Abstract
Introduction
Chronic kidney disease (CKD) requires patients and caregivers to invest in self-care and self-management of their disease. We aimed to describe the work for adult patients that follows from these investments and develop an understanding of burden of treatment (BoT).
Methods
Systematic review of qualitative primary studies that builds on EXPERTS1 Protocol, PROSPERO registration number: CRD42014014547. We included research published in English, Spanish and Portuguese, from 2000 to present, describing experience of illness and healthcare of people with CKD and caregivers. Searches were conducted in MEDLINE, Embase, CINAHL Plus, PsycINFO, Scopus, Scientific Electronic Library Online and Red de Revistas Científicas de América Latina y el Caribe, España y Portugal. Content was analysed with theoretical framework using middle-range theories.
Results
Searches resulted in 260 studies from 30 countries (5115 patients and 1071 carers). Socioeconomic status was central to the experience of CKD, especially in its advanced stages when renal replacement treatment is necessary. Unfunded healthcare was fragmented and of indeterminate duration, with patients often depending on emergency care. Treatment could lead to unemployment, and in turn, to uninsurance or underinsurance. Patients feared catastrophic events because of diminished financial capacity and made strenuous efforts to prevent them. Transportation to and from haemodialysis centre, with variable availability and cost, was a common problem, aggravated for patients in non-urban areas, or with young children, and low resources. Additional work for those uninsured or underinsured included fund-raising. Transplanted patients needed to manage finances and responsibilities in an uncertain context. Information on the disease, treatment options and immunosuppressants side effects was a widespread problem.
Conclusions
Being a person with end-stage kidney disease always implied high burden, time-consuming, invasive and exhausting tasks, impacting on all aspects of patients' and caregivers’ lives. Further research on BoT could inform healthcare professionals and policy makers about factors that shape patients’ trajectories and contribute towards a better illness experience for those living with CKD.
PROSPERO registration number
CRD42014014547.
Keywords: treatment burden, chronic kidney disease, systematic review, haemodialysis, kidney transplant
Strengths and limitations of this study.
We analysed data with a coding framework supported by middle-range theories to understand the work involved in being a person with chronic kidney disease.
Comprehensive inclusion of publications in English, Spanish and Portuguese, which may enhance the transferability of our findings.
The variety of methodologies, quality of reporting and heterogeneity of perspectives make synthesis difficult.
Introduction
Chronic kidney disease (CKD) contributes significantly to global morbidity and mortality.1–4 Even in its early stages, the risk of death, cardiovascular events, cerebrovascular disorders, hospitalisation, reduced health-related quality of life, anxiety, depression and suicidal ideation is increased.1–6
Worldwide, about 500 million people are affected by CKD; about 80% of these live in low-income and middle-income countries (LMIC); an estimated 3 million people with end-stage kidney disease (ESKD) receive renal replacement therapy (RRT) with either dialysis or transplantation.1 7 8 The number of people receiving RRT is increasing and will more than double by 2030, but a significant number of people without access to this type of live-saving treatment will remain.9 In 2010, at least 2.28 million people might have died because of lack of access to RRT, mostly in LMIC in Asia, Africa and Latin America.9
Much is now known about the pathophysiological and treatment trajectories of CKD, and about the associated burden of symptoms experienced by patients. More recently, there has been increasing interest in the way that complex long-term conditions require patients and their carers to invest in self-care and self-management of their disease.10–15 The work for patients and carers that follows from these investments, including medication management, medical visits, laboratory tests, lifestyle changes and monitoring in addition to the activities done as part of life, is here termed burden of treatment (BoT), which adds to the burden of symptoms (BoS).10 13 16 Research on BoT has focused on long-term conditions such as diabetes, chronic obstructive pulmonary disease and chronic heart failure, with the development of analytic framework and patient-created taxonomies.10 16–27 Patients and carers are expected to actively participate in managing both index conditions and comorbidities and, depending on their resources or lack thereof, they often need to negotiate or renegotiate the responsibilities that healthcare providers and healthcare systems assign to them.13 28 29 Patients' and carers’ experience in managing the disease and its treatment, including their choices and expectations, is affected by structural, relational and resilience factors; the interactions among these factors remain understudied.30 The aim of this study is to develop specific understanding of treatment burden experienced by people with CKD and ESKD extending it to experiences of uninsured and underinsured patients in LMIC.
Methods
This is a systematic review of primary qualitative studies, which builds on the published EXPERTS1 Protocol and its meta-review of qualitative reviews.30 31 PROSPERO registration number is CRD42014014547. This review follows the Enhancing Transparency in Reporting the Synthesis of Qualitative Research framework.32 We interrogated a subset of qualitative primary research papers concerned with CKD identified by EXPERTS1 qualitative meta-review to understand the dynamics of patient experience of complexity and treatment burden in long-term life-limiting conditions. EXPERTS1 search was updated and expanded to Spanish and Portuguese language literature.
Eligibility, inclusion and exclusion criteria
Eligibility criteria for study inclusion were developed using the participants, interventions, comparators and outcomes framework (table 1). Inclusion criteria were primary qualitative and mixed-method studies of adult patients diagnosed with CKD in any stage and their formal or informal carers; in any type of treatment or healthcare provision; not limited to comparative studies; with qualitative data on the patients' and carers’ experiences on any aspect of CKD, in any stage, and its treatments; in English, Spanish and Portuguese. Following the EXPERTS1 protocol, studies were excluded if they were of other EXPERTS1 index conditions; if they reported results of treatments, interventions, tests or surveys; were guidelines, discussions of the literature or editorials, notes, news, letters and case reports; if the experiences described by patients and carers could not be clearly discriminated.31 Studies describing experiences of children with CKD were excluded because their BoT may be significantly different from that of adult patients. The year of publication 2000 onwards was established to include current treatments.
Table 1.
PICO criteria for including studies
| Population | Patients of at least 18 years of age, diagnosed with CKD, and formal and informal carers. |
| Intervention | Experiences of healthcare provision, any type of treatment for CKD. |
| Comparator | Not limited to comparator studies. |
| Outcomes | Qualitative data on patients' and carers’ experiences of care for those patients with CKD. |
| Study type | Primary studies, qualitative or mixed methods studies. |
| Time | From 2000 to present. |
CKD, chronic kidney disease; PICO, participants, interventions, comparators and outcomes.
Study selection
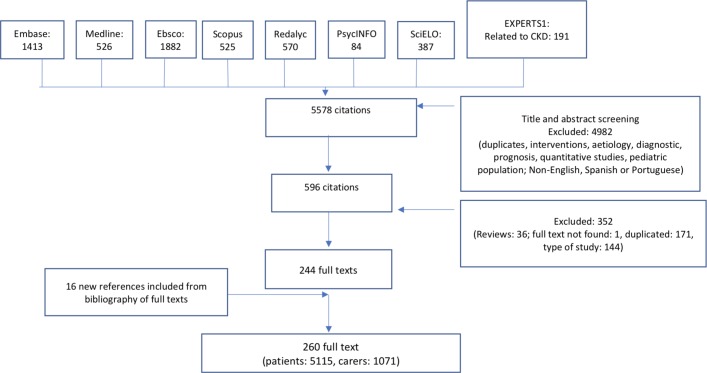
A first search for the EXPERTS1 meta-review was conducted in MEDLINE, Embase, CINAHL Plus, PsycINFO and Scopus. For this review, searches were updated using the same databases and expanded to include studies published in Spanish and Portuguese with additional searches in the Iberoamerican databases Scientific Electronic Library Online and Red de Revistas Científicas de América Latina y el Caribe, España y Portugal. Searches were completed by April 2017 and identified papers published between 1 January 2000 and March 2017. Search strategy is included in supplementary appendix 1. For a first set of studies, titles and abstracts were independently screened by AC, MM and CRM, disagreements resolved by JH. Full-text papers (n=1238) were obtained and screened by JH, KAL and MM; disagreements resolved by KH or AC. Of 606 articles, 191 were related to CKD. For a second set, updated results in English and studies in Spanish and Portuguese were screened by JR, JPA, disagreements resolved by FC. Two authors (JR, JPA) assessed papers against the Critical Appraisal Skills Programme qualitative research checklist.33 As there is no accepted criteria for the exclusion of qualitative studies-based appraisal score, we did not exclude studies based on quality. See figure 1 for screening and selection process.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart of screening and selection process. CKD, chronic kidney disease.
bmjopen-2018-023507supp001.pdf (21.9KB, pdf)
Data extraction and analysis
Data outlining study characteristics are shown in table 2. Manuscripts were entered into Atlas.Ti V.7.5.12 (Scientific Software Development GmbH). The results sections and participant quotations of the primary studies were analysed line-by-line using directed content analysis, sometimes called framework analysis.34 The coding frame drew on concepts from the Burden of Treatment Theory and the Cognitive Authority Theory.18–21 29 35 36 Coding was conducted by JR and CRM, with a third party involved for disagreements (JPA), and reviewed and discussed by two researchers (AC, MM). Refinement of the coding frame and analysis was iterative, codes were identified or merged reading the result sections of primary studies and consulting the theoretical framework. Investigator triangulation (comparison of results of two or more researchers) was used to capture relevant issues, reflect participants’ experience as reported and ensure the credibility of the findings.
Table 2.
Characteristics of included studies
| Author | Year | Country | Setting | Patients | Carers | Type of patient | Data collection | Data analysis reported |
| Aasen et al 107 | 2012 | Norway | 5 H, East, West | 11 | ESKD | Interviews | Critical discourse | |
| Aasen et al 246 | 2012 | Norway | 5 H, East, West | 7 | ESKD | Interviews | Critical discourse | |
| Aasen287 | 2012 | Norway | 5 H, East, West | 11 | 17 | ESKD | Interviews | Critical discourse |
| Al-Arabi104 | 2006 | USA | 1 C, Southwest | 80 | ESKD | Interviews | Naturalistic inquiry, thematic | |
| Allen et al 173 | 2011 | Canada | 1 H, urban | 7 | ESKD | Ethnographic observations, interviews | Participatory action, thematic | |
| Allen et al 64 | 2015 | Canada | 2 H | 6 | 11 | ESKD | Ethnographic observations, interviews | Thematic |
| Anderson et al 77 | 2008 | Australia | 9 H, 17 C | 241 | ESKD | Interviews | Thematic | |
| Anderson et al 53 | 2012 | Australia | 9 H, 17 C | 241 | ESKD | Interviews | Thematic | |
| Arslan and Ege200 | 2009 | Turkey | 1 H, Kenya | 10 | ESKD | Interviews | Content | |
| Ashby et al 38 | 2005 | Australia | 2 H, Melbourne | 16 | ESKD | Interviews | Grounded theory | |
| Avril-Sephula et al 118 | 2014 | UK | 1 H, North | 8 | ESKD | Interviews | Thematic | |
| Axelsson et al 187 | 2012 | Sweden | 2 H, 2 C | 8 | ESKD | Interviews | Phenomenological, hermeneutical | |
| Axelsson et al 136 | 2012 | Sweden | 2 H, 2 C | 8 | ESKD | Interviews | Phenomenological, hermeneutical | |
| Axelsson et al 134 | 2015 | Sweden | 2 H, 1 C, urban | 14 | ESKD | Interviews | Content | |
| Bailey et al 235 | 2015 | UK | Bristol | 32 | Transplanted | Interviews | Constant comparison | |
| Bailey et al 39 | 2016 | UK | Bristol | 13 | Transplanted | Interviews | Constant comparison | |
| Baillie and Lankshear156 | 2015 | UK | Wales | 16 | 9 | ESKD | Interviews | Thematic |
| Baillie and Lankshear157 | 2015 | UK | Wales | 16 | 9 | ESKD | Interviews | Thematic |
| Barbosa and Valadares145 | 2009 | Brazil | 1 C, Rio de Janeiro | 10 | ESKD | Interviews | Grounded theory | |
| Bath et al 252 | 2003 | UK | South | 10 | ESKD | Interviews | Phenomenological | |
| Beanlands et al 210 | 2005 | Canada | Ontario | 37 | ESKD | Interviews | Grounded theory | |
| Bennett et al 197 | 2013 | Australia | 4 C | 9 | 2 | ESKD | Interviews facilitated by images | Thematic |
| Blogg and Hyde69 | 2008 | Australia | Urban | 5 | ESKD | Interviews | Ethnographic | |
| Boaz and Morgan175 | 2014 | UK | Rural, urban | 25 | Transplanted | Interviews | Constant comparison | |
| Bourbonnais and Tousignant105 | 2012 | Canada | 1 H | 25 | ESKD | Interviews | Content | |
| Bridger238 | 2009 | UK | GP, South | 23 | CKD | Interviews, drawings, journals | Grounded theory | |
| Bristowe et al 126 | 2015 | UK | 2 C, London | 20 | ESKD | Interviews | Thematic | |
| de Brito-Ashurst et al 121 | 2011 | UK | London | 20 | CKD | Focus groups, vignettes and diaries | Thematic | |
| Browne et al 226 | 2016 | USA | South | 40 | ESKD | Focus groups | Content | |
| Buldukoglu et al 186 | 2005 | Turkey | Antalya | 40 | Transplanted | Open-ended questions | Constant comparison | |
| Burnette and Kickett78 | 2009 | Australia | 1 C, Perth | 6 | ESKD | Interviews | Thematic | |
| Cadena et al 154 | 2015 | Mexico | Coyotepec, Mexico | 5 | ESKD | Interviews | Interpretative phenomenological | |
| Calvey and Mee146 | 2011 | Ireland | NA | 7 | ESKD | Interviews | Colaizzi’s method | |
| Calvinl 251 | 2004 | USA | 3 C, Texas | 12 | ESKD | Interviews | Constant comparison | |
| Calvin et al 292 | 2014 | USA | Texas | 18 | ESKD | Interviews | Interpretative, Glaserian | |
| Campos and Turato234 | 2003 | Brazil | 1 H, Sao Paulo | 7 | ESKD | Interviews | Thematic | |
| Campos and Turato87 | 2010 | Brazil | 1 H, Sao Paulo | 7 | ESKD | Interviews | Thematic | |
| Campos et al 88 | 2015 | Brazil | H, C, Paraná | 23 | ESKD | Interviews | Content | |
| Cases et al 279 | 2011 | UK | NA | 6 | ESKD | Interviews | Phenomenological | |
| Cervantes et al 52 | 2017 | USA | 1 H, Colorado | 20 | ESKD | Interviews | Thematic | |
| Chatrung et al 188 | 2015 | USA | California | 8 | CKD | Interviews | Thematic | |
| Chenitz et al 86 | 2014 | USA | 4 C, Pennsylvania | 30 | ESKD | Interviews | Grounded theory | |
| Chiaranai40 | 2016 | Thailand | 1 H | 26 | ESKD | Interviews | Thematic | |
| Cho and Shin41 | 2016 | South Korea | 1 H, South | 5 | ESKD | Interviews | Colaizzi’s method | |
| Chong et al 164 | 2016 | South Korea | 1 H, South | 8 | ESKD | Interviews | Content | |
| Clarkson and Robinson106 | 2010 | USA | Oklahoma | 10 | ESKD | Interviews | Thematic | |
| Costa et al 198 | 2014 | Brazil | 3 H, Paraíba | 26 | ESKD | Interviews | Lexical | |
| Costantini et al 92 | 2008 | Canada | Ontario | 14 | CKD | Interviews | Content | |
| Cox et al 148 | 2016 | USA | 6 C, New Mexico | 50 | ESKD | Interviews | Interpretive description | |
| Cramm et al 219 | 2015 | The Netherlands | 1 H, Rotterdam | 15 | 12 | ESKD | Interviews | Factor analysis, Q methodology |
| Cristóvao et al 113 | 2013 | Portugal | 1 C, Lisbon | 20 | ESKD | Interviews | Thematic | |
| Crowley-Matoka et al 83 | 2005 | Mexico | 2 prog, Guadalajara | 50 | Transplanted | Interviews | NA | |
| Curtin et al 265 | 2001 | USA | Diverse | 18 | ESKD | Interviews | Content | |
| Curtin et al 264 | 2002 | USA | 18 | ESKD | Interviews | Content | ||
| da Silva et al 103 | 2016 | Brazil | 1 C, Northeast | 30 | ESKD | Interviews | Content and thematic | |
| da Silva et al 338 | 2011 | Brazil | 1 H, Rio Grande do Sul | 9 | ESKD | Interviews | Qualitative | |
| Darrell et al 281 | 2016 | USA | 1 H | 12 | ESKD | Interviews | Giorgi’s method | |
| Davison et al 231 | 2006 | Canada | Alberta | 24 | ESKD | Interviews | Constant comparison, iterative | |
| Davison et al 291 | 2006 | Canada | 1 H | 19 | ESKD | Interviews | inductive | |
| de Brito et al 89 | 2015 | Brazil | 1 H, Minas Gerais | 50 | Transplanted | Interviews | Collective subject technique | |
| de Rosenroll et al 277 | 2013 | Canada | 1 H | 10 | ESKD | Interviews | Constant comparison | |
| Dekkers et al 42 | 2005 | The Netherlands | 2 C | 7 | ESKD | Interviews | Phenomenological | |
| DePasquale et al 221 | 2013 | USA | NP, 1 C | 68 | 62 | CKD | Group interviews | Mixed method |
| dos Reis et al 155 | 2008 | Brazil | 1 H, Sao Paulo | 8 | ESKD | Interviews | Content | |
| dos Santos et al 162 | 2011 | Brazil | Rio de Janeiro | 8 | ESKD | Interviews | Grounded theory | |
| dos Santos et al 259 | 2015 | Brazil | 3 NP, Rio Grande do Sul | 20 | Transplanted | Interviews | Critical incident | |
| Ekelund et al 43 | 2010 | Sweden | 1 C, South | 39 | 21 | ESKD | Interviews | Content |
| Erlang et al 203 | 2015 | Denmark | 1 H | 9 | CKD (predialysis) | Interviews | Systematic text condensation | |
| Eslami et al 214 | 2016 | Iran | 4 C, Isfahan | 20 | ESKD | Interviews | Thematic | |
| Finnegan-John et al 90 | 2013 | UK | 1 trust, London | 118 | 12 | CKD/ESKD | Interviews and focus groups | Thematic |
| Flores et al 165 | 2004 | Brazil | 1 H, Rio Grande do Sul | 9 | ESKD | Interviews | Content | |
| Fraguas et al 37 | 2008 | Brazil | 2 H, Minas Gerais | 18 | ESKD | Interviews | Content | |
| Ghadami et al 239 | 2012 | Iran | 1 charity, Isfahan | 15 | Transplanted | Interviews | Content | |
| Giles et al 159 | 2003 | Canada | 1 H, urban | 4 | ESKD | Interviews | Thematic | |
| Giles et al 160 | 2005 | Canada | 4 | ESKD | Interviews | Phenomenological | ||
| Goff et al 288 | 2015 | USA | New Mexico | 13 | 9 | ESKD | Interviews | Thematic |
| Goldane et al 176 | 2011 | USA | 1 C | 39 | Transplanted | Focus groups and interviews | Iterative analysis | |
| Gordon et al 180 | 2007 | USA | 20 | Transplanted | Diary entries | Thematic | ||
| Gordon et al 84 | 2009 | USA | 2 H, Illinois, New York | 82 | Transplanted | Interviews | Thematic | |
| Gricio et al 114 | 2009 | Brazil | 1 H, Sao Paulo | 20 | ESKD | Interviews | Thematic | |
| Gullick et al 339 | 2016 | Australia | 1 H, Sydney | 11 | 5 | ESKD | Interviews | Hermeneutic interpretation |
| Hagren et al 282 | 2001 | Sweden | 1 H | 15 | ESKD | Interviews | Content | |
| Hagren et al 115 | 2005 | Sweden | 3 H | 41 | ESKD | Interviews | Content | |
| Hain et al 189 | 2011 | USA | 6 C, Southeast | 56 | ESKD | Interviews | Story inquiry method | |
| Hanson et al 70 | 2016 | Australia | 1 C, West | 20 | ESKD | Interviews | Thematic | |
| Harrington et al 283 | 2016 | UK | 8 H | 24 | Transplanted | Interviews | Thematic | |
| Harwood et al 270 | 2014 | Canada | 1 H | 13 | ESKD | Interviews | Content | |
| Harwood et al 248 | 2005 | UK | 1 H, London | 11 | CKD/ESKD | Interviews | Content | |
| Haspeslagh et al 240 | 2013 | Belgium | 1 H, Leuven | 31 | Transplanted | Interviews and questionnaires | Thematic | |
| Heiwe et al 137 | 2003 | Sweden | 1 H, Karolinska | 16 | ESKD | Interviews | Contextual | |
| Heiwe et al 140 | 2004 | Sweden | 1 H, Karolinska | 16 | CKD/ESKD | Interviews | Contextual | |
| Herbias et al 116 | 2016 | Chile | 1 C, Santiago | 12 | ESKD | Interviews | Streubert’s method | |
| Herlin et al 284 | 2010 | Sweden | 3 C | 9 | ESKD | Interviews | Giorgi’s method | |
| Hollingdale et al 227 | 2008 | UK | 20 | CKD/ESKD | Focus groups | Framework approach | ||
| Hong et al 120 | 2017 | Singapore | 1 H | 14 | ESKD | Interviews | Thematic | |
| Horigan et al 138 | 2013 | USA | 1 C, Mid-Atlantic | 14 | ESKD | Interviews | Content | |
| Hutchison et al 290 | 2017 | Canada | 1 clinic, urban | 9 | 16 | CKD/ESKD | Interviews | Interpretive description |
| Iles-Smith et al 232 | 2005 | UK | 1 C, Manchester | 10 | CKD (predialysis) | Interviews | Thematic | |
| Johnston et al 128 | 2012 | UK | 1 trust, London | 9 | ESKD | Interviews | Thematic | |
| Kaba et al 340 | 2007 | Greece | 2 H, Athens | 23 | ESKD | Interviews | Qualitative | |
| Kahn et al 35 | 2015 | USA | 2 NP, New York | 34 | CKD | Interviews | Thematic | |
| Karamanidou et al 15 | 2014 | UK | 1 C, London | 7 | ESKD | Interviews | Interpretative, phenomenological | |
| Kazley et al 44 | 2015 | USA | 1 C, Southeast | 20 | CKD/ESKD | Focus groups | Thematic | |
| Keeping et al 73 | 2001 | Canada | East | 8 | ESKD | Interviews | Thematic | |
| Kierans et al 167 | 2001 | Ireland | 5 | ESKD | Interviews, life stories | Phenomenological | ||
| Kierans et al 166 | 2005 | Ireland | 5 | CKD/ESKD | Interviews | Phenomenological | ||
| Kierans et al 125 | 2013 | Mexico | 1 H, Jalisco | 51 | 87 | CKD/ESKD, transplanted | Interviews, observation* | Ethnographic approach |
| King et al 91 | 2002 | UK | 1 C | 22 | CKD/ESKD | Interviews | Template approach | |
| Knihs et al 168 | 2013 | Brazil | 1 C, South | 20 | ESKD | Interviews | Content | |
| Krespi-Boothby et al 147 | 2004 | UK | 1 H, 4 C | 16 | ESKD | Interviews | Thematic | |
| Krespi-Boothby et al 151 | 2013 | UK | 1 H, 4 C | 16 | ESKD | Interviews | Template approach | |
| Ladin et al 202 | 2016 | USA | 2 C, Massachusetts | 23 | ESKD | Interviews | Thematic | |
| Ladin et al 269 | 2017 | USA | 2 C, Massachusetts | 31 | ESKD | Interviews | Thematic Nutbeam’s framework | |
| Landreneau et al 274 | 2006 | USA | 1 C, 1 NP, South | 6 | ESKD | Interviews | Colaizzi’s method | |
| Landreneau et al 278 | 2007 | USA | 2 C, South | 12 | ESKD | Interviews | Colaizzi’s method | |
| Lawrence et al 169 | 2013 | UK | 1 C | 10 | ESKD | Interviews | Conceptual and categorical | |
| Lederer et al 266 | 2015 | USA | 1 C | 32 | CKD/ESKD | Interviews | Thematic | |
| Lee et al 223 | 2008 | Denmark | Diverse | 27 | 18 | ESKD | Focus groups | Thematic |
| Lee et al 45 | 2016 | Singapore | 1 organisation | 20 | ESKD | Interviews | Thematic | |
| Lenci et al 256 | 2012 | USA | 4 | ESKD | Interviews | Thematic | ||
| Leung et al 181 | 2007 | Hong Kong | 1 C | 12 | Transplanted | Interviews | Content | |
| Lewis et al 285 | 2015 | UK | 14 H | 40 | ESKD | Interviews | Grounded theory | |
| Lin et al 190 | 2015 | Taiwan | 1 C, S, rural | 15 | ESKD | Interviews | Constant comparison | |
| Lindberg et al 46 | 2008 | Sweden | 1 C, mid-country | 10 | ESKD | Interviews | Content | |
| Lindberg et al 262 | 2013 | Sweden | 1 C, mid-country | 10 | ESKD | Interviews | Content | |
| Lindsay et al 280 | 2014 | Australia | 1 C, Sydney | 7 | ESKD | Interviews | Thematic | |
| Llewellyn et al 271 | 2014 | UK | 4 C, London | 19 | ESKD | Interviews | Thematic | |
| Lo et al 129 | 2016 | Australia | 4 H, Melbourne, Sydney | 58 | CKD/ESKD | Interviews and focus groups | Thematic | |
| Lopes et al 170 | 2014 | Brazil | 1 C, Santa Catarina | 12 | ESKD | Interviews | Interpretative | |
| Lopez-Vargas et al 94 | 2014 | Australia | 3 C, New South Wales | 38 | CKD | Focus groups | Thematic | |
| Lopez-Vargas et al 93 | 2016 | Australia | 3 C, New South Wales | 38 | CKD/ESKD | Focus groups | Thematic | |
| Lovink et al 217 | 2015 | The Netherlands | 1 C | 12 | ESKD | Interviews | Content | |
| Low et al 161 | 2014 | UK | 5 C, Southeast | 26 | ESKD | Interviews | Thematic | |
| Machado et al 149 | 2003 | Brazil | Sao Paulo | 18 | ESKD | Interviews | Discourse | |
| Marques et al 228 | 2014 | Brazil | Paraná | 10 | ESKD | Interviews | Content | |
| Martin-McDonald et al 194 | 2003 | Australia | 5 C | 10 | ESKD | Interviews | Thematic | |
| Martin-McDonald et al 195 | 2003 | Australia | 1 C | 10 | ESKD | Interviews | Thematic | |
| Mason et al 95 | 2007 | UK | 1 C | 9 | 5 | CKD | Focus groups | Framework approach |
| McCarthy et al 163 | 2010 | Australia | 1 H | 5 | ESKD | Interviews | Sequential | |
| McKillop et al 267 | 2013 | UK | Clinics | 10 | CKD | Interviews | Thematic | |
| Mercado-Martínez et al 49 | 2014 | Mexico | Jalisco, San Luis Potosí | 21 | Transplanted | Interviews | Thematic | |
| Mercado-Martínez et al 48 | 2015 | Brazil | 1 H, South | 11 | 5 | ESKD | Interviews | Content |
| Mercado-Martínez et al 47 | 2015 | Mexico | Public H and institutions, Jalisco | 37 | 50 | ESKD | Interviews | Content |
| Mitchell et al 205 | 2009 | UK | 1 C | 10 | CKD/ESKD | Interviews | Content | |
| Molzahn et al 294 | 2012 | Canada | Middle size city | 14 | CKD | Interviews | Thematic | |
| Moran et al 204 | 2009 | Ireland | 1 H | 16 | ESKD | Interviews | Interpretive | |
| Moran et al 150 | 2009 | Ireland | 1 H | 16 | ESKD | Interviews | Interpretive | |
| Moran et al 133 | 2011 | Ireland | H | 16 | ESKD | Interviews | Interpretative | |
| Morton et al 79 | 2010 | Australia | Diverse | 95 | ESKD | Interviews | Thematic | |
| Muduma et al 96 | 2016 | UK | 2 C | 37 | Transplanted | Focus groups | Qualitative | |
| Nagpal et al 218 | 2017 | USA | 1 C, New York | 36 | ESKD | Interviews | Coding | |
| Namiki et al 220 | 2010 | Australia | 1 H | 4 | ESKD | Interviews | Thematic | |
| Niu et al 196 | 2017 | China | 1 C, Jiangsu | 23 | ESKD | Interviews | Continuous comparison | |
| Nobahar et al 67 | 2016 | Iran | 1 H, Semnan | 8 | 12 | ESKD | Interviews | Graneheim Lundman content |
| Nobahar et al 68 | 2016 | Iran | 1 H, Semnan | 8 | 12 | ESKD | Interviews | Granheim and Lundman’s approach |
| Noble et al 293 | 2009 | UK | 1 service, London | 30 | 17 | ESKD | Interviews | Constant comparison |
| Noble et al 98 | 2010 | UK | 1 service, London | 30 | 17 | ESKD | Interviews | Constant comparison |
| Noble et al 97 | 2012 | UK | 1 service | 19 | ESKD | Interviews | Constant comparison | |
| Nygardh et al 289 | 2011 | Sweden | 1 C, South | 12 | CKD (predialysis) | Interviews | Content | |
| Nygardh et al 236 | 2011 | Sweden | 1 C, South | 20 | CKD | Interviews | Latent content | |
| Malheiro Oliveira et al 209 | 2012 | Brazil | Bahia | 19 | ESKD | Interviews | Categorical | |
| Orr et al 182 | 2007 | UK | 1 C | 26 | Transplanted | Focus groups | Thematic | |
| Orr et al 183 | 2007 | UK | 1 C | 26 | Transplanted | Focus groups | Thematic | |
| Oyegbile et al 65 | 2016 | Nigeria | 2 H, Southwest | 15 | ESKD | Interviews | Content | |
| Pelletier-Hibbert et al 286 | 2001 | Canada | East | 41 | ESKD | Focus groups | Thematic | |
| Piccoli et al 224 | 2010 | Italy | 1 H | 12 | CKD/ESKD, transplanted | Focus groups | Not clear | |
| Pietrovski et al 208 | 2006 | Brazil | 1 H, Paraná | 15 | ESKD | Interviews | Content | |
| Pilger et al 225 | 2010 | Brazil | 1 C, Paraná | 22 | ESKD | Interviews | Thematic | |
| Polaschek et al 54 | 2003 | New Zealand | 1 C | 6 | ESKD | Interviews | Thematic | |
| Polaschek et al 55 | 2006 | New Zealand | 1 regional department | 20 | ESKD | Interviews | Thematic | |
| Polaschek et al 56 | 2007 | New Zealand | 1 regional department | 20 | ESKD | Interviews | Thematic | |
| Prieto et al 130 | 2011 | Spain | Andalusia | 22 | ESKD | Interviews | Discourse | |
| Rabiei et al 141 | 2015 | Iran | Isfahan | 20 | ESKD | Interviews | Thematic | |
| Ravenscroft et al 260 | 2005 | Canada | 3 C | 7 | ESKD | Interviews | Inductive | |
| Reid et al 268 | 2012 | UK | 1 C, clinics | 11 | CKD/ESKD | Interviews | Thematic | |
| Reta et al 131 | 2014 | Spain | 1 H, Araba | 14 | ESKD | Interviews | Content | |
| Richard et al 108 | 2010 | USA | 14 | ESKD | Interviews | Cultural negotiation model framework | ||
| Rifkin et al 99 | 2010 | USA | 1 C | 20 | CKD/ESKD | Interviews | Thematic | |
| Rix et al 58 | 2014 | Australia | New South Wales, rural | 18 | ESKD | Interviews | Thematic | |
| Rix et al 57 | 2015 | Australia | New South Wales, rural | 18 | 29 | ESKD | Interviews | Thematic |
| Rodrigues et al 191 | 2011 | Brazil | 1 C, South | 8 | ESKD | Interviews | Categorical | |
| Ros et al 244 | 2012 | USA | 1 H, Maryland | 19 | ESKD | Focus groups | Thematic | |
| Roso et al 119 | 2013 | Brazil | 1 H, South | 15 | ESKD | Narrative interviews | Thematic | |
| Russ et al 229 | 2005 | USA | 2 C, California | 43 | ESKD | Interviews | Anthropologic study | |
| Russell et al 241 | 2003 | USA | 1 C, Midwest | 16 | Transplanted | Interviews | Constant comparison | |
| Rygh et al 71 | 2012 | Norway | North | 11 | ESKD | Interviews | Inductive, actor’s point of view | |
| Sadala et al 72 | 2012 | Brazil | 1 H | 19 | ESKD | Narrative interviews | Phenomenological, hermeneutical | |
| Sahaf et al 222 | 2017 | Iran | 2 hour, Sari | 9 | ESKD | Interviews | van Manen’s thematic | |
| Salvalaggio et al 82 | 2003 | Canada | 1 H, Ontario | 12 | ESKD | Interviews | Immersion/crystalisation | |
| Schell et al 272 | 2012 | USA | 1 university system, 1 NP, North Carolina | 29 | 11 | CKD/ESKD | Interviews and focus groups | Thematic |
| Schipper et al 184 | 2014 | The Netherlands | 5 H | 30 | Transplanted | Focus groups and interviews | Thematic | |
| Schmid-Mohler et al 85 | 2014 | Switzerland | 1 H, Zurich | 12 | Transplanted | Interviews | Content | |
| Schober et al 206 | 2016 | USA | 14 states | 48 | ESKD | Interviews | Thematic | |
| Seah et al 50 | 2013 | Singapore | 3 H | 9 | ESKD | Interviews | Interpretative phenomenological | |
| Shahgholian et al 142 | 2015 | Iran | 1 H, Isfahan | 17 | ESKD | Interviews | Colaizzi’s method | |
| Shaw et al 275 | 2015 | New Zealand | Diverse | 24 | ESKD | Interviews | Phenomenological | |
| Sheu et al 245 | 2012 | USA | Maryland | 27 | 23 | ESKD | Focus groups | Thematic |
| Shih et al 59 | 2011 | New Zealand | 1 C, North | 7 | ESKD | Interviews | Hermeneutical and thematic | |
| Shirazian et al 123 | 2016 | USA | 1 C, Northeast | 23 | CKD | Focus groups | Thematic | |
| Sieverdes et al 174 | 2015 | USA | 1 C, South Carolina | 27 | Transplanted | Focus groups | Thematic | |
| Smith et al 207 | 2010 | USA | 2 C | 19 | ESKD | Focus groups | Content | |
| Spiers et al 177 | 2015 | UK | 1 C, London | 4 | Transplanted | Interviews | Interpretative phenomenological | |
| Spiers et al 171 | 2016 | UK | 2 online groups | 10 | ESKD | Interviews | Thematic | |
| Stanfill et al 178 | 2012 | USA | 1 C, mid-South | 7 | Transplanted | Focus groups | Iterative | |
| Stewart et al 81 | 2012 | USA | 2 C, urban | 19 | ESKD | Interviews | Coding | |
| Tanyi et al 201 | 2006 | USA | Mid-West | 16 | ESKD | Interviews | Colaizzi’s method | |
| Tanyi et al 192 | 2008 | USA | 2 C, mid-West | 16 | ESKD | Interviews | Colaizzi’s method | |
| Tanyi et al 193 | 2008 | USA | Mid-West | 16 | ESKD | Interviews | Colaizzi’s method | |
| Tavares et al 216 | 2016 | Brazil | 1 H, Rio de Janeiro | 19 | ESKD | Interviews and groups | Content | |
| Taylor et al 111 | 2016 | Australia | 2 H, Sydney | 26 | ESKD | Interviews | Thematic | |
| Taylor et al 215 | 2015 | UK | 6 trusts | 15 | 11 | ESKD | Interviews | Constant comparison |
| Theofilou et al 122 | 2013 | Greece | 1 H, Athens | 10 | ESKD | Interviews | Phenomenological | |
| Thomé et al 247 | 2011 | Brazil | 1H, Rio Grande do Sul | 10 | ESKD | Interviews | Cultural | |
| Tielen et al 179 | 2011 | The Netherlands | 1 C | 26 | Transplanted | Interviews | Q methodology | |
| Tijerina et al 76 | 2006 | USA | 8 C, Texas | 26 | ESKD | Interviews | Coding | |
| Tong et al 63 | 2009 | Australia | 4 H, Brisbane, Sydney, Melbourne | 63 | CKD/ESKD | Focus groups | Thematic | |
| Tong et al 152 | 2013 | Italy | 4 C, Bari, Marsala, Nissoria, Taranto | 22 | 20 | ESKD | Interviews | Thematic |
| Tong et al 237 | 2015 | Australia | 1 C, Adelaide | 15 | CKD/ESKD | Interviews | Thematic | |
| Tonkin-Crine et al 127 | 2015 | UK | 9 C | 42 | ESKD | Interviews | Thematic | |
| Torchi et al 153 | 2014 | Brazil | 1 C, Rio de Janeiro | 10 | ESKD | Interviews | Collective subject technique | |
| Tovazzi et al 117 | 2012 | Italy | North | 12 | ESKD | Interviews | Phenomenological | |
| Tweed et al 109 | 2005 | UK | 1 C, Leicester | 9 | ESKD | Interviews | Phenomenological | |
| Urstad et al 242 | 2012 | Norway | 1 C | 15 | Transplanted | Interviews | Hermeneutic | |
| Valsaraj et al 60 | 2014 | India | 1 H, South Karnataka | 10 | ESKD | Interviews | Phenomenological | |
| Velez et al 100 | 2006 | Spain | 1 C | 12 | ESKD | Interviews | Thematic | |
| Vestman et al 263 | 2014 | Sweden | 1 H | 9 | ESKD | Written narratives | Thematic | |
| Visser et al 276 | 2009 | The Netherlands | 1 C | 14 | ESKD | Interviews | Thematic | |
| Wachterman et al 172 | 2015 | USA | 1 C | 16 | ESKD | Interviews | Thematic | |
| Walker et al 124 | 2012 | UK | 1 H | 9 | CKD | Interviews | Thematic | |
| Walker et al 51 | 2016 | New Zealand | 3 C | 43 | 9 | ESKD | Interviews | Thematic |
| Walker et al 61 | 2016 | New Zealand | 3 C | 43 | 9 | ESKD | Interviews | Thematic |
| Walker et al 80 | 2017 | New Zealand | 3 C | 13 | ESKD | Interviews | Thematic | |
| Walton et al 258 | 2002 | USA | 1 H, rural, Northwest | 11 | ESKD | Interviews | Grounded theory | |
| Walton257 | 2007 | USA | 1 C | 21 | ESKD | Interviews | Grounded theory | |
| Weil253 | 2000 | USA | 2 C, rural, Northwest | 14 | ESKD | Interviews | Thematic | |
| Wells254 | 2015 | USA | 3 C, 1 NP, Texas | 17 | 17 | ESKD | Interviews | Thematic |
| Wells62 | 2015 | USA | 3 C, 1 NP, Texas | 15 | 21 | ESKD | Interviews | Thematic |
| White et al 139 | 2004 | USA | 1 C, Colorado | 6 | 9 | ESKD | Interviews | Thematic |
| Wiederhold et al 185 | 2012 | Germany | 1 C | 10 | Transplanted | Interviews | Content | |
| Wilkinson et al 75 | 2011 | UK | Luton, West London, Leicester | 48 | ESKD | Interviews | Thematic | |
| Wilkinson et al 233 | 2014 | UK | 4 C | 16 | 45 | Transplanted | Interviews and focus groups | Thematic |
| Wilkinson et al 74 | 2016 | UK | 4 C | 16 | 45 | ESKD | Interviews and focus groups | Thematic |
| Williams et al 101 | 2009 | Australia | 2 H | 20 | CKD | Interviews | Qualitative | |
| Williams et al 102 | 2008 | Australia | 2 H, Melbourne | 23 | CKD | Interviews and focus groups | Interpretative | |
| Williams et al 261 | 2009 | Australia | 1 H, Melbourne | 23 | CKD | Interviews | Qualitative | |
| Wilson et al 255 | 2015 | UK | 3 C | 15 | 15 | ESKD | Focus groups | Thematic |
| Winterbottom et al 230 | 2012 | UK | 1 C, Northern England | 20 | CKD | Interviews | Thematic | |
| Wu et al 66 | 2015 | Taiwan | 2 C, Central | 15 | ESKD | Interviews | Thematic | |
| Xi et al 110 | 2011 | Canada | 1 C, Ontario | 13 | ESKD | Interviews | Thematic | |
| Xi et al 158 | 2013 | Canada | 1 C, Ontario | 10 | ESKD | Interviews | Thematic | |
| Yeun et al 143 | 2016 | South Korea | 1 H, Seoul | 33 | ESKD | Interviews | Q methodology | |
| Yngman-Uhlin et al 135 | 2010 | Sweden | Southeast | 14 | ESKD | Interviews | Phenomenological | |
| Yngman-Uhlin et al 132 | 2016 | Sweden | 1 H, Southeast | 8 | ESKD | Interviews | Content | |
| Yodchai et al 249 | 2016 | Thailand | 2 H, Songkhla | 20 | ESKD | Interviews | Qualitative | |
| Yodchai et al 199 | 2012 | Thailand | 1 C, South | 5 | ESKD | Interviews | Grounded theory | |
| Yu et al 112 | 2014 | Singapore | NKF | 32 | ESKD | Interviews | Thematic | |
| Yumang et al 144 | 2009 | Canada | 1 H, Quebec | 9 | ESKD | Interviews | Colaizzi’s method | |
| Ziegert et al 213 | 2001 | Sweden | 12 | ESKD | Interviews | Pragmatic approach | ||
| Ziegert et al 211 | 2006 | Sweden | Southwest | 13 | ESKD | Interviews | Content | |
| Ziegert et al 212 | 2009 | Sweden | Southwest | 20 | ESKD | Interviews | Content |
*Includes healthcare staff.
C, centre, unit or clinic; CKD, chronic kidney disease; D, dialysis; ESKD, end-stage kidney disease; GP, general practice; H, hospital; HD, haemodialysis; NA, not available; NKF, National Kidney Foundation (Singapore); NP, nephrology practice; PD, peritoneal dialysis.
Patient and public involvement
Patients and/or public were not involved in the development of the research question. To ensure wide dissemination of this systematic review, it is published in peer-reviewed open-access journal and presented in research meetings.
Results
Combined searches yielded 5407 citations and resulted in 260 studies from 30 countries included in the final analysis. A total of 5115 patients and 1071 carers were included. Countries most frequently represented in the studies were: the USA with 52 (20%), the UK with 46 (18%), Brazil with 28 (11%), Australia with 25 (10%), Canada with 20 (8%), Sweden with 19 (7%), New Zealand with 8 (3%) and Iran with 7 (3%) studies. Most studies (n=193, 74%) described the experiences of patients with ESKD, in dialysis or conservative treatment, 28 (11%) studies reported on transplanted patients, 17 (6%) studies referred to patients with CKD stages 1–4 and the remainder studies described experiences of patients with CKD in all stages. Table 2 shows characteristics of studies included in the review, box 1 shows illustrative quotations, table 3 shows summary of results and table 4 shows main challenges related to BoT.
Box 1. Illustrative quotations.
Structural inequalities
(Undocumented immigrant in US without access to scheduled haemodialysis) When you enter through the emergency department, you arrive in bad shape…you need to have a high potassium or they send you home even though you feel you are dying. Sometimes, you crawl out when they decide to not do dialysis. You eat a banana because it is high in potassium even though you may die and you go back and wait and hope that they will do dialysis so that you don’t feel like you are drowning and so that the anxiety goes away (American patient).52
My mother got some help from DIF (Mexican social assistance office), it was five haemodialysis sessions; when there was no session left, we went to a private centre, there is a foundation there and they helped us… they gave me eight sessions. After that, my mom went to DIF in Zapopan again and they sent us to DIF in Guadalajara. We got some help there (Mexican patient without coverage).47
Workload
Sometimes I have to sit and wait at least an hour and I have to call and say my ride is not here yet, which makes me late getting there, which makes me late getting on the machine, which makes me late getting off the machine. And then… coming to pick you up, if you’re not ready when they get there, they will leave you and you’ll have to sit and wait and wait and wait (American patient).86
It is always in the back of your mind that it (the transplant) will fail, at times. And I think if anything that makes you more inclined to comply with your treatment, comply with your medication because at the end of the day if, you know, if you do the utmost that you can and you take your medicine and you go to your follow up appointments, then there’s hopefully less chance of it failing in the long run (woman, 3 years+post-transplant).175
I suppose mine being genetic. It’s been very difficult to find what kind of diet you’re supposed to follow. You read one bit of information and it tells you this and you read another bit and it tells you don’t eat that, which the other one said you must eat. there’s no clear guideline on what it is you can or can’t eat (man, 38 years, CKD stage 3).94
It was a lot more work because of all the things that you had to learn… I don’t eat out anymore… It’s tough taking so many pills (patient with CKD).92
Capacity
Before she left (pause) when everything was happy and happy sort of thing, you know, I think it was—she was going to give a kidney to somebody else and somebody else was going to give a kidney to somebody and somebody was going to give a kidney to me—like a triangle… she was willing to do that. It didn’t happen, um (pause) ‘cos she left (UK patient).39
it’s a kind of tiredness that you wouldn’t wish on your worst enemy… when you can’t read, you’re too tired to watch the telly, you’re too tired to do anything, because your brain is so tired like all of you… it feels like you’re kind of hollow inside… like it’s only a kind of shell that’s functioning.137
Well about five years ago, I went to the hospital because I wasn’t feeling good and they took my blood pressure and it was 200 over something…Then while they were trying to get my blood pressure down, they said something about my kidneys. And I didn’t know the connection between high blood pressure and kidneys (Evan, African-American male, 50, CKD stage 3).35
It wasn’t till about 2 years ago, until I fully understood and I’ve had the kidney disease from the age of 15, what exactly my (kidney) function was and I got a fright. No one had ever told me (man, 38 years, CKD stage 3).94
Control and decision-making
I have free rein of whatever days I want to take off. They don’t tell me when I have to dialyse or when I can’t dialyse. Everything is under my control. That’s what I like (talking on home dialysis, patient from Canada).158
If I’m going to feel this bad for the rest of my life, do I just want to end it now? (woman, 40s, CKD stage 4).63
Carers’ involvement
I just sit here like a robot. Nurses asked me to buy items that my mother needed. They never told me why she needed them. They ordered me to pay for dialysis, laboratory investigations and other things. I don’t like it when I do not know the reason behind my actions. I am sad to see myself as a fool being tossed around (caregiver from Nigeria).65
End of life
Then (the home care nurse) said ‘Well you haven’t got to go on. We’ll make it quite peaceful for you to pass on'. They can tell you, but it’s your body. It’s up to me to decide what I want to do (patient from the UK).205
I have heard (about) a lot of people that died on dialysis and had strokes on dialysis… Once I sit down there, I don’t know whether I’m gonna come out alive or dead (Berta, aged 45 years, blind amputee, dialysis patient for 18 months).76
I think about (death) everyday. I mean you can’t help it. I know that it is a terminal illness and it’s not going to get better and that there is only one way out (wife of a Canadian patient on peritoneal dialysis).286
CKD, chronic kidney disease.
Table 3.
Summary of results
| Qualitative analysis | ||
| Primary category | Secondary category | Summary results |
| Structural disadvantage | Access to care | Socioeconomic status is central to experience of CKD.35 37–63 125
Treatment costs were major obstacle to care47–49 64 125 as was limited access to healthcare for the uninsured or underinsured.35 40 48 50 52 60 67 68 Transplants, dialysis and drug treatments were often beyond the reach of low-income patients.35 47–49 66 83–85 125 Uninsured or underinsured people experienced increased dependence on emergency care.35 47–49 52 66 Poorly funded or unfunded healthcare was often fragmented and of indeterminate duration.47 48 64 For non-native speakers, language was an important barrier for having a discussion with care providers.53 74–76 Patients were often poorly informed about disease progression and treatment options.38 50 57 58 63 64 125 127–129 188 205 219–222 |
| Housing | Homelessness, unsuitable housing, lack of utilities (electricity, clean running water) are critical to self-care and home dialysis.51 61 70 86 | |
| Employment status | Loss of employment may lead to uninsurance or underinsurance that limits or prevents access to treatment.35 39 45 52 60 69 72 87–91 | |
| Workload | Self-care | Complex medication regimens were managed through dispensing aids, associated activities, family support.40 46 71 86 92–103
When taking care of their vascular access, patients made efforts to protect the arm.108 111 Patients controlled their diets and fluid intake, and managed food cravings and thirst.63 112 Many modified social activities to minimise exposure to hot weather, temptation and social pressure.112 118–120 Women could face family conflicts if they followed prescribed diets.45 62 121–124 Restrictive diets were sometimes stigmatised as a sign of poverty.121 |
| Navigating healthcare structures | When pathways in system were not established, patients and carers had to identify institutions to obtain treatment and laboratory results.48 49 125 161
In settings with healthcare coverage, socioeconomically disadvantaged patients found it difficult to access financial support.51 Lack of continuity of care contributed to patients using services without sufficient expertise in CKD.49 101 The efficiency focus of medical system was perceived as a barrier to a personal connection.102 173 |
|
| Negotiating costs and fund-raising | Fund-raising was important for those who were uninsured or underinsured, sold goods or services, organised raffles or obtained loans.47–49 125
Patients contacted centres, other patients and organisations to ask for free treatment when they were uninsured or underinsured.47 49 52 125 217 218 |
|
| Travel and time management | Patients often travelled for long distances to dialysis centres, three times a week.15 47–49 53 76 86 126–133
Home dialysis patients had to pay transport to training, appointments and other check-ups.53 61 69–72 Patients arranged daily activities between sessions, adjusted activities to their fatigue and tried to schedule medical appointments all on one day.55 134–145 Parents arranged child care while they were in sessions or when they were tired.49 53 55 154 155 |
|
| Home dialysis | Training was required with extended periods off work.61 70 156–158
Homes needed physical adaptation, carers invested efforts in maintaining cleanliness and hygiene.152 158–162 Specific tasks were managing treatment at set times, recording blood pressure and body weight, titrating medications, adopting aseptic techniques.156 157 163 |
|
| Pretransplant adaptation | Patients adjusted to being on transplant waiting-list, prepared for transplant from a deceased donor at any time.43 115 133 164–170
Specific adjustment tasks included: hospital visits, tests and organising payment for treatment.132 133 164 165 170–173 Some people needed to negotiate donation of a kidney by living relatives or others.39 47 164 174 |
|
| Post-transplant adjustment | Transplanted patients managed complex medication regimens, balanced against the need to re-enter the labour market to pay off loans.84 85 175–180
Post-transplant, patients needed to manage relationships, finances and family responsibilities in context of prognostic uncertainty.83 85 175–177 181–186 |
|
| Capacity | Physical and mental capacity | Daily activities were limited by symptoms associated with dialysis (pain, fatigue, anxiety and depression).37 44 55 63 90 96 138 140 154 187–199
Symptoms were sometimes overlooked by healthcare professionals.58 94 101 202–204 When in poor health, patients relied on wider networks for food preparation, transportation, shopping, ordering supplies, symptom management and training.37 118 161 205–208 Carers were involved in the treatment, accompanying patients to dialysis and responding to psychosocial needs.45 69 97 129 141 143 161 210–215 |
| Managing information | Information on disease and treatment was often insufficient or difficult to comprehend, particularly during early stages.61 77 92 109 121 130 131 223–227
Short clinic visits, jargon and anxiety were barriers to accessing information.61 102 223 231–234 For organ donation and transplantation, patients relied on information from other patients, healthcare professionals, social workers, financial representatives, meetings and the internet.117 174 235–238 Information about the effects and side effects of immunosuppression was important but hard to come by.178 184 185 239–242 Stress and urgency affected how people with CKD processed information provided by healthcare professionals.240 242–245 |
|
| Social support | Support from friends, family, neighbours, healthcare professionals and other patients was essential.39 44 60 62 215 247 252–256
Lack of social support was a frequently reported problem.44 60 247 259 Patients ought to maintain a sense of normalcy, integrating dialysis community into their network.42 139 210 260 Younger patients sometimes considered home dialysis as an opportunity for employment and contact with social networks.61 152 |
|
| Experienced control | Personal control and decision-making | When clinicians failed to discuss care, eligibility for transplant and potential donors, patients felt disempowered.39 55 57 58 77 78 169 282
When relatives offered to donate a kidney, many patients were reluctant to accept because of concerns on future health of donor; other patients had reservations about kidneys from deceased donors because of the donor’s age, medical history.172 181 235 Once transplanted, main clinical objective was preserving the graft.49 63 89 96 167 283–285 |
| Carers’ involvement | Carers needed more information on dialysis techniques to feel confident, stressed the importance of 24 hours telephone support, wanted to be involved in decision-making as dialysis would also affect them.55 70 111 156–158 223 279 286
When carers perceived patient was in pain with no response to treatment, they sometimes yearned for the patient’s freedom of this condition through a peaceful death.134 141 161 |
|
| End-of-life decisions | Patients and carers emphasised self-determination, autonomy and dignity.134 136 205 251 294
End-of-life decisions were influenced by ideas about personal fulfilment, nature taking its course, fears of dependence or of dialysis accelerating death.128 293 Decisions often passed to trusted carers or professionals.290–292 Acceptance of decisions was influenced by treatment modality, patient age and ineffectiveness of haemodialysis.64 128 134 161 Families emphasised importance of respecting patients’ wishes.202 233 292 |
|
CKD, chronic kidney disease.
Table 4.
Main challenges related to burden of treatment
| Challenge | Group of patient mostly affected | Type of country mostly affected | Severity |
| Limited access to healthcare for the uninsured or underinsured. | CKD, ESKD | LMIC | +++ |
| Dialysis, transplant surgery, immunosuppressive drugs were often beyond the reach of low-income patients. | ESKD | LMIC | +++ |
| Healthcare was often fragmented and of indeterminate duration for the uninsured or underinsured. | CKD, ESKD | LMIC | +++ |
| In settings with healthcare coverage, socially disadvantaged patients found it difficult to access financial support. | CKD, ESKD | HIC | ++ |
| Fund-raising was important for those who were uninsured or underinsured. | ESKD | LMIC | +++ |
| For non-native speakers, language was an important barrier for having a discussion with care providers. | CKD, ESKD | LMIC, HIC | ++ |
| Patients were often poorly informed about disease progression and treatment options. | CKD, ESKD | LMIC, HIC | ++ |
| Patients and carers had to identify institutions to obtain diagnosis, laboratory results and treatment. | CKD, ESKD | LMIC | ++ |
| Homelessness, unsuitable housing, lack of utilities, critical to self-care and home dialysis. | ESKD | HIC, LMIC | ++ |
| Loss of employment may lead to uninsurance or underinsurance limiting or preventing access to treatment. | ESKD | HIC, LMIC | +++ |
| Complex medication regimens were managed through dispensing aids, associated activities, family support. | CKD, ESKD | HIC, LMIC | + |
| When taking care of their vascular access, patients made efforts to protect the arm. | ESKD | HIC, LMIC | + |
| Patients controlled diets and fluid intake, modified social activities to minimise exposure and pressure. | CKD, ESKD | HIC, LMIC | ++ |
| Patients often travelled for long distances to dialysis centres, three times a week. | ESKD | HIC, LMIC | ++ |
| Home dialysis patients had to pay transport to training, appointments and other check-ups. | ESKD | HIC, LMIC | ++ |
| Patients arranged daily activities between sessions. | ESKD | HIC, LMIC | + |
| For home dialysis, training was required with extended periods off work. | ESKD | HIC, LMIC | + |
| For home dialysis, homes needed physical adaptation. | ESKD | HIC, LMIC | + |
| For home dialysis, tasks were managing treatment, monitoring, titrating medications, adopting aseptic techniques. | ESKD | HIC, LMIC | ++ |
| Pretransplantation, specific adjustment tasks included: hospital visits, tests and organising payment for treatment. | ESKD | HIC, LMIC | |
| Some people needed to negotiate donation of a kidney by living relatives or others. | ESKD | HIC, LMIC | ++ |
| Transplanted patients managed complex medication regimens. | ESKD | HIC, LMIC | + |
| Transplanted patients needed to manage relationships, finances and family responsibilities. | ESKD | HIC, LMIC | ++ |
| Symptoms associated with dialysis limited daily activities, sometimes overlooked by healthcare professionals. | ESKD | HIC, LMIC | ++ |
| When in poor health, wider networks were necessary for daily activities, transportation, symptom management. | ESKD | HIC, LMIC | ++ |
| Information on disease and treatment was often insufficient or difficult to comprehend. | ESKD | HIC, LMIC | ++ |
| Information about immunosuppression was hard to obtain. | ESKD | HIC, LMIC | ++ |
| Lack of social support was a frequently reported problem. | ESKD | HIC, LMIC | ++ |
| Many clinicians failed to discuss care, eligibility for transplant and potential donors. | CKD, ESKD | HIC, LMIC | ++ |
| Carers needed more information on dialysis techniques to feel confident. | ESKD | HIC | + |
| Patients and carers emphasised self-determination, autonomy and dignity when nearing end of life. | ESKD | HIC | ++ |
Severity: + mild, ++ moderate, +++ very severe.
CKD, chronic kidney disease; ESKD, end-stage kidney disease; HIC, high-income country; LMIC, low-income and middle-income country.
Structural inequalities
Access to care
Poverty and other socioeconomic disadvantages such as unemployment or poor housing conditions were defining factors for lack of treatment or interrupted care.37–52 Living as a person with CKD and ESKD always implied some degree of financial burden, from having to pay for the whole dialysis treatment or transplantation surgery to out-of-pocket payments of incidentals, even in countries with universal coverage.35 47–49 51 53–63 Poorly funded or unfunded healthcare resulted in fragmented treatment across healthcare systems.47 48 64 Although patients who had difficulties affording treatment were naturally more concerned with accessing healthcare than in improving services, they recognised fragmentation and lack of integration as important problems.40 45 48–51 Where government or private insurance coverage of ESKD treatment was limited, for example, Mexico or India, patients paid for some or all the following: vascular access, hospitalisation, medical visits, haemodialysis sessions, medication, tests, prescribed food, transport and meals.45 47–50 60 65 In such settings, patients received dialysis treatment only if they could afford it or when they had access to free sessions.45 47–50 60 65 Medication was sometimes counterfeit, obtained on the black market, as legitimate medication was beyond patients’ reach.49 For the uninsured, dependence on emergency care added uncertainty and risk, whatever their treatment modality, as in the case of many undocumented and uninsured immigrants in the USA.35 47–49 52 66 In countries with poor healthcare infrastructure, patients reported shortage of public specialised hospitals, long delays to undergo examinations, limited number of haemodialysis machines available, lack of ward space or poor bed conditions in hospitals, for example, poor hygiene, worn-out mattresses, shortage of linen; to avoid delays, patients sometimes had tests performed by private providers.40 50 60 67 68
When home dialysis was available, patients had to pay for transport to training, appointments and other check-ups; moreover, some equipment, supplies, increased utility bills and home modifications represented unexpected expenses.51 53 61 69–73 In countries with coverage of RRT, for patients whose first language was different from that where treatment was received, as in the case of migrants, communication was a barrier for discussions with healthcare professionals; family members and neighbours acted as translators at appointments.53 74–76 Where language was shared, communications between clinicians and patients of different ethnic origins—for example, Australian Aborigines and New Zealand Maoris—was often itself a source of conflict and disadvantage, because of prejudice.53 57–59 77–82
In some countries, the transplantation procedure could be particularly expensive, even at public hospitals.35 47–49 66 83 Moreover, patients sometimes found that the expensive immunosuppressants necessary after the transplant were not covered by their insurance; other patients who obtained information about the high costs of immunosuppressants and realising that they could not afford them, were forced to continue with dialysis until it failed.49 83–85 In Mexico, structural constraints resulted in transplanted patients being sent back to small peripheral clinics with no transplantation expertise, increasing the risk of iatrogenic or poorly managed complications.83
Housing conditions
Unsuitable housing was a barrier to home dialysis if it could not accommodate equipment, and was impossible without an adequate electricity supply.51 61 In rented accommodation, landlords might not approve of necessary modifications. Home dialysis was not a treatment option for those with no fixed abode.51 61 70 86
Employment status
Patients who were physically able to continue working often had informal or temporary jobs, with diminished income; others were forced into unemployment, leading to new financial problems.39 45 52 60 69 72 87–91 Unemployed patients in the USA were covered by government or state schemes; however, this coverage either diminished or ceased if they found work with a new insurance.35 52
Patient workload
Self-care
People with CKD and ESKD had complex medication regimens managed through dispensing aids, daily activities associated with medication taking such as meals, family support or a combination of these.40 46 71 86 92–106 Anticipating dialysis, patients underwent vascular access, a way to reach the blood for haemodialysis, undergoing minor surgery and care needed to be taken to prevent infections or clotting.66 107–110 To care for their vascular access, patients kept the access area clean, changed bandages, restricted themselves from lifting heavy objects and were alert for pain or hardness in the area.108 111
Patients controlled their diets and fluid intake between dialysis sessions, and managed food cravings and thirst with strategies such as thinking of the potential detrimental consequences of drinking water, avoiding thoughts and behaviours that could trigger thirst and modifying social activities to minimise exposure to hot weather, social pressure and temptation to intake certain foods or fluids.46 63 112–120 Women also faced potential family conflicts if they followed prescribed diets.45 62 121–124 In certain cultures, including immigrants who preserved their customs in other countries, the perceived association of a rich diet and wealth acted as a barrier to adherence to a restrictive diet, essential to self-care, as patients feared being stigmatised as poor.62 121 125
Travel and time management
People with ESKD travelled to haemodialysis centres three times a week, received treatment for several hours and then transported themselves home again; very often, transportation represented a problem for patients because of pick-up delays, long distances or high costs.15 47–49 53 76 86 126–133 Patients receiving dialysis arranged their daily activities between treatment sessions, adjusted the timing and intensity of their activities to their fatigue and tried to schedule medical appointments all on one day to avoid further interactions with the healthcare system.55 134–145 The treatment was seen by most patients as an emotional and time imposition that caused boredom and frustration.63 146–152 Time was often spent waiting for visits, prescriptions and tests.55 134–145 153 Parents also arranged child care while they were in sessions, or had to travel for treatment.49 53 55 154 155
Home dialysis
For patients receiving home dialysis, training was required which necessitated extended periods of leave from work.61 70 156–158 They and their families had to adapt their home to accommodate equipment and materials, and spent more time cleaning in case healthcare workers assessed their housing conditions.152 158–162 Tasks associated included managing treatment at set times each day, recording blood pressure and body weight, titrating medications and adopting aseptic techniques, as well as adhering to diet and fluid restrictions.156 157 163 In the case of developing peritonitis, workload increased as antibiotics had to be reconstituted and injected.156 157
Pretransplantation adaptation
People with ESKD adjusted to being on the transplant waiting list and prepared for the possibility of receiving a kidney from a deceased donor at any time.43 115 133 164–170 The tasks included hospital visits, several investigations and tests, saving money for the operation and maintaining robust health; many potential recipients felt overwhelmed by all that was necessary.132 133 164 165 170–173 Talking to others about their requirement for a kidney transplant involved making the request itself to potential living donors, educating people about CKD, treatment options and donation.39 47 164 174
Post-transplantation adjustment
After transplantation, patients’ workload included financial and occupational changes resulting from a new type of treatment and status, managing complex medication regimens and managing social relations.84 85 175–180 These tasks had to be balanced against the work of safeguarding access to healthcare, organising their disability insurance, interacting with healthcare providers, managing symptoms, monitoring medication side effects and managing self-care in relation to diet, fluid and physical activity.84 85 175–180 Although transplantation was seen as a route back to normality, it was laden with ambiguous feelings towards the donor, unanticipated challenges in forming or maintaining relationships, financial worries, the responsibility of supporting their family, disappointments when side effects were noticed and a prevailing prognostic uncertainty.83 85 175–177 181–186
Navigating healthcare structures
Very often, patients had to identify and call on the appropriate institutions to obtain a diagnosis, laboratory exams, treatment or coverage; contacting several public and private healthcare providers, social insurance offices, charity organisations and non-governmental organisations.48 49 125 161 In settings with coverage of RRT, socioeconomically disadvantaged patients could also find it difficult to access financial support and navigate the social support system, which resulted in not receiving the assistance to which they were entitled.51 Lack of continuity of care contributed to patients using services without sufficient expertise in CKD or ESKD, such as emergency departments or peripheral health centres.49 101 The efficiency focus of the medical system was perceived by patients and professionals as a barrier to a personal connection; moreover, patients also recognised professionals’ dismissive attitudes towards patients’ experiential knowledge.102 173
Negotiating costs and fund-raising
Those patients and carers in countries with limited health coverage needed to perform additional work; poor families sold goods, products or services, organised raffles to collect money or obtained loans.47–49 125 They also contacted treatment centres, other patients, hospitals and non-government organisations to ask for free dialysis sessions or medication. For this reason, disadvantaged people were advised by healthcare staff on how to seek help in charities and advocacy organisations.47 In more affluent settings, patients also struggled to negotiate coverage of extra expenses, such as those related to home dialysis or conservative management.51 161
Capacity
Physical and mental capacity
The ability of people with ESKD to carry out daily activities, including their paid job, was limited by symptoms associated with the disease and dialysis treatment, such as pain, fatigue, anxiety, depression and sexual problems,37 44 55 63 90 96 138 140 154 187–201 sometimes overlooked by healthcare professionals.58 94 101 202–204 When in poor physical health, patients relied on wider family networks and neighbours to help with activities related to BoT such as scheduling and attending medical appointments, arranging transportation to those appointments, ordering and arranging medical supplies and training; also, other daily tasks such as food preparation, or shopping.37 118 161 205–209 Carers were involved in the dialysis procedure, accompanying patients to dialysis and responding to psychosocial needs.45 69 97 129 141 143 161 210–216 Patients’ capacity to carry out the activities related to healthcare were affected by insufficient financial resources and the fear of catastrophic consequences, such as death because of lack of dialysis treatment or immunosuppressive medication in the case of transplanted patients.47 49 52 217 218
Managing information
Obtaining information on the disease and treatment was a significant burden for patients and carers. Patients reported that their information on the disease and treatment options was often insufficient or difficult to comprehend, particularly during the early stages of their trajectory, independent of income or coverage level.38 50 57 58 61 63 64 77 92 109 121 125 127–131 188 205 219–230 Patients may not have asked for clarification for fear of not understanding or because they did not even know what to ask; the desire for more patient-centred care were widely expressed. Short clinic visits, unknown technical jargon and high levels of anxiety were barriers to accessing information.61 102 223 231–234 Other patients could sometimes supply information about dialysis options, travelling, hygiene regimens, dietary restrictions, benefit advice, timing of treatment and pain management.117 174 235–238 For organ donation and transplantation, people usually received information through discussions with other patients, providers, social workers, financial representatives, the internet and, in affluent populations, informative meetings.117 174 235–238 In relation to transplantation, patients reported they needed practical information about the unexpected side effects of immunosuppressive medication; most frequently mentioned were higher risk of cancer, infections, weight gain and fragile skin.178 184 185 239–242 Other information needs for transplanted patients included coping with emotions related to the transplant, what to do when a suitable organ became available, alternatives to transplantation and how the waiting list worked.240 242–245 Family members were afraid to bother the healthcare team,246 and perceiving little power in comparison to healthcare professionals, downplayed their knowledge in front of them.210 Patients and carers were responsible for obtaining and carrying their medical files and test results to appointments when the healthcare administrative systems were not integrated.49 125 Some had anticipated that transplantation would offer dramatic health improvement but were disappointed when they experienced side effects, particularly cancer.44 63 101 106 122 167 190 193 199 206 214 247–251
Social support
Most people highlighted the support from family, neighbours, friends, staff, other patients and church communities; friends, staff and spiritual groups were particularly important for those living alone.39 44 60 62 215 247 249 252–258 A lack of social support was also frequently reported.44 60 247 259 In a UK study, patients' socioeconomic disadvantage adversely affected the availability of social support, and it was suggested that personal relationships sometimes broke down when potential donors declined to donate.39 Attending dialysis was sometimes seen as a social outlet, where they could make friends with staff and patients. Younger participants often considered the schedule flexibility of home dialysis as an opportunity for maintaining their employment and contact with their family and established social networks.61 152 To demonstrate resilience, some patients tried to maintain a sense of normalcy, integrating the dialysis community into their social network.42 139 210 260
Experienced control
Personal control
Feelings of personal control were achieved through learning how to manage CKD and ESKD, finding a balance between illness and normalcy, or even denying the seriousness of their condition.218 260 261 The experience of feelings of personal control led to increased self-confidence and well-being.15 189 251 Strategies for maintaining control included requesting tests, withholding information from clinicians, monitoring and modifying their treatments and checking the activities of dialysis nurses assisting them.139 246 251 262–265 People with ESKD experimented with their therapy to determine if the prescriptions were really necessary, they also shortened dialysis hours to reduce worsening symptoms, to meet work commitments, or to participate in an unexpected social situation.54 55 Lengthening treatment hours could facilitate higher than usual fluid removal or managing symptoms.54 55 Some patients entrusted decisions entirely to the care team, and this promoted feelings of security.61 70 102 107 266 267 The main barrier to personal control was lack of information about treatments, test results and the course of their illness and that they could not choose when and where to travel.15 43 61 63 197 239 268 However, even when patients knew they were not in control, they felt unsafe if the treatment went differently from what was expected.269 Patients recognised prognostic uncertainty, and their own fear of incompetence as an obstacle to choosing the appropriate dialysis modality.54 72 92 132 133 150 161 223 251 268 270–274 For many patients, home dialysis restored a sense of control and freedom to manage their schedule, especially if it was nocturnal.51 70 158 220 263 275 Dependence on emergency care or on fund-raising tasks to cover life-saving treatment represented a severe case of lack of experienced control.35 47–49 52 66
Control and decision-making
Control translated into participation in decision-making, which was affected by the healthcare staff’s attitude towards the patients’ adherence to treatment.236 Lack of choice in decision-making about dialysis modality was very common; when possible, modality was negotiated and agreed after discussions with clinicians and family members, reading educational material or attending informational meetings.202 248 270 273 274 276–278 Home dialysis patients appreciated training to build confidence and skills to use the machine.54 70 111 270 279 280 Patients in dialysis aspired to improve their situation by receiving a transplant, motivating them to adhere to treatment; other motivations included family, especially their children, work and beliefs.55 58 281 People with ESKD whose clinicians failed to discuss care, eligibility and ineligibility for transplant, and potential donors with them felt disempowered.39 55 57 58 77 78 169 282 When relatives offered to donate a kidney, many patients felt reluctant to accept this because of their concerns about the future health of the donor; other patients had reservations about accepting kidneys from deceased donors because of the donor’s age and medical history.172 181 235 Once transplanted, the main clinical objective was preserving the graft. However, the disease and its treatment continued to be a significant burden on patients’ social capital and financial capacity, with unexpected side effects.49 63 89 96 167 283–285
Carers involvement
Relatives wanted to be involved in discussions on dialysis modality as dialysis would take up a large part of their lives.55 70 111 156–158 223 279 286 Carers of patients on home dialysis needed to know more about the dialysis techniques to feel confident about self-managing the treatment, they stressed the importance of 24 hours telephone access for advice.61 69 Family members were afraid to bother the healthcare team,246 and perceiving little power in comparison to healthcare professionals, used strategies to downplay their knowledge of the disease or the treatment in front of them.210 287 To cope with caring, carers sought support in psychiatric help or religion when available, or support in religion.141 247 Patients who decided to stop dialysis did not usually ask for their carers’ opinion; when physicians thought the patient was too ill to decide, carers were consulted and felt death could be liberating if the patient was in pain and with no response to treatment.134 141 161
End-of-life decisions
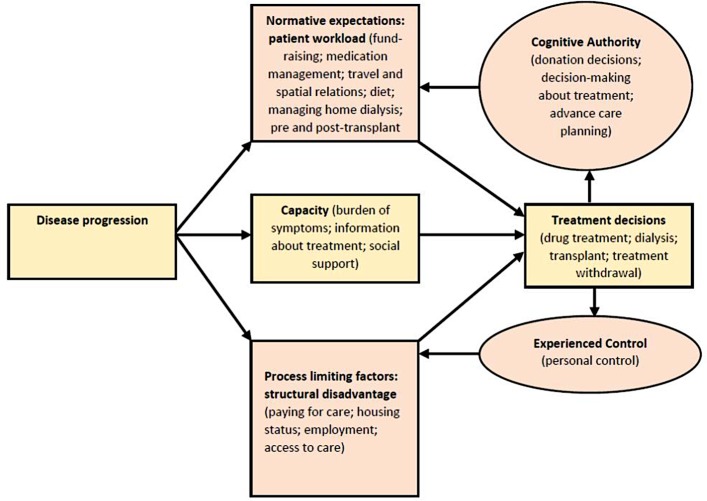
Some patients felt that advance care planning (ACP) was hard and unnecessary as they trusted their families to make decisions; others were less concerned, trusted their healthcare team and felt empowered.236 288 289 Family members felt ACP was necessary as a means to protect patients.290–292 At the end of life, maintaining control was a struggle with respect to autonomy and dignity.134 136 205 251 Patients based their dialysis withdrawal or non-acceptance decision on having lived a full life, on nature taking its course, on their fear of being a burden for their families, their bodies being invaded and dialysis accelerating death.128 293 For some, the decision to withdraw from dialysis meant asserting their self-determination.251 294 Carers’ acceptance of patients’ decision was influenced by the perception of conservative management as a non-invasive treatment, the advanced age of the patient and the lack of benefit received from haemodialysis.64 128 134 161 Although family members were often uncomfortable about making end-of-life decisions, they tended to recognise it was important to respect the patient’s wishes.202 233 292 Figure 2 shows thematic schema of experienced control and cognitive authority in CKD.
Figure 2.
Thematic schema of experienced control and cognitive authority in chronic kidney disease.
Discussion
Our findings demonstrate that the work and capacity of patients and carers are highly unstable situational factors that make up the BoT. Capacity is particularly diminished by socioeconomic factors, which ultimately exacerbates the work of patients and their carers; this may occur even in regions with universal health coverage. Particularly in LMICs, patients with ESKD are often underinsured or not at all, which makes it almost impossible for them to attain life-saving treatments. Patients with ESKD can be caught in a vicious cycle, whereby they lose their job and health insurance because of ill health or because they need time off from work to attend dialysis, leading to exacerbations in disease, lack of financial access to treatment and difficulty obtaining a job because of poor health. Patients often fear catastrophic consequences due to a lack of financial capacity, and make strenuous efforts to prevent them. Thematic syntheses with robust methods have covered different aspects of being a patient with CKD.295–308 Here, we focused on three elements of BoT, namely workload, capacity and experienced control, to develop an understanding of the BoT of CKD, focusing on ESKD and including the experiences of patients in contexts of structural inequalities.
Worldwide, many individuals with CKD and especially with ESKD receive no treatment or receive only fragmented care.8 35 309–314 Millions of preventable deaths occur because of lack of access to RRT.9 Moreover, in some LMICs with universal health coverage, resources may be limited because of geography or poor infrastructure; in such cases, the use of free health providers can create delays that compromise the treatment itself, resulting in patients struggling to pay for private providers. When this occurs, healthcare becomes fragmented and uncoordinated. Even in some modern welfare states, health inequalities persist, particularly affecting minorities, those who are unemployed or undocumented.315 One example is the use of emergency haemodialysis by undocumented and uninsured immigrants with ESKD.52 Several studies have highlighted the imperative necessity to address this disturbing reality.316–323
When health systems fail to meet patients’ treatment needs, patients mobilise resources and develop coping strategies such as accepting charity or selling assets.13 29 312 This distressing scenario adds to their workload and very easily overwhelms patients’ capacity. Transportation to and from dialysis centres is a frequent challenge, it is time-consuming, costly or simply not available. Those patients living in non-urban areas in countries where home dialysis is not available have to travel long distances or relocate to access treatment; some may be faced with the decision of leaving their young children in the care of others for long periods of time. In many LMICs, the costs of RRT remain prohibited for both individuals and healthcare systems; dialysis and transplantation costs often lead to financial ruin of the family, discontinuation and death.324 In fact, patients, families and healthcare professionals are burdened with having to choose between life and death.324 On the other hand, in countries with robust health coverage, patients may feel overwhelmed even by having to travel short distances to the treatment centre every 2 days, especially if they do not have support or, if offered home dialysis, they may experience social isolation, unexpected costs and lack of sufficient technical assistance. In settings in which RRT costs are covered, patients may have the choice of not initiating or withdrawing from dialysis.324 Among other factors, advanced age, white ethnicity and chronic disease are associated with dialysis withdrawal.325
Support from social networks, professionals and other patients is critical in improving patient’s capacity. Spirituality and church communities are significant resources for coping with illness and its treatment, as seen in several studies.21 201 249 257 326–329 However, social support is not guaranteed; in some cultures, patients perceive lack of support by their own networks caused by discrimination because of their illness, leading to intolerable levels of BoT.44 60 247 259 It has also been shown that informal care offered by family, friends or neighbours can burden patients through uncomfortable feelings of dependency or the obligation to have an optimistic attitude towards their condition.330 Our findings support this view; patients often fear becoming a burden on their families, which affects their decisions related to treatment options.
We confirmed that patients’ capacity can be undermined by insufficient or inadequate information. Deficits in communication between patients and professionals are endemic and rooted in structural and system factors.20 30 296 308 331 This shortfall affects decisions regarding dialysis modality, medication management and the possibility of using a living donation. Patient discussions with professionals must result in a collaborative partnership and should not simply provide information.330 For example, patients’ concerns and expectations about waitlists, eligibility and allocation for transplantation could be addressed via additional information, clinical conversations and access to specialised psychological therapists.306
Immigrant populations do not always have access to healthcare; when they do, language, cultural and religious differences can act as barriers to care and contribute to the BoT. In high-income countries, the need to provide RRT for migrants and refugees with ESKD will increase as more people are displaced to countries where RRT is available; this situation poses ethical challenges at the societal and individual levels.321 It is necessary to promote and support equitable access to care for those living within any border by means of organisational position statements and focused research.322 For migrants with access to care, culturally competent navigator programmes could contribute to the improvement of healthcare disparities.332
Surprisingly, patients who undergo haemodialysis tend to perceive that staff underestimate their capacities.58 94 101 202–204 When healthcare professionals do not take into consideration patients’ knowledge or values, a diminished participation in self-care and relationally induced non-adherence can occur. Treatment plans should be discussed against an assessment of patient and caregiver capacity, as well as their material, social and cognitive resources.28 333
Changes in treatment may be needed as CKD progresses to its later stages—symptom control may become the main treatment focus.10 11 Our results relate predominantly to the BoT of patients with ESKD, as most reports included in this systematic review have addressed the experiences of this group of patients. Indeed, a large proportion of patients with early stage CKD are unaware of their diagnosis.334 In patients whose kidney function will not decline to a point necessitating RRT, the overall BoT may be related to a reduction of risk.10 11 In the later stages of CKD, symptom control may become the main treatment focus, and the time-consuming and invasive treatment of dialysis, by any modality, and all tasks related to dialysis represent considerable portions of the burden.10 11 Moreover, the BoT is influenced by patients’ financial resources, family support and comorbidities, as well as the healthcare setting. In fact, because of the likely coexistence of multiple conditions, elderly patients experience a greater BoT than do younger patients.24 Management should be coordinated among professionals, particularly for patients with ESKD and multiple morbidities,23 who frequently experience fragmented care with a substantial time and travel burden, as well as contradictory healthcare advice.23
Challenged by constraints, a patient’s sense of control can become fragile. As seen in our review, patients often employ a range of strategies to retain their control, such as withholding clinical information from professionals, asking for additional tests or modifying their treatment. Although a patient’s capacity to cope with BoT is often exceeded, healthcare systems increasingly delegate responsibilities to patients and carers, focusing on self-management and compliance.30 335 When overwhelmed, patients may be forced to renegotiate their responsibilities with actors in the health system and their own social networks.29
Our review has important limitations. The variety of methodologies, quality of reporting and heterogeneity of perspectives make synthesis difficult. Only studies that included face-to-face interviews were included to capture rich qualitative data, and studies that reported methods such as telephone and postal questionnaires or surveys were excluded. Studies with paediatric patients and/or their carers were excluded, as BoT may significantly differ. Although the use of framework analysis can improve the transparency of coding and identify underlying assumptions, it can also be interpreted as a limitation because findings may be influenced by and connected to these theories. For a more global perspective, studies published in other languages could have been included. Grey literature was excluded to manage the scope of the review. We analysed data with a coding framework supported by middle-range theories to understand the work involved in being a person with CKD and how practises are organised and integrated into social contexts. The major strengths of this study are the comprehensive inclusion of publications in the English, Spanish and Portuguese languages to understand the experience of patients in LMICs, which may enhance the transferability of our findings, the broad description of BoT across all stages of CKD and the use of theories to underpin our findings. However, the included studies representing only some LMICs can hardly be presumed to reflect patients’ experiences in these countries.
Conclusion
To the best of our knowledge, this is the first theory-led review that focuses on the structural inequalities that shape patients' and caregivers’ experiences related to BoT in CKD. The inclusion of LMICs extends our understanding of the experiences of individuals living in these countries and the work they undertake to manage their conditions. CKD can result in invasive and exhausting BoT, which is exacerbated in contexts of limited health coverage, socioeconomic disadvantages and marked imbalances in power. An urgent, collaborative, multipronged approach is needed to address the overwhelming BoT of CKD that, in many populations, results in premature death.8 312 However, knowledge gaps persist in resource-limited settings and the nephrology community need to quantify the burden of CKD, understand its social impact, raise awareness of the disease among healthcare workers and advocate for cost-effective and setting-specific detection and prevention strategies.9 324 336 337 The design of innovative policies, interventions and activities are warranted to support and empower patients, considering the constraints and structure of systems that patients navigate in their disease trajectory. This will lead to a better understand of their burden, with the objective of improving quality of care and the illness experience.
Supplementary Material
Acknowledgments
The authors would like to thank the systematic reviews group of the York Health Economics Consortium (YHEC) for developing the original search strategy.
Footnotes
Contributors: JR drafted the paper. AC, MM, CRM and JH screened titles and abstracts in first search round. Full papers were screened by JH, KL, MM, KH and AC. JR performed database searches for update and extension of search. JR, JPA and FC screened updated results. JR, CRM and JPA performed content analysis. CRM, MM, AC and JPA critically reviewed the manuscript for important intellectual content; all authors approved the final version of the paper.
Funding: The first stages of this project (EXPERTS1 Protocol, search strategy and meta review) were partially funded by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care (NIHR CLAHRC) Wessex, which is a partnership between Wessex NHS organisations and partners and the University of Southampton.
Disclaimer: The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. Funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: EXPERTS1 Protocol is published in BMJ Open, with open access CRM, Masters J, Welch L, Hunt K, Pope C, Myall M, Griffiths P, Roderick P, Glanville J, Richardson A: EXPERTS1—experiences of long-term life-limiting conditions among patients and carers: protocol for a qualitative meta-synthesis and conceptual modelling study. BMJ Open 2015, 5(4):e007372. Meta-review of systematic reviews is published in BMJ Open, with open access CRM, Cummings A, Myall M, Harvey J, Pope C, Griffiths P, Roderick P, Arber M, Boehmer K, Mair FS et al: experiences of long-term life-limiting conditions among patients and carers: what can we learn from a meta-review of systematic reviews of qualitative studies of chronic heart failure, chronic obstructive pulmonary disease and chronic kidney disease? BMJ Open 2016, 6(10):e011694. Search strategy is included as supplementary file.
References
- 1. Ene-Iordache B, Perico N, Bikbov B, et al. . Chronic kidney disease and cardiovascular risk in six regions of the world (ISN-KDDC): a cross-sectional study. Lancet Glob Health 2016;4:e307–e319. 10.1016/S2214-109X(16)00071-1 [DOI] [PubMed] [Google Scholar]
- 2. Schlieper G, Hess K, Floege J, et al. . The vulnerable patient with chronic kidney disease. Nephrology Dialysis Transplantation 2016;31:382–90. 10.1093/ndt/gfv041 [DOI] [PubMed] [Google Scholar]
- 3. As G, Chertow GM, Fan D, et al. . Chronic Kidney Disease and the Risks of Death, Cardiovascular Events, and Hospitalization. N Engl J Med 2016;351:1296–305. [DOI] [PubMed] [Google Scholar]
- 4. Chillon JM, Massy ZA, Stengel B. Neurological complications in chronic kidney disease patients. Nephrol Dial Transplant 2016;31:1606–14. 10.1093/ndt/gfv315 [DOI] [PubMed] [Google Scholar]
- 5. Jhee JH, Lee E, Cha MU, et al. . Prevalence of depression and suicidal ideation increases proportionally with renal function decline, beginning from early stages of chronic kidney disease. Medicine 2017;96:e8476 10.1097/MD.0000000000008476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goh ZS, Griva K. Anxiety and depression in patients with end-stage renal disease: impact and management challenges - a narrative review. Int J Nephrol Renovasc Dis 2018;11:93–102. 10.2147/IJNRD.S126615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Levin A, Tonelli M, Bonventre J, et al. . Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. Lancet 2017;390:1888–917. 10.1016/S0140-6736(17)30788-2 [DOI] [PubMed] [Google Scholar]
- 8. Stanifer JW, Muiru A, Jafar TH, et al. . Chronic kidney disease in low- and middle-income countries. Nephrology Dialysis Transplantation 2016;31:868–74. 10.1093/ndt/gfv466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Liyanage T, Ninomiya T, Jha V, et al. . Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet 2015;385:1975–82. 10.1016/S0140-6736(14)61601-9 [DOI] [PubMed] [Google Scholar]
- 10. Fraser SD, Roderick PJ, May CR, et al. . The burden of comorbidity in people with chronic kidney disease stage 3: a cohort study. BMC Nephrol 2015;16:193 10.1186/s12882-015-0189-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fraser SD, Taal MW. Multimorbidity in people with chronic kidney disease: implications for outcomes and treatment. Curr Opin Nephrol Hypertens 2016;25:465–72. 10.1097/MNH.0000000000000270 [DOI] [PubMed] [Google Scholar]
- 12. Holman HR. Chronic disease and the healthcare crisis. Chronic Illn 2005;1:265–74. 10.1177/17423953050010040601 [DOI] [PubMed] [Google Scholar]
- 13. May CR, Eton DT, Boehmer K, et al. . Rethinking the patient: using burden of treatment theory to understand the changing dynamics of illness. BMC Health Serv Res 2014;14:281 10.1186/1472-6963-14-281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. May C. Chronic illness and intractability: professional-patient interactions in primary care. Chronic Illn 2005;1:15–20. 10.1177/17423953050010011201 [DOI] [PubMed] [Google Scholar]
- 15. Karamanidou C, Weinman J, Horne R. A qualitative study of treatment burden among haemodialysis recipients. J Health Psychol 2014;19:556–69. 10.1177/1359105313475898 [DOI] [PubMed] [Google Scholar]
- 16. Eton DT, Elraiyah TA, Yost KJ, et al. . A systematic review of patient-reported measures of burden of treatment in three chronic diseases. Patient Relat Outcome Meas 2013;4:7–20. 10.2147/PROM.S44694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bohlen K, Scoville E, Shippee ND, et al. . Overwhelmed patients: a videographic analysis of how patients with type 2 diabetes and clinicians articulate and address treatment burden during clinical encounters. Diabetes Care 2012;35:47–9. 10.2337/dc11-1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gallacher K, Jani B, Morrison D, et al. . Qualitative systematic reviews of treatment burden in stroke, heart failure and diabetes: methodological challenges and solutions. BMC Med Res Methodol 2013;13:10 10.1186/1471-2288-13-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gallacher K, May CR, Montori VM, et al. . Understanding patients' experiences of treatment burden in chronic heart failure using normalization process theory. Ann Fam Med 2011;9:235–43. 10.1370/afm.1249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gallacher K, Morrison D, Jani B, et al. . Uncovering treatment burden as a key concept for stroke care: a systematic review of qualitative research. PLoS Med 2013;10:e1001473 10.1371/journal.pmed.1001473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ridgeway JL, Egginton JS, Tiedje K, et al. . Factors that lessen the burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Prefer Adherence 2014;8:339–51. 10.2147/PPA.S58014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shippee ND, Shah ND, May CR, et al. . Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. J Clin Epidemiol 2012;65:1041–51. 10.1016/j.jclinepi.2012.05.005 [DOI] [PubMed] [Google Scholar]
- 23. Sav A, Kendall E, McMillan SS, et al. . ’You say treatment, I say hard work': treatment burden among people with chronic illness and their carers in Australia. Health Soc Care Community 2013;21:n/a–74. 10.1111/hsc.12052 [DOI] [PubMed] [Google Scholar]
- 24. Sav A, King MA, Whitty JA, et al. . Burden of treatment for chronic illness: a concept analysis and review of the literature. Health Expect 2015;18:312–24. 10.1111/hex.12046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Eton DT, Ramalho de Oliveira D, Egginton JS, et al. . Building a measurement framework of burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Relat Outcome Meas 2012;3:39–49. 10.2147/PROM.S34681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Eton DT, Ridgeway JL, Egginton JS, et al. . Finalizing a measurement framework for the burden of treatment in complex patients with chronic conditions. Patient Relat Outcome Meas 2015;6:117–26. 10.2147/PROM.S78955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tran VT, Barnes C, Montori VM, et al. . Taxonomy of the burden of treatment: a multi-country web-based qualitative study of patients with chronic conditions. BMC Med 2015;13:115 10.1186/s12916-015-0356-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Boehmer KR, Gionfriddo MR, Rodriguez-Gutierrez R, et al. . Patient capacity and constraints in the experience of chronic disease: a qualitative systematic review and thematic synthesis. BMC Fam Pract 2016;17:127 10.1186/s12875-016-0525-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hunt KJ, May CR. Managing expectations: cognitive authority and experienced control in complex healthcare processes. BMC Health Serv Res 2017;17:459 10.1186/s12913-017-2366-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. May CR, Cummings A, Myall M, et al. . Experiences of long-term life-limiting conditions among patients and carers: what can we learn from a meta-review of systematic reviews of qualitative studies of chronic heart failure, chronic obstructive pulmonary disease and chronic kidney disease? BMJ Open 2016;6:e011694 10.1136/bmjopen-2016-011694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. May CR, Masters J, Welch L, et al. . EXPERTS 1-experiences of long-term life-limiting conditions among patients and carers: protocol for a qualitative meta-synthesis and conceptual modelling study. BMJ Open 2015;5:e007372 10.1136/bmjopen-2014-007372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tong A, Flemming K, McInnes E, et al. . Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12:181 10.1186/1471-2288-12-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.CASP Checklists. Critical Appraisal Skills Program (CASP). Oxford: CASP Checklists, 2014. [Google Scholar]
- 34. May C, Finch T. Implementing, Embedding, and Integrating Practices: an outline of normalization process theory. Sociology 2009;43:535–54. 10.1177/0038038509103208 [DOI] [Google Scholar]
- 35. Kahn LS, Vest BM, Madurai N, et al. . Chronic kidney disease (CKD) treatment burden among low-income primary care patients. Chronic Illn 2015;11:171–83. 10.1177/1742395314559751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Demain S, Gonçalves AC, Areia C, et al. . Living with, managing and minimising treatment burden in long term conditions: a systematic review of qualitative research. PLoS One 2015;10:e0125457 10.1371/journal.pone.0125457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fráguas G, Soares SM, Silva PA. The Family in the Context of the Care to the Diabetic Nephropathy-holder: demands and resources. Escola Anna Nery - Revista de Enfermagem 2008;12:271–7. [Google Scholar]
- 38. Ashby M, op’t Hoog C, Kellehear A, et al. . Renal dialysis abatement: lessons from a social study. Palliat Med 2005;19:389–96. 10.1191/0269216305pm1043oa [DOI] [PubMed] [Google Scholar]
- 39. Bailey PK, Ben-Shlomo Y, Tomson CR, et al. . Socioeconomic deprivation and barriers to live-donor kidney transplantation: a qualitative study of deceased-donor kidney transplant recipients. BMJ Open 2016;6:e010605 10.1136/bmjopen-2015-010605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chiaranai C. The lived experience of patients receiving hemodialysis treatment for end-stage renal disease: a qualitative study. J Nurs Res 2016;24:101–8. 10.1097/jnr.0000000000000100 [DOI] [PubMed] [Google Scholar]
- 41. Cho MK, Shin G. Gender-based experiences on the survival of chronic renal failure patients under hemodialysis for more than 20 years. Appl Nurs Res 2016;32:262–8. 10.1016/j.apnr.2016.08.008 [DOI] [PubMed] [Google Scholar]
- 42. Dekker W, Uerz I, Wils JP. Living well with end stage renal disease: patients' narratives interrupted from a virtue perspective. Ethical Theory Moral Pract 2005;8:485–506. 10.1007/s10677-005-8242-9 [DOI] [PubMed] [Google Scholar]
- 43. Ekelund ML, Andersson SI. "I need to lead my own life in any case"–a study of patients in dialysis with or without a partner. Patient Educ Couns 2010;81:30–6. 10.1016/j.pec.2009.10.025 [DOI] [PubMed] [Google Scholar]
- 44. Kazley AS, Johnson E, Simpson K, et al. . African American patient knowledge of kidney disease: a qualitative study of those with advanced chronic kidney disease. Chronic Illn 2015;11:245–55. 10.1177/1742395314556658 [DOI] [PubMed] [Google Scholar]
- 45. Lee VY, Seah WY, Kang AW, et al. . Managing multiple chronic conditions in Singapore - Exploring the perspectives and experiences of family caregivers of patients with diabetes and end stage renal disease on haemodialysis. Psychol Health 2016;31:1220–36. 10.1080/08870446.2016.1203921 [DOI] [PubMed] [Google Scholar]
- 46. Lindberg M, Lindberg P. Overcoming obstacles for adherence to phosphate binding medication in dialysis patients: a qualitative study. Pharm World Sci 2008;30:571–6. 10.1007/s11096-008-9212-9 [DOI] [PubMed] [Google Scholar]
- 47. Mercado-Martínez FJ, Correa-Mauricio ME. [Living in hemodialysis without social insurance: the voices of renal sick people and their families]. Salud Publica Mex 2015;57:155–60. [PubMed] [Google Scholar]
- 48. Mercado-Martinez FJ, Silva DGVda, Souza SdaSde, et al. . Vivendo com insuficiência renal: obstáculos na terapia da hemodiálise na perspectiva das pessoas doentes e suas famílias. Physis: Revista de Saúde Coletiva 2015;25:59–74. 10.1590/S0103-73312015000100005 [DOI] [Google Scholar]
- 49. Mercado-Martínez FJ, Hernández-Ibarra E, Ascencio-Mera CD, et al. . Viviendo con trasplante renal, sin protección social en salud: ¿Qué dicen los enfermos sobre las dificultades económicas que enfrentan y sus efectos? Cadernos de Saúde Pública 2014;30:2092–100. 10.1590/0102-311X00150713 [DOI] [PubMed] [Google Scholar]
- 50. Seah AS, Tan F, Srinivas S, et al. . Opting out of dialysis – Exploring patients' decisions to forego dialysis in favour of conservative non-dialytic management for end-stage renal disease. Health Expect 2015;18:1018–29. 10.1111/hex.12075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Walker RC, Howard K, Tong A, et al. . The economic considerations of patients and caregivers in choice of dialysis modality. Hemodial Int 2016;20:634–42. 10.1111/hdi.12424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Cervantes L, Fischer S, Berlinger N, et al. . THe illness experience of undocumented immigrants with end-stage renal disease. JAMA Intern Med 2017;177:529–35. 10.1001/jamainternmed.2016.8865 [DOI] [PubMed] [Google Scholar]
- 53. Anderson K, Cunningham J, Devitt J, et al. . "Looking back to my family": indigenous Australian patients' experience of hemodialysis. BMC Nephrol 2012;13:114 10.1186/1471-2369-13-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Polaschek N. Living on dialysis: concerns of clients in a renal setting. J Adv Nurs 2003;41:44–52. 10.1046/j.1365-2648.2003.02504.x [DOI] [PubMed] [Google Scholar]
- 55. Polaschek N. Managing home dialysis: the client perspective on independent treatment. Renal Society of Australasia Journal 2006;2:53–63. [Google Scholar]
- 56. Polaschek N. ’Doing dialysis at home': client attitudes towards renal therapy. J Clin Nurs 2007;16(3A):51–8. 10.1111/j.1365-2702.2006.01622.x [DOI] [PubMed] [Google Scholar]
- 57. Rix EF, Barclay L, Stirling J, et al. . The perspectives of Aboriginal patients and their health care providers on improving the quality of hemodialysis services: a qualitative study. Hemodial Int 2015;19:80–9. 10.1111/hdi.12201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rix EF, Barclay L, Stirling J, et al. . ’Beats the alternative but it messes up your life': aboriginal people’s experience of haemodialysis in rural Australia. BMJ Open 2014;4:e005945 10.1136/bmjopen-2014-005945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Shih LC, Honey M. The impact of dialysis on rurally based Māori and their whānau/families. Nurs Prax N Z 2011;27:5–15. [PubMed] [Google Scholar]
- 60. Valsaraj BP, Bhat SM, Prabhu R, et al. . A qualitative research on the experience of haemodialysis in South Karnataka: lived experience of persons undergoing haemodialysis. Journal of Krishna Institute of Medical Sciences University 2014;3:90–100. [Google Scholar]
- 61. Walker RC, Howard K, Morton RL, et al. . Patient and caregiver values, beliefs and experiences when considering home dialysis as a treatment option: a semi-structured interview study. Nephrol Dial Transplant 2016;31:133–41. 10.1093/ndt/gfv330 [DOI] [PubMed] [Google Scholar]
- 62. Wells SA. Determinants of adherence to living on dialysis for Mexican Americans. Sage Open 2015;5:215824401557496–12. 10.1177/2158244015574961 [DOI] [Google Scholar]
- 63. Tong A, Sainsbury P, Chadban S, et al. . Patients' experiences and perspectives of living with CKD. Am J Kidney Dis 2009;53:689–700. 10.1053/j.ajkd.2008.10.050 [DOI] [PubMed] [Google Scholar]
- 64. Allen D, Badro V, Denyer-Willis L, et al. . Fragmented care and whole-person illness: Decision-making for people with chronic end-stage kidney disease. Chronic Illn 2015;11:44–55. 10.1177/1742395314562974 [DOI] [PubMed] [Google Scholar]
- 65. Oyegbile YO, Brysiewicz P. Family caregiver’s experiences of providing care to patients with End-Stage Renal Disease in South-West Nigeria. J Clin Nurs 2017;26(17-18):2624–32. 10.1111/jocn.13689 [DOI] [PubMed] [Google Scholar]
- 66. Wu CC, Lin CC, Hsieh HF, et al. . Lived experiences and illness representation of Taiwanese patients with late-stage chronic kidney disease. J Health Psychol 2016;21:2788–98. 10.1177/1359105315587134 [DOI] [PubMed] [Google Scholar]
- 67. Nobahar M. Exploring experiences of the quality of nursing care among patients, nurses, caregivers and physicians in a haemodialysis department. Journal of Renal Care 2016;xx(xx):1–10. [DOI] [PubMed] [Google Scholar]
- 68. Nobahar M, Tamadon MR. Barriers to and facilitators of care for hemodialysis patients; a qualitative study. J Renal Inj Prev 2016;5:39–44. 10.15171/jrip.2016.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Blogg AH, Hyde C. The experience of spouses caring for a person on home haemodialysis: an ethnography. Renal Society of Australasia Journal 2008;4:75–80. [Google Scholar]
- 70. Hanson CS, Chapman JR, Craig JC, et al. . Patient experiences of training and transition to home haemodialysis: a mixed-methods study. Nephrology 2017;22:631–41. 10.1111/nep.12827 [DOI] [PubMed] [Google Scholar]
- 71. Rygh E, Arild E, Johnsen E, et al. . Choosing to live with home dialysis-patients' experiences and potential for telemedicine support: a qualitative study. BMC Nephrol 2012;13:13(13):13 10.1186/1471-2369-13-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. MLcAj S, GAdS B, Pereira ER, et al. . Patients’ experiences of peritoneal dialysis at home: a phenomenological approach. Rev Latino-am Enfermagem 2012;20:68–75. [DOI] [PubMed] [Google Scholar]
- 73. Keeping LM, English LM. Informal and incidental learning with patients who use continuous ambulatory peritoneal dialysis. Nephrol Nurs J 2001;28:313–23. [PubMed] [Google Scholar]
- 74. Wilkinson E, Randhawa G, Brown E, et al. . Exploring access to end of life care for ethnic minorities with end stage kidney disease through recruitment in action research. BMC Palliat Care 2016;15:57 10.1186/s12904-016-0128-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Wilkinson E, Randhawa G, Farrington K, et al. . Lack of awareness of kidney complications despite familiarity with diabetes: a multi-ethnic qualitative study. J Ren Care 2011;37:2–11. 10.1111/j.1755-6686.2011.00199.x [DOI] [PubMed] [Google Scholar]
- 76. Tijerina MS. Psychosocial factors influencing Mexican-American women’s adherence with hemodialysis treatment. Soc Work Health Care 2006;43:57–74. 10.1300/J010v43n01_04 [DOI] [PubMed] [Google Scholar]
- 77. Anderson K, Devitt J, Cunningham J, et al. . "All they said was my kidneys were dead": Indigenous Australian patients' understanding of their chronic kidney disease. Med J Aust 2008;189:499–503. [DOI] [PubMed] [Google Scholar]
- 78. Burnette L, Kickett M. ’You are just a puppet': Australian Aboriginal people’s experience of disempowerment when undergoing treatment for end-stage renal disease. Renal Society of Australasia Journal 2009;5:113–8. [Google Scholar]
- 79. Morton RL, Devitt J, Howard K, et al. . Patient views about treatment of stage 5 CKD: a qualitative analysis of semistructured interviews. Am J Kidney Dis 2010;55:431–40. 10.1053/j.ajkd.2009.11.011 [DOI] [PubMed] [Google Scholar]
- 80. Walker RC, Walker S, Morton RL, et al. . Māori patients' experiences and perspectives of chronic kidney disease: a New Zealand qualitative interview study. BMJ Open 2017;7:e013829 10.1136/bmjopen-2016-013829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Stewart M. Qualitative inquiry: perceptions of sexuality by African Americans experiencing haemodialysis. J Adv Nurs 2013;69:1704–13. 10.1111/jan.12028 [DOI] [PubMed] [Google Scholar]
- 82. Salvalaggio GK, L.: Minore B. Perspectives on health: experiences of First Nations dialysis patients relocated from remote communities for treatment. Canadian Journal of Rural Medicine 2003;8:19–24. [Google Scholar]
- 83. Crowley-Matoka M. Desperately seeking "normal": the promise and perils of living with kidney transplantation. Soc Sci Med 2005;61:821–31. 10.1016/j.socscimed.2004.08.043 [DOI] [PubMed] [Google Scholar]
- 84. Gordon EJ, Prohaska TR, Gallant M, et al. . Self-care strategies and barriers among kidney transplant recipients: a qualitative study. Chronic Illn 2009;5:75–91. 10.1177/1742395309103558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Schmid-Mohler G, Schäfer-Keller P, Frei A, et al. . A mixed-method study to explore patients' perspective of self-management tasks in the early phase after kidney transplant. Prog Transplant 2014;24:8–18. 10.7182/pit2014728 [DOI] [PubMed] [Google Scholar]
- 86. Chenitz KB, Fernando M, Shea JA. In-center hemodialysis attendance: patient perceptions of risks, barriers, and recommendations. Hemodial Int 2014;18:364–73. 10.1111/hdi.12139 [DOI] [PubMed] [Google Scholar]
- 87. Campos CJ, Turato ER. [Hemodialysis treatment as perceived by the renal patient: clinical qualitative study]. Rev Bras Enferm 2010;63:799–805. [DOI] [PubMed] [Google Scholar]
- 88. Campos CG, Mantovani MF, Nascimento ME, et al. . [Social representations of illness among people with chronic kidney disease]. Rev Gaucha Enferm 2015;36:106–12. 10.1590/1983-1447.2015.02.48183 [DOI] [PubMed] [Google Scholar]
- 89. de Brito DC, de Paula AM, Grincenkov FR, et al. . Analysis of the changes and difficulties arising from kidney transplantation: a qualitative study. Rev Lat Am Enfermagem 2015;23:419–26. 10.1590/0104-1169.0106.2571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Finnegan-John J, Thomas VJ. The psychosocial experience of patients with end-stage renal disease and its impact on quality of life: findings from a needs assessment to shape a service. ISRN Nephrol 2013;2013:1–8. 10.5402/2013/308986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. King N, Carroll C, Newton P, et al. . "You can’t cure it so you have to endure it": the experience of adaptation to diabetic renal disease. Qual Health Res 2002;12:329–46. 10.1177/104973202129119928 [DOI] [PubMed] [Google Scholar]
- 92. Costantini L, Beanlands H, McCay E, et al. . The self-management experience of people with mild to moderate chronic kidney disease. Nephrol Nurs J 2008;35:147–55. [PubMed] [Google Scholar]
- 93. Lopez-Vargas PA, Tong A, Howell M, et al. . Patient awareness and beliefs about the risk factors and comorbidities associated with chronic kidney disease : a mixed-methods study. Nephrology 2017;22:374–81. 10.1111/nep.12829 [DOI] [PubMed] [Google Scholar]
- 94. Lopez-Vargas PA, Tong A, Phoon RK, et al. . Knowledge deficit of patients with stage 1-4 CKD: a focus group study. Nephrology 2014;19:234–43. 10.1111/nep.12206 [DOI] [PubMed] [Google Scholar]
- 95. Mason J, Stone M, Khunti K, et al. . Educational needs for blood pressure control in chronic kidney disease. J Ren Care 2007;33:134–8. 10.1111/j.1755-6686.2007.tb00059.x [DOI] [PubMed] [Google Scholar]
- 96. Muduma G, Shupo FC, Dam S, et al. . Patient survey to identify reasons for non-adherence and elicitation of quality of life concepts associated with immunosuppressant therapy in kidney transplant recipients. Patient Prefer Adherence 2016;10:27–36. 10.2147/PPA.S96086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Noble H, Kelly D, Hudson P. Experiences of carers supporting dying renal patients managed without dialysis. J Adv Nurs 2013;69:1829–39. 10.1111/jan.12049 [DOI] [PubMed] [Google Scholar]
- 98. Noble H, Meyer J, Bridges J, et al. . Examining renal patients' death trajectories without dialysis. End of Life Care 2010;4:26–34. [Google Scholar]
- 99. Rifkin DE, Laws MB, Rao M, et al. . Medication adherence behavior and priorities among older adults with CKD: a semistructured interview study. Am J Kidney Dis 2010;56:439–46. 10.1053/j.ajkd.2010.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Vélez E, Ramasco M. Meaning of illness and illness representations, crucial factors to integral care. Edtna Erca J 2006;32:81–5. 10.1111/j.1755-6686.2006.tb00456.x [DOI] [PubMed] [Google Scholar]
- 101. Williams AF, Manias E. Perceptions of pain control by consumers with chronic kidney disease. J Nurs Healthc Chronic Illn 2009;1:199–209. 10.1111/j.1752-9824.2009.01022.x [DOI] [Google Scholar]
- 102. Williams AF, Manias E, Walker R. Adherence to multiple, prescribed medications in diabetic kidney disease: a qualitative study of consumers’ and health professionals’ perspectives. Int J Nurs Stud 2008;45:1742–56. 10.1016/j.ijnurstu.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 103. RARd S, VLd S, GJNd O, et al. . Coping strategies used by chronic renal failure patients on hemodialysis. Escola Anna Nery - Revista de Enfermagem 2016;20:147–54. [Google Scholar]
- 104. Al-Arabi S. Quality of life: subjective descriptions of challenges to patients with end stage renal disease. Nephrol Nurs J 2006;33:285–92. [PubMed] [Google Scholar]
- 105. Bourbonnais FF, Tousignant KF. The pain experience of patients on maintenance hemodialysis. Nephrol Nurs J 2012;39:13–19. [PubMed] [Google Scholar]
- 106. Clarkson KA, Robinson K. Life on dialysis: a lived experience. Nephrol Nurs J 2010;37:29–35. [PubMed] [Google Scholar]
- 107. Aasen EM, Kvangarsnes M, Heggen K. Perceptions of patient participation amongst elderly patients with end-stage renal disease in a dialysis unit. Scand J Caring Sci 2012;26:61–9. 10.1111/j.1471-6712.2011.00904.x [DOI] [PubMed] [Google Scholar]
- 108. Richard CJ, Engebretson J. Negotiating living with an arteriovenous fistula for hemodialysis. Nephrol Nurs J 2010;37:363–74. [PubMed] [Google Scholar]
- 109. Tweed AE, Ceaser K. Renal replacement therapy choices for pre-dialysis renal patients. Br J Nurs 2005;14:659–64. 10.12968/bjon.2005.14.12.18287 [DOI] [PubMed] [Google Scholar]
- 110. Xi W, Harwood L, Diamant MJ, et al. . Patient attitudes towards the arteriovenous fistula: a qualitative study on vascular access decision making. Nephrol Dial Transplant 2011;26:3302–8. 10.1093/ndt/gfr055 [DOI] [PubMed] [Google Scholar]
- 111. Taylor MJ, Hanson CS, Casey JR, et al. . “You know your own fistula, it becomes a part of you”-Patient perspectives on vascular access: a semistructured interview study. Hemodial Int 2016;20:5–14. 10.1111/hdi.12340 [DOI] [PubMed] [Google Scholar]
- 112. Yu J, Ng HJ, Nandakumar M, et al. . The management of food cravings and thirst in hemodialysis patients: a qualitative study. J Health Psychol 2016;21:217–27. 10.1177/1359105314525066 [DOI] [PubMed] [Google Scholar]
- 113. Cristóvão AF. Dificultades y estrategias en el manejo del régimen terapéutico en el paciente renal crónico en hemodiálisis. Enfermería Nefrológica 2013;16:247–55. 10.4321/S2254-28842013000400006 [DOI] [Google Scholar]
- 114. Gricio TC, KusumotaI L, MldL Cândido. Perceptions and knowledge of patients with chronic kidney disease under conservative treatment. Rev Eletr Enf 2009;11:884–93. [Google Scholar]
- 115. Hagren B, Pettersen IM, Severinsson E, et al. . Maintenance haemodialysis: patients' experiences of their life situation. J Clin Nurs 2005;14:294–300. 10.1111/j.1365-2702.2004.01036.x [DOI] [PubMed] [Google Scholar]
- 116. Herbias LH, Soto RA, Figueroa HB, et al. . Meaning of quality of life in patients on hemodialysis therapy: a phenomenological study. Revista de la Sociedad Espanola de Enfermeria Nefrologica 2016;19:37–44. [Google Scholar]
- 117. Tovazzi ME, Mazzoni V. Personal paths of fluid restriction in patients on hemodialysis. Nephrol Nurs J 2012;39:207–15. [PubMed] [Google Scholar]
- 118. Avril-Sephula B, Meekums B, Jackson C. How do partners living with haemodialysis patients cope? Journal of Renal Nursing 2014;6:133–7. 10.12968/jorn.2014.6.3.133 [DOI] [Google Scholar]
- 119. Roso CC, Beuter M, Kruse MHL, et al. . Self-care of patients in conservative treatment of chronic renal insufficiency. Text Context Nursing 2013;22:739–45. [Google Scholar]
- 120. Hong LI, Wang W, Chan EY, et al. . Dietary and fluid restriction perceptions of patients undergoing haemodialysis: an exploratory study. J Clin Nurs 2017;26:3664–76. 10.1111/jocn.13739 [DOI] [PubMed] [Google Scholar]
- 121. de Brito-Ashurst I, Perry L, Sanders TA, et al. . Barriers and facilitators of dietary sodium restriction amongst Bangladeshi chronic kidney disease patients. J Hum Nutr Diet 2011;24:86–95. 10.1111/j.1365-277X.2010.01129.x [DOI] [PubMed] [Google Scholar]
- 122. Theofilou P, Synodinou C, Panagiotaki H. Undergoing haemodialysis: a qualitative study to investigate the lived experiences of patients. Europe’s Journal of Psychology 2013;9:19–32. 10.5964/ejop.v9i1.338 [DOI] [Google Scholar]
- 123. Shirazian S, Crnosija N, Weinger K, et al. . The self-management experience of patients with type 2 diabetes and chronic kidney disease: A qualitative study. Chronic Illn 2016;12:18–28. 10.1177/1742395315614381 [DOI] [PubMed] [Google Scholar]
- 124. Walker R, James H, Burns A. Adhering to behaviour change in older pre-dialysis populations–what do patients think? A qualitative study. J Ren Care 2012;38:34–42. 10.1111/j.1755-6686.2012.00262.x [DOI] [PubMed] [Google Scholar]
- 125. Kierans C, Padilla-Altamira C, Garcia-Garcia G, et al. . When health systems are barriers to health care: challenges faced by uninsured Mexican kidney patients. PLoS One 2013;8:e54380 10.1371/journal.pone.0054380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Bristowe K, Horsley HL, Shepherd K, et al. . Thinking ahead–the need for early advance care planning for people on haemodialysis: a qualitative interview study. Palliat Med 2015;29:443–50. 10.1177/0269216314560209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Tonkin-Crine S, Okamoto I, Leydon GM, et al. . Understanding by older patients of dialysis and conservative management for chronic kidney failure. Am J Kidney Dis 2015;65:443–50. 10.1053/j.ajkd.2014.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Johnston S, Noble H. Factors influencing patients with stage 5 chronic kidney disease to opt for conservative management: a practitioner research study. J Clin Nurs 2012;21(9-10):1215–22. 10.1111/j.1365-2702.2011.04001.x [DOI] [PubMed] [Google Scholar]
- 129. Lo C, Ilic D, Teede H, et al. . The perspectives of patients on health-care for co-morbid diabetes and chronic kidney disease: a qualitative study. PLoS One 2016;11:e0146615 10.1371/journal.pone.0146615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Prieto MA, Escudero MJ, Suess A, et al. . Patients’ opinions and expectations about the dialysis care process. An Sist Sanit Navar 2011;34:21–31. [PubMed] [Google Scholar]
- 131. IaS R, Larrea AA, OGa U, et al. . Withdrawing dialysis in End-stage renal disease: What do patients think? Enferm Nefrol 2014;17:110–9. [Google Scholar]
- 132. Yngman-Uhlin P, Fogelberg A, Uhlin F. Life in standby: hemodialysis patients' experiences of waiting for kidney transplantation. J Clin Nurs 2016;25(1-2):92–8. 10.1111/jocn.12994 [DOI] [PubMed] [Google Scholar]
- 133. Moran A, Scott A, Darbyshire P. Waiting for a kidney transplant: patients’ experiences of haemodialysis therapy. J Adv Nurs 2011;67:501–9. 10.1111/j.1365-2648.2010.05460.x [DOI] [PubMed] [Google Scholar]
- 134. Axelsson L, Klang B, Lundh Hagelin C, et al. . End of life of patients treated with haemodialysis as narrated by their close relatives. Scand J Caring Sci 2015;29:776–84. 10.1111/scs.12209 [DOI] [PubMed] [Google Scholar]
- 135. Yngman-Uhlin P, Friedrichsen M, Gustavsson M, et al. . Circling around in tiredness: perspectives of patients on peritoneal dialysis. Nephrol Nurs J 2010;37:407–13. [PubMed] [Google Scholar]
- 136. Axelsson L, Randers I, Jacobson SH, et al. . Living with haemodialysis when nearing end of life. Scand J Caring Sci 2012;26:45–52. 10.1111/j.1471-6712.2011.00902.x [DOI] [PubMed] [Google Scholar]
- 137. Heiwe S, Clyne N, Dahlgren MA. Living with chronic renal failure: patients' experiences of their physical and functional capacity. Physiother Res Int 2003;8:167–77. 10.1002/pri.287 [DOI] [PubMed] [Google Scholar]
- 138. Horigan AE, Schneider SM, Docherty S, et al. . The experience and self-management of fatigue in patients on hemodialysis. Nephrol Nurs J 2013;40:113–22. [PMC free article] [PubMed] [Google Scholar]
- 139. White N, Richter J, Koeckeritz J, et al. . “Going Forward”: Family resiliency in patients on hemodialysis. J Fam Nurs 2004;10:357–78. 10.1177/1074840704267163 [DOI] [Google Scholar]
- 140. Heiwe S, Dahlgren MA. Living with chronic renal failure: Coping with physical activities of daily living. Adv Physiother 2004;6:147–57. 10.1080/14038190410019540 [DOI] [Google Scholar]
- 141. Rabiei L, Eslami AA, Abedi H, et al. . Caring in an atmosphere of uncertainty: perspectives and experiences of caregivers of peoples undergoing haemodialysis in Iran. Scand J Caring Sci 2016;30:594–601. 10.1111/scs.12283 [DOI] [PubMed] [Google Scholar]
- 142. Shahgholian N, Yousefi H. Supporting hemodialysis patients: a phenomenological study. Iran J Nurs Midwifery Res 2015;20:626–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Yeun EJ, Bang HY, Kim EJ, et al. . Attitudes toward stress and coping among primary caregivers of patients undergoing hemodialysis: a Q-methodology study. Hemodial Int 2016;20:453–62. 10.1111/hdi.12404 [DOI] [PubMed] [Google Scholar]
- 144. Yumang MJ, Hammond L, Filteau N, et al. . Perceptions of risk for foot problems and foot care practices of patients on hemodialysis. Nephrol Nurs J 2009;36:509–16. [PubMed] [Google Scholar]
- 145. Barbosa GDS, Valadares GV. Hemodialysis: patient’s adaptation and life style. Acta Paul Enferm 2009;22(Especial Nefrologia:524–7. [Google Scholar]
- 146. Calvey D, Mee L. The lived experience of the person dependent on haemodialysis. J Ren Care 2011;37:201–7. 10.1111/j.1755-6686.2011.00235.x [DOI] [PubMed] [Google Scholar]
- 147. Krespi R, Bone M, Ahmad R, et al. . Haemodialysis patients’ beliefs about renal failure and its treatment. Patient Educ Couns 2004;53:189–96. 10.1016/S0738-3991(03)00147-2 [DOI] [PubMed] [Google Scholar]
- 148. Cox KJ, Parshall MB, Hernandez SHA, et al. . Symptoms among patients receiving in-center hemodialysis: a qualitative study. Hemodial Int 2017;21:524–33. 10.1111/hdi.12521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Machado LRC, Car MR. A dialetic of patients' daily life with chronic renal failure in hemodialysis: the unavoidable and the casual. Rev Esc Enferm USP 2003;37:27–35. [DOI] [PubMed] [Google Scholar]
- 150. Moran A, Scott PA, Darbyshire P. Existential boredom: the experience of living on haemodialysis therapy. Med Humanit 2009;35:70–5. 10.1136/jmh.2009.001511 [DOI] [PubMed] [Google Scholar]
- 151. Krespi Boothby MR, Salmon P. [Self-efficacy and hemodialysis treatment: a qualitative and quantitative approach]. Turk Psikiyatri Derg 2013;24:84–93. [PubMed] [Google Scholar]
- 152. Tong A, Palmer S, Manns B, et al. . The beliefs and expectations of patients and caregivers about home haemodialysis: an interview study. BMJ Open 2013;3:e002148 10.1136/bmjopen-2012-002148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Torchi TS, STCd A, Guimarães AM AGM, et al. . Clinical conditions and health care demand behavior of chronic renal patients. Acta Paul Enferm 2014;27:585–90. [Google Scholar]
- 154. Cadena DMaGn, GPAb H, Atilano BF, et al. . Anchored to a machine: experiences of patients with chronic kidney disease. Revista CONAMED 2015;20(S1):16–20. [Google Scholar]
- 155. Klava dos Reis C, Guirardello EB, Gomes Campos CJ. [The person with renal chronic disease and caring demands]. Rev Bras Enferm 2008;61:336–41. [PubMed] [Google Scholar]
- 156. Baillie J, Lankshear A. Patient and family perspectives on peritoneal dialysis at home: findings from an ethnographic study. J Clin Nurs 2015;24(1-2):222–34. 10.1111/jocn.12663 [DOI] [PubMed] [Google Scholar]
- 157. Baillie J, Lankshear A. Patients' and relatives' experiences of peritonitis when using peritoneal dialysis. J Ren Care 2015;41:177–86. 10.1111/jorc.12118 [DOI] [PubMed] [Google Scholar]
- 158. Xi W, Singh PM, Harwood L, et al. . Patient experiences and preferences on short daily and nocturnal home hemodialysis. Hemodial Int 2013;17:201–7. 10.1111/j.1542-4758.2012.00731.x [DOI] [PubMed] [Google Scholar]
- 159. Giles S. Transformations: a phenomenological investigation into the life-world of home haemodialysis. Soc Work Health Care 2004;38:29–50. [DOI] [PubMed] [Google Scholar]
- 160. Giles S. Struggles between the body and machine: the paradox of living with a home haemodialysis machine. Soc Work Health Care 2005;41:19–35. [DOI] [PubMed] [Google Scholar]
- 161. Low J, Myers J, Smith G, et al. . The experiences of close persons caring for people with chronic kidney disease stage 5 on conservative kidney management: contested discourses of ageing. Health 2014;18:613–30. 10.1177/1363459314524805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. FKd S, Valadares GV. Living between the nightmare and the awakening - the first time in dealing with peritoneal dialysis. Escola Anna Nery - Revista de Enfermagem 2011;15:39–46. [Google Scholar]
- 163. McCarthy A, Shaban R, Boys J, et al. . Compliance, normality, and the patient on peritoneal dialysis. Nephrol Nurs J 2010;37:243–50. [PubMed] [Google Scholar]
- 164. Chong HJ, Kim HK, Kim SR, et al. . Waiting for a kidney transplant: the experience of patients with end-stage renal disease in South Korea. J Clin Nurs 2016;25(7-8):930–9. 10.1111/jocn.13107 [DOI] [PubMed] [Google Scholar]
- 165. Flores RV, Thome EG. Feelings of patients on the waiting list for a kidney transplant]. Rev Bras Enferm 2004;57:687–90. [DOI] [PubMed] [Google Scholar]
- 166. Kierans C. Narrating kidney disease: the significance of sensation and time in the emplotment of patient experience. Cult Med Psychiatry 2005;29:341–59. 10.1007/s11013-005-9171-8 [DOI] [PubMed] [Google Scholar]
- 167. Kierans CM, Maynooth NUI. Sensory and narrative identity: the narration of illness process among chronic renal sufferers in Ireland. Anthropol Med 2001;8(2-3):237–53. 10.1080/13648470120101381 [DOI] [Google Scholar]
- 168. Knihs NDS, Sartori DL, Zink V, et al. . The experience of patients who need renal transplantation while waiting for a compatible organ. Text Context Nursing 2013;22:1160–8. [Google Scholar]
- 169. Lawrence C, Sharma S, Da Silva-Gane M, et al. . Exploring the views of patients not on the transplant waiting list: a qualitative study. J Ren Care 2013;39:118–24. 10.1111/j.1755-6686.2013.12012.x [DOI] [PubMed] [Google Scholar]
- 170. Lopes SGR, Silva DMGVda. Narratives of women on hemodialysis: waiting for a kidney transplant. Texto & Contexto - Enfermagem 2014;23:680–7. 10.1590/0104-07072014002540013 [DOI] [Google Scholar]
- 171. Spiers J, Smith JA. Waiting for a kidney from a deceased donor: an interpretative phenomenological analysis. Psychol Health Med 2016;21:836–44. 10.1080/13548506.2015.1112415 [DOI] [PubMed] [Google Scholar]
- 172. Wachterman MW, McCarthy EP, Marcantonio ER, et al. . Mistrust, misperceptions, and miscommunication: a qualitative study of preferences about kidney transplantation among African Americans. Transplant Proc 2015;47:240–6. 10.1016/j.transproceed.2015.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Allen D, Wainwright M, Hutchinson T. ’Non-compliance' as illness management: Hemodialysis patients' descriptions of adversarial patient-clinician interactions. Soc Sci Med 2011;73:129–34. 10.1016/j.socscimed.2011.05.018 [DOI] [PubMed] [Google Scholar]
- 174. Sieverdes JC, Nemeth LS, Magwood GS, et al. . African American kidney transplant patients' perspectives on challenges in the living donation process. Prog Transplant 2015;25:164–75. 10.7182/pit2015852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Boaz A, Morgan M. Working to establish ’normality' post-transplant: a qualitative study of kidney transplant patients. Chronic Illn 2014;10:247–58. 10.1177/1742395313504789 [DOI] [PubMed] [Google Scholar]
- 176. Goldade K, Sidhwani S, Patel S, et al. . Kidney transplant patients' perceptions, beliefs, and barriers related to regular nephrology outpatient visits. Am J Kidney Dis 2011;57:11–20. 10.1053/j.ajkd.2010.08.023 [DOI] [PubMed] [Google Scholar]
- 177. Spiers J, Smith JA, Drage M. A longitudinal interpretative phenomenological analysis of the process of kidney recipients' resolution of complex ambiguities within relationships with their living donors. J Health Psychol 2015. (published Online First: 2015/05/02). [DOI] [PubMed] [Google Scholar]
- 178. Stanfill A, Bloodworth R, Cashion A. Lessons learned: experiences of gaining weight by kidney transplant recipients. Prog Transplant 2012;22:71–8. 10.7182/pit2012986 [DOI] [PubMed] [Google Scholar]
- 179. Tielen M, van Exel NJ, van Buren MC, et al. . Attitudes towards medication non-adherence in elderly kidney transplant patients: a Q methodology study. Nephrol Dial Transplant 2011;26:1723–8. 10.1093/ndt/gfq642 [DOI] [PubMed] [Google Scholar]
- 180. Gordon EJ, Prohaska TR, Gallant MP, et al. . Adherence to immunosuppression: a prospective diary study. Transplant Proc 2007;39:3081–5. 10.1016/j.transproceed.2007.02.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Leung SS, Shiu AT. Experience of Hong Kong patients awaiting kidney transplantation in mainland China. J Clin Nurs 2007;16:341–9. 10.1111/j.1365-2702.2007.02070.x [DOI] [PubMed] [Google Scholar]
- 182. Orr A, Orr D, Willis S, et al. . Patient perceptions of factors influencing adherence to medication following kidney transplant. Psychol Health Med 2007;12:509–17. 10.1080/13548500701294556 [DOI] [PubMed] [Google Scholar]
- 183. Orr A, Willis S, Holmes M, et al. . Living with a kidney transplant: a qualitative investigation of quality of life. J Health Psychol 2007;12:653–62. [DOI] [PubMed] [Google Scholar]
- 184. Schipper K, Abma TA, Koops C, et al. . Sweet and sour after renal transplantation: a qualitative study about the positive and negative consequences of renal transplantation. Br J Health Psychol 2014;19:580–91. 10.1111/bjhp.12057 [DOI] [PubMed] [Google Scholar]
- 185. Wiederhold D, Langer G, Landenberger M. Ambivalent lived experiences and instruction need of patients in the early period after kidney transplantation: a phenomenological study. Nephrol Nurs J 2011;38:417–23. [PubMed] [Google Scholar]
- 186. Buldukoglu K, Kulakac O, Kececioglu N, et al. . Recipients??? Perceptions of their transplanted kidneys. Transplantation 2005;80:471–6. 10.1097/01.tp.0000168149.95310.6e [DOI] [PubMed] [Google Scholar]
- 187. Axelsson L, Randers I, Lundh Hagelin C, et al. . Thoughts on death and dying when living with haemodialysis approaching end of life. J Clin Nurs 2012;21(15-16):2149–59. 10.1111/j.1365-2702.2012.04156.x [DOI] [PubMed] [Google Scholar]
- 188. Chatrung C, Sorajjakool S, Amnatsatsue K. Wellness and religious coping among thai individuals living with chronic kidney disease in southern california. J Relig Health 2015;54:2198–211. 10.1007/s10943-014-9958-4 [DOI] [PubMed] [Google Scholar]
- 189. Hain DJ, Wands L, Liehr P. Approaches to resolve health challenges in a population of older adults undergoing hemodialysis. Res Gerontol Nurs 2011;4:53–62. 10.3928/19404921-20100330-01 [DOI] [PubMed] [Google Scholar]
- 190. Lin CC, Han CY, Pan IJ. A qualitative approach of psychosocial adaptation process in patients undergoing long-term hemodialysis. Asian Nurs Res 2015;9:35–41. 10.1016/j.anr.2014.10.007 [DOI] [PubMed] [Google Scholar]
- 191. Rodrigues DFD, Schwartz E, MdG S, et al. . Experience of men undergoing hemodialysis about their sexuality. Avengerm 2011;XXIX:255–62. [Google Scholar]
- 192. Tanyi RA, Werner JS. Women’s experience of spirituality within end-stage renal disease and hemodialysis. Clin Nurs Res 2008;17:32–49. 10.1177/1054773807311691 [DOI] [PubMed] [Google Scholar]
- 193. Tanyi RA, Werner JS. Toward a trajectory of adjustment in women with end-stage renal disease on haemodialysis. J Clin Nurs 2008;17(5A):43–50. 10.1111/j.1365-2702.2007.02199.x [DOI] [PubMed] [Google Scholar]
- 194. Martin-McDonald K. Being dialysis-dependent: a qualitative perspective. Collegian 2003;10:29–33. 10.1016/S1322-7696(08)60052-9 [DOI] [PubMed] [Google Scholar]
- 195. MartinMcDonald K. Dialysis-dependency: the reformulated or remnant person. Contemp Nurse 2004;16(1-2):151–61. 10.5172/conu.16.1-2.151 [DOI] [PubMed] [Google Scholar]
- 196. H-y N, J-f L. The psychological trajectory from diagnosis to approaching end of life in patients undergoing hemodialysis in China: a qualitative study. International Journal of Nursing Sciences 2017;4:29–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Bennett PN, Bonner A, Andrew J, et al. . Using images to communicate the hidden struggles of life on dialysis. J Commun Healthc 2013;6:12–21. 10.1179/1753807613Y.0000000031 [DOI] [Google Scholar]
- 198. Costa FG, Coutinho MdaPdeL, Santana IOde. Insuficiência renal crônica: representações sociais de pacientes com e sem depressão. Psico-USF 2014;19:387–98. 10.1590/1413-82712014019003002 [DOI] [Google Scholar]
- 199. Yodchai K, Dunning T, Hutchinson AM, et al. . How do Thai patients with end stage renal disease adapt to being dependent on haemodialysis?: a pilot study. J Ren Care 2011;37:216–23. 10.1111/j.1755-6686.2011.00232.x [DOI] [PubMed] [Google Scholar]
- 200. Arslan SY, Ege E. Sexual experiences of women exposed to hemodialysis treatment. Sex Disabil 2009;27:215–21. 10.1007/s11195-009-9132-1 [DOI] [Google Scholar]
- 201. Tanyi RA, Werner JS, Recine AC, et al. . Perceptions of incorporating spirituality into their care: a phenomenological study of female patients on hemodialysis. Nephrol Nurs J 2006;33:532–8. [PubMed] [Google Scholar]
- 202. Ladin K, Lin N, Hahn E, et al. . Engagement in decision-making and patient satisfaction: a qualitative study of older patients' perceptions of dialysis initiation and modality decisions. Nephrol Dial Transplant 2017;32:gfw307 10.1093/ndt/gfw307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Erlang AS, Nielsen IH, Hansen HO, et al. . Patients experiences of involvement in choice of dialysis mode. J Ren Care 2015;41:260–7. 10.1111/jorc.12141 [DOI] [PubMed] [Google Scholar]
- 204. Moran A, Scott AP, Darbyshire P. Communicating with nurses: patients' views on effective support while on haemodialysis. Nurs Times 2009;105:42146. [PubMed] [Google Scholar]
- 205. Mitchell A, Farrand P, James H, et al. . Patients' experience of transition onto haemodialysis: a qualitative study. J Ren Care 2009;35:99–107. 10.1111/j.1755-6686.2009.00094.x [DOI] [PubMed] [Google Scholar]
- 206. Schober GS, Wenger JB, Lee CC, et al. . Dialysis Patient Perspectives on CKD Advocacy: a semistructured interview Study. Am J Kidney Dis 2017;69:29–40. 10.1053/j.ajkd.2016.06.018 [DOI] [PubMed] [Google Scholar]
- 207. Smith K, Coston M, Glock K, et al. . Patient perspectives on fluid management in chronic hemodialysis. J Ren Nutr 2010;20:334–41. 10.1053/j.jrn.2009.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Pietrovsk V, Dall’Agnol CM. Situações significativas no espaço-contexto da hemodiálise: o que dizem os usuários de um serviço? Rev Bras Enferm 2006;59:630–5. 10.1590/S0034-71672006000500007 [DOI] [PubMed] [Google Scholar]
- 209. Malheiro Oliveira P, Arruda Soares D. Percepciones de las personas con insuficiencia renal crónica sobre la calidad de vida. Enfermería Global 2012;28:257–75. [Google Scholar]
- 210. Beanlands H, Horsburgh ME, Fox S, et al. . Caregiving by family and friends of adults receiving dialysis. Nephrol Nurs J 2005;32:621–31. [PubMed] [Google Scholar]
- 211. Ziegert K, Fridlund B, Lidell E. Health in everyday life among spouses of haemodialysis patients: a content analysis. Scand J Caring Sci 2006;20:223–8. 10.1111/j.1471-6712.2006.00400.x [DOI] [PubMed] [Google Scholar]
- 212. Ziegert K, Fridlund B, Lidell E. "Time for dialysis as time to live": experiences of time in everyday life of the Swedish next of kin of hemodialysis patients. Nurs Health Sci 2009;11:45–50. 10.1111/j.1442-2018.2009.00429.x [DOI] [PubMed] [Google Scholar]
- 213. Ziegert K, Fridlund B. Conceptions of life situation among next-of-kin of haemodialysis patients. J Nurs Manag 2001;9:231–9. 10.1046/j.1365-2834.2001.00233.x [DOI] [PubMed] [Google Scholar]
- 214. Eslami AA, Rabiei L, Abedi HA, et al. . Coping skills of Iranian family careivers in caretaking of patients undergoing haemodialysis: a qualitative study. Journal of renal care 2016;XX(XX):1–10. [DOI] [PubMed] [Google Scholar]
- 215. Taylor F, Gutteridge R, Willis C. Peer support for CKD patients and carers: overcoming barriers and facilitating access. Health Expect 2016;19:617–30. 10.1111/hex.12348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Tavares JM, Lisboa MT, Ferreira MA, et al. . Peritoneal dialysis: family care for chronic kidney disease patients in home-based treatment. Rev Bras Enferm 2016;69:1172–8. [DOI] [PubMed] [Google Scholar]
- 217. Lovink MH, Kars MC, de Man-van Ginkel JM, et al. . Patients’ experiences of safety during haemodialysis treatment - a qualitative study. J Adv Nurs 2015;71:2374–83. 10.1111/jan.12690 [DOI] [PubMed] [Google Scholar]
- 218. Nagpal N, Boutin-Foster C, Melendez J, et al. . Experiences of patients undergoing dialysis who are from ethnic and racial minorities. J Ren Care 2017;43:29–36. 10.1111/jorc.12185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Cramm JM, Leensvaart L, Berghout M, et al. . Exploring views on what is important for patient-centred care in end-stage renal disease using Q methodology. BMC Nephrol 2015;16:74):74 10.1186/s12882-015-0071-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. Namiki S, Rowe J, Cooke M. Living with home-based haemodialysis: insights from older people. J Clin Nurs 2010;19(3-4):547–55. 10.1111/j.1365-2702.2009.02901.x [DOI] [PubMed] [Google Scholar]
- 221. DePasquale N, Ephraim PL, Ameling J, et al. . Selecting renal replacement therapies: what do African American and non-African American patients and their families think others should know? A mixed methods study. BMC Nephrol 2013;14:9 10.1186/1471-2369-14-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Sahaf RP, Sadat Ilali EPS, Peyrovi HP, et al. . Uncertainty, the overbearing lived experience of the elderly people undergoing Hemodialysis: a qualitative study. Int J Community Based Nurs Midwifery 2017;5:13–21. [PMC free article] [PubMed] [Google Scholar]
- 223. Lee A, Gudex C, Povlsen JV, et al. . Patients' views regarding choice of dialysis modality. Nephrol Dial Transplant 2008;23:3953–9. 10.1093/ndt/gfn365 [DOI] [PubMed] [Google Scholar]
- 224. Piccoli GB, Consiglio V, Deagostini MC, et al. . Starting together: a focus group for the organization of a CKD outpatient care unit. Journal of nephrology 2010;23:699–704. [PubMed] [Google Scholar]
- 225. Pilger C, Rampari EM, Waidman MAP, et al. . Hemodialysis: its meaning and impact in the elderly life. Escola Anna Nery - Revista de Enfermagem 2010;14:677–83. [Google Scholar]
- 226. Browne T, Amamoo A, Patzer RE, et al. . Everybody needs a cheerleader to get a kidney transplant: a qualitative study of the patient barriers and facilitators to kidney transplantation in the Southeastern United States. BMC Nephrol 2016;17:108 10.1186/s12882-016-0326-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Hollingdale R, Sutton D, Hart K. Facilitating dietary change in renal disease: investigating patients' perspectives. J Ren Care 2008;34:136–42. 10.1111/j.1755-6686.2008.00034.x [DOI] [PubMed] [Google Scholar]
- 228. Marques FRB, Botelho MR, Marcon SS, et al. . Coping strategies used by family members of individuals receiving hemodialysis. Texto & Contexto - Enfermagem 2014;23:915–24. 10.1590/0104-07072014002220011 [DOI] [Google Scholar]
- 229. Russ AJ, Shim JK, Kaufman SR. "Is there life on dialysis?": time and aging in a clinically sustained existence. Med Anthropol 2005;24:297–324. 10.1080/01459740500330639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. Winterbottom A, Bekker HL, Conner M, et al. . Choosing dialysis modality: decision making in a chronic illness context. Health Expect 2014;17:710–23. 10.1111/j.1369-7625.2012.00798.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. Davison SN. Facilitating advance care planning for patients with end-stage renal disease: the patient perspective. Clin J Am Soc Nephrol 2006;1:1023–8. 10.2215/CJN.01050306 [DOI] [PubMed] [Google Scholar]
- 232. Iles-Smith H. Perceptions and experiences of pre-dialysis patients. Edtna Erca J 2005;31:130–3. 10.1111/j.1755-6686.2005.tb00411.x [DOI] [PubMed] [Google Scholar]
- 233. Wilkinson E, Randhawa G, Brown EA, et al. . Communication as care at end of life: an emerging issue from an exploratory action research study of renal end-of-life care for ethnic minorities in the UK. J Ren Care 2014;40 Suppl 1(S1):23–9. 10.1111/jorc.12084 [DOI] [PubMed] [Google Scholar]
- 234. Campos CJG, Turato ER. The professional health team, the renal patient undergoing hemodialysis and interpersonal relationships. Rev Bras Enferm 2003;56:508–12. [PubMed] [Google Scholar]
- 235. Bailey PK, Ben-Shlomo Y, de Salis I, et al. . Better the donor you know? A qualitative study of renal patients' views on ’altruistic' live-donor kidney transplantation. Soc Sci Med 2016;150:104–11. 10.1016/j.socscimed.2015.12.041 [DOI] [PubMed] [Google Scholar]
- 236. Nygårdh A, Malm D, Wikby K, et al. . The experience of empowerment in the patient-staff encounter: the patient’s perspective. J Clin Nurs 2012;21(5-6):897–904. 10.1111/j.1365-2702.2011.03901.x [DOI] [PubMed] [Google Scholar]
- 237. Tong A, Gow K, Wong G, et al. . Patient perspectives of a young adult renal clinic: a mixed-methods evaluation. Nephrology 2015;20:352–9. 10.1111/nep.12396 [DOI] [PubMed] [Google Scholar]
- 238. Bridger J. Enabling patients with chronic kidney disease to self-care. Journal of Renal Nursing 2009;1:173–8. 10.12968/jorn.2009.1.4.45315 [DOI] [Google Scholar]
- 239. Ghadami A, Memarian R, Mohamadi E, et al. . Patients’ experiences from their received education about the process of kidney transplant: a qualitative study. Iran J Nurs Midwifery Res 2012;17(2 Sup1):157–64. [PMC free article] [PubMed] [Google Scholar]
- 240. Haspeslagh A, De Bondt K, Kuypers D, et al. . Completeness and satisfaction with the education and information received by patients immediately after kidney transplant: a mixed-models study. Prog Transplant 2013;23:12–22. 10.7182/pit2013249 [DOI] [PubMed] [Google Scholar]
- 241. Russell CL, Kilburn E, Conn VS, et al. . Medication-taking beliefs of adult renal transplant recipients. Clin Nurse Spec 2003;17:200–8. 10.1097/00002800-200307000-00018 [DOI] [PubMed] [Google Scholar]
- 242. Urstad KH, Wahl AK, Andersen MH, et al. . Renal recipients' educational experiences in the early post-operative phase–a qualitative study. Scand J Caring Sci 2012;26:635–42. 10.1111/j.1471-6712.2012.00972.x [DOI] [PubMed] [Google Scholar]
- 243. Calestani M, Tonkin-Crine S, Pruthi R, et al. . Patient attitudes towards kidney transplant listing: qualitative findings from the ATTOM study. Nephrol Dial Transplant 2014;29:2144–50. 10.1093/ndt/gfu188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Ros RL, Kucirka LM, Govindan P, et al. . Patient attitudes toward CDC high infectious risk donor kidney transplantation: inferences from focus groups. Clin Transplant 2012;26:247–53. 10.1111/j.1399-0012.2011.01469.x [DOI] [PubMed] [Google Scholar]
- 245. Sheu J, Ephraim PL, Powe NR, et al. . African American and non-African American patients' and families' decision making about renal replacement therapies. Qual Health Res 2012;22:997–1006. 10.1177/1049732312443427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Aasen EM, Kvangarsnes M, Wold B, et al. . The next of kin of older people undergoing haemodialysis: a discursive perspective on perceptions of participation. J Adv Nurs 2012;68:1716–25. 10.1111/j.1365-2648.2011.05854.x [DOI] [PubMed] [Google Scholar]
- 247. EGdR Thomé, Meyer DEE. Women caregivers for men with chronic kidney disease: a cultural approach. Text Context Nursing 2011;20:503–11. [Google Scholar]
- 248. Harwood L, Locking-Cusolito H, Spittal J, et al. . Preparing for hemodialysis: patient stressors and responses. Nephrol Nurs J 2005;32:295–302. [PubMed] [Google Scholar]
- 249. Yodchai K, Dunning T, Savage S, et al. . The role of religion and spirituality in coping with kidney disease and haemodialysis in Thailand. Scand J Caring Sci 2017;31:359–67. 10.1111/scs.12355 [DOI] [PubMed] [Google Scholar]
- 250. Wise M, Schatell D, Klicko K, et al. . Successful daily home hemodialysis patient-care partner dyads: benefits outweigh burdens. Hemodial Int 2010;14:278–88. 10.1111/j.1542-4758.2010.00443.x [DOI] [PubMed] [Google Scholar]
- 251. Calvin AO. Haemodialysis patients and end-of-life decisions: a theory of personal preservation. J Adv Nurs 2004;46:558–66. 10.1111/j.1365-2648.2004.03030.x [DOI] [PubMed] [Google Scholar]
- 252. Bath J, Tonks S, Edwards P. Psychological care of the haemodialysis patient. Edtna Erca J 2003;29:85–8. 10.1111/j.1755-6686.2003.tb00279.x [DOI] [PubMed] [Google Scholar]
- 253. Weil CM. Exploring hope in patients with end stage renal disease on chronic hemodialysis. Nephrol Nurs J 2000;27:219–24. [PubMed] [Google Scholar]
- 254. Wells SA. Occupational deprivation or occupational adaptation of Mexican Americans on renal dialysis. Occup Ther Int 2015;22:174–82. 10.1002/oti.1394 [DOI] [PubMed] [Google Scholar]
- 255. Wilson PM, Reston JD, Bieraugel R, et al. . You cannot choose your family: sociological ambivalence in the hemodialysis unit. Qual Health Res 2015;25:27–39. 10.1177/1049732314549030 [DOI] [PubMed] [Google Scholar]
- 256. Lenci LT, Campbell JD. Peritoneal dialysis in elderly patients. Adv Perit Dial 2012;28:79–83. [PubMed] [Google Scholar]
- 257. Walton J. Prayer warriors: a grounded theory study of American Indians receiving hemodialysis. Nephrol Nurs J 2007;34:377–86. [PubMed] [Google Scholar]
- 258. Walton J. Finding a balance: a grounded theory study of spirituality in hemodialysis patients. Nephrol Nurs J 2002;29:447–56. [PubMed] [Google Scholar]
- 259. BPd S, Schwartz E, Beuter M, et al. . Consequences attributed to kidney transplantation: critical incident technique. Texto & Contexto - Enfermagem 2015;24:748–55. [Google Scholar]
- 260. Ravenscroft EF. Diabetes and kidney failure: how individuals with diabetes experience kidney failure. Nephrol Nurs J 2005;32:502–10. [Google Scholar]
- 261. Williams AF, Manias E, Walker R. The role of irrational thought in medicine adherence: people with diabetic kidney disease. J Adv Nurs 2009;65:2108–17. 10.1111/j.1365-2648.2009.05077.x [DOI] [PubMed] [Google Scholar]
- 262. Bäckström-Andersson H, Lindberg B, Lindström R. Dry weight from the haemodialysis patient perspective. Renal Society of Australasia Journal 2013;9:68–73. [Google Scholar]
- 263. Vestman C, Hasselroth M, Berglund M. Freedom and confinement: Patients’ experiences of life with home haemodialysis. Nurs Res Pract 2014;2014:1–7. 10.1155/2014/252643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264. Curtin RB, Mapes D, Petillo M, et al. . Long-term dialysis survivors: a transformational experience. Qual Health Res 2002;12:609–24. 10.1177/104973202129120133 [DOI] [PubMed] [Google Scholar]
- 265. Curtin RB, Mapes DL. Health care management strategies of long-term dialysis survivors. Nephrol Nurs J 2001;28:385–92. [PubMed] [Google Scholar]
- 266. Lederer S, Fischer MJ, Gordon HS, et al. . Barriers to effective communication between veterans with chronic kidney disease and their healthcare providers. Clin Kidney J 2015;8:766–71. 10.1093/ckj/sfv079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267. McKillop G, Joy J. Patients' experience and perceptions of polypharmacy in chronic kidney disease and its impact on adherent behaviour. J Ren Care 2013;39:200–7. 10.1111/j.1755-6686.2013.12037.x [DOI] [PubMed] [Google Scholar]
- 268. Reid K, Morris M, Cormack M, et al. . Exploring the process of adjusting to diabetic kidney disease. J Ren Care 2012;38 Suppl 1:30–9. 10.1111/j.1755-6686.2012.00278.x [DOI] [PubMed] [Google Scholar]
- 269. Ladin K, Buttafarro K, Hahn E, et al. . "End-of-life care? I’m not going to worry about that yet." Health literacy gaps and end-of-life planning among elderly dialysis patients. Gerontologist 2017;00:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270. Harwood L, Clark AM. Dialysis modality decision-making for older adults with chronic kidney disease. J Clin Nurs 2014;23(23-24):3378–90. 10.1111/jocn.12582 [DOI] [PubMed] [Google Scholar]
- 271. Llewellyn H, Low J, Smith G, et al. . Narratives of continuity among older people with late stage chronic kidney disease who decline dialysis. Soc Sci Med 2014;114:49–56. 10.1016/j.socscimed.2014.05.037 [DOI] [PubMed] [Google Scholar]
- 272. Schell JO, Patel UD, Steinhauser KE, et al. . Discussions of the kidney disease trajectory by elderly patients and nephrologists: a qualitative study. Am J Kidney Dis 2012;59:495–503. 10.1053/j.ajkd.2011.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Walker RC, Morton RL, Tong A, et al. . Patient and caregiver preferences for home dialysis–the home first study: a protocol for qualitative interviews and discrete choice experiments. BMJ Open 2015;5:e007405 10.1136/bmjopen-2014-007405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Landreneau K, Ward-Smith P. Patients' perceptions concerning choice among renal replacement therapies: a pilot study. Nephrol Nurs J 2006;33:397–402. [PubMed] [Google Scholar]
- 275. Shaw R. Being-in-dialysis: The experience of the machine-body for home dialysis users. Health 2015;19:229–44. 10.1177/1363459314539775 [DOI] [PubMed] [Google Scholar]
- 276. Visser A, Dijkstra GJ, Kuiper D, et al. . Accepting or declining dialysis: considerations taken into account by elderly patients with end-stage renal disease. J Nephrol 2009;22:794–9. [PubMed] [Google Scholar]
- 277. de Rosenroll A, Higuchi KS, Dutton KS, et al. . Perspectives of significant others in dialysis modality decision-making: a qualitative study. Cannt J 2013;23:17–24. [PubMed] [Google Scholar]
- 278. Landreneau KJ, Ward-Smith P. Perceptions of adult patients on hemodialysis concerning choice among renal replacement therapies. Nephrol Nurs J 2007;34:513–9. [PubMed] [Google Scholar]
- 279. Cases A, Dempster M, Davies M, et al. . The experience of individuals with renal failure participating in home haemodialysis: an interpretative phenomenological analysis. J Health Psychol 2011;16:884–94. 10.1177/1359105310393541 [DOI] [PubMed] [Google Scholar]
- 280. Lindsay H, MacGregor C, Fry M. The experience of living with chronic illness for the haemodialysis patient: an interpretative phenomenological analysis. Health Sociology Review 2014;23:232–41. 10.1080/14461242.2014.11081976 [DOI] [Google Scholar]
- 281. Darrell L. Faith that God cares: the experience of spirituality with African American hemodialysis patients. Social Work & Christianity 2016;43:189–212. [Google Scholar]
- 282. Hagren B, Pettersen I-M, Severinsson E, et al. . The haemodialysis machine as a lifeline: experiences of suffering from end-stage renal disease. J Adv Nurs 2001;34:196–202. 10.1046/j.1365-2648.2001.01745.x [DOI] [PubMed] [Google Scholar]
- 283. Harrington J, Morgan M. Understanding kidney transplant patients' treatment choices: the interaction of emotion with medical and social influences on risk preferences. Soc Sci Med 2016;155:43–50. 10.1016/j.socscimed.2016.02.027 [DOI] [PubMed] [Google Scholar]
- 284. Herlin C, Wann-Hansson C. The experience of being 30-45 years of age and depending on haemodialysis treatment: a phenomenological study. Scand J Caring Sci 2010;24:693–9. 10.1111/j.1471-6712.2009.00764.x [DOI] [PubMed] [Google Scholar]
- 285. Lewis H, Arber S. The role of the body in end-stage kidney disease in young adults: Gender, peer and intimate relationships. Chronic Illn 2015;11:184–97. 10.1177/1742395314566823 [DOI] [PubMed] [Google Scholar]
- 286. Pelletier-Hibbert M, Sohi P. Sources of uncertainty and coping strategies used by family members of individuals living with end stage renal disease. Nephrol Nurs J 2001;28:411–9. [PubMed] [Google Scholar]
- 287. Aasen EM. A comparison of the discursive practices of perception of patient participation in haemodialysis units. Nurs Ethics 2015;22:341–51. 10.1177/0969733014533240 [DOI] [PubMed] [Google Scholar]
- 288. Goff SL, Eneanya ND, Feinberg R, et al. . Advance care planning: a qualitative study of dialysis patients and families. Clin J Am Soc Nephrol 2015;10:390–400. 10.2215/CJN.07490714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289. Nygårdh A, Wikby K, Malm D, et al. . Empowerment in outpatient care for patients with chronic kidney disease - from the family member’s perspective. BMC Nurs 2011;10:21 10.1186/1472-6955-10-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290. Hutchison LA, Raffin-Bouchal DS, Syme CA, et al. . Readiness to participate in advance care planning: a qualitative study of renal failure patients, families and healthcare providers. Chronic Illn 2017;13:171–87. 10.1177/1742395316675023 [DOI] [PubMed] [Google Scholar]
- 291. Davison SN, Simpson C. Hope and advance care planning in patients with end stage renal disease: qualitative interview study. BMJ 2006;333:886 10.1136/bmj.38965.626250.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292. Calvin AO, Engebretson JC, Sardual SA. Understanding of advance care planning by family members of persons undergoing hemodialysis. West J Nurs Res 2014;36:1357–73. 10.1177/0193945913514637 [DOI] [PubMed] [Google Scholar]
- 293. Noble H, Meyer J, Bridges J, et al. . Reasons renal patients give for deciding not to dialyze: a prospective qualitative interview study. Dial Transplant 2009;38:82–9. 10.1002/dat.20288 [DOI] [Google Scholar]
- 294. Molzahn A, Sheilds L, Bruce A, et al. . Perceptions regarding death and dying of individuals with chronic kidney disease. Nephrol Nurs J 2012;39:197–204. [PubMed] [Google Scholar]
- 295. Casey JR, Hanson CS, Winkelmayer WC, et al. . Patients' perspectives on hemodialysis vascular access: a systematic review of qualitative studies. Am J Kidney Dis 2014;64:937–53. 10.1053/j.ajkd.2014.06.024 [DOI] [PubMed] [Google Scholar]
- 296. Jamieson NJ, Hanson CS, Josephson MA, et al. . Motivations, challenges, and attitudes to self-management in kidney transplant recipients: a Systematic review of qualitative studies. Am J Kidney Dis 2016;67:461–78. 10.1053/j.ajkd.2015.07.030 [DOI] [PubMed] [Google Scholar]
- 297. Palmer SC, Hanson CS, Craig JC, et al. . Dietary and fluid restrictions in CKD: a thematic synthesis of patient views from qualitative studies. Am J Kidney Dis 2015;65:559–73. 10.1053/j.ajkd.2014.09.012 [DOI] [PubMed] [Google Scholar]
- 298. Ralph A, Chapman JR, Gillis J, et al. . Family perspectives on deceased organ donation: thematic synthesis of qualitative studies. Am J Transplant 2014;14:923–35. 10.1111/ajt.12660 [DOI] [PubMed] [Google Scholar]
- 299. Tong A, Brown MA, Winkelmayer WC, et al. . Perspectives on pregnancy in women with ckd: a semistructured interview study. Am J Kidney Dis 2015;66:951–61. 10.1053/j.ajkd.2015.08.023 [DOI] [PubMed] [Google Scholar]
- 300. Tong A, Chapman JR, Wong G, et al. . The experiences of commercial kidney donors: thematic synthesis of qualitative research. Transpl Int 2012;25:1138–49. 10.1111/j.1432-2277.2012.01534.x [DOI] [PubMed] [Google Scholar]
- 301. Tong A, Cheung KL, Nair SS, et al. . Thematic synthesis of qualitative studies on patient and caregiver perspectives on end-of-life care in CKD. Am J Kidney Dis 2014;63:913–27. 10.1053/j.ajkd.2013.11.017 [DOI] [PubMed] [Google Scholar]
- 302. Tong A, Jesudason S, Craig JC, et al. . Perspectives on pregnancy in women with chronic kidney disease: systematic review of qualitative studies. Nephrol Dial Transplant 2015;30:652–61. 10.1093/ndt/gfu378 [DOI] [PubMed] [Google Scholar]
- 303. Tong A, Lowe A, Sainsbury P, et al. . Experiences of parents who have children with chronic kidney disease: a systematic review of qualitative studies. Pediatrics 2008;121:349–60. 10.1542/peds.2006-3470 [DOI] [PubMed] [Google Scholar]
- 304. Tong A, Rangan GK, Ruospo M, et al. . A painful inheritance-patient perspectives on living with polycystic kidney disease: thematic synthesis of qualitative research. Nephrol Dial Transplant 2015;30:790–800. 10.1093/ndt/gfv010 [DOI] [PubMed] [Google Scholar]
- 305. Walker RC, Hanson CS, Palmer SC, et al. . Patient and caregiver perspectives on home hemodialysis: a systematic review. Am J Kidney Dis 2015;65:451–63. 10.1053/j.ajkd.2014.10.020 [DOI] [PubMed] [Google Scholar]
- 306. Tong A, Hanson CS, Chapman JR, et al. . ’Suspended in a paradox'-patient attitudes to wait-listing for kidney transplantation: systematic review and thematic synthesis of qualitative studies. Transpl Int 2015;28:771–87. 10.1111/tri.12575 [DOI] [PubMed] [Google Scholar]
- 307. Bailey P, Tomson C, Risdale S, et al. . From potential donor to actual donation: does socioeconomic position affect living kidney donation? A systematic review of the evidence. Transplantation 2014;98:918–26. 10.1097/TP.0000000000000428 [DOI] [PubMed] [Google Scholar]
- 308. Reid C, Seymour J, Jones C. A thematic synthesis of the experiences of adults living with hemodialysis. Clin J Am Soc Nephrol 2016;11:1206–18. 10.2215/CJN.10561015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309. Arokiasamy P, Uttamacharya U, Jain K, et al. . The impact of multimorbidity on adult physical and mental health in low- and middle-income countries: what does the study on global ageing and adult health (SAGE) reveal? BMC Med 2015;13:178 10.1186/s12916-015-0402-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310. Kim TJ, Vonneilich N, Lüdecke D, et al. . Income, financial barriers to health care and public health expenditure: a multilevel analysis of 28 countries. Soc Sci Med 2017;176:158–65. 10.1016/j.socscimed.2017.01.044 [DOI] [PubMed] [Google Scholar]
- 311. Mackenbach JP, Looman CWN, Artnik B, et al. . ’Fundamental causes' of inequalities in mortality: an empirical test of the theory in 20 European populations. Sociol Health Illn 2017;39:1117–33. 10.1111/1467-9566.12562 [DOI] [PubMed] [Google Scholar]
- 312. Prasad N, Jha V. Hemodialysis in Asia. Kidney Dis 2015;1:165–77. 10.1159/000441816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313. Rajapurkar MM, John GT, Kirpalani AL, et al. . What do we know about chronic kidney disease in India: first report of the Indian CKD registry. BMC Nephrol 2012;13:10 10.1186/1471-2369-13-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314. Obrador GT, Rubilar X, Agazzi E, et al. . The challenge of providing renal replacement therapy in developing countries: the latin American perspective. Am J Kidney Dis 2016;67:499–506. 10.1053/j.ajkd.2015.08.033 [DOI] [PubMed] [Google Scholar]
- 315. Mackenbach JP. The persistence of health inequalities in modern welfare states: the explanation of a paradox. Soc Sci Med 2012;75:761–9. 10.1016/j.socscimed.2012.02.031 [DOI] [PubMed] [Google Scholar]
- 316. Rodriguez RA. Dialysis for undocumented immigrants in the United States. Adv Chronic Kidney Dis 2015;22:60–5. 10.1053/j.ackd.2014.07.003 [DOI] [PubMed] [Google Scholar]
- 317. Pavli A, Maltezou H. Health problems of newly arrived migrants and refugees in Europe. J Travel Med 2017;24 10.1093/jtm/tax016 [DOI] [PubMed] [Google Scholar]
- 318. Matesanz R, Marazuela R, Domínguez-Gil B, et al. . The 40 donors per million population plan: an action plan for improvement of organ donation and transplantation in Spain. Transplant Proc 2009;41:3453–6. 10.1016/j.transproceed.2009.09.011 [DOI] [PubMed] [Google Scholar]
- 319. Acevedo-Garcia D, Almeida J. Special issue introduction: place, migration and health. Soc Sci Med 2012;75:2055–9. 10.1016/j.socscimed.2012.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320. Terasaki G, Ahrenholz NC, Haider MZ. Care of adult refugees with chronic conditions. Med Clin North Am 2015;99:1039–58. 10.1016/j.mcna.2015.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321. Van Biesen W, Vanholder R, Ernandez T, et al. . Caring for migrants and refugees with end-stage kidney disease in Europe. Am J Kidney Dis 2018;71:701–9. 10.1053/j.ajkd.2017.10.015 [DOI] [PubMed] [Google Scholar]
- 322. Raghavan R. Caring for Undocumented Immigrants With Kidney Disease. Am J Kidney Dis 2018;71:488–94. 10.1053/j.ajkd.2017.09.011 [DOI] [PubMed] [Google Scholar]
- 323. Wild V, Dawson A. Migration: a core public health ethics issue. Public Health 2018;158:66–70. 10.1016/j.puhe.2018.02.023 [DOI] [PubMed] [Google Scholar]
- 324. Luyckx VA, Miljeteig I, Ejigu AM, et al. . Ethical Challenges in the Provision of Dialysis in Resource-Constrained Environments. Semin Nephrol 2017;37:273–86. 10.1016/j.semnephrol.2017.02.007 [DOI] [PubMed] [Google Scholar]
- 325. Qazi HA, Chen H, Zhu M. Factors influencing dialysis withdrawal: a scoping review. BMC Nephrol 2018;19:96 10.1186/s12882-018-0894-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326. EdCL C, TPd C, Carvalho CC, et al. . Associação entre bem-estar espiritual e autoestima em pessoas com insuficiência renal crônica em hemodiálise. Psicologia: Reflexão e Crítica 2015;28:737–43. [Google Scholar]
- 327. Cruz JP, Colet PC, Alquwez N, et al. . Influence of religiosity and spiritual coping on health-related quality of life in Saudi haemodialysis patients. Hemodial Int 2017;21:125–32. 10.1111/hdi.12441 [DOI] [PubMed] [Google Scholar]
- 328. Saisunantararom W, Cheawchanwattana A, Kanjanabuch T, et al. . Associations among spirituality, health-related quality of life, and depression in pre-dialysis chronic kidney disease patients: An exploratory analysis in thai buddhist patients. Religions 2015;6:1249–62. 10.3390/rel6041249 [DOI] [Google Scholar]
- 329. Lucchetti G, Almeida LG, Granero AL. [Spirituality for dialysis patients: should the nephrologist address?]. J Bras Nefrol 2010;32:126–30. [PubMed] [Google Scholar]
- 330. Dwarswaard J, Bakker EJ, van Staa A, et al. . Self-management support from the perspective of patients with a chronic condition: a thematic synthesis of qualitative studies. Health Expect 2016;19:194–208. 10.1111/hex.12346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331. Morton RL, Tong A, Howard K, et al. . The views of patients and carers in treatment decision making for chronic kidney disease: systematic review and thematic synthesis of qualitative studies. BMJ 2010;340:c112 10.1136/bmj.c112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332. Shommu NS, Ahmed S, Rumana N, et al. . What is the scope of improving immigrant and ethnic minority healthcare using community navigators: a systematic scoping review. Int J Equity Health 2016;15:6 10.1186/s12939-016-0298-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333. Boehmer KR, Shippee ND, Beebe TJ, et al. . Pursuing minimally disruptive medicine: disruption from illness and health care-related demands is correlated with patient capacity. J Clin Epidemiol 2016;74:227–36. 10.1016/j.jclinepi.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 334. Jha V, Garcia-Garcia G, Iseki K, et al. . Chronic kidney disease: global dimension and perspectives. Lancet 2013;382:260–72. 10.1016/S0140-6736(13)60687-X [DOI] [PubMed] [Google Scholar]
- 335. Rosenzveig A, Kuspinar A, Daskalopoulou SS, et al. . Toward patient-centered care: a systematic review of how to ask questions that matter to patients. Medicine 2014;93:e120 10.1097/MD.0000000000000120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336. Nugent RA, Fathima SF, Feigl AB, et al. . The burden of chronic kidney disease on developing nations: a 21st century challenge in global health. Nephron Clin Pract 2011;118:c269–c277. 10.1159/000321382 [DOI] [PubMed] [Google Scholar]
- 337. Garcia-Garcia G, Jha V. World Kidney Day Steering C. Chronic kidney disease in disadvantaged populations. Transplantation 2015;99:13–16. [DOI] [PubMed] [Google Scholar]
- 338. Silva AS, Silveira RS, Fernandes GF, et al. . [Perceptions and changes in the quality of life of patients submitted to hemodyalisis]. Rev Bras Enferm 2011;64:839–44. [DOI] [PubMed] [Google Scholar]
- 339. Gullick J, Monaro S, Stewart G. Compartmentalising time and space: a phenomenological interpretation of the temporal experience of commencing haemodialysis. J Clin Nurs 2017;26:3382–95. 10.1111/jocn.13697 [DOI] [PubMed] [Google Scholar]
- 340. Kaba E, Bellou P, Iordanou P, et al. . Problems experienced by haemodialysis patients in Greece. Br J Nurs 2007;16:868–72. 10.12968/bjon.2007.16.14.24325 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-023507supp001.pdf (21.9KB, pdf)