Abstract
Surgical treatment of femoroacetabular impingement (FAI) focuses on improving the clearance for hip motion and alleviation of femoral abutment against the acetabular rim. Cam type of impingement is managed by performing an osteochondroplasty to remove the excess impinging bone from the head neck junction, thus improving the head neck offset. This procedure can be done by safe surgical dislocation, arthroscopy assisted mini-open method or all arthroscopy technique. Whatever be the approach, adequate excision of the Cam deformity is necessary to avoid suboptimal results. Under-excision leads to persistent symptoms and progression of disease, while over-excision can lead to weak bone vulnerable to fracture or disturb the labral seal. Various techniques utilized for intra-operative evaluation of amount of excision required described in literature are fluoroscopy, spherometer gauges, intra-operative Computed Tomography (CT) scan, navigation etc. Rapid prototyping, also called as three dimensional (3D) printing, is a technology to create dimensionally accurate model from a computer-assisted design. Accurate physical models can be designed from the medical imaging data like CT scans and 3D printed to aid in various medical applications. Its application in orthopaedic field is on a rise, recently. However, there is no report on utilization of this technique in surgeries for FAI. We have reported a case of Cam type FAI in an eighteen year old boy, which we treated surgically by performing osteochondroplasty using safe surgical dislocation. We did CT based virtual surgical planning to design femoral head and neck jigs, which were 3D printed and used intra-operatively to guide for adequate and optimum excision of bone at head neck junction. We found these customized jigs accurate and useful for the surgery. However, a comparison study with various other techniques is warranted for a detailed research on its usefulness and challenges. The main purpose of this article is to elaborate on the technical steps for designing of jigs for 3D printing to guide in osteochondroplasty surgery for FAI.
Keywords: Femoroacetabular impingement, 3D printed jigs, Virtual planning, Osteochondroplasty, Surgical dislocation
1. Introduction
Femoroacetabular impingement is considered as a common cause of hip pain and secondary arthritis in young adults.1 It is characterized by an abnormal patho-anatomy of the hip leading to abutment of the anterolateral head neck junction of femur against the anterolateral rim of acetabulum during the end range of motion.2 This repeated pathologic contact eventually leads to the development of symptomatic FAI, a precursor to osteoarthritis.2 The two distinct forms described in literature are cam and pincer types. Surgical correction of patho-anatomy can halt the progression of the disease. Osteochondroplasty with open or arthroscopic approach is the mainstay surgery for cam type impingement. The goal of such surgeries is improving the clearance for hip motion and alleviation of femoral abutment against the acetabular rim by removing the aspherical portion of femoral head. Various techniques described in literature to assess the adequacy of osteochondroplasy are fluoroscopy, spherical gauges, computer-assisted surgery, intra-operative CT scan etc. Our report is the first ever description of cam type impingement surgically treated by using customized 3D printed jigs designed from CT scan through virtual planning.
2. Case report
An eighteen year old boy presented with complaints of limp, pain and restricted movements of left hip, which gradually progressed over two years. He was unable to squat and do crossed leg sitting. He had a thirty degree of abduction deformity of left hip with restricted further abduction as well as internal rotation. There was an apparent lengthening of 3 cm on left side; however, true lengths of both lower limbs were equal.
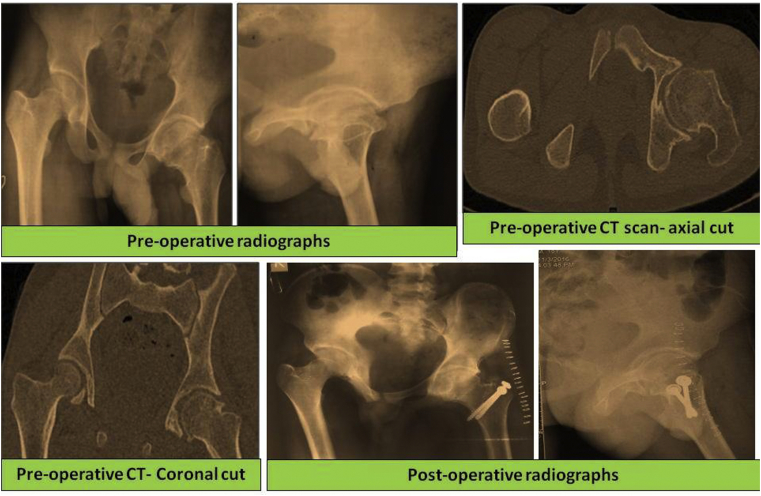
Plain radiograph of pelvis with bilateral hip and CT scan with 1 mm sections were obtained [Fig. 1]. The imaging suggested Cam type of deformity on left side. We performed a virtual planning based on CT scan to design jigs for guiding in osteochondroplasty to decide on optimum excision.
Fig. 1.
Pre-operative plain radiographs, pre-operative CT sections and post-operative radiographs.
Steps of the virtual planning and designing of the jigs are mentioned below.
-
1)
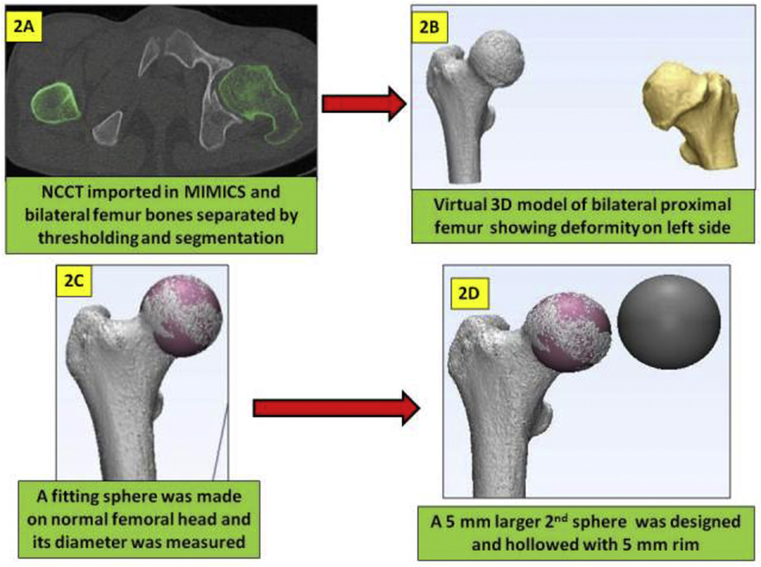
CT scan was imported in Mimics Version 17.0 (Materialise NV, Belgium) software and thresholding was done to separate bone from soft tissue based on density. Segmentation and region growing steps were carried out to develop virtual 3D models of bilateral proximal femur bones [Fig. 2A and B]. The virtual proximal femoral 3D models were then transferred to 3-matic software (Version 9.0) as Stereolithography (STL) files. The models were then assessed. A sphere was designed on the right side (normal) femoral head matching its dimensions, hence called as fitting sphere [Fig. 2C]. The steps included marking of the femoral head surface using “brush mark” command and then selecting “fit sphere” method while designing the sphere based on the marked area. The diameter of the fitting sphere was measured and another sphere of 5 mm larger diameter was designed [Fig. 2D].
-
2)
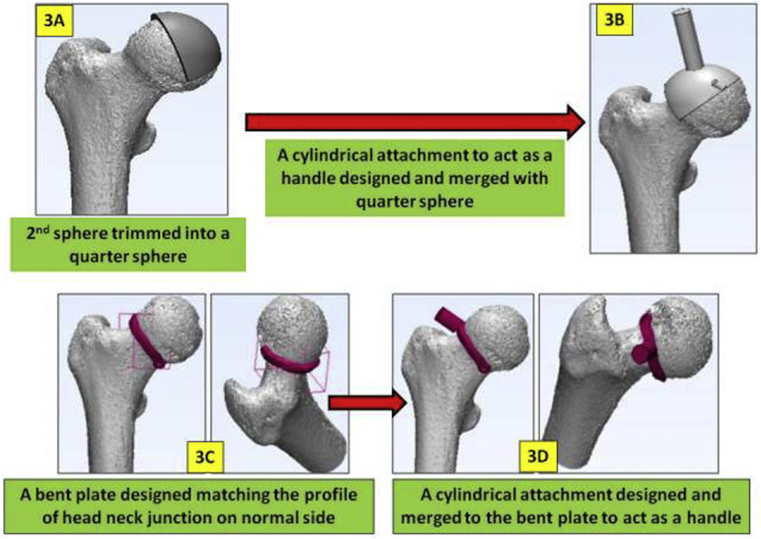
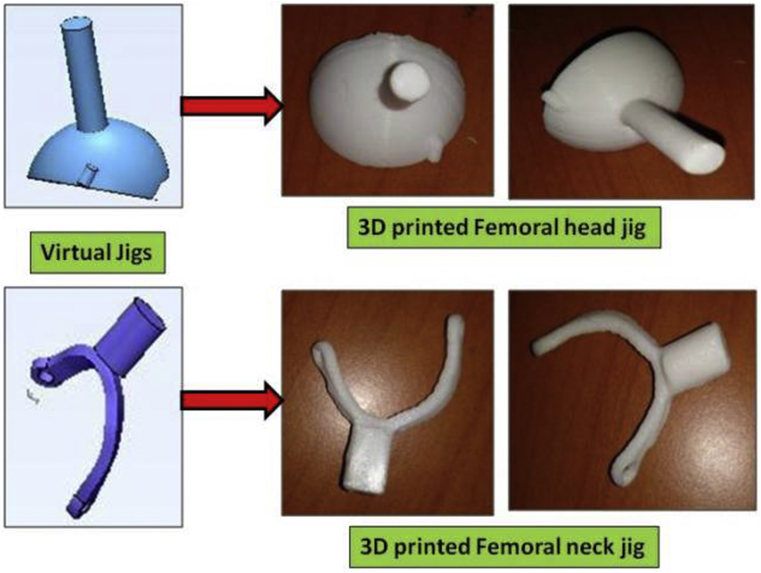
The second sphere was further hollowed using “hollow” command with 5 mm rim thickness. The hollowed sphere was then trimmed into a quarter of the sphere [Fig. 3A]. Further, a cylindrical attachment of 8 mm diameter and 3 cm length was designed and merged with this trimmed quarter-sphere to act as a handle for holding during surgery. Another small cylindrical peg was designed and merged on anterior aspect of the jig for easy intra-operative identification of anterior and posterior side [Fig. 3B]. We named this jig as femoral head jig.
-
3)
A bent plate (6 mm width and 3 mm thickness) matching the contour of neck at head neck junction on right side was designed [Fig. 3C]. A cylindrical attachment (8 mm diameter and 1.5 cm length) was designed and merged to this bent plate to act as a handle of this femoral neck jig [Fig. 3D].
-
4)
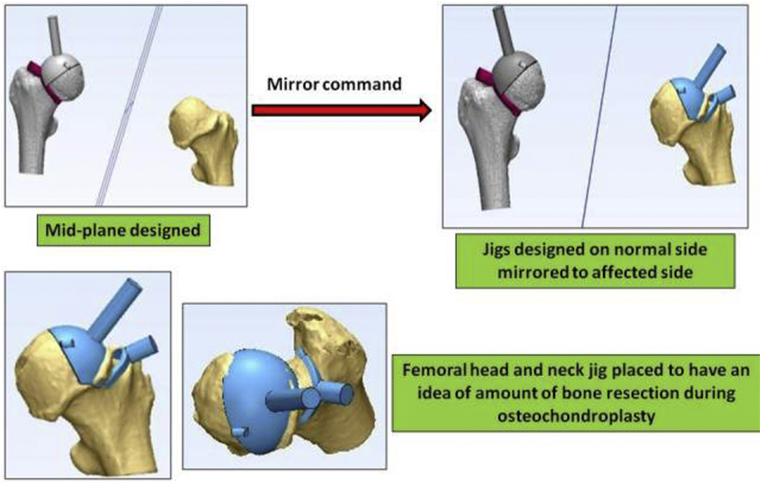
The femoral head and neck jigs designed on the contra-lateral normal femur were then mirrored to left side using mid-plane as reference [Fig. 4]. The jigs were exported as STL files and converted into 3D printable G code in Slic3r software.
-
5)
The jigs were printed in a 3D printer at 30% density using polylactic acid material and autoclaved before use in surgery [Fig. 5]. The total cost of 3D printed jigs was around 500 Indian Rupees (INR).
Fig. 2.
2A and 2B: Designing of virtual 3D model of bilateral proximal femur bones from CT scan in Mimics software. 2C and 2D: Designing of fitting sphere and 5 mm larger sphere on normal side.
Fig. 3.
Designing of femoral head jig (3A and 3B) and neck jig (3C and 3D) on normal side.
Fig. 4.
Mirroring of Femoral head and neck jig based on normal side to affected side.
Fig. 5.
3D printed jigs.
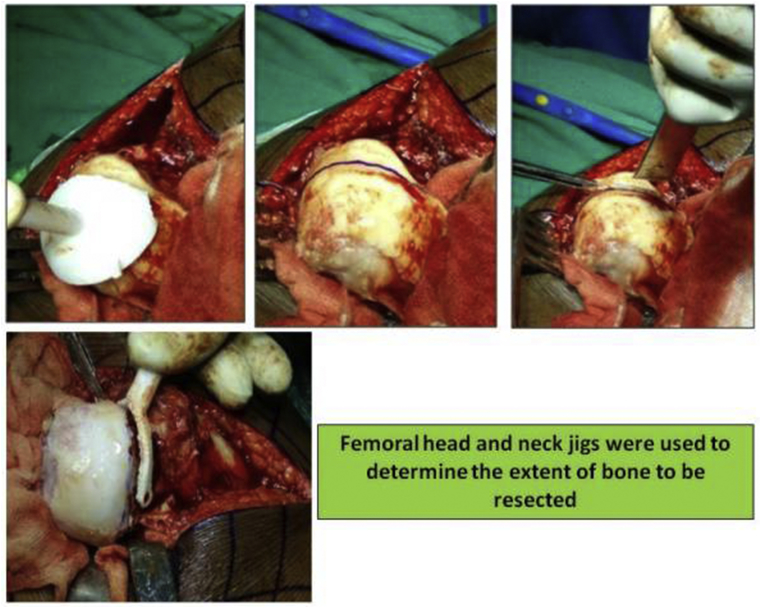
Informed consent for surgery was obtained from patient and his parents. Open osteochondroplasty was performed in lateral position using Ganz's trochanteric flip approach with Z shaped anterior capsulotomy for safe surgical dislocation as described in literature. The femoral head was dislocated anteriorly. The femoral head cartilage was continuously irrigated with ringer lactate solution. The head and neck jigs helped us to guide the extent of resection at head-neck junction to obtain a spherical contour and appropriate head neck offset [Fig. 6]. Trochanteric flip osteotomy was fixed with two cancellous screws. Patient was kept on well leg traction for 3 weeks. Skate board exercises were initiated for range of motion. Patient was pain free with a fair range of motion on his last follow up one year after the surgery.
Fig. 6.
Intra-operative pictures showing the use of jigs for guiding in extent of excision.
3. Discussion
FAI is a distinct pathologic entity that results from an abnormal morphologic relationship between the proximal femur and the acetabulum. Two distinct types of FAI have been identified- Cam and Pincer type.3 Cam impingement results from an abnormal bump in antero-superior portion of femoral head neck junction which leads to jamming of the non-spherical head into the concavity of the acetabulum. The pincer type is characterized by the linear impact of the acetabular rim against the head–neck junction in a local (acetabular retroversion) or global (coxa profunda or protrusio) over-coverage of the acetabulum. Various surgical techniques have been described for pre-arthritic and early arthritic impingement disease to halt progression, relieve pain and improve function. These techniques include surgical dislocation of the hip, periacetabular osteotomy, combined hip arthroscopy with a limited open exposure and all arthroscopic techniques.4 Complex bony abnormalities including extra-articular impingement, major deformities, and global pincer FAI seem to be more precisely treated by open techniques. Severe acetabular retroversion with intact cartilage might require an acetabular reorientation. Minor structural deformities become a domain of osteochondroplasty with all arthroscopic or arthroscopically assisted mini open techniques. Mini open techniques without visualizing the cartilaginous surfaces are surely limited as the surgeon can obtain no information about the cartilage conditions.
Assessing the adequacy of bone resection when correcting cam-type femoroacetabular impingement can be difficult when the surgeon is inexperienced or when less-invasive arthroscopic surgical techniques are used.5 Under-resection of the bone bump results in compromised outcome with persistent impingement and pain.5 Over-resection can lead to weakening of the bone, increased probability of fracture and loss of the labral seal.5 Arthroscopic techniques pose more difficulty in estimating the size of lesion for accurate resection. Various methods have been used for better assessment of extent of resection during surgery. Fluoroscopic control may be used in order to assess the femoral osteochondroplasty. As proposed by some authors, spherometer gauges can be also be used.6 Mofidi et al. have described use of intra-operative CT scan to assist in arthroscopic osteochondroplasty for Cam impingement.7 Anxiety about under- or over-resection of cam impingement during osteoplasty has been significant enough to result in the use of computer navigation in performing osteoplasty, but with limited success.8 Almoussa et al. performed computer assisted navigation for osteochondroplasty in their study for Cam type deformity on saw bones and reported it to be accurate and particularly more useful in inexperienced hands for adequate resection of cam deformity.5 Nawabi et al. have discussed the computer assisted surgeries in arthroscopic osteochondroplasty for hip impingement and concluded that navigation and robotic-assisted surgery can preoperatively plan and execute osseous resection with greater accuracy compared to freehand techniques, although the clinical success and cost-effectiveness has yet to be demonstrated.9
Rapid prototyping, also known as 3D Printing is defined as Additive Manufacturing technology used to accurately construct a 3D model from a computer aided design. Dimensionally accurate physical models of human anatomy can be made from medical image data using 3D printers. Virtual surgical planning is utilization of medical image data to accurately plan surgery in computer environment. It involves formation of Virtual 3-D models from CT scan to yield patient specific information and design customized instrumentation or prosthesis using various functions of virtual planning software. Use 3D printing and virtual planning in various orthopaedic ailments has increased recently. However, 3D printed jigs designed by virtual planning based on CT scan have never been reported for FAI surgery till date.
In our patient with Cam type impingement, we used a femoral head jig and a femoral neck jig to aid in deciding the required about of resection during open osteochondroplasty. The jigs were patient specific as these were virtually designed on normal side of patient's own proximal femoral 3D virtual model. The jigs definitely helped us intra-operatively and we could be sure that we had resected a correct amount of bone during the procedure. We believe that such customized jigs can also be helpful to young surgeons with lesser experience in doing an optimum osteochondroplasty.
The cost of such 3D printed jigs may vary in individual cases from INR 300 to 600. Also, it may require around 1 hour in designing and further 1 hour in 3D printing of the jigs. We believe the above mentioned factors like additional cost and time can be ignored as these are not too much.
Hence, we conclude that 3D printing is an accurate aid for use in surgeries like this and provides customized solutions to improve the surgical outcomes. However, a comparison study between the custom made jigs and other methods is warranted to have concrete evidence on the usefulness of this technique.
Conflicts of interest
The authors declare that there is no conflict of interest.
Informed consent for surgery and submission of data for publication was taken from the patient and his parents.
Funding
There is no funding source.
Contributor Information
Tarun Verma, Email: tarunamiabledpv@gmail.com.
Abhishek Mishra, Email: mishra.abhishek85@gmail.com.
Gaurang Agarwal, Email: gaurang140389@gmail.com.
Lalit Maini, Email: lalit_maini@rediffmail.com.
References
- 1.Clohisy J.C., Knaus E.R., Hunt D.M., Lesher J.M., Harris-Hayes M., Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467:638–644. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ganz R., Leunig M., Leunig-Ganz K., Harris W.H. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ganz R., Parvizi J., Beck M., Leunig M., Notzli H., Siebenrock K.A. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 4.Clohisy J.C., St John L.C., Schutz A.L. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res. 2010;468(2):555–564. doi: 10.1007/s11999-009-1138-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Almoussa S., Barton C., Speirs A.D., Gofton W., Beaule P.E. Computer-assisted correction of cam-type femoracetabular impingement. A sawbones study. J Bone Jt Surg Am. 2011;93(Suppl 2):70–75. doi: 10.2106/JBJS.J.01706. [DOI] [PubMed] [Google Scholar]
- 6.Laude F., Sariali E., Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009;467(3):747–752. doi: 10.1007/s11999-008-0656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mofidi A., Shields J.S., Tan J.S., Poehling G.G., Stubbs A.J. Use of intraoperative computed tomography scanning in determining the magnitude of arthroscopic osteochondroplasty. Arthroscopy. 2011;27:1005–1013. doi: 10.1016/j.arthro.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Brunner A., Horisberger M., Herzog R.F. Evaluation of a computed tomography-based navigation system prototype for hip arthroscopy in the treatment of femoroacetabular cam impingement. Arthroscopy. 2009;25:382–391. doi: 10.1016/j.arthro.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Nawabi D.H., Nam D., Park C., Ranawat A.S. Hip arthroscopy: the use of computer assistance. HSS J. 2013;9(1):70–78. doi: 10.1007/s11420-012-9313-9. [DOI] [PMC free article] [PubMed] [Google Scholar]