The phrase “a stitch in time saves nine” was first recorded in 1732 (albeit with slightly less confidence as “a stitch in time may save nine”) in Thomas Fuller’s Gnomologia: Adagies and Proverbs; Wise Sentences and Witty Sayings, Ancient and Modern, Foreign and British.1 The phrase is particularly apropos for those of us in public health who seek to prevent untoward things from occurring in the first place (primary prevention) and to prevent things that occur from becoming even more serious (secondary prevention).
PUBLIC HEALTH PREPAREDNESS SUPPLEMENT
This second special public health preparedness supplement (“Public Health Emergencies: Unpacking Medical Countermeasures Management for Preparedness and Response”) of AJPH, developed in collaboration with the Centers for Disease Control and Prevention, provides insights into the challenges and successes of the evolution of the system for medical countermeasures (MCMs), with examples both domestically and from abroad; and complements the first special public health preparedness supplement,2 which emphasized the full spectrum of public health emergency management from preparedness to response and recovery.
HOW MANY “STITCHES” TO KEEP AT THE READY
In a previous editorial, “Public Health Disasters: Be Prepared,” I outlined the dilemma public health emergency preparedness professionals and societies face in paying the price for preparedness and noted that societies ultimately must make conscious decisions of how much preparedness they can afford to “buy” in light of resources being finite and competing priorities.3 Even within the “price” of preparedness, professionals must choose among priorities such as stockpiling of MCMs, hardening communities (e.g., seismic retrofitting of buildings to prepare for earthquakes; building and maintaining levees to prepare for flooding), deploying early-warning systems (e.g., the BioWatch monitoring system of highly specialized sensors positioned by the US Department of Homeland Security; Centers for Disease Control and Prevention’s National Syndromic Surveillance Program BioSense Platform), and funding research for new vaccines, medications, and devices that may be used as MCMs in the future.
WHAT “STITCHES” TO KEEP AT THE READY
Which MCMs should be stockpiled (either centrally, regionally, with manufacturers, or locally)?
For some MCMs, such decisions also must consider, beyond just the likelihood of the need for the MCMs or funding constraints, the staffing resources (either existing trained staff or staff who can receive “just-in-time” training) needed to actually use them. For example, stockpiled MCM devices such as ventilators, even if deployed to an area of need, may not have sufficient staff to use them for all the patients who may need them (and, if there were a situation of pandemic influenza, staffing may not be available through mutual aid if such staff were fighting the pandemic in their own jurisdictions).
WHERE TO KEEP THE FIRST “STITCH”
Some MCMs, when needed, may be needed immediately. Therefore, conceivably, such MCMs could be prepositioned in every home. However, problems arise with this approach, including unintended consequences (e.g., poisoning of children caused by accidental ingestion of MCMs) and expenses (e.g., the cost of MCMs distributed to every home is very high given that the most likely scenarios for their ever being needed are in an unpredictable locality, and unused MCMs will ultimately expire and need to be replenished).
Therefore, preparedness and response planners attempt to achieve rapid access to MCMs through a mixture of national and regional stockpiles of MCMs, rapid transport and deployment mechanisms, and close coordination among the preparedness and response personnel at national, state, regional, and local levels to be able to receive and dispense MCMs. Frequent exercises and drills to improve and monitor response capabilities to deliver MCMs are an important component of MCM preparedness and response capability.
USING THE FIRST “STITCH”: DECISION TO DEPLOY
As noted in this supplement, preparedness and response exercises are an important component of training and readiness on MCMs. The plans delineating when an MCM is to be deployed can be refined through such exercises. These plans must strike a balance between sensitivity and specificity—terms often used in public health for screening and testing. If the plan to deploy the first “stitch” is too sensitive without sufficient specificity that the event criteria have been met, needless mobilization of personnel and shipment of MCMs (and even their possible use in the population) will have been made (i.e., responding to a false-positive event). At the other extreme, if the plan to deploy the first “stitch” is too specific, the MCMs may not be deployed in a timely manner, and lives could be lost because of delays (i.e., not responding to a false-negative event). This balance comes into play especially for early-warning systems, such as BioWatch, in which decisions about deployment of MCMs based on an alert of a possible bioterrorist event detected before actual human illness may be especially challenging.
PROBLEM WHEN DEPLOYING THE “STITCHES IN TIME”
Depending on the perceived severity of the natural or man-made disaster by individuals, the MCMs being deployed for an event may be in extremely high demand, especially if the MCMs are limited in number and insufficient to cover the entire affected population and prioritization is required (e.g., to use the MCMs only in those persons most heavily exposed to a bioterrorist agent).
Protecting the MCM supply and delivery chain, the MCM storage facilities, and the MCM points of dispensing may be a critical need in such situations. National, state, regional, and local public health and law enforcement personnel coordinate in planning and exercising such scenarios, and elected officials and the media need to be aware and supportive of the plans for MCM deployment so that they can help to explain the rationale for MCM distribution and call for calm and cooperation by the public they serve.
NOVEL APPROACHES TO MEDICAL COUNTERMEASURES
Some of the innovative approaches to MCMs that have been the result of collaboration, planning, and exercising of MCM protocols between public health and emergency response agencies are included in this supplement.
Other examples include the voluntary program for specific, targeted predistribution of potassium iodide tablets by the San Luis Obispo County, California, Public Health Department to each person who lives or works within the Protective Action Zone surrounding the Diablo Canyon nuclear power plant4 and the possible use of the US Postal Service to distribute MCMs in some settings.
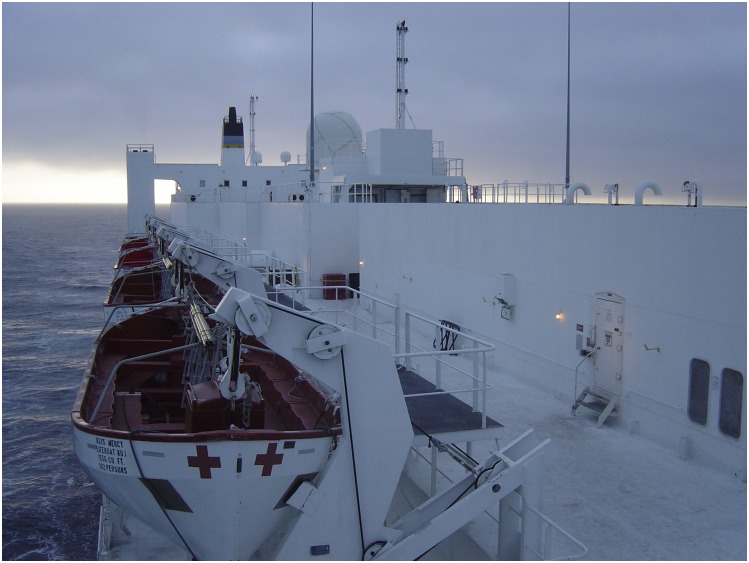
There are even possibilities for the use of unusual resources in public health disasters. For example, although the primary mission is to support military operations, the US Naval Ship Mercy (Figure 1), homeported in San Diego, California, and her sister US Naval Ship, Comfort, homeported in Norfolk, Virginia, also may be deployed to support other US government agencies in disaster settings5 and could, conceivably, be deployed to a port city to assist in MCM distribution or dispensing.
FIGURE 1—
US Naval Hospital Ship Mercy (T-AH-19) at Sea, April 2007
Source. Photo courtesy of Robert Kim-Farley, MD, MPH.
As more experience is gained in the field of MCMs, additional MCM strategies and approaches undoubtedly will emerge, challenging us to balance currently known needs with uncertain predicted or predictable events when a “stitch in time” truly would have lifesaving consequences for any or all of us.
REFERENCES
- 1.Fuller T. Gnomologia: Adagies and Proverbs; Wise Sentences and Witty Sayings, Ancient and Modern, Foreign and British. London, England: B. Barker; A. Bettesworth and C. Hitch; 1732:ix. Available at: https://books.google.com/books?id=3y8JAAAAQAAJ&pg=PA5&source=gbs_toc_r&cad=4#v=onepage&q=stitch&f=false. Accessed June 8, 2018.
- 2.Special Public Health Preparedness Supplement. Am J Public Health. 2017;107(S2) doi: 10.2105/AJPH.2017.303963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim-Farley RJ. Public health disasters: be prepared. Am J Public Health. 2017;107(S2):S120–S121. doi: 10.2105/AJPH.2017.304039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borenstein P. County of San Luis Obispo: potassium iodide (KI) pre-distribution. Available at: https://www.slocounty.ca.gov/Departments/Health-Agency/Public-Health/All-Public-Health-Services/Potassium-Iodide-(KI)-Pre-Distribution.aspx. Accessed June 10, 2018.
- 5.US Navy. USNS Mercy: steaming to assist. Available at: http://www.mercy.navy.mil. Accessed June 8, 2018.