Abstract
Background
Autism spectrum disorder (ASD) is characterised by significant impairment in social communication and the presence of restrictive and repetitive behaviour or interest. Intervention during early childhood could decrease ASD symptoms. We aimed to identify the most effective intervention based on cognitive, developmental, and behavioural approaches and the factors that impact the effectiveness of the intervention.
Methods
We performed a systematic review and meta-analysis of existing interventions for ASD in preschool-aged children. Electronic databases were searched for related articles with randomised controlled trial (RCT) designs published between 2001 to 2015. Outcome measures were communication, behavioural and cognitive skills, reported as standardised mean differences (SMD) compared to a control group. A Random-effects model was utilised to calculate the pooled estimate effect. Between-study variability was also assessed. The registering number of this study is CRD42017035354.
Findings
Out of the initial 5174 studies that were identified, there were 14 RCTs (746 children) that were included in the final systematic review and meta-analysis. Pooled estimate effect provided by random-effects model was 0.23 (95% confidence interval, CI [0.08–0.37]) with no between-study heterogeneity (I2 = 0.00%, p = 0.0018). Three studies of music therapy interventions provided the greatest outcome effects with a shorter duration and lower intensity. SMD for music therapies ranged from 0.40 to 0.62 with 95% CI [0.22 to 1.85]. The quality of the health care provider, the duration, and the intensity of intervention played an important role in the effectiveness of the intervention.
Interpretation
Music therapy appears to be an effective tool for improving social interaction in preschool-aged children with ASD. However, more evidence-based trials are required to further validate the effectiveness of music therapy in ASD.
Keywords: Education, Psychiatry
1. Introduction
Autism Spectrum Disorder (ASD) is a syndrome which is characterised by persistent significant impairment in social interaction and social communication, as well as the existence of restrictive and repetitive behaviour, interests, or activities [1]. The overall prevalence of ASD is one in 59 children [2] and one in 100 adults [3]. People with ASD have poor social integration and independence, and they require special support for education, living arrangements, and employment [4]. Adolescents with ASD suffer from poor companionship and loneliness [5] such that 47.7% of affected individuals develop poor outcomes in adulthood [6]. In some individuals with high functioning ASD, symptoms may go unrecognised in early life, and the individual may be regarded as rigid, complicated, or odd because of their poor social competence. Such situations can lead to chronic interpersonal crisis, anxiety, social withdrawal, and depression in later life [7]. In fact, these undesirable adulthood outcomes are due to the problems associated with ASD in childhood.
Many aspects of social abilities, including the theory of mind (ToM), develop during the first four to five years of life [8]. The ToM is the ability to recognise and attribute mental states such as thoughts, perceptions, desires, intentions, feelings about oneself and others and to understand the effects of these mental states on one's behaviour. Atypical development of such abilities may occur in people with Asperger's syndrome, and autism [9]. The changes have been linked to the early maturation of brain mechanism that plays an important role in developing language [10, 11], working memory [12], executive functioning for the cognitive control of behavior [13], and joint attention (JA) for social skill [14]. JA is the ability to engage in the referential triangle of self, social partner, and external object or event by jointly participating and responding to a social interaction. It is also a human-specific capacity that underlines ToM [15].
Therefore, interventions that target early childhood should produce favourable outcomes for individuals with ASD [16, 17, 18]. However, no single intervention was universally effective for all children with ASD [19]. In previous review articles, researchers found that the Treatment and Education of Autistic and Communication Handicapped Children (TEACCH) program, Developmental Individualized Relationship (DIR) based interventions, the intensive University of California, Los Angeles (UCLA)/Lovaas-based interventions, the Learning Experiences and Alternate Programs for Preschoolers and their parents (LEAP) program, and Early Start Denver Model (ESDM) showed more beneficial outcomes and effects compared to other parent training and comprehensive intervention approaches [20, 21, 22, 23]. Due to the inability to assess the effectiveness of individual study, researchers have not clarified which intervention is superior among the various treatment strategies for ASD. In a comprehensive review for ASD in children, youth, and young adults, researchers have identified evidence-based practices (EBP) which included behavioural, developmental, and educational approaches for children and young adults ranging in age from birth to 22 years old. Outcomes of the studies have been related to changes in communication, social skills, challenging behaviours, play and school readiness skills, pre-academic and academic skills, adaptive and self-help skills, JA, motor, cognitive, and vocational skills of affected individuals with ASD. Knowledge of existing approaches for ASD was available in that previous study. However, researchers did not calculate the effect sizes (ES) to explore the relative strength of interventions [24]. Here, evidence obtained from a meta-analysis of several randomised controlled trials (RCTs) could be ranked as the first level of evidence-based information [25]. Therefore, in the present study, we aimed to identify the most effective cognitive, developmental, and behavioural interventions for ASD in preschool-aged children as well as the factors that affect the effectiveness of interventions by systematically reviewing of RCTs and conducting a meta-analysis.
2. Main text
2.1. Methods
2.1.1. Search strategy and selection criteria
We conducted a systematic review and meta-analysis guided by Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) guidelines [26] (Appendix A). Given that the literature search was conducted in February 2016, the timeframe of published articles was from January 2001 to December 2015 for the purpose of defined publication period and for ensuring researchers' effort of data handling. There were no language restrictions; however, the study population included only preschool-aged children with ASD (e.g., children aged 1 to 6 years old). Only RCTs with human subjects were considered. Additionally, to be included in the meta-analysis, the interventions needed to focus on the core characteristics of ASD such as communication and social interaction deficits, restrictive and repetitive behaviour, and language skill deficit. In contrast, studies that focused on parental or caregiver outcomes rather than the outcomes of children, studies that emphasised strictly medical problems, and studies that evaluated medication effects were excluded. The following search engines were utilised: the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medical Literature Analysis and Retrieval System Online (MEDLINE), Psychological Information Database (PsycINFO), Web of Science, and Education Resources Information Centre (ERIC).
Search terms included “Autism Spectrum Disorder,” “Childhood,” “Children,” “Preschool Children,” “Treatment,” and “Education.” Those terms were used both separately and together with other variations such as “autism” and “intervention” (Appendix B). The first author conducted the initial article screening, and confirmation was performed through a discussion with the second author. Agreement for full article review was performed by both authors. Hand searching of related articles and checking the bibliographies of retrieved studies were carried out simultaneously. Corresponding authors of included articles were contacted by electronic mail to obtain complete data for the meta-analysis. The authors designed a standardised form to retrieve necessary information, which included the study characteristics, outcome, and risk of bias. The first author performed the data extraction and assessed the quality of included studies using the Cochrane risk of bias assessment tool [27], which was verified by the second author. To assess the empirical evidence for determining whether the study could be considered as EBP, the “Evaluating method for determining evidence-based practices in autism” was applied [28]. The reliability of the literature search was checked by one external reviewer (kappa = 0.83, perfect agreement).
2.1.2. Analysis
Studies that reported continuous outcomes on core deficits of ASD were included in this review. The included studies used different outcome measures for different interventions, none of which were common to all trials. Therefore, the Standardised Mean Difference (SMD; Cohen's d) and its 95% Confidence Interval (CI) of each outcome measure was calculated. Then, the mean effect (Hedges' g) was calculated to reduce measurement error by taking between-scale correlation into account. For the studies that assessed the outcome results at different time period (i.e., in-between intervention, post-intervention and follow-up), the results from the longest assessment period were retrieved for final evaluation.
A random-effects model was utilised for the assumption that the included studies represent a mere random sampling of the larger population of studies that could have been conducted on ASD children [29]. We also considered that the type of interventions and outcome measures varied among studies, and the true effect would be most likely varied from one study to the next. The meta-analysis was performed using the statistical software RStudio (version 1.0.143) [30] with Metafor-package, as it is a comprehensive collection of functions for calculating various ESs and outcome measures for the random-effects model. This software can also create meta-analytical plots (e.g., forest, funnel plots) [31]. The basic meta-analysis function rma() was filled with variables (SMD, Variance), data frame, and the “DL” (random-effects using the DerSimonnian-Laird estimator) to measure the heterogeneity in SMD and to estimate the between-study variability. Weights of studies were also used to know the contribution of each study on overall estimate effect. In addition, a forest plot was generated to summarise the effectiveness of studies based on the between studies heterogeneity. Publication bias was tested by examining the funnel plot. This study is registered with PROSPERO, number CRD42017035354.
2.2. Results
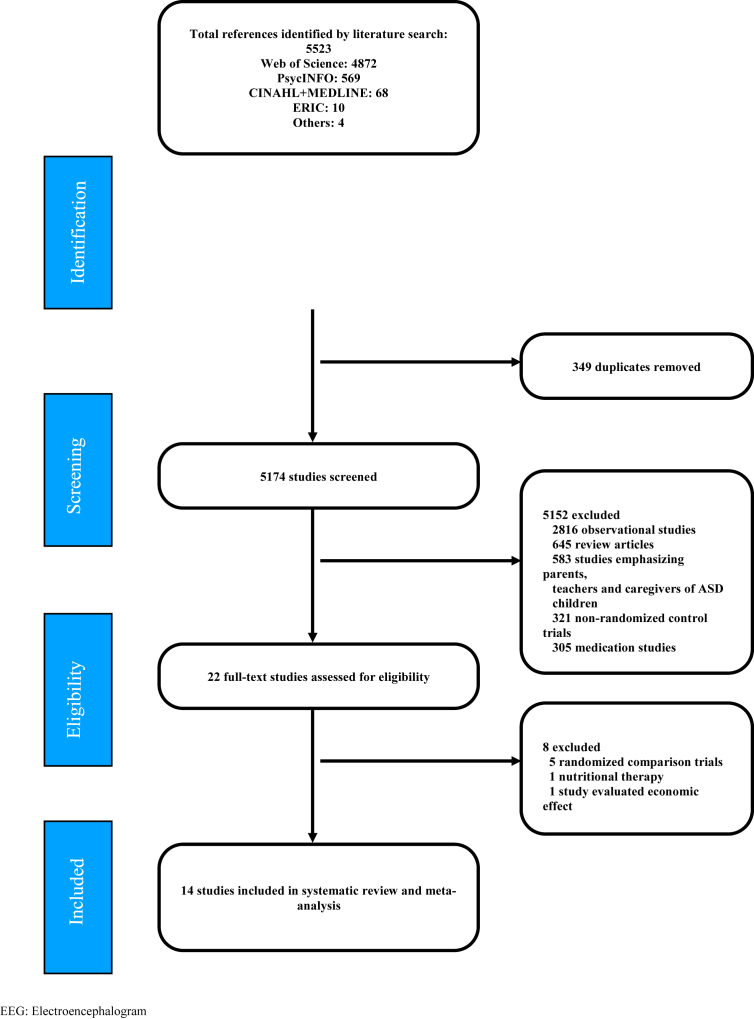
We initially identified 5174 studies that related to ASD in preschool-aged children that were published between January 2001 and December 2015. Most of these studies were observational studies, non-randomised intervention trials, and investigations assessing the effectiveness of medications. After excluding ineligible studies, 22 studies were left for full-text review. Among them, eight studies were excluded because they assessed randomised comparison trials without a control group (n = 5), nutritional therapy (n = 1), the economic effect of intervention (n = 1), and electroencephalogram status of children rather than core characteristics of ASD (n = 1; Appendix C). The final sample included 14 RCTs for the systematic review and meta-analysis (Fig. 1). The total number of children involved in these RCTs was 746 (416 in intervention groups and 330 in control groups) and included 72% boys and 14% girls. Three studies did not provide gender information about their participants. Twelve studies had a low risk of bias, and two studies had a high risk of bias. Random sequence generation and allocation concealment were reported in ten studies. All studies were free from selective reporting and incomplete outcome data. Ten studies attempted for high fidelity of treatment among intervention providers while 12 studies could make outcome assessment by blinded personnel (Appendix D). Despite this, only one study could perform masking of health care providers and participants because of the complex nature of the intervention. The reporting of inter-observer agreement in all studies was unclear, and the quality indicators of the included studies for EBP could be rated as strong and adequate (Appendix E). According to the symmetrical funnel plot, publication bias was not apparent although the estimate effects were scattered in the middle of the plot (Appendix F).
Fig. 1.
Flow of information through the literature search.
Intervention providers were specialist therapists and trained professional (n = 9), parents (n = 3), teachers (n = 1), and parents and teachers together (n = 1). The duration of the interventions lasted from two weeks to two years, and the mean intervention duration was 7.5 months. The intensity of the intervention ranged from 30 minutes (min) per week to 600 min/week with a mean intensity of 153 min/week. Outcome assessments were performed in-between intervention (n = 3), post-intervention (n = 14), at Time 1 follow-up (n = 3), and at Time 2 follow-up (n = 1). Descriptions of the study characteristics, outcome measuring instruments, and the effectiveness of each intervention in SMD are explored in Table 1.
Table 1.
Description of study characteristics and effectiveness of interventions.
| Study (Author/Year/Country) | Risk of bias | Age of children | Intervention focused problem | Type of intervention | Intervention approach | Outcome measures and ES (Cohen's d) | Overall effectiveness (SMD/95% CI) |
|---|---|---|---|---|---|---|---|
| Hardan et al. 2015, USA | Low | 2 to 6 years | Communication deficit | Pivotal response training | ABA | SLO (0.59), Vineland (0.34), MBCDI (0.14), PLS (0.54) | 0·14 (−0·44 to 0·72) |
| Siller et al. 2014, USA | Low | 2 to 6 years | Communication and language skill deficits | Focused playtime intervention | Developmental | MPCA (0.55), Observed attachment behaviors (0.41), PCSB (0.21), AB (0.50) | 0·41 (−0·03 to 0·98) |
| Tong et al. 2014, Australia | Low | 2.5 to 5 years | Adaptive behavior | (1) PEAC, (2) PEBM | Cognitive and behavioral | PEAC group: VABS (communication (−0.56), daily living (−0.14), social (−0.27), motor (−0.31)) DBC (ASA (0.11), TBPS −0.26) CARS (0.22), PEP-R DQ (−0.53), RDLS comprehension (−0.76), RDLS expression (−0.58) PEBM: VABS (communication (0.10), daily living (0.46), social (0.36), motor (0.46)) DBC (ASA (−0.22), TBPS (−0.40)) CARS (−0.44), PEP-R DQ (0.17), RDLS comprehension (−0.24), RDLS expression (−0.06) |
(1) −0·31 (−0·82 to 0·20) (2) 0·02 (−0·48 to 0·52) |
| Thompson et al. 2014, Norway | High | 36 to 60 months | Social engagement | In home FCMT | Developmental | VSEEC (1.96), SRS-PS (−0.43), MBCDI (0.26), PCRI (0.80) | 0·62 (−0·22 to 1·54) |
| Ingersoll, 2012, USA | Low | 27 to 47 months | Imitation skill | Reciprocal imitation training | Developmental and behavioral | ESCS (0.42), Social emotional scale (0.89), MIS (0.79), Unstructured imitation assessment (0.72) | 0·68 (−0·08 to 1·48) |
| Aldred et al. 2012, UK | Low | 2 to 5 years | Social interaction and communication deficits | Manualized parent-mediated intervention | Developmental | Parent synchrony (0.95), ADOS social communication algorithm (−0.78) | 0·08 (−0·69 to 0·86) |
| Kaale et al. 2012, Norway | Low | 29 to 60 months | Communication deficit | Joint attention | Developmental and behavioral | JA during ESCS (0.04), JA during teacher-child play (0.44), JA during mother-child play (0.37) | 0·16 (−0·35 to 0·64) |
| Lim & Draper, 2011, USA | Low | 3 to 5 years | Communication deficit | (1) Music incorporated ABA VB, (2) Speech incorporated ABA VB | ABA | Music incorporated ABA VB: VPES (0.63) Speech incorporated ABA VB: VPES (0.51) |
(1) 0·60 (0·09 to 1·85) (2) 0·49 (0·28 to 2·09) |
| Casenhiser et al. 2011, Canada | Low | 2 to 5 years | Social interaction and communication deficits | DIR based intervention | Developmental | CBRS: Attention to activity (0.69), Involvement (0.87), Compliance (0.51), Initiation for JA (1.02), Enjoyment in interaction (0.63) | 0·52 (−0·04 to 1·09) |
| Green et al. 2010, UK | Low | 2 to 5 years | Communication deficit | Parent-mediated PACT | Developmental | ADOS (−0.14), PLS: receptive (−0.20), PLS: expressive (−0.03), Parent CSBS-DP (−0.30), Parent MCDI: receptive (0.09), Parent MCDI: expressive (0), Teacher Vineland: Communication (0.48), Teacher Vineland: adaptive behavior composite (0.33) | 0·03 (−0·26 to 0·38) |
| Dawson et al. 2010, USA | Low | 18 to 30 months | Adaptive behavior | ESDM | Developmental and behavioral | MSEL (0.52), VABS (0.66), RBS (−0.35) | 0·45 (−0·14 to 1·04) |
| Kasari et al, 2008, USA | Low | 3 to 4 years | Communication deficit | (1) Joint attention, (2) Symbolic play | ABA and developmental | JA group: JA initiation composite (0.99), JA responses (0.17), Child-initiated JA (0.85), Mother-initiated JA (0.74) SP group: JA initiation composite (1.12), JA responses (0.37), Child-initiated JA (0.63), Mother-initiated JA (0.25) |
(1) 0·38 (−0·24 to 1·11) (2) 0·64 (−0·06 to 1·37) |
| Kim et al. 2008, Korea | High | 3 to 5 years | Communication deficit | Improvisational music therapy | Inherent and communicative musicality | PDDBI (0.16), ESCS (0.63) | 0·40 (0 to 0·78) |
| Rickards et al. 2007, Australia | Low | 3 to 5 years | Cognitive development and behavior | Home-based intervention | Cognitive developmental and behavioral | IQ (0.35), BRS (0.40), BSQ (−0.02), PBCL (−0.68), VABS (0.25) | 0·06 (−0·45 to 0·71) |
AB: Avoidant behavior scale, ABA: Applied behavioral analysis, ADOS: Autistic diagnostic observation schedule, ASA: Autism disorder screening algorithm, BRS: Behavior rating scale, BSQ: Behavior screening questionnaire, CBRS: Child Behavior Rating Scale, CI: Confidence interval, CSBS-DP: Communication and Symbolic Behavior Scales Developmental Profile, DBC: Developmental behavior checklist, DIR: Developmental individualized relationships-based intervention, ES: Effect Size, ESCS: Early social communication scale, ESDM: Early start Denver model, FCMT: Family centered music therapy, JA: Joint attention, MBBCDI: MacArthur-Bates communicative development inventories, MIS: Motor imitation scale, MPCA: Maternal perception of child attachment questionnaire, MSEL: Mullen scale of early learning, MTDA: Music therapy diagnostic assessment, PACT: Preschool autism communication trial, PBCL: Preschool behavior checklist, PCRI: Parent-child relationship inventory, PCSB: Proximity/Contact seeking behavior scale rated based on the separation-reunion episode, PDDBI: Pervasive developmental disorder behavior inventory, PEAC: Parent education and counseling, PEBM: Parent education and behavior management, PLS: Preschool language scale, RBS: Repetitive behavior scale, SLO: Structured laboratory observation, SMD: Standardized mean difference, SRS-PS: Social responsiveness scale preschool version for 3-years-olds, TBPS: Total behavior problem score, VABS: Vineland adaptive behavior rating scales scaled score, VB: Verbal behavior, Vineland: Vineland adaptive behavior scales, VPES: Verbal production evaluation scale, VSEEC: Vineland social-emotional early childhood scales.
Researchers in the included interventions greatly emphasised communication and social interaction deficit as these are more common problems than other domains (n = 12). There were fewer studies that emphasised restrictive and repetitive behaviour (n = 2). Communication-focused trials used PRT, focused playtime intervention, in-home family-centered music therapy (FCMT), reciprocal imitation training (RIT), manualized parent-mediated and video-aided intervention, JA intervention, music-incorporated applied behavioural analysis-verbal behaviour (ABA VB), speech-incorporated ABA VB, DIR-based intervention, parent-mediated preschool autism communication trials (PACT), symbolic play (SP), ESDM, and improvisational music therapy [32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43]. Trials aimed for improving the adaptive behaviour of children examined the impact of parent education and counselling (PEAC), parent education and behaviour management (PEBM), and home-based interventions [44, 45].
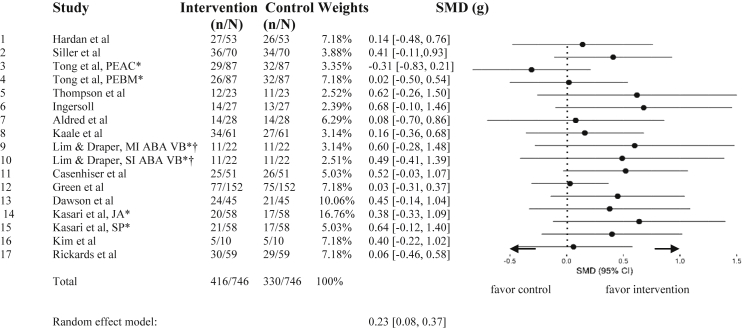
Across all studies, the pooled estimate effect provided by a random-effects model was 0.23 (95% CI [0.08–0.37]). There was no evidence for between-study heterogeneity (I2 = 0.00%, T2, p = 0.0018; Fig. 2). Studies with largest ES were RIT (SMD 0.68, 95% CI [0.08 to 1.48]) [35], SP (SMD 0.64, 95% CI [−0.06 to 1.37]) [41], and in-home FCMT (SMD 0.62, 95% CI [−0.22 to 1.54]) [34]. All interventions were provided by professionals. Duration ranged from 1.5 months to 4 months, and the intensity of the interventions was from 30 min/week to 210 min/week. RIT emphasised on the imitation skill whereas SP focused on language skill and FCMT based on reciprocal interaction. All were aimed for developing social engagement of ASD children. Even though RIT produced the largest SMD, it was a pilot study and investigators could not continue with a larger trial [35]. Similarly, SP provided intervention only for 13.5 months, and outcome measures were assessed at six months and 12 months follow-up. Longer duration between intervention period and assessment time could lead to a maturation effect. In contrast, FCMT could produce a larger effect within the lowest intensity (30 min/week) and shorter duration (four months) [34]. Other musical interventions produced preferable ES (SMD 0.60, 95% CI [0.09 to 1.85]) compared with parallel intervention; speech-incorporated ABA VB (0.49, 95% CI [0.28 to 2.09]) [38]. Improvisational music therapy based on inherent and communicability of children also produced large ES (SMD 0.40, 95% CI [0 to 0.78]) [42]. Other trials that produced preferable ES were DIR-based intervention (SMD 0.52, 95% CI [−0.04 to 1.09]) [39], PACT (SMD 0.45, 95% CI [−0.14 to 1.04]) [40], and focused playtime intervention (0.41, 95% CI [−0.03 to 0.98]) [33]. DIR-based intervention and PACT approach were provided by specialist therapists and duration of both interventions was 12 months with the intensity of 60 min/week and 210 min/week. In contrast, focused playtime intervention was provided by parents with the intensity of 90 min/week within a three-month period.
Fig. 2.
Effectiveness of interventions based on standardized mean difference (Hedges' g). MI ABA VB = Music incorporated applied behavioral analysis verbal behavior. PEAC = Parental education and counseling. PEBM = Parental education and behavioral management. SI ABA VB = Speech incorporated applied behavioral analysis verbal behavior. SMD = Standardized mean difference. g = Hedges' g. *Studies compared two intervention trials with one control group. They have common control group and so the number of participants in control group for both interventions was same. For this reason, the total number of population was different from individual study to combined studies. †Study used no intervention period for control condition. Therefore, number of participants in two interventions and control group was same. Heterogeneity: I2 = 0.00%, T2 = 0, p = 0.0018.
In decreasing order of ES, there were JA interventions (SMD 0.38, 95% CI [−0.24 to 1.11] [41] and SMD 0.16, 95% CI [−0.35 to 0.64]) [37], PRT (SMD 0.14, 95% CI [−0.44 to 0.72]) [32], parent-mediated communication-focused treatment (SMD 0.08, 95% CI [−0.69 to 0.86]) [36], home-based intervention (SMD 0.06, 95% CI [−0.45 to 0.71]) [45], PACT (SMD 0.03, 95% CI [−0.26 to 0.38]) [40], and two parallel interventions for adaptive behaviour; PEAC and PEBM (SMD -0.31, 95% CI [−0.82 to 0.20] for PEAC and SMD 0.02, 95% CI [−0.48 to 0.52] for PEBM) [44] respectively. In JA intervention with low ES [37], preschool teachers involved as intervention providers over two months period with the intensity of 100 min/week while another JA approach that produced larger ES used trained graduates [41] as care providers. One common characteristic of studies that produced lower effects involved parents [32, 33, 43, 45] and teachers [37, 45] as care providers. Delivering interventions by trained and specialist therapists produced larger ES and not all interventions that provided high intensity could develop more effective results. In summary, the quality of care provider, as well as the duration and intensity of the interventions, could be considered as situational factors that influence the effectiveness of cognitive, developmental, and behavioural approaches for children with ASD.
3. Conclusions
The purpose of our study was to identify the most effective interventions for preschool-aged children with ASD based on cognitive, developmental, and behavioural approaches and to explore the factors that may impact the effectiveness of the intervention. All studies reviewed were RCTs, and most of them were high-quality designs. Meta-analysis through use of the random-effects model suggested favourable outcomes to interventions included improving the communication and social interaction of children. Studies that emphasised restrictive and repetitive behaviour were limited, and the two studies that assessed these deficits produced lower effects. We have found that RIT, SP, and music therapy showed the largest effects for improving the communication and social interactions of affected children. The quality of the care provider, duration of the intervention, and intensity of the intervention were discovered as influencing factors for effective intervention outcomes. Since RIT was a pilot study and the SP produced larger effect over a longer period of intervention, we concluded that music therapy was the most effective intervention with shorter duration and lower intensity of intervention.
Three studies assessed the effectiveness of music therapy intervention by using the approaches of developmental [34], behavioural [38], and the inherent communicative ability of children [42]. The children in these studies were three to five years old, and the major improvements were reported in the areas of the parent-child relationship [34], speech and language production [38], JA behaviours, and non-verbal social communication [42]. Our finding is consistent with a Cochrane review, which assessed the effects of music therapy for people with ASD and concluded that music therapy might help increase social adaptation skills in children with ASD and promote the quality of parent-child relationships [46]. In that study, music therapy was superior to the control group in terms of social interaction which included non-verbal communicative skills, verbal communication skills, and social-emotional reciprocity.
The World Federation of Music Therapy defined music therapy as the professional use of music and its elements as an intervention in medical, educational, and everyday environments with individuals, groups, families, or communities who seek to optimise their quality of life and improve their physical, social, communicative, emotional, intellectual, and spiritual health and wellbeing [47]. Listening to well-known songs, playing musical games, and making improvised music could be included in a typical music therapy session [48]. Despite this, in the state guidance documents of USA published in 2010 for young children with ASD, music therapy was not recommended as a primary intervention while PRT, PECS, and other well-known approaches were mentioned as acceptable therapies [49]. The lack of recommendations for music therapy could be due to the inadequate scientific evidence of its effectiveness.
Similarly, there were preliminary results that favour evidence-based behavioural intervention such as PRT for ASD children. Recent reviews have provided empirical support for PRT through the neuroimaging evidence of affected children [50], analysing the results of meta-analysis [51], and systematically reviewing published articles [52]. The small sample size of included studies, single case study designs, lack of comparison group, and the wide range of age group led to inconclusive result for ensuring the effectiveness of PRT in preschool-aged children with ASD. Similar patterns have been found in the reviews that evaluate diverse disciplines and the wide range of views regarding the empirical and theoretical bases of naturalistic and ABA approaches for ASD [53, 54]. Although complete explorations of existing studies were appreciable, the lack of comparative evaluations of different programs limits hinder the universal agreement of reviews.
In our review, we identified and compared various interventions using cognitive, developmental, and behavioural approaches for ASD children. Among them, three different studies of music therapy intervention produced beneficial effects in focused areas of the core ASD symptoms. Music therapy may be effective through the use of behavioural, biomedical, developmental, educational, humanistic, adaptive music instructions and other models [55]. In this study, music therapy interventions used developmental, behavioural, and inherent communicative musicality approaches. In fact, music has been found to be a stimulant for the human capacity in the brain [56]. Engaging in musical stimuli for therapeutic purposes could provoke a foundation for practising social skills such as social interaction, and JA [57]. Similarly music has a strong connection with ToM [58], and it might also impact JA [59].
Here, we need to consider some situational factors that may influence the results of treatment. In the current review, intervention delivery by trained therapists who were professionally supervised by experts produced better outcomes than intervention provided by parents and teachers. In addition, the longer duration of treatment and increased intensity did not usually produce better outcome especially in JA [41], ESDM [43], and home-based interventions [45]. This finding was consistent with one previous trial that assessed the efficacy of interventions for improving feeding difficulties in children with ASD [60]. Its conclusions were contrary to previous recommendations that longer duration and increased intensity are basic principles for effective intervention [24, 49]. Although we also found some contrary evidence, the best timing and intensity of intervention were beyond the scope of our review. We would like to propose that the quality of the intervention provider, duration, and intensity of intervention are influencing factors for effective intervention. To use music therapy in clinical practice, more evidence-based results with larger samples are necessary to ensure and confirm the effectiveness of music therapy. According to our results, children with ASD should be treated flexibly in terms of the duration and intensity of therapy, and they should be cared for as normally developing children.
Our study has several limitations. First, the comparative evaluation of a broad range of interventions inevitably produced scattered outcome measures, and it was difficult to draw precise conclusions by meta-analysis. Second, we only searched the published articles and related literature, so did not search grey materials and unpublished data. Finally, specifying a definite publication period overlooked articles that were published before 2001 and after 2015. Despite these limitations, our study could identify the most effective intervention among the existing widely treatment approaches for pre-schoolers. Including only RCTs for our review process ensures the validity of this study, and by focusing on specific age group, we were able to reduce the inconsistency of sample population.
The evidence from this review suggests the further need for developing intervention strategies that focus on the restrictive and repetitive behaviour of children with ASD. Focusing on behavioural problems and simultaneously supporting communication and social interaction are hypothesised to represent comprehensive and successful therapy for affected children. Sequential study of systematic review and meta-analysis are also encouraged to clarify the strongly evidence-based practice for preschool-aged children with ASD.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This work was supported by Grants-in-Aid for Scientific Research awarded by the Japan Society for the Promotion of Science KAKENHI (Grant Number: KAKENHI15K1591307).
Competing interest statement
The authors declare no conflict of interest.
Additional information
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.American Psychiatric Association . fifth ed. vol. 5. American Psychiatric Association; Washington DC: 2013. (Diagnostic and Statistical Manual of Mental Disorders). [Google Scholar]
- 2.Biao J., Wiggins L., Christensen D.L., Maenner M.J., Daniels J., Warren Z. Prevalence of autism spectrum disorder among children aged 8 years — autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveill. Summ. 2018;67:1–23. doi: 10.15585/mmwr.ss6706a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brugha T.S., McManus S., Bankart J. Epidemiology of autism spectrum disorders in adults in the community in England. Arch. Gen. Psychiatry. 2011;68:459–466. doi: 10.1001/archgenpsychiatry.2011.38. [DOI] [PubMed] [Google Scholar]
- 4.Magiati I., Tay X.W., Howlin P. Cognitive, language, social and behavioural outcomes in adults with autism spectrum disorders: a systematic review of longitudinal follow-up studies in adulthood. Clin. Psychol. Rev. 2014;34:73–86. doi: 10.1016/j.cpr.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Locke J., Ishijima E.H., Kasari C., London N. Loneliness, friendship quality and the social networks of adolescents with high-functioning autism in an inclusive school setting. J. Res. Spec. Educ. Needs. 2010;10:74–81. [Google Scholar]
- 6.Steinhauen H.C., Mohr Jensen C., Lauristen M.B. A systematic review and meta-analysis of the long-term overall outcome of autism spectrum disorders in adolescence and adulthood. Acta Psychiatr. Scand. 2016;133:445–452. doi: 10.1111/acps.12559. [DOI] [PubMed] [Google Scholar]
- 7.van Elst L.T., Pick M., Biscaldi M., Fangmeier T., Riedel A. High-functioning autism spectrum disorder as a basic disorder in adult psychiatry and psychotherapy: psychopathological presentation, clinical relevance and therapeutic concepts. Eur. Arch. Psychiatry Clin. Neurosci. 2013;263:S189–S196. doi: 10.1007/s00406-013-0459-3. [DOI] [PubMed] [Google Scholar]
- 8.Korkmaz B. Theory of mind and neurodevelopmental disorders of childhood. Pediatr. Res. 2011;69:101R–108R. doi: 10.1203/PDR.0b013e318212c177. [DOI] [PubMed] [Google Scholar]
- 9.Pedersen T. Psych Central; 2018. Theory of Mind.https://psychcentral.com/encyclopedia/theory-of-mind/ Available from: [Google Scholar]
- 10.Child Welfare Information Gateway . 2015. Understanding the Effects of Maltreatment on Brain Development.https://www.childwelfare.gov/pubPDFs/brain_development.pdf Available from: [Google Scholar]
- 11.Kuhl P.K. Brain mechanisms in early language acquisition. Neuron. 2010;67:713–727. doi: 10.1016/j.neuron.2010.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dommet E. The structure of the human brain. In: Oates J., editor. vol. 7. The Open University; United kingdom: 2012. (Early Childhood in Focus). Available from http://oro.open.ac.uk/33493/1/Developing_Brains.pdf. [Google Scholar]
- 13.Craig F., Margari F., Legrottaglie A.R., Plaumbi R., de Giambattia C., Margari L. A review of executive function deficits in autism spectrum disorder and attention-deficit/hyperactivity disorder. Neuropsychiatric Dis. Treat. 2016;12:1191–1202. doi: 10.2147/NDT.S104620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Daymut J.A. 2009. Joint Attention Skills and the Child with Autism.https://www.superduperinc.com/handouts/pdf/196_joinattentionandasd.pdf Available from: [Google Scholar]
- 15.Little E. 2018. Joint Attention.https://carta.anthropogeny.org/moca/topics/joint-attention Available from: [Google Scholar]
- 16.Scott J.G., Mihalopoulos C., Erskine H.E., Roberts J., Rahman A. Childhood mental and developmental disorders. In: Patel V., editor. Mental, Neurological, and Substance Use Disorders. World bank group; Washington DC: 2015. [Google Scholar]
- 17.Smith V.K., Dillenbeck A. Developing and implementing early intervention plans for children with Autism Spectrum Disorders. Semin. Speech Lang. 2006;27:10–20. doi: 10.1055/s-2006-932435. [DOI] [PubMed] [Google Scholar]
- 18.National Research Council . The National Academy Press; Washington, DC: 2001. Educating Children with Autism. [Google Scholar]
- 19.Lindgren S., Doobay A. Iowa Department of Human Services; 2011. Evidence-based Interventions for Autism Spectrum Disorders.http://www.interventionsunlimited.com/editoruploads/files/Iowa%20DHS%20Autism%20Interventions%206-10-11.pdf Available from. [Google Scholar]
- 20.Narzisi A., Costanza C., Umberto B., Filippo M. Non-pharmacological treatments in Autism Spectrum Disorders: an overview on early interventions for pre-schoolers. Curr. Clin. Pharmacol. 2014;9:17–26. doi: 10.2174/15748847113086660071. [DOI] [PubMed] [Google Scholar]
- 21.Warren Z., McPheeters M., Sathe N., Foss-Feig J.H., Glasser A.C., Veenstra-VanderWeele J. A systematic review of early intensive intervention for Autism Spectrum Disorders. Pediatrics. 2011;127:e1303–e1311. doi: 10.1542/peds.2011-0426. [DOI] [PubMed] [Google Scholar]
- 22.Seida J.K., Ospina M.B., Karkhaeh M., Hartling L., Smith V., Clark B. Systematic reviews of psychosocial interventions for autism: an umbrella review. Dev. Med. Child Neurol. 2009;51:95–104. doi: 10.1111/j.1469-8749.2008.03211.x. [DOI] [PubMed] [Google Scholar]
- 23.Fernandes F.D., Amato C.A. Applied behavior analysis and autism spectrum disorders: literature review. CoDAS. 2013;25:289–296. doi: 10.1590/s2317-17822013000300016. [DOI] [PubMed] [Google Scholar]
- 24.Wong C., Odom S.L., Hume K.A., Cox A.W., Fettig A., Kucharczyk S. Evidence-based practices for children, youth, and young adults with Autism Spectrum Disorder: a comprehensive review. J. Autism Dev. Disord. 2015;45:1951–1966. doi: 10.1007/s10803-014-2351-z. [DOI] [PubMed] [Google Scholar]
- 25.Masic I., Miokovic M., Muhamedagic B. Evidence based medicine – new approaches and challenges. Acta Inf. Med. 2008;16:219–225. doi: 10.5455/aim.2008.16.219-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 27.The Cochrane Collaboration . 2017. Assessing Risk of Bias in Included Studies.http://methods.cochrane.org/bias/assessing-risk-bias-included-studies Available from: [Google Scholar]
- 28.Reichow B. Development, procedures, and application of the evaluative method for determining evidence-based practices in autism. In: Reichow B., editor. Evidence-based Practices and Treatments for Children with Autism. 2011. pp. 25–39. [Google Scholar]
- 29.Field A.P. Is the meta-analysis of correlation coefficients accurate when population correlations vary? Psychol. Meth. 2005;4:444–467. doi: 10.1037/1082-989X.10.4.444. [DOI] [PubMed] [Google Scholar]
- 30.Viechtbauer W. 2017. Package 'metafor': Meta-analysis Package for R.https://cran.r-project.org/web/packages/metafor/metafor.pdf Available from: [Google Scholar]
- 31.Field A.P. Meta-analysis in clinical psychology research. In: Comer J.S., Kendall P.C., editors. The Oxford Handbook of Research Strategies for Clinical Psychology. Oxford University Press; 2012. pp. 317–335. [Google Scholar]
- 32.Hardan A.Y., Gengoux G.W., Berquist K.L., Libove R.A., Ardel C.M., Phillips J. A randomized controlled trial of pivotal response treatment group for parents of children with autism. J. Child Psychol. Psychiatry. 2015;56:884–892. doi: 10.1111/jcpp.12354. [DOI] [PubMed] [Google Scholar]
- 33.Siller M., Swanson M., Gerber A., Hutman T., Sigman M. A parent-mediated intervention that targets responsive parental behaviors increases attachment behaviors in children with ASD: results from a randomized clinical trial. J. Autism Dev. Disord. 2014;44:1720–1732. doi: 10.1007/s10803-014-2049-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thompson G.A., McFerran K.S., Gold C. Family-centred music therapy to promote social engagement in young children with severe autism spectrum disorder: a randomized controlled study. Child Care Health Dev. 2014;40:840–852. doi: 10.1111/cch.12121. [DOI] [PubMed] [Google Scholar]
- 35.Ingersoll B. Brief report: effect of a focused imitation intervention on social functioning in children with autism. J. Autism Dev. Disord. 2012;42:1768–1773. doi: 10.1007/s10803-011-1423-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aldred C., Green J., Emsley R., McConachie H. Brief report: mediation of treatment effect in a communication intervention for pre-school children with autism. J. Autism Dev. Disord. 2012;42:447–454. doi: 10.1007/s10803-011-1248-3. [DOI] [PubMed] [Google Scholar]
- 37.Kaale A., Smith L., Sponheim E. A randomized controlled trial of preschool-based joint attention intervention for children with autism. J. Child Psychol. Psychiatry. 2012;53:97–105. doi: 10.1111/j.1469-7610.2011.02450.x. [DOI] [PubMed] [Google Scholar]
- 38.Lim H.A., Draper E. The effects of music therapy incorporated with applied behavior analysis verbal behavior approach for children with Autism Spectrum Disorders. J. Music Ther. 2011;48:532–550. doi: 10.1093/jmt/48.4.532. [DOI] [PubMed] [Google Scholar]
- 39.Casenhiser D.M., Shanker S.G., Stieben J. Learning through interaction in children with autism: preliminary data from asocial-communication-based intervention. Autism. 2011;17:220–241. doi: 10.1177/1362361311422052. [DOI] [PubMed] [Google Scholar]
- 40.Green J., Charman T., McConachie H., Aldred C., Slonims V., Howlin P. Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. Lancet. 2010;375:2152–2160. doi: 10.1016/S0140-6736(10)60587-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kasari C., Paparella T., Freeman S., Jahromi L.B. Language outcome in autism: randomized comparison of joint attention and play interventions. J. Consult. Clin. Psychol. 2008;76:125–137. doi: 10.1037/0022-006X.76.1.125. [DOI] [PubMed] [Google Scholar]
- 42.Kim J., Wigram T., Gold C. The effects of improvisational music therapy on joint attention behaviors in autistic children: a randomized controlled study. J. Autism Dev. Disord. 2008;38:1758–1766. doi: 10.1007/s10803-008-0566-6. [DOI] [PubMed] [Google Scholar]
- 43.Dawson G., Rogers S., Munson J., Smith M., Winter J., Greenson J. Randomized controlled trial of an intervention for toddlers with autism: the early start Denver model. Pediatrics. 2010;125:e17–e23. doi: 10.1542/peds.2009-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tonge B., Brereton A., Kiomall M., Mackinnon A., Rinehart N.J. A randomised group comparison controlled trial of ‘preschoolers with autism’: a parent education and skills training intervention for young children with autistic disorder. Autism. 2014;18:166–177. doi: 10.1177/1362361312458186. [DOI] [PubMed] [Google Scholar]
- 45.Rickards A.L., Walstab J.E., Wright-Rossi R.A., Simpson J., Reddihough D.S. A randomized controlled trial of a home-based intervention program for children with autism and developmental delay. J. Dev. Behav. Pediatr. 2007;28:308–316. doi: 10.1097/DBP.0b013e318032792e. [DOI] [PubMed] [Google Scholar]
- 46.Geretsegger M., Elefant C., Mossler K.A., Gold C. Music therapy for people with autism spectrum disorder. Cochrane Database Syst. Rev. 2014;17:1–63. doi: 10.1002/14651858.CD004381.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Federation of Music Therapy . 2011. What Is Music Therapy?http://www.wfmt.info/WFMT/Info_Cards_files/ENGLISH%20-%20NEW%20What%20is%20music%20therapy.pdf Available from: [Google Scholar]
- 48.Guy's and St Thomas' NHS Foundation Trust . 2017. Music Therapy at Evelina London.https://www.evelinalondon.nhs.uk/resources/patient-information/music-therapy.pdf Available from. [Google Scholar]
- 49.Coakley T. State guidance documents for young children with autism spectrum disorders content and comparison. Infants Young Child. 2010;23:145–164. [Google Scholar]
- 50.Lei J., Ventola P. Pivotal response treatment for autism spectrum disorder: current perspectives. Neuropsychiatric Dis. Treat. 2017;13:1613–1626. doi: 10.2147/NDT.S120710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bozkus-Genc G., Yucesoy-Ozkan S. Meta-analysis of pivotal response training for children with Autism Spectrum Disorder. Educ. Train. Autism Dev. Disabil. 2016;51:13–26. http://daddcec.org/Portals/0/CEC/Autism_Disabilities/Research/Publications/Education_Training_Development_Disabilities/2015v50/ETADD_51(1)_13-26.pdf Available from. [Google Scholar]
- 52.Verschuur R., Didden R., Lang R., Sigafoos J., Huskens B. Pivotal response treatment for children with Autism Spectrum Disorders: a systematic review. Rev. J. Autism Dev. Disord. 2014;1:34–61. [Google Scholar]
- 53.Schreibman L., Dawson G., Stahmer A.C., Landa R., Rogers S.J., McGee G.G. Naturalistic developmental behavioral interventions: empirically validated treatments for Autism Spectrum Disorder. J. Autism Dev. Disord. 2015;45:2411–2428. doi: 10.1007/s10803-015-2407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Magiati I., Tay X.W., Howlin P. Early comprehensive behaviorally based interventions for children with autism spectrum disorders: a summary of findings from recent reviews and meta-analyses. Neuropsychiatry. 2012;2:543–570. [Google Scholar]
- 55.American Music Therapy Association . 2012. Music Therapy as a Treatment Modality for Autism Spectrum Disorders.http://www.musictherapy.org/assets/1/7/MT_Autism_2012.pdf Available from: [Google Scholar]
- 56.Wolf L., Wolf T. 2011. Music and Health Care.http://wolfbrown.com/42-books-and-reports/491-music-healthcare Available from: [Google Scholar]
- 57.LaGasse A.B. Social outcomes in children with autism spectrum disorder: a review of music therapy outcomes. Patient Relat. Outcome Meas. 2017;20:23–32. doi: 10.2147/PROM.S106267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Livingstone S.R., Thompson W.F. The emergence of music therapy from Theory of Mind. Music. Sci. 2009:83–115. [Google Scholar]
- 59.Malczewski P. 2010. Critical Review: what Is the Impact of Music Therapy on the Joint Attention Skills of Preschoolers with Autism Spectrum Disorder?https://www.uwo.ca/fhs/csd/ebp/reviews/2009-10/Malczewski.pdf Available from: [Google Scholar]
- 60.Marshall J., Ware R., Ziviani J., Hill R.J., Dodrill P. Efficacy of interventions to improve feeding difficulties in children with autism spectrum disorders: a systematic review and meta-analysis. Child Care Health Dev. 2015;41:278–302. doi: 10.1111/cch.12157. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.