Abstract
Objective:
CBT and SSRIs are effective treatments for pediatric anxiety disorders. However, the mechanisms of these treatments are unknown. Previous research indicated that somatic symptoms are reduced following treatment, but it is unclear if their reductions are merely a consequence of treatment gains. This study examined reductions in somatic symptoms as a potential mediator of the relationship between treatment and anxiety outcomes.
Method:
Participants were 488 anxious youth ages 7–17 (M=10.7), 50.4% male, 78.9% Caucasian, enrolled in Child/Adolescent Anxiety Multimodal Study (CAMS), a large randomized control trial comparing 12-week treatments of cognitive behavioral therapy (CBT), sertraline (SRT), a combination of CBT and sertraline (COMB), and a pill placebo (PBO). Causal mediation models were tested in R using data from baseline, 8-, and 12-week evaluations. Somatic symptoms were assessed using the Panic/Somatic subscale from the Screen for Child Anxiety Related Emotional Disorders (SCARED-P/C). Youth outcomes were assessed using the Pediatric Anxiety Rating Scale (PARS) and Children’s Global Assessment Scale (CGAS).
Results:
Reductions in somatic symptoms mediated improvement in anxiety symptoms and global functioning for those in the sertraline-only condition based on parent report. Conditions involving CBT and data based on child reported somatic symptoms did not show a mediation effect.
Conclusions:
Findings indicate that reductions in somatic symptoms may be a mediator of improvements for treatments including pharmacotherapy and not CBT. Although the overall efficacy of sertraline and CBT for anxiety may be similar, the treatments appear to function via different mechanisms.
Keywords: anxiety, somatic symptoms, mediators, CBT, pharmacotherapy
Anxiety disorders are among the most common psychiatric conditions in children and adolescents (Costello, Egger, & Angold, 2004; Velting, Setzer, & Albano, 2002). The multitude of anxiety’s negative effects on youth has been well established, with impairment documented across academic, social, and familial domains of functioning (Hughes, Hedtke, & Kendall, 2008; Mazzone et al., 2007; Muroff & Ross, 2011; Swan & Kendall, 2016). In addition, anxiety disorders are related to physical well-being for many affected youth. Models of anxiety emphasize the role of physiological arousal and catastrophic interpretations of somatic symptoms in the development and maintenance of anxiety (Clark & Watson, 1991; see Domschke, Stevens, Pfleiderer, & Gerlach, 2010 and Kerstner, et al., 2015 for examples), and somatic symptoms are part of the diagnostic criteria of many anxiety disorders. Among anxious youth, 50–95% report somatic complaints including headaches, abdominal pain, shortness of breath, sweating, racing heart, fatigue, and other symptoms (Crawley et al., 2014; Ginsburg, Riddle, & Davies, 2006; Hofflich, Hughes, & Kendall, 2006). Somatic symptoms have been associated with a range of academic, social, and intrapersonal difficulties (Campo, 2012) as well as with lower global functioning (Crawley et al., 2014; Ginsburg et al., 2006; Hofflich et al., 2006; Storch et al., 2008).
In addition to being associated with greater impairment in anxious youth, somatic symptoms are related to treatment outcomes. In one study, higher pre-treatment somatic symptoms were associated with less anxiety improvement (Crawley et al., 2014) and reductions in somatic symptoms have been associated with decreases in overall anxiety (Crawley et al., 2014; Ginsburg et al., 2006). In a cognitive behavioral treatment (CBT) that targeted both cognitive and somatic symptoms, Masia Warner and colleagues (2011) found that reductions in somatic symptoms (as measured by the Children’s Somatization Inventory; Garber, Walker, & Zeman, 1991) were positively related to reductions in anxiety symptoms. Thus, it appears that when treatments are efficacious somatic symptoms decrease. It is unclear, however, whether this change in somatic symptoms is a mediator (i.e. accounts for the relationship between variables of interest) or simply a correlate of overall reductions in anxiety. Somatic symptoms have not been found to moderate treatment response for anxiety (Compton et al., 2014; Crawley et al., 2014).
Attention to the role of somatic symptoms in treatment is relatively new: in Chu and Harrison’s (2007) meta-analysis of potential mediators of change, only three of the anxiety studies reviewed reported specifically on physiological measures. Most studies measured somatic symptoms alongside other anxiety outcomes so the temporal nature of the relationship between somatic symptoms and anxiety treatment is unclear. This situation is of note because hypothesized mechanisms of change must be measured before outcomes (Hayes, Laurenceau, Feldman, Strauss, & Cardaciotto, 2007). Although somatic symptoms are theorized to be an important part of anxiety that can be treated (most CBT protocols include psychoeducation about somatic symptoms and relaxation exercises to reduce somatic symptoms), there is little data examining this issue.
A better understanding of treatment mediators—for both CBT and medication – could facilitate improved efficacy and efficiency by increasing active ingredients, dropping elements that do not contribute to change, and/or target treatments specifically to those who may benefit more from specific elements (Kazdin, 2007). Research on mediators could inform our understanding of mechanisms of change and refine interventions, leading to more effective treatments (Silverman & Hinshaw, 2008). This should be an important goal in pediatric anxiety given the challenges of significant numbers of non-responders to acute treatment, and relapse rates post-intervention (Ginsburg et al., 2014).
Although CBT is the most-researched treatment for anxiety, little is known about how it works. Numerous scholars have called for greater exploration into its mediators and mechanisms of change (Chu & Harrison, 2007; Hudson, 2005; Kendall & Treadwell, 2007; Seligman & Ollendick, 2011; Silverman, Pina, & Viswesvaran, 2008), but few studies have examined mediators of CBT outcomes in anxious children and adolescents. For example, studies have examined and found support for changes in anxious self-talk as a significant mediator of reduced anxiety (Kendall et al., 2016; Kendall & Treadwell, 2007; Treadwell & Kendall, 1996); other mediators include self-efficacy (e.g., Maric, Heyne, MacKinnon, van Widenfelt, & Westenberg, 2013), coping (Kendall et al, 2016; Lau, Chan, Li, & Au, 2010), therapeutic relationship (Cummings et al., 2013), and decreases in loneliness (Alfano et al., 2009). Given CBT’s emphasis on changing cognitions and behaviors these findings are important, but other mediators should be considered (Muris, Mayer, den Adel, Roos, & van Wamelen, 2008).
According to the tripartite model, high physiological arousal (e.g. racing heart, dizziness, shortness of breath, sweating) is a key component of anxiety (Clark & Watson, 1991). The reciprocal activation of the sympathetic nervous system and deactivation of the parasympathetic system influences heartrate, breathing, and other aspects of physiology (Edgar, Keller, Heller, & Miller, 2007; Kreibig, 2010). Research suggests that anxious individuals may be particularly sensitive to sensations of physiological arousal so that they not only experience physiological arousal but interpret it as more threatening (Anderson & Hope, 2009; Domschke et al., 2010; Eley, Stirling, Ehlers, Gregory, & Clark, 2004; Joiner et al., 1999). Given the apparent relationships between somatic symptoms and treatment outcomes, their conceptual role as part of the tripartite model of anxiety, and the fact that these are targets of CBT, it seems reasonable to hypothesize that reductions in somatic symptoms could mediate treatment response.
Similarly, research supports the efficacy of the selective serotonin reuptake inhibitors ((SSRIs); Rynn, Siqueland, & Rickels, 2001; Walkup et al., 2001, 2008) and mixed reuptake inhibitors (March et al., 2007; Strawn, Welge, Wehry, Keeshin, & Rynn, 2015). As with CBT, however, few mediators have been identified (Walkup et al., 2003). Current theories suggest both SSRIs and CBT may exert their effects via changes in the functional activity of the brain’s fear networks (Strawn, Wehry, DelBello, Rynn, & Strakowski, 2012), but no clinical linkages between neural mechanisms of change to reductions somatic symptoms have been examined in anxious youth.
Although research has indicated that CBT and sertraline are similarly efficacious in overall response rates for treating anxiety and a combination of the two is even more effective (Walkup et al., 2008), little is known about how and why they work. Within the adult anxiety treatment literature, research suggests that different treatments have disparate mechanisms of action (Donegan & Dugas, 2012; Quidé, Witteveen, El-Hage, Veltman, & Olff, 2012), but the nuances of these differences are still unknown. Some research suggests that medication may act specifically via changes in fear circuitry activation (Strawn et al., 2012) – which in turn presumably reduces individuals’ experience of arousal (e.g. heart beating quickly, breathing quickly). Thus, medication may offer a relatively simple explanation for how change takes place, in contrast to CBT’s multiple theorized reasons for its effectiveness (e.g., cognitions and reductions in somatic symptoms, therapeutic alliance, etc.).
The current study’s research questions were twofold and examined: 1) whether reductions in somatic symptoms mediated treatment outcomes among anxious youth and 2) if so, whether the role of somatic symptoms in mediating treatment outcomes varied by treatment condition. Based on the literature reviewed above, we hypothesized that reductions in somatic symptoms would be a mediator in the pathway from baseline to end of treatment, and that the role of somatic symptoms in mediating treatment outcomes and the indirect effects would be strongest in the treatment conditions containing active medication.
Methods
Participants
Participants were the 488 children and adolescents 7–17 years old who participated in the multi-site Child/Adolescent Anxiety Multimodal Study (CAMS). Inclusion criteria required that all participants meet DSM-IV criteria for separation anxiety disorder (SAD), generalized anxiety disorder (GAD), and/or social phobia (SoP). The age of participants was selected to represent the broadest age range possible while relying on previously validated measures. Participants were recruited across six different primarily urban study sites (New York, NY; Philadelphia, PA; Baltimore, MD; Durham, SC; Los Angeles, CA; Pittsburgh, PA) via advertisements and referrals to university-based clinics. Exclusionary criteria for the study included 1) prior failed CBT trial or 2) failed selective serotonin reuptake inhibitor (SSRI) trials for anxiety, as well as the presence of any comorbid mood, psychotic, or pervasive developmental disorder. Detailed demographic and diagnostic information regarding participants can be found in Compton et al. (2010), Kendall et al. (2010) and Walkup et al. (2008).
Procedures
Enrollment in the study required a three-stage screening process including a preliminary phone screen, a diagnostic evaluation and physical exam to ensure eligibility, and a final baseline assessment to obtain pre-treatment ratings on all measures. IRB approval was obtained from each site, and participants and at least one parent provided written informed consent prior to entering the study. Participants were compensated for time and travel according to local IRB guidelines. Eligible participants were randomized into CBT (Coping Cat), medication (sertraline; SRT), a combination of CBT and medication (COMB), and a pill placebo. CAMS included 12 weeks of acute treatment, with data regarding somatic symptoms gathered at baseline, mid-treatment (Weeks 4 and 8) and post-treatment (Week 12). Evaluations of outcomes were completed by independent evaluators (IEs) masked to treatment assignment.
Content of treatment included a CBT protocol (the Coping Cat manual) or a fixed-flexible dosing schedule for sertraline. The CBT treatment included 14 60-minute sessions, including two possible parent sessions. Somatic symptoms were introduced in Session 3 and relaxation skills in Session 5, followed by a multi-session focus on cognitive restructuring and exposure. The fixed-flexible dosing schedule allowed dosing changes based on clinical response and tolerability. Participants were initially prescribed 25 mg per day and doses were increased by 25 mg based on response and side effects, with a maximum dose of 200 mg daily. Almost all participants in the SRT or COMB conditions received ≤50 mg of sertraline before Week 4, with most reaching ≥100 mg after that time.
Measures
Treatment outcomes.
To parallel the CAMS primary outcomes paper, two treatment outcomes were selected including:
Pediatric Anxiety Rating Scale (PARS; Research Units on Pediatric Psychopharmacology (RUPP) Anxiety Study Group, 2002).
The PARS is a clinician-administered measure of anxiety symptoms within the past week with a total score ranging from 0–30. In CAMS, six items were summed reflecting anxiety severity, frequency, distress, avoidance, and interference inside and outside the home over the previous week. Items were rated on a scale of 0–5, with higher scores indicating greater severity and totals >13 indicating clinically significant anxiety. Previously, the PARS demonstrated acceptable internal consistency (α = 0.64), strong interrater reliability (r = .97), moderate retest reliability (r = .55), and expected correlations with validity indicators (see Ginsburg, Keeton, Drazdowski, & Riddle, 2011; Research Units on Pediatric Psychopharmacology Anxiety Study Group, 2002). The PARS’ inter-rater reliability for anxiety severity in this sample was high (r = .85) and intraclass correlation coefficients at baseline were .69.
Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983).
The CGAS is a measure of global functioning over the previous week. CGAS scores range from 1 to 100, with scores >70 indicating superior functioning, scores <60 indicating a need for treatment, and ratings ≤50 indicating moderate impairment. The CGAS has acceptable psychometric properties, with previous studies finding interrater reliabilities of r = .73 −.85 (Green, Shirk, Hanze, & Wanstrath, 1994; Lundh, Kowalski, Sundberg, Gumpert, & Landén, 2010).
Potential mediator: Somatic symptoms.
Screen for Child Anxiety Related Emotional Disorders (SCARED-P/C; Birmaher et al., 1997, 1999).
The SCARED is a 41-item measure completed by parent and child of the child’s anxiety symptoms rated on a 3-point scale: 0 - Not True or Hardly Ever True, 1- Somewhat True or Sometimes True and 2 - Very True or Often True. This study utilized the 13-item Panic/Somatic subscale which includes statements such as, “When I feel frightened, it is hard to breathe,” “When I get frightened, I feel like passing out,” and “When I get frightened, I feel like throwing up.” A score of 7 or higher on the Panic/Somatic subscale indicates clinically significant anxiety and somatic symptoms. The SCARED has been used widely in many settings and has strong psychometric properties (Hale, Raaijmakers, Muris, & Meeus, 2005; Wren, Bridge, & Birmaher, 2004). In this sample the SCARED-P/C’s panic/somatic subscale had Cronbach’s alphas of .84 and .87 for the child and parent reports respectively. Pairwise correlations indicated that parent and child reports were positively correlated (r =.45, p <.01).
Statistical analysis
Analysis of variance (ANOVA) and χ2 tests were used to detect any baseline differences across randomized treatment groups as well as between completers and non-completers. To answer the research questions, causal mediation models (Imai, Keele, & Tingley, 2010) were used to determine if somatic symptoms at Week 8 mediated treatment effects on two treatment outcomes: anxiety symptoms (PARS) and global functioning (CGAS), both at Week 12 (Figure 1). The analytic approach utilized a quasi-Bayesian Monte Carlo approximation to estimate direct, indirect and total effects, and provided their corresponding 95% CI and p-values (for details regarding mathematical theorems and proofs, as well as estimation algorithms, see Imai et al. 2010). Week 8 was chosen as the mid-treatment mediator time point because CBT and COMB participants did not have relaxation-focused sessions until Week 5, and participants in the SRT and COMB conditions were still titrating up to their full doses at Week 4 (the other potential mid-treatment time point). Using Week 8 as the mid-treatment point ensured that participants in all active treatment groups had time to benefit from these interventions by engaging in CBT and/or receiving SRT dose adjustment. The primary somatic symptom measure was the Panic/Somatic subscale of the SCARED-P and the treatment outcome measures were the PARS for anxiety symptoms and CGAS for global functioning. Hence completers were subjects with baseline and Week 8 SCARED-P, and baseline and Week 12 PARS and CGAS. To explore the effect of differences between parent and child somatic symptoms reporting on the above causal mediation models, the SCARED-C Panic/Somatic subscale was used as a secondary mediator measure. The R package mediation was used to conduct all causal mediation analyses (Tingley, Yamamoto, Hirose, Keele, & Imai, 2014).
Figure 1: Diagram of Causal Mediation Models.
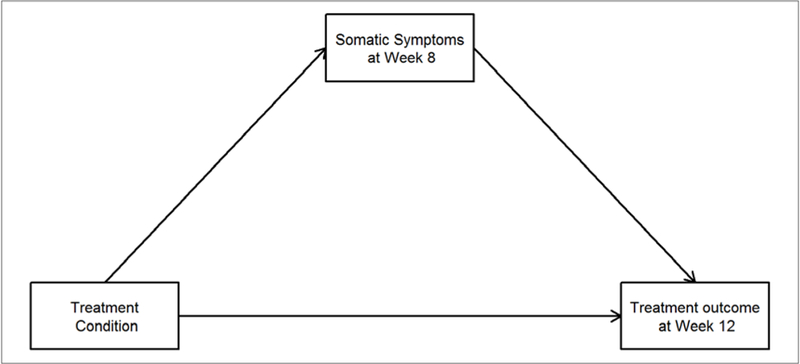
Note: Four treatment conditions include medication (SRT), cognitive behavioral therapy (CBT), combination of CBT and medication (COMB), and placebo. Somatic symptoms reported by parent and child using the SCARED Panic/Somatic subscale. Two treatment outcomes (one for each model): anxiety symptoms (PARS) and global functioning (CGAS) rated by independent evaluator. Both models controlled for child demographics, baseline somatic symptoms and anxiety symptoms/global functioning.
For each treatment outcome measure (PARS and CGAS), causal mediation analysis was carried out in three steps and results from each step determined if the analysis should continue to subsequent steps. First, analysis of covariance (ANCOVA) was used to test if treatment conditions resulted in different outcomes (without adjusting for mediator). If there was a significant treatment effect, then in step 2 another ANCOVA was used to test if treatment conditions were associated with the mediator. Only after a treatment effect was detected on both outcome and mediator, a third ANCOVA was conducted in step 3. In this ANCOVA, both baseline treatment conditions and mid-treatment mediator were included, and three post-hoc contrast tests were used to determine whether the mediator was significant for any/which of the three active conditions: SRT, CBT, COMB, compared with placebo. All causal mediation models controlled for child demographics (gender, age and race), baseline somatic symptoms (SCARED-P/C), anxiety symptoms (PARS), and/or global functioning (CGAS).
Results
Descriptive statistics
Previous publications have described demographics and treatment outcomes in detail for this sample (Kendall et al., 2010; Walkup et al., 2008) as well as relationships between somatic symptoms, demographic factors, and treatment outcomes (Crawley et al., 2014). The mean age of participants was 10.7 years (SD = 2.8), with the majority (74.2%) 7–12 years old. The sample was evenly distributed by gender (50.4% male, n = 246). The sample was primarily White (78.9%; n = 385), with 9.0% Black (n = 44), 2.5% Asian (n = 12), 1.2% American Indian (n = 6), 0.4% Native Hawaiian/Other Pacific Islander (n = 2), and 8.0% Other (n = 39). The sample was predominately non-Hispanic (87.9%), and 25.4% (n = 124) were categorized as low socioeconomic status (i.e. a score of 3 or less on the Hollingshead Two-Factor Scale).
Of the 524 children evaluated at baseline, 488 participants (93.1%) were randomized to treatment and 440 of these (90.2%) completed the assessment at Week 12. The complete CONSORT diagram detailing study recruitment, randomization, and retention has been previously published in Walkup et al. (2008). The mean number of therapy sessions completed out of 14 in the CBT group was 13.2 (SD = 2.0) and 12.6 (SD = 2.8) in the COMB group. The mean dose of sertraline was 146.0 mg (SD = 60.8) per day for the SRT group, and 133.7 mg (SD = 59.9) per day for the COMB group. For more information on participants and procedures see Compton et al. (2010), Kendall et al. (2010), and Walkup et al. (2008).
Table 1 presents the descriptive statistics for somatic symptoms for each treatment group and time point. Notably, although there was some variation in the reduction of somatic symptom levels reported over time across the treatment conditions, the means were below the cutoff for clinically significant somatic symptoms. There were no significant treatment group differences at baseline on any measure used in this study, nor were there any baseline differences between completers and non-completers.
Table 1.
SCARED-P/C Panic/Somatic Means and Standard Deviations
| Treatment Condition |
Reporter | Baseline Mean (SD) |
Week 8 Mean (SD) |
Week 12 Mean (SD) |
|---|---|---|---|---|
| SRT | Parent | 4.30 (4.46) | 1.52 (2.33) | 1.01 (1.91) |
| Child | 4.09 (4.93) | 1.63 (2.84) | 1.61 (2.84) | |
| CBT | Parent | 4.97 (4.75) | 2.88 (3.25) | 1.71 (2.94) |
| Child | 4.24 (4.37) | 2.59 (3.09) | 1.92 (2.91) | |
| COMB | Parent | 4.34 (4.46) | 2.17 (3.13) | 1.01 (1.97) |
| Child | 4.36 (4.85) | 2.33 (3.59) | 1.62 (3.04) | |
| PBO | Parent | 4.47 (4.73) | 2.95 (3.83) | 2.30 (3.49) |
| Child | 4.38 (4.92) | 2.95 (4.60) | 2.55 (4.24) |
Note: SCARED-P/C = Screen for Child Anxiety and Related Disorders – Parent or Child report, Panic/Somatic subscale. SRT = sertraline, CBT = cognitive behavioral therapy, COMB = combined sertraline/CBT, and PBO = placebo.
Mediation Analysis Results: PARS
To assess the potential role of somatic symptoms as a mediator in anxiety improvements generally, we ran a causal mediation analysis using the PARS as a measure of anxiety severity. The first ANCOVA found significant treatment effects on anxiety symptoms (F(3, 408) = 14.10, p < .001). Moreover, treatment affected mid-treatment somatic symptoms as measured by the SCARED-P (F(3, 408) = 6.70, p < .001) in the second ANCOVA. This implied that mid-treatment somatic symptoms could be a mediator for at least one of the three active interventions. Table 2a displays the estimated indirect (i.e. mediation), direct and total effects on anxiety symptoms for the three post-hoc contrast tests in the third ANCOVA along with 95% confidence interval (CI) and p-values. The total effect column further supported that SRT and/or CBT resulted in greater anxiety symptoms reduction compared with placebo. The direct effect column suggested that there were significant treatment effects on anxiety symptoms reduction after including mid-treatment somatic symptoms as mediator in the causal pathway. Notably, however, the indirect effect results indicated that mid-treatment somatic symptoms were only a statistically significant mediator for the SRT intervention.
Table 2.
Primary Causal Mediation Models Effects by Outcome with SCARED-P Panic/Somatic Subscale Score as Mediator
| A. Effects on Anxiety Symptoms (PARS) | |||
| Active treatment arm (placebo as reference) |
Estimated (95% CI) effect [p-value] | ||
| Indirect | Direct | Total | |
| SRT | −0.69 (−1.32, −0.15) [p = .01] |
−2.04 (−3.89, −0.32) [p = .03] |
−2.73 (−4.51, −0.91) [p = .01] |
| CBT | −0.004 (−0.53, 0.47) [p = .99] |
−1.90 (−3.63, −0.18) [p = .03] |
−1.90 (−3.62, −0.07) [p = .04] |
| COMB | −0.40 (−0.93, 0.13) [p = .13] |
−5.33 (−7.09, −3.53) [p < .001] |
−5.73 (−7.53, −3.89) [p < .001] |
| B. Effects on Global Functioning (CGAS) | |||
| Active treatment arm (placebo as reference) |
Estimated (95% CI) effect [p-value] | ||
| Indirect | Direct | Total | |
| SRT | 1.09 (0.25, 2.14) [p = .01] |
4.18 (1.13, 7.53) [p = .01] |
5.27 (2.18, 8.66) [p < .001] |
| CBT | 0.06 (−0.71, 0.84) [p = .90] |
4.01 (0.91, 7.17) [p = .02] |
4.07 (1.00, 7.15) [p = .02] |
| COMB | 0.59 (−0.17, 1.49) [p = .12] |
8.67 (5.58, 11.88) [p < .001] |
9.26 (6.06, 12.70) [p < .001] |
Note: All effects based on data from parent reported somatic symptoms using the SCARED-P Panic/Somatic subscale.
Replacing parent report mid-treatment somatic symptoms by child report from SCARED-C, the ANCOVA in step 2 found that treatment condition was not associated with somatic symptoms (F(3, 403) = 2.64, p = .05). This resulted in the termination of this exploratory analysis.
Mediation Analysis Results: CGAS
To assess the potential role of somatic symptoms as a mediator in improvements in global functioning, we ran a causal mediation analysis using the CGAS. The first ANCOVA found significant treatment effects on the CGAS score (F(3, 408) = 11.52, p <.001). The second ANCOVA detected treatment effects on mid-treatment somatic symptoms based on the SCARED-P (F(3, 408) = 6.67, p < .001). This implied that mid-treatment somatic symptoms could be a mediator for at least one of the three active interventions. Table 2b displays the estimated indirect, direct and total effects on global functioning score for the three post-hoc contrast tests in the third ANCOVA along with 95% confidence interval (CI), and p-values.
The findings for the CGAS causal mediation analyses were consistent with the above PARS causal mediation analysis. The total effect column provided additional evidence that SRT and/or CBT resulted in greater improvement of global functioning compared with placebo. The direct effect column supported that there were significant treatment effects on global functioning improvement after including mid-treatment somatic symptoms as a mediator in the causal pathway. As in the PARS mediation analysis, a significant indirect effect due to mid-treatment somatic symptoms was only detected in the SRT intervention.
Replacing parent report mid-treatment somatic symptoms by child report from SCARED-C, the ANCOVA in step 2 found that treatment condition was not associated with somatic symptoms (F(3, 403) = 2.63, p = .05). This resulted in the termination of this exploratory analysis.
Discussion
Although both CBT and SSRIs are effective treatments for pediatric anxiety disorders, research regarding the active mechanisms of these treatments is limited and further research on mediators of treatment is needed. This paper evaluated the mediating role of somatic symptoms, a necessary step prior to considering it as a possible mechanism of change. The study’s first hypothesis examined the extent to which changes to anxiety-related somatic symptoms contributed to anxiety improvements for at least one of the three active treatment conditions. Analyses indicated that reductions in physical symptoms of anxiety (e.g. autonomic arousal, cardiac symptoms) appeared to be a significant contributor to anxiety reductions for both anxiety-specific symptoms and global functioning, based on parent report. The second hypothesis examined to what extent reductions in somatic symptoms of anxiety were responsible for improvements in anxiety following specific treatments. Findings indicated that reductions in somatic symptoms (e.g., less tension, calmer heartbeat) mediated the effects of sertraline but not CBT treatments for both anxiety-specific symptoms and global functioning. As before, the effects were true only for the parent report.
The differences in mediation results across treatment conditions offer preliminary support for the notion that although sertraline and CBT are similarly efficacious and their combined treatment is most effective (Walkup et al., 2008), reductions in anxiety may indeed operate via different mechanisms across treatments. This finding is consistent with some of the adult literature on this topic (e.g., Quidé et al., 2012), and with previous analyses on the CAMS dataset finding that treatment trajectories changed with the introduction of cognitive restructuring and exposures but not relaxation (Peris et al., 2015).
Based on these results it appears that medication’s improvements are mediated through physiological changes, such that the physiologic changes underlying reductions in individuals’ physical symptoms of anxiety lead to improvements in overall anxiety burden. As noted earlier, data from the adult and child literature suggests that anxiety is associated with abnormal activation of brain fear networks partly regulating arousal (Strawn et al., 2012) and perhaps these reductions in arousal are evident in the self-reported reductions of somatic symptoms. It is intriguing to note that a indirect effect appeared in spite of the fact that the youth in this sample did not score exceptionally high on the Panic/Somatic subscale of the SCARED; all participants had clinically significant anxiety, but most did not have clinically significant somatic symptoms.
In contrast to the SRT condition, we failed to find support for somatic symptoms as a mediator of CBT gains. There are several potential explanations for this. One possibility is that somatic symptom reductions are not a critical component to how CBT works, and that the reductions in somatic symptom reductions found are occurring only as a consequence – not a contributor to – improvements. Previous studies of mediators of CBT outcomes (including in this sample) found that changes in anxious self-talk (Kendall et al., 2016; Kendall & Treadwell, 2007; Lau et al., 2010; Treadwell & Kendall, 1996) and changes in perceived coping (Kendall et al, 2016) were mediators of CBT treatment outcomes, so perhaps it is simply that these cognitive elements are why CBT works, not the reductions to somatic symptoms which occur.
Alternatively, our findings may have been influenced by the dosage and timing of sessions focused on somatic symptoms in relation to our study assessments. As noted earlier, somatic symptoms were the focus of Coping Cat sessions three and five, with later sessions having the strongest emphasis on exposures. By Week 8 (our mid-treatment assessment point) we had hoped that participants would have had time to implement their newly-learned relaxation skills, but it is possible that the three weeks was insufficient. Thus, the low dose of relaxation (given of the timing of our assessments) may have weakened the effect of changes in somatic symptoms. It should be noted that although the CAMS study did include later assessments at Weeks 24 and 36 which would have allowed for a potentially higher dose of relaxation to take effect, our ability to reliably detect group differences in this dataset at those times was hampered by the fact that after Week 12 participants could engage in alternative forms of treatment (e.g., CBT for those in the SRT condition, sertraline for those in the initial CBT group, or either treatment to youth in the placebo group).
Another important finding from this study was that reduction in anxiety-related somatic symptoms contributed to improvements in global functioning, at least within the sertraline-only condition. This highlights both the burden of somatic symptoms (e.g., more missed days of school, avoiding activities if they have an upset stomach or are experiencing other somatic symptoms) and the opportunity of treatments to enhance functioning by reducing these somatic symptoms. In this context, reducing somatic symptoms appeared to have a ripple effect such that not only did the symptoms go down, but overall functioning was also improved.
Importantly, the indirect effect found was only present based on parental reports. The problem of discrepancies between reporters is common (see De Los Reyes, Alfano, & Beidel, 2011 for a discussion) and has been previously documented in this sample (e.g., Wei et al., 2014). Some studies found that youth report of anxiety was lower than that of their parents (Comer & Kendall, 2004; Silverman et al., 1999), and others have found inconsistencies between parent- and child-reported reductions from pre to post interventions (e.g., Ginsburg, 2009). Unfortunately, it is impossible to know whether the parental or child report of somatic symptoms was more accurate in this case. One possibility is that perhaps given the relatively young age of participants parents were better assessors of the frequency of somatic symptoms, and parents were able to notice the connection between panic/somatic symptoms and child anxiety in ways that children were less likely to observe. Indeed, previous research indicated that anxious youth were not always able to accurately perceive their own somatic symptoms (e.g., Anderson & Hope, 2009) and other analyses within this sample found that parental reports of anxiety were more highly correlated with IE reports (Becker, Jensen-Doss, Kendall, Birmaher, & Ginsburg, 2016). Alternatively, it is possible that the children were in fact more accurate reporters of somatic symptoms in this sample, with parents making misattributions regarding somatic symptoms.
Limitations
This study has several limitations that must be considered when interpreting results. First, there are no objective measures of somatic symptoms (e.g. autonomic arousal), so it is impossible to determine the degree to which somatic symptoms actually changed or remained stable. Although this is a common problem in treatment research on child and adolescent anxiety (De Los Reyes & Aldao, 2015), the absence of objective measures is problematic especially since the literature is clear that anxious individuals are not always able to accurately report their physiological symptoms (e.g., Anderson & Hope, 2009). Additionally, the lack of an anxiety sensitivity measure (e.g., Children’s Anxiety Sensitivity Index; Silverman, Fleisig, Rabian, & Peterson, 1991) means that there was no way to control for the influence that this construct may have had on individuals’ perception of anxious experiences. The lack of objective data on physiological reactivity and anxiety sensitivity, while common in other studies of child and adolescent anxiety (see Silverman & Ollendick, 2005, and Villabø, Gere, Torgersen, March, & Kendall, 2012) is particularly problematic because parents consistently reported their children as having more somatic symptoms than the youths themselves in this sample. Because of the lack of concordance and inconsistency in findings (indirect effect appearing in analyses using the parent but not child reports), conclusions drawn must necessarily be tentative.
Other limitations have to do with additional aspects of measurement. We cannot determine which symptoms specifically were driving the indirect effect since the SCARED-P/C Panic/Somatic subscale was comprised of multiple items. Relatedly, it should be noted that the SCARED-P/C has a strong emphasis on symptoms related to feeling tense and autonomic factors (e.g., panic-like symptoms). Other physical symptoms of anxiety including sleep and more gastrointestinal problems may also merit consideration as important factors that may change (or be changed by) anxiety.
Final limitations have to do with the generalizability of findings. The majority of participants were White, non-Hispanic, and only 25% were from a low SES background. Although the sample size ensured that other groups had some representation, the findings may not be applicable to those from lower SES and/or other ethnic or racial groups. Additionally, this sample consisted of clinically anxious children who did not have clinically significant somatic symptoms; thus the findings may not generalize to other populations with much more complex physical symptoms.
Clinical Significance and Future Directions
The results of these analyses, while necessarily tentative, raise important clinical implications and suggest avenues for future research. In terms of the clinical implications regarding medication, understanding more about how sertraline works may be useful as prescribers seek to engage those hesitant to begin a trial of the medication. Research has shown that parents of anxious children are not always as open to medication as they are to behavioral treatments (Brown, Deacon, Abramowitz, Dammann, & Whiteside, 2007; Chavira, Stein, Bailey, & Stein, 2003). Although much remains to be learned about how and why SSRIs function, the ability to provide some additional information about the relationship between medication and somatic symptoms may be helpful to providers as they seek to engage families in shared decision-making.
In terms of CBT, much remains to be learned and applied by practitioners. The lack of indirect effect found in the CBT treatment condition may indicate a focus on somatic symptoms is not as critical a component of CBT as previously thought. It may be possible to streamline CBT protocols, reducing the number of sessions and/or allowing clinicians to focus more attention on the elements known to be mediators of change (e.g., the cognitive factors mentioned earlier). Alternatively, it may be that there are moderators of this mediation effect such as different types of anxiety disorders, medical diagnoses, or levels of somatic symptoms that would indicate a need for more (or less) focus on somatic symptoms within CBT protocols. Several researchers have already begun designing CBT protocols with increased focus on somatic symptoms for youths who struggled significantly more with physical symptoms, with positive results (Eisen & Silverman, 1998; Reigada, Fisher, Cutler, & Masia Warner, 2008; Masia Warner et al., 2011). Similarly, Szigethy et al. (2007) modified a CBT depression protocol for adolescents with inflammatory bowel disease which focused on these somatic symptoms. More research could clarify whether factors of dosage (i.e., amount of time spent focusing on relaxation and somatic symptoms) and/or participant characteristics (e.g., diagnosis, level of pre-treatment somatic symptoms) impacts the need to integrate somatic symptoms into treatment.
Finally, one need for future research is that additional studies should consider measuring physiological data more objectively using one of many different methods available (Thomas, Aldao, & De Los Reyes, 2012). The past reliance on self report and parent report is now largely unnecssary given technological advances, and the ability to accurately measure symptoms will no doubt help researchers draw accurate conclusions moving forward.
Conclusions
Although previous studies had showed that reductions in somatic symptoms coincided with reductions in anxiety (Crawley et al., 2014; Ginsburg et al., 2006; Masia Warner et al., 2011), the current analyses utilized statistical techniques and CAMS’ longitudinal design to analyze causal pathways from pre- to post treatment via mid-treatment somatic symptoms. Results indicated that reductions in anxiety-related somatic symptoms mediated treatment response on measures of both anxiety specifically and global functioning more broadly in sertraline-only treatment condition. Thus, although the overall efficacy of sertraline and CBT for anxiety may be similar, the treatments appear to function via different mediators.
Acknowledgments
FUNDING
This research was supported by an NIMH grants (MH063747; MH086438; HD080097 to Kendall; MH64003 to Birmaher; MH64003 to Compton; MH64088 to Piacentini; MH64089 to Walkup; MH64092 to Albano).
References
- Alfano CA, Pina AA, Villalta IK, Beidel DC, Ammerman RT, & Crosby LE (2009). Mediators and moderators of outcome in the behavioral treatment of childhood social phobia. Journal of the American Academy of Child & Adolescent Psychiatry, 48(9), 945–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson ER, & Hope DA (2009). The relationship among social phobia, objective and perceived physiological reactivity, and anxiety sensitivity in an adolescent population. Journal of Anxiety Disorders, 23(1), 18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker EM, Jensen-Doss A, Kendall PC, Birmaher B, & Ginsburg GS (2016). All anxiety is not created equal: Correlates of parent/youth agreement vary across subtypes of anxiety. Journal of Psychopathology and Behavioral Assessment, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent D. a, Chiappetta L., Bridge J., Monga S, & Baugher M. (1999). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child & Adolescent Psychiatry, 38(10), 1230–1236. doi: 10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SM (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 545–553. doi: 10.1097/00004583-199704000-00018 [DOI] [PubMed] [Google Scholar]
- Brown AM, Deacon BJ, Abramowitz JS, Dammann J, & Whiteside SP (2007). Parents’ perceptions of pharmacological and cognitive-behavioral treatments for childhood anxiety disorders. Behaviour Research and Therapy, 45(4), 819–828. [DOI] [PubMed] [Google Scholar]
- Campo JV (2012). Annual research review: Functional somatic symptoms and associated anxiety and depression - developmental psychopathology in pediatric practice. Journal of Child Psychology and Psychiatry, 53(5), 575–592. doi: 10.1111/j.1469-7610.2012.02535. [DOI] [PubMed] [Google Scholar]
- Chavira DA, Stein MB, Bailey K, & Stein MT (2003). Parental opinions regarding treatment for social anxiety disorder in youth. Journal of Developmental & Behavioral Pediatrics, 24(5), 315–322. [DOI] [PubMed] [Google Scholar]
- Chu BC, & Harrison TL (2007). Disorder-specific effects of CBT for anxious and depressed youth: A meta-analysis of candidate mediators of change. Clinical Child and Family Psychology Review, 10(4), 352–372. doi: 10.1007/s10567-007-0028-2 [DOI] [PubMed] [Google Scholar]
- Clark LA, & Watson D (1991). Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100(3), 316–336. doi: 10.1037/0021-843X.100.3.316 [DOI] [PubMed] [Google Scholar]
- Comer JS, & Kendall PC (2004). A symptom-level examination of parent-child agreement in the diagnosis of anxious youths. Journal of the American Academy of Child & Adolescent Psychiatry, 43(7), 878–886. doi: 10.1097/01.chi.0000125092.35109.c5 [DOI] [PubMed] [Google Scholar]
- Compton SN, Peris TS, Almirall D, Birmaher B, Sherrill J, Kendall PC, … Albano AM. (2014). Predictors and moderators of treatment response in childhood anxiety disorders: results from the CAMS trial. Journal of Consulting and Clinical Psychology, 82(2), 212–224. doi: 10.1037/a0035458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton SN, Walkup JT, Albano AM, Piacentini JC, Birmaher B, Sherrill JT, … March JS. (2010). Child/Adolescent Anxiety Multimodal Study (CAMS): Rationale, design, and methods. Child and Adolescent Psychiatry and Mental Health, 4, 1–15. doi: 10.1186/1753-2000-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello JE, Egger HL, & Angold A (2004). The developmental epidemiology of anxiety disorders In Ollendick T & March J (Eds.), Phobic and Anxiety Disorders in Children and Adolescents (pp. 61–91). New York: Oxford University Press. [Google Scholar]
- Crawley SA, Caporino NE, Birmaher B, Ginsburg G, Piacentini J, Albano AM, … Kendall PC. (2014). Somatic complaints in anxious youth. Child Psychiatry & Human Development, 45(4), 398–407. doi: 10.1007/s10578-013-0410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings CM, Caporino NE, Settipani CA, Read KL, Compton SN, March J, … Kendall PC. (2013). The therapeutic relationship in cognitive-behavioral therapy and pharmacotherapy for anxious youth. Journal of Consulting and Clinical Psychology, 81(5), 859–864. doi: 10.1037/a0033294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, & Aldao A (2015). Introduction to the special issue: Toward implementing physiological measures in clinical child and adolescent assessments. Journal of Clinical Child & Adolescent Psychology, 44(2), 221–237. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Alfano CA, & Beidel DC (2011). Are clinicians’ assessments of improvements in children’s functioning ‘global’?. Journal of Clinical Child & Adolescent Psychology, 40(2), 281–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domschke K, Stevens S, Pfleiderer B, & Gerlach AL (2010). Interoceptive sensitivity in anxiety and anxiety disorders: An overview and integration of neurobiological findings. Clinical Psychology Review, 30(1), 1–11. [DOI] [PubMed] [Google Scholar]
- Donegan E, & Dugas MJ (2012). Generalized anxiety disorder: A comparison of symptom change in adults receiving cognitive-behavioral therapy or applied relaxation. Journal of Consulting and Clinical Psychology, 80(3), 490–496. doi: 10.1037/a0028132 [DOI] [PubMed] [Google Scholar]
- Edgar JC, Keller J, Heller W, & Miller GA (2007). Psychophysiology in research on psychopathology. Handbook of Psychophysiology, 665–687. [Google Scholar]
- Eisen AR, & Silverman WK (1998). Prescriptive treatment for generalized anxiety disorder in children. Behavior Therapy, 29(1), 105–121. doi: 10.1016/S0005-7894(98)80034-8 [DOI] [Google Scholar]
- Eley TC, Stirling L, Ehlers A, Gregory AM, & Clark DM (2004). Heart-beat perception, panic/somatic symptoms and anxiety sensitivity in children. Behaviour Research and Therapy, 42(4), 439–448. doi: 10.1016/S0005-7967(03)00152-9 [DOI] [PubMed] [Google Scholar]
- Garber J, Walker LS, & Zeman J (1991). Somatization symptoms in a community sample of children and adolescents: further validation of the Children’s Somatization Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 3(4), 588–595. [Google Scholar]
- Ginsburg GS (2009). The child anxiety prevention study: Intervention model and primary outcomes. Journal of Consulting and Clinical Psychology, 77(3), 580–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Becker EM, Keeton CP, Sakolsky D, Piacentini J, Albano AM, … Kendall PC. (2014). Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry, 71(3), 310–8. doi: 10.1001/jamapsychiatry.2013.4186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Keeton CP, Drazdowski TK, & Riddle MA (2011). The utility of clinicians’ ratings of anxiety using the Pediatric Anxiety Rating Scale (PARS). Child and Youth Care Forum, 40(2), 93–105. doi: 10.1007/s10566-010-9125-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Riddle MA, & Davies M (2006). Somatic symptoms in children and adolescents with anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 45(10), 1179–1187. doi: 10.1097/01.chi.0000231974.43966.6e [DOI] [PubMed] [Google Scholar]
- Green B, Shirk S, Hanze D, & Wanstrath J (1994). The Children’s Global Assessment Scale in clinical practice: An empirical evaluation. Journal of the American Academy of Child & Adolescent Psychiatry, 33(8), 1158–1164. [DOI] [PubMed] [Google Scholar]
- Hale WW, Raaijmakers Q, Muris P, & Meeus WIM (2005). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED) in the general adolescent population. Journal of the American Academy of Child & Adolescent Psychiatry, 44(3), 283–290. [DOI] [PubMed] [Google Scholar]
- Hayes AM, Laurenceau J-P, Feldman G, Strauss JL, & Cardaciotto L (2007). Change is not always linear: the study of nonlinear and discontinuous patterns of change in psychotherapy. Clinical Psychology Review, 27(6), 715–23. doi: 10.1016/j.cpr.2007.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofflich SA, Hughes AA, & Kendall PC (2006). Somatic complaints and childhood anxiety disorders. International Journal of Clinical and Health Psychology, 6(2), 229–242. [Google Scholar]
- Hudson JL (2005). Mechanisms of change in cognitive behavioral therapy for anxious youth. Clinical Psychology: Science and Practice, 12(2), 161–165. doi: 10.1093/clipsy/bpi019 [DOI] [Google Scholar]
- Hughes AA, Hedtke KA, & Kendall PC (2008). Family functioning in families of children with anxiety disorders. Journal of Family Psychology , 22(2), 325–328. doi: 10.1037/0893-3200.22.2.325 [DOI] [PubMed] [Google Scholar]
- Imai K, Keele L, & Tingley D (2010). A general approach to causal mediation analysis. Psychological Methods, 15(4), 309–334. doi: 10.1037/a0020761 [DOI] [PubMed] [Google Scholar]
- Joiner TE Jr, Steer RA, Beck AT, Schmidt NB, Rudd MD, & Catanzaro SJ (1999). Physiological hyperarousal: Construct validity of a central aspect of the tripartite model of depression and anxiety. Journal of Abnormal Psychology, 108(2), 290–298. [DOI] [PubMed] [Google Scholar]
- Kazdin AE (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- Kendall PC, Compton SN, Walkup JT, Birmaher B, Albano AM, Sherrill J, … Piacentini J. (2010). Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders, 24(3), 360–365. doi: 10.1016/j.janxdis.2010.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Cummings CM, Villabø MA, Narayanan MK, Treadwell K, Birmaher B, ... Albano AM. (2016). Mediators of change in the Child/Adolescent Anxiety Multimodal Treatment Study. Journal of Consulting and Clinical Psychology, 84(1), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, & Treadwell KRH (2007). The role of self-statements as a mediator in treatment for youth with anxiety disorders. Journal of Consulting and Clinical Psychology, 75(3), 380–389. doi: 10.1037/0022-006X.75.3.380 [DOI] [PubMed] [Google Scholar]
- Kerstner T, Witthöft M, Mier D, Diener C, Rist F, & Bailer J (2015). A diary-based modification of symptom attributions in pathological health anxiety: Effects on symptom report and cognitive biases. Journal of Consulting and Clinical Psychology, 83(3), 578–589. [DOI] [PubMed] [Google Scholar]
- Kreibig SD (2010). Autonomic nervous system activity in emotion: A review. Biological Psychology, 84(3), 394–421. doi: 10.1016/j.biopsycho.2010.03.010 [DOI] [PubMed] [Google Scholar]
- Lau WY, Chan CKY, Li JCH, & Au TKF (2010). Effectiveness of group cognitive-behavioral treatment for childhood anxiety in community clinics. Behaviour Research and Therapy, 48(11), 1067–1077. doi: 10.1016/j.brat.2010.07.007 [DOI] [PubMed] [Google Scholar]
- Lundh A, Kowalski J, Sundberg CJ, Gumpert C, & Landén M (2010). Children’s Global Assessment Scale (CGAS) in a naturalistic clinical setting: Inter-rater reliability and comparison with expert ratings. Psychiatry Research, 177(1), 206–210. [DOI] [PubMed] [Google Scholar]
- March JS, Franklin ME, Leonard H, Garcia A, Moore P, Freeman J, & Foa E (2007). Tics moderate treatment outcome with sertraline but not cognitive-behavior therapy in pediatric obsessive-compulsive disorder. Biological Psychiatry, 61(3), 344–347. doi: 10.1016/j.biopsych.2006.09.035 [DOI] [PubMed] [Google Scholar]
- Maric M, Heyne DA, MacKinnon DP, Van Widenfelt BM, & Westenberg PM (2013). Cognitive mediation of cognitive-behavioural therapy outcomes for anxiety-based school refusal. Behavioural and Cognitive Psychotherapy, 41(5), 549–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masia Warner C, Colognori D, Kim RE, Reigada LC, Klein RG, Browner-Elhanan KJ, … Benkov K. (2011). Cognitive-behavioral treatment of persistent functional somatic complaints and pediatric anxiety: An initial controlled trial. Depression and Anxiety, 28(7), 551–559. doi: 10.1002/da.20821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzone L, Ducci F, Scoto MC, Passaniti E, D’Arrigo VG, & Vitiello B (2007). The role of anxiety symptoms in school performance in a community sample of children and adolescents. BMC Public Health, 7(1), 347. doi: 10.1186/1471-2458-7-347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Mayer B, den Adel M, Roos T, & van Wamelen J (2008). Predictors of change following cognitive-behavioral treatment of children with anxiety problems: A preliminary investigation on negative automatic thoughts and anxiety control. Child Psychiatry and Human Development, 40(1), 139–151. doi: 10.1007/s10578-008-0116-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muroff J, & Ross A (2011). Social disability and impairment in childhood anxiety In McKay D & Storch E. a. (Eds.), Handbook of Child and Adolescent Anxiety Disorders (pp. 457–478). New York: Springer. [Google Scholar]
- Peris TS, Compton SN, Kendall PC, Birmaher B, Sherrill J, March J, ... & Piacentini J. (2015). Trajectories of change in youth anxiety during cognitive—behavior therapy. Journal of Consulting and Clinical Psychology, 83(2), 239–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quidé Y, Witteveen AB, El-Hage W, Veltman DJ, & Olff M (2012). Differences between effects of psychological versus pharmacological treatments on functional and morphological brain alterations in anxiety disorders and major depressive disorder: A systematic review. Neuroscience and Biobehavioral Reviews, 36(1), 626–644. doi: 10.1016/j.neubiorev.2011.09.004 [DOI] [PubMed] [Google Scholar]
- Reigada LC, Fisher PH, Cutler C, & Masia Warner C (2008). An innovative treatment approach for children with anxiety disorders and medically unexplained somatic complaints. Cognitive and Behavioral Practice, 15(2), 140–147. doi: 10.1016/j.cbpra.2007.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Units on Pediatric Psychopharmacology Anxiety Study Group (2002). The pediatric anxiety rating scale (PARS): Development and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry, 41(9), 1061–1069. doi: 10.1097/00004583-200209000-00006 [DOI] [PubMed] [Google Scholar]
- Rynn MA, Siqueland L, & Rickels K (2001). Placebo-controlled trial of sertraline in the treatment of children with generalized anxiety disorder. American Journal of Psychiatry, 158(12), 2008–2014. [DOI] [PubMed] [Google Scholar]
- Seligman LD, & Ollendick TH (2011). Cognitive-behavioral therapy for anxiety disorders in youth. Child and Adolescent Psychiatric Clinics of North America, 20(2), 217–238. doi: 10.1016/j.chc.2011.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, & Aluwahlia S (1983). A children’s global assessment scale (CGAS). Archives of General Psychiatry, 40(11), 1228–1231. doi: 10.1001/archpsyc.1983.01790100074010 [DOI] [PubMed] [Google Scholar]
- Silverman WK, Fleisig W, Rabian B, & Peterson RA (1991). Childhood anxiety sensitivity index. Journal of Clinical Child & Adolescent Psychology, 20(2), 162–168. [Google Scholar]
- Silverman WK, & Hinshaw SP (2008). The second special issue on evidence-based psychosocial treatments for children and adolescents: A 10-year update. Journal of Clinical Child & Adolescent Psychology, 37(1), 1–7. doi: 10.1080/15374410701817725 [DOI] [PubMed] [Google Scholar]
- Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Lumpkin PW, & Carmichael DH (1999). Treating anxiety disorders in children with group cognitive-behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 67(6), 995–1003. [DOI] [PubMed] [Google Scholar]
- Silverman WK, & Ollendick TH (2005). Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology, 34(3), 380–411. doi: 10.1207/s15374424jccp3403_2 [DOI] [PubMed] [Google Scholar]
- Silverman WK, Pina AA, & Viswesvaran C (2008). Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology, 37(1), 105–130. doi: 10.1080/15374410701817907 [DOI] [PubMed] [Google Scholar]
- Storch EA, Merlo LJ, Larson MJ, Geffken GR, Lehmkuhl HD, Jacob ML, … Goodman WK. (2008). Impact of comorbidity on cognitive-behavioral therapy response in pediatric obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 47(5), 583–592. doi: 10.1097/CHI.0b013e31816774b1 [DOI] [PubMed] [Google Scholar]
- Strawn JR, Wehry AM, DelBello MP, Rynn MA, & Strakowski S (2012). Establishing the neurobiologic basis of treatment in children and adolescents with generalized anxiety disorder. Depression and Anxiety, 29(4), 328–339. [DOI] [PubMed] [Google Scholar]
- Strawn JR, Welge JA, Wehry AM, Keeshin B, & Rynn MA (2015). Efficacy and tolerability of antidepressants in pediatric anxiety disorders: A systematic review and meta-analysis. Depression and Anxiety, 32(3), 149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan A & Kendall PC (2016). Fear and missing out: Youth anxiety and functional outcomes. Clinical Psychology: Science and Practice. [Google Scholar]
- Szigethy E, Kenney E, Carpenter J, Hardy DM, Fairclough D, Bousvaros A, ... DeMaso DR. (2007). Cognitive-behavioral therapy for adolescents with inflammatory bowel disease and subsyndromal depression. Journal of the American Academy of Child & Adolescent Psychiatry, 46(10), 1290–1298. [DOI] [PubMed] [Google Scholar]
- Thomas SA, Aldao A, & De Los Reyes A (2012). Implementing clinically feasible psychophysiological measures in evidence-based assessments of adolescent social anxiety. Professional Psychology: Research and Practice, 43(5), 510. [Google Scholar]
- Tingley D, Yamamoto T, Hirose K, Keele L, & Imai K (2014). Mediation: R package for causal mediation analysis. [Google Scholar]
- Treadwell KRH, & Kendall PC (1996). Self-talk in youth with anxiety disorders: States of mind, content specificity, and treatment outcome. Journal of Consulting and Clinical Psychology, 64(5), 941–950. doi: 10.1037/0022-006X.64.5.941 [DOI] [PubMed] [Google Scholar]
- Velting ON, Setzer NJ, & Albano AM (2002). Anxiety disorders In Marsh DT & Fristad MA (Eds.), Handbook of Serious Emotional Disturbance (pp. 204–227). New York: Wiley. [Google Scholar]
- Villabø M, Gere M, Torgersen S, March JS, & Kendall PC (2012). Diagnostic efficiency of the child and parent versions of the Multidimensional Anxiety Scale for Children. Journal of Clinical Child & Adolescent Psychology, 41(1), 75–85. doi: 10.1080/15374416.2012.632350 [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, … Kendall PC. (2008). Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine, 359(26), 2753–2766. doi: 10.1056/NEJMoa0804633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Labellarte MJ, Riddle MA, Pine DS, Greenhill L, Klein R, … Hack S. (2001). Fluvoxamine for the treatment of anxiety disorders in children and adolescents. New England Journal of Medicine, 344(17), 1279–1285. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Labellarte MJ, Riddle MA, Pine DS, Greenhill L, Klein R, Roper M (2003). Searching for moderators and mediators of pharmacological treatment effects in children and adolescents with anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 42(1), 13–21. [DOI] [PubMed] [Google Scholar]
- Wei C, Hoff A, Villabø MA, Peterman J, Kendall PC, Piacentini J, ... & Sherrill J. (2014). Assessing anxiety in youth with the Multidimensional Anxiety Scale for Children. Journal of Clinical Child & Adolescent Psychology, 43(4), 566–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wren FJ, Bridge JA, & Birmaher B (2004). Screening for childhood anxiety symptoms in primary care: Integrating child and parent reports. Journal of the American Academy of Child & Adolescent Psychiatry, 43(11), 1364–1371. [DOI] [PubMed] [Google Scholar]


