Abstract
While behavioral interventions can improve blood pressure (BP) in individuals with hypertension, getting such services to people who could benefit remains difficult. Workplace programs have potential as dissemination vehicles. The objective is to evaluate the effectiveness of a standardized stress management program delivered in groups at the workplace for reducing BP compared with enhanced usual care. This randomized controlled trial studied 92 urban medical center employees with hypertension randomized into two groups. The intervention was a 10-week group workshop on cognitive-behavioral coping skills. Enhanced usual care included self-help materials for BP reduction and physician referral. Intervention group participants’ systolic BP (SBP) decreased 7.5 mm Hg over controls between baseline and follow-up, from 149.1 (95% CI: 146.0–152.1) to 140.0 (95% CI: 134.7–145.2), p < .001. The differential change between intervention and enhanced usual care groups (Group × Time interaction) was 7.5 mm Hg (t = −2.05; p = .04). Diastolic BP reductions were not significantly different. Scores on measures of emotional exhaustion and depressive rumination showed significant improvements and correlated with reductions in SBP. There was no significant change in the usual care group. A standardized worksite group intervention produced clinically meaningful reductions in SBP in participants with hypertension.
Keywords: Hypertension, Stress, Psychosocial intervention, Workplace intervention, Clinical trials
Employees with high blood pressure who participated in a weekly stress and anger management group in the workplace reduced their systolic blood pressure more than employees who did not participate.
Implications
Practice: A standardized 10-session stress and anger management program delivered in groups in the workplace proved to be a practical and successful approach to reducing SBP in hypertensive employees.
Research: The possibility of decreases in BP being mediated by changes in emotional exhaustion or depressive rumination should be explored in future research and can be effective in reducing BP in hypertensive employees.
Policy: The workplace may be an excellent venue for dissemination of group psychosocial interventions to address chronic conditions or health behaviors, given the high rate of retention of participants in completing the intervention.
INTRODUCTION
Hypertension affects approximately one third of adults in the USA [1] and is one of the most important modifiable cardiovascular risk factors [2]. Large epidemiologic studies have shown that psychosocial risk factors including hostility [3, 4], chronic psychosocial stress [5], nonadaptive coping [6], depression [7, 8], work stress [9, 10], and low socioeconomic status [11, 12] contribute to the development of hypertension, so it seemed logical that interventions targeting these psychosocial risk factors could help improve blood pressure (BP) control [13, 14]. The potential usefulness of such approaches is heightened by patient preferences for alternatives to pharmacotherapy [15]. A number of previous intervention studies have focused on modifying stress [16–20], hostility [21], and other psychosocial risk factors [22] and have found beneficial effects on BP (or the ability to reduce antihypertension medications [23]) compared with control conditions. Recent reviews [14, 24] suggest psychosocial interventions using multiple components of stress or anger management (cognitive-behavioral approaches often combined with meditative or other relaxation techniques) [21–23] are more effective in reducing BP than single-modality interventions.
The dissemination of behavioral and psychosocial interventions focused on stress reduction and health presents a difficult challenge. Most interventions for hypertension noted above have been developed and delivered in clinical settings. However, medical practices are often overburdened, often lack the resources to deliver psychosocial interventions, and can be a difficult setting for patients to attend regular sessions [25, 26]. Worksite health promotion programs offer easy access for employees during work hours. The Federal Government has emphasized the importance of worksite wellness programs and provided incentives in the Affordable Care Act [27, 28], making it likely that employers will be increasingly committed to health promotion and the improved management of chronic conditions in their workforces.
Workplace interventions for BP and other cardiovascular risk factors have primarily targeted physical activity, diet, and weight loss [29]. Some have included small stress management components [30], but few have focused on BP with stress management. Some recent workplace programs have taken a “mind–body health” approach to stress reduction, focusing on yoga or mindfulness-based techniques [31, 32], or biofeedback [33], with modest BP changes in nonhypertensive participants. Only one study [34] to our knowledge has targeted hypertensives based on workplace screenings, and the stress management intervention was effective in reducing systolic BP (SBP).
The purpose of the present randomized controlled trial was to test the effects of a well-described, standardized, multicomponent cognitive-behavioral intervention for stress and anger management (Williams LifeSkills Workshop, Williams LifeSkills, Inc., Durham, NC), delivered in groups in a multiethnic, urban workplace, on BP in employees with hypertension. This intervention has previously been shown to reduce emotional distress, anger, depression, social isolation, and perceived stress, as well as BP and heart rate both at rest and during acute stress in healthy populations [35–38],in CHD patients [39] and in groups with known stressors [40, 41]. The workplace is a particularly useful intervention site because hypertension is common in working-age adults; there is little stigma attached to either hypertension or workplace interventions, and therefore, treatment tends to be acceptable to participants [34, 42].
METHODS
Study population
Participants were employees (aged 18–70 years) of a large urban medical center who were identified through workplace BP screenings. Staff were placed at tables in high-traffic areas and offered employees a $5 public transit card as an incentive for BP screening. Employees whose screening BP (average of three measurements) was ≥140 mm Hg SBP or 90 mm Hg diastolic BP (DBP) and whose average readings did not exceed 180/110 mm Hg at both this screening and the subsequent baseline evaluation were eligible and invited to participate in the RCT. The exclusion criteria were pregnancy and end-stage renal disease. The study was approved by the Institutional Review Board at Columbia (University Medical Center); all participants gave informed consent. Data collection began in 2003, and the trial is registered at clinicaltrials.gov (Identifier NCT01262066).
Investigator involvement
Although this project was funded with a Small Business Innovation Research (SBIR) grant from the National Institutes of Health (NIH) through Williams LifeSkills, Inc, Durham, NC and the founders (R.B.W. and V.P.W.) share authorship on this paper, the founders’ involvement in the study was restricted to ensuring treatment fidelity through the training and initial supervision of the clinician (L.P.C.) who subsequently trained and supervised the clinicians who delivered the intervention. Otherwise, the design and conduct of this study, the data collection, analysis, and interpretation of results occurred completely independent of the developers of the intervention. They were involved in the editing of the manuscript.
Procedures
At the first baseline visit, participants gave informed consent, had a second set of three BP measurements taken, and completed questionnaires to assess stress, depression, and other psychosocial conditions. They also completed a structured interview either during the baseline visit or at a separate visit within 2 weeks. Those with average BP measurements that were in the hypertensive range at the baseline visit and did not exceed 180/110 mm Hg were invited to participate in the trial. Those who agreed to participate were randomly assigned to one of two groups: intervention (LifeSkills workshop) or minimally enhanced usual care. Randomization was done by calling an off-site person holding the randomization envelopes, using random-sized randomization blocks provided by the study statistician (J.E.S.), in accordance with CONSORT (Consolidated Standards of Reporting Trials) guidelines [43]. To ensure that any observed treatment benefits were not occurring only in patients with high hostility levels, the randomization was stratified for baseline hostility (two categories based on Barefoot’s [44] criterion of a score ≥13 on the Cook-Medley Hostility Scale [45]). Treatment groups included a mixture of high and nonhigh hostile participants. Follow-up assessments were identical to baseline assessments and occurred approximately 60 days after the end of the intervention. Participants were paid $125 for completing the trial.
BP measurement
At screening, baseline, and follow-up 2 months following the last group session, three BP readings were taken at 1-min intervals using an automated device (BP-TRU BPM-100; VSM MedTech Ltd., Vancouver, BC, Canada). This BP-TRU device is a highly accurate and objective measure of BP considered the “gold standard” [46, 47] for office BP measurement regarding reliability and consistency with ambulatory measurement. BP readings were done in accordance with American Heart Association [48] and JNC 7 [49] guidelines for office BP measurement. That is, persons are seated quietly for at least 5 min in a chair with feet on the floor and arm supported at heart level; caffeine, exercise, eating, and smoking have been avoided for at least 30 min prior to measurement. These measurement sessions generally took place during midday breaks or immediate after-work hours.
Demographic measures and medications
Self-report measures were completed at baseline and at follow-up. Table 1 shows the demographic characteristics of the sample by randomization group. Participants listed all current medications for hypertension and any other conditions. A hypertension specialist (T.G.P.) compared hypertension medications at baseline and follow-up and evaluated changes as to whether medication had been increased, decreased, or not changed.
Table 1.
Baseline characteristics of all participants who were randomizeda
| Variable | All (N = 92) | Control group (n = 46) | Intervention group (n = 46) | p |
|---|---|---|---|---|
| Age, yearsb | 48.5 (8.7) | 48.7 (9.0) | 48.4 (8.4) | .89 |
| Height, inb | 64.9 (3.4) | 65.5 (3.4) | 64.2 (3.2) | .08 |
| Weight, lbb | 188.6 (43.6) | 187.7 (49.1) | 189.5 (37.4) | .85 |
| BMIb | 31.3 (6.4) | 30.6 (6.8) | 32.1 (6.0) | .26 |
| Systolic blood pressure, mm Hgb | 148.0 (10.4) | 147.0 (10.2) | 149.1 (10.6) | .35 |
| Diastolic blood pressure, mm Hgb | 90.8 (7.7) | 90.3 (8.7) | 91.3 (6.5) | .54 |
| Hypertension type | ||||
| Controlled on medication | 2 (2) | 0 (0) | 2 (4) | .20 |
| Stage 1 | 66 (72) | 36 (78) | 30 (65) | |
| Stage 2 | 24 (26) | 10 (22) | 14 (30) | |
| Female | 71 (77) | 33 (72) | 38 (83) | .21 |
| Male | 21 (23) | 13 (28) | 8 (17) | |
| Hypertension medication use at baseline | ||||
| No | 34 (38) | 15 (33) | 19 (43) | .30 |
| Yes | 56 (62) | 31 (67) | 25 (57) | |
| Race | ||||
| White (non-Hispanic) | 14 (15) | 6 (13) | 8 (17) | .83 |
| White (Hispanic) | 14 (15) | 6 (13) | 8 (17) | |
| Black (non-Hispanic) | 42 (46) | 20 (43) | 22 (48) | |
| Black (Hispanic) | 8 (9) | 5 (11) | 3 (7) | |
| Asian/Indian | 4 (4) | 2 (4) | 2 (4) | |
| Asian/Pacific Islander | 4 (4) | 3 (7) | 1 (2) | |
| Other | 6 (7) | 4 (9) | 2 (4) | |
| Ethnicity | ||||
| Latino | 26 (28) | 14 (30) | 12 (26) | .64 |
| Non-Latino | 66 (72) | 32 (70) | 34 (74) | |
| Marital status | ||||
| Never married | 20 (22) | 9 (20) | 11 (24) | .80 |
| Currently married | 41 (46) | 22 (49) | 19 (42) | |
| Separated, divorced, or widowed | 29 (32) | 14 (31) | 15 (33) | |
| Education | ||||
| Some college or less | 46 (51) | 22 (49) | 24 (52) | .75 |
| College graduate or graduate school | 45 (49) | 23 (51) | 22 (48) | |
| Income | ||||
| ≤$50,000 | 48 (56) | 23 (54) | 25 (58) | .66 |
| >$50,000 | 38 (44) | 20 (47) | 18 (42) | |
| Cook-Medley Hostility Scale26 | ||||
| Below 13 | 50 (54) | 25 (54) | 25 (54) | 1.00 |
| At or above 13 | 42 (46) | 21 (46) | 21 (46) | |
BMI indicates body mass index, calculated as weight in kilograms divided by height in meters squared.
aData are presented as number (%) unless indicated otherwise.
bData are presented as mean (SD).
Psychosocial measures
Psychosocial instruments included measures of distress used previously in studies of the LifeSkills Intervention, including the 27-item Barefoot version of the Cook-Medley Hostility Scale [44, 45], formatted as true–false responses, Centers for Epidemiological Studies–Depression Scale (CES-D) [50], a 20-item measure of self-rated depressive symptoms, and the 10-item Perceived Stress Scale [51]. As this was a workplace study, we also included the Maslach Burnout Scale [52], a 22-item measure made up of three internally consistent domains: emotional exhaustion, depersonalization (or cynicism), and personal accomplishment (or professional efficacy; Maslach and Leiter, 2016) [53]. The measure has good reliability but is sensitive to changes in circumstance. Work strain was measured by the Karasek Job Content Questionnaire, assessing with 42 items the amount of perceived job strain (defined as low job control vs. high job demand) [54]. Assertiveness, related to issues targeted in the intervention, was measured by the Personal Assertion Analysis (PAA) [55], a 50-item questionnaire for adults that provides scores for assertive, passive, and aggressive interpersonal behavior. Social support was measured by the Interpersonal Support Evaluation List (ISEL) [56]. A final exploratory measure, the Ruminative Response Scale (RRS) [57], was added partway through data collection. The RRS is a 20-item measure widely used in studies of emotional regulation and depression, in which respondents rate items comprising three dimensions of ruminative thinking: depressive rumination, reflection, and brooding. All measures have been subjected to extensive psychometric study and have adequate levels of internal consistency and reliability. Measures were completed on paper and were taken at baseline and 2 months post treatment.
Intervention
Participants assigned to the treatment condition attended 10 weekly 1-hr sessions in groups of 8–10 participants. Group sessions were conducted at midday lunch breaks, during the workday, between 12 noon and 2:00 pm. Sessions followed the Williams LifeSkills Workshop manual and video [32]. The LifeSkills Workshop is a structured cognitive-behavioral group intervention that draws on cognitive-behavioral techniques and stress reduction approaches. It is framed as training to increase a person’s resiliency for coping with stressful situations, rather than as treatment for a mental disorder. The facilitator leads participants through each of several behavioral skills, modeling them as necessary. A video [38] developed as an adjunct to the program was integrated into each session, which standardized the presentation of material. Skills included self-monitoring, such as identification and evaluation of thoughts, feelings, and behaviors in response to stressful situations; problem solving; assertiveness in dealing with anger- and stress-inducing events and/or demands; deflection skills to reduce distress in stressful situations, such as breathing and muscle relaxation, distraction, and increasing distress tolerance; communication skills; and increasing empathy and building positive relationships. The weekly sessions were audio recorded to monitor treatment fidelity and to allow for supervision of the facilitators. The same facilitator worked with the same group of participants throughout the course of the intervention. Facilitators offered individual consultation to participants who missed a session. Three doctoral-level clinical or counseling psychologists were trained according to the guidelines used by Williams LifeSkills, Inc., to serve as group facilitators; they received ongoing supervision from the senior study clinician (L.P.C.) to ensure fidelity to the material.
Participants in the minimally enhanced usual care group received a brochure on BP control developed by the National Heart, Lung, and Blood Institute [58], containing information about hypertension and suggestions for making lifestyle changes to reduce BP. With patients’ permission, their BP readings were sent to their physicians, along with the two-page JNC 7 reference card summarizing guidelines for the management of high BP [59]. There were no group meetings for the usual care condition.
Statistical analyses
An intent-to-treat analysis was performed on all randomized participants. A multilevel, repeated-measures regression analysis was performed to generate full information maximum likelihood estimates of the group-specific average change in SBP and DBP between baseline and the 2-month posttreatment assessments and to estimate and test the differential change between the intervention and usual care groups. Consistent with intent-to-treat principles, all participants who were randomized, including two participants who were subsequently deemed ineligible (described below), were included in the analysis [60, 61], In the multilevel model, treatment group, time (baseline vs. 2-month follow-up), and the interaction of treatment group and time were entered as fixed effects predicting the primary outcomes, SBP, and DBP. Because the randomization was stratified by hostility group, hostility group and the interaction of hostility group and time were included as covariates. In secondary analyses, we repeated the analysis excluding those who did not complete the study and repeated the intent-to-treat analysis controlling for the use of hypertension medications at baseline and changes in medication use.
Psychosocial variables were tested for baseline group differences, and change scores from baseline to 2-month follow-up were tested using t-tests for group differences. Correlational analyses were conducted to explore relationships between change scores for BP and psychosocial variables. Finally, we conducted exploratory analyses to test whether psychosocial variables that changed significantly mediated the differential decline in BP associated with the intervention. Given that the assessments of both the mediators and dependent variables were conducted prior to and following the intervention, we followed the procedures of Bauer et al. [62] for conducting mediation in multilevel models.
RESULTS
Participants
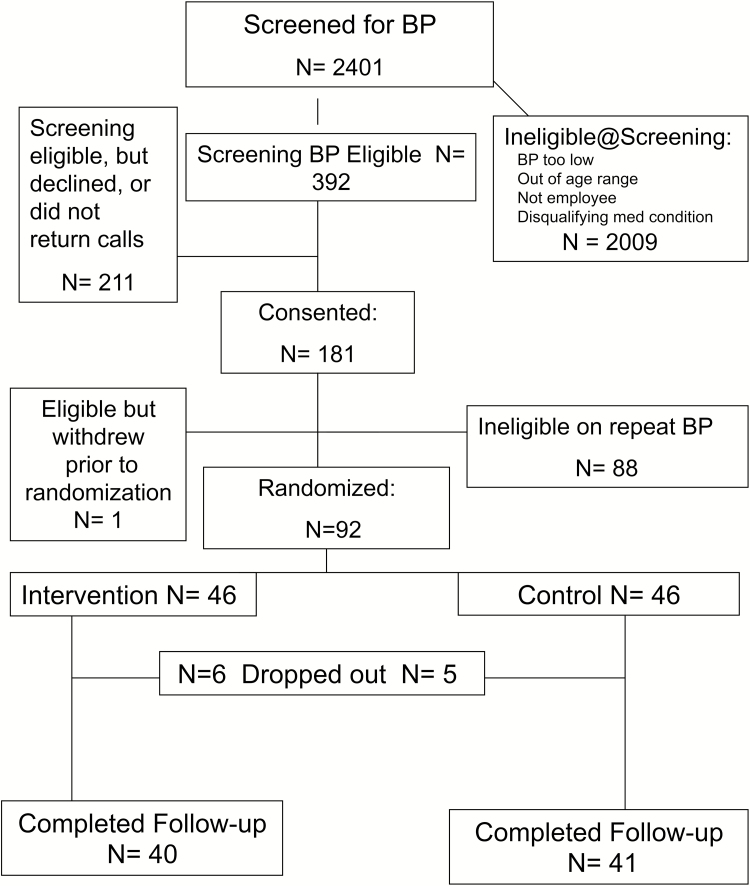
As shown in the CONSORT diagram (Fig. 1), of the 2,401 people seen at the worksite BP screenings, 2,009 (84%) were ineligible or declined to participate in research, while 392 (16%) employees were eligible at screening on the basis of BP measurement (≥140/90 mm Hg and <180/110 mm Hg) and agreed to be contacted for research.
Fig 1.
CONSORT diagram.
Of the 392 eligible employees, 211 declined to participate in this study or could not be contacted after three telephone messages. The remaining 181 employees agreed to participate, but 88 of these individuals were ineligible because the average of their second set of baseline BP readings was below 140/90 mm Hg. One additional person was eligible but declined to participate prior to randomization. Of the 92 who were randomized, 46 were assigned to the intervention group, and 46 were assigned to the usual care control group. Eleven participants dropped out after randomization (six in the intervention group and five in the usual care control group). Two participants, both in the intervention group, were later found to have been ineligible because their average BP measurements were computed in error and were actually below the cutoff.
Baseline demographic and clinical characteristics
No significant differences were observed between the intervention and control groups on demographic and clinical characteristics at baseline (Table 1). Participants were primarily female, were ethnically diverse (approximately 50% self-identified as black and more than one fourth as Latino/a), and had a mean age of approximately 48 years. They tended to be obese, and most met criteria for Stage 1 hypertension, with an average BP of 148/91 mm Hg. Approximately, 62% (56/92) of participants reported taking BP medication at baseline, and 46% (42/92) scored in the high hostility range based on the Barefoot [39] scoring of the Cook-Medley Hostility Scale.
Intervention process data
Randomized participants attended with mean (SD) of 8.1 (1.8) group sessions, with 89.3% attending seven or more sessions.
Intent-to-treat analysis
Blood pressure
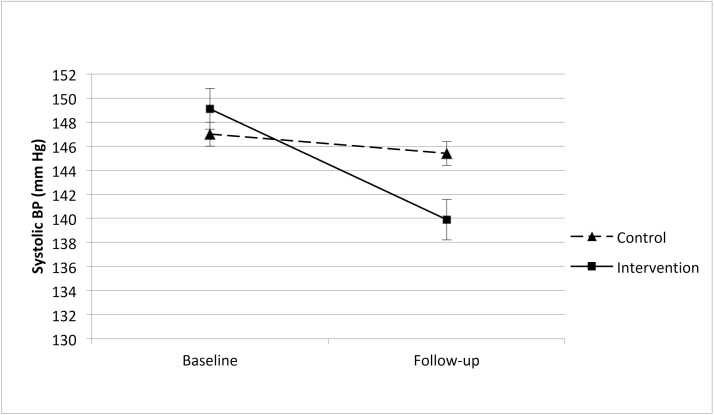
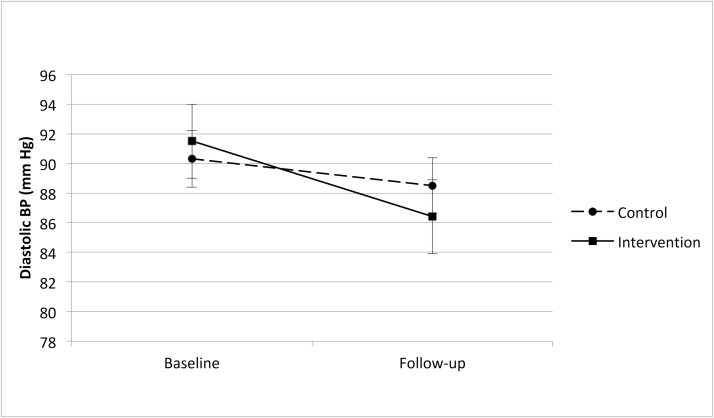
All 92 participants who were randomized were included in the analysis. Table 2 shows the adjusted mean levels of BP by treatment group and assessment, the group differences within assessment, the temporal changes within group, and the overall treatment effect (Group × Time interaction) for SBP and DBP. The intent-to-treat, repeated-measures regression analysis showed a small, nonsignificant 1.7 mm Hg decline in SBP in the control group (t = −0.66, p = .51) and a 9.1 mm Hg decline in the intervention group (t = 3.47, p < .001). At baseline, SBP and DBP were similar between the two groups. The differential change between groups (Group × Time interaction) was 7.5 mm Hg (t = −2.05, p =.04; Table 2). The effect size (Cohen’s d) for this treatment effect was 0.72. Although the pattern of results for DBP (Table 2) was similar to that for SBP—a nonsignificant decline in DBP in the control group and a significant decline of 4.8 mm Hg (t = 3.33, p =.001) in the intervention group—the differential decline (i.e., treatment effect) of 3.1 mm Hg was not statistically significant (t = −1.51, p =.14). These SBP and DBP findings are illustrated in Figs. 2 and 3. In secondary analyses, we repeated the previous analyses after restricting the sample to those who completed the protocol (i.e., those in the control group who completed the follow-up assessment [n = 41] and those in the intervention group who attended at least six sessions and completed the follow-up assessment [n = 39]). The treatment effect for SBP (−7.2 mm Hg; t = 1.96, p = .05) was essentially identical to that from the intent-to-treat analysis. Similarly, the treatment effect for DBP (−3.0 mm Hg; t = 1.45, p = .15) was nearly identical to that from the intent-to-treat analysis. We also repeated the intent-to-treat analysis including use of hypertension medication at baseline and change in medication as covariates, and the results were again unchanged; the treatment effects were −7.2 mm Hg (t = −1.95, p = .05) for SBP and −3.0 mm Hg (t = 1.46, p = .15) for DBP.
Table 2.
Adjusted mean blood pressure by treatment group and perioda
| Response variable | Baseline | Follow-up | Change | p |
|---|---|---|---|---|
| Systolic blood pressure, mm Hg | ||||
| Control group | 147.0 (144.0 to 150.1) | 145.4 (140.4 to 150.4) | −1.7 (−6.6 to 3.4) | .51 |
| Intervention group | 149.1 (146.0 to 152.1) | 140.0 (134.7 to 145.2) | −9.1 (−14.4 to −3.9) | <.001 |
| Difference | 2.0 (−2.3 to 6.4) | −5.4 (−12.6 to 1.8) | −7.5 (−14.7 to −0.2) | .04 |
| p | .35 | .14 | .04 | … |
| Diastolic blood pressure, mm Hg | ||||
| Control group | 90.3 (88.0 to 92.6) | 88.5 (85.3 to 91.7) | −1.8 (−4.6 to 1.0) | .21 |
| Intervention group | 91.3 (89.0 to 93.5) | 86.4 (83.2 to 89.6) | −4.8 (−7.7 to −2.0) | .001 |
| Difference | 1.0 (−2.2 to 4.2) | −2.1 (−6.6 to 2.4) | −3.1 (−7.1 to 1.0) | .14 |
| p | .55 | .36 | .14 | … |
aData are presented as mean (95% confidence interval) unless indicated otherwise. Multilevel repeated-measures analysis, controlling for hostility category (high vs. other), and Hostility × Period interaction (randomization was stratified by hostility). Ellipses indicate not applicable.
Fig 2.
Systolic blood pressure measurement, mm Hg, at Baseline and at 2 month follow-up in control and Intervention groups. Data are presented as mean (vertical bars represent ±1 SE).
Fig 3.
Diastolic blood pressure measurement, mm Hg, at baseline and at 2 month follow-up in control and intervention groups. Data are presented as mean (vertical bars represent ±1 SE).
Psychosocial variables
Baseline psychosocial characteristics did not vary between treatment and control groups (Table 3). Only two psychosocial variables showed significant differences between groups in pre- and postchange: (a) the Emotional Exhaustion Scale of the Maslach Burnout Inventory and (b) the Depressive Rumination Scale of the RSS, with the treatment group self-reporting greater reductions in emotional exhaustion (p = .03) and depressive rumination (p = .02).
Table 3.
Baseline characteristics and change scores of randomized participants on psychosocial variables
| Baseline | Change Scores | p= | |||
|---|---|---|---|---|---|
| Variable | Control (n = 46) | Intervention (n = 46) | Control | Intervention | |
| Cook-Medley hostility | 12.2 (5.6) | 12.8 (5.6) | 0.0 (5.4) | 0.32 (5.3) | ns |
| CES-D | 11.2 (10.2) | 14.5 (8.7) | 1.0 (5.9) | 0.10 (8.9) | ns |
| Maslach Burnout inventory | |||||
| Emotional exhaustion | 23.2 (12.6) | 19.2 (10.8) | 3.12 (9.7) | −2.5 (9.6) | .03 |
| Depersonalization | 4.2 (4.4) | 5.4 (5.2) | −0.06 (4.5) | −0.89 (4.1) | ns |
| Personal accomplishment | 31.5 (11.3) | 32.3 (9.7) | −0.7 (7.6) | 1.9(10.2) | ns |
| John Henryism | 47.8 (5.6) | 48.4 (5.6) | −1.0 (5.4) | 1.3 (6.1) | ns |
| Karasek job questionnaire | |||||
| Skill discretion | 33.6 (4.9) | 33.2 (5.8) | 0.7 (4.6) | 0.16 (4.6) | ns |
| Decision-making authority | 30.7 (6.3) | 29.7 (4.3) | 1.7 (6.1) | −0.27 (5.7) | ns |
| Job demands | 32.9 (6.8) | 31.2 (5.4) | 1.0 (6.5) | −0.70 (6.9) | ns |
| PAA (interpersonal behavior) | |||||
| Passive behavior | 28.3 (5.8) | 27.4 (5.5) | −0.85 (3.6) | −0.32 (5.2) | ns |
| Aggressive | 31.7 (5.8) | 31.4 (5.0) | −0.28 (4.2) | −0.06 (4.3) | ns |
| Assertive | 21.9 (5.8) | 21.2 (4.5) | −0.62 (3.5) | 0.14 (3.7) | ns |
| ISEL (social support) | |||||
| Belonging | 13.7 (2.1) | 13.0 (2.8) | −0.08 (1.9) | 0.09 (2.4) | ns |
| Appraisal | 13.4 (3.1) | 12.9 (3.4) | −0.75 (1.9) | −0.49 (2.5) | ns |
| Tangible | 13.6 (2.9) | 13.0 (2.3) | −0.12 (2.6) | 0.03 (2.5) | ns |
| Ruminative Response Scale | |||||
| Depressive rumination | 17 (5.1) | 19.0 (6.1) | 1.5 (3.1) | −1.3 (2.6) | .02 |
| Reflection | 8.9 (4.1) | 9.9 (3.3) | 1.2 (3.2) | 0.09 (4.5) | ns |
| Brooding | 8.2 (2.1) | 10.2 (3.6) | 0.35 (1.7) | 0.09 (1.9) | ns |
PAA personal assertion analysis.
All continuous variables, mean (SD) is given.
Correlational analyses
Pearson product moment correlations were calculated between change scores in SBP and DBP and change in the two psychosocial measures that showed significant group differences. Reductions in SBP in all participants correlated significantly with reductions in emotional exhaustion (r = .31, p = .02) and the depressive rumination subscale of the RRS (r = .58, p = .001). Decreases in DBP correlated significantly with decreases in depressive rumination (r = .42, p = .03). In the intervention group, the number of group sessions attended did not correlate significantly with changes in either SBP or DBP, though the number of sessions attended did correlate with emotional exhaustion (r = .45, p = .03). Neither hypertension medication use at baseline nor changes over time affected the outcomes.
Mediation analyses
Supplemental, exploratory analyses were conducted to test whether the reduction in emotional exhaustion or depressive rumination mediated the larger decline in BP associated with the intervention. Neither of these two potential mediators explained the differential decline in either SBP or DBP. However, this study may have been underpowered to detect a mediation effect, and thus, the possibility of mediation should be explored in future trials with more participants.
DISCUSSION
A cognitive-behavioral stress and anger management intervention delivered in groups in the workplace for employees with hypertension was effective in reducing SBP compared with minimally enhanced usual care. Effects on DBP were more modest and were nonsignificant in the intent-to-treat analysis. The 9.1 mm Hg reduction in SBP in the intervention group was clinically noteworthy compared with the 1.7 mm Hg reduction in the usual care group. This reduction in SBP compares favorably with the findings of other studies of nonpharmacological approaches to reduce BP, including one that employed stress management in the worksite and found a significant decrease in SBP but not DBP in the intervention group [34, 42].
The intervention had relatively small effects on psychosocial variables compared with previous studies of the LifeSkills Workshop intervention, which had shown substantial reductions in depressive symptoms and hostility [35–41]. However, in this study, participants were selected for high BP, rather than elevated levels of emotional distress that served as entry criteria in some other studies, and the baseline emotional distress levels were relatively low, leaving less room for improvement in these participants.
Improvements in the intervention group for a measure of work-specific distress, the Emotional Exhaustion Scale of the Maslach Burnout Inventory, correlated moderately with reductions in SBP. It may be that an intervention at the worksite is particularly effective at addressing problems that affect workplace stress. For example, a recent study of workers on sick leave for work stress found that employees who underwent a similar stress management program returned to work sooner and with fewer symptoms than wait-list controls [63]. The second measure that changed significantly in the intervention group, despite having been added to the protocol later resulting in less power to detect change, was the Depressive Rumination Scale of the RSS. Rumination seems to sustain the physiological impact of stress or anger-inducing events on BP [64, 65] and has been proposed as a mechanism by which episodic stressors may lead to sustained high BP [65, 66].
The potential clinical significance of the 7.5 mm Hg differential change in SBP between the groups is supported by a recent meta-analysis involving 1 million patients in 61 studies reporting that even a 2 mm Hg reduction in SBP was associated with a 10% lower risk of mortality due to stroke and a 7% lower risk of mortality due to ischemic heart disease or other vascular causes in middle-aged persons [67]. The current findings suggest that the intervention used in this study has the potential to be used on a larger scale to reduce BP in patients with hypertension. It might also prove to be applicable to individuals in high-risk groups, such as employees with high job demands [54], persons of lower socioeconomic status (who have been recently reported to have higher SBP levels [11, 12]), and other populations exposed to chronic stress. The group format could be more cost-efficient than individual interventions. Given that the same LifeSkills program delivered via video with telephone coaching has been found to reduce BP in stressed caregivers, with maintenance of BP reductions over 6 months [40], it is possible that such stress reduction training could be disseminated on a larger scale among hypertensive patients in a wide range of real-world settings using video or online platforms.
Several limitations of this study should be noted. First, research staff were not blinded to participant group assignment. However, we attempted to mitigate the potential influence of this problem by using automated BP measurements, which are blinded to group assignment and less susceptible to bias than manual BP measurements. While our intent was to use a measurement that is standard in clinical care, replication of these findings with ambulatory BP data would strengthen the results. Ambulatory daytime DBP was reduced in healthy normotensive youth who received LifeSkills training in one prior trial [41]. In the absence of an attention-control group, it is not possible to be sure how much of the positive BP change was due to the intervention content itself or the psychologist-led meetings with employees in a group setting. In any case, the intervention as delivered was superior to usual care. A final limitation is that specific cost data were not collected, so cost-effectiveness analyses could not be performed.
Summary
This trial using a standardized stress and anger management intervention led to statistically significant and clinically meaningful reductions in SBP compared with enhanced usual care among employed persons with elevated BP. DBP was not significantly reduced. The magnitude of change in BP between groups is clinically significant and comparable with that shown in other successful studies of nonpharmacologic approaches to hypertension treatment. Although the current trial is relatively small, it featured careful ascertainment of office BP and a standard manualized intervention, which previous stress reduction intervention studies have been criticized for lacking. It also was conducted with an ethnically diverse population. If the present findings are confirmed in future trials with larger samples, it would indicate that this approach to teaching cognitive-behavioral coping skills has the potential to be a useful adjunct to pharmacotherapy with the potential to be delivered on a larger scale in real-world workplace settings for the treatment of hypertension.
Acknowledgments
Funding provided by NIH grant #HL67584 from the National Heart, Lung, and Blood Institute (Principal Investigator : L.P.C.).
Compliance with Ethical Standards
Conflict of Interest: R.B.W. and V.P.W. are founders and major stockholders in Williams LifeSkills, Inc. Their involvement in the project, as noted in the Methods section, was limited to treatment fidelity and initial training and initial supervision in the intervention. They also assisted in the editing of the manuscript. Otherwise, the design and conduct of the study, the data collection and analyses, and interpretation of results occurred independently of the developers of the intervention. The other authors (L.P.C., T.G.P., K.W.D., J.E.S., V.P.W., J.A.S., R.B.W., W.G.) have no conflicts to disclose.
Primary Data: The authors have full control of all primary data, and they agree to allow the journal to review their data if requested. The findings reported here have not been previously published, and the manuscript is not being simultaneously submitted elsewhere. Portions of these data were presented at the Society of Behavioral Medicine Annual Meeting, 2009.
Ethical Approval: We declare that our protocol is in compliance with the Declaration of Helsinki principles. There were no animals involved in the study.
Informed Consent: The study was approved by the Institutional Review Board at Columbia University Medical Center, and all participants gave informed consent.
References
- 1. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043–2050. [DOI] [PubMed] [Google Scholar]
- 2. Gu Q, Dillon CF, Burt VL, Gillum RF. Association of hypertension treatment and control with all-cause and cardiovascular disease mortality among US adults with hypertension. Am J Hypertens. 2010;23(1):38–45. [DOI] [PubMed] [Google Scholar]
- 3. Yan LL, Liu K, Matthews KA, Daviglus ML, Ferguson TF, Kiefe CI. Psychosocial factors and risk of hypertension: The Coronary Artery Risk Development in Young Adults (CARDIA) study. JAMA. 2003;290(16):2138–2148. [DOI] [PubMed] [Google Scholar]
- 4. Miller TQ, Smith TW, Turner CW, Guijarro ML, Hallet AJ. A meta-analytic review of research on hostility and physical health. Psychol Bull. 1996;119(2):322–348. [DOI] [PubMed] [Google Scholar]
- 5. Lucini D, Di Fede G, Parati G, Pagani M. Impact of chronic psychosocial stress on autonomic cardiovascular regulation in otherwise healthy subjects. Hypertension. 2005;46(5):1201–1206. [DOI] [PubMed] [Google Scholar]
- 6. Sparrenberger F, Cichelero FT, Ascoli AM et al. Does psychosocial stress cause hypertension? A systematic review of observational studies. J Hum Hypertens. 2009;23(1):12–19. [DOI] [PubMed] [Google Scholar]
- 7. Markovitz JH, Jonas BS, Davidson K. Psychologic factors as precursors to hypertension. Curr Hypertens Rep. 2001;3(1):25–32. [DOI] [PubMed] [Google Scholar]
- 8. Levenstein S, Smith MW, Kaplan GA. Psychosocial predictors of hypertension in men and women. Arch Intern Med. 2001;161(10):1341–1346. [DOI] [PubMed] [Google Scholar]
- 9. Landsbergis PA, Schnall PL, Pickering TG, Warren K, Schwartz JE. Life-course exposure to job strain and ambulatory blood pressure in men. Am J Epidemiol. 2003;157(11):998–1006. [DOI] [PubMed] [Google Scholar]
- 10. Clougherty JE, Eisen EA, Slade MD, Kawachi I, Cullen MR. Workplace status and risk of hypertension among hourly and salaried aluminum manufacturing employees. Soc Sci Med. 2009;68(2):304–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chaix B, Bean K, Leal C et al. Individual/neighborhood social factors and blood pressure in the RECORD Cohort Study: Which risk factors explain the associations?Hypertension. 2010;55(3):769–775. [DOI] [PubMed] [Google Scholar]
- 12. Brummett BH, Babyak MA, Siegler IC et al. Systolic blood pressure, socioeconomic status, and biobehavioral risk factors in a nationally representative US young adult sample. Hypertension. 2011;58(2):161–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jacob RG, Chesney MA, Williams DM, Ding Y, Shapiro AP. Relaxation therapy for hypertension: Design effects and treatment effects. Ann Behav Med. 1991;13(1):5–7. [Google Scholar]
- 14. Linden W, Moseley JV. The efficacy of behavioral treatments for hypertension. Appl Psychophysiol Biofeedback. 2006;31(1):51–63. [DOI] [PubMed] [Google Scholar]
- 15. Benson J, Britten N. Patients’ views about taking antihypertensive drugs: Questionnaire study. BMJ. 2003;326(7402):1314–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schneider RH, Alexander CN, Staggers F et al. A randomized controlled trial of stress reduction in African Americans treated for hypertension for over one year. Am J Hypertens. 2005;18(1):88–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schneider RH, Alexander CN, Staggers F et al. Long-term effects of stress reduction on mortality in persons ≥55 years of age with systemic hypertension. Am J Cardiol. 2005;95(9):1060–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Crowther JH. Stress management training and relaxation imagery in the treatment of essential hypertension. J Behav Med. 1983;6(2):169–187. [DOI] [PubMed] [Google Scholar]
- 19. García-Vera MP, Sanz J, Labrador FJ. Blood pressure variability and stress management training for essential hypertension. Behav Med. 2004;30(2):53–62. [DOI] [PubMed] [Google Scholar]
- 20. García-Vera MP, Labrador FJ, Sanz J. Stress-management training for essential hypertension: A controlled study. Appl Psychophysiol Biofeedback. 1997;22(4):261–283. [DOI] [PubMed] [Google Scholar]
- 21. Gidron Y, Davidson K, Bata I. The short-term effects of a hostility-reduction intervention on male coronary heart disease patients. Health Psychol. 1999;18(4):416–420. [DOI] [PubMed] [Google Scholar]
- 22. Linden W, Lenz JW, Con AH. Individualized stress management for primary hypertension: A randomized trial. Arch Intern Med. 2001;161(8):1071–1080. [DOI] [PubMed] [Google Scholar]
- 23. Dusek JA, Hibberd PL, Buczynski B et al. Stress management versus lifestyle modification on systolic hypertension and medication elimination: A randomized trial. J Altern Complement Med. 2008;14(2):129–138. [DOI] [PubMed] [Google Scholar]
- 24. Hänsel A, von Känel R. [Psychosomatic medicine and arterial hypertension—Love it or leave it?]. Ther Umsch. 2012;69(5):315–323. [DOI] [PubMed] [Google Scholar]
- 25. Lambourne K, Washburn RA, Gibson C et al. Weight management by phone conference call: A comparison with a traditional face-to-face clinic. Rationale and design for a randomized equivalence trial. Contemp Clin Trials. 2012;33(5):1044–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wadden TA, Butryn ML, Hong PS, Tsai AG. Behavioral treatment of obesity in patients encountered in primary care settings: A systematic review. JAMA. 2014;312(17):1779–1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. US Department of Labor. Fact Sheet: The Affordable Care Act and Wellness Programs. Washington, DC: Employee Benefits Security Administration; 2014. [Google Scholar]
- 28. Taskforce CPS. The Guide to Community Preventive Services, Centers for Disease Control and Prevention. Oxford, England: Oxford University Press; 2015. [Google Scholar]
- 29. Plotnikoff R, Collins CE, Williams R, Germov J, Callister R. Effectiveness of interventions targeting health behaviors in university and college staff: A systematic review. Am J Health Promot. 2015;29(5):e169–e187. [DOI] [PubMed] [Google Scholar]
- 30. Holben DH, Rambo C, Howe C, Murray DH, Shubrook JH. Cardiovascular disease risk factors after an employer-based risk reduction program: An observational cohort study. J Am Osteopath Assoc. 2017;117(7):425–432. [DOI] [PubMed] [Google Scholar]
- 31. Wolever RQ, Bobinet KJ, McCabe K et al. Effective and viable mind-body stress reduction in the workplace: A randomized controlled trial. J Occup Health Psychol. 2012;17(2):246–258. [DOI] [PubMed] [Google Scholar]
- 32. Riley KE, Park CL, Wilson A et al. Improving physical and mental health in frontline mental health care providers: Yoga-based stress management versus cognitive behavioral stress management. J Workplace Behav Health. 2017;6(1):26–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McCraty R, Atkinson M, Lipsenthal L, Arguelles L. New hope for correctional officers: An innovative program for reducing stress and health risks. Appl Psychophysiol Biofeedback. 2009;34(4):251–272. [DOI] [PubMed] [Google Scholar]
- 34. Lucini D, Riva S, Pizzinelli P, Pagani M. Stress management at the worksite: Reversal of symptoms profile and cardiovascular dysregulation. Hypertension. 2007;49(2):291–297. [DOI] [PubMed] [Google Scholar]
- 35. Williams VP, Brenner SL, Helms MJ, Williams RB. Coping skills training to reduce psychosocial risk factors for medical disorders: A field trial evaluating effectiveness in multiple worksites. J Occup Health. 2009;51(5):437–442. [DOI] [PubMed] [Google Scholar]
- 36. Campo AE, Williams V, Williams RB, Segundo MA, Lydston D, Weiss SM. Effects of LifeSkills training on medical students’ performance in dealing with complex clinical cases. Acad Psychiatry. 2008;32(3):188–193. [DOI] [PubMed] [Google Scholar]
- 37. Li C, Chu F, Wang H, Wang XP. Efficacy of Williams LifeSkills training for improving psychological health: A pilot comparison study of Chinese medical students. Asia Pac Psychiatry. 2014;6(2):161–169. [DOI] [PubMed] [Google Scholar]
- 38. Kirby ED, Williams VP, Hocking MC, Lane JD, Williams RB. Psychosocial benefits of three formats of a standardized behavioral stress management program. Psychosom Med. 2006;68(6):816–23. [DOI] [PubMed] [Google Scholar]
- 39. Bishop GD, Kaur D, Tan VL, Chua YL, Liew SM, Mak KH. Effects of a psychosocial skills training workshop on psychophysiological and psychosocial risk in patients undergoing coronary artery bypass grafting. Am Heart J. 2005;150(3):602–609. [DOI] [PubMed] [Google Scholar]
- 40. Williams VP, Bishop-Fitzpatrick L, Lane JD et al. Video-based coping skills to reduce health risk and improve psychological and physical well-being in Alzheimer’s disease family caregivers. Psychosom Med. 2010;72(9):897–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Barnes VA, Johnson MH, Williams RB, Williams VP. Impact of Williams LifeSkills® training on anger, anxiety and ambulatory blood pressure in adolescents. Transl Behav Med. 2012;2(4):401–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McVicar A. Workplace stress in nursing: A literature review. J Adv Nurs. 2003;44(6):633–642. [DOI] [PubMed] [Google Scholar]
- 43. Schulz KF, Altman DG, Moher D; CONSORT Group CONSORT 2010 statement: Updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152(11):726–732. [DOI] [PubMed] [Google Scholar]
- 44. Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB Jr. The Cook-Medley hostility scale: Item content and ability to predict survival. Psychosom Med. 1989;51(1):46–57. [DOI] [PubMed] [Google Scholar]
- 45. Cook W, Medley D. Proposed hostility and pharisaic-virtue scales for the MMPI. J Appl Psychol. 1954;38(6):414–418. [Google Scholar]
- 46. Beckett L, Godwin M. The BpTRU automatic blood pressure monitor compared to 24 hour ambulatory blood pressure monitoring in the assessment of blood pressure in patients with hypertension. bmc Cardiovasc Disord. 2005;5(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Goldberg EM, Wilson T, Saucier C et al. Achieving the BpTRUth: Emergency department hypertension screening and the Centers for Medicare & Medicaid Services quality measure. J Am Soc Hypertens. 2017;11(5):290–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pickering TG, Hall JE, Appel LJ et al. ; Council on High Blood Pressure Research Professional and Public Education Subcommittee, American Heart Association Recommendations for blood pressure measurement in humans: An AHA scientific statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. J Clin Hypertens (Greenwich). 2005;7(2):102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chobanian AV, Bakris GL, Black HR et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289(19):2560–2571. [DOI] [PubMed] [Google Scholar]
- 50. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 51. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. j Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 52. Maslach C, Jackson SE, Leiter MP.. Maslach Burnout Inventory Manual. Mountain View. Sunnyvale, CA: CPP; 1996. [Google Scholar]
- 53. Maslach C, Leiter MP. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. [DOI] [PubMed] [Google Scholar]
- 55. Hedlund BL, Lindquist CU. The development of an inventory for distinguishing among passive, aggressive, and assertive behavior. Behav Assess. 1984;6(4):379–390. [Google Scholar]
- 56. Cohen S, Hoberman H. Positive events and social supports as buffers of life change stress. J Appl Soc Psychol. 1983;13(2):99–125. [Google Scholar]
- 57. Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognit Ther Res. 2003;27(3):247–259. [Google Scholar]
- 58. National Institutes of Health. Facts About Lowering Blood Pressure. Washington, DC: US Department of Health and Human Services, NIH publication number 03-5232; 2000. [Google Scholar]
- 59. National Institutes of Health. Reference Card from the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of high blood pressure (NJC-7). Washington, DC: US Department of Health and Human Services, NIH 03-5231; 2003. [Google Scholar]
- 60. Little R, Yau L. Intent-to-treat analysis for longitudinal studies with drop-outs. Biometrics. 1996;52(4):1324–1333. [PubMed] [Google Scholar]
- 61. Chakraborty H, Gu H.. A Mixed-model Approach for Intent-to-treat Analysis in Longitudinal Clinical Trials With Missing Values. Research Triangle Park. NC: RTI International; 2009. [PubMed] [Google Scholar]
- 62. Bauer DJ, Preacher KJ, Gil KM. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychol Methods. 2006;11(2):142–163. [DOI] [PubMed] [Google Scholar]
- 63. Netterstrøm B, Friebel L, Ladegaard Y. Effects of a multidisciplinary stress treatment programme on patient return to work rate and symptom reduction: Results from a randomised, wait-list controlled trial. Psychother Psychosom. 2013;82(3):177–186. [DOI] [PubMed] [Google Scholar]
- 64. Key BL, Campbell TS, Bacon SL, Gerin W. The influence of trait and state rumination on cardiovascular recovery from a negative emotional stressor. j Behav Med. 2008;31(3):237–248. [DOI] [PubMed] [Google Scholar]
- 65. Gerin W, Davidson KW, Christenfeld NJ, Goyal T, Schwartz JE. The role of angry rumination and distraction in blood pressure recovery from emotional arousal. Psychosom Med. 2006;68(1):64–72. [DOI] [PubMed] [Google Scholar]
- 66. Hogan BE, Linden W. Anger response styles and blood pressure: At least don’t ruminate about it!Ann Behav Med. 2004;27(1):38–49. [DOI] [PubMed] [Google Scholar]
- 67. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913. [DOI] [PubMed] [Google Scholar]