Abstract
Objective.
We conducted meta-analyses of studies that investigated the associations between tobacco outlet density around homes and schools and adolescents’ past-month cigarette smoking.
Data sources.
Systematic literature searches of eight databases were carried out in February 2017. Searches were not limited by date, language, country, or peer-reviewed status.
Study selection.
After screening for quality, studies that examined the relationship between tobacco outlet density and adolescents’ past-month smoking were selected for inclusion.
Data extraction.
Two investigators screened study abstracts and full texts and independently extracted data. Consensus was reached at each stage.
Data synthesis.
Random effects meta-analyses were conducted on 11 studies that provided 13 effect sizes. Results showed that there was a significant association between tobacco outlet density around homes and adolescents’ past-month smoking behavior with an overall effect size of OR = 1.08 (95% CI = 1.04, 1.13; p <.001; I2 = 0%). For density around schools, the association was not statistically significant (OR = 1.01, 95% CI = 0.98, 1.03; p =.53; I2 = 39%).
Conclusions.
These findings suggest that exposure to tobacco outlets near home environments may be important for understanding adolescents’ past-month smoking. Restricting access to tobacco outlets and controlling the number of outlets in residential areas may be an effective preventive strategy to help reduce adolescents’ smoking.
INTRODUCTION
Exposure to tobacco outlets may be an important risk factor for cigarette smoking during adolescence. Potential mechanisms by which exposure to tobacco outlets may influence adolescents’ cigarette use include increased access to cigarettes1–3, exposure to tobacco marketing2,4,5, and exposure to other cigarette smokers (i.e., role models)6. In addition, exposure to outlets may normalize tobacco smoking and tobacco products in the landscape of available goods7. Exposure to tobacco outlets may affect adolescents’ cigarette smoking directly or may be mediated through perceived ease of obtaining cigarettes (subjective availability), perceptions of the prevalence acceptability of smoking (normative beliefs), or perceptions of the personal consequences associated with cigarette smoking (expectancies)8–11. Controls over the number of tobacco outlets (i.e., outlet density per unit area) and their distance from residential areas or schools (i.e., proximity) are approaches advocated to reduce adolescents’ exposure and access to tobacco and cigarette use12.
A growing body of mostly cross-sectional research has investigated the association between tobacco outlet density around residential areas or around schools and adolescents’ cigarette smoking1,3,6,13,14–23. Findings from this literature are mixed, with some studies indicating no or small effects1,3,17,22 and others demonstrating significant associations with adolescents’ smoking outcomes6,13–16,18,23.
These inconsistencies may be due to study factors, including differences in locations (e.g., countries, states), populations (e.g., racial or ethnic makeup), smoking outcomes (e.g., past-month cigarette smoking, lifetime smoking), definitions of tobacco outlet density (e.g., buffer sizes around homes or schools), and inclusion or exclusion of potential confounding variables. A recent narrative review summarized nine studies examining the association between the density and proximity of tobacco retailers and diverse adolescents’ smoking outcomes24. Of the reviewed studies, two assessed lifetime smoking, one assessed past 12-month smoking, and eight assessed past-month smoking. Yet, this study concluded that tobacco retailer density was more frequently associated with adolescents’ lifetime or past 12-month smoking than past-month smoking or susceptibility to smoking. In addition, this narrative review did not distinguish between exposure to outlets around homes versus schools and the variation in measures of outlet density or proximity across the different studies was not considered. Given the heterogeneity of studies included, it is difficult to draw conclusions from this review.
To date, no systematic reviews or meta-analyses of tobacco outlet density and adolescents’ smoking have been conducted. A meta-analysis that combines and evaluates the results from multiple studies can help address the uncertainty about the association between tobacco outlet density and adolescents’ smoking by providing an estimate of the effect size of this relationship. Therefore, the goal of the current study was to conduct meta-analyses to investigate the association between tobacco outlet density around homes and schools and adolescents’ past-month cigarette smoking. Past-month smoking was selected as the outcome of interest in the current study based on multiple factors. First, given past-month cigarette smoking is associated with a range of adverse health and developmental outcomes25–30, identifying environmental factors is important to public health. Second, past-month smoking is not subject to recall bias to the same degree as other indicators of smoking31,32. Finally, our read of the literature suggests that past-month smoking is the most common outcome assessed across studies examining tobacco outlet density and adolescent smoking. Results from this study may better inform policy makers and help guide future research on tobacco outlet density.
METHODS
Literature search strategy
Literature searches were conducted in February 2017 across the following eight databases: PubMed, PsycArticles, PsycINFO, SocINDEX, MEDLINE Complete, Psychology and Behavioral Sciences Collection, E-Journals, and Biomedical Reference Collection: Corporate. Literature searches of databases were not limited by date, language, country, or peer-review status. Search terms included MeSH and text word combinations relating to young people (i.e., adolescen*, teenager*, youth, young adult, middle school, high school, elementary school, or minors), the behavior of interest (i.e., tobacco, nicotine, smoking, or cigarette), and outlet density (i.e., outlet, store, shop, or retail and density or spatial). Two of the databases index grey literature (e.g., books/monographs, conference papers, and other non-periodical sources). Titles and abstracts of the studies identified were screened for inclusion by two independent researchers (LF and SLK). Disagreements were resolved through discussion. The full text of each article was obtained where further clarification on the measures or study objectives was needed. Further searches were conducted based on the reference lists of retrieved articles.
Inclusion criteria
Studies were evaluated for inclusion based on sample, exposure measure, and outcome. For the sample, we included only research that focused on children and adolescents younger than 18 years old (or ≤ 12th grade). For exposure measures, only studies that examined tobacco outlet densities around homes, schools, or both were included. Finally, for the outcome measure, only studies that examined current cigarette smoking (e.g., any past-month or past 30-day cigarette smoking) were included. Studies that examined other concurrent tobacco use with cigarette smoking were included. Studies were excluded if they (a) measured school-level prevalence of cigarette smoking rather than individual-level smoking (e.g.,33) and (b) focused only on outcomes other than past-month cigarette smoking such as past year smoking or changes in cigarette smoking (e.g.,6,21). Studies that examined these factors were excluded to ensure the meta-analyses yielded precise estimates which allowed for a meaningful interpretation of the overall effect between tobacco outlet density and adolescent past-month smoking34. Further, studies were excluded if they only measured outlet density at larger geographical areas such as at city- or school district-level (e.g.,35), rather than specifically assessing density around school addresses/borders or home addresses or census tracts.
We used the Newcastle-Ottawa Quality Assessment Scale (NOQAS) adapted for cross-sectional studies to ensure the quality of the reviewed papers36. Studies were scored on a scale of 0–10, with greater scores indicating greater study quality. Each study was reviewed by two authors (LF and SLK or MA) and disagreements were resolved through discussion. Specifically, we evaluated studies based on the following criteria: representativeness of the sample, sample size, non-respondents (i.e., response rate), ascertainment of the exposure, inclusion of confounding factors, assessment of the outcome, and the appropriateness of the statistical tests used. For the inclusion of confounding factors assessment indicator, we assessed studies for the inclusion of individual-level (e.g., age, gender, socioeconomic status, etc.) and community-level (e.g., urbanicity, socioeconomic indicators, etc.) factors known to be associated with adolescents’ cigarette smoking. All papers included in the current meta-analyses met these quality assessment criteria and were scored as either seven or eight out of ten.
Data extraction
Extracted data included study authors, publication year, data collection year, country, definition and operationalization of the outcome measure, definition and operationalization of tobacco outlet density, whether the focus was on home or school areas, individual- and community-level covariates included in the analyses, participant age group, sample size, and effect sizes. Each study was reviewed independently by two reviewers (LF and SLK or MA) who extracted the required data from each article and assessed the quality of the paper. Reviewed papers were discussed and discrepancies in extracted data were resolved by consensus among reviewers. Where effect size information was not reported or other information was missing, the authors of the papers were contacted.
Several factors were considered when deciding which effect size would be included when a single study provided more than one effect size. First, if studies provided effect sizes for the association between tobacco outlet density and adolescents’ smoking at various levels of tobacco outlet density (e.g., low vs high density and medium vs high density), the effect size for the most extreme comparison (e.g., low vs high) was included to capture the full range of exposures. Second, if studies provided multiple effect size estimates for the association between tobacco outlet density and adolescents’ smoking at various buffer sizes around homes or schools (e.g., 100 meters, 200 meters, etc.), we used the estimate that was closest to the average distance across all studies. Finally, when more than one past-month smoking outcome was reported within a single study (e.g., experimental and occasional past-month use), we selected the past-month smoking outcome that corresponded most closely with those reported in other included studies to allow for a meaningful interpretation of the overall effect34.
Analytic Strategy
Random effects meta-analyses were conducted to examine the associations between tobacco outlet density near homes and schools and adolescents’ past-month cigarette smoking. Random effects models were chosen over fixed effects models given the diversity among the studies and given the goal of this study was to generalize findings34. Further, the random effects model is more conservative than the fixed effects model because it accounts for both within- and between-study variance.
Most studies reported odds ratios (ORs) and 95% confidence intervals (CIs) as indicators of the relationships between tobacco outlet density and adolescents’ past-month cigarette use. When ORs were not reported, effect sizes were converted to ORs to allow comparison among studies34. All analyses were conducted in Stata version 1537, using metan and metareg. The I2 statistic was used to assess heterogeneity of the effect sizes. This statistic indicates the proportion of the variability explained by between-study heterogeneity rather than sampling error38. Finally, we examined funnel plots to explore potential publication bias and conducted sensitivity analyses to examine if results were strongly influenced by any individual study in either the home or school model.
RESULTS
Figure 1 displays the flow diagram for the studies reviewed for inclusion. We identified 192 studies through the search of the literature and four studies through manual searching of reference lists. After removing duplicate studies, 102 abstracts were screened and 74 articles were excluded as they did not meet eligibility criteria. A full-text review of the remaining 28 studies was conducted (see online Supplemental Table for full list of studies). Of the 28 studies, 17 were excluded because a more thorough, full-text review revealed they did not meet eligibility criteria (n =15) or because we were unable to obtain necessary information (e.g., effect sizes) for inclusion after contacting the authors (n = 2). A total of 11 studies were included in the meta-analyses (see Table 1). All of the 11 studies that met the inclusion criteria were observational studies and all but one16 employed a cross-sectional design. Finally, only one study did not use models that adjusted for the clustering of the data as the authors noted most cases were from independent geographic regions in their sample16 (i.e., cases were not nested within geographic region).
Figure 1.
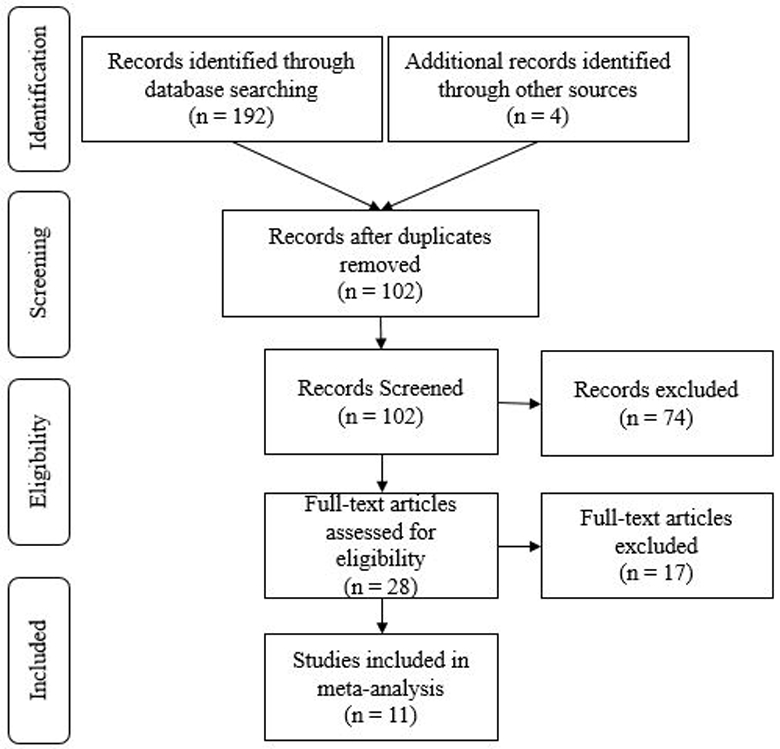
Flow diagram depicting the literature reviewed for inclusion in the meta-analyses
Table 1:
Characteristics and effect sizes of studies included in the meta-analysis
| Author Year |
Data Collection Year | Country | Sample Size | Sample Age | Outlet Density Buffer Distance (km) | Controls | Outlet Density Measurea | Distribution of Outlet Densityb | OR (95% CI)c |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Homes | ||||||||||
| Novak (2006)16 | 1995–1999 | USA | 2,116 | 11–23d | 0.43e | Minor status, age, race/ethnicity, gender, parental education, commercial land use, neighborhood racial composition, and neighborhood poverty | Trend | M = 7.1 | 1.21 (1.04, 1.40) |
|
| Adachi-Mejia (2012)22 | 2007 | USA | 1,263 | 13–18 | 0.80 | Age, race/ethnicity, SES, sibling smoking, friend smoking, exposure to movie smoking, team sport participation, sensation seeking, tobacco outlet proximity, and proportion of community population Black, Hispanic, and families with income below the poverty level | Trend | Median =.34 | 1.11 (0.70, 1.79) |
|
| Lipperman-Kreda (2014)14 | 2010 | USA | 832 | 13–18 | 1.21 | Gender, race/ethnicity, age, population density, median family income, and city % of minors <18 years, % African Americans, % Hispanic, % college educated, and % unemployed | Trend | M = 3.88 SD = 5.24 Range = 0–37.20 | 1.08 (1.01, 1.16) |
|
| Shortt (2016)18 | 2010 | Scotland | 20,446 | 13–15 | 0.80 | Age group, sex, ethnicity, received free school meals, perceived family wealth, family structure, parental smoking status, rurality, and Carstairs deprivation score | Trend | Range = 0- >5.63 | 1.06 (1.00, 1.12) |
|
| Schools | ||||||||||
| Leatherdale (2007)1 | 2001–2002 | Canada | 19,464 | 14–18 | 1.00 | Gender, age, parent smoking, older sibling smoking, ever smoked with family member, 5 closest friends smoking, and school student smoking rate |
Trend | M = 6.3 Range = 1–13 | 1.01 (0.99, 1.03) |
|
| McCarthy (2009)15 | 2003–2004 | USA | 19,306 | M = 14.9 | 1.61 | Age, gender, race/ethnicity, English-language use in the home, grades, peer smoking, friends’ smoking, ease of obtaining cigarettes, depressive symptoms, school type, school rurality, and school-level parental education |
Trend | M = 10.8 SD = 8.9 | 1.11 (1.02, 1.21) |
|
| Chan (2011)13 | 2005–2006 | Canada | 22,764 | 9–12 grade | 1.00 | Grade, gender, older sibling smoking, parent smoking, up to 5 closest friends smoking, and neighborhood disadvantage |
Trend | M = 2.68 Range = 0–16 | 0.99 (0.97, 1.01) |
|
| Adams (2013)19 | 2002 | USA | 9,704 | 7–10 grade | 0.80 | Sex, race/ethnicity, grade, illegal tobacco sales rate, median neighborhood income, and mean neighborhood density | Trend | M = 2.76 SD = 2.45 Range = 0–9 | 1.04 (0.95, 1.14) |
|
| Scully (2013)20 | 2008 | Australia | 2,044 | 12–17 | 0.50 | Age, sex, personal spending money, perceived ease of buying cigarettes, smoking status of parents/caretakers, and neighborhood SES | Trend | M = 2.37 SD = 1.65 Range = 0–7 | 1.06 (0.90, 1.25) |
|
| Lipperman-Kreda (2014)14 | 2010 | USA | 832 | 13–18 | 1.21 | Gender, race/ethnicity, age, population density, median family income, and city % of minors <18 years, % African Americans, % Hispanic, % college educated, % unemployed | Trend | M = 4.97 SD = 5.45 Range = 0–44.62 | 1.02 (0.93, 1.11) |
|
| Mistry (2015)23 | 2010 | India | 1,320 | 8–10 grade | 0.50 | Age, gender, religion, monthly receipt of pocket money, hopelessness, ease of access to tobacco, parental tobacco use, peer tobacco use, and school annual fee |
Low vs high density | M = 60.0 SD = 43.9 Range = 2–199 | 1.99 (0.92, 4.33)f |
|
| Marsh (2016)3 | 2012 | New Zealand | 27,238 | 14–15 | 1.00 | Sex, age, ethnicity, family smoking, peer smoking, school decile, and school location | Zero vs high density | Median = 2 | 0.94 (0.82, 1.07) |
|
| Shortt (2016)18 | 2010 | Scotland | 20,446 | 13–15 | 0.80 | Age group, sex, ethnicity, received free school meals, perceived family wealth, family structure, parental smoking status, rurality, and Carstairs deprivation score | Trend | Range = 0- >6.72 | 0.98 (0.92, 1.04) |
|
|
| ||||||||||
This column represents how the number of tobacco outlets was measured. Most studies used a count measure in which higher scores indicted a greater number of outlets (trend). Some studies compared zero/low vs high density areas.
These values represent descriptive statistics of tobacco outlet density provided in each study. These values may not be directly comparable due to differences in density and buffer size conceptualizations. Please refer to the “Outlet Density Buffer Distance” and “Outlet Density Measure” columns for more information about how to interpret these values.
These values represent adjusted ORs by the controls listed in the “Controls” column.
Although the age range extended beyond our initial cutoff of 18 years old, legal age to purchase cigarettes did not significantly influence the association between tobacco outlet density and current smoking.
We calculated the average census tract distance from the city in which the study was conducted to represent the outlet density catchment distance.
This study outcome included both smoked and non-smoked tobacco products.
Within the 11 studies, 33 effect sizes were provided. Two studies compared varying degrees of outlet density (e.g., low versus high density)3,23. For both studies, we selected the effect size associated with the zero/low outlet density versus high outlet density comparison. Three studies3,14,23 examined outlet density at multiple distances (e.g., 100 meters, 200 meters, etc.). Because the average distance used across all studies was .76 kilometers, we selected effect sizes from each study that were closest to this average. Finally, three studies included more than one indicator of adolescents’ past-month smoking3,13,15. Indicators of experimental smoking or occasional smoking were selected over established or daily smoking for these studies as these were most similar to outcomes used in other studies. A total of 13 effect sizes were included in the meta-analyses. Of these, two studies provided effect sizes for density around homes, seven studies provided effect sizes for density around schools, and two studies provided effect sizes for density around homes and schools (see Table 1).
Results of the meta-analyses are displayed in Figure 2. For homes, there was an association between tobacco outlet density and adolescents’ cigarette smoking with an overall effect size of OR = 1.08 (95% CI = 1.04, 1.13; p < .001; I2 = 0%). However, for schools, this association was not statistically significant (OR = 1.01, 95% CI = 0.98, 1.03; p =.53; I2 = 39%). Although the study heterogeneity was low38, an exploratory meta-regression was conducted to test whether the buffer size for measuring tobacco outlet density surrounding schools moderated the association between outlet density and adolescents’ cigarette smoking. Results indicated buffer size was not a significant predictor (p =.21). A similar analysis was not conducted for tobacco outlet density surrounding homes because of the small number of studies and non-heterogeneity.
Figure 2.
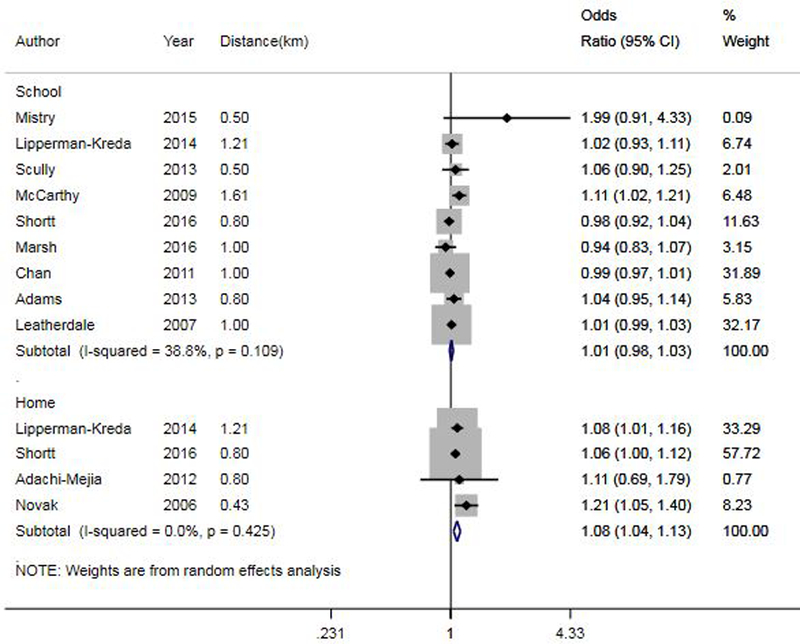
Forest plot for effects of tobacco outlet density around schools (top) and homes (bottom) on adolescents’ past-month cigarette smoking.
Sensitivity analyses were conducted by replicating models where each study was removed one by one. Results indicated that the overall effect estimates from these models were within the 95% CI range of the complete models, suggesting no one study strongly influenced findings for either the home or school models. Examination of funnel plots suggested that the included studies in the home and school models were not symmetrically distributed around the mean effect size, providing some evidence of publication bias (Supplementary Figures 1 and 2).
DISCUSSION
We conducted meta-analyses to investigate the associations between tobacco outlet density around homes and schools and adolescents’ past-month cigarette smoking. Studies included in the meta-analyses were from six different countries (most drawing from the U.S.) and included samples that ranged from 832 to 27,238 adolescents. These studies controlled for individual-, family-, and community-level characteristics that have been associated with adolescent smoking (e.g., age, gender or parental smoking14,39) and tobacco outlet density (e.g., indicators of neighborhood disadvantage33). Our findings indicate that for homes, but not for schools, there was an association between tobacco outlet density and adolescents’ past-month cigarette smoking, such that a one unit increase in tobacco outlet density around homes was associated with an 8% increase in the odds of adolescents’ past-month smoking. The current study findings are similar to results from individual studies that demonstrate that higher tobacco outlet density near homes, but not near schools, is associated with adolescents’ smoking outcomes6,14,18.
Results from our previous studies demonstrate the importance of community norms and show that personal beliefs mediate the relationships between community norms and cigarette smoking among adolescents10,40. It is possible that the environment surrounding the home is more important for the development of perceptions about community norms and personal beliefs and thus adolescents’ smoking behaviors. Alternatively, it may be that outlet density around homes is a better proxy for exposure to tobacco retail outlets than is measurement of exposure around schools (e.g., adolescents may spend more unstructured time around homes than schools). Similarly, the association between tobacco outlet density and adolescents’ smoking is complicated by the fact that some jurisdictions enact policies that restrict locations of tobacco outlets around schools12 but not homes. However, given the limited research related to effects of tobacco outlet density around homes on adolescents’ smoking behaviors, additional research is needed.
Several limitations of this study should be noted. First, there was a lack of consistency in how variables were defined across studies. For example, there was wide variation in distances or buffer sizes used to capture the density of tobacco outlets3,23, and in the definitions used for past-month cigarette smoking13,15. Because of this variability, we were limited in our ability to make a general conclusion about the relationship between tobacco outlet density and past-month cigarette use. Further, it is possible that our methods for choosing buffer sizes around homes and schools, measures of outlet density, and smoking outcomes within studies may have biased the results. For example, for studies that included a range of buffer sizes, we selected effect size estimates associated with the buffer distance closest to the average buffer distance across the included studies. Perhaps using effect size estimates at smaller buffer sizes (e.g., .10km instead of .50km) may have strengthened the association between tobacco outlet density and adolescents’ past-month smoking.
Second, it is possible that tobacco outlet density around homes or schools may be associated with other smoking behaviors (e.g., lifetime use). It is important that future studies build the literature examining the association between tobacco outlet density and other smoking behaviors for this population. Third, although we attempted to capture grey literature, potentially important unpublished research may have been excluded from the current study. Relatedly, examination of funnel plots for the home and school models suggested there was evidence of publication bias. As such, findings from the current study should be interpreted with caution as they may not represent the full range of research addressing the association between tobacco outlet density and adolescents’ past-month smoking. Finally, due to the limited number of studies, we were not able to fully explore moderating factors in the relationship between tobacco outlet density and adolescents’ past-month smoking. For example, point-of-sale tobacco advertising restrictions may be an important moderator for future studies to explore given policy differences across the various countries included in this study.
Results from this meta-analysis suggest that there is no significant association between tobacco outlet density around schools and adolescents’ past-month smoking and a relatively small, although meaningful, association between the number of outlets around homes and adolescents’ past-month smoking. Although based on a small number of studies, these results nonetheless suggest that restricting access to tobacco outlets and controlling the number of outlets in residential areas may help to reduce adolescents’ cigarette smoking. This finding may be important for informing policies about regulating outlet density through licensing or zoning processes. For example, policies which restrict the location or the number of tobacco outlets in residential areas may help reduce adolescent cigarette smoking. However, additional research is need given the small number of studies. In addition, future studies should be consistent in terms of measures used to calculate tobacco outlet density and to capture adolescents’ cigarette smoking or tobacco use. Moreover, as suggested by results of an exploratory study conducted by our research team41, it is possible that the traditional measures that are used to understand the relationship between tobacco outlet density and adolescents’ cigarette smoking are inadequate. It is important to more accurately measure adolescents’ exposure to tobacco outlets in their broader activity spaces in order to more fully understand the relationship between exposure to tobacco outlets and their smoking behavior. Through the construction of daily activity spaces, researchers may be able to better capture adolescents’ exposures to tobacco outlets and thus more clearly establish the relationships between such exposures and smoking behaviors.
Supplementary Material
What this paper adds.
A growing body of research examines the association between tobacco outlet density around residential areas or schools and adolescents’ cigarette smoking.
However, findings from this literature are mixed, with some studies indicating no or small effects and others demonstrating stronger associations with adolescents’ smoking.
Although a narrative review has been conducted on the association between the density and proximity of tobacco retailers and diverse smoking outcomes, meta-analyses of tobacco outlet density and adolescents’ smoking have not been conducted.
Findings from this meta-analysis indicate that higher tobacco outlet density around homes, but not schools, was associated with increased odds of adolescents’ past-month cigarette smoking.
Acknowledgment:
We would like to thank the authors of the studies included in this meta-analysis for their responsiveness to questions about their work.
Funding:
This research and preparation of this manuscript were supported by grant 25IR-0029 from the California Tobacco-Related Disease Research Program (TRDRP) and grants P60-AA006282 and T32-AA014125 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the TRDRP, NIAAA or NIH.
References
- 1.Leatherdale ST, Strath JM. Tobacco retailer density surrounding schools and cigarette access behaviors among underage smoking students. Annals of Behavioral Medicine. 2007;33(1):105–111. [DOI] [PubMed] [Google Scholar]
- 2.Loomis BR, Kim AE, Busey AH, Farrelly MC, Willett JG, Juster HR. The density of tobacco retailers and its association with attitudes toward smoking, exposure to point-of-sale tobacco advertising, cigarette purchasing, and smoking among New York youth. Preventive Medicine. 2012;55(5):468–474. [DOI] [PubMed] [Google Scholar]
- 3.Marsh L, Ajmal A, McGee R, Robertson L, Cameron C, Doscher C. Tobacco retail outlet density and risk of youth smoking in New Zealand. Tobacco Control. 2016;25(2):e71–e74. [DOI] [PubMed] [Google Scholar]
- 4.Robertson L, McGee R, Marsh L, Hoek J. A systematic review on the impact of point-of-sale tobacco promotion on smoking. Nicotine & Tobacco Research. 2014;17(1):2–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henriksen L Comprehensive tobacco marketing restrictions: Promotion, packaging, price and place. Tobacco Control. 2012;21:147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schleicher NC, Johnson TO, Fortmann SP, Henriksen L. Tobacco outlet density near home and school: Associations with smoking and norms among US teens. Preventive Medicine. 2016;91:287–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnett R, Moon G, Pearce J, Thompson L, Twigg L. Smoking Geographies: Space, Place and Tobacco Wiley-Blackwell; 2016. [Google Scholar]
- 8.Bandura A Social foundations of thought and action: A social cognitive theory Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 9.Fishbein M, Ajzen I. Predicting and changing behavior: The reasoned action approach New York: Psychology Press; 2010. [Google Scholar]
- 10.Lipperman-Kreda S, Grube JW. Students’ perception of community disapproval, perceived enforcement of school antismoking policies, personal beliefs, and their cigarette smoking behaviors: results from a structural equation modeling analysis. Nicotine & Tobacco Research. 2009;11(5):531–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lipperman-Kreda S, Grube JW, Friend KB, Mair C. Tobacco outlet density, retailer cigarette sales without ID checks and enforcement of underage tobacco laws: Associations with youths’ cigarette smoking and beliefs. Addiction. 2016;111(3):525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ackerman A, Etow A, Bartel S, Ribisl K. Reducing the Density and number of tobacco retailers: Policy solutions and legal issues. Nicotine & Tobacco Research. 2017;19(2):133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan WC, Leatherdale ST. Tobacco retailer density surrounding schools and youth smoking behaviour: A multi-level analysis. Tobacco Induced Diseases. 2011;9(1):9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lipperman-Kreda S, Mair C, Grube JW, Friend KB, Jackson P, Watson D. Density and proximity of tobacco outlets to homes and schools: Relations with youth cigarette smoking. Prevention Science. 2014;15(5):738–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCarthy WJ, Mistry R, Lu Y, Patel M, Zheng H, Dietsch B. Density of tobacco retailers near schools: Effects on tobacco use among students. American Journal of Public Health. 2009;99(11):2006–2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Novak SP, Reardon SF, Raudenbush SW, Buka SL. Retail tobacco outlet density and youth cigarette smoking: a propensity-modeling approach. American Journal of Public Health. 2006;96(4):670–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pokorny SB, Jason LA, Schoeny ME. The relation of retail tobacco availability to initiation and continued smoking. Journal of Clinical Child and Adolescent Psychology. 2003;32(2):193–204. [DOI] [PubMed] [Google Scholar]
- 18.Shortt NK, Tisch C, Pearce J, Richardson EA, Mitchell R. The density of tobacco retailers in home and school environments and relationship with adolescent smoking behaviours in Scotland. Tobacco Control. 2016;25(1):75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adams ML, Jason LA, Pokorny S, Hunt Y. Exploration of the link between tobacco retailers in school neighborhoods and student smoking. The Journal of School Health. 2013;83(2):112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scully M, McCarthy M, Zacher M, Warne C, Wakefield M, White V. Density of tobacco retail outlets near schools and smoking behaviour among secondary school students. Australian and New Zealand Journal of Public Health. 2013;37(6):574–578. [DOI] [PubMed] [Google Scholar]
- 21.Mason MJ, Mennis J, Zaharakis NM, Way T. The dynamic role of urban neighborhood effects in a text-messaging adolescent smoking intervention. Nicotine & Tobacco Research. 2016;18(5):1039–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adachi-Mejia AM, Carlos HA, Berke EM, Tanski SE, Sargent JD. A comparison of individual versus community influences on youth smoking behaviours: A cross-sectional observational study. BMJ open. 2012;2(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mistry R, Pednekar M, Pimple S, et al. Banning tobacco sales and advertisements near educational institutions may reduce students’ tobacco use risk: Evidence from Mumbai, India. Tobacco control. 2015;24(e1):e100–107. [DOI] [PubMed] [Google Scholar]
- 24.Gwon SH, DeGuzman PB, Kulbok PA, Jeong S. Density and Proximity of licensed tobacco retailers and adolescent smoking. The Journal of School Nursing. 2017;33(1):18–29. [DOI] [PubMed] [Google Scholar]
- 25.Sabado MD, Haynie D, Gilman SE, Simons-Morton B, Choi K. High school cigarette smoking and post-secondary education enrollment: Longitudinal findings from the NEXT Generation Health Study. Preventive medicine. 2017;105:250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brook JS, Schuster E, Zhang C. Cigarette Smoking and depressive symptoms: A longitudinal study of adolescents and young adults. Psychological Reports. 2004;95(1):159–166. [DOI] [PubMed] [Google Scholar]
- 27.Grant BF. Age at smoking onset and its association with alcohol consumption and DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1998;10(1):59–73. [DOI] [PubMed] [Google Scholar]
- 28.Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: A systematic review. Nicotine & Tobacco Research. 2017;19(1):3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Audrain-McGovern J, Rodriguez D, Kassel JD. Adolescent smoking and depression: evidence for self-medication and peer smoking mediation. Addiction. 2009;104(10):1743–1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General Atlanta (GA): Centers for Disease Control and Prevention (US);2012. [PubMed] [Google Scholar]
- 31.Stanton WR, McClelland M, Elwood C, Ferry D, Silva PA. Prevalence, reliability and bias of adolescents’ reports of smoking and quitting. Addiction. 1996;91(11):1705–1714. [PubMed] [Google Scholar]
- 32.Rockwood T Assessing Physical Health. In: Johnson TP, ed. Handbook of Health Survey Methods 1st ed. Hoboken, New Jersey: John Wiley & Sons, Inc; 2015:104–141. [Google Scholar]
- 33.Henriksen L, Feighery EC, Schleicher NC, Cowling DW, Kline RS, Fortmann SP. Is adolescent smoking related to the density and proximity of tobacco outlets and retail cigarette advertising near schools? Preventive Medicine. 2008;47(2):210–214. [DOI] [PubMed] [Google Scholar]
- 34.Bornstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis United Kingdom: Wiley; 2009. [Google Scholar]
- 35.Lipperman-Kreda S, Grube JW, Friend KB. Local tobacco policy and tobacco outlet density: associations with youth smoking. The Journal of Adolescent Health. 2012;50(6):547–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000; http://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf. Accessed July 14, 2017. [Google Scholar]
- 37.StataCorp. Stata Statistical Software: Release 15 In. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 38.Thorlund K, Imberger G, Johnston BC, et al. Evolution of heterogeneity (I2) estimates and their 95% confidence intervals in large meta-analyses. PloS one. 2012;7(7):e39471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Loughlin J, Karp I, Koulis T, Paradis G, DiFranza J. Determinants of first puff and daily cigarette smoking in adolescents. American Journal of Epidemiology. 2009;170(5):585–597. [DOI] [PubMed] [Google Scholar]
- 40.Thrul J, Lipperman-Kreda S, Grube JW, Friend KB. Community-level adult daily smoking prevalence moderates the association between adolescents’ cigarette smoking and perceived smoking by friends. J Youth Adolesc. 2014;43(9):1527–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lipperman-Kreda S, Morrison C, Grube JW, Gaidus A. Youth activity spaces and daily exposure to tobacco outlets. Health & Place. 2015;34:30–33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


