Abstract
Autism spectrum disorder can be differentiated into three subtypes (aloof, passive, and active-but-odd) based on social behaviors according to the Wing Subgroups Questionnaire (WSQ). However, the correlations between the scores on some individual items and the total score are poor. In the present study, we translated the WSQ into Chinese, modified it, validated it in autistic and typically-developing Chinese children, and renamed it the Beijing Autism Subtyping Questionnaire (BASQ). Our results demonstrated that the BASQ had improved validity and reliability, and differentiated autistic children into these three subtypes more precisely. We noted that the autistic symptoms tended to be severe in the aloof, moderate in the passive, and mild in the active-but-odd subtypes. The modified questionnaire may facilitate etiological studies and the selection of therapeutic regimes.
Electronic supplementary material
The online version of this article (10.1007/s12264-018-0224-8) contains supplementary material, which is available to authorized users.
Keywords: Autism spectrum disorder, Subtypes, Wing Subgroups Questionnaire, Beijing Autism Subtyping Questionnaire
Introduction
All individuals with a diagnosis of autism spectrum disorder (ASD) show characteristic impairments in social interaction and (non-)verbal communication, as well as restricted and repetitive behaviors. However, the social interaction impairments can be present in various forms. A thorough understanding of this diversity is critical to the work of clinicians and researchers, since it results in diversity in intervention and responsiveness [1].
Based on the different patterns of social behavior in an epidemiological study, Wing and Gould [2] identified three social subtypes: aloof, passive, and active-but-odd. The validity of these subtypes has been explored and confirmed in the literature [3–7]. According to Castelloe and Dawson [4], the aloof and active-but-odd groups fall at two ends of a continuum. Other investigators have also reported similar results that children in the aloof group are “the most autistic” and those in the active-but-odd group are “the least autistic” [3, 5, 7]. Moreover, biological variables based on the Wing subtypes have been discovered. Modahl et al. indicated that the aloof subtype tends to have lower levels of oxytocin than controls [8]. Dawson and colleagues found biological differences between the passive and active-but-odd subgroups using electroencephalographic analysis [9]. The three subtypes have also been compared with regard to clinical interventions and have shown different responses to the same intervention [1, 10]. For example, transcutaneous electrical acupoint stimulation was administered as an intervention for children with ASD after they were sub-grouped based on Wing’s sub-classification. The results demonstrated that members of the aloof and passive subgroups improved significantly while children in the active-but-odd subgroup remained unaffected [10].
Identifying ASD subtypes is crucial not only for understanding its etiology and cause, but also for developing individualized medical approaches to treat the core and associated symptoms [11–13]. A parent or teacher questionnaire to diagnose subtypes according to Wing’s sub-classification system, the Wing Subgroups Questionnaire (WSQ), was developed by Castelloe and Dawson [4]. They indicated that the determination of subtypes based on the WSQ was strongly associated with the clinical diagnosis. The WSQ has been suggested to be a useful tool for evaluation and the treatment planning process [14]. In a study of emotional understanding, the authors found that the autistic groups showed worse emotion recognition than groups with attention-deficit/hyperactivity disorder and oppositional defiant disorder, while the active-but-odd group was the worst [15]. In an Early Intensive Behavioral Intervention (EIBI) study, all three subtypes had a different IQ after a period of intervention, among which the aloof group had significantly lower IQ scores and greater IQ changes after EIBI than the other two groups [1]. Scheeren et al. suggested that social interaction style might explain part of the heterogeneity among children with high-functioning ASD, since the active-but-odd style was positively associated with the symptoms of autism, attention deficit, executive functioning problems, and hyperactivity, but negatively associated with psychosocial health [16]. Several other studies also have used the WSQ as a tool for determining the social behavioral subtypes in their observational studies [17, 18].
However, as pointed out by O’Brien [6], although the WSQ has advantages in classifying ASD, the correlations between certain items from several groups of descriptions and their subtype summary scores are poor (r < 0.30), which has caused some confusion. In addition, prior to this study, no cross-culturally validated version of WSQ was available for native Chinese speakers. In this study, we translated and modified the WSQ, aiming to develop a validated cross-cultural Chinese version.
Methods
Participants
ASD Group
Autistic children (n = 550) were recruited from seven autism rehabilitation centers in Beijing (The Rehabilitation Center of Beijing for Disabled Children, Wucailu Rehabilitation Center, Yangguanyouyi Rehabilitation Center, Xiaofeixiang Rehabilitation Center, Changyuchuntong Rehabilitation Center, Caihongcunzhuang Rehabilitation Center, and Peking University Care Brain Health), one in Henan (The Third Affiliated Hospital of Zhengzhou University), one in Shandong (Yilin Rehabilitation Center), and one in Guangzhou (Kangna Rehabilitation Center) where autistic children received the applied behavior analysis (ABA)-based early intervention program between 2014 and 2016. Since most autistic children in northern China had rehabilitation training in Beijing, Henan, and Shandong, children from these rehabilitation centers to some extent represented ASD patients in northern China. In addition, we selected another center in Guangzhou to represent southern China. The diagnosis of ASD was made by experienced psychiatrists using the Diagnostic and Statistical Manual of Mental Disorders-5 [19].
Typically-Developing Children
Typically-developing children (n = 280) were recruited from three general kindergartens in Beijing (those of Peking University, Renmin University of China, and Peking University Health Science Center). This research was approved by the Institutional Review Board of Peking University and signed informed consent was obtained from all parents involved in this study.
Instruments
The Wing Subgroups Questionnaire
The WSQ is composed of 50 items, each of which is a statement that describes a child’s behavior. The 50 items are divided into 13 groups of descriptions, each containing either three or four items. Each group is designed to evaluate a specific type of behavior according to a Wing construct (e.g., communication, social approach, and social response). And the three or four items in each group correspond to the three Wing subtypes or to normal behaviors, resulting in four subscales. Each item is rated by parents on a Likert scale from zero to six according to how frequently the child shows the behavior. The scores for items in different groups corresponding to the same subtype are added together to obtain a total score for that subtype, yielding four total scores for each child. The subtype of an autistic child is determined by the highest among the four scores. Thus, a child can fall into one of the four categories aloof, passive, active-but-odd, or typical [4]. If the same scores for two different subtypes are obtained in one questionnaire, the child may have characteristics between these subtypes.
Autism Behavior Checklist (ABC)
This scale describes a series of typical autistic behaviors to assess their presence in a given individual. The scale is composed of 57 items, each corresponding to a single score referring to a single symptomatological area. The scale uses an observer’s rating of the child’s behavior to quantify behaviors typically associated with autism [20].
Childhood Autism Rating Scale (CARS)
This scale consists of 15 items and evaluates behaviors in 14 categories that are generally affected in children with severe autism, plus one category for general impressions of autism; it is widely used by psychiatrists during the diagnosis of autism. We used ABC and CARS to evaluate the severity of defects in social behaviors in the autistic children [20].
Procedures
Translation and Modification of the WSQ
To reach linguistic and cultural equivalence between the original questionnaire and the translated version, the WSQ was translated according to the international recommendations for cross-cultural adaptation of questionnaires [21]. After obtaining permission from Dr. Geraldine Dawson, author of the WSQ, the questionnaire was first translated from English to Chinese independently by two researchers. These two questionnaires were then harmonized into one Chinese version, which was later translated back to English by an English expert, who was not aware of the original English version. This back-translated version was compared with the original English version by the researchers and the final Chinese version of WSQ was agreed upon by all researchers after several rounds of discussion and editing.
Three groups (Routine, Physical Agility, and Irritating physical behaviors) were removed from the WSQ since these groups had the greatest number of items with a poor ability to discriminate subtypes. Then nine new groups were added after consulting experienced behavioral therapists, child psychiatrists, and parents of autistic children in order to better differentiate the subtypes. The Autism Diagnostic Interview–Revised (ADI-R) [22] and the Autism Diagnostic Observation Schedule (ADOS)[23] were also referred to during this process. Similar to the original WSQ, there were three or four items in each group representing aloof, passive, active-but-odd, and typical subtypes. This new version of the WSQ consisted of 19 groups and was named the original Beijing Autism Subgrouping Questionnaire (original BASQ).
Item Selection
The parents of 250 autistic children and 130 typically-developing children filled in the original BASQ according to the guidelines provided by investigators while they were visiting the research centers. After selection and the exclusion of incomplete questionnaires, a total of 334 copies for 284 boys and 50 girls with a mean age of 4.58 years (range: 2–10) were used for further analysis. The completion rate for questionnaires was 87.89% (334/380). The method of calculating scores for the original BASQ was the same as for the WSQ. Pearson’s correlation coefficient, Cronbach’s α, and communality and factor loading were used in the procedure of item selection. Several groups were removed from the original BASQ after the selection and a new BASQ was developed.
Reliability and Validity Analysis
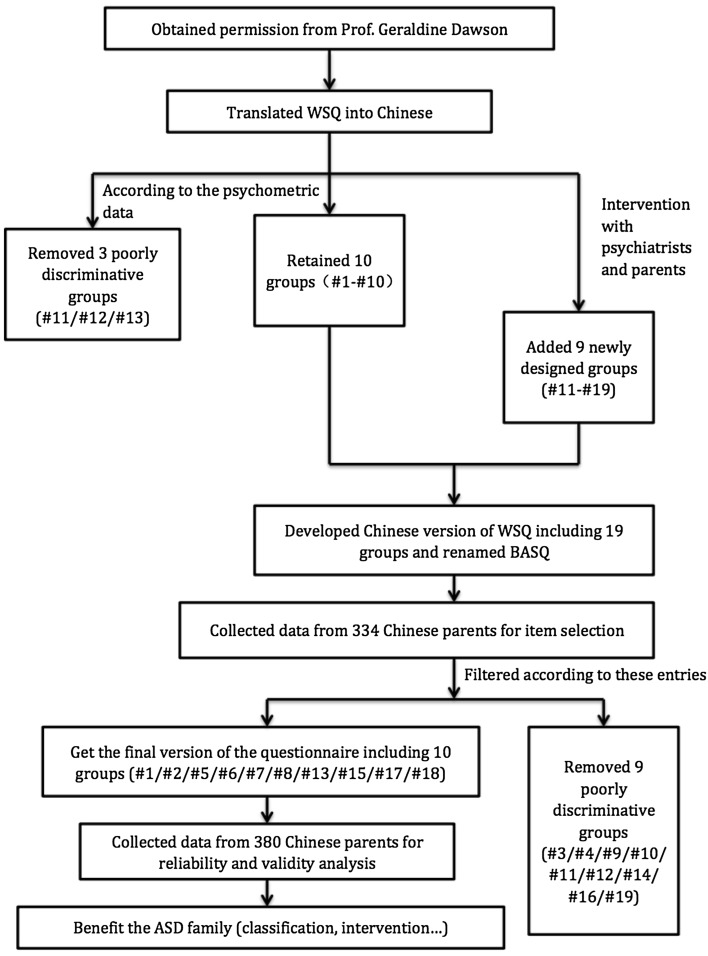
A new group of children with ASD and their parents were recruited for reliability and validity analysis. The new BASQ was filled in by 300 ASD parents and 150 parents of typically-developing children in the same way as described in item selection. A total of 380 completed BASQs were used for reliability and validity analysis, of which 336 were for boys and 44 for girls with a mean age of 4.53 years (range: 2–10). The completion rate was 84.44% (380/450). Among them, 51 ASD parents participated in the test-retest reliability analysis by filling in the same BASQ again 3–4 weeks later. Subtypes were analyzed among 73 children with ASD from the new group and determined by a child psychiatrist based on the sub-classification system described by Gould and Wing [2] after playing games with the children for 30–50 min in the criterion validity analysis (Fig. 1).
Fig. 1.
Procedure for developing the Beijing Autism Subgrouping Questionnaire.
Generally, the sample size should be 5–10 times the item size when developing a questionnaire [24]. Thus the sizes of our samples in the process of item selection and reliability and validity analysis were decided based on this rule. Data from this relatively large sample size would yield a more valid conclusion.
Relationship Analysis
To evaluate the severity of the defects in social behavior, 93 autistic children from among the participants in item selection or reliability and validity analysis were evaluated by a child psychiatrist using CARS. The parents of 94 children with ASD from among the participants in item selection or reliability and validity analysis completed the ABC.
Statistical Analysis
Item Selection
Data were analyzed with SPSS (Version 22.0; IBM Inc., Chicago, IL). The Pearson correlation coefficient was used to evaluate the correlation between the score for each item and its subtype summary score. An item was believed to have good homogeneity and therefore was included in the BASQ when the item had a high correlation coefficient with the subtype summary score. Otherwise, it was excluded. The criterion for exclusion was P > 0.05 or r < 0.4. Cronbach’s α was used to test the internal consistency of the four subtypes of the BASQ. An item was retained if Cronbach’s α decreased after removing the item from the questionnaire. On the contrary, an item was removed if Cronbach’s α remained the same or increased after removing the item [25]. Communality and factor loading were employed to evaluate the construct validity. An item was considered to have good homogeneity and was retained if the communality of the item was > 0.20 and the factor loading of this item was > 0.45. Otherwise it was removed [26].
Reliability and Validity Analysis
Content-related validity, face validity, construct validity, criterion validity, test-retest reliability, and internal consistency were used for reliability and validity analysis. The content-related validity and face validity were evaluated using a series of processes such as literature review and expert consultation. We also referred to advice from non-professionals and the parents of autistic children. The construct validity of the BASQ was tested by factor analysis and there were four factors: (1) aloof, (2) passive, (3) active but odd, and (4) typical. For criterion validity, Spearman correlation was conducted between BASQ scores and the rater’s subjective evaluation. For analysis of test-retest reliability, the scores of each subtype were examined using Pearson correlations. Cronbach’s α was used to test internal consistency.
Relationship Analysis
To test for significant differences between each of the three subtypes (aloof, passive and active-but-odd) in the severity of individual symptoms, the mean score for each CARS item and each score of the five aspects of ABC were compared between subtypes using one-way analysis of variance.
Results
Translation and Modification of the WSQ
WSQ was translated into Chinese from the original form and structure. It was renamed the original BASQ. The groups Insistence on Routine, Physical Agility, and Irritating Physical Behaviors were removed and nine new groups were added: eye contact, response to affiliative behavior, behaviors in group games, response to name, recognition of others, absent-mindedness, emotional response, game ability, and interest point in new environment. This new questionnaire consisted of 19 groups.
Item Selection
General Description
A total of 334 original BASQs were collected, in which 87 children were indicated to be aloof, 113 to be passive, 26 to be active-but-odd, and 108 to be typical (Table 1). There were no significant differences in terms of age (F = 2.372, P = 0.070) or gender ratio (χ2 = 1.697, P = 0.638) among these four subtypes.
Table 1.
Demographics for item selection.
| Subtypes | ||||
|---|---|---|---|---|
| Aloof | Passive | Active-but-odd | Typical | |
| n | 87 | 113 | 26 | 108 |
| Chronological age (years) | 4.61 ± 0.16 | 4.35 ± 0.11 | 4.74 ± 0.22 | 4.77 ± 0.09 |
| Gender (M:F) | 76:11 | 98:15 | 22:4 | 88:20 |
Data are presented as mean ± standard deviation.
M male, F female.
Correlation Analysis
The criterion for exclusion of groups was P > 0.05 or r < 0.4. The correlation coefficients for items representing the passive subtype and the passive subtype summary scores were 0.341 in #4, 0.333 in #14, and 0.299 in #16. The correlation coefficients for items representing active-but-odd with the summary score were 0.353 in #9, 0.295 in #12, 0.217 in #16 and 0.298 in #19. For the item in #16 representing the typical subtype the correlation coefficient was 0.385 (Table 2). Therefore, based on our inclusion and exclusion criteria, #4, #9, #12, #14, #16, and #19 were removed.
Table 2.
Results of item selection.
| Item | Aloof | Passive | Active-but-odd | Typical | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CR | Cα | CM | FL | CR | Cα | CM | FL | CR | Cα | CM | FL | CR | Cα | CM | FL | |
| #1 | 0.705** | 0.915 | 0.505 | 0.711 | 0.462** | 0.817 | 0.199a | 0.446a | 0.457** | 0.812 | 0.229 | 0.478 | 0.793** | 0.954 | 0.639 | 0.799 |
| #2 | 0.608** | 0.917 | 0.370 | 0.609 | 0.483** | 0.816 | 0.239 | 0.489 | 0.571** | 0.805 | 0.343 | 0.585 | 0.787** | 0.955 | 0.624 | 0.790 |
| #3 | 0.518** | 0.920a | 0.253 | 0.503 | 0.468** | 0.819 | 0.212 | 0.461 | 0.499** | 0.810 | 0.258 | 0.508 | 0.853** | 0.953 | 0.740 | 0.860 |
| #4 | 0.709** | 0.915 | 0.503 | 0.709 | 0.341**a | 0.824a | 0.090a | 0.300a | 0.616** | 0.803 | 0.389 | 0.624 | 0.756** | 0.955 | 0.578 | 0.760 |
| #5 | 0.564** | 0.919 | 0.296 | 0.544 | 0.529** | 0.814 | 0.296 | 0.544 | 0.573** | 0.805 | 0.334 | 0.578 | 0.710** | 0.956 | 0.506 | 0.711 |
| #6 | 0.766** | 0.913 | 0.594 | 0.770 | 0.564** | 0.812 | 0.310 | 0.557 | 0.673** | 0.799 | 0.490 | 0.700 | 0.878** | 0.953 | 0.784 | 0.886 |
| #7 | 0.653** | 0.917 | 0.411 | 0.641 | 0.590** | 0.810 | 0.367 | 0.606 | 0.678** | 0.798 | 0.507 | 0.712 | 0.885** | 0.953 | 0.789 | 0.888 |
| #8 | 0.612** | 0.917 | 0.354 | 0.595 | 0.543** | 0.813 | 0.318 | 0.564 | 0.504** | 0.809 | 0.249 | 0.499 | 0.793** | 0.954 | 0.636 | 0.797 |
| #9 | 0.471** | 0.920a | 0.220 | 0.469 | 0.479** | 0.817 | 0.234 | 0.484 | 0.353**a | 0.819a | 0.103a | 0.321a | 0.696** | 0.956 | 0.474 | 0.689 |
| #10 | 0.600** | 0.918 | 0.347 | 0.589 | 0.417** | 0.820 | 0.157a | 0.397a | 0.604** | 0.803 | 0.382 | 0.618 | 0.705** | 0.956 | 0.487 | 0.698 |
| #11 | 0.685** | 0.915 | 0.476 | 0.690 | 0.566** | 0.811 | 0.340 | 0.583 | 0.409** | 0.814 | 0.150a | 0.388a | 0.766** | 0.955 | 0.588 | 0.767 |
| #12 | 0.415** | 0.921a | 0.160a | 0.400a | 0.424** | 0.819 | 0.161a | 0.401a | 0.295**a | 0.820a | 0.087a | 0.294a | 0.712** | 0.956 | 0.494 | 0.703 |
| #13 | 0.802** | 0.912 | 0.660 | 0.812 | 0.565** | 0.811 | 0.339 | 0.582 | 0.563** | 0.806 | 0.344 | 0.586 | 0.855** | 0.953 | 0.742 | 0.861 |
| #14 | 0.704** | 0.915 | 0.501 | 0.708 | 0.333**a | 0.824a | 0.084a | 0.290a | 0.406** | 0.815 | 0.111a | 0.334a | 0.637** | 0.957a | 0.398 | 0.631 |
| #15 | 0.774** | 0.913 | 0.616 | 0.785 | 0.604** | 0.809 | 0.388 | 0.623 | 0.536** | 0.807 | 0.307 | 0.554 | 0.867** | 0.953 | 0.761 | 0.872 |
| #16 | 0.591** | 0.917 | 0.358 | 0.598 | 0.299**a | 0.825a | 0.061a | 0.247a | 0.217**a | 0.830a | 0.010a | 0.099a | 0.385**a | 0.961a | 0.117a | 0.342a |
| #17 | 0.704** | 0.915 | 0.517 | 0.719 | 0.554** | 0.813 | 0.326 | 0.571 | 0.478** | 0.811 | 0.244 | 0.494 | 0.765** | 0.955 | 0.581 | 0.762 |
| #18 | 0.719** | 0.914 | 0.536 | 0.732 | 0.645** | 0.807 | 0.459 | 0.678 | 0.569** | 0.806 | 0.357 | 0.597 | 0.815** | 0.954 | 0.674 | 0.821 |
| #19 | 0.574** | 0.918 | 0.343 | 0.585 | 0.409** | 0.819 | 0.155a | 0.394a | 0.298**a | 0.819a | 0.058a | 0.240a | 0.668** | 0.956 | 0.455 | 0.675 |
CR correlation analysis, Cα Cronbach’s alpha, CM communalities, FL factor load.
**P < 0.001.
aResults did not meet the inclusion criteria described in the Item Selection.
Evaluation Based on Cronbach’s α Values
The value of Cronbach’s α was 0.920 for the aloof subtype, increased to 0.921 after the exclusion of #12, and remained the same after removing #3 or #9; α was 0.824 for the passive subtype, increased to 0.825 with the removal of #16, and remained the same after exclusion of #4 or #14; α was 0.819 for the active-but-odd subtype, increased to 0.820 and 0.830 after the exclusion of #12 or #16, and remained the same after removal of #9 or #19; and α was 0.957 for the typical subtype, increased to 0.961 after the removal of #16, and remained the same with the exclusion of #14. Thus, #3, #4, #9, #12, #14, #16, and #19 were removed (Table 2).
Communality and Factor Loading
As to communality and factor loading, the criteria for item inclusion were communality > 0.2 and factor loading > 0.45. Items #4, # 9, #10, #11, #12, #14, #16, and #19 did not meet these criteria and were removed (Table 2). It should be noted that the item in #1 representing the passive subtype did not meet the communality and factor loading criteria. However, we all agreed that #1 should be retained since it describes social interaction behavior, which is one of the core symptoms of ASD and is important for differentiating between the 3 subtypes.
In summary, #3, #4, #9, #10, #11, #12, #14, #16, and #19 were removed in the first round. The removed groups were: how he/she approaches unfamiliar (#3), response to unfamiliar (#4), imitation (#9), unusual behavior or body movements (#10), eye contact (#11), response to affiliative behavior (#12), response to name (#14), absent-mindedness (#16), and interest point in a new environment (#19). Four of these were from the original WSQ and 5 were from the newly-included groups. Ultimately, a new questionnaire consisting of 10 groups with 40 items was created, and a part view of the questionnaire is available in Supplementary Material.
Reliability and Validity Analysis
General Description
A total of 380 new BASQs were collected, and 69 children were suggested to be aloof, 162 were passive, 39 were active-but-odd, and 102 were typical (Table 3). Subtypes could not be determined clearly by the BASQ for 8 children, since the same scores for two different subtypes were obtained in one questionnaire, suggesting that they had characteristics between two subtypes. There was a significant difference in age (F = 15.76, P < 0.0001) between them. No statistically significant differences were noted in the gender ratio (χ2 = 3.161, P = 0.367) among these four groups.
Table 3.
Demographics for reliability and validity analysis.
| Subtypes | |||||
|---|---|---|---|---|---|
| Aloof | Passive | Active-but-odd | Typical | Atypical | |
| n | 69 | 162 | 39 | 102 | 8 |
| Chronological age (years) | 3.92 ± 0.11 | 4.35 ± 0.11 | 5.04 ± 0.21 | 4.99 ± 0.07 | 5.06 ± 0.63 |
| Gender (M:F) | 62:7 | 139:23 | 37:2 | 92:10 | 6:2 |
Data are presented as mean ± standard deviation.
M male, F female.
Content-Related Validity and Face Validity
For the content-related validity, we reviewed the literature regarding ADOS and ADI-R. We also consulted two child psychiatrists from the Sixth Affiliated Hospital of Peking University and the Beijing Children’s Hospital about the methods of revising the questionnaire. For face validity, we sought advice from non-professionals and parents regarding ambiguous statements in the questionnaire and told the parents to inquire about what they did not understand. After that, we modified all the controversial item descriptions.
Construct Validity
Factor analysis for the 40 items of the BASQ showed that 10 items related to the typical subtype had the highest factor loading in factor one (typical). Ten items related to the aloof subtype had the highest factor loading in factor two (aloof), and 10 items related to the active-but-odd subtype had the highest factor loading in factor four (active-but-odd). Eight out of 10 items related to the passive subtype had the highest factor loading in factor three (passive). Our results demonstrated that the item distribution structure was consistent with the designed structure of the BASQ, suggesting that the questionnaire has satisfactory construct validity.
The item relating to the passive subtype in #9 had a higher factor loading in factor two. This might be due to the fact that the description of passive behavior was closer to aloof behavior. At the same time, the item in #3 representing the passive subtype had a negative load in factor one and had a similar load in the other three subtypes, indicating that this item described opposite behavior of the typical subtype and had a low degree of differentiation power for the other three subtypes (Table 4).
Table 4.
Results of factor analysis.
| Factors | ||||
|---|---|---|---|---|
| 1 (typical) | 2 (aloof) | 3 (passive) | 4 (active-but-odd) | |
| #4 Typical | 0.816 | −0.353 | −0.065 | −0.026 |
| #5 Typical | 0.815 | −0.322 | −0.135 | 0.075 |
| #7 Typical | 0.814 | −0.300 | −0.266 | −0.015 |
| #8 Typical | 0.804 | −0.332 | −0.152 | −0.008 |
| #6 Typical | 0.783 | −0.346 | −0.190 | −0.037 |
| #10 Typical | 0.746 | −0.286 | −0.251 | 0.061 |
| #2 Typical | 0.740 | −0.134 | −0.046 | 0.043 |
| #3 Typical | 0.735 | −0.134 | −0.046 | −0.072 |
| #9 Typical | 0.659 | −0.403 | −0.007 | −0.107 |
| #1 Typical | 0.630 | −0.326 | −0.255 | 0.117 |
| #3 Passive | −0.406 | 0.280 | 0.382 | 0.032 |
| #8 Aloof | −0.179 | 0.789 | −0.001 | −0.040 |
| #10 Aloof | −0.208 | 0.754 | 0.035 | 0.110 |
| #9 Aloof | −0.159 | 0.751 | −0.042 | 0.007 |
| #7 Aloof | −0.298 | 0.744 | 0.116 | 0.017 |
| #4 Aloof | −0.256 | 0.722 | 0.101 | −0.015 |
| #1 Aloof | −0.274 | 0.618 | 0.305 | −0.071 |
| #2 Aloof | −0.198 | 0.598 | −0.032 | −0.003 |
| #3 Aloof | −0.250 | 0.573 | −0.045 | 0.023 |
| #6 Aloof | −0.212 | 0.554 | 0.092 | 0.043 |
| #9 Passive | −0.388 | 0.549 | 0.308 | 0.106 |
| #5 Aloof | −0.355 | 0.540 | −0.032 | −0.128 |
| #4 Passive | 0.105 | −0.035 | 0.731 | 0.118 |
| #5 Passive | −0.155 | 0.068 | 0.694 | 0.130 |
| #10 Passive | −0.298 | 0.113 | 0.680 | −0.010 |
| #7 Passive | 0.016 | 0.024 | 0.667 | 0.132 |
| #1 Passive | 0.064 | −0.040 | 0.661 | −0.037 |
| #2 Passive | −0.210 | −0.029 | 0.554 | 0.164 |
| #8 Passive | −0.259 | 0.385 | 0.545 | −0.069 |
| #6 Passive | −0.252 | 0.141 | 0.448 | 0.178 |
| #5 Active-but-odd | 0.048 | −0.014 | 0.200 | 0.720 |
| #4 Active-but-odd | −0.025 | −0.042 | 0.049 | 0.708 |
| #8 Active-but-odd | −0.080 | −0.039 | 0.270 | 0.671 |
| #10 Active-but-odd | 0.181 | −0.088 | −0.114 | 0.669 |
| #7 Active-but-odd | 0.040 | 0.018 | 0.014 | 0.642 |
| #1 Active-but-odd | −0.260 | 0.206 | 0.018 | 0.626 |
| #9 Active-but-odd | −0.114 | 0.078 | 0.005 | 0.582 |
| #6 Active-but-odd | 0.036 | 0.025 | 0.385 | 0.492 |
| #3 Active-but-odd | 0.376 | −0.275 | 0.176 | 0.444 |
| #2 Active-but-odd | 0.166 | 0.03 | 0.408 | 0.430 |
Criterion Validity
Analysis of 73 children was independently performed by a rater based on the description of the three subtypes proposed by Wing and Gould [2] and by parents using the BASQ. The results from these two subtyping methods were compared and showed a significant positive correlation, with a correlation coefficient of 0.76 (P < 0.0001), indicating that the BASQ has satisfactory criterion validity.
Test–Retest Reliability
The test-retest reliability was assessed in 51 children. The interval between test and retest was 3–4 weeks. Our results showed a correlation value (r) of test-retest reliability of 0.723 (P < 0.0001) for the passive score, 0.884 (P < 0.0001) for the active-but-odd score, and 0.781 (P < 0.0001) for the typical score. The test-retest reliability was satisfactory since the satisfaction criterion was r > 0.7 for this analysis. At the same time, the correlation value for the aloof score was 0.650 (P < 0.0001), which was not satisfactory.
Internal Consistency
The value of Cronbach’s α was 0.891 for the aloof subtype, 0.836 for the passive subtype, 0.821 for the active-but-odd subtype, and 0.951 for the typical subtype. The values for all tests were > 0.7, indicating that the BASQ has good internal consistency.
Relationship Analysis
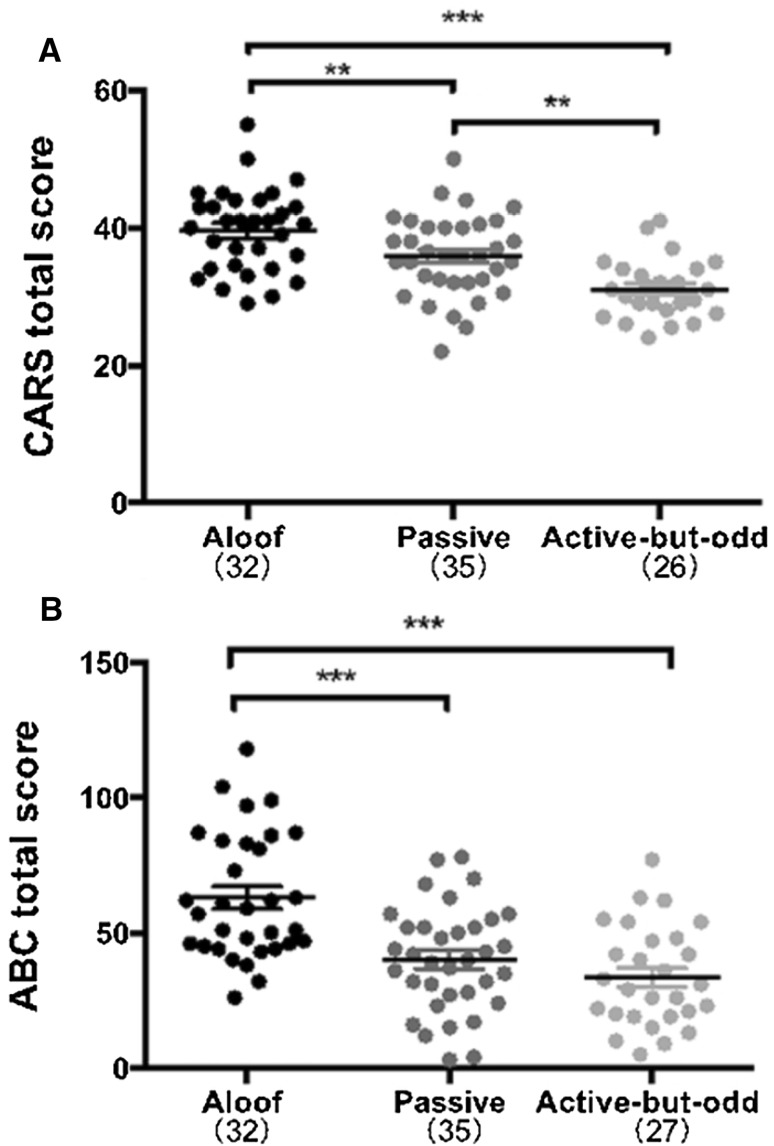
The severity of symptoms of abnormal behavior was evaluated using ABC and CARS among the 3 different subtypes (aloof, passive, and active-but-odd) differentiated by the BASQ. The ABC behavior values were: sensory, F(2, 91) = 14.41, P < 0.001; relating, F(2, 91) = 10.77, P < 0.001; stereotypes and objective use, F(2, 91) = 15.89, P < 0.001; language, F(2, 91) = 6.37, P = 0.003; self-help and social, F(2, 91) = 6.59, P = 0.002; and the total score, F(2, 91) = 18.40, P < 0.001. The values for behaviors analyzed by CARS were: relating to people, F(2, 90) = 10.34, P < 0.001; imitative behavior, F(2, 90) = 14.53, P < 0.001; emotional response, F(2, 90) = 10.67, P < 0.001; subject use, F(2, 90) = 9.16, P < 0.001; visual response, F(2, 90) = 7.03, P = 0.001; verbal communication, F(2, 90) = 19.24, P < 0.001; non-verbal communication, F(2, 90) = 17.27, P < 0.001; level of intellective relations, F(2, 90) = 21.40, P < 0.001; general impression, F(2, 90) = 12.94, P < 0.001; and total score, F(2, 90) = 16.95, P < 0.01. These results clearly showed that the symptoms were most severe in children of the aloof subtype and less severe in the active-but-odd subtype, with the passive subtype in between. There were no evident differences in the behaviors of body use, adaptation to change, listening response, perceptive response, fear of anxiety, and activity level among the three subtypes. And there were clear differences in each score of the five aspects and total ABC score (Table 5).
Table 5.
Behavioral characteristics of different social subtypes.
| Subtypes | F | P | |||
|---|---|---|---|---|---|
| Aloof | Passive | Active-but-odd | |||
| Childhood autism rating scale, mean (SD) | |||||
| Number of case | 32 | 35 | 26 | ||
| Relating to people | 3.16 (± 0.65) | 2.77 (± 0.52) | 2.48 (± 0.52) | 10.34 | < 0.001 |
| Imitative behavior | 2.69 (± 0.58) | 2.36 (± 0.49) | 2.02 (± 0.22) | 14.53 | < 0.001 |
| Emotional response | 3.16 (± 0.76) | 2.63 (± 0.71) | 2.33 (± 0.60) | 10.67 | < 0.001 |
| Body use | 1.86 (± 0.89) | 1.97 (± 0.61) | 1.83 (± 0.61) | 0.36 | 0.70 |
| Subject use | 2.92 (± 0.72) | 2.54 (± 0.67) | 2.17 (± 0.65) | 9.16 | < 0.001 |
| Adaptation to change | 1.64 (± 0.76) | 1.84 (± 0.69) | 1.50 (± 0.44) | 2.07 | 0.13 |
| Visual response | 2.86 (± 0.50) | 2.73 (± 0.46) | 2.40 (± 0.45) | 7.03 | 0.001 |
| Listening response | 2.55 (± 0.68) | 2.70 (± 0.39) | 2.37 (± 0.52) | 2.88 | 0.06 |
| Perceptive response | 1.91 (± 0.81) | 1.94 (± 0.60) | 1.60 (± 0.47) | 2.42 | 0.09 |
| Fear of anxiety | 1.88 (± 0.70) | 1.80 (± 0.61) | 1.56 (± 0.45) | 2.12 | 0.13 |
| Verbal communication | 3.25 (± 0.72) | 2.59 (± 0.60) | 2.27 (± 0.51) | 19.24 | < 0.001 |
| Non-verbal communication | 3.02 (± 0.41) | 2.56 (± 0.54) | 2.21 (± 0.62) | 17.27 | < 0.001 |
| Activity level | 2.33 (± 0.78) | 2.34 (± 0.65) | 2.31 (± 0.71) | 0.18 | 0.98 |
| Level of intellective relations | 3.17 (± 0.81) | 2.44 (± 0.86) | 1.79 (± 0.72) | 21.40 | < 0.001 |
| General impression | 3.23 (± 0.84) | 2.64 (± 0.75) | 2.27 (± 0.53) | 12.94 | < 0.001 |
| Total score | 39.61 (± 6.02) | 35.86 (± 5.90) | 31.10 (± 4.27) | 16.95 | < 0.001 |
| Autism behavior checklist, mean (SD) | |||||
| Number of case | 32 | 35 | 27 | ||
| Sensory | 10.28 (± 4.46) | 6.60 (± 5.08) | 4.19 (± 3.27) | 14.41 | < 0.001 |
| Relating | 17.09 (± 6.76) | 11.51 (± 7.13) | 9.22 (± 6.37) | 10.77 | < 0.001 |
| Stereotypes and object use | 9.84 (± 7.28) | 3.40 (± 3.46) | 3.70 (± 3.73) | 15.89 | < 0.001 |
| Language | 14.16 (± 7.61) | 11.37 (± 7.67) | 7.81 (± 6.51) | 6.37 | 0.003 |
| Self-help and social | 11.06 (± 5.12) | 7.23 (± 4.45) | 7.60 (± 4.36) | 6.59 | 0.002 |
| Total score | 62.94 (± 23.15) | 40.11 (± 19.38) | 32.52 (± 18.01) | 18.40 | < 0.001 |
The total CARS scores in all three subtypes clearly showed that the highest mean total score was in the aloof subtype and the lowest was in the active-but-odd subtype (Fig. 2A). These data indicated that children in the aloof subtype had the most severe autistic symptoms, while the passive and active-but-add subtypes had moderate and mild symptoms, respectively. A similar distribution was found when the total ABC scores were plotted (Fig. 2B).
Fig. 2.
Total CARS and ABC scores in all three subtypes of autistic children. The total scores for CARS (A) and ABC (B) differed significantly among the three subtypes (P < 0.001).
Discussion
The sub-classification of ASD is important for diagnosis and treatment. But unfortunately, there are few well-designed instruments for sub-classification. Although the original sub-classification by Wing and WSQ has been applied in American populations [1, 5, 9, 17, 27], it has been used by only one study in China [10]. The limited application in the Chinese population may be due to its popularity and language. The objectives of this study were to cross-culturally adapt and validate a Chinese version of the WSQ. Translation of a questionnaire from English to Chinese requires using a unique method to achieve linguistic and cultural equivalence between the original and translated versions [28]. Our translation ensured that the Chinese description of an item was reported in a way similar to that in English.
Compared to the three classes of severity listed in DSM-5, based on all the core features of ASD [19], the WSQ differentiates ASD solely based on social interaction [4]. Moreover, since this questionnaire is filled in by the caregivers of autistic children, it is very easy to use in clinical settings.
One of the critical steps for modifying the questionnaire was the selection and removal of groups. According to O’Brien [6], three groups (Insistence on Routine, Physical Agility, and Irritating Physical Behaviors) are not good discriminators for sub-classification. Moreover, Volkmar et al. [7] and Borden et al. [3] found that the aloof and passive subtypes demonstrated more stereotypic behaviors than the active-but-odd subtype, but O’Brien [6] indicated that the aloof and active-but-odd subtypes had similar levels. So the associations between social sub-classification and stereotypic behavior, temper/physical aggression was not clear. Based on the above considerations, we removed these three groups from the WSQ.
Our results showed that the reliability and validity of the BASQ was more satisfactory than the WSQ [4, 6]. First of all, the results of factor analysis supported the conclusion that the BASQ was composed of four subtypes which were independent of each other. Second, since there is no gold standard for the Wing sub-classification, we chose raters’ subjective assessment as the comparative standard and found that the correlation coefficient was > 0.7, demonstrating that the BASQ accurately reflected the subtypes of ASD children. In addition, most results of test-retest reliability showed a correlation coefficient > 0.7, demonstrating that the results of the BASQ were stable. Notably, the correlation for the aloof score was only 0.650 and < 0.7; this limitation should be considered when this test is administered to children in the aloof subgroup. A lower level of reliability might arise from the high heterogeneity of ASD, since the subtype of some ASD children could change after intervention [29]. Finally, Cronbach’s α for the 4 subtypes was between 0.821 and 0.951, higher than that for the WSQ (0.63–0.85), demonstrating that the BASQ has good internal consistency.
Interestingly, when ASD children were differentiated using the BASQ, there was evident heterogeneity within the autistic syndrome among the three subtypes. In our study, the severity of symptoms was determined using the ABC and CARS scales. This demonstrated that the aloof subtype was “most autistic” and the active-but-odd subtype was moderate. This result is similar to that of Borden [3]. To date, the intrinsic connections between BASQ subtypes and symptom severity are not clear. Hopefully, this subtyping questionnaire will facilitate the understanding of this intrinsic connection, as well as the etiology, development, pathogenesis, and prognosis of ASD.
Age is a very important variable in evaluation. In our study, the participants’ mean age in the process of item selection was 4.58 years (range, 2–10), and in the reliability and validity analysis it was 4.53 years (range, 2–10). Data from this study suggested that the BASQ is suitable for ASD children between 2 and 10 years old. However, whether it can also be applied to children older than 10 has yet to be determined.
IQ might be a predictor of social subtypes [7]. Since it is difficult to directly assess the IQ of children under the age of 6, especially those with ASD, we assessed the developmental quotient (DQ) to represent their mental development. The DQs of 55 ASD children (16 aloof, 22 passive, and 17 active-but-odd) recruited in this study were evaluated using the Gesell Developmental Schedule. Notably, we found that the DQ scores in the scatter-plot largely overlapped among the different social subtypes, suggesting that the children could not be assigned to their corresponding social subgroups solely according to their DQ scores. These results suggested that though the intellectual/developmental level might be partially related to the social subtypes, they are two different subtyping approaches based on different measurements. These different subtyping approaches might serve as external validity for each other to some extent, but they explain different aspects of the symptom heterogeneity of ASD. In addition, since the BASQ is filled in by the caregivers, the influence of IQ levels on the results would be less than in a questionnaire finished by participants themselves. In this study, we found that, at least for children with a DQ between 20 and 98, the BASQ subtyped them reliably, but for children with a DQ < 20, whether the BASQ is equally applicable remains to be further studied. Moreover, since we had only 55 participants in this part of the study, we did not include it in the Methods and Results sections.
Several shortcomings of this study should be noted. First, in the ASD group, the numbers of children of different subtypes were not equal, the active-but-odd subtype accounting for only 12.90% of the population (26+39/226+278). This might reflect the natural distribution of the subtypes in China, especially in the Beijing area, since our questionnaires were randomly distributed among rehabilitation centers. There was a significant difference in age among the different subtypes in the reliability and validity analysis. Generally, members of the active-but-odd subtype were older than those in the other two subtypes. One possible reason might be the language skills of the active-but-odd subtype were good and they would be regarded as normal until more symptoms developed as they got older. That children in the active-but-odd subtype tend to be older has also been reported by other researchers but the reason is unclear [3]. Second, we recruited most of our participants from rehabilitation centers where the number of boys was much greater than that of girls. This is because ASD is male-biased [30] and we did not seek girls to have a balanced sex ratio. Thus, whether the BASQ is equally applicable to girls and boys is unclear. Third, the methods used for validity and reliability analysis were not comprehensive and should be further explored.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
This work was supported by the grant from the University of Ulm–Peking University Health Science Center Joint Center for Neuroscience Fund (BMU20160563) and the grant from the National Natural Science Foundation of China (81601196).
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
Ji-Sheng Han, Email: hanjisheng@bjmu.edu.cn.
Rong Zhang, Phone: 13717971821, Email: zhangrong@bjmu.edu.cn.
References
- 1.Beglinger L, Smith T. Concurrent validity of social subtype and IQ after early intensive behavioral intervention in children with autism: a preliminary investigation. J Autism Dev Disord. 2005;35:295–303. doi: 10.1007/s10803-005-3292-3. [DOI] [PubMed] [Google Scholar]
- 2.Wing L, Gould J. Severe impairments of social interaction and associated abnormalities in children: Epidemiology and classification. J Autism Dev Disord. 1979;9:11–29. doi: 10.1007/BF01531288. [DOI] [PubMed] [Google Scholar]
- 3.Borden MC, Ollendick TH. An examination of the validity of social subtypes in autism. J Autism Dev Disord. 1994;24:23–37. doi: 10.1007/BF02172210. [DOI] [PubMed] [Google Scholar]
- 4.Castelloe P, Dawson G. Subclassification of children with autism and pervasive developmental disorder: a questionnaire based on Wing’s subgrouping scheme. J Autism Dev Disord. 1993;23:229. doi: 10.1007/BF01046217. [DOI] [PubMed] [Google Scholar]
- 5.Eaves LC, Ho HH, Eaves DM. Subtypes of autism by cluster analysis. J Autism Dev Disord. 1994;24:3–22. doi: 10.1007/BF02172209. [DOI] [PubMed] [Google Scholar]
- 6.O’Brien SK. The validity and reliability of the Wing Subgroups Questionnaire. J Autism Dev Disord. 1996;26:321–335. doi: 10.1007/BF02172477. [DOI] [PubMed] [Google Scholar]
- 7.Volkmar FR, Cohen DJ, Bregman JD, Hooks MY, Stevenson JM. An examination of social typologies in autism. J Am Acad Child Adolesc Psychiatry. 1989;28:82–86. doi: 10.1097/00004583-198901000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Modahl C, Green L, Fein D, Morris M, Waterhouse L, Feinstein C, et al. Plasma oxytocin levels in autistic children. Biol Psychiatry. 1998;43:270. doi: 10.1016/S0006-3223(97)00439-3. [DOI] [PubMed] [Google Scholar]
- 9.Dawson G, Klinger LG, Panagiotides H, Lewy A, Castelloe P. Subgroups of autistic children based on social behavior display distinct patterns of brain activity. J Abnorm Child Psychol. 1995;23:569–583. doi: 10.1007/BF01447662. [DOI] [PubMed] [Google Scholar]
- 10.Zhang R, Jia MX, Zhang JS, Xu XJ, Shou XJ, Zhang XT, et al. Transcutaneous electrical acupoint stimulation in children with autism and its impact on plasma levels of arginine-vasopressin and oxytocin: a prospective single-blinded controlled study. Res Dev Disabil. 2012;33:1136. doi: 10.1016/j.ridd.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Ecker C, Spooren W, Murphy D. Developing new pharmacotherapies for autism. J Intern Med. 2013;274:308–320. doi: 10.1111/joim.12113. [DOI] [PubMed] [Google Scholar]
- 12.Odom S, Hume K, Boyd B, Stabel A. Moving beyond the intensive behavior treatment versus eclectic dichotomy: evidence-based and individualized programs for learners with ASD. Behav Modif. 2012;36:270. doi: 10.1177/0145445512444595. [DOI] [PubMed] [Google Scholar]
- 13.Schreibman L. Intensive behavioral/psychoeducational treatments for autism: Research needs and future directions. J Autism Dev Disord. 2000;30:373. doi: 10.1023/A:1005535120023. [DOI] [PubMed] [Google Scholar]
- 14.Volkmar FR, Paul R, Rogers SJ, Pelphrey KA, Powers MD, Palmieri MJ, et al. Behavioral assessment of individuals with autism: current practice and future directions. In: Volkmar FR, Paul R, Rogers SJ, Pelphrey KA (Eds.). Handbook of Autism and Pervasive Developmental Disorders, Fourth Edition. John Wiley & Sons, Inc., 2014.
- 15.Downs A, Smith T. Emotional understanding, cooperation, and social behavior in high-functioning children with autism. J Autism Dev Disord. 2004;34:625. doi: 10.1007/s10803-004-5284-0. [DOI] [PubMed] [Google Scholar]
- 16.Scheeren AM, Koot HM, Begeer S. Social interaction style of children and adolescents with high-functioning autism spectrum disorder. J Autism Dev Disord. 2012;42:2046–2055. doi: 10.1007/s10803-012-1451-x. [DOI] [PubMed] [Google Scholar]
- 17.Hoddenbach E, Koot HM, Clifford P, Gevers C, Clauser C, Boer F, et al. Individual differences in the efficacy of a short theory of mind intervention for children with autism spectrum disorder: a randomized controlled trial. Trials. 2012;13:206. doi: 10.1186/1745-6215-13-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Candini M, Giuberti V, Manattini A, Grittani S, Di PG, Frassinetti F. Personal space regulation in childhood autism: Effects of social interaction and person’s perspective. Autism Res. 2016;10:144–154. doi: 10.1002/aur.1637. [DOI] [PubMed] [Google Scholar]
- 19.Association AP. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). American Psychiatric Association, 2013.
- 20.Rellini E, Tortolani D, Trillo S, Carbone S, Montecchi F. Childhood Autism Rating Scale (CARS) and Autism Behavior Checklist (ABC) correspondence and conflicts with DSM-IV criteria in diagnosis of autism. J Autism Dev Disord. 2004;34:703. doi: 10.1007/s10803-004-5290-2. [DOI] [PubMed] [Google Scholar]
- 21.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 22.Rutter M, LeCouteur A, Lord C. The Autism Diagnostic Interview-Revised. Newcastle University. 2003;52:345–349. [Google Scholar]
- 23.Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30:205–223. doi: 10.1023/A:1005592401947. [DOI] [PubMed] [Google Scholar]
- 24.Lu Y, Fang J, Tian L, Jin H. Advanced Medical Statistics (2nd Edition). World Scientific, 2015.
- 25.Santos JRA. Cronbach’s alpha: A tool for assessing the reliability of scales. J Ext 1999, 37.
- 26.Bollen KA, Long JS. Testing Structural Equation Models. SAGE publications, Inc, 1993, 69: 66–67.
- 27.Downs A, Downs RC, Johansen M, Fossum M. Using discrete trial teaching within a public preschool program to facilitate skill development in students with developmental disabilities. Educ Treat Children. 2007;30:1–27. doi: 10.1353/etc.2007.0015. [DOI] [Google Scholar]
- 28.González-Calvo J, González VM, Lorig K. Cultural diversity issues in the development of valid and reliable measures of health status. Arthritis Care Res. 1997;10:448. doi: 10.1002/art.1790100613. [DOI] [PubMed] [Google Scholar]
- 29.Beglinger LJ, Smith TH. A review of subtyping in autism and proposed dimensional classification model. J Autism Dev Disord. 2001;31:411–422. doi: 10.1023/A:1010616719877. [DOI] [PubMed] [Google Scholar]
- 30.Taylor B. Vaccines and the changing epidemiology of autism. Child Care Health Dev. 2006;32:511–519. doi: 10.1111/j.1365-2214.2006.00655.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.