Abstract
Objectives
To examine associations between concentrations of hsTnI (measured using a single molecule counting method) and obstructive CAD in 1844 stable, symptomatic outpatients with suspected CAD randomized to coronary computed tomography angiography (CTA) in the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) trial.
Background
Elevated concentrations of high-sensitivity troponin I (hsTnI) are associated with coronary artery disease (CAD) in patients with myocardial infarction. The meaning of hsTnI concentrations in stable symptomatic outpatients is not well-understood.
Methods
Clinical characteristics and CTA results (including coronary artery calcium [CAC] scores) were expressed across hsTnI quartiles. Determinants of hsTnI concentration were identified. Multivariable logistic regression identified independent predictors of obstructive CAD50 (≥50% stenosis in any vessel) and CAD70 (≥70% stenosis or ≥50% left main).
Results
The median hsTnI concentration was 1.5 ng/L; nearly all (98.5%) subjects had measurable hsTnI, and 6.1% had concentrations ≥99th percentile concentration for this assay (6 ng/L). Higher CAC scores, as well as more prevalent and diffuse CAD, was seen in upper hsTnI quartiles (all P<0.001). Independent predictors of hsTnI concentrations included age, sex, and CAC score (all P<0.05). After adjusting for demographic and clinical characteristics, ln-transformed hsTnI concentrations were associated with obstructive CAD50 (odds ratio [OR]= 1.15 per interquartile range [IQR]; P=0.02) and CAD70 (OR = 1.25 per IQR; P=0.001).
Conclusions
In stable symptomatic outpatients undergoing non-emergent coronary CTA for diagnosis of suspected CAD, higher concentrations of hsTnI were associated with increasing presence and severity of coronary atherosclerosis (PROMISE; NCT01174550).
CLINICAL TRIAL
Keywords: troponin, coronary artery disease, coronary computed tomographic angiography
Introduction
Chest discomfort is one of the most commonly-encountered complaints in outpatient medicine, and represents a major diagnostic challenge. Stable patients with chest discomfort may be a diagnostic challenge as they often present with a broad range of non-specific symptoms or signs; though traditional risk factors for development of coronary artery disease (CAD) are important for development of disease, their role in assisting clinical decision making in the context of symptoms is somewhat more limited. Given this, classical history and physical examination for determining cause of chest discomfort is neither sensitive nor specific to identify obstructive CAD as the cause of this common complaint.
Adjunctive testing has been added to the armamentarium of the modern physician to assist in diagnostic detection of obstructive CAD. Such testing may include stress modalities with or without imaging. More recently, interest has grown regarding use of coronary computed tomographic angiography (CTA) for the diagnostic evaluation of chest discomfort. Advantages of coronary CTA include high sensitivity and negative predictive value (NPV) for obstructive CAD; coronary CTA also allows the opportunity to identify and quantify coronary artery calcium (CAC), itself a diagnostic and prognostic finding in patients with chest discomfort (1,2). Coronary CTA also can provide additional prognostic information through the detection of non-obstructive CAD (3).
Beyond imaging, development of circulating biomarkers to assist in the diagnostic evaluation of patients with suspected stable obstructive CAD would be of interest. High-sensitivity troponin (hsTn) has grown in use for evaluation of patients with more acute presentations, such as those with suspected myocardial infarction (MI); in such patients, concentrations of hsTn are now accepted as the biomarker gold standard for diagnosis of acute cardiac injury and correlate well with presence, extent and complication of obstructive CAD in these patients (4). In contrast, the meaning of hsTn concentrations in less acute patients—such as those presenting with stable chest discomfort in the outpatient setting—remains uncertain. In this analysis, we measured concentrations of hsTnI using a single molecule counting hsTnI assay in symptomatic outpatients in the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) trial randomized to CTA imaging (5,6). We hypothesized that concentrations of hsTnI would identify presence and quantify severity of CAD in these subjects.
Methods
All study procedures were approved by appropriate local or central institutional review boards.
Study design and population
Design and primary results of PROMISE (NCT01174550) have been previously published (5,6). In brief, PROMISE was a pragmatic comparative effectiveness trial enrolling 10003 participants at 193 sites in North America. Stable symptomatic outpatients without known CAD who were referred by their physician for non-urgent, non-invasive cardiovascular testing were randomly allocated to receive either functional testing (typically stress modalities, such as exercise electrocardiography, exercise or pharmacologic nuclear stress testing or stress echocardiography) versus coronary CTA. All patients were required to have a serum creatinine below 1.70 mg/dL. The PROMISE Diagnostic Testing Coordinating Center certified study sites with respect to testing methods. In addition, study participants were approached for consent for baseline blood collection to the PROMISE Study Biorepository; of these, 4022 consented for and had blood samples collected for measurement of hsTnI. No significant differences in baseline variables between those participating in the biorepository versus those who did not participate were found (Supplemental Table 1).
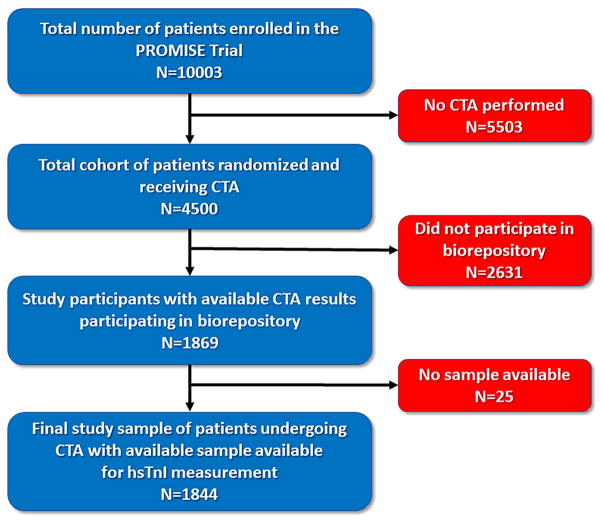
A study flow diagram is detailed in Figure 1. For the purposes of this analysis, we focused on those subjects who were randomized to and received coronary CTA with interpretable results and had available blood samples drawn prior to invasive angiography or revascularization or any acute coronary event. Thus, the total study sample for this analysis was 1844 subjects.
Figure 1.
A study flow for the present analysis. Following exclusions, 1844 subjects had available CT results and available blood samples for hsTnI testing.
hsTnI measurement
Concentrations of hsTnI were quantified using a single molecule counting method (SMC TnI; Singulex, Alameda, CA) on an Erenna Platform. This very highly sensitive TnI assay has a limit of detection of 0.5 ng/L and a 99th percentile reference limit of 6 ng/L in apparently healthy individuals (7). The assay, a quantitative fluorescent one-step sandwich immunoassay, was developed and validated to measure human cTnI levels in EDTA plasma samples. Samples and controls were added to a 96-well assay plate with an automated TECAN EVO 150 robotic system. Standards, capture reagent, and detection reagent were added to the assay plate. During incubation, the cTnI in the specimen bound to capture antibodies biotinylated to microparticles and to fluorescently-conjugated detection antibodies. After the unbound fluorescent detection antibody was removed by a wash procedure, an elution buffer was added to dissociate bead-bound antibody sandwiches, releasing fluorescent detection antibody into the eluent. The eluate was automatically transferred into a new microwell plate, which was then manually loaded onto the Erenna System for single molecule counting. For this study, the assay provided inter-run imprecision of 10% at 1.5 pg/mL and 6% at 13 pg/mL.
Coronary CTA
The methods for coronary CTA in the PROMISE Trial have been previously reported in detail (5). For the purposes of this analysis, presence and severity of CAD was based on site reads. Quantification of CAC was determined using the Agatston method (8). Site reports were assessed for the presence and extent of obstructive CAD as either CAD50 (≥50% stenosis in any vessel ≥2.0 mm in diameter) or CAD70 (≥70% stenosis in any vessel ≥2.0 mm in diameter or ≥50% stenosis involving the left main coronary artery).
Statistical methods
Baseline characteristics across hsTnl quartiles were compared using a Chi-squared test for categorical variables and the Kruskal–Wallis test for continuous variables. All models used the same pre-specified set of covariates: age, sex, smoking, diabetes mellitus, systolic blood pressure, race and use of antihypertensive medications. Multivariable linear regression was utilized to identify independent predictors of log-transformed hsTnI concentrations. Effect sizes in the linear model were reported as the difference between 75th and 25th quartiles for continuous variables, while race was modeled as “white”, “black”, and “other”. The rate of missingness was low and missing values were imputed with medians for continuous variables and the most frequent category for categorical variables. CAC scores were log-transformed for all analyses and the Spearman correlation was used to examine association between log-transformed CAC scores and log-transformed hsTnI concentration. Receiver operator characteristic (ROC) curves examined diagnostic utility of hsTnI for the goal standard outcomes of any CAD, CAD50 and CAD70; the area under the curve (AUC) and operating characteristics such as sensitivity, specificity, and positive and negative predictive value (PPV, NPV) were determined. Distribution of CAD50 and CAD70 across quartiles of hsTnI was evaluated, including average proportion of vessels with significant stenoses; in a similar fashion, we performed these analyses using the 99th percentile concentration for a healthy population of 6 ng/L as well as the 99th percentile value from the PROMISE Trial of 32.7 ng/L. Model-based predicted probabilities were estimated by fixing covariates at their median or most frequent category; hsTnI was varied over its observed range. In a second model, hsTnI was dichotomized at the 99th percentile of 6 ng/L.
Multivariable logistic regression analyses was used to evaluate the association between hsTnI and presence of CAD50 and CAD70. The model included traditional risk factors for CAD, including age, male sex, current smoking, diabetes mellitus, systolic blood pressure, and black race; hsTnI results were then fitted into this base model. The non-linearity of continuous predictors was assessed using restricted cubic splines, and a linear functional form was found to be adequate. The incremental value of adding hsTnI to a base model including pre-specified covariates (listed above) was further evaluated via change in model discrimination and a likelihood ratio test; calibration of models was assessed using the Hosmer-Lemeshow test. Lastly, reclassification of model performance with addition of hsTnI was tested using the category-free net reclassification improvement (NRI) method (9). P values are two-sided, with results <0.05 considered significant. All analyses were performed in the R environment for statistical computing (R Foundation for Statistical Computing, Vienna, Austria) (10).
Results
Baseline hsTnI concentrations
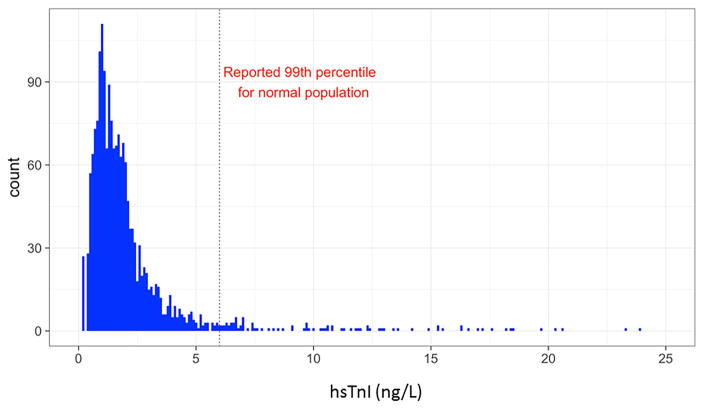
A histogram of hsTnI concentrations in the study participants is displayed as Figure 2. Among study participants, concentrations of hsTnI ranged from below the limit of detection of 0.5 ng/L to a maximum of 1434.6 ng/L; 98.5% had a measurable hsTnI. The median hsTnI value for the whole group was 1.5 (IQR 1.0, 2.4) ng/L. Notably, 6.1% of study participants were ≥ 6 ng/L, the assay’s 99th percentile for patients free of risk factors for CAD or prevalent atherosclerosis, heart failure, or kidney disease. The 99th percentile hsTnI concentration for the PROMISE Trial was 32.7 ng/L.
Figure 2.
Distribution of hsTnI in patients from PROMISE with available CT data. The median hsTnI concentration was 1.5 ng/L, with 6.1% above the 99th percentile for a healthy population (6 ng/L).
Baseline clinical characteristics
Clinical characteristics as a function of hsTnI quartiles are detailed in Table 1. In higher hsTnI quartiles, we observed increasing prevalence and number of CAD risk factors; patients in the higher hsTnI quartiles were more likely to be older, to be male, and to have prevalent risk factors and/or preventive treatment for CAD. Clinical characteristics as a function of the 99th percentile value of 6 ng/L are detailed in Supplemental Table 2.
Table 1.
Baseline characteristics as a function of hsTnI quartiles.
| hsTnI Quartile | |||||
|---|---|---|---|---|---|
|
| |||||
| Characteristic | Q1 (≤1.0 ng/L) N=537 |
Q2 (1.1–1.5 ng/L) N=391 |
Q3 (1.6–2.4 ng/L) N=483 |
Q4 ≥2.5 ng/L N=433 |
P value |
| Age, years, mean (SD) | 57.3 (6.9) | 60.1 (7.5) | 60.5 (8.4) | 61.2 (8.6) | <0.001 |
|
| |||||
| Males, N (%) | 193 (35.9%) | 172 (44.0%) | 261 (54.0%) | 247 (57.0%) | <0.001 |
|
| |||||
| Race, N (%) | 0.09 | ||||
| Black | 39 (7.3%) | 29 (7.4%) | 44 (9.1%) | 53 (12.2%) | |
| Other | 20 (3.7%) | 14 (3.6%) | 23 (4.8%) | 12 (2.8%) | |
| White | 475 (88.5%) | 347 (88.7%) | 413 (85.5%) | 367 (84.8%) | |
|
| |||||
| Cardiac risk factors, N (%) | |||||
| Hypertension | 294 (54.7%) | 270 (69.1%) | 325 (67.3%) | 309 (71.4%) | <0.001 |
| Dyslipidemia | 372 (69.3%) | 271 (69.3%) | 320 (66.3%) | 274 (63.3%) | 0.17 |
| PAD or Cerebrovascular Disease | 21 (3.9%) | 16 (4.1%) | 31 (6.4%) | 29 (6.7%) | 0.11 |
| Diabetes | 99 (18.4%) | 80 (20.5%) | 93 (19.3%) | 107 (24.7%) | 0.09 |
| Smoker | 0.48 | ||||
| Never | 254 (47.3%) | 205 (52.4%) | 234 (48.4%) | 196 (45.3%) | |
| Current | 103 (19.2%) | 62 (15.9%) | 88 (18.2%) | 90 (20.8%) | |
| Former | 180 (33.5%) | 124 (31.7%) | 161 (33.3%) | 147 (33.9%) | |
| Family history of premature CAD | 217 (40.4%) | 119 (30.4%) | 159 (32.9%) | 122 (28.2%) | <0.001 |
| Depression | 135 (25.1%) | 93 (23.8%) | 105 (21.7%) | 105 (24.2%) | 0.64 |
| Sedentary lifestyle | 242 (45.1%) | 190 (48.6%) | 221 (45.8%) | 207 (47.8%) | 0.68 |
|
| |||||
| Framingham Risk Score, mean (SD) | 16.0 (10.9) | 19.4 (13.0) | 22.5 (14.7) | 26.3 (16.9) | <0.001 |
|
| |||||
| BMI, Kg/m2, mean (SD) | 29.9 (5.5) | 30.6 (5.9) | 30.3 (5.3) | 31.2 (5.7) | 0.002 |
|
| |||||
| SBP, mm Hg, mean (SD) | 126.8 (15.2) | 130.3 (16.6) | 131.7 (16.9) | 135.3 (16.4) | <0.001 |
|
| |||||
| DBP, mm Hg, mean (SD) | 77.6 (9.6) | 78.6 (10.0) | 78.4 (10.2) | 80.4 (10.0) | <0.001 |
|
| |||||
| Type of angina, N (%) | 0.96 | ||||
| Typical | 64 (11.9%) | 49 (12.5%) | 62 (12.8%) | 57 (13.2%) | |
| Atypical | 423 (78.8%) | 303 (77.5%) | 382 (79.1%) | 339 (78.3%) | |
| Non-cardiac | 50 (9.3%) | 39 (10.0%) | 39 (8.1%) | 37 (8.5%) | |
|
| |||||
| Medication, N (%) | |||||
| Aspirin | 214 (39.9%) | 184 (47.1%) | 238 (49.3%) | 196 (45.3%) | 0.01 |
| Statin | 242 (45.1%) | 177 (45.3%) | 195 (40.4%) | 188 (43.4%) | 0.55 |
| Beta blocker | 107 (19.9%) | 88 (22.5%) | 126 (26.1%) | 133 (30.7%) | <0.001 |
| ACEi or ARB | 173 (32.2%) | 177 (45.3%) | 189 (39.1%) | 220 (50.8%) | <0.001 |
| Antihypertensive | 284 (52.9%) | 237 (60.6%) | 295 (61.1%) | 298 (68.8%) | <0.001 |
SD denotes: standard deviation; PAD denotes: peripheral arterial disease; CAD denotes: coronary artery disease; BMI denotes: body-mass index; Kg denotes: kilogram; m denotes: meter; SBP denotes: systolic blood pressure; DBP denotes: diastolic blood pressure; mmHg denotes: millimeters of mercury; ACEi denotes: angiotensin converting enzyme inhibitor; ARB denotes: angiotensin receptor blocker.
Predictors of hsTnI concentration
In multivariable linear regression models, independent predictors of log hsTnI concentration included age, male sex, Black race, use of antihypertensives, and systolic blood pressure (all P<0.005; Supplemental Figure 1A). Notably, CAC scores (missing in 10.1% of subjects and imputed by single imputation) exhibited weak bivariate correlation with log hsTnI (ρ =0.16; P <0.001; Supplemental Figure 2); when added to multivariable linear regression models, CAC remained an independent predictor of hsTnI (difference per IQR [6.5] was estimated at 0.093; 95% CI 0.004–0.182, P=0.04; Supplemental Figure 1B).
Coronary CTA and hsTnI
Table 2 details results of coronary CTA as a function of hsTnI quartiles. With higher concentrations of hsTnI, we observed more prevalent and more extensive obstructive CAD with higher CAC scores, higher average most significant stenosis, and greater frequency or proportion of vessels with CAD50 or CAD70. Those in the highest hsTnI quartile had a nearly 8-fold higher median CAC score, and near doubling in prevalence of obstructive CAD between lowest and highest quartile. Results of CTA as a function of the 99th percentile value of 6 ng/L as well as for the 99th percentile of the PROMISE Trial population (32.7 ng/L) are detailed in Supplemental Table 3; those subjects above both cut-offs had more diffuse and severe CAD.
Table 2.
Presence and extent of coronary artery calcium or obstructive coronary artery disease as a function of hsTnI quartile.
| hsTnI quartile | |||||
|---|---|---|---|---|---|
| Q1 (≤1.0 ng/L) N=537 |
Q2 (1.1–1.5 ng/L) N=391 |
Q3 (1.6–2.4 ng/L) N=483 |
Q4 ≥2.5 ng/L N=433 |
P value | |
| Coronary artery calcium score, median (IQR) | 5.0 (0.0,90.2) | 25.0 (0.0,144.9) | 36.9 (0.0,266.1) | 38.5 (0.0,247.0) | <0.001 |
| Coronary artery calcium score = 0, N (%) | 212 (39.5%) | 128 (32.7%) | 125 (25.9%) | 124 (28.6%) | <0.001 |
| Coronary artery calcium score = 1–99, N (%) | 154 (28.7%) | 121 (30.9%) | 132 (27.3%) | 108 (24.9%) | 0.32 |
| Coronary artery calcium score ≥100, N (%) | 113 (21.0) | 109 (27.9) | 171 (35.4) | 157 (36.3) | <0.001 |
| ≥50% stenosis, N (%) | 102 (19.0%) | 89 (22.8%) | 130 (26.9%) | 128 (29.6%) | <0.001 |
| ≥70% stenosis or left main stenosis ≥50%, N (%) | 51 (9.5%) | 41 (10.5%) | 65 (13.5%) | 70 (16.2%) | 0.009 |
| Average proportion of vessels with ≥50% stenosis | 7.0% | 8.3% | 10.8% | 12.7% | <0.001 |
| Average proportion of vessels with ≥70% stenosis or left main stenosis ≥50% | 3.2% | 3.2% | 4.7% | 6.7% | 0.004 |
hsTnI to evaluate absence or presence of CAD
Given association between hsTnI and prevalent CAD, we then examined whether concentrations of hsTnI could exclude or predict presence of CAD of varying severities.
Relative to exclusion of any CAD, of the 1845 study participants, 615 (33.4%) had no evidence of even minor CAD or any CAC. In ROC analyses, hsTnI yielded an AUC of 0.57 (95% CI = 0.54–0.60; P <0.001); assuming need for low hsTnI concentrations to exclude presence of any anatomically-defined CAD, we evaluated a range of hsTnI values starting at the median for the group (1.5 ng/L) to the limit of detection (0.5 ng/L) and found no cut-off providing NPV greater than 49%. As expected, therefore, in a model designed to exclude presence of any CAD in the PROMISE Trial (11), concentrations of hsTnI did not add to the model discrimination, calibration or reclassification (results not shown).
We then examined whether higher concentrations of hsTnI predict or exclude presence of obstructive CAD50 or CAD70. In ROC analyses for the diagnosis of CAD50, hsTnI had AUC of 0.57 (95% CI = 0.54–0.60; P <0.001) while for CAD70, similar AUC of 0.59 (95% CI = 0.55–0.63; P <0.001). At the 99th percentile value of 6.0 ng/L, hsTnI had sensitivity of 9% (95% CI=6–12%), specificity of 95% (95% CI=93–96%), PPV of 35% (95% CI =27–45%) and NPV of 76% (95% CI=74–78%) for CAD50. Corresponding operating characteristics for CAD70 were sensitivity of 11% (95% CI=7–16%), specificity of 95% (95% CI=93–96%), PPV of 22% (95% CI =15–31%) and NPV of 88% (95% CI=87–90%). Using the optimal value from the ROC via the Youden method (1.6 ng/L), hsTnI had a sensitivity of 57% (95% CI=53–62%), specificity of 53% (95% CI=50–55%) with PPV of 28% (95% CI=25–31%) and NPV of 90% (95% CI=77–82%) for CAD50. Corresponding operating characteristics for CAD70 were sensitivity of 47% (95% CI=40–53%), specificity of 67% (95% CI=64–69%), PPV of 16% (95% CI =14–19%) and NPV of 90% (95% CI=88–92%).
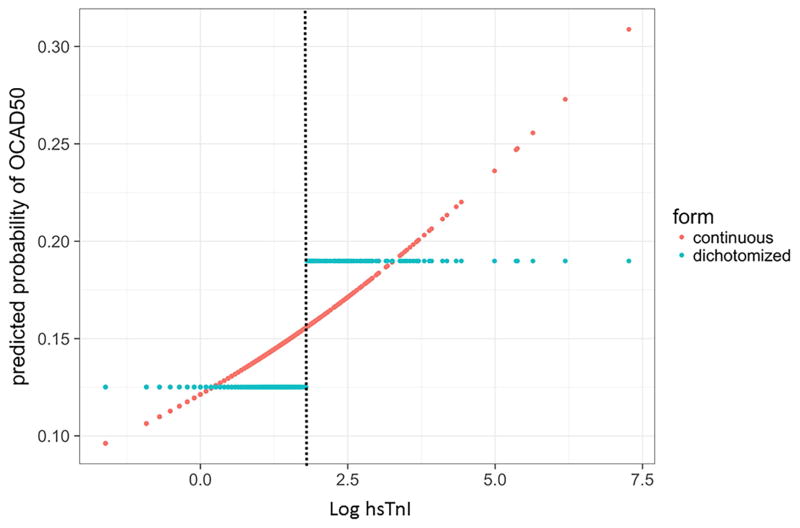
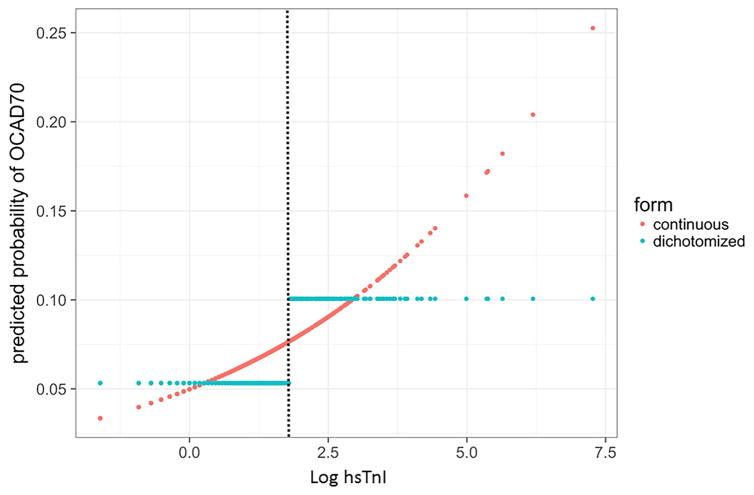
Figure 3 details predicted probability of CAD50 and CAD70 as a function of log-transformed hsTnI or dichotomized around the 99th percentile hsTnI concentration of 6 ng/L. In multivariable modeling including demographics and traditional risk factors to identify obstructive CAD (Table 3), log-transformed concentrations of hsTnI were independent predictors of CAD50 (OR = 1.15 per IQR of log hsTnI; 95% CI = 1.12–1.48; P =0.02) and CAD70 (OR = 1.25 per IQR of log hsTnI; 95% CI = 1.09–1.44; P=0.001); in this analysis, the IQR corresponds to a 0.875 difference on the log scale. Addition of concentrations of hsTnI to a base model for CAD50 increased the C-statistic from 0.68 to 0.69; in doing so, the likelihood ratio test was significant (P = 0.02), and the model demonstrated adequate calibration (Hosmer-Lemeshow P value of 0.30); adding hsTnI resulted in a non-significant change in the category-free NRI of 0.04 (95% CI = −0.068–0.14) beyond the base model (event NRI + non-event NRI = −0.149 + 0.1857). Similarly, in a model for CAD70 addition of hsTnI increased the C-statistic (0.68 to 0.69), the likelihood ratio was significant (P=0.002), and the model demonstrated adequate calibration (Hosmer-Lemeshow P = 0.21). The category-free NRI analysis again demonstrated non-significant change in the continuous NRI for obstructive CAD (category-free NRI = 0.11; 95% CI = −0.32–0.24) beyond the base model (event NRI + non-event NRI = −0.137–0.242).
Figure 3.
Predicted probabilities of A) coronary stenosis ≥50% in any vessel or B) coronary stenosis ≥70% in any vessel or left main coronary artery stenosis ≥50% as a function of hsTnI concentration. Probability for obstructive CAD is depicted as continuous log-transformed hsTnI concentration (red dots) as well as dichotomized around the 99th percentile concentration of 6 ng/L (blue dots). In both figures, the 99th percentile cut-off of 6 ng/L is identified by a dotted line.
Table 3.
Multivariable models to predict presence of any vessel with A) ≥50% stenosis or B) ≥70% stenosis or left main stenosis ≥50%. Addition of hsTnI concentrations to each model increased the C-statistic, improved calibration, and led to reclassification for correct diagnosis.
| A) | |||
|---|---|---|---|
| Variable | Odds ratio | 95% Confidence Interval | P value |
| Age | 1.78 | 1.49–2.11 | <0.001 |
| Male sex | 2.38 | 1.89–3.01 | <0.001 |
| Current smoking | 1.62 | 1.21–2.16 | 0.001 |
| Diabetes mellitus | 1.85 | 1.42–2.41 | <0.001 |
| Systolic blood pressure | 1.29 | 1.12–1.48 | <0.001 |
| hsTnI | 1.15 | 1.03–1.29 | 0.02 |
| Black race | 0.59 | 0.38–0.91 | 0.03 |
| B) | |||
|---|---|---|---|
| Variable | Odds ratio | 95% Confidence Interval | P value |
| Age | 1.63 | 1.31–2.03 | <0.001 |
| Male sex | 2.55 | 1.88–3.46 | <0.001 |
| Current smoking | 1.67 | 1.16–2.39 | 0.006 |
| Diabetes mellitus | 1.74 | 1.25–2.44 | 0.001 |
| Systolic blood pressure | 1.23 | 1.04–1.47 | 0.02 |
| HsTnI | 1.25 | 1.09–1.44 | 0.001 |
| Black race | 0.43 | 0.22–0.82 | 0.04 |
Discussion
In our study from the PROMISE Trial, we tested blood using a very highly sensitive “single molecule counting” assay for TnI. We found concentrations of hsTnI were measurable in nearly all study participants, with a broad range of hsTnI concentrations detected. Those stable symptomatic outpatients with higher concentrations of hsTnI had more prevalent risk factors for CAD, and on non-invasive imaging, higher concentrations of hsTnI were associated with increasing presence and severity of CAD, as reflected in CAC scores or evidence of obstructive disease on CTA. In models adjusted for traditional risk factors, higher hsTnI concentrations independently predicted moderate and severe coronary obstruction. Thus, presence and severity of CAD is an important determinant of hsTnI concentrations in those with stable chest discomfort, though the diagnostic role of the biomarker in such patients is not clarified: while lower concentrations provided NPV approaching 90%, no hsTnI concentration had high enough PPV or NPV for CAD in the same manner as it is for diagnosis of acute MI (4).
The standard approach for evaluation of patients with suspected CAD includes diagnostic imaging modalities, including stress testing (with/without nuclear or echo imaging); newer approaches, such as coronary CTA are now being explored, which may afford value for evaluating stable chest pain (1,6). Though imaging has substantial advantages it may have drawbacks, including higher cost, limited availability, time lag for completion relative to presentation, need for ionizing radiation in some cases and requirement for specialized interpretation. Thus, a more rapidly available means by which to supplement clinical decision making in this setting would be welcome. Biomarker testing might be a reasonable approach to support clinical information and/or other objective test information to assist in diagnosis of CAD (11).
Given prior studies suggesting associations between hsTnI and presence of CAD in patients without ACS (12), we hypothesized concentrations of TnI as measured with the very highly sensitive ‘single molecule’ counting assay employed in this study would be helpful in this regard. Indeed, measurement of hsTn for evaluating stable chest pain is a reasonable prospect, but has not been well-explored. Among 378 patients with stable angina and unknown CAD status in the Evaluation of Integrated Cardiac Imaging (EVINCI) study, concentrations of hsTnT were higher in those with CAD (13); much as in our study, extent of atherosclerosis was independently associated with hsTnT concentrations in EVINCI. In a separate study of 99 study participants from the Virtual Histology in Vulnerable Atherosclerosis trial (14), Brown and colleagues examined results from intra-coronary ultrasound as a function of a different hsTnI method than used in our analysis, demonstrating hsTnI concentrations were associated with higher risk plaque features such as higher plaque burden and more thin-capped fibroatheroma; hsTnI also predicted risk for major adverse cardiovascular events during 3.5 year follow up of this small study cohort (15). In our analysis, using a more sensitive hsTnI assay, we substantially extend understanding of the role this biomarker may play in stable chest pain evaluation. An important observation was the demonstrated graded association between hsTnI and CAD, present well within the normal range for this assay. Though the 99th percentile value of this assay is 6 ng/L (found in the upper quartile of our subjects), we nonetheless found a monotonic rise in CAC scores and prevalence of obstructive CAD from the lowest hsTnI quartile (<1.0 ng/L) to the highest (≥2.5 ng/L).
Though CAD plays a role in partially determining hsTnI concentrations in our subjects, it is clear more work is necessary to understand this finding. Prior work with this assay in patients undergoing functional testing utilizing stress nuclear imaging suggest those with higher hsTnI concentrations were more likely to have inducible perfusion defects, suggesting greater ischemic burden contributes to higher concentrations of the biomarker (16). In moderate-risk patients with acute chest discomfort presenting to the Emergency Department subsequently judged to be without acute coronary syndrome, hsTnI was associated with prevalent coronary atherosclerosis as assessed by coronary CTA (12,17). Our findings extend these observations, demonstrating independent association of CAD with hsTnI concentrations in much more stable patients. Burden of CAD and consequent coronary injury is therefore a likely contributor to why hsTnI might be higher in such patients. However, while CAD presence and extent plays a significant role, our results suggest this is a modest contributor. Taken together, while our data suggest more refined and sensitive Tn methods may be influenced by presence of obstructive CAD in a more stable chest pain population, stand-alone measurement of hsTnI cannot replace imaging for the diagnosis or exclusion of coronary atherosclerosis in stable patients. However, integrative role of hsTnI with clinical variables and imaging (including coronary CTA, CAC scoring, or myocardial perfusion imaging) to optimize diagnostic accuracy for those patients at higher risk is currently being explored. Furthermore, we are analyzing prognostic meaning of hsTnI at enrollment in PROMISE; a testable hypothesis will be to explore how hsTnI concentrations may be useful to triage downstream testing based on risk as opposed to coronary anatomy alone.
Though our data are novel, it is necessary to accept limitations of our study. First, this is a moderate size, well-characterized cohort of patients enrolled in a clinical trial subject to inclusion/exclusion criteria, thus our results may not extend to more “every day” patients; on the other hand, the pragmatic design of the PROMISE Trial together with measurement of blood samples obtained prior to coronary CTA, along with use of site reads for the coronary CTA results make the associations between hsTnI and CAD presence/severity compelling, and likely more broadly applicable. The hsTnI method used in this study is more highly sensitive than other methods that are currently commercially available; our results therefore do not necessarily extend to other hsTn methods. We did not examine sex-specific hsTnI cut-offs, though it is hard to envision substantial difference in results, given associations between hsTnI and CAD were found so deeply into the normal range. Though hsTnI concentrations independently predicted CAD presence, neither the PPV or NPV was sufficient to use the test as a stand-alone modality; the role of hsTnI in this setting remains to be determined. Understanding discordant groups (such as those with significant CAD but with low hsTnI or those without CAD but high hsTnI) may help to further inform a role. Further, efforts toward understanding a potential prognostic role for hsTnI in PROMISE is being explored. In this regard, the optimal utility of hsTnI in patients with stable chest pain may be to assess risk for major adverse cardiovascular events and inform future diagnostic strategies; such analyses are underway in this cohort.
In conclusion, among stable outpatient participants with chest pain enrolled in the PROMISE Trial, increasing concentrations of hsTnI were significantly associated with presence and severity of CAD subsequently diagnosed with coronary CTA. Future studies are needed in larger and more diverse patient populations with stable chest pain to better understand how hsTnI measurement integrated with further diagnostic studies might facilitate accurate, safe and cost-effective evaluation.
Supplementary Material
Perspectives.
Competency in medical knowledge
The role of troponin testing in patients with less acute presentations, such as stable outpatients, is unknown. In the PROMISE Trial of stable outpatients with suspected CAD, concentrations of hsTnI were significantly with CAC as well as obstructive CAD. The role of hsTnI for diagnostic testing in this population remains ambiguous however.
Translational outlook
Understanding factors leading to hsTnI elevation in stable patients with obstructive CAD may lead to new therapies for treatment of the diagnosis.
Acknowledgments
Funding: Sponsored in part by an unrestricted grant from Singulex, Inc. This project was also supported by grants R01HL098237, R01HL098236, and R01HL98305 from the National Heart, Lung, and Blood Institute (NHLBI). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents. This paper does not necessarily represent the official views of NHLBI. Dr. Januzzi is supported in part by the Hutter Family Professorship in Cardiology. Dr. Ferencik was supported in part by American Heart Association Fellow to Faculty Award 13FTF16450001.
Abbreviations
- AIC
Akaike information criterion
- CAC
Coronary artery calcium
- CAD
Coronary artery disease
- CTA
Computed tomographic angiography
- hsTn
High-sensitivity troponin
- MI
Myocardial infarction
- NPV
Negative predictive value
- PPV
Positive predictive value
- PROMISE
Prospective Multicenter Imaging Study for Evaluation of Chest Pain
- ROC
Receiver operator characteristic
Footnotes
Disclosures: Dr. Januzzi reports grant support from Singulex, consulting income from Roche Diagnostics, Critical Diagnostics, Philips, and Novartis, and participates in clinical endpoint committees/data safety monitoring boards for Siemens, Abbvie, Pfizer, Amgen, Janssen, and Boehringer Ingelheim; Dr. Patel has received research grants from AstraZeneca, Janssen, Bayer, NHLBI, Philips, and Heartflow, and serves on advisory boards for Janssen, AstraZeneca, and Bayer. Dr. Hoffmann has received research grants from HeartFlow and Kowa Pharmaceuticals. Dr. Ginsburg has served as a consultant or advisory board member for CardioDx, Interleukin Genetics, Pappas Ventures, Fabric Genomics, Genome Magazine; has stock options from CardioDx, Alere, Fabric Genomics, and Origin Commercial Advisors; has served on the board of directors for Alere; and has received royalties from Elsevier and research funding to his institution from Singulex, Abbott, and 23andMe. Dr. Douglas has received research grants from GE and HeartFlow.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bittner DO, Ferencik M, Douglas PS, Hoffmann U. Coronary CT Angiography as a Diagnostic and Prognostic Tool: Perspective from a Multicenter Randomized Controlled Trial: PROMISE. Curr Cardiol Rep. 2016;18:40. doi: 10.1007/s11886-016-0718-9. [DOI] [PubMed] [Google Scholar]
- 2.Budoff MJ, Mayrhofer T, Ferencik M, et al. The Prognostic Value of Coronary Artery Calcium in the PROMISE Study. Circulation. 2017;136(21):1993–2005. doi: 10.1161/CIRCULATIONAHA.117.030578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoffmann U, Ferencik M, Udelson JE, et al. Prognostic Value of Noninvasive Cardiovascular Testing in Patients With Stable Chest Pain: Insights From the PROMISE Trial (Prospective Multicenter Imaging Study for Evaluation of Chest Pain) Circulation. 2017;135:2320–2332. doi: 10.1161/CIRCULATIONAHA.116.024360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60:1581–98. doi: 10.1016/j.jacc.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Douglas PS, Hoffmann U, Lee KL, et al. PROspective Multicenter Imaging Study for Evaluation of chest pain: rationale and design of the PROMISE trial. Am Heart J. 2014;167:796–803e1. doi: 10.1016/j.ahj.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Douglas PS, Hoffmann U, Patel MR, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372:1291–300. doi: 10.1056/NEJMoa1415516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Estis J, Wu AHB, Todd J, Bishop J, Sandlund J, Kavsak PA. Comprehensive age and sex 99th percentiles for a high-sensitivity cardiac troponin I assay. Clin Chem. 2017 doi: 10.1373/clinchem.2017.276972. In Press. [DOI] [PubMed] [Google Scholar]
- 8.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 9.Pencina MJ, D’Agostino RB, Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011;30:11–21. doi: 10.1002/sim.4085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrell F. Regression Modeling Strategies. R Foundation for Statistical Computing; 2017. [Google Scholar]
- 11.Ibrahim NE, Januzzi JL, Jr, Magaret CA, et al. A Clinical and Biomarker Scoring System to Predict the Presence of Obstructive Coronary Artery Disease. J Am Coll Cardiol. 2017;69:1147–1156. doi: 10.1016/j.jacc.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 12.Januzzi JL, Jr, Bamberg F, Lee H, et al. High-sensitivity troponin T concentrations in acute chest pain patients evaluated with cardiac computed tomography. Circulation. 2010;121:1227–34. doi: 10.1161/CIRCULATIONAHA.109.893826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caselli C, Prontera C, Liga R, et al. Effect of Coronary Atherosclerosis and Myocardial Ischemia on Plasma Levels of High-Sensitivity Troponin T and NT-proBNP in Patients With Stable Angina. Arterioscler Thromb Vasc Biol. 2016;36:757–64. doi: 10.1161/ATVBAHA.115.306818. [DOI] [PubMed] [Google Scholar]
- 14.Brown AJ, Shah AS, West NE, et al. High-Sensitivity Troponin I is Associated With High-Risk Plaque and MACE in Stable Coronary Artery Disease. JACC Cardiovasc Imaging. 2017;10(10 Pt A):1200–1203. doi: 10.1016/j.jcmg.2016.09.025. [DOI] [PubMed] [Google Scholar]
- 15.Calvert PA, Obaid DR, O’Sullivan M, et al. Association between IVUS findings and adverse outcomes in patients with coronary artery disease: the VIVA (VH-IVUS in Vulnerable Atherosclerosis) Study. JACC Cardiovasc Imaging. 2011;4:894–901. doi: 10.1016/j.jcmg.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Lee G, Twerenbold R, Tanglay Y, et al. Clinical benefit of high-sensitivity cardiac troponin I in the detection of exercise-induced myocardial ischemia. Am Heart J. 2016;173:8–17. doi: 10.1016/j.ahj.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 17.Januzzi JL, Sharma U, Zakroysky P, et al. Sensitive troponin assays in patients with suspected acute coronary syndrome: Results from the multicenter rule out myocardial infarction using computer assisted tomography II trial. Am Heart J. 2015;169:572–8e1. doi: 10.1016/j.ahj.2014.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.