Abstract
Purpose
Three dimensional (3D) printing, also called ‘rapid prototyping’ and ‘additive manufacturing’ is considered as a “second industrial revolution.” With this rapidly emerging technology, CT or MR images are used for the creation of graspable objects from 3D reconstituted images. Patient-specific anatomical models can be, therefore, manufactured efficiently. These can enhance surgeon's understanding of their patients' patho-anatomy and also help in precise preoperative planning. The 3D printed patient-specific guides can also help in achieving accurate bony cuts, precise implant placement, and nice surgical results. Customized implants, casts, orthoses and prosthetics can be created to match an individual patient's anatomy. The 3D printing of individualized artificial cartilage scaffolds and 3D bioprinting are some other areas of growing interest. We aim to study the publication trends in 3D printing as applied to the field of orthopaedics.
Materials and methods
A literature search was performed to extract all papers related to 3D printing applications in orthopaedics and allied sciences on the Pubmed, Web of Science and SCOPUS databases. Suitable keywords and boolean operators (“3D Printing” OR “3-dimensional printing” OR “3D printed” OR “additive manufacturing” OR “rapid prototyping”) AND (‘‘Orthopaedics” OR “Orthopaedics’’) were used, in May 2018. Search was attempted in Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, and Database of Abstracts of Review of Effectiveness (DARE) databases, using keywords 3d printing orthopaedics. A similar search was repeated in pubmed and SCOPUS to get more specific papers.
No limits were set on the period or evidence level, as 3D printing in orthopaedics is relatively new and evidence available is usually limited to low-level studies. Trends in a publication on these topics were analyzed, focussing on publications, type of research (basic science or clinical), type of publication, authors, institution, and country. Some citations received by these papers were also analyzed in SCOPUS and Web of Science. MS Excel (2008 - Mac version) and VOS Viewer1.6.8 (2018- Mac version) software were used to analyze the search results and for citation mapping respectively. We also identified top 10 most cited articles in the field.
Results
An increasing trend in publications in 3D printing-related work in orthopedic surgery and related fields was observed in the recent past. A search on Pubmed using the above strategy revealed 389 documents. A similar search revealed 653 documents on SCOPUS, many (314) of which were from an engineering background and only 271 were related to medicine. No papers were found in the Cochrane database. Search on TRIP database revealed 195 papers. A similar search revealed 237 papers on orthopedic applications on Pubmed and 269 documents on SCOPUS, whereas a search on Web of Science revealed only 23 papers. Publication trends were then analyzed on data derived from SCOPUS database. Overall, most papers were published from China, followed by United States, United Kingdom, and India.
Conclusion
There has been an upsurge of interest in 3D printing in orthopedic surgery, as is evident by an increasing trend in research and publications in this area in the recent years. Presently, 3D printing is in a primitive stage in the field of orthopedic surgery as our knowledge is still insufficient, and costs and learning curve are somewhat high. However, looking at latest publication trends, we are enthusiastic that it holds the key to future in orthopaedics and trauma cases.
Keywords: 3D printing, Rapid prototyping, Additive manufacturing, Orthopaedics, Spine, Arthroplasty
1. Introduction
Three dimensional (3D) printing, also called ‘rapid prototyping’ and ‘additive manufacturing’ may be considered as a “second industrial revolution.” With this rapidly emerging technology, CT or MR images are used for the creation of graspable objects from 3D reconstituted images. Patient-specific anatomical models can now be manufactured easily. These can enhance surgeon's understanding of their patients' patho-anatomy and also help in precise preoperative planning. These models can also help in the training of novice surgeons in complicated areas like pelvi-acetabular trauma and spine deformity surgery. A 3D printed patient-specific guides help in achieving accurate bony cuts, precise implant placement, and nice surgical results. Customized implants, casts, orthoses and prosthetics can be created to match an individual patient's anatomy. Finally, it can also help in the evaluation of restoration of individual anatomy after surgery. In some cases, it can help in making a precise anatomical diagnosis, where it is not otherwise apparent, and in planning subsequent management. 3D printing of individualized artificial cartilage scaffolds and 3D bioprinting are some areas of growing interest.1, 2, 3, 4, 5
Despite the significant quantity of 3D printing related literature published recently, overall trends in the scope of 3D printing related basic research and applications in orthopedic surgery and publications and citations patterns related to the same remain underexplored. The number of scientific papers contributed by each country toward the global research output, along with the number of citations received by them, has become one of the critical indicators for assessing the strength of research in a nation.6, 7, 8 Since academic publications in a particular field, at least partly, reflect priorities and strategies, it is useful to analyze publication trends and compare them with trends in other related areas.9 The term bibliometrics refers to a set of techniques used to quantitatively analyze literature databases to find out the productivity, quality, performance, and publication trends of researchers, organizations, journals, countries or specific research areas. It reveals historical evolution, quantifies existing trends, and predicts the future of a given academic domain. The results can be used to analyze overall strengths and weaknesses (knowledge gaps) in the current evidence in a field, and for facilitating a comprehensive strategic plan for further advancement of the field.9, 10, 11 We aim to study the publication trends in 3D printing applications in orthopaedics.
2. Materials and methods
A literature search was performed to extract all papers related to 3D printing applications in orthopaedics and allied sciences using the suitable bibliometric approach on the Pubmed, Web of Science and SCOPUS databases. Suitable keywords and boolean operators (“3D Printing”, “3D printed, “3-dimensional printing”,“additive manufacturing,” “rapid prototyping,” Orthopaedics,” “Orthopaedics'’) were used, in May 2018. The search strategy used has been described in Table 1. Search was also attempted in Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, and DARE databases, using keywords 3D printing orthopaedics. A similar search was repeated in pubmed and SCOPUS to get more specific papers.
Table 1.
Literature search strategy.
| Search Strategy | Keywords combined with Boolean operators |
|---|---|
| 1. |
#1 “3D Printing” OR “3D printed” OR “3-dimensional printing” OR “additive manufacturing” OR “rapid prototyping.” |
| 2. |
#2 ‘‘Orthopaedics” OR “Orthopaedics’’ |
| 3. | #1 AND#2 |
No limit was set on the period or evidence level, as 3D printing in orthopaedics is relatively new and available evidence is usually limited to low-level studies. Trends in a publication on these topics were analyzed, focussing on some publications, type of research (basic science/engineering or clinical), type of publication, authors, institution, and country. Some citations received by these papers were also analyzed in SCOPUS and Web of Science. MS Excel (Microsoft Corporation) 2008 - Mac version and VOS Viewer1.6.8 (Leiden University, Leiden, Netherlands) 2018- Mac version software were used for analysis of the search results for publication trends and citation mapping respectively. The VOS viewer, a devoted citation network analysis, and visualization software were used for analysis of the relationships among cited references and productive authors, and also to generate the knowledge maps of authors, journals, keyword networks, and cited references related to 3D printing applications in Orthopaedics. Research is teamwork, and all authors and institutions contribute to a paper. So all the authors and institutions of papers were analyzed in the software.
The papers were then ranked and arranged according to the number of citations they received in SCOPUS. The top 10 most cited papers in the area of 3D Printing applications in orthopaedics in SCOPUS were tabulated, along with the number of citations they received along with citation density in SCOPUS and Web of Science. The final ranking was done as per the number of citations in SCOPUS, as it has more comprehensive coverage compared to the WoS.12, 13, 14, 15, 16, 17 and this was evident in our search also. We also looked for citations received by these articles in Google Scholar, a free citation database with extensive coverage, but we did not use it due to lack of quality control, incorrect citation counts, content gaps, duplication, and manipulation of citations.15,16
3. Results
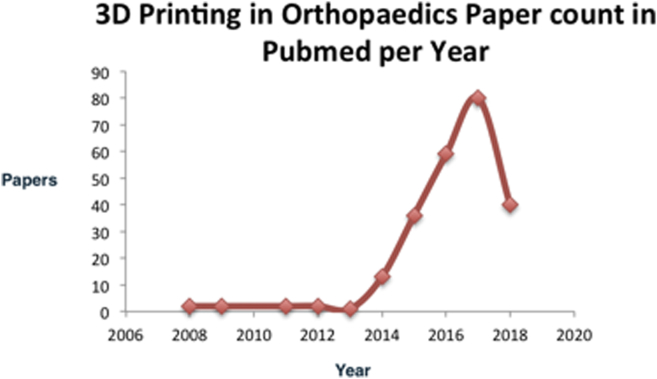
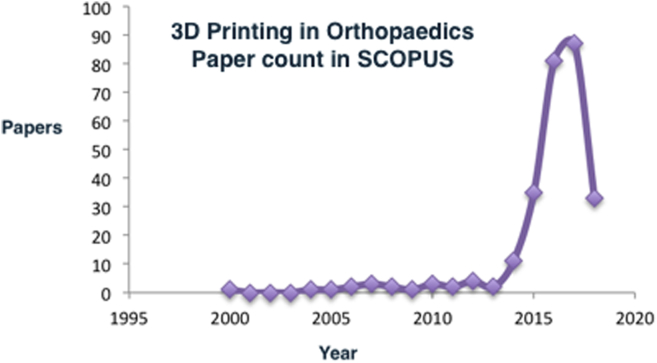
An increasing trend in research and publications involving applications of 3D printing in orthopedic surgery and related fields was observed, especially in the recent past (last ten years) (Fig. 1, Fig. 2). A search on Pubmed using the above strategy revealed 389 documents. A similar search revealed 653 documents on SCOPUS, many (314) of which were from an engineering background and only 271 were related to medicine. No papers were found in the Cochrane database. Search on TRIP database revealed 195 papers. A similar search revealed 237 papers on orthopedic applications on Pubmed and 269 documents on SCOPUS, whereas a search on Web of Science revealed only 23 papers. Publication trends were then analyzed on data derived from SCOPUS, which is the most comprehensive database.
Fig. 1.
An increasing trend in publications related to 3D printing in orthopedic surgery in Pubmed.
Fig. 2.
An increasing trend in publications related to 3D printing in orthopedic surgery in SCOPUS.
We have done some specific data analysis to see the trends of publications author, institution, country and journal-wise, as follow:
-
I)
Countries/regions contributing to global publications and growing trends in Orthopedic applications of 3D printing:
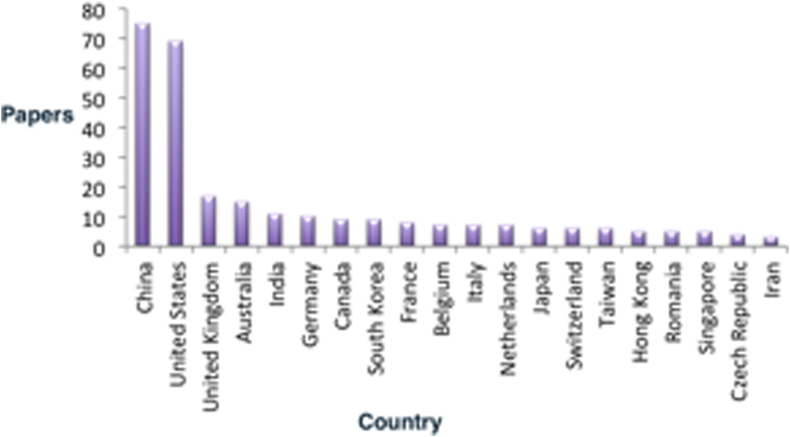
Overall, most papers were published from China (75), followed by United States (69), United Kingdom (17), Australia (15) and India (11). (Fig. 3).
-
II)
Institutions/universities contributing to global publications and growing trends in Orthopedic applications of 3D printing:
Fig. 3.
Distribution of countries/regions contributing to global publications in Orthopedic applications of 3D printing in SCOPUS data.
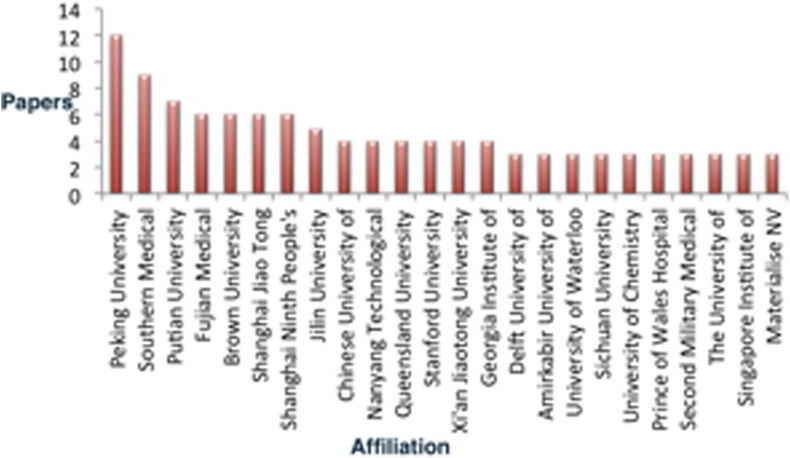
Most papers in 3D printing about orthopaedics were published from Peking University (12), followed by Southern Medical University (9), Putian University (7), Fujian Medical University (6), and Brown University (6). (Fig. 4).
-
III)
Distribution of authors of papers on 3D printing in Orthopaedics
Fig. 4.
Distribution of institutions/universities contributing to global publications in Orthopedic applications of 3D printing in SCOPUS data.
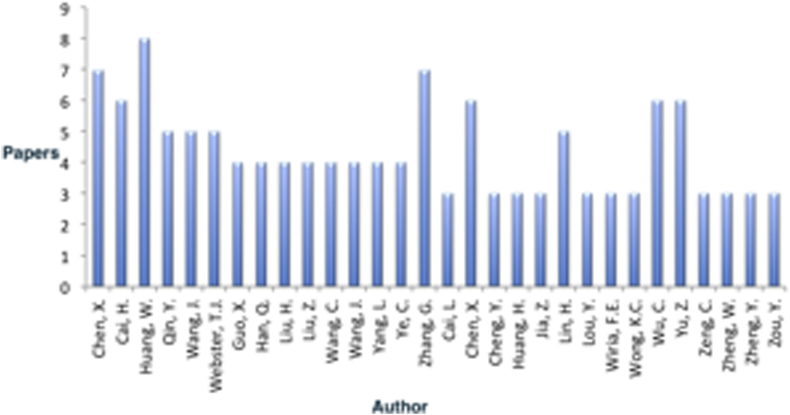
Huang W was the most published author on SCOPUS (8 papers), followed closely by Chen X (7 papers), Zhang G (7 papers) and Cai H (6 papers). (Fig. 5).
-
IV)
Distribution of published journals publishing papers on 3D printing in Orthopaedics:
Fig. 5.
Distribution of authors of papers on 3D printing in Orthopaedics in SCOPUS data.
Most 3D printing related work was published by Chinese Journal of tissue engineering research (15), followed by Acta Biomaterialia (6), Techniques in Orthopaedics (5), Injury (4) and Journal of Orthopedic research (4). (Fig. 6 and a and 6b).
Fig. 6.
Distribution of published journals publishing papers on 3D printing in Orthopaedics. – Overall distribution of SCOPUS data (Fig. 6a. Distribution of published journals publishing papers on 3D printing in Orthopaedics-Growth over the years in SCOPUS, Fig. 6b. Distribution of published journals publishing papers on 3D printing in Orthopaedics-in established orthopedic journals with growth over the years in SCOPUS).
If we consider Orthopedic journals only, most papers were published by Techniques in Orthopaedics (5), followed by Injury (4) and Journal of Orthopedic research (4), Journal of foot and ankle surgery (3), Orthopedic Surgery (3), and Orthopaedics and Traumatology (3) (Fig. 7). Two papers each also appeared in Indian Journal of Orthopaedics and Journal of Clinical Orthopaedics and Trauma.
-
V)
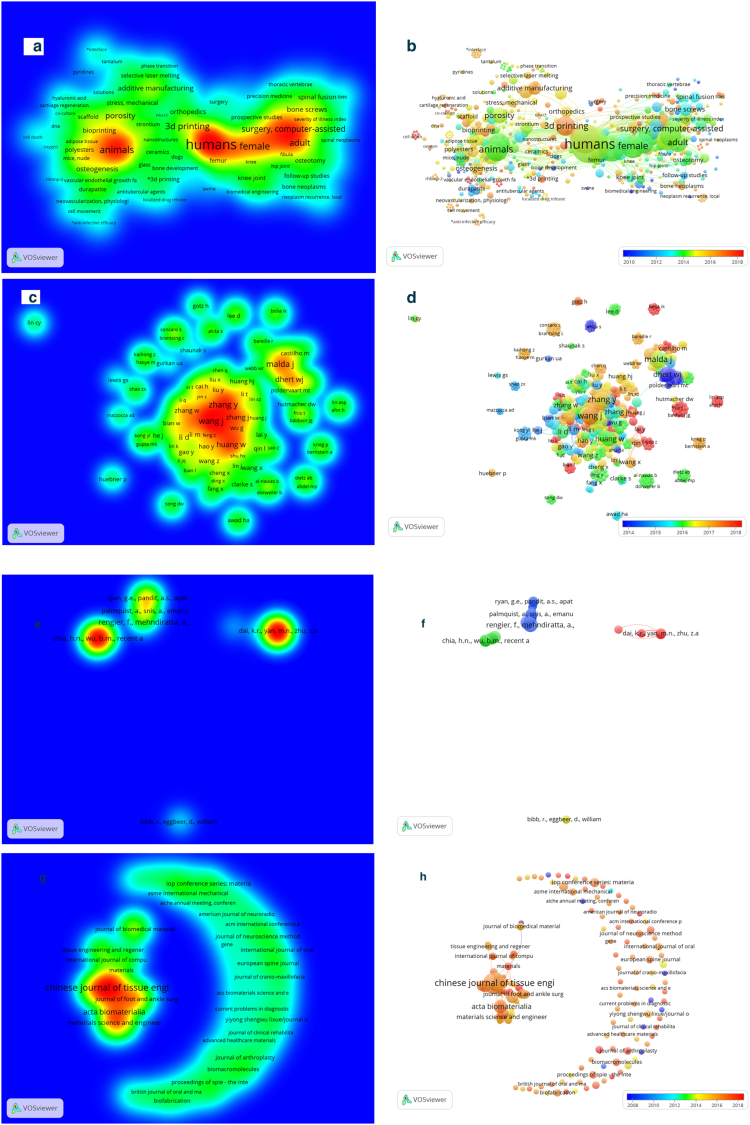
Keyword mapping, author mapping, and co-citation network visualization on VOSviewer revealed exciting trends. (Fig. 7a–h)
-
VI)
Citation analysis and top 10 papers
Fig. 7.
Knowledge mapping and network visualization on VOSviewer.
7a)Density visualization on keywords on 3D Printing in orthopaedics on Pubmed data. The words in the central red area were used most frequently.
7b)Networking of keywords in Pubmed data. Two terms are said to co-occur if they both occur on the same line. The smaller the distance between the two terms, the more significant the number of co-occurrences of the terms.
7c)Density visualization of co-authorship on 3D Printing in orthopaedics in Pubmed data.
7d)Networking of co-authorship in pubmed data.
7e)Density visualization of co-cited references on SCOPUS data. Different colors represent different co-cited times of articles. The color of an item was determined by the co-cited times, where by default colors range from blue (few times) to green (average times) to red (many times). Items in one red circle linked closer to each other than items in other areas. So the valuable papers with high co-cited times can be found in red circles.
7f)Networking on co-cited references of papers on 3D Printing in orthopaedics on SCOPUS data. Only a few papers were included. (The line between every 2 points means both were cited in one paper: if the line is thicker, the link between 2 papers is closer).
7g)Density visualization of journals publishing research on 3D Printing in orthopaedics in SCOPUS data.
7h)Networking of journals publishing research on 3D Printing in orthopaedics in SCOPUS data.
The top 10 most cited papers on SCOPUS on 3D printing in Orthopedic Surgery are shown in Table 2, along with citations received and citation density on SCOPUS and Web of Science (Table 2).
Table 2.
Top 10 most cited papers on 3D printing applications in orthopaedics.
| S no | Paper title | Citations in Scopus (Citation density) | Citations in WoS(Citation Density |
|---|---|---|---|
| 1 | Ryan GE, Pandit AS, Apatsidis DP. Porous titanium scaffolds fabricated using a rapid prototyping and powder metallurgy technique. Biomaterials. 2008 Sep 1; 29 (27):3625–35. | 182 (18.2) | 166 (16.6) |
| 2 | Sing SL, An J, Yeong WY, Wiria FE. Laser and electron-beam powder-bed additive manufacturing of metallic implants: A review on processes, materials and designs. Journal of Orthopedic Research. (2016) Mar 1; 34 (3):369–85. | 92 (46) | 94 (47) |
| 3 | Curodeau A, Sachs E, Caldarise S. Design and fabrication of cast orthopedic implants with freeform surface textures from 3-D printed ceramic shell. Journal of Biomedical Materials Research: An Official Journal of The Society for Biomaterials, The Japanese Society for Biomaterials, and The Australian Society for Biomaterials and the Korean Society for Biomaterials. 2000 Sep; 53 (5):525–35. | 90 (5) | 84 (4.67) |
| 4 | Marro A, Bandukwala T, Mak W. Three-dimensional printing and medical imaging: a review of the methods and applications. Current problems in diagnostic radiology. 2016 Jan 1; 45 (1):2–9. | 57 (28.5) | – |
| 5 | Martelli N, Serrano C, van den Brink H, Pineau J, Prognon P, Borget I, El Batti S. Advantages and disadvantages of 3-dimensional printing in surgery: a systematic review. Surgery. 2016 Jun 1; 159 (6):1485–500. | 52 (26) | 45 (22.5) |
| 6 | Tack P, Victor J, Gemmel P, Annemans L. 3D-printing techniques in a medical setting: a systematic literature review. Biomedical engineering online. 2016 Dec; 15 (1):115. | 47 (23.5) | 35 (17.5) |
| 7 | Sugawara T, Higashiyama N, Kaneyama S, Takabatake M, Watanabe N, Uchida F, Sumi M, Mizoi K. Multistep pedicle screw insertion procedure with patient-specific lamina fit-and-lock templates for the thoracic spine. Journal of Neurosurgery: Spine. 2013 Aug; 19 (2):185–90. | 37 (7.4) | 30 (6) |
| 8 | Xu N, Wei F, Liu X, Jiang L, Cai H, Li Z, Yu M, Wu F, Liu Z. Reconstruction of the upper cervical spine using a personalized 3D-printed vertebral body in an adolescent with Ewing sarcoma. Spine. 2016 Jan 1; 41 (1): E50-4. | 35 (17.5) | 26 (13) |
| 9 | Roohani-Esfahani SI, Newman P, Zreiqat H. Design and fabrication of 3D printed scaffolds with a mechanical strength comparable to the cortical bone to repair large bone defects. Scientific reports. 2016 Jan 19; 6:19468. | 33 (16.5) | 22 (11) |
| 10 | Rhee S, Puetzer JL, Mason BN, Reinhart-King CA, Bonassar LJ. 3D bioprinting of spatially heterogeneous collagen constructs for cartilage tissue engineering. ACS Biomaterials Science & Engineering. 2016 Aug 4; 2 (10):1800–5. | 29 (14.5) | 30 (15) |
4. Discussion and conclusion
Kacl et al., in 1997 found that rapid prototyping was useful in training and planning for surgery.18 His paper could not find any difference between stereolithography and workstation-based 3-D reformation for the treatment of intra-articular calcaneal fractures. Subsequently, many other researchers have reported the usefulness of 3D printing in orthopedic surgery. Yang et al. retrospectively studied the usefulness of this technique in the surgical management of idiopathic scoliosis and found that this technique might lower operative time and blood loss, but the rate of complications was unaltered.19 Guarino et al. treated ten patients with pediatric scoliosis and three patients with complex pelvic fractures and found that 3-D printing improved the accuracy of the pedicle and pelvic screw placement, thereby reducing the risk of iatrogenic neurovascular trauma.20 Brown et al. found that 3-D printing helped in planning for surgery and in reducing radiation exposure during 117 complex cases.21 Hurson et al. treated 12 patients with acetabular fractures classified and planned using 3D printing before surgery and proved that 3D models remarkably helped in surgeons' understanding the of individual fracture anatomy, especially so for novice surgeons.22 Maini et al. in their case-control study of ten cases (3D printing used for planning and recontoured plate manufacturing) and 11 controls (conventional planning and surgery) found that Patient-specific pre-contoured plate for acetabular fractures created with the help of a 3D model was a better-matched implant as compared to the intraoperatively contoured plate. Also, the 3D pelvic model provided an accurate technique for pre-operative planning for acetabular fracture surgery.23 Bagaria et al. found that 3D printing could help surgeons in understanding complex fractures and in achieving anatomical reduction where necessary.24 Xu et al. studied the value of 3D printing in surgical planning for developmental hip dysplasia cases and concluded that it facilitated surgery due to better preoperative planning and better surgeon orientation to complex individual anatomy.25
3D printing can help surgeons in creating surgical cutting guides and patient-specific instrumentation implants (PSIs) that can perfectly match an individual patients' anatomy. In total knee replacement (TKR), accurate bony cuts can be achieved, but some authors have reported no significant differences in overall alignment between PSI and conventional instrumentation, and further research was suggested for accessing the longevity and functional outcomes of prostheses implanted using PSI.26, 27, 28, 29, 30, 31, 32, 33, 34 Rathod et al.35 reported that PSI reduced bleeding in bilateral TKR, as it avoided intra-medullary instrumentation and Nunley et al.32 found that PSI reduced surgical time. Senior authors of this study (Vaishya et al.) found that CT based patient-specific blocks could help to achieve significantly better restoration of mechanical axis in cases undergoing primary total knee arthroplasty, and also proposed that it might lead to reduced revision rates.36 They also concluded that the extra cost and time necessary for CT scanning and customized block creation was offset by various advantages like lower operating time, lesser pain and blood transfusion needs, the lesser requirement for analgesics.37,38 However, in the latest study, they found that prediction of component size using computed tomography-based technology for PSI was not fooled proof, as accuracy for tibial and femoral components (72% and 66% respectively) were low and were, therefore, not fully reliable.39
Cartiaux et al.40 reported that PSI improved pelvic bone tumor resection by enabling right margins, whereas Bella-Nova et al.41 reported that PSI-assisted resection improved the accuracy of resection margins in tibial sarcoma. Kunz et al. utilized PSI for performing distal radial osteotomy and discovered that it helped in minimizing the requirement for intraoperative imaging.42 Otsuki et al.43 studied seven cases with acetabular dysplasia who were treated by PSI-assisted periacetabular osteotomy. Actual bony cut matched precisely with the planned cut. For the individually printed implants and synthetic devices, this technique is mainly being used for complicated cases, like pelvic and spinal tumors.44 Further research is necessary to find out its long-term clinical benefits, complications, and cost-effectiveness.45
Bone tissue engineering utilities the knowledge of cells, biomaterials and biochemical factors to create a scaffold which encourages cell attachment, proliferation and subsequent bone formation in vivo.46 3-D printing may be helpful for producing sophisticated and biocompatible scaffolds.47 Bioscaffold for bone regeneration must be structurally stable, and a flexible scaffold is necessary for cartilage regeneration. Structural parameters, like porosity, pore diameter, and interconnectivity, is controlled precisely by a computer program to maintain cell adhesion, proliferation, and differentiation. It may facilitate superior fracture healing.48, 49, 50 Calcium phosphate and hydroxyapatite are mainly used for porous scaffold fabrication, as they are very much biocompatible and are biodegradable. Low structural strength is the main challenge. Usually, scaffolds are used only for non-load bearing region.51 3D printing of bioscaffolds for cartilage and other tissues has also shown many advancements.52
A citation signifies the value given by the author to others' work on a given topic of interest.53 Scientometrics refers to a method using which the status of research and development and trends of the same in any scientific field can be accessed through accessing the publication output of scientific literature in that field.54
Scientometric indicators are appropriate for both macro-analysis (e.g., a given nation's share in the global scientific research output) and micro-studies (e.g., an institution's role in publishing scientific papers in a given field).55 This study explores the relationships among, authors, journals, citations and keywords through a provided algorithm and to find core groups by using the VOSviewer software. Knowledge mapping, also called visualization technology, includes gathering data, surveying, exploration, discovery, conversation, disagreement, analysis of knowledge gaps and finally synthesis. In the present study, co-author, keywords, and cluster analysis techniques were used for analyzing collaboration of authors, etc. through visualization or knowledge mapping technology.54,56,57
4.1. Hotspots of studies on 3D printing in orthopaedics and knowledge mapping
We found on keyword mapping on SCOPUS data using VOSviewer that there were two major niche areas of research and publication in 3D printing in orthopaedics. One involving animal studies including 3D bioprinting and other basic science studies, and another involving human study on applications of 3D printing in preoperative planning and patient-specific prosthesis, implants and instrumentation.
Similar mapping and network analysis show excellent networking of researchers in different countries and institutions. It shows that research groups are establishing in these areas. However, co-citation network map is not as strong. It may be because 3D Printing is a relatively new field, and a relatively small number of papers have been published in last few years. Many basic science and engineering journals, especially those on biomaterials have dominated on research and publications in 3D printing in the field of orthopaedics. However, in the last five years, many papers have appeared in well established orthopedic journals also, including several review articles1,2 and editorials/opinions4,5 aiming to acquaint orthopedic surgeons to the basics and applied aspects of 3D printing (Fig. 7a–h).
Ours is the first report of publication trends and knowledge mapping in 3D printing in Orthopaedics to the best of our knowledge. We tried to collect the data and analyze it comprehensively and objectively. Still, this study has few limitations that should be considered. Not all journals are indexed in Scopus, and therefore the total number of retrieved papers may be lower than their actual number. Also, we tried our best to use all the keywords relevant to our topic and also did a manual check, but some false positive or negative may still be there. For ranking, we extracted data from Scopus database. However, due to different spellings of author names or institution names, some authors may be shown to have multiple profiles that the authors themselves may not be not aware. Citation numbers vary with databases; questioning the usefulness and validity of such analyses. There are some of the problems with citation analysis like self-citation, preferential citation of articles in target journal, preference to cite English papers, etc.7,12, 13, 14, 15, 16, 17 Also, in VOSviewer, a minimum threshold was used to draw networks, and therefore, not all items could be shown. We are aware of these limitations and tried to reduce them, for example, by lowering the threshold in VOS viewer.
There has been an upsurge of interest in 3D printing in orthopedic surgery, as is evident by an increasing trend in research and publications in this area in recent years. Presently, 3D printing is in a primitive stage in the field of orthopedic surgery as our knowledge is still insufficient, and costs and learning curve are somewhat high. However, looking at latest publication trends, we are enthusiastic that it holds the key for future orthopaedics.
Footnotes
The manuscript has been approved by all authors, and they do not have any conflict of interest to be disclosed.
Contributor Information
Raju Vaishya, Email: raju.vaishya@gmail.com.
Mohit Kumar Patralekh, Email: mohit_patraekh@yahoo.co.in, mohitkumarpatralekh@gmail.com.
Abhishek Vaish, Email: drabhishekvaish@gmail.com.
Amit Kumar Agarwal, Email: amitorthopgi@yahoo.co.in.
Vipul Vijay, Email: dr_vipulvijay@yahoo.com.
References
- 1.Wong T.M., Jin J., Lau T.W. The use of three-dimensional printing technology in orthopaedic surgery: a review. J Orthop Surg. 2017 Jan 31;25(1) doi: 10.1177/2309499016684077. 2309499016684077. [DOI] [PubMed] [Google Scholar]
- 2.Gadia A., Shah K., Nene A. Emergence of three-dimensional printing technology and its utility in spine surgery. Asian Spine J. 2018 Apr 1;12(2):365–371. doi: 10.4184/asj.2018.12.2.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garg B, Gupta M, Singh M, Kalyanasundaram D. Outcome and safety analysis of 3D printed patient specific pedicle screw jigs for complex spinal deformities: A comparative study. The Spine Journal. Article in press. doi: 10.1016/j.spinee.2018.05.001. Available online at https://www.thespinejournalonline.com/article/S1529-9430(18)30200-6/fulltext on 3rd May 2018; last accessed on 24th July 2018. [DOI] [PubMed]
- 4.Vaish A., Vaish R. 3D printing and its applications in Orthopedics. J. Clin. Orthop. Trauma. 2018 Mar 1;9 doi: 10.1016/j.jcot.2018.02.003. S74-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trauner K.B. The Emerging Role of 3D Printing in Arthroplasty and Orthopedics. The Journal of arthroplasty. J Arthroplasty. 2018;33(8):2352–2354. [Google Scholar]
- 6.Kanna R.M., Falavigna A., da Silva P.G. Trends in scientific publications of Indian spine surgeons over 14 years. Indian J Orthop. 2000-2013;2016(50):322–326. doi: 10.4103/0019-5413.181797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaishya R., Patralekh M., Vaish A., Agarwal A.K., Vijay V. The top 10 most cited indian articles in arthroscopy in last 10 years. Indian J Orthop. 2017;51(5):505–515. doi: 10.4103/ortho.IJOrtho_168_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaishya R., Patralekh M.K., Bijukchhe A.R., Vaish A., Vijay V., Agarwal A.K. The top 10 arthroplasty articles published in last 10 years by Indian authors. J. Clin. Orthop. Trauma. 2018 Jan 1;9(1):94–100. doi: 10.1016/j.jcot.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sweileh W.M., Sawalha A.F., Al-Jabi S.W., Sa’ed H.Z., Shraim N.Y., Abu-Taha A.S. A bibliometric analysis of literature on malaria vector resistance:(1996–2015) Glob Health. 2016 Dec;12(1):76. doi: 10.1186/s12992-016-0214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang F., Jia X., Wang X., Zhao Y., Hao W. Particulate matter and atherosclerosis: a bibliometric analysis of original research articles published in 1973–2014. BMC Publ Health. 2016 Dec;16(1):348. doi: 10.1186/s12889-016-3015-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yao Q., Chen K., Yao L. Scientometric trends and knowledge maps of global health systems research. Health Res Pol Syst. 2014 Dec;12(1):26. doi: 10.1186/1478-4505-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fingerman S. Web of science and Scopus: current features and capabilities. Issues Sci Technol Librarianship. 2006:48. http://www.istl.org/06-fall/electronic2.html12 Available online from: [Google Scholar]
- 13.Burnham J.F. Scopus database: a review. Biomed Digit Libr. 2006;3(1) doi: 10.1186/1742-5581-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.LaGuardia C. E-views and reviews: Scopus vs.Web of science. Libr J. 2005;130:40–43. [Google Scholar]
- 15.Jacso P. As we may search-comparison of major features of the Web of Science, Scopus, and Google Scholar citation based and citation-enhanced databases. Curr Sci. 2005;89:1537–1547. [Google Scholar]
- 16.Waltman W. A review of the literature on citation impact indicators. J Inf. 2016;10:365–391. [Google Scholar]
- 17.Martínez M.A., Herrera M., López-Gijón J., Herrera-Viedma E. H-Classics: characterizing the concept of citation classics through H-index. Scientometrics. 2014;98:1971–1983. [Google Scholar]
- 18.Kacl G.M., Zanetti M., Arngwerd M. Rapid prototyping (stereolithography) in the management of intra-articular calcaneal fractures. Eur Radiol. 1997;7(2):187–191. doi: 10.1007/s003300050132. [DOI] [PubMed] [Google Scholar]
- 19.Yang M., Li C., Li Y. Application of 3D rapid prototyping technology in posterior corrective surgery for Lenke 1 adolescent idiopathic scoliosis patients. Medicine. 2015;94(8):e582. doi: 10.1097/MD.0000000000000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guarino J., Tennyson S., McCain G. Rapid prototyping technology for surgeries of the pediatric and pelvis. J Pediatr Orthop. 2007;27(8):955–960. doi: 10.1097/bpo.0b013e3181594ced. [DOI] [PubMed] [Google Scholar]
- 21.Brown G.A., Firoozbakhsh K., DeCoster T.A. Rapid prototyping: the future of trauma surgery? J. Bone Joint Surg. Am. 2003;85-A(Suppl 4):49–55. [PubMed] [Google Scholar]
- 22.Hurson C., Tansey A., O'Donnchadha B. Rapid prototyping in the assessment, classification and pre-operative planning of acetabular fractures. Injury. 2007;38:1158–1162. doi: 10.1016/j.injury.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 23.Maini L., Sharma A., Jha S., Tiwari A. Three-dimensional printing and patient-specific pre-contoured plate: future of acetabulum fracture fixation? Eur J Trauma Emerg Surg. 2018;44(2):215–224. doi: 10.1007/s00068-016-0738-6. [DOI] [PubMed] [Google Scholar]
- 24.Bagaria V., Deshpande S., Rasalkar D.D. Use of rapid prototyping and three-dimensional reconstruction modeling in the management of complex fractures. Eur J Radiol. 2011;80(3):814–820. doi: 10.1016/j.ejrad.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 25.Xu J., Li D., Ma R.F. Application of rapid prototyping pelvic model for patients with DDH to facilitate arthroplasty planning: a pilot study. J Arthroplasty. 2015;30(11):1963–1970. doi: 10.1016/j.arth.2015.05.033. [DOI] [PubMed] [Google Scholar]
- 26.Barrack R.L., Ruh E.L., Williams B.M. Patient-specific cutting blocks are currently of no proven value. J Bone Joint Surg Br. 2012;94:95–99. doi: 10.1302/0301-620X.94B11.30834. [DOI] [PubMed] [Google Scholar]
- 27.Boonen B., Schotanus M.G., Kort N.P. Preliminary experience with the patient-specific templating total knee arthroplasty. Acta Orthop. 2012;83:387–393. doi: 10.3109/17453674.2012.711700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chareancholvanich K., Narkbunnam R., Pornrattanamaneewong C. A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. Bone Joint J. 2013;95(3):354–359. doi: 10.1302/0301-620X.95B3.29903. [DOI] [PubMed] [Google Scholar]
- 29.Dossett H.G., Swartz G.J., Estrada N.A. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics. 2012;35:e160–e169. doi: 10.3928/01477447-20120123-04. [DOI] [PubMed] [Google Scholar]
- 30.Ng V.Y., DeClaire J.H., Berend K.R. Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012;470:99–107. doi: 10.1007/s11999-011-1996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Noble J.W., Jr., Moore C.A., Liu N. The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplast. 2012;27:153–155. doi: 10.1016/j.arth.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 32.Nunley R.M., Ellison B.S., Ruh E.L. Are patient-specific cutting blocks cost effective for total knee arthroplasty? Clin Orthop Relat Res. 2012;470(3):889–894. doi: 10.1007/s11999-011-2221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nunley R.M., Ellison B.S., Zhu J. Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop Relat Res. 2012;470(3):895–902. doi: 10.1007/s11999-011-2222-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vundelinckx B.J., Bruckers L., DeMulder K. Functional and radiographic short-term outcome evaluation of the Visionaire system, a patient-matched instrumentation system for total knee arthroplasty. J Arthroplasty. 2013;28:964–970. doi: 10.1016/j.arth.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 35.Rathod P.A., Deshmukh A.J., Cushner F.D. Reducing blood loss in bilateral total knee arthroplasty with patient-specific instrumentation. Orthop Clin North Am. 2015;46(3):343–350. doi: 10.1016/j.ocl.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Vaishya R., Vijay V., Birla V., Agarwal A.K. CT based ‘Patient Specific Blocks’ improve postoperative mechanical alignment in primary Total Knee Arthroplasty. World J Orthop. 2016;7(7):426–433. doi: 10.5312/wjo.v7.i7.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vaishya R., Vijay V. Patient-specific instruments in total knee arthroplasty. Int Orthop. 2014;38:1123. doi: 10.1007/s00264-014-2335-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vaishya R., Vijay V., Agarwal A.K. Functional outcome and quality of life after Patient-Specific Instrumentation (PSI) in Total Knee Arthroplasty (TKA): our concerns. J Arthroplasty. 2016;31(4):924. doi: 10.1016/j.arth.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 39.Vaishya R., Vijay V., Krishnan M., Agarwal A.K. Fallacies of CT based component size prediction in total knee arthroplasty – Are patient-specific instruments the answer? J Clin Orthop Trauma. 2018;9(1):34–39. doi: 10.1016/j.jcot.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cartiaux O., Paul L., Francq B.G. Improved accuracy with 3D planning and patient-specific instruments during simulated pelvic bone tumor surgery. Ann Biomed Eng. 2014;42(1):205–213. doi: 10.1007/s10439-013-0890-7. [DOI] [PubMed] [Google Scholar]
- 41.Bellanova L., Paul L., Docquier P.L. Surgical guides (patient-specific instruments) for pediatric tibial bone sarcoma resection and allograft reconstruction. Sarcoma. 2013;2013 doi: 10.1155/2013/787653. 787653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kunz M., Ma B., Rudan J.F. Image-guided distal radius osteotomy using patient-specific instrument guides. J Hand Surg. 2013;38A:1618–1624. doi: 10.1016/j.jhsa.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 43.Otsuki B., Takemoto M., Kawanabe K. Developing a novel custom cutting guide for curved peri-acetabular osteotomy. Int Orthop. 2013;37(6):1033–1038. doi: 10.1007/s00264-013-1873-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wong K.C., Kumta S.M., Geel N.V. One-step reconstruction with a 3D-printed, biomechanically evaluated custom implant after complex pelvic tumor resection. Comput Aided Surg. 2015;20(1):14–23. doi: 10.3109/10929088.2015.1076039. [DOI] [PubMed] [Google Scholar]
- 45.Xu N., Wei F., Liu X. Reconstruction of the upper cervical spine using a personalized 3d-printed vertebral body in an adolescent with Ewing sarcoma. Spine (Phila Pa 1976) 2016;41(1):E50–E54. doi: 10.1097/BRS.0000000000001179. [DOI] [PubMed] [Google Scholar]
- 46.Peltola S.M., Melchels F.P., Grijpma D.W. A review of rapid prototyping techniques for tissue engineering purposes. Ann Med. 2008;40(4):268–280. doi: 10.1080/07853890701881788. [DOI] [PubMed] [Google Scholar]
- 47.Hoque M.E., Hutmacher D.W., Feng W. Fabrication using a rapid prototyping system and in vitro characterization of PEG-PCL-PLA scaffolds for tissue engineering. J Biomater Sci Polym Ed. 2005;16(12):1595–1610. doi: 10.1163/156856205774576709. [DOI] [PubMed] [Google Scholar]
- 48.Billiet T., Vandenhaute M., Schelfhout J. A review of trends and limitations in hydrogel-rapid prototyping for tissue engineering. Biomaterials. 2012;33(26):6020–6041. doi: 10.1016/j.biomaterials.2012.04.050. [DOI] [PubMed] [Google Scholar]
- 49.Huang S.L., Wen B., Bian W.G. Reconstruction of comminuted long-bone fracture using CF/CPC scaffolds manufactured by rapid prototyping. Med Sci Monit. 2012;18(11):BR435–BR440. doi: 10.12659/MSM.883536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zein I., Hutmacher D.W., Tan K.C. Fused deposition modeling of novel scaffold architectures for tissue engineering applications. Biomaterials. 2002;23(4):1169–1185. doi: 10.1016/s0142-9612(01)00232-0. [DOI] [PubMed] [Google Scholar]
- 51.Miranda P., Pajares A., Saiz E. Mechanical properties of calcium phosphate scaffolds fabricated by robocasting. J Biom ed Mater Res A. 2008;85A:218. doi: 10.1002/jbm.a.31587. [DOI] [PubMed] [Google Scholar]
- 52.Shaunak S.S., Dhinsa B.S., Khan W. The role of 3D modeling and printing in orthopedic tissue engineering: a review of the current literature. Current stem cell research & therapy. 2017 Apr 1;12(3):225–232. doi: 10.2174/1574888X11666160429122238. [DOI] [PubMed] [Google Scholar]
- 53.Banaszkiewicz P.A. Main introduction. In: Banaszkiewicz P.A., Kader D.F., editors. Classic Papers in Orthopaedics. 1st ed. Springer-Verlag; London: 2014. pp. 1–3. [Google Scholar]
- 54.Yao Q., Chen K., Yao L. Scientometric trends and knowledge maps of global health systems research. Health Research Policy and Systems. 2014;12:26. doi: 10.1186/1478-4505-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pouris A., Pouris A. Scientometrics of a pandemic: HIV/AIDS research in South Africa and the World. Scientometrics. 2011;86:541–552. [Google Scholar]
- 56.Dang Y., Zhang Y.L., Hu P.J.H., Brown S.A., Chen H.C. Knowledge mapping for rapidly evolving domains: a design science approach. Decision Support Systems. 2011;50:415–427. [Google Scholar]
- 57.Zhang S.L., Wang J.P., Zhao Y.J. Proceedings of the 7th National Conference on Functional Materials and Applications (FMA 2010 E-BOOK) 2010. Analysis of international proprietary technology development of solid state lighting material; pp. 984–992. [Google Scholar]