):1507–1518. doi: 10.1007/s00586-006-0289-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mizutani J., Matsubara T., Fukuoka M. Application of full-scale three-dimensional models in patients with rheumatoid cervical spine. Eur Spine J. 2008;17(5):644–649. doi: 10.1007/s00586-008-0611-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mao K., Wang Y., Xiao S. Clinical application of computer-designed polystyrene models in complex severe spinal deformities: a pilot study. Eur Spine J. 2010;19(5):797–802. doi: 10.1007/s00586-010-1359-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang M., Li C., Li Y. Application of 3D rapid prototyping technology in posterior corrective surgery for lenke 1 adolescent idiopathic scoliosis patients. Medicine (Baltim) 2015;94(8) doi: 10.1097/MD.0000000000000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li C., Yang M., Xie Y. Application of the polystyrene model made by 3-D printing rapid prototyping technology for operation planning in revision lumbar discectomy. J Orthop Sci. 2015;20(3):475–480. doi: 10.1007/s00776-015-0706-8. [DOI] [PubMed] [Google Scholar]
- 12.Xiao J., Huang W., Yang X. En bloc resection of primary malignant bone tumor in the cervical spine based on 3-dimensional printing technology. Orthop Surg. 2016;8(2):171–178. doi: 10.1111/os.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim M.P., Ta A.H., Ellsworth W.A., Marco R.A., Gaur P., Miller J.S. Three dimensional model for surgical planning in resection of thoracic tumors. Int J Surg Case Rep. 2015;16:127–129. doi: 10.1016/j.ijscr.2015.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsu MR, Haleem MS, Hsu W. 3D printing applications in minimally invasive spine surgery. Minim. Invasive Surg. . doi:10.1155/2018/4760769. [DOI] [PMC free article] [PubMed]
- 15.Zhao W., Shen C., Cai R. Minimally invasive surgery for resection of ossification of the ligamentum flavum in the thoracic spine. Videosurg Other Miniinvasive Tech. 2017;12(1):96. doi: 10.5114/wiitm.2017.66473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilcox B., Mobbs R.J., Wu A.-M., Phan K. Systematic review of 3D printing in spinal surgery: the current state of play. J. Spine Surg. 2017;3(3):433. doi: 10.21037/jss.2017.09.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D'Urso P.S., Barker T.M., Earwaker W.J. Stereolithographic biomodelling in cranio-maxillofacial surgery: a prospective trial. J. Cranio-Maxillofacial Surg. 1999;27(1):30–37. doi: 10.1016/s1010-5182(99)80007-9. [DOI] [PubMed] [Google Scholar]
- 18.Rehder R., Abd-El-Barr M., Hooten K., Weinstock P., Madsen J.R., Cohen A.R. The role of simulation in neurosurgery. Child’s Nerv Syst. 2016;32(1):43–54. doi: 10.1007/s00381-015-2923-z. [DOI] [PubMed] [Google Scholar]
- 19.Chen H., Wu D., Yang H., Guo K. Clinical use of 3D printing guide plate in posterior lumbar pedicle screw fixation. Med Sci Mon Int Med J Exp Clin Res: Int Med J Exp Clin Res. 2015;21:3948. doi: 10.12659/MSM.895597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu S., Xu Y.Q., Zhang Y.Z., Xie L., Guo H., Li D.P. A novel computer-assisted drill guide template for placement of C2 laminar screws. Eur Spine J. 2009;18(9):1379. doi: 10.1007/s00586-009-1051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu S., Xu Y.Q., Chen G.P. Efficacy and accuracy of a novel rapid prototyping drill template for cervical pedicle screw placement. Comput Aided Surg. 2011;16(5):240–248. doi: 10.3109/10929088.2011.605173. [DOI] [PubMed] [Google Scholar]
- 22.Deng T., Jiang M., Lei Q., Cai L., Chen L. The accuracy and the safety of individualized 3D printing screws insertion templates for cervical screw insertion. Int J Med Robot Comput Assist Comput Assist Surg. 2016;21(1):143–149. doi: 10.1080/24699322.2016.1236146. [DOI] [PubMed] [Google Scholar]
- 23.Liu K., Zhang Q., Li X. Preliminary application of a multi-level 3D printing drill guide template for pedicle screw placement in severe and rigid scoliosis. Eur Spine J. 2017;26(6):1684–1689. doi: 10.1007/s00586-016-4926-1. [DOI] [PubMed] [Google Scholar]
- 24.Garg B., Gupta M., Singh M., Kalyanasundaram D. Outcome and safety analysis of 3D printed patient specific pedicle screw jigs for complex spinal deformities: a comparative study. Spine J. 2018 May 3 doi: 10.1016/j.spinee.2018.05.001. pii: S1529-9430(18)30200-6. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Otsuki B., Takemoto M., Fujibayashi S., Kimura H., Masamoto K., Matsuda S. Utility of a custom screw insertion guide and a full-scale, color-coded 3D plaster model for guiding safe surgical exposure and screw insertion during spine revision surgery. J Neurosurg Spine. 2016;25(1):94–102. doi: 10.3171/2015.12.SPINE15678. [DOI] [PubMed] [Google Scholar]
- 26.Takemoto M., Fujibayashi S., Ota E. Additive-manufactured patient-specific titanium templates for thoracic pedicle screw placement: novel design with reduced contact area. Eur Spine J. 2016;25(6):1698–1705. doi: 10.1007/s00586-015-3908-z. [DOI] [PubMed] [Google Scholar]
- 27.Rong X., Wang B., Chen H. Use of rapid prototyping drill template for the expansive open door laminoplasty: a cadaveric study. Clin Neurol Neurosurg. 2016;150:13–17. doi: 10.1016/j.clineuro.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 28.Xu N., Wei F., Liu X. Reconstruction of the upper cervical spine using a personalized 3D-printed vertebral body in an adolescent with Ewing sarcoma. Spine. 2016;41(1):E50–E54. doi: 10.1097/BRS.0000000000001179. [DOI] [PubMed] [Google Scholar]
- 29.Choy W.J., Mobbs R.J., Wilcox B., Phan S., Phan K., Sutterlin C.E. Reconstruction of thoracic spine using a personalized 3d-printed vertebral body in adolescent with T9 primary bone tumor. World Neurosurgery. 2017;105 doi: 10.1016/j.wneu.2017.05.133. 1032.e13-1032.e17. [DOI] [PubMed] [Google Scholar]
- 30.Mobbs R.J., Coughlan M., Thompson R., Sutterlin C.E., III, Phan K. The utility of 3D printing for surgical planning and patient-specific implant design for complex spinal pathologies: case report. J Neurosurg Spine. 2017;26(4):513–518. doi: 10.3171/2016.9.SPINE16371. [DOI] [PubMed] [Google Scholar]
- 31.Phan K., Sgro A., Maharaj M.M., D'Urso P., Mobbs R.J. Application of a 3D custom printed patient specific spinal implant for C1/2 arthrodesis. J Spine Surg. 2016;2(4):314–318. doi: 10.21037/jss.2016.12.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amelot A., Colman M., Loret J.-E. Vertebral body replacement using patient-specific three–dimensional-printed polymer implants in cervical spondylotic myelopathy: an encouraging preliminary report. Spine J. 2018;18(5):892–899. doi: 10.1016/j.spinee.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 33.Serra T., Capelli C., Toumpaniari R. Design and fabrication of 3D-printed anatomically shaped lumbar cage for intervertebral disc (IVD) degeneration treatment. Biofabrication. 2016;8(3) doi: 10.1088/1758-5090/8/3/035001. 035001. [DOI] [PubMed] [Google Scholar]
- 34.Weiss H.-R., Kleban A. Development of CAD/CAM based brace models for the treatment of patients with scoliosis-classification based approach versus finite element modelling. Asian Spine Journal. 2015;9(5):661–667. doi: 10.4184/asj.2015.9.5.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whatley B.R., Kuo J., Shuai C., Damon B.J., Wen X. Fabrication of a biomimetic elastic intervertebral disk scaffold using additive manufacturing. Biofabrication. 2011;3(1) doi: 10.1088/1758-5082/3/1/015004. 015004. [DOI] [PubMed] [Google Scholar]
- 36.de Beer N., van der Merwe A. Patient-specific intervertebral disc implants using rapid manufacturing technology. Rapid Prototyp J. 2013;19(2):126–139. [Google Scholar]
- 37.Pati F., Ha D.-H., Jang J., Han H.H., Rhie J.-W., Cho D.-W. Biomimetic 3D tissue printing for soft tissue regeneration. Biomaterials. 2015;62:164–175. doi: 10.1016/j.biomaterials.2015.05.043. [DOI] [PubMed] [Google Scholar]
- 38.Ursan I.D., Chiu L., Pierce A. Three-dimensional drug printing: a structured review. J Am Pharmaceut Assoc. 2013;53(2):136–144. doi: 10.1331/JAPhA.2013.12217. [DOI] [PubMed] [Google Scholar]
- 39.Dong J., Zhang S., Liu H., Li X., Liu Y., Du Y. Taylor & Francis; 2014. Novel Alternative Therapy for Spinal Tuberculosis during Surgery: Reconstructing with Anti-tuberculosis Bioactivity Implants. [DOI] [PubMed] [Google Scholar]
- 40.Martelli N., Serrano C., Brink H van den. Advantages and disadvantages of 3-dimensional printing in surgery: a systematic review. Surgery. 2016;159(6):1485–1500. doi: 10.1016/j.surg.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 41.Murray D.J., Edwards G., Mainprize J.G., Antonyshyn O. Optimizing craniofacial osteotomies: applications of haptic and rapid prototyping technology. J Oral Maxillofac Surg. 2008;66(8):1766–1772. doi: 10.1016/j.joms.2007.08.031. [DOI] [PubMed] [Google Scholar]
- 42.Waran V., Narayanan V., Karuppiah R., Owen S.L., Aziz T. Utility of multimaterial 3D printers in creating models with pathological entities to enhance the training experience of neurosurgeons. J Neurosurg. 2014;120(2):489–492. doi: 10.3171/2013.11.JNS131066. [DOI] [PubMed] [Google Scholar]