Abstract
Background/Aims
We evaluated the management and educational status of adult anaphylaxis patients at emergency departments (EDs).
Methods
Anaphylaxis patients who visited ED from 2011 to 2013 were enrolled from three hospitals. We analyzed clinical features, prior history of anaphylaxis, management and provided education for etiology and/or prevention. For analyzing associated factors with epinephrine injection, Pearson chi-square test was used by SPSS version 21 (IBM Co.).
Results
A total of 194 anaphylaxis patients were enrolled. Ninety-nine patients (51%) visited ED by themselves. Time interval from symptom onset to ED visit was 62 ± 70.5 minutes. Drug (56.2%) was the most frequent cause of anaphylaxis. Forty-seven patients (24.2%) had prior history of anaphylaxis and 33 patients had same suspicious cause with current anaphylaxis. Cutaneous (88.7%) and respiratory (72.7%) symptoms were frequent. Hypotension was presented in 114 patients (58.8%). Mean observation time in ED was 12 ± 25.7 hours and epinephrine was injected in 114 patients (62%). In 68 patients, epinephrine was injected intramuscularly with mean dose of 0.3 ± 0.10 mg. Associated factor with epinephrine injection was hypotension (p = 0.000). Twenty-three patients (13%) were educated about avoidance of suspicious agent. Epinephrine auto-injectors were prescribed only in five patients. Only 34 (19%) and 72 (40%) patients were consulted to allergist at ED and outpatient allergy department respectively.
Conclusions
We suggested that management and education of anaphylaxis were not fully carried out in ED. An education and promotion program on anaphylaxis is needed for medical staff.
Keywords: Patient care management, Education, Professional, Anaphylaxis, Emergency medical services
INTRODUCTION
Anaphylaxis is a serious generalized hypersensitivity reaction that could lead to death and occurs through an immunologic or non-immunologic mechanism [1,2]. This condition is very rare and the true prevalence is unknown because of underdiagnosis [2]. In international studies, the lifetime prevalence of anaphylaxis was estimated at 0.05% to 2% [3]. In Korea, according to a recent multicenter study [4], the prevalence of anaphylaxis was 13.30 cases per 100,000 adult patients visiting hospitals and 47.33 cases per 100,000 adult visitors in emergency departments (EDs) in 2011. It is not easy to notice the cause of anaphylaxis in some patients, and in these patients, the opportunity for appropriate management could be missed. Thus, clarifying the cause of anaphylaxis and providing education to avoid suspicious causes are very important in the prevention of anaphylaxis recurrence especially in an emergent setting. In addition, doctors should help patients to avoid triggering factors and educate them on how to use epinephrine auto-injectors in emergency situations. We collected the medical record data of anaphylaxis patients and evaluated whether management and education were done appropriately at three domestic university hospital EDs.
METHODS
Participants and data collection
Adult patients (age over 18-year-old) who visited the EDs from 2011 to 2013 were enrolled from two tertiary hospitals and one secondary hospital in Korea. We reviewed the electronic medical records retrospectively by searching for the following International Statistical Classification of Disease (ICD) codes for the anaphylaxis group: anaphylactic shock/anaphylaxis (T78.0), anaphylaxis, unspecified (T78.2), anaphylactic shock due to serum (T80.5) and anaphylactic shock due to adverse effect from the correct drug or from medicament properly administered (T88.6), and for additional diagnoses, insect allergy (T63.4), food allergy (T87.1), allergy angioedema (T78.3), allergy (T78.4), antibiotics, aspirin, contrast media, drug, nonsteroidal anti-inflammatory drug allergy (T88.7), other urticaria (L50.88), acute urticaria (L50.9), and anaphylactic reaction due to arthropod bite (T63.4). We re-confirmed a diagnosis of anaphylaxis according to the diagnostic criteria described below in all collected cases. However, we did not exclude patients who were diagnosed as anaphylaxis by their clinician even if their information was insufficient. Clinical information about clinical features, prior history of anaphylaxis, management and education was collected.
This study was approved as deliberation exemption by the Institutional Review Board of Inje University Busan Paik Hospital (IRB No. 14-0097). This study based on medical record, so there was no need for informed consent.
Diagnostic criteria of anaphylaxis
We used the diagnostic criteria according to the anaphylaxis guideline of the World Allergy Organization (WAO) [5]. Anaphylaxis is highly likely when any one of the following criteria here is fulfilled: (1) sudden onset of an illness, with involvement of the skin, mucosal tissue, or both and at least one of the following: sudden respiratory symptoms and signs or sudden reduced blood pressure (BP) or symptoms of end-organ dysfunction; (2) two or more of the following that occur suddenly after exposure to a likely allergen or other trigger for that patient: sudden skin or mucosal symptoms and signs, sudden respiratory symptoms and signs, sudden reduced BP or symptoms of end-organ dysfunction or sudden gastrointestinal symptoms; and (3) reduced BP after exposure to a known allergen for that patient.
Statistical analysis
Statistical analyses were performed with SPSS version 21.0 (IBM Co., Armonk, NY, USA). We did statistical analyses using linear regression and independent samples t test to evaluate associated factors about the duration of the emergency room stay. Pearson chi-square test was used to analyze associated factors with the injection of epinephrine. Results were considered significant when two-sided p values were < 0.05.
RESULTS
Clinical characteristics of the patients
We enrolled 194 anaphylaxis patients who were diagnosed as anaphylaxis at our hospitals or at transferred hospitals. One hundred and eighty-five patients (95.4%) fulfilled the criteria according to the World Health Organization (WHO) criteria, but nine patients could not be assessed because of insufficient information (Supplementary Table 1). The characteristics of the anaphylaxis patients are described in Table 1. The mean age was 46 ± 17.1 years, and 87 patients (45%) were men. Only 52 patients (26.8%) used emergency rescue teams, and 99 patients (51%) visited by themselves. Mean time latency from symptom onset to hospital visit was 62 ± 70.5 minutes. The most common cause of anaphylaxis was drug (56.2%) followed by food (26.8%), insects (9.8%), and exercise (1.5%) in descending order. Seven patients were not assessed. Forty-seven patients (24.2%) have a previous history of anaphylaxis, and among them, 70 % of those patients had experienced anaphylaxis caused by the same suspicious agent. More than half of the patients (n = 115, 59.3%) had an allergic disease other than anaphylaxis. Cutaneous (88.7%) and respiratory (72.7%) symptoms were frequent. Hypotension was presented in 114 patients (58.8%). Cardiovascular symptoms except for hypotension such as chest tightness or palpitation, etc. were present in 45 patients (23.2%).
Table 1.
Characteristics of patients of anaphylaxis who visited our emergency departments (n = 194)
| Characteristic | Value |
|---|---|
| Age, yr | 46 ± 17.1 |
| Male sex | 87 (44.8) |
| Type of visit | |
| Themselves | 99 (51.0) |
| Emergency rescue team | 52 (26.8) |
| Transfer from other hospital | 43 (22.2) |
| Time interval from symptom onset to visit, mina | 62 ± 70.5 |
| Suspicious cause | |
| Drug | 109 (56.2) |
| Food | 52 (26.8) |
| Insect | 19 (9.8) |
| Exercise | 3 (1.5) |
| Others | 4 (2.1) |
| Not assessed | 7 (3.6) |
| History of anaphylaxis | 47 (24.2) |
| Same suspicious cause | 33 (17.0) |
| Others | 5 (2.6) |
| Unknown | 9 (4.6) |
| History of allergic disease other than anaphylaxis | 77 (39.7) |
| Urticaria and/or angioedema | 42 (21.6) |
| Allergic rhinitis | 35 (18.0) |
| Asthma | 14 (7.2) |
| Others | 24 (12.4) |
| Symptoms | |
| Cutaneous | 172 (88.7) |
| Respiratory | 141 (72.7) |
| Hypotension | 114 (58.8) |
| Neurologic | 85 (43.8) |
| Gastrointestinal | 50 (25.8) |
| Cardiovascular (except hypotension) | 45 (23.2) |
Values are presented as mean ± SD or number (%).
Patients who were transferred from other hospitals were excluded.
Therapeutic options and prescription patterns in emergency departments
Information about the types of management was evaluated in 184 patients and described in Table 2. Epinephrine was injected in 114 patients. Seventy patients were not injected with epinephrine, and among them, two patients were infused with other types of inotropics. The route and dose of epinephrine are shown in Table 3. The time latency from visit to epinephrine injection was 26 ± 38.2 minutes (maximum 214 minutes). Sixty-eight patients (59.6%) were initially injected with epinephrine intramuscularly, and 20 patients (17.5%) were injected with epinephrine by intravascular bolus. The mean dose of the initial intramuscular injection was 0.3 ± 0.1 mg. Twenty-four patients (21.1%) needed a second epinephrine injection, and one patient needed continuous infusion after the initial epinephrine injection (Table 3). Hypotension was a significant associated symptom with the injection of epinephrine in anaphylaxis patients (p = 0.000) (Fig. 1). Among the patients injected with epinephrine, most patients (95 patients) were treated with systemic steroid, antihistamine and hydration. Among the patients who were not injected with epinephrine, three patients did not receive antihistamine but were injected with systemic steroid and hydrated as well. Dexamethasone was the most common steroid which was injected (Table 3).
Table 2.
Management of anaphylaxis patients who visited our emergency departments (n = 184)
| Type of managements | No. (%) |
|---|---|
| Management with epinephrine | 114 (62) |
| Systemic steroid, antihistamine and hydration | 95 (52) |
| Systemic steroid and antihistamine | 0 |
| Antihistamine and hydration | 2 (1) |
| Hydration | 2 (1) |
| Unknown | 15 (8) |
| Management without epinephrine | 70 (38) |
| Systemic steroid, antihistamine and hydration | 51 (28) |
| Systemic steroid and antihistamine | 2 (1) |
| Antihistamine and hydration | 3 (2) |
| Hydration | 3 (2) |
| Unknown | 11 (6) |
| Management with other inotropicsa | |
| With epinephrine | 10 (5) |
| Without epinephrine | 2 (1) |
Types of other inotropics (dopamine: 7 cases; norepinephrine: 5 cases; atropine: 1 case).
Table 3.
Types of administration of epinephrine and systemic steroid in patients of anaphylaxis
| Variable | Value |
|---|---|
| Epinephrine | 114 |
| Time latency from visit to epinephrine injection, min | 26 ± 38.2 |
| Route of initial injection | |
| Intramuscular | 68 (59.6) |
| Intravascular bolus | 20 (17.5) |
| Subcutaneous | 19 (16.7) |
| Nebulizer | 4 (3.5) |
| Intravascular infusion | 3 (2.6) |
| Dose of initial injection, mg | |
| Intramuscular | 0.3 ± 0.10 |
| Intravascular bolus | 0.3 ± 0.36 |
| Subcutaneous | 0.3 ± 0.18 |
| Nebulizer | 2.3 ± 0.50 |
| Intravascular infusion | 2.1 ± 2.76 |
| Patients who needed repeating dose | 24 (21.1) |
| Patients who needed continuous infusion after initial dose | 1 (0.9) |
| Systemic steroid | 148 |
| Type of steroid | |
| Dexamethasone | 79 (53.4) |
| Methylprednisolone | 74 (50.0) |
| Hydrocortisone | 27 (18.2) |
| Cortisone | 1 (0.7) |
| Dose of steroida, mg/kg | |
| Methylprednisolone | 2.2 ± 1.65 |
| Hydrocortisone | 0.7 ± 0.46 |
| Dexamethasone | 0.6 ± 0.50 |
| Cortisone | 0.1 (single case) |
Values are presented as mean ± SD or number (%).
Dose of steroid was converted as equivalent dose of methylprednisolone.
Figure 1.
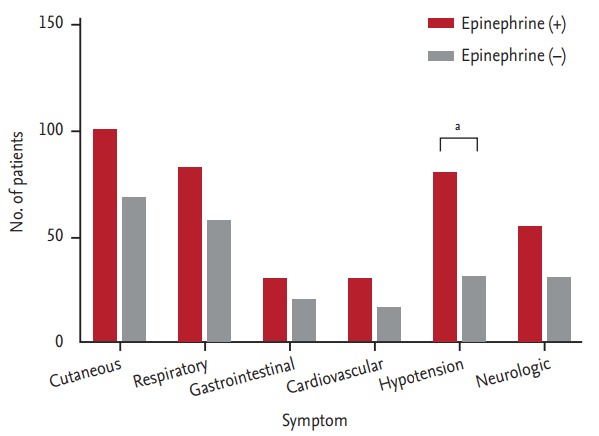
Associated symptoms with injection of epinephrine in patients of anaphylaxis who visited our emergency department (n = 184). aHypotension was significant associated symptom with injection of epinephrine in patients of anaphylaxis (p = 0.000, Pearson chi-square test).
The progression and education status
The progression of 180 patients were analyzed because 14 patients were discharged against medical advice (AMA) (Table 4). One hundred and fifty-five patients were discharged from the EDs, and 24 patients needed to be readmitted. One patient was managed at the intensive care unit. The mean time for overall observation in the ED was 12 ± 25.7 hours. In patients who were injected with epinephrine, the mean observation time was 15 ± 29.3 hours. On the other hand, the mean observation time in patients who were not injected with epinephrine was just 5 ± 4.7 hours.
Table 4.
Progression and education of anaphylaxis patients who visited our emergency departments (n = 180)
| Variable | Value |
|---|---|
| Progressiona | |
| Results of visit | |
| Discharge | 155 (86) |
| Admission | |
| Ward | 21 (12) |
| Intensive care unit | 3 (2) |
| Transfer | 1 (1) |
| Observation time in ED, hr | 12 ± 25.7 (1–194) |
| Patients who were injected epinephrine | 15 ± 29.3 (1–192) |
| Patients who were not injected epinephrine | 5 ± 4.7 (1–27) |
| Education | |
| Education about avoidance of suspicious agents | 23 (13) |
| Prescription and education of epinephrine auto-injector | 5 (3) |
| Request a consultation to allergy department | |
| At emergency departments | 34 (19) |
| To outpatient departmentb | 72 (40) |
Values are presented as number (%) or mean ± SD (minimum–maximum).
ED, emergency department.
14 (7.2%) of against medical advice discharge, they were not included in this analysis.
The number of patients who actually visit the outpatient department: 56 (77.8%).
The education status in the EDs is described in Table 4. The number of patients who underwent education on avoiding suspicious agents was 23 (13%). Only five patients (3%) were prescribed auto-injective epinephrine at the ED. Moreover, only 34 patients (19%) requested a consultation from the allergy department at the ED, and 72 patients (40%) were sent to the outpatient department after discharge. However, among them, only 56 patients actually visited the outpatient department. Among them 10 patients (17.9%) were prescribed auto-injective epinephrine. And 34 patients (60.7%) were confirmed cause of anaphylaxis by provocation test or serum antibody.
Associated factors affecting the duration of stay in the emergency department
Except for AMA discharge patients, a total of 142 patients who had complete information were analyzed (Table 5). There was a tendency to stay longer in patients who visited earlier after symptom onset (R2 = 0.029, B = –0.066, p = 0.048). The duration of the ED stay was significantly longer in patients with hypotension (13.32 ± 24.34 hours vs. 4.8 ± 5.54 hours, p = 0.004) and those were treated with epinephrine injection (12.1 ± 23.30 hours vs. 4.5 ± 3.34 hours, p = 0.014). Age, initial dose of epinephrine, and time latency of the epinephrine injection were not associated with the duration of the ED stay. Gender and organ specific symptoms were also not associated with the duration of the ED stay.
Table 5.
Associated factors affecting the duration of stay in emergency department in patients of anaphylaxis (n = 142)
| Variable | Mean ± SD, hr | p value |
|---|---|---|
| Age | 0.237 (R2 = 0.010, B = 0.104) | |
| Time latency from symptom onset to ED visit | 0.048 (R2 = 0.029, B = –0.066) | |
| Initial dose of epinephrine | 0.685 (R2 = 0.002, B = –2.496) | |
| Time latency of epinephrine injection | 0.170 (R2 = 0.024, B = 0.105) | |
| Gender | 0.162 | |
| Male | 6.9 ± 7.46 | |
| Female | 10.2 ± 23.29 | |
| Cutaneous symptom | 0.120 | |
| (+) | 7.0 ± 8.13 | |
| (–) | 42.1 ± 60.55 | |
| Respiratory symptom | 0.379 | |
| (+) | 8.7 ± 16.17 | |
| (–) | 12.5 ± 28.69 | |
| Gastrointestinal symptom | 0.271 | |
| (+) | 14.4 ± 33.63 | |
| (–) | 7.9 ± 9.62 | |
| Cardiovascular symptom | 0.379 | |
| (+) | 19.1 ± 35.38 | |
| (–) | 5.8 ± 6.01 | |
| Hypotension | 0.004 | |
| (+) | 13.32 ± 24.34 | |
| (–) | 4.8 ± 5.54 | |
| Neurologic symptom | 0.118 | |
| (+) | 12.5 ± 26.77 | |
| (–) | 6.6 ± 8.93 | |
| Injection of epinephrine | 0.014 | |
| Injected | 12.1 ± 23.30 | |
| Not injected | 4.5 ± 3.34 |
Linear regression and independent-samples t test were used in analysis.
ED, emergency department.
DISCUSSION
To our knowledge, there have been many studies on the clinical features and management of anaphylaxis [6-8], but there have been only a few studies on whether education was appropriately provided in the actual clinical field especially in Korea. In our study, we evaluated how many patients were treated according to guidelines in real situations. In addition, we could encourage the appropriate management and education by presenting these problems. Unfortunately, inappropriate management and education were done rather than following the international guideline in the actual clinical field [5].
The time to visit the ED from symptom onset was over 60 minutes. In one study in Korea, the mean time to arrival at hospital after development of symptoms was even 279.8 minutes [4]. Because prompt intervention is very important in anaphylaxis, the delayed injection of epinephrine is associated with a poor prognosis. Patients should visit the ED as soon as possible. In fact, many patients transported themselves to the ED. If they went to the hospital using an ambulance, they would have arrived earlier. Critical time is consumed on the road during transportation to the hospital. For a patient who has experienced anaphylaxis more than one time, he or she must be educated to request the help of paramedics. Like cardiopulmonary resuscitation, anaphylaxis should be educated all people about first aid procedures. Additionally, epinephrine auto-injectors should be kept by paramedics in the ambulance, and they should be educated on how to use them. According to the international guideline, it is recommended to inject epinephrine intramuscularly [2] because injection through other routes, especially intravenous bolus, has risks of cardiovascular complications and overdose [9]. The optimal intramuscular dose is 0.5 mg maximum in adults and 0.3 mg in children [2]. Actually, there were many patients who were not injected intramuscularly with epinephrine. About 40% of the patients were not injected intramuscularly with epinephrine but instead through other routes. Furthermore, the dose of epinephrine (0.3 ± 0.10 mg intramuscularly) was lower than recommended dose according to WAO guideline (0.01 mg/kg, if the patient was over 50 kg, 0.5 mg of epinephrine should be injected) [2]. There was a tendency (although we did not analyze it statistically) that mean dose of epinephrine was higher in patient of single dose epinephrine injected intramuscularly (0.325 mg in 53 patients) than multiple dose injected (0.3 mg in 15 patients). One patient was injected just 0.3 mg dose of epinephrine intramuscularly four times. Three patients without epinephrine injections were only just hydrated. In patients who were not injected with epinephrine, they fortunately recovered in all cases and had a shorter observation time than the patients with epinephrine injections, and those patients would have only mild anaphylaxis. The negative relation between time latency from symptom onset to ED visit and the duration of the ED observation could be caused by the same reason. Here, one question arises. That is whether the patient with mild anaphylaxis needs epinephrine. However, we cannot predict any further reactions after the initial symptom; thus, epinephrine must be injected into all anaphylaxis patients promptly. In our study, the associated symptom with the injection of epinephrine was hypotension, and the patients without hypotension could be underdiagnosed and be not injected with epinephrine. According to the WHO criteria, we could diagnose patients without hypotension as anaphylaxis if they fulfill other criteria [5]. Thus, clinicians need to pay more attention when diagnosing anaphylaxis. It should be educated that anaphylaxis can be diagnosed without hypotension.
Corticosteroid was used in most cases to prevent a delayed reaction despite of unclear efficacy [2]. The WAO guideline recommend it as second line medication [2]. Dexamethasone and methylprednisolone were preferred. There have been no studies in which corticosteroid was more effective, and the recommended dose of corticosteroid was extrapolated from acute asthma treatment [2]. In the global initiative for the asthma guideline, they recommend 1 mg/kg of prednisolone (maximum 50 mg) [10]. In our study, there was a tendency to use a low dose corticosteroid in anaphylaxis when other types of corticosteroids were also used except for methylprednisolone. Additionally, a higher dose of methylprednisolone was used instead of the recommended dose. Corticosteroid was used to prevent biphasic anaphylaxis [11], but more studies are needed to determine the efficacy, adequate dose, and type. In addition, the physicians should understand the purpose and unclear efficacy.
Education on avoiding the causative agent was also important but not sufficient. Just 23 patients (13%) were educated to avoid suspicious agents. The most frequent causative agent was drug. In these cases, the causative drug could be identified through the medical history and with suitable tests. We could prevent anaphylaxis caused by same drug if the agent is defined and avoided. For this, active evaluation and education on avoidance by doctors are needed. In many cases, education about avoidance and the use of an epinephrine auto-injector were not recorded. Hospitals should provide education programs and record this education to prevent any legal problems. One good method is to consult an allergist for an evaluation and follow-up. There was a study that reported follow-up was effective in achieving good outcomes [12]. In that study, 35% of the patients who were diagnosed with anaphylaxis in the ED had an alteration in the diagnosis or trigger [12]. Sometimes, it could be difficult to diagnose a patient with anaphylaxis due to vague symptoms and the absence of hypotension or urticaria. Underdiagnosis could lead to under-treatment especially epinephrine [13]. It is important to confirm the diagnosis and to define the trigger for further education and prevention. In our study, just 106 patients transferred to an allergist at the ED or to an out-patient department. Among them, 90 patients actually met an allergist (34 patients at ED and 56 patients at out-patient department). Seventy-eight percent of the patients who were transferred to an outpatient department actually visited an allergist, so compliance was not low. Among them, 10 patients (17.9%) were prescribed epinephrine auto-injectors. If close cooperation with the ED and an allergist is possible, more help such as diagnosis, education and emotional support can be provided to anaphylaxis patients. In addition, it is necessary to educate the medical staff that anaphylaxis has a risk of recurrence to trigger re-exposure, so trigger should be evaluated at first attack. And they should know that anaphylaxis could be diagnosed without hypotension.
Our study has some limitations. First, the patient group did not represent the general state of EDs in Korea because we evaluated just three hospitals. Thus, more studies are needed. Second, we enrolled patients by searching the ICD codes inputted subjectively, so some patients who were recoded with other diagnoses such as hypotension could be missed. Third, it could be possible that they did not record education although they educated patients because our study depended on medical records.
In conclusion, many patients received the appropriate management of anaphylaxis, but some patients received a little different management from the guideline such as epinephrine injection. An education and promotion program on anaphylaxis is needed for medical staff especially emergency healthcare workers. Education on avoiding triggers and an emergency action plan are important to avoid recurrence of anaphylaxis and to get a good prognosis. It could be helpful to request an allergist for follow-up after acute management by emergency healthcare workers.
KEY MESSAGE
1. Associated factor with epinephrine injection was hypotension in our study population.
2. Some patients received a little different management from the guideline such as epinephrine injection.
3. An education and promotion program on anaphylaxis is needed for medical staf
Footnotes
No potential conflict of interest relevant to this article was reported.
Supplementary Materials
Distribution of patients by World Allergy Organization diagnostic criteria for anaphylaxis
REFERENCES
- 1.Brown SG, Stone SF, Fatovich DM, et al. Anaphylaxis: clinical patterns, mediator release, and severity. J Allergy Clin Immunol. 2013;132:1141–1149. doi: 10.1016/j.jaci.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 2.Simons FE, Ardusso LR, Bilo MB, et al. World Allergy Organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J. 2011;4:13–37. doi: 10.1097/WOX.0b013e318211496c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lieberman P, Camargo CA, Jr, Bohlke K, et al. Epidemiology of anaphylaxis: findings of the American College of Allergy, Asthma and Immunology Epidemiology of Anaphylaxis Working Group. Ann Allergy Asthma Immunol. 2006;97:596–602. doi: 10.1016/S1081-1206(10)61086-1. [DOI] [PubMed] [Google Scholar]
- 4.Ye YM, Kim MK, Kang HR, et al. Predictors of the severity and serious outcomes of anaphylaxis in Korean adults: a multicenter retrospective case study. Allergy Asthma Immunol Res. 2015;7:22–29. doi: 10.4168/aair.2015.7.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simons FE, Ardusso LR, Bilo MB, et al. 2012 Update: World Allergy Organization Guidelines for the assessment and management of anaphylaxis. Curr Opin Allergy Clin Immunol. 2012;12:389–399. doi: 10.1097/ACI.0b013e328355b7e4. [DOI] [PubMed] [Google Scholar]
- 6.Yang MS, Lee SH, Kim TW, et al. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol. 2008;100:31–36. doi: 10.1016/S1081-1206(10)60401-2. [DOI] [PubMed] [Google Scholar]
- 7.Jang GC, Chang YS, Choi SH, et al. Overview of anaphylaxis in Korea: diagnosis and management. Allergy Asthma Respir Dis. 2013;1:181–196. [Google Scholar]
- 8.Moon IJ, Park HJ, Kim SR, et al. Drug-induced anaphylaxis in a single Korean tertiary hospital. Korean J Med. 2015;88:281–287. [Google Scholar]
- 9.Campbell RL, Bellolio MF, Knutson BD, et al. Epinephrine in anaphylaxis: higher risk of cardiovascular complications and overdose after administration of intravenous bolus epinephrine compared with intramuscular epinephrine. J Allergy Clin Immunol Pract. 2015;3:76–80. doi: 10.1016/j.jaip.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 10.Global Initiative for Asthma . Global Initiative for Asthma (GINA); c2016. Global strategy for asthma management and prevention 2014 [Internet] [cited 2017 Oct 13]. Available from: http://ginasthma.org. [Google Scholar]
- 11.Simons FE, Ardusso LR, Dimov V, et al. World Allergy Organization Anaphylaxis Guidelines: 2013 update of the evidence base. Int Arch Allergy Immunol. 2013;162:193–204. doi: 10.1159/000354543. [DOI] [PubMed] [Google Scholar]
- 12.Campbell RL, Park MA, Kueber MA, Jr, Lee S, Hagan JB. Outcomes of allergy/immunology follow-up after an emergency department evaluation for anaphylaxis. J Allergy Clin Immunol Pract. 2015;3:88–93. doi: 10.1016/j.jaip.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 13.Sclar DA, Lieberman PL. Anaphylaxis: underdiagnosed, underreported, and undertreated. Am J Med. 2014;127(1 Suppl):S1–S5. doi: 10.1016/j.amjmed.2013.09.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Distribution of patients by World Allergy Organization diagnostic criteria for anaphylaxis


