Abstract
Objective
To study the role of Computed tomography (CT) and Magnetic resonance imaging (MRI) for design and development of orthopaedic model using additive manufacturing (AM) technologies.
Methods
A significant number of research papers in this area are studied to provide the direction of development along with the future scope.
Results
Briefly discussed various steps used to create a 3D model by Additive Manufacturing using CT and MRI scan. These scanning technologies are used to produce medical as well as orthopaedic implants by using AM technologies. The images so produced are exported in different software like OsiriX Imaging Software, 3D slicer, Mimics, Magics, 3D doctor and InVesalius to produce a 3D digital model. Various criteria's achieved by CT and MRI scan for design and development of orthopaedic implant using additive manufacturing are also discussed briefly. AM model created by this process show exact shape, size, dimensions, textures, colour and features.
Conclusion
AM technologies help to convert the digital model into a 3D physical object, thereby improving the understanding of patient anatomy for treatment as well as for educational purpose. These scanning technologies have various applications to enhance the AM in the field of orthopaedic. In orthopaedic every patient model is a customised unit, sourced from the individual patient. 3D CAD data captured by these scanning technologies are directly exported in standard triangulate language (STL) format for printing by AM technologies. Crossestion of the physical model fabricated by this process shows a patient's anatomy if the model prepared by using the bone-like material.
Keywords: Additive manufacturing (AM), Computed tomography (CT), Magnetic resonance imaging (MRI), Orthopaedic
1. Introduction
Additive manufacturing has a revolutionising effect on many industries, and same is being observed in the area of orthopaedics, as it assists with the printing of human bone and helps in transplantation.1
In orthopaedic it is applied to create a physical model of patient bone to examine the defect. This process takes data from CT and MRI and makes a 3D model with precise dimension. 3D printed model by these techniques has a unique purpose which allows the surgeon to practice before the operation and provides a meaningful experience to surgeons depending upon the specific circumstance. These scanning technologies take imaging of patient creates a virtual 3D model that is printable. The customised 3D physical model is printed rapidly by using various AM technologies as per the clinical translation. The Orthopaedic surgeon can use a 3D model for surgical guides, teaching, and learning of high-risk operation which was a challenge to teach. We can section orthopaedic 3D model captured by CT/MRI in any plane and can rotate in all axes on screen. By 3D printed physical model we can precisely analyse about the surgery before an interventional procedure/actual surgery2,3,.4
These technologies as applied to create models like prosthetics, dental appliances, custom implant, prosthetic limbs, which look and feel like a real one through a 3D digital file prepared by various scanning techniques.5
2. CT scan
CT scan is used to capture data of an inside organ and at a different level of density of the human body. It captures detailed information of bones, eyes, heart, spine, neck, shoulder and other inner parts of the body with the help of X-ray beam. CT scanners improve patient comfort due to its fast scanning. It captures high-resolution images and helps doctors to make diagnoses such as visualisation of tumours or small nodules which cannot be seen by X-ray. It is used to check the status of spine, brain, chest and other defects in the body. Without doing any invasive angiography, a surgeon can view clear 3 D images produced with the help of different software6,7,.8
3. MRI scan
MRI is used to capture detail structure of human body like bones, joints, spinal cord, brain, organs, heart, liver, soft tissue and other body parts with the help of powerful magnetic field and radio frequency pulses. This technology provides information about the normal and abnormal tissue. It also provides useful information about blood circulation in the body, and it detects the related problems. A radiographer is used to operate the MRI scanner and controls the machine with the help of a computer. MRI scan is a painless, safe and extremely accurate method of disease detection and provides information about patient's diagnosis. It provides information about the swelling, bleeding, tumours of the brain, brain aneurysms as well as inflammation of the spine9,10,.11
4. Additive manufacturing
It is a process of joining materials layer by layer to make a 3D physical objects from 3D digital model data produced from designing software or a 3D scanner or from other medical scanning techniques like MRI and CT scan. It easily allows producing a customised model with low cost and with no requirement of any additional tooling. It allows the production of individual and complex parts such as bones, heart, prosthetic and other medical implants. Medical is one of the rapidly growing areas of additive manufacturing to fabricate patient-specific devices.12 There are seven main techniques of additive manufacturing technology such as VAT Photopolymerization, Powder Bed Fusion, Binding jetting, Material jetting, Sheet Lamination; Material Extrusion and Directed Energy Deposition. By using AM, manufacturing of patient-specific implant are possible and help the surgeon to reduce the time to perform surgery. In medical AM bring a new way to treat and diagnose patients precisely as per need.13 There are various techniques used in additive manufacturing technologies.
-
•
Stereolithography (SLA)
-
•
Selective laser sintering (SLS)
-
•
Fused deposition modelling (FDM)
-
•
Direct metal laser sintering (DMLS)
-
•
Polyjet 3D printing (PJP)
-
•
Inkjet 3D printing (IJP)
-
•
Laminated Object Manufacturing (LOM)
-
•
Colour-Jet-Printing (CJP)
-
•
Multi-Jet-Printing (MJP)
-
•
Electron Beam Melting (EBM)
Basically three categories of material are used to manufacture prosthetic devices which are discussed in Table 1 by the application of different AM techniques.
Table 1.
Material used to manufacture Orthopaedic implants by different AM technique.
| S No | Material | Additive Manufacturing techniques used |
|---|---|---|
| 1 | Metal (Stainless steel, cobalt-chromium alloys and titanium alloys used as a metal to manufacture orthopaedic implants) | Direct metal laser sintering, Electron Beam Melting, Laminated Object Manufacturing |
| 2 | Polymers (High-density polyethylene) | Fused deposition modelling, Polyjet 3D printing |
| 3 | Ceramics (aluminium oxide, calcium phosphates, powder) | Stereolithography, Selective laser sintering, Inkjet 3D printing, Colour-Jet-Printing, Multi-Jet Printing |
5. Need for the study
In the current scenario, there is a requirement of innovation in medical as well as in orthopaedic area to achieve higher customisation and precision. The need is to undertake a study for determining how CT and MRI scan play a significant role in fabricating exact fit patient-specific patient orthopaedic model by the application of additive manufacturing to fulfil the requirement of customisation and innovation. In this study, we explore that how MRI and CT benefit the area of orthopaedics with the use of AM technologies. This study provides steps to create an orthopaedic model with the help of AM from CT and MRI and the material used for printing. The study also states various criteria's that can be achieved by these scanning technologies for design and development of orthopaedic implant using additive manufacturing and provides a good co-operation between surgeon and patient.
6. Steps to create a 3D model by additive manufacturing using CT and MRI
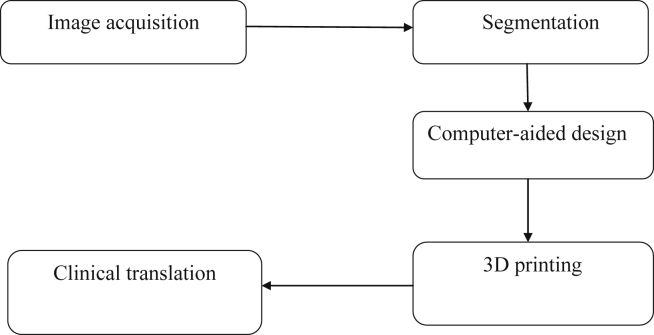
Additive manufacturing technologies use a 3D digital model to create an orthopaedic 3D physical model by using the layer by layer techniques. Fig. 1 shows the steps to create a 3D model by Additive Manufacturing using CT and MRI.
Fig. 1.
Steps to create a 3D model by Additive Manufacturing using CT and MRI.
6.1. Image acquisition
CT and MRI scan are useful for image acquisition as it provides a representation of the hidden part of the skin like bone, tissue, organ etc. In the design process, it is a crucial step as it captures accurate data of the patient.14,15
6.2. Segmentation
There are different software used to create a 3D virtual model from images as captured by CT and MRI. It is helpful for an anatomical structure, volume, shape and size of tissue as used for virtual surgery simulation.16,17 Different software used to convert CT and MRI file into the 3D model are as;
-
•
OsiriX Imaging Software
-
•
3D Slicer
-
•
Mimics
-
•
Magics
-
•
3D doctor
-
•
InVesalius
6.3. Computer-aided design
A digital 3D CAD model developed from patient data from segmentation is exported into STL format for printing by using additive manufacturing technologies. Layer thickness is also increased or decreased in slicing software to increases accuracy of implants.18
6.4. 3D printing
AM is used to create a 3D a physical implants from 3D CAD model. This technology is proliferating in the medical field for customisation and precision towards providing a better idea to the surgeon. Manufactures complex shapes, which are specific to patient's anatomy and internal structure with higher flexibility without any additional requirement of tools and equipment.19,20
6.5. Clinical translation
3D physical implants manufactured by AM technologies helps in treatment/diagnoses of the disease, through better understanding as It addresses clinical translation and provides good collaboration between doctors and patient.21,22
7. Criteria's achieved by CT and MRI scan for design and development of orthopaedic implant using additive manufacturing
3D printed implant help surgeon for patient counselling. When implants manufactured by traditional manufacturing techniques do not fit properly, then AM technologies provides the surgeon with the best-fit implants. Now surgeon can practice the procedure to perform a successful operation. Table 2 discusses different criteria of design and development of orthopaedic implants, achieved by using AM.
Table 2.
Criteria's achieved by CT and MRI scan for design and development of orthopaedic implant using additive manufacturing.
| S No | Role | Description | References |
|---|---|---|---|
| 1 | Designing of implant |
|
Wake et al., 201622; Ballyns et al., 200823 |
| 2 | Manufacturing of Orthopaedic implant |
|
Mitsouras et al., 201511; Javaid and Haleem, 20181 |
| 3 | Medical modelling |
|
Werner et al., 20102; Junior et al., 201615 |
| 4 | Surgical planning |
|
Suzuki et al., 200424; Ventola 201425 |
| 5 | Exact dimensioning |
|
Hochman et al., 201526; Haleem and Javaid 201827 |
| 6 | Surgical guidance |
|
Suzuki et al., 200424; Cohen and Reyes 201528 |
| 7 | A replica of the orthopaedic model |
|
Hochman et al., 201526; Ripley et al., 20166 |
| 8 | Speed |
|
Kusaka et al., 201529; Mitsouras et al., 20179 |
| 9 | Lesser cost |
|
Cai et al., 201514; Thompson et al., 201730 |
| 10 | Flexibility |
|
Leng et al., 201531; Javaid and Haleem 201818 |
| 11 | Rapid manufacturing |
|
Starosolki et al., 201421; Negi et al., 201412 |
| 12 | Development of tools and devices surgical training |
|
Suzuki et al., 200424; Javaid and Haleem 201713 |
| 13 | Improved patient care |
|
Markl et al., 200532; Khalyfa et al.,200719 |
| 14 | Accuracy |
|
Wake et al., 201622; Ruffins et al., 200733 |
| 15 | Digital storage of patient data |
|
Herrmann et al., 20143; Leng et al., 201531 |
| 16 | Procedural planning |
|
Ruffins et al., 200733; Ogden et al., 201534; Vaish and Vaish35 |
| 17 | Create innovation |
|
Khalyfa et al., 200719; Cloonan et al., 201436 |
| 18 | Simple manipulation |
|
Rengier et al., 20107; Ventola 201425 |
AM technologies suit the orthopaedic field. A model can be well designed using these scanning technologies/supporting software and printed by AM technologies. A 3D model allows the surgeon to learn about the problem. A physical 3D model shows better understanding regarding what happens in the body parts.
8. Discussion
Additive manufacturing applications are useful in orthopaedic to make an accurate anatomical model to explain, understand and prepare the procedures of surgeries. It fulfils various criteria's due to its flexibility in design and manufacturing. Images are constructed from CT and MRI, then converted into a 3D CAD model with the help of different software, and this CAD model is easily printable by AM technologies using the layer by layer technique. Missing part of the bone is also created by this technique. Data is captured by CT, and MRI scan and AM technologies are used to make surgery successful. This technology is also successfully applied for an exact replica of the orthopaedic implant with great flexibility and exact dimensioning which improve patient care. It merely manipulates and creates innovation by redesigning of the implant in digital CAD model. Doctors and surgeon can understand the working of anatomies of the individual patient. AM technologies also print colour 3D model that shows both patients and doctors clear information as compared to CT and MRI data. Implant precisely produced by this technology reduces the risk during the operation with minimizes the stress of the patient. In the current scenario, scanning technologies are suitable for doctors and surgeon for everyday practice and act as a supporting technology for AM to create an implant. The digital 3D file of the patient defect can be stored digitally and can be easily edited according to the required shape and dimensions which is finally printable by AM technologies. It can translate innovative doctors/surgeon ideas into reality.
9. Future scope
In future, AM will be used towards better customisation at a reasonable cost with the help of CT/MRI. This disruptive technology will change traditional fabrication system in medical as well as in orthopaedic to print any patient-specific 3D model with an exact dimension that is applicable in the best surgical planning of complicated procedure and surgery. In future, it will provide a close collaboration between doctors, surgeon and researcher. The 3D physical model can help surgeons to understand better about the patient-specific pathology and anatomy as compared to the 2D picture on a computer screen. It is a great capability enhancer towards manufacturing of custom shaped orthopaedic implants and prostheses, medical devices, living constructs, tissue scaffolds, biological chips and training apparatuses. It minimises unpleasant side effects and expanding its capabilities to fulfil various challenges of design and development of orthopaedic implant.
10. Conclusion
Additive Manufacturing quickly fabricates complex-shapes with the help of data acquired by CT/MRI scan. Surgical planning, implant design and development, reverse engineering applications, rapid tooling in orthopaedic field is possible with AM, and it opens a new market in medical customisation, modelling, preparing accurate replica, medical education and training, and for decision making. Artificial bone printed by AM give similar shape, size, dimensions as real one which act as biomechanical function. AM Facilitates improved designs & development of personalised prostheses, implants with desired shape and size. CT and MRI are the supporting technologies which help to solve various problems in the area of orthopaedic. Patient-specific model printed by AM provide a visual and tactile understanding of the patient-specific pathology and anatomy which increases the patient safety and satisfaction. It provides a better understanding of different types of defects and fractures; thus surgeon can easily understand the medical conditions of the patient.
Conflict to interest
None.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jcot.2018.07.002.
Contributor Information
Abid Haleem, Email: ahaleem@jmi.ac.in.
Mohd Javaid, Email: mjavaid@jmi.ac.in.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Javaid M., Haleem A. Additive manufacturing applications in orthopaedics: a review. J. Clin. Orthop. Traumatol. 2018 doi: 10.1016/j.jcot.2018.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Werner H., dos Santos J.R., Fontes R. Additive manufacturing models of fetuses built from three-dimensional ultrasound, magnetic resonance imaging and computed tomography scan data. Ultrasound Obstet Gynecol. 2010;36(3):355–361. doi: 10.1002/uog.7619. [DOI] [PubMed] [Google Scholar]
- 3.Herrmann K.H., Gartner C., Gullmar D., Kramer M., Reichenbach J.R. 3D printing of MRI compatible components: why every MRI research group should have a low-budget 3D printer. Med Eng Phys. 2014;36(10):1373–1380. doi: 10.1016/j.medengphy.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Vaishya R., Lal H. Learn through innovation, research and publication. J. Clin. Orthop. Traumatol. 2016;7:219–220. doi: 10.1016/j.jcot.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fedorov A., Beichel R., Kalpathy-Cramer J. 3D slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging. 2012;30(9):1323–1341. doi: 10.1016/j.mri.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ripley B., Kelil T., Cheezum M.K. 3D printing based on cardiac CT assists anatomic visualization prior to transcatheter aortic valve replacement. J. Cardiovasc. Comput. Tomogr. 2016;10(1):28–36. doi: 10.1016/j.jcct.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rengier F., Mehndiratta A., von Tengg-Kobligk H. 3D printing based on imaging data: review of medical applications. Int. J. Comput. Assist. Radiol Surg. 2010;5(4):335–341. doi: 10.1007/s11548-010-0476-x. [DOI] [PubMed] [Google Scholar]
- 8.Vaishya R., Lal H. Three common orthopaedic surgical procedures of the lower limb. J. Clin. Orthop. Traumatol. 2018;9:101–102. doi: 10.1016/j.jcot.2018.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitsouras D., Lee T.C., Liacouras P. Three-dimensional printing of MRI-visible phantoms and MR image-guided therapy simulation. Magn Reson Med. 2017;77(2):613–622. doi: 10.1002/mrm.26136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lal H., Kumar L., Kumar R., Boruah T., Jindal P.K., Sabharwal V.K. Inserting pedicle screws in lumbar spondylolisthesis – the easy bone conserving way. J. Clin. Orthop. Traumatol. 2017 doi: 10.1016/j.jcot.2016.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mitsouras D., Liacouras P., Imanzadeh A. Medical 3D printing for the radiologist. Radiographics. 2015;35(7):1965–1988. doi: 10.1148/rg.2015140320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Negi S., Dhiman S., Sharma R.K. Basics and applications of rapid prototyping medical models. Rapid Prototyp J. 2014;20(3):256–267. [Google Scholar]
- 13.Javaid M., Haleem A. Additive manufacturing applications in medical cases: a literature-based review. Alexandria J. Med. 2017 doi: 10.1016/j.ajme.2017.09.003. [DOI] [Google Scholar]
- 14.Cai T., Rybicki F.J., Giannopoulos A.A. The residual STL volume as a metric to evaluate accuracy and reproducibility of anatomic models for 3D printing: application in the validation of 3D-printable models of maxillofacial bone from reduced radiation dose CT images. 3D Print Med. 2015;1(2):1–9. doi: 10.1186/s41205-015-0003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Junior H.W., Santos J.L.D., Belmonte S. Applicability of three-dimensional imaging techniques in fetal medicine. Radiol Bras. 2016;49(5):281–287. doi: 10.1590/0100-3984.2015.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huotilainen E., Jaanimets R., Valášek J. Inaccuracies in additive manufactured medical skull models caused by the DICOM to STL conversion process. J Cranio-Maxillo-Fac Surg. 2014;42(5):259–265. doi: 10.1016/j.jcms.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Rosset A., Spadola L., Ratib O. OsiriX: an open-source software for navigating in multidimensional DICOM images. J Digit Imag. 2004;17(3):205–216. doi: 10.1007/s10278-004-1014-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Javaid M., Haleem A. Current status and challenges of Additive manufacturing in orthopaedics: an overview. J. Clin. Orthop. Traumatol. 2018 doi: 10.1016/j.jcot.2018.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khalyfa A., Vogt S., Weisser J. Development of a new calcium phosphate powder-binder system for the 3D printing of patient specific implants. J Mater Sci Mater Med. 2007;18(5):909–916. doi: 10.1007/s10856-006-0073-2. [DOI] [PubMed] [Google Scholar]
- 20.Javaid M., Kumar L., Kumar V., Haleem A. Product design and development using Polyjet rapid prototyping technology. Int. J. Contr. Theor. Inf. 2015;5(3):12–19. [Google Scholar]
- 21.Starosolki Z.A., Kan J.H., Rosenfeld S.D., Krishnamurthy R., Annapragada A. Application of 3-D printing (rapid prototyping) for creating physical models of pediatric orthopedic disorders. Pediatr Radiol. 2014;44:216–221. doi: 10.1007/s00247-013-2788-9. [DOI] [PubMed] [Google Scholar]
- 22.Wake N., Chandarana H., Huang W.C., Taneja S.S., Rosenkrantz A.B. Application of anatomically accurate, patient-specific 3D printed models from MRI data in urological oncology. Clin Radiol. 2016;71(6):610–614. doi: 10.1016/j.crad.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 23.Ballyns J.J., Gleghorn J.P., Niebrzydowski V. Image-guided tissue engineering of anatomically shaped implants via MRI and micro-CT using injection molding. Tissue Eng A. 2008;14(7):1195–1202. doi: 10.1089/ten.tea.2007.0186. [DOI] [PubMed] [Google Scholar]
- 24.Suzuki M., Ogawa Y., Kawano A., Hagiwara A., Yamaguchi H., Ono H. Rapid prototyping of temporal bone for surgical training and medical education. Acta Otolaryngol. 2004;124(4):400–402. doi: 10.1080/00016480410016478. [DOI] [PubMed] [Google Scholar]
- 25.Ventola C.L. Medical applications for 3D printing: current and projected uses. Pharmacol Therapeut. 2014;39(10):704–711. [PMC free article] [PubMed] [Google Scholar]
- 26.Hochman J.B., Rhodes C., Wong D., Kraut J., Pisa J., Unger B. Comparison of cadaveric and isomorphic three-dimensional printed models in temporal bone education. Laryngoscope. 2015;125(10):2353–2357. doi: 10.1002/lary.24919. [DOI] [PubMed] [Google Scholar]
- 27.Haleem A., Javaid M. 3D scanning applications in medical field: a literature-based review. Clin. Epidemiol. Global Health. 2018 doi: 10.1016/j.cegh.2018.05.006. [DOI] [Google Scholar]
- 28.Cohen J., Reyes S.A. Creation of a 3D printed temporal bone model from clinical CT data. Am J Otolaryngol. 2015;36(5):619–624. doi: 10.1016/j.amjoto.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 29.Kusaka M., Sugimoto M., Fukami N. Initial experience with a tailor-made simulation and navigation program using a 3-D printer model of kidney transplantation surgery. Transplant Proc. 2015;47(3):596–599. doi: 10.1016/j.transproceed.2014.12.045. [DOI] [PubMed] [Google Scholar]
- 30.Thompson A., McNally D., Maskery I., Leach R.K. X-ray computed tomography and additive manufacturing in medicine: a review. Int. J. Metrol. Qual. Eng. 2017;8:1–15. [Google Scholar]
- 31.Leng S., Diehn F.E., Lane J.I. Temporal bone CT: improved image quality and potential for decreased radiation dose using an ultra-high-resolution scan mode with an iterative reconstruction algorithm. AJNR (Am. J. Neuroradiol.) 2015;36(9):1599–1603. doi: 10.3174/ajnr.A4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Markl M., Schumacher R., Küffer J., Bley T.A., Hennig J. Rapid vessel prototyping: vascular modeling using 3t magnetic resonance angiography and rapid prototyping technology. Magma. 2005;18(6):288–292. doi: 10.1007/s10334-005-0019-6. [DOI] [PubMed] [Google Scholar]
- 33.Ruffins S.W., Martin M., Keough L. Digital three-dimensional atlas of quail development using high-resolution MRI. Sci World J. 2007;7:592–604. doi: 10.1100/tsw.2007.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ogden K.M., Aslan C., Ordway N., Tillapaugh-Fay G., Soman P. Factors affecting dimensional accuracy of 3-D printed anatomical structures derived from CT data. J Digit Imag. 2015;28(6) doi: 10.1007/s10278-015-9803-7. 654–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vaish A., Vaish R. 3D printing and its applications in Orthopedics. J. Clin. Orthop. Traumatol. 2018;95:S74–S75. doi: 10.1016/j.jcot.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cloonan A.J., Shahmirzadi D., Li R.X., Doyle B.J., Konofagou E.E., Mcgloughlin T.M. 3D-printed tissue-mimicking phantoms for medical imaging and computational validation applications. 3D Print Addit Manuf. 2014;1(1) doi: 10.1089/3dp.2013.0010. 14–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.