Abstract
Objective
To develop an intervention to improve the mental health referral and care process for children referred by primary care providers (PCPs) to community mental health clinics (MHCs) using a community partnered approach.
Design
A Project Working Group (PWG) with representatives from each partner organization met monthly for 6 months.
Setting
Multi-site federally qualified health center (FQHC) and two community MHCs in Los Angeles county.
Participants
26 stakeholders (14 FQHC clinic providers/staff, 8 MHC providers/staff, 4 parents) comprised the PWG.
Data Sources
Qualitative interviews, PWG meeting notes, intervention processes and workflow reports.
Intervention
The PWG reviewed qualitative data from stakeholders (interviews of 7 parents and 13 providers/staff). The PWG met monthly to identify key transition points where access to and coordination of care were likely compromised and to develop solutions.
Results
Three critical transition points and system solutions were identified: 1) Parents refuse initial referral to the MHC due to stigma regarding mental health services. Solution: During initial referral, parents watch a video introducing them to the MHC. 2) Parents don’t complete the MHC’s screening after referral. Solution: A live videoconference session connecting parents at the FQHC with MHC staff ensures completion of the screening and eligibility process. 3) PCPs reject transfer of patients back to primary care for ongoing psychotropic medication management. Solution: Regularly scheduled live videoconferences connect PCPs and MHC providers.
Conclusions
A community partnered approach to care design utilizing telehealth for care coordination between clinics can potentially be used to address key challenges in MHC access for children.
Keywords: Primary Care, Mental Health Care, Coordination, Collaboration
Introduction
Research indicates that 15%-20% of US children suffer from a mental health (MH) disorder, but nearly 80% of those who need MH services don’t receive them.1-4 Among publicly insured children, this unmet need is even more pronounced.4 Medicaid-insured children who require specialty MH care are often referred to community mental health clinics (MHCs) for diagnostic and therapeutic services; however, families often face multiple barriers in accessing these MHCs, including unfamiliarity with the clinic’s screening and enrollment process,5 stigma of attending a MHC,6-8 and clinic location.9 Within primary care clinics, implementation of care models for collaborative care, co-located care, and integrated MH care is often challenged by logistic and financial barriers. Nevertheless, several studies suggest that interventions aimed at creating collaborative care models linking primary care with specialty MH care can improve utilization of behavioral health services and outcomes for children.10-17
The modality of telehealth, using live videoconference sessions, may enhance opportunities for improved access to care and care coordination among primary care and specialty MH providers.18-29 There is some evidence from both adult and pediatric studies to suggest that outcomes related to treatment recommendations,30,31 clinical outcomes,21,31,32 and access to care31 for telehealth encounters may be comparable to in-person clinical encounters.
To address these challenges and capitalize on the use of telehealth, we partnered with a multi-site federally qualified health center (FQHC) and two community MHCs that serve a large population of publicly insured children in Los Angeles, California. When children are referred to MH from this multi-site FQHC, they are largely referred to one of these two MHCs. Together, our objective was to identify key transition points in the referral and care coordination process when MH care access was most likely to be compromised and develop an intervention to address these challenges. Several studies have utilized a structured process to engage communities and clinics to produce comprehensive, site-specific innovative models to address health.33-35 We describe a community-partnered approach to 1) identification of barriers and potential solutions in the referral and care process, and 2) development of a community-based, telehealth-coordinated intervention tailored to the needs of the families served and the existing clinic organizational characteristics.
Our group has used this community-partnered design process in previous studies to partner with clinic stakeholders in clinical delivery design projects aimed at improving care for publicly insured children.33 The core element of this process is a Project Working Group (PWG). The PWG consists of clinic providers, staff, and administration, as well as parents of children served by the clinical entities. During a series of meetings guided by the research team, the PWG outlines the problem in detail, and then develops an intervention to address it. A summary of what is known on the topic and of previously conducted qualitative interviews of stakeholders, provided by the academic research team, helps guide the PWG. The process is based on the principles of community-based participatory research,36 with the “community” defined as the partnered clinic collaborating with the academic research team to improve care delivery. This community-partnered approach to intervention development for clinical care delivery allows for a community-engaged and structured process for intervention design that addresses the needs of stakeholders.
Methods
Our community partners were the multi-site FQHC and two MHCs. The FQHC provides 112,101 primary health care visits for 37,367 children aged 0-18 years annually; 98% of these patients have an annual household income <200% of the federal poverty level and 86% are Latino. The two MHCs are contracted by the County of Los Angeles Department of Mental Health (DMH) to provide MH services to publicly insured children near the geographical area served by six clinical sites of the FQHC.
The purpose of the PWG was to systematically engage the stakeholders in development of a new referral process to enhance FQHC patients’ access to and successful enrollment into MHCs. The PWG included primary care providers (PCPs) from each of the six participating FQHC clinical sites, the FQHC pediatric medical director, the FQHC clinic managers, and parents. Parent representatives were nominated from PCPs and MHC providers; all had gone through the MH referral process at the FQHC. The PWG also included MHC providers and staff, including medical directors, psychiatrists, therapists, and managers. The PWG had 26 members (14 FQHC clinic providers/staff, 8 MHC providers/staff, 4 parents), who met monthly for six meetings from April 2014-September 2014 to develop the intervention.
Our data sources included a summary of stakeholder qualitative interviews, PWG meeting notes, and intervention processes and workflow reports created by the PWG. The qualitative interview data summary was created by the academic team, and all other materials were developed by the PWG during meeting time, and reviewed for accuracy and agreement at a subsequent PWG meeting. The study was approved by the UCLA Institutional Review Board.
At the first PWG meeting, the PWG defined a governance plan and reviewed project goals and objectives. The PWG received a summary of previously collected stakeholder data to assess parent, provider, and staff perspectives (7 parents, 10 FQHC PCPs/staff, and 3 MHC providers/staff) on current processes for MH referrals for the FQHC’s pediatric patients, and perspectives on how to improve it. These data were key to helping the PWG frame future discussions and focus on the problem areas identified by individuals in each organization and by parents who had encountered the referral process; findings are reported elsewhere.5 Briefly, we found that PCPs and parents highlighted challenges at initial referral, and MH providers cited challenges at the time when patients were ready to be transferred back to PCPs for ongoing psychotropic medication management.
The next three meetings focused on identifying problems in the referral and care process, and then creating a telehealth-based referral and care intervention to address these problems. The PWG first outlined each step of their current referral and care process from initial identification of a need for a MH referral by the PCP, to referral and enrollment at the MHC, to treatment, stabilization, and transfer back to primary care. Through discussions at PWG meetings 2-4, the PWG identified areas in the process where access was most likely to be compromised. The PWG created solutions to address the problems at each identified critical transition point in the referral system, with the goal of enhancing access for families in underserved communities (PWG meetings 4-6). The PWG designed solutions to directly address these problems, and when appropriate, incorporated telehealth or videoconferencing technology when it was helpful as a tool to enhance communication and coordination among PCPs, MH care providers, and parents. The PWG included telehealth modality as an available tool in designing the intervention, but was not limited to activities solely related to telehealth. The PWG took these solutions and created the intervention itself, with detailed structures, processes, and workflows.
PWG meetings are planned to continue through implementation, piloting, and then a randomized trial of the developed intervention. PWG decisions were by consensus. Meetings were conducted in English; however, to accommodate monolingual Spanish-speaking parent members, we utilized bilingual research staff to provide real-time interpretation during meetings.
PWG members completed a survey assessing their experiences with the project. A detailed assessment of PWG member experience is beyond the scope of this paper; however, a brief meeting evaluation survey was created for the PWG, and provided at the end of every PWG meeting and asked participants whether: 1) the project purpose and objectives were clearly stated; 2) the meeting time and place were convenient; 3) shared decision-making was used during the meeting; 4) meeting time was used effectively; and 5) they felt satisfied with their participation during the meeting, and satisfied with the meeting generally. Participants could respond strongly disagree, disagree, agree, or strongly agree.
Referral Process
Specialty MH is a carved-out benefit for most publicly insured patients at the FQHC; there are two main DMH clinical partners to which the majority of the patients are referred. Parents receive a MHC referral from their PCP at the FQHC. The referral is then faxed from the primary care clinic to the MHC. The MHC initiates contact with the family via a phone eligibility screening. The parent is called using the phone number provided on the referral form, a case manager from the MHC screening department asks the parent a series of questions regarding insurance coverage, their child’s MH concerns, and other issues. The screener makes an initial determination of eligibility for the family and provides this information to a MHC therapist. The parent is then scheduled for a 2-hour intake visit with the therapist, which serves as the full assessment of MH needs for the child. After this intake visit, patients are enrolled in a therapy program that generally includes behavioral therapy for approximately eight weeks. The therapist then consults with a supervisor about whether the patient needs a referral to a child psychiatrist. If the referral is deemed necessary, the patient is scheduled for an initial assessment with a psychiatrist at the MHC, who prescribes medication if indicated, and continues to see the patient on a regular basis.
Results
Critical Transition Points in the Current Referral Process
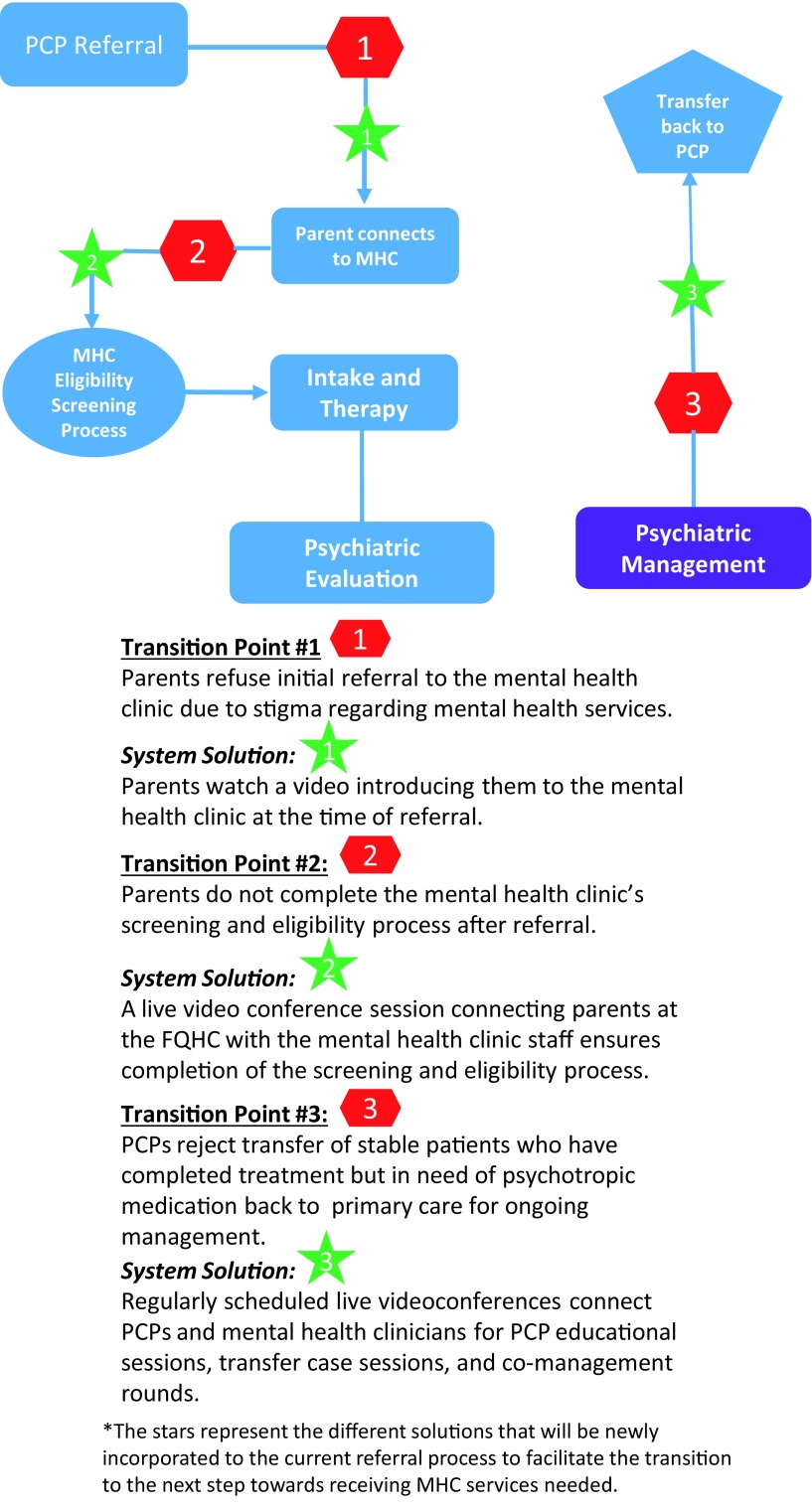
As the PWG outlined each step of the current referral process, it identified critical transition points in which MHC access was most likely to be compromised. The PWG designed the Telehealth-Coordinated Collaborative Care intervention to address the key problems at these critical transition points that could negatively impact patient access and primary care specialty communication and coordination. The identified transition points and accompanying solutions were as follows and are summarized in Figure 1; these were developed by the PWG during their meetings.
Figure 1. Identified critical transition points in current referral process.
Transition Point #1: Parents refuse initial referral to the MH clinic due to stigma regarding MH services.
The initial barrier to a successful referral process was viewed as occurring at the time of referral to the MHC from the PCP. During a primary care visit, the FQHC PCP may recognize a MH need and inform the parent that a referral will be made to the MHC. For a number of reasons identified by PWG members, families may decide not to pursue MH services at this initial referral point. Parents on the PWG, and in the parent qualitative interviews,5 reported having several concerns about using a MHC for their child. Parents didn’t know what services would be provided at a MHC, and were unfamiliar with the MHC’s screening and intake system. Parents also reported stigma attached to MHCs in their community—they were often viewed as places associated with child protective services or severe mental illness, treated only with medication, rather than as a family-friendly center for child-focused behavioral health services.
System Solution #1: Parents watch a video introducing them to the MHC at the time of initial referral.
PWG parents suggested that a video introducing them to the MHC, including a description of services, staff, and procedures, would be helpful in creating greater comfort with the idea of utilizing a MHC for their child’s MH needs. PWG members wanted the video to illustrate to parents that the MHC was a child-focused, friendly environment with staff dedicated to providing comprehensive services to children and families. At the time of the initial referral by the PCP at the FQHC site, parents will watch a 5-minute video (Funches Productions) created by the MHCs (http://www.childguidance.org/, http://www.childfamilycenter.org/), providing them with an introduction to the MHC and a step-by-step explanation of the process for receiving services. A medical assistant at each intervention primary care clinic will show the parents the video in the exam room or provide a link to the video via text message.
Transition Point #2: Many parents don’t complete the MHC’s screening and eligibility process in a timely manner after referral.
The current system of phone screening for eligibility was problematic from the perspective of parents and MHC staff. Parents often received these phone calls from the MHC weeks after the initial referral from their PCP. This delay in the first contact was often due to elapsed time to receive the initial referral by fax from the FQHC and failed attempts to reach the parent by phone. Parents reported viewing these calls as “cold-calls”; for many parents, the information requested during the call (eg, household income) seemed somewhat intrusive when elicited via phone. The MHCs reported several challenges to contacting parents via phone; numbers were frequently no longer valid by the time of the phone screening contact, parents often didn’t seem to remember that a referral was made, and at times didn’t seem to be expecting or receptive to the MHC contact.
System Solution #2: Parents at the FQHC use a live videoconference session to connect with MHC staff to enhance completion of the screening and eligibility process.
To address this problem, the PWG designed the phone eligibility screening as a live videoconference session in which the parent (located at the FQHC) connects with the MHC case manager (located at the MHC). The perspective from PWG parents was that parents would feel more comfortable going to the FQHC clinic and being assisted through this unfamiliar process by FQHC staff. The parent will meet with the FQHC MH care coordinator, and together they connect to the MHC via live videoconference, using a HIPPA compliant platform, for the eligibility screening process. These sessions will occur within just a few days of the initial PCP referral; questions to determine eligibility are the same as those asked via phone (eg, insurance, income).
Transition Point #3: PCPs reject transfer of stable patients who have completed treatment back to primary care for ongoing psychotropic medication management.
Once a patient has completed treatment and management at the MHCs, there was often a need to transfer back to primary care for ongoing psychotropic medication management.
However, the MHCs were usually not successful in getting a PCP at the FQHC to accept patients back for primary care psychotropic medication management, for a number of different reasons. PCPs often didn’t feel comfortable prescribing the psychiatric medications (due to lack of experience with these medications), didn’t feel as if they had adequate specialty MH support to take full responsibility for these patients, and weren’t confident that they could readily get the patient re-enrolled into the MHC if necessary. Ongoing psychotropic medication management, thus, remained the responsibility of the MHC. This often presented problems with reimbursement; MHCs were often unable to receive ongoing funding from DMH for medication management alone on stable patients.
System Solution #3: Regularly scheduled live videoconferences to connect PCPs and MH clinicians for PCP educational sessions, transfer case sessions, and co-management rounds.
The PWG developed three distinct elements of the Telehealth-Coordinated Collaborative Care intervention to address the concern regarding transfer patients. These were created to facilitate transfer of care back to the PCP for children who have completed the initial treatment and management of their MH condition at the MHCs and were recommended by psychiatry for transfer back to primary care for ongoing psychotropic medication management. Educational sessions were created to increase the comfort level of PCPs on a range of commonly encountered MH conditions. Transfer case sessions were designed to provide the PCP with an opportunity to meet with the transferring MH provider and gain a comprehensive understanding of the transfer case and how it should be managed. The co-management rounds sessions were designed to provide another venue for PCPs and MH providers to discuss shared patients, and for PCPs to more closely follow their previously referred patients, who may eventually return for primary care management as a transfer case. Each element aimed to increase the level of communication and collaboration between PCPs and specialty providers, and the comfort of PCPs in managing MH disorders in patients with specialty MH support. Sessions were planned to be held during lunch, to maximize provider attendance, and CME credit would be offered for faculty attendance at educational sessions.
Educational sessions were designed as topic-based webinars in which the specialty clinician provides a live, brief presentation on diagnosis, management, and referral and post-referral follow-up on a range of MH problems that the PCP may encounter. These monthly, hour-long webinars were created to be attended by PCPs, and to include time for discussion and questions. Topics will include attention deficit hyperactivity disorder (ADHD), anxiety, depression, oppositional defiant disorder (ODD), post-traumatic stress disorder (PTSD), and anorexia nervosa.
Transfer case sessions were designed to occur when the MHC had a patient who had completed treatment and management at the MHC, and was ready to be transferred back for PCP management of psychotropic medication and the MH condition. Generally, these patients should be enrolled in the MHC for at least 6-12 months prior to transfer. These “transfer patients” should have completed the behavioral therapy portion of services, yet still need frequent visits with the psychiatrist for ongoing medication management. The FQHC and MHCs together explicitly defined which patients would be appropriate for transfer: 1) mild-moderate severity, 2) simple-moderate complexity, and 3) diagnosis of one or more of five conditions: ADHD, depression, anxiety, ODD, and PTSD. During transfer sessions, the psychiatrist hoping to transfer a patient back to primary care will connect with an accepting PCP via live videoconference. The PCP and psychiatrist will discuss the specific primary care management of the patient who is ready to be transferred. All providers, including the accepting PCP, will be encouraged to participate in these sessions to learn and prepare for potential transfer cases.
Co-management rounds were planned to be held as needed, and can often be added to either the end of an educational session or transfer case session. These co-management sessions will allow the PCPs and MH specialist to discuss ongoing management concerns for shared patients. These could be patients who were recently transferred back to primary care, or new patients who are in the referral process.
After the initial psychiatric visit at the MHC, subsequent visits will be conducted via telehealth (ie, live videoconference visits) with the patient at the FQHC location, accompanied by the FQHC MH care coordinator, and the psychiatrist at the MHC. The PWG envisioned that this would help ease the transfer of patients back to primary care by having the patient located at the FQHC for psychiatric follow-up visits, encouraging the parent to build trust with the care coordinator, and including the PCP in the process by enlisting their assistance in medication prescription refill.
PWG Process Evaluation and Challenges
Attendance at PWG meetings averaged 72% of all members at meetings 1-6, which were dedicated to development of the intervention. PWG members were also asked to evaluate the PWG process after each meeting; this survey was completed by 75% of meeting attendees, for meetings 1-6. A majority of PWG respondents reported that shared decision-making was used at meetings (97%), that the project purpose and objectives were clearly stated at meetings (94%), and that the meeting time and place were convenient (92%). Ninety-six percent of the PWG respondents felt satisfied with their participation in the meetings, and 97% felt satisfied with the meeting generally.
The major challenge encountered using the PWG to design the intervention was that the primary care organization perspective was often different from the MHC perspective on the same problem. When this occurred, we used a consensus approach to come to agreement, but often it was the parent’s input on the PWG that brought these two groups to consensus.
Discussion
Using a community-partnered approach, the Telehealth-Coordinated Collaborative Care intervention was designed to meet the specific needs of a multi-site FQHC, community MHCs, and its families. The PWG developed a multi-stepped intervention that addressed the major gaps in the referral system, including the challenges of connecting patients to the MHC from primary care, and supporting PCPs in accepting them back after completion of treatment.
The key elements of the intervention focused on the main access points to the MHC and back to primary care. These were critical transition points, and were identified as the most important elements of the referral and treatment process to target through intervention by the PWG. Other interventions that have aimed to improve access to MH among low-income school-aged children have focused on co-location of MH within primary care, collaborative care models of care that may include MH mid-level providers working with the PCPs, and immediate access to psychiatry consultation for PCPs.16,17,37 Each of these models has been studied, with varying levels of evidence of effectiveness in increasing MH care access. These models, however, may require a re-structuring of services, staff, or financing. Together, using the community-partnered approach, the partner organizations in our study developed a referral process that would both help the parent connect with the MHC and later support the PCP in accepting the patient back and taking responsibility for managing mental health care, yet be minimally disruptive to their core model of care. Essentially, few changes were made to the actual services that parents and children received, organizational structure and staffing, or billing arrangements. Without drastic organizational level changes, a new referral process was created to address the main concerns of all stakeholders involved.
The knowledge of all three barriers and accompanying solutions were not held by any one stakeholder group on the PWG —these were only discoverable by including parents, primary care, and MH clinicians and staff together in the same discussions over a period of time. For example, the focus on the challenges of transferring patients back to primary care was not a major concern for the FQHC as the PCPs didn’t feel comfortable taking on the responsibility of managing even stable patients on psychotropic medication5; their major concern was the difficulty in getting families connected to the MHC.
An unintended outcome from this project was a more collaborative working relationship between the FQHC and MHCs. The organizations tackled other issues that affected patient care, but were not directly a part of the intervention, such as how to improve MH care access for children with developmental disabilities, and how to improve the quality of documentation shared between the FQHC and MHCs.
There are limitations to this study. As this is a community-partnered approach to intervention development, the telehealth-based intervention is adapted to address the specific needs of the partners, and may not be generalizable to other locations or settings. We describe development of the intervention here; a pilot study is underway that focuses on the primary outcome of MHC access. Thus, conclusions about the feasibility, acceptability, and effectiveness of this intervention cannot be made. The target points for the intervention are improved access to care and care coordination across primary and specialty MH care; thus, even if the intervention is found to be promising, it does not address the quality of services that patients receive once they do gain access to care at the MHCs. We do not provide details on the cost of the intervention development process or ongoing maintenance; much of these costs relate to staff and provider time at meetings, and the cost of the FQHC MH care coordinator’s time. Finally, payers of MH care for this population were not involved, limiting our capacity to identify barriers and system solutions that may improve the intervention’s sustainability.
Despite these limitations, this community-partnered approach to intervention design and development created a telehealth-based intervention plan that aims to improve MH care access to publicly insured children and improve collaboration and coordination of care among primary care and specialty MH care providers. Our next steps are intervention implementation and testing through a cluster-randomized controlled trial.
Acknowledgments
This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Award (IH-12-11-4168) and a grant from the California Community Foundation (CCF) Award (BAPP-14-107111). All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
References
- 1. Briggs-Gowan MJ, Horwitz SM, Schwab-Stone ME, Leventhal JM, Leaf PJ. Mental health in pediatric settings: distribution of disorders and factors related to service use. J Am Acad Child Adolesc Psychiatry. 2000;39(7):841-849. 10.1097/00004583-200007000-00012 [DOI] [PubMed] [Google Scholar]
- 2. Leaf PJ, Alegria M, Cohen P, et al. . Mental health service use in the community and schools: results from the four-community MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry. 1996;35(7):889-897. 10.1097/00004583-199607000-00014 [DOI] [PubMed] [Google Scholar]
- 3. US Public Health Service Mental Health: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. [Google Scholar]
- 4. Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548- 1555. https://doi.org/ 10.1176/appi ajp.159.9.1548 PMID:12202276 [DOI] [PubMed]
- 5. Porras-Javier L, Bromley E, Lopez M, Coker TR. Challenges to effective primary care-specialty communication and coordination in the mental health referral and care process for publicly insured children. J Behav Health Serv Res. 2018:1-10; Epub ahead of print. 10.1007/s11414-018-9585-z [DOI] [PubMed] [Google Scholar]
- 6. Golberstein E, Eisenberg D, Gollust SE. Perceived stigma and mental health care seeking. Psychiatr Serv. 2008;59(4):392-399. 10.1176/ps.2008.59.4.392 [DOI] [PubMed] [Google Scholar]
- 7. Owens PL, Hoagwood K, Horwitz SM, et al. . Barriers to children’s mental health services. J Am Acad Child Adolesc Psychiatry. 2002;41(6):731-738. 10.1097/00004583-200206000-00013 [DOI] [PubMed] [Google Scholar]
- 8. Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and U.S.-born Black and Latina women from seeking mental health care? Psychiatr Serv. 2007;58(12):1547-1554. 10.1176/ps.2007.58.12.1547 [DOI] [PubMed] [Google Scholar]
- 9. Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976-993. 10.1007/s10900-013-9681-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kolko DJ, Perrin E. The integration of behavioral health interventions in children’s health care: services, science, and suggestions. J Clin Child Adolesc Psychol. 2014;43(2):216- 228. https://doi.org/ 10.1080/15374416.201 3.862804 PMID:24588366 [DOI] [PMC free article] [PubMed]
- 11. Asarnow JR, Rozenman M, Wiblin J, Zeltzer L. Integrated Medical-Behavioral Care Compared With Usual Primary Care for Child and Adolescent Behavioral Health: A Meta-analysis. JAMA Pediatr. 2015;169(10):929-937. 10.1001/jamapediatrics.2015.1141 [DOI] [PubMed] [Google Scholar]
- 12. Merikangas KR, He JP, Burstein M, et al. . Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2011;50(1):32-45. 10.1016/j.jaac.2010.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sarvet B, Gold J, Bostic JQ, et al. . Improving access to mental health care for children: the Massachusetts Child Psychiatry Access Project. Pediatrics. 2010;126(6):1191-1200. 10.1542/peds.2009-1340 [DOI] [PubMed] [Google Scholar]
- 14. Gruttadaro DMD. Integrating mental health and pediatric primary caree. Arlington, VA: National Alliance on Mental Illness; 2011. [Google Scholar]
- 15. Williams J, Shore SE, Foy JM. Co-location of mental health professionals in primary care settings: three North Carolina models. Clin Pediatr (Phila). 2006;45(6):537-543. 10.1177/0009922806290608 [DOI] [PubMed] [Google Scholar]
- 16. Ford JSK, Pidano A, Honigfeld L, Meyers J. Behavioral health services in pediatric primary caree. Farmington, CT: Child Health and Development Institute of Connecticut; 2006. [Google Scholar]
- 17. Briggs RD, Racine AD, Chinitz S. Preventive pediatric mental health care: A co-location model. Infant Ment Health J. 2007;28(5):481-495. 10.1002/imhj.20149 [DOI] [PubMed] [Google Scholar]
- 18. Hjelm NM. Benefits and drawbacks of telemedicine. J Telemed Telecare. 2005;11(2):60-70. 10.1258/1357633053499886 [DOI] [PubMed] [Google Scholar]
- 19. Goldstein F, Myers K. Telemental health: a new collaboration for pediatricians and child psychiatrists. Pediatr Ann. 2014;43(2):79-84. 10.3928/00904481-20140127-12 10.3928/00904481-20140127-12 [DOI] [PubMed] [Google Scholar]
- 20. Hilt RJ, Barclay RP, Bush J, Stout B, Anderson N, Wignall JR. A Statewide Child Telepsychiatry Consult System Yields Desired Health System Changes and Savings. Telemed J E Health. 2015;21(7):533-537. 10.1089/tmj.2014.0161 [DOI] [PubMed] [Google Scholar]
- 21. Nelson EL, Barnard M, Cain S. Treating childhood depression over videoconferencing. Telemed J E Health. 2003;9(1):49-55. 10.1089/153056203763317648 [DOI] [PubMed] [Google Scholar]
- 22. Soares NS, Langkamp DL. Telehealth in developmental-behavioral pediatrics. J Dev Behav Pediatr. 2012;33(8):656-665. 10.1097/DBP.0b013e3182690741 [DOI] [PubMed] [Google Scholar]
- 23. Yellowlees PM, Hilty DM, Marks SL, Neufeld J, Bourgeois JA. A retrospective analysis of a child and adolescent eMental Health program. J Am Acad Child Adolesc Psychiatry. 2008;47(1):103-107. 10.1097/chi.0b013e31815a56a7 [DOI] [PubMed] [Google Scholar]
- 24. Myers KM, Valentine JM, Melzer SM. Child and adolescent telepsychiatry: utilization and satisfaction. Telemed J E Health. 2008;14(2):131-137. 10.1089/tmj.2007.0035 [DOI] [PubMed] [Google Scholar]
- 25. Diamond JM, Bloch RM. Telepsychiatry assessments of child or adolescent behavior disorders: a review of evidence and issues. Telemed J E Health. 2010;16(6):712-716. 10.1089/tmj.2010.0007 [DOI] [PubMed] [Google Scholar]
- 26. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010;79(11):736-771. 10.1016/j.ijmedinf.2010.08.006 [DOI] [PubMed] [Google Scholar]
- 27. Grady B, Myers KM, Nelson EL, et al. ; American Telemedicine Association Telemental Health Standards and Guidelines Working Group . Evidence-based practice for telemental health. Telemed J E Health. 2011;17(2):131-148. 10.1089/tmj.2010.0158 [DOI] [PubMed] [Google Scholar]
- 28. Thomas CR, Holzer CE III. National distribution of child and adolescent psychiatrists. J Am Acad Child Adolesc Psychiatry. 1999;38(1):9-15. 10.1097/00004583-199901000-00013 [DOI] [PubMed] [Google Scholar]
- 29. Thomas CR, Holzer CE III. The continuing shortage of child and adolescent psychiatrists. J Am Acad Child Adolesc Psychiatry. 2006;45(9):1023-1031. 10.1097/01.chi.0000225353.16831.5d [DOI] [PubMed] [Google Scholar]
- 30. Elford R, White H, Bowering R, Ghandi A, Maddiggan B, John KS. A randomized, controlled trial of child psychiatric assessments conducted using videoconferencing. J Telemed Telecare. 2000;6(2):73-82. 10.1258/1357633001935086 [DOI] [PubMed] [Google Scholar]
- 31. Hersh WR, Hickam DH, Severance SM, Dana TL, Pyle Krages K, Helfand M Diagnosis, access and outcomes: update of a systematic review of telemedicine services. J Telemed Telecare. 2006;12(2_suppl)(suppl 2):S3-S31. https:// doi.org/ 10.1258/135763306778393117 PMID:16989671 [DOI] [PubMed]
- 32. Glueckauf RL, Fritz SP, Ecklund-Johnson EP, Liss HJ, Dages P, Carney P. Videoconferencing-based family counseling for rural teenagers with epilepsy: phase 1 findings. Rehabil Psychol. 2002;47(1):49-72. 10.1037/0090-5550.47.1.49 [DOI] [Google Scholar]
- 33. Coker TR, Moreno C, Shekelle PG, Schuster MA, Chung PJ. Well-child care clinical practice redesign for serving low-income children. Pediatrics. 2014;134(1):e229-e239. 10.1542/peds.2013-3775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vastine A, Gittelsohn J, Ethelbah B, Anliker J, Caballero B. Formative research and stakeholder participation in intervention development. Am J Health Behav. 2005;29(1):57-69. 10.5993/AJHB.29.1.5 [DOI] [PubMed] [Google Scholar]
- 35. Westfall JM, Fagnan LJ, Handley M, et al. . Practice-based research is community engagement. J Am Board Fam Med. 2009;22(4):423-427. 10.3122/jabfm.2009.04.090105 [DOI] [PubMed] [Google Scholar]
- 36. Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19(1):173-202. 10.1146/annurev.publhealth.19.1.173 [DOI] [PubMed] [Google Scholar]
- 37. Connor DF, McLaughlin TJ, Jeffers-Terry M, et al. . Targeted child psychiatric services: a new model of pediatric primary clinician--child psychiatry collaborative care. Clin Pediatr (Phila). 2006;45(5):423-434. 10.1177/0009922806289617 [DOI] [PubMed] [Google Scholar]