Abstract
Abstract Aim: To study the objectives, processes, and ideologies expressed during participatory design of information systems (PDIS) in health care.
Design: Longitudinal documentation of project meetings by video recording. Grounded theory development in three steps.
Setting: Systems development project in primary care.
Results: The developing system was discussed mainly from a clinical and practical, as opposed to a technical, viewpoint. The design decisions were related to societal-level participants and institutions. This external influence on design decisions was mediated by design voices in discussions, each having its own scope.
Conclusions: The social environment has to be considered when applying PDIS in health care. Instructions for nondesigners can be used to introduce them to the design objectives, processes, and ideologies on which PDIS is based and to support them when relating clinical and practical design questions to the existing social constraints and norms.
Every time a patient contacts a health care professional, the information handled includes patient data, scientific knowledge, and professional communication.1 Technical systems used in this environment must therefore meet a variety of goals, adhere to work routines, and serve different users.2 When such complex information systems are designed, the early design phase, when the overall design is specified, is crucial. This early phase in systems development has seldom been addressed in medical informatics.3 In the field of informations systems development, the early stages in design have been a focus of organizational change analyses during in-house development4 and in software engineering as requirements engineering for product development.5
An alternative approach is participatory design,6 an emerging software design strategy characterized by active engagement of the end-users in all the phases of design. It is iterative in nature and grounds information system design in the end-user's perspective of work. For example, when physician users describe their diagnostic tasks, they identify data elements and communication functions that a system must support. After repeated discussions with various groups of users, the multiple system perspectives are integrated into a composite information strategy that can later be implemented using a wide range of system engineering tools.
Participatory design follows from an emerging philosophy of knowledge representation and system design that makes a clear separation between the conceptual model of a system and the implementation model. It represents a departure from traditional approaches to information system design and software engineering in that it emphasizes system functionality and rapid prototyping rather than system performance and technical production.7 For instance, by using video or workflow graphs, co-viewing settings are constructed to “bring the field home” to designers.8 The approach has been used both for in-house and commercial system development.9
Although participatory design has been available, few have attempted to use it in health care.10 A reason for this may be the theoretic background, which has shifted from ideologic aims toward making the design process more cooperative and efficient.11 The objective has thus changed from strengthening the practitioners' rights to quality and productivity in the service or product delivery.12 This hesitation to use the method is worth noticing, since in theory it is consistent with current general trends regarding design—i.e., that an artifact should be the result of the social exchange in a design group13 and that design should be performed close to users.14
The aim of this study is to develop a model of design objectives, processes, and ideologies as these are expressed during participatory design of information systems (PDIS) in health care. The intention is that the model should make it possible for system developers to structure the decision to use PDIS. The study is based on qualitative research methods and uses data from one particular system design setting.15
Support of Teamwork in Primary Care
The project was a system development collaboration at a primary care center in the town of Linköping (pop. 120,000), Sweden. At the time of the study, the center employed eight general practitioners (GPs) and 52 other staff, including nurses, district nurses, occupational therapists, and physiotherapists. Each GP team had about 2,500 patients listed. The number of patient appointments at the center ranged between 200 and 225 per day. The project objective was to develop a national demonstrator for how modern computer network technology could be used for support of teamwork and organizational learning in health care. The partners were the county council, responsible for the health care provision in the area, a software company, and researchers from the local university.16
The computer system was to be a combination of adapted commercial products and software developed within the project. The commercial products were jointly chosen by the project partners from listings of equipment accredited by the county council. The objective was to merge three system types: Web site authoring and presentation systems, electronic messaging, and a computerized patient record (CPR). The implementation was to be built on the OLE 2.0 standard and a client-server architecture. For the management of hypermedia documents, the Synkop Interactive Reference Book system was used, based on the MEDEA prototype.17,18 The hypermedia prototype held 5,000 text pages at the time of the study, and 400 color images linked to the texts. The software for electronic messages was implemented using modules from the ICL Embla and Microsoft Mail e-mail interfaces, and connections over a firewall to the local Internet node. The CPR chosen for the project was a commercial product (DialogJournalen) for use in primary care. The system supported a full-text medical record, a controlled medical terminology, a structured patient database, and tools for analyzing and reporting patient data.
The development of the information system followed the action design method,19 which prescribes a smallgroup design process with equal participation from health care practitioners, designers, and engineers. An agenda was prepared for each meeting, and before the close of each session the meeting process was evaluated. In the beginning the meeting agenda was prepared by the design team and later by the health care team. Equal-opportunity rules were used during the small-group meetings (see Appendix).20 The role of the chairman was taken in turn by the design group members.
Methods
Data Collection
The data consist of video recordings from all 13 participatory design meetings held in the case study project over a two-year period. The design meetings, which lasted between one and two hours, were documented in approximately 24 hours of video recordings. On average, 11 participants were present at each meeting and each member participated in an average of six meetings. Two GPs, three nurses, two district nurses, a nurse's aide, a secretary, and an external pharmacist represented primary care. The designers were a systems analyst, a system designer with a background in health care, a psychologist, four engineers, and an external medical engineer. The recordings were transcribed by the first author and extended to 300 pages and 6,400 utterances. Out of concern for the ethical aspects of transcribing real-life dialogues, fictitious names of persons, places, and organizations were used.
Data Analyses
The structured version of the grounded theory method was used for the analyses.21 Three analysis cycles were finished, and for every cycle a new research question was added. In each cycle, the meeting data was read and worked through by open coding, when conceptual labels were placed on all observed events, and axial coding, where the data were put back in a new way depending on interactional strategies and consequences. The final model was constructed by selective coding, by which the emerging dimensions were combined into an integrated model.
In the first analysis cycle, the research question was what issues the PDIS group dealt with throughout the design process. The transcribed data were divided into topics, which were found to be overlapping and therefore coded into more general concepts. From these, using axial coding methods, four themes were constructed and illustrated with excerpts from the meetings. For the second analysis cycle, the research question was how the different intentions of the members of a multidisciplinary design group influence their way of expressing themselves in design discussions. To analyze the meeting interaction from this perspective, a definition of voice was formulated from sociocultural theory22,23: “A voice is employed by a speaker in a dialogue to express the speaker's intention, perspective, and orientation. The voice is the user of different social languages. A speaker in a dialogue shifts voice depending on the intention of the utterance.”
A set of design voices was identified.24 These were applied to the data to analyze how the voices were used during the entire design process.
For the third analysis cycle, the research question was how the external contexts and conditions referred to by the participatory design group influence the design. Three social arenas were thus distinguished. Each meeting in the participatory design group was studied from the identified arenas and a set of typical utterances for each arena in each meeting was collected. Finally, to conceptualize the design process, the theme, voice, and arena dimensions were connected to each other for the purpose of visualizing their relations.
Results
The PDIS meetings were based on four discussion themes: clinical practice, system design, cooperation, and the project. The specific topics ranged from abstract issues, such as professionalism in health care, to concrete subjects, such as furnishing a surgery. References to work practice appeared constantly throughout all meetings.
The themes were addressed in three voices, which differed in the ways they were used during meetings (e.g., the approach to power and ways of storytelling): 1) the voice of participatory design, characterized by coordination, consensus, and comparative stories; (2) the Voice of Practice, characterized by work, challenge and “war stories” from clinical experience; and 3) the Voice of Engineering, characterized by technology, explanation, and theoretic anecdotes. Over time, the use of the voices was distributed among most group members. The voice of participatory design, in particular, came to be applied independent of professional background. This voice appeared as an adhesive in the dialogues and was used by the design group to balance the other two voices. The voice of practice was used for joint telling of clinical stories.
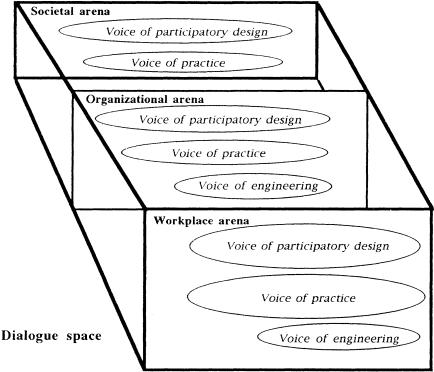
The design discussions took place in three arenas, which show how the PDIS process was related to the social environment (▶). A workplace arena was used to make references to colleagues, to organizational changes at the health care center, and to the work in the PDIS group. An organizational arena was entered for general references to other clinical organizations involved in the process, the county council and primary care management. The societal arena was used for references to health care, the political system, and the funding providers, i.e., describing a local, national, and international community level.
Figure 1.
The observed dialogue space for participatory design of information systems (PDIS) in health care. The relationship between the design voices and dialogue arenas is displayed. Discussions of clinical issues, the system, cooperation and the project (the design themes) are performed in different voices and move constantly between the dialogue arenas. Note that the voice of engineering is not represented in the societal arena.
The Model Exemplified
The model uses the constructs theme, voice, and arena to display the connection between the meeting content, the personal interaction, and the power relations involved in the design. The voices mediate influences from background societal institutions on the design meetings. Having strong foundations in the societal and workplace arenas, the voice of participatory design and the voice of practice came to dominate the development of the meeting themes in the case study project. Consequently, because it lacked a corresponding structural basis, the voice of engineering was given mainly a consultative position in the design. This dominance is expressed in the boxed excerpt, in which the cooperation theme, the three voices, and the three arenas are evident.
In line 120 of the excerpt, an engineer uses the voice of engineering to address the practitioners to explain electronic messaging. This utterance is situated in the organizational arena, by the use of references to other applications and sites. The viewpoint is questioned by a designer in the voice of participatory design, who demands a clarification from the engineer (lines 121 and 123). The designer's critique starts by stating a difficulty in understanding, i.e., that the engineer has not explained the issue in an accurate manner. The argument is strengthened by visits to the societal arena (line 121), with references to the county council. The designer connects the project goals to council plans with the aim of fitting the technology to practice. Yet when the engineer agrees in the voice of participatory design (line 122), the designer moves back to the workplace arena and tries to cooperate with the engineer by pointing to the need to mention patient information in e-mail. This statement is further supported by the engineer who, in the voice of participatory design, moves up to the societal arena and also refers to the county council policy and their e-mail system (line 124). The designer agrees (line 125), the two seem to have settled, and the conflict appears to be straightened out.
In this example the design at the workplace level (an e-mail system to send patient information) was influenced by structures in the organizational and societal arenas (policies and accredited e-mail system to be used by all health care units). As the meeting proceeded, however, the external engineer changed back to the voice of engineering and challenged the designers, now in the organizational arena. This time she revealed information not previously known to the other engineers and designers in the group (line 126). The computer department at the county council could provide the health care center with the e-mail function. Thus, once again the social power of external organizations was used to influence the design. One of the practitioners (GP1) tried to enter the discussion (line 127) but was interrupted by Designer 1 (line 128). The designer tried, in the voice of design, to end the discussion and postpone the decision by referring to two other engineers not present at the meeting. The expression “but I see the problem as yours” was a means to distance the engineer from the participatory design group and the design content. The designer used and was in control of the structures in the workplace arena. The issue was also left without the involvement of the computer department.
Yet, to finish this dialogue sequence, the practitioner returned in the voice of practice to “we who are out in the field,” an utterance in the workplace arena. For the practitioners, at the time of the discussion, it was important to have an e-mail system that would support work routines. The GP declared that the technical part of the problem was uninteresting. It seemed that until the technical issues were solved, the practitioners were not interested in discussing the matter. Here the voice of practice was powerfully used, and the practitioner managed to turn the issue into a secondary technical problem to be solved by the designers.
Limitations of the Model
The project leaders and the management of the health care center were not always present at the meetings. When they were present, the discourse became more often located in the societal arena and the design group came to address health care practice and the participatory design process. It might be that, because software product suppliers were not represented in the group, the representation of technical matters in the societal arena was missing in the case study project. Hence, the group composition seems to have a major impact on the constitution of democracy in the PDIS process. If the group had been composed differently—with a stronger representation of engineers from industry, for instance—the themes, voices, and arenas would have had a different internal relationship.
Discussion
Based on meeting data, the results describe the design objectives, processes, and ideologies expressed during PDIS in health care. In accordance with the user-centered ideology, the developing system was discussed mainly from a clinical-practical, as opposed to a technical, point of view. The design decisions were also closely related to societal-level participants and institutions. This external influence on the design group was mediated in discussions by design voices, each having its own scope. The voices were not bound to specific persons or roles but could be used by any member in the design team.
Previously, industrial software design projects have been found to be situated within corporate culture, politics, and procedures.25,26 In socialized health care, the services provided are under public, rather than customer, control. Changes in society at large can therefore influence the health care organization through both political and administrative mechanisms.27 These complex influences on the decision-making in an information system design group have to be considered and dealt with when using PDIS in health care. To support a more prevalent use of the method, additional research is needed, e.g., on the design arena concept.▶
Table 1.
| Excerpt from Participatory Design Meeting |
| 120 External engineer: No, because in the other CPR system, [trade name 1], they have used internal electronic mail in the health care system, you know, and it's perfectly alright and it is used extensively to send messages to each other. You don't have it in [trade name 2], it's supposed to be a complement within Primus and to use this other mail system...the large mail system...they say there will be a mail then and we have to get along with encryption so it gets going. |
| 121 Designer 1:...well, but I'm not really with it, this within Primus. You're saying it because, when [the head at the computer department at the county council] was present...discussions were that we should wait and see which mail system the county council is going to settle for themselves. And then there was, because he said so last at the last meeting here in fact that...er...that he was about to, well, get it here. It is important that we don't deviate from the traditional mail system chosen by the county council. |
| 122 External engineer: Yes, right! |
| 123 Designer 1: And we have had discussions with your group/turns to the External Engineer/, that we want to do exactly what you're after with being able to encrypt and send documents. Which is something between an e-mail |
| 124 External engineer: Yes, but this is what I have been trying to get across, too, that we must choose, according to the county council policy, a certain system. |
| 125 Designer 1: Exactly. |
| 126 External engineer: And this is because they're going to create a post for being in charge of mail and then it will be so that we can use the service just like all the other units. But at the same time we have problems, we need to send information, and I thought that this was part of the encryption we had talked about as a complement to the county council standard.... |
| 127 GP1: Questions.... |
| 128 Designer 1 (Turns to the external engineer): Well, we have just talked, but I see the problem as yours and that's why I want to take your request to Erik and Anders [two engineers not present at the meeting] who can go through this and look at.... |
| 129 GP1: I think it is...actually we who are out in the field believe that this [encrypted mail] will come automatically...and I have...said different things and sometimes I don't follow the technical way of thinking, and I think that I feel we haven't been clear enough about that this doesn't work. |
The study was performed in a Scandinavian context, which has to be taken into consideration when assessing the general applicability of the model. The PDIS process was observed to have its foundations in the societal and workplace arenas. In other contexts, the organizational arena—including, for instance, software companies—could have had more influence. Even though there are differences between Scandinavia and the United States in economic and political systems, however, the health care policies are converging towards similar managed care models.28 The PDIS method used in this study is representative of the Scandinavian participatory design approach, for example, by the fact that equal opportunity rules are used.20 The project may still not be altogether consistent with a typical PDIS process.29,30 The design group was comparatively large. At times, the group consisted of 11 members, which could have had a negative effect on efficiency. In other studies, the design groups have been smaller.31 Furthermore, the group was extended during the design process to include new designers, engineers, and practitioners, to serve the needs gradually identified by the group. Other design groups in other studies may have been more stable. Moreover, this group was not solely a product design group11 or a product test group, which does not benefit from the design results. Instead, it was a combination of these, because the systems developed and the organizational model were intended to be used at the workplace on a daily basis and later to be developed into commercial products. Such a setting is still not unusual for medical informatics projects. A more substantial shortcoming of this study, however, is that the patient perspective was not represented by membership in the design group. Further study and development of PDIS in health care, in which patients' views are made more central in the design process, is therefore necessary.
The qualitative research method based on a case study provided a rich picture of one PDIS setting.32 When the present study is compared with previous qualitative research in medical informatics, a distinction must be made between studies of technology use in clinical practice and studies of design processes. While the former type of study has become prevalent,33,34,35 the latter, to which this study belongs, is less common. For both types, it must be remembered that qualitative research is not a design method. A misconception may prevail within the medical informatics community that empirical research can be built directly into systems design. Before research results can be used by a design group, however, any description or conception has to be transformed into a representation that can be interpreted as an argument, i.e., that can help to decide between design alternatives.36 It is important to consider this design orientation when planning studies of systems development.
In PDIS, the intention has been to maintain a close connection between research results, local data, personal experiences, and their use in design. Several implications for implementing PDIS in health care follow from this study. One is that it is necessary to consider what form of participation is used.10 When a strong participatory approach is established, the design group members have an equal control over information and decisions. Arnstein37 describes a ladder of participation, from manipulation and therapy to delegated power and control. Common to most of these settings, however, is the fact that the instructions for the design process are written for the designers, while few guidelines are available for direct use by the other participants.20 The most important message to take away from this study is, thus, that special design instructions for nondesigners should be used to introduce them to the design objectives, processes, and ideologies on which PDIS is based. This would support them in relating the clinical-practical questions to the existing societal constraints and increase the ways they might find to influence the development process.38 In this way, PDIS methods can come to support the development of systems that are both situated in the clinical workplace and approved by external participants and institutions.
Appendix
Participatory Design Meeting Rules Applied in the Case Study Project
The rules should be applied as a whole set in the work group. After each meeting, the participants are to discuss whether the rules are being followed and report if they are not.
Session Chairman Rules
The chairperson:
Is elected for one meeting at a time.
Makes sure that the meeting form is shared in the group.
Ensures that the meeting form is followed.
Carries out the meeting plan.
Summarizes the meeting by asking the participants how they personally experienced the meeting and what the meeting gave them, and how they think the group handled their task.
Closes the meeting by announcing the time of the next meeting.
Group Rules
The basic principle for the dialogue during a meeting is free sharing of ideas and opinions.
All involved in the subject discussed should have the opportunity to participate in the meeting.
Attendance is not enough. Everybody has to be active. Each person should both give their own opinions and help other participants to give theirs.
All participants have equal rights in the dialogue.
Everyone's work experience should be the basis of the dialogue (in our case, health care and systems development work).
All involved must be able to understand the discussion.
All statements must be personal, i.e., `He thinks that...' is not an acceptable statement.
All participants should try to settle or explore differences in opinions within the group.
The dialogue should lead to a common action.
All participants should immediately let others know if they think that someone is not following any of the above rules.
References
- 1.Covell DG, Uman GC, Manning PR. Information needs in office practice: are they being met? Ann Intern Med. 1985; 103: 596-9. [DOI] [PubMed] [Google Scholar]
- 2.Lorenzi NM, Riley RT, Blyth AJC, Southon G, Dixon BJ. Antecedents of the people and organizational aspects of medical informatics: review of the literature. J Am Med Inform Assoc. 1997;4: 79-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forsythe DE. Blaming the users in medical informatics: the cultural nature of scientific practice. Knowledge and Society. 1992;9: 95-111. [Google Scholar]
- 4.Goldkuhl G, Röstlinger A. The legitimacy of information systems development: a need for change analysis. In: Proceedings of the First IFIP Conference on Human-Computer Interaction. London: IFIP, 1984.
- 5.Boehm BW. A spiral model of software development and enhancement. Computers. 1988;21: 61-72. [Google Scholar]
- 6.Special Issue on Participatory Design. Communications of the ACM. 1993;36.
- 7.Luff P, Heath C, Greatbatch D. Work, interaction and technology: the naturalistic analysis of human conduct and requirement analysis. In: Jirotka M, Goguen J (eds.). Requirement Engineering: Social and Technical Issues. London, England: Academic Press, 1994: 259-88.
- 8.Brun-Cottan F, Wall P. Using video to re-present the user. Communications of the ACM. 1995;38: 61-71. [Google Scholar]
- 9.Kyng M. Creating contexts for design. In: Carroll JM (ed.). Scenario-Based Design: Envisioning Work and Technology in Systems Development. New York: John Wiley & Sons, 1995: 85-107.
- 10.Rifkin S. Lessons from community participation in health care. Health Policy and Planning. 1986;1: 240-9. [Google Scholar]
- 11.Anderson WL, Crocca WT. Experiences in reflective engineering practice: co-development of product prototypes. In: Muller MJ, Kuhn S, Meskill JA (eds.). Proceedings of Participatory Design Conference. Palo Alto, CA: CPSR, 1992.
- 12.Greenbaum J. A design of one's own: towards participatory design in the United States. In: Schuler D, Namioka A (eds.). Participatory Design: Principles and Practices. Hillsdale, NJ: Lawrence Erlbaum, 1993: 27-37.
- 13.Bucciarelli LL. An ethnographic perspective on engineering design. Design Studies. 1988;9: 159-68. [Google Scholar]
- 14.Lawson B. How designers think: the design process demystified. Oxford, England: Butterworth Architecture, 1990.
- 15.Denzin N, Lincoln Y. Entering the field of qualitative research. In: Denzin N, Lincoln Y (eds.). Handbook of Qualitative Research. Thousand Oaks, CA: Sage Publications, 1994: 1-17.
- 16.Timpka T, Marmolin H. Beyond computer-based clinical reminders: improvement of the total service quality by small-group based organizational learning in primary care. In: Greenes RA, Peterson HE, Protti DJ (eds.). Proceedings of Eight World Congress on Medical Informatics. Amsterdam, The Netherlands: Elsevier-North Holland, 1995. [PubMed]
- 17.Sjöberg C, Timpka T, Nyce J, Peolsson M, af Klercker T. From clinical literature to medical hypermedia: procedures and experiences. In: Lun KC, Degoulet P, Piemme TE, Rienhoff O (eds.). Proc Medinfo 92. Amsterdam, The Netherlands: Elsevier-North Holland, 1992.
- 18.Timpka T, Sjöberg C, Svensson B. The pragmatics of clinical hypermedia: experiences from five years of participatory design in the MEDEA project. Comput Methods Programs Biomed. 1995;46: 175-86. [DOI] [PubMed] [Google Scholar]
- 19.Timpka T, Nyce JM, Sjöberg C, Johansson M. Action design: from modeling to support of the software process. In: Blum B (ed.). Proceedings of the 5th International Conference on Software Engineering and Knowledge Engineering. San Francisco, CA: IEEE Computer Society Press, 1993.
- 20.Gustavsen B. Workplace reform and democratic dialogue. Economic and Industrial Democracy. 1985;6: 461-79. [Google Scholar]
- 21.Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park, CA: Sage Publications, 1990.
- 22.Wertsch JV. Voices of the Mind. Cambridge, MA: Harvard University Press, 1991.
- 23.Engeström R. Voices as Communicative Action. Mind, Culture and Activity. 1995;2: 192-215. [Google Scholar]
- 24.Sjöberg C. Voices in Design: Argumentation in Participatory Development. Licentiate Thesis (Thesis no. 436), Linköping Studies in Science and Technology, Department of Computer and Information Science, Linköping University, Linköping, Sweden, 1994.
- 25.Curtis B, Krasner H, Iscoe N. A field study of the software design process for large systems. Communications of the ACM. 1988;31: 1268-85. [Google Scholar]
- 26.Engeström Y. Mundane tool or object of affection: the rise and fall of the postal buddy. In: Nardi BA (ed.). Context and Consciousness: Activity Theory and Human-Computer Interaction. Cambridge, MA: MIT Press, 1995.
- 27.Korpela M. Nigerian Practice in Computer Systems Development: A Multidisciplinary Theoretical Framework, Applied to Health Informatics. Dissertation. Faculty of Information Technology, Department of Computer Science, Helsinki University of Technology, 1994.
- 28.Weiner JA. A comparison of primary care in the USA, Denmark, Finland and Sweden: lessons for Scandinavia? Scand J Prim Health Care. 1988;6: 13-27. [DOI] [PubMed] [Google Scholar]
- 29.Mumford E. The participation of users in systems design: an account of the origin, evolution and use of the ETHICS method. In: Schuler, Namioka A (eds.). Participatory Design: Principles and Practices. Hillsdale, NJ: Lawrence Erlbaum, 1993; 257-70.
- 30.Bödker S, Grönbaek K, Kyng M. Cooperative design: techniques and experiences from the Scandinavian scene. In: Schuler D, Namioka A (eds.). Participatory Design: Principles and Practices. Hillsdale, NJ: Lawrence Erlbaum, 1993: 157-75.
- 31.Thoresen K. Principles in practice: two cases of situated participatory design. In: Schuler D, Namioka A (eds.). Participatory Design: Principles and Practices. Hillsdale, NJ: Lawrence Erlbaum, 1993: 271-87.
- 32.Keen J, Packwood T. Case study evaluation. In: Mays N, Pope C (eds.). Qualitative research in health care. London, England: BMJ Publishing Group, 1996: 59-67.
- 33.Lundsgaarde HP, Fisher PJ, Steele DJ. Human problems in computerized medicine. University of Kansas Publications of Anthropology, no. 13. Lawrence, Kansas: University of Kansas, 1981.
- 34.Nyce JM, Timpka T. Work, knowledge and argument in specialist consultations: incorporating tacit knowledge into systems design and development. Med Biol Eng Comput. 1993;31: HTA16-9. [DOI] [PubMed] [Google Scholar]
- 35.Forsythe DE. New bottles, old wine: hidden cultural assumptions in a computerized explanation system for migraine sufferers. Med Anthropol Q. 1996;10. in press. [DOI] [PubMed]
- 36.Rittel H. Second-generation design methods. In: Cross N (ed.). Developments in Design Methodology. Chichester, England: John Wiley & Sons, 1984.
- 37.Arnstein SR. A ladder of citizen participation. J Am Inst Planners. 1969;35: 216-22. [Google Scholar]
- 38.Emery M. Towards a heuristic theory of diffusion. Human Relations. 1986;39: 411-32. [Google Scholar]