Key Points
Question
Do state laws permitting the denial of services to same-sex couples affect mental distress among sexual minority adults?
Findings
This difference-in-difference-in-differences analysis indicated that state laws permitting the denial of services to same-sex couples were associated with a 46% increase in the proportion of sexual minority adults experiencing mental distress.
Meaning
Policymakers and courts considering laws permitting the denial of services to same-sex couples should take into account that these laws are associated with increases in mental distress among sexual minority adults.
This study investigates whether US state laws permitting refusal of services to sexual minority individuals were associated with changes in the proportion of sexual minority adults reporting mental distress.
Abstract
Importance
Recent evidence suggests that state policies affecting sexual minorities are associated with health disparities. Twelve states have laws permitting the denial of services to same-sex couples, and the US Supreme Court is considering whether states can prohibit the denial of services to same-sex couples.
Objective
We investigated whether state laws permitting individuals to refuse services to sexual minorities were associated with changes in the proportion of sexual minority adults reporting mental distress.
Design, Setting, and Participants
This difference-in-difference-in-differences linear regression analysis with state fixed effects used Behavioral Risk Factor Surveillance System (BRFSS) data from 2014 through 2016 from adults aged 18 to 64 years in 3 states that implemented laws permitting the denial of services to same-sex couples (Utah, Michigan, and North Carolina) and 6 nearby control states (Idaho and Nevada, Ohio and Indiana, and Virginia and Delaware, respectively). Sexual minority adults were defined as those who identified as gay, lesbian, bisexual, or not sure of their sexual orientation under a module on sexual orientation that BRFSS implemented in 2014 and each state could opt to include. Analysis controlled for year and individual-level sex, race, ethnicity, age group, educational attainment, income, employment, and marital status. A permutation test was conducted to precisely estimate statistical significance.
Exposures
An interaction term indicating whether individuals identified as a sexual minority and lived in a state with a law permitting denial of services to same-sex couples in 2015.
Main Outcomes and Measures
Mental distress, defined as poor mental health on 14 or more of the past 30 days.
Results
Of 109 089 participants, 4656 (4.8%; all percentages incorporate survey weights) identified as sexual minorities, 86141 (72.1%) were non-Hispanic white, and ages were uniformly distributed between 18 and 64 years. In 2014, 2038 of 16637 heterosexual adults (12.6%) and 156 of 815 sexual minority adults (21.9%) in the 3 same-sex denial states reported mental distress. The proportion of sexual minority adults reporting mental distress increased by 10.1 percentage points (95% CI, 1.8 to 18.5 percentage points, permutation-adjusted P value = .046) between 2014 and 2016 in states that passed laws permitting denial of services to same-sex couples compared with control states, a 46% relative increase in sexual minority adults experiencing mental distress. Laws permitting denial of services to same-sex couples were not associated with significant changes in heterosexual adults experiencing mental distress (−0.36 percentage points, 95% CI, −1.73 to 1.01 percentage points).
Conclusions and Relevance
Laws permitting denial of services to same-sex couples, which exist in 12 states and are under consideration by the US Supreme Court, are associated with a 46% increase in sexual minority adults experiencing mental distress.
Introduction
Sexual minorities in the United States bear a disproportionate burden of depression, anxiety, mental distress, and suicide attempts compared with heterosexuals.1 Poor mental health is associated with worse quality of life, worse physical health,2,3 and elevated mortality.4,5 Fundamental cause theory6 stipulates that stigma—“the co-occurrence of labeling, stereotyping, separation, status loss, and discrimination in a context in which power is exercised”7(p813)—is a persistent cause of population health inequities.7,8 According to fundamental cause theory, social factors, or circumstances (including stigma), remain persistently associated with health inequities because they entail access to resources (including knowledge, money, power, and social relationships) that contribute to health and well-being. Consistent with the application of fundamental cause theory to sexual orientation health disparities,7 evidence indicates that sexual orientation–related stigma at the neighborhood,9 school,10 family,11 peer,12 and individual13 levels is associated with adverse mental health outcomes. Further evidence indicates changes in state-level institutional stigma, such as through same-sex marriage laws, are associated with changes in mental health outcomes among sexual minorities.14,15,16
The United States is at a turning point with regard to institutional stigma in the form of federal and state laws permitting the denial of services to sexual minorities. The Supreme Court decision in Masterpiece Cakeshop vs the Colorado Civil Rights Commission17 could have implications for the 21 states with laws protecting sexual minorities from discrimination. At the national level, the new Conscience and Religious Freedom Division of the US Department of Health and Human Services may permit health care professionals to deny services to sexual minorities across the country. At the state level, 12 US states had implemented laws permitting the denial of services to sexual minorities by 2017.18 We aimed to evaluate whether the implementation of laws permitting denial of services to same-sex couples was associated with changes in mental distress among sexual minority adults.
Methods
We used Behavioral Risk Factor Surveillance System (BRFSS) data collected by the US Centers for Disease Control and Prevention (CDC) in partnership with state health departments (eAppendix 1 in the Supplement). The BRFSS data were collected through a combination of disproportionate stratified sampling of landline telephones and random sampling of cellular telephones.19 The CDC computes weights to make BRFSS data representative of all adults in each state. All study analyses accounted for the BRFSS sampling structure and weights. Each state survey consists of core health questions designated by the CDC, a set of optional modules developed by the CDC, and any additional questions designated by the state. We included data from 2014 to 2016, all years available since the CDC first included an optional module with questions on sexual orientation and gender identity in 2014. We included all adults aged 18 to 64 years who responded to questions about their sexual orientation and mental health.
The Boston University institutional review board determined that this study did not qualify as human subjects research because of the deidentified nature of the data. Accordingly, consent procedures were not needed.
We included data from all 3 states that passed laws permitting denial of services to same-sex couples in 2015 and that collected data on sexual orientation identity: Utah, Michigan, and North Carolina. We took a data-driven approach to selecting sets of geographically nearby control states (Idaho and Nevada, Ohio and Indiana, and Virginia and Delaware, respectively) that were most similar based on demographic characteristics (described in detail in eAppendix 2 and eTables 1-3 in the Supplement).
We defined the exposure as being a sexual minority and living in a state that implemented 1 or more laws permitting denial of services to same-sex couples for reasons associated with religious beliefs during the study period. We considered individuals to be sexual minorities if they identified as gay, lesbian, bisexual, or not sure of their sexual orientation.
In May 2015, Utah implemented Senate Bill 297,20 permitting government officials to refuse to participate in issuing marriage licenses for same-sex couples. Michigan passed House Bills 4188, 4189, and 4190 in June 2015,21 permitting adoption and child welfare agencies to refuse to permit same-sex couples to adopt children. North Carolina passed Senate Bill 2 in June 2015,22 allowing magistrates to refuse to perform same-sex marriages and passed House Bill 2 in March 2016,23 prohibiting cities or counties from passing laws preventing discrimination based on sexual orientation or gender identity. For the 3 states with laws permitting denial of services to same-sex couples, we excluded 2015 from the analysis because it would have contained a mix of participants interviewed before and after implementation of pertinent laws.
While Indiana passed Senate Bill 101 in March 2015,24 allowing individuals or companies to claim their exercise of religion as a legal defense for discriminatory practices against same-sex individuals, it prohibited sexual orientation discrimination with Senate Bill 5025 in April 2015; we therefore did not consider Indiana a same-sex denial state. Although Arkansas passed 2 bills and Kansas issued an executive order permitting denial of services to same-sex couples during the study period, these states were excluded because they did not collect BRFSS data on sexual orientation in all 3 study years.
The main outcome of interest was mental distress defined as poor mental health in 14 or more of the past 30 days. This binary outcome was based on dichotomizing the BRFSS mentally unhealthy days measure, which was designed to capture self-reported quality of life.26 The question read, “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” Response options ranged from 0 to 30 days. In a prior study, the 2-week test-retest reliability was 0.70 for adults aged 18 to 64 years and 0.55 for adults older than 65 years, whom we excluded from the main analysis.27 Validation studies indicate the mentally unhealthy days measure has high construct validity for depression28 and high (>70%) concurrent validity with the Short Form-36 and Patient Health Questionnaire depression scales.28,29,30 Our definition of mental distress as poor mental health in 14 or more of the past 30 days is consistent with the approach used to track population health since 199831,32,33 and with a study documenting sexual orientation mental health disparities.1
We first evaluated whether mental distress was comparable at baseline in states that passed laws permitting denial of services to same-sex couples vs control states. Because 2014 was the first year that the CDC included a question on sexual orientation, we evaluated the comparability of mental distress among sexual minority adults in same-sex denial states and control states in 2014 with a logistic regression controlling for all demographic variables included in the main analysis. We also evaluated whether there were parallel trends in mental distress in the full adult population by estimating a logistic regression model using BRFSS data from 2012 to 2014, with mental distress as the outcome and the main exposure variable defined as the interaction term consisting of living in a same-sex denial state and linear year, again controlling for all demographic variables included in the main analysis. We began with 2012 as the first year after a BRFSS design change to include interviews conducted via mobile telephones as well as landline telephones.
We next evaluated the association between same-sex denial laws and mental distress using a difference-in-differences approach, which involves comparing before and after changes in an outcome in a treatment group (defined here as living in a same-sex denial state) to before and after changes in a control group34,35; difference-in-difference-in-differences methods include a second control group. We conducted a difference-in-difference-in-differences analysis comparing changes in mental distress among sexual minority adults in states that permit the denial of services to same-sex couples with changes in mental distress among heterosexual adults living in the same states and with changes in mental distress among sexual minority adults in control states. We estimated a linear regression model with mental distress as the outcome, using a linear model rather than logit model with the binary outcome because of the linear model’s unbiased estimation properties with fixed effects analyses.36 The main exposure of interest was a binary term interacting implementation of a state law permitting denial of services to same-sex couples with a binary term for sexual orientation identity. We also included separate terms for sexual minority orientation and for state laws permitting denial of services to same-sex couples and controlled for individual-level sex, race, ethnicity, age group, educational attainment, income, employment status, and marital status (categories described in Table 1). We included state and year fixed effects to control for each state and year overall and terms interacting each state and year with sexual orientation. Controlling for each state controlled for differences in baseline levels of mental distress in each state, as well as for all state characteristics that did not change over the study period. Controlling for each year accounted for potential shocks in each year (eg, same-sex marriage becoming legal nationwide in June 2015).
Table 1. Participant Characteristics in States With Laws Permitting Denial of Services to Same-Sex Couples and Control States.
| Characteristic (N = 109 089) | No. (%)a | ||
|---|---|---|---|
| Control States (n = 71 575) | Same-Sex Denial States (n = 37 514) | P Valueb | |
| Sexual orientation | |||
| Straight | 68 473 (94.9) | 35 960 (95.8) | <.001 |
| Gay, lesbian, bisexual, or not sure | 3102 (5.1) | 1554 (4.2) | <.001 |
| Race/ethnicity | |||
| Non-Hispanic white | 56 486 (72.6) | 29 655 (71.0) | <.001 |
| Non-Hispanic black | 6545 (12.6) | 3080 (15.3) | <.001 |
| Hispanic | 4083 (7.9) | 2530 (7.3) | .04 |
| Other race/ethnicity | 2176 (4.1) | 1277 (4.0) | .71 |
| Non-Hispanic multiracial | 1308 (1.5) | 587 (1.4) | .13 |
| Unknown/other | 977 (1.3) | 385 (0.9) | <.001 |
| Sex | |||
| Male | 31 038 (49.2) | 17 475 (49.3) | .77 |
| Female | 40 537 (50.8) | 20 039 (50.7) | .77 |
| Age group, y | |||
| 18-24 | 5052 (15.3) | 3903 (16.2) | .04 |
| 25-34 | 9174 (19.6) | 6247 (20.0) | .35 |
| 35-44 | 12 345 (20.2) | 7775 (20.6) | .31 |
| 45-54 | 18 529 (22.6) | 8653 (21.8) | .04 |
| 55-64 | 26 475 (22.3) | 10 936 (21.4) | .01 |
| Educational attainment | |||
| Did not graduate high school | 4894 (11.7) | 2237 (11.7) | .96 |
| High school graduate | 20 830 (30.3) | 9662 (27.2) | <.001 |
| Attended college/technical school | 19 841 (32.2) | 11 890 (35.9) | <.001 |
| Graduated from college/technical school | 25 849 (25.6) | 13 670 (25.1) | .17 |
| Not reported | 161 (0.2) | 55 (0.1) | .01 |
| Income group, $ | |||
| <10 000 | 3103 (4.5) | 1488 (5.3) | .001 |
| 10 000-14 999 | 2917 (3.8) | 1360 (4.1) | .11 |
| 15 000-19 999 | 4152 (6.1) | 1930 (6.4) | .15 |
| 20 000-24 999 | 5210 (7.9) | 2475 (7.5) | .17 |
| 25 000-34 999 | 5967 (8.5) | 2977 (8.8) | .26 |
| 35 000-49 999 | 8687 (12.3) | 4459 (12.0) | .39 |
| 50 000-74 999 | 10 913 (14.7) | 5978 (14.4) | .37 |
| 75 000 or more | 22 775 (30.2) | 12 272 (27.8) | <.001 |
| Not reported | 7851 (12.1) | 4575 (13.7) | <.001 |
| Employment status | |||
| Employed | 41 595 (60.5) | 21 944 (57.0) | <.001 |
| Self-employed | 6263 (8.3) | 3541 (8.7) | .13 |
| Out of work >1 y | 1914 (2.9) | 912 (3.1) | .13 |
| Out of work <1 y | 1897 (3.3) | 1017 (3.5) | .27 |
| Homemaker | 4530 (5.9) | 3099 (6.4) | .03 |
| Student | 2243 (6.2) | 1645 (7.0) | .01 |
| Retired | 6039 (4.9) | 2368 (5.1) | .41 |
| Unable to work | 6692 (7.5) | 2792 (8.7) | <.001 |
| Not reported | 402 (0.6) | 196 (0.5) | .10 |
| Marital status | |||
| Married | 40 512 (51.5) | 22 527 (51.9) | .46 |
| Divorced | 10 536 (11.6) | 4339 (10.7) | .001 |
| Widowed | 2705 (2.2) | 972 (2.1) | .55 |
| Separated | 1729 (2.5) | 867 (2.9) | .02 |
| Never married | 13 342 (26.9) | 7474 (27.8) | .05 |
| Unmarried couple | 2390 (4.8) | 1197 (4.3) | .06 |
| Not reported | 361 (0.5) | 138 (0.3) | <.001 |
Percentages incorporate population survey weights.
P values are derived from χ2 tests.
Difference-in-difference analyses with a small number of groups can produce standard errors that are too low, making confidence intervals overly narrow.37 We therefore estimated the P value with permutation tests using the 3-state groups included in the main analysis, as well as selecting 1 additional 3-state group from among the 8 other states that collected data on sexual orientation identity: Minnesota, Wisconsin, and Pennsylvania. In 1000 permutations, we randomly selected 3 of the 4 state groups and randomly selected a so-called treatment state and 2 control states for each group. The P value is based on the percent chance of obtaining the estimated t statistic from the permutation test distribution of t statistics. We considered P values less than .05 statistically significant. We also conducted sensitivity analyses, repeating the main analysis using a logistic regression model, including participants older than 65 years, excluding participants who reported that they were unsure of their sexual orientation, including same-sex marriage laws, and using the continuous measure of mentally unhealthy days as the main outcome.
Results
The sample included 109 089 adults, with 71 575 in 6 control states and 37 514 in 3 states that passed laws permitting denial of services to same-sex couples. We describe the characteristics of participants in Table 1. Of the adults in the full sample, 4656 (4.8%; all percentages incorporate survey weights) identified as sexual minorities; 17 146 (11.8%) of adults were excluded because of nonresponses to the sexual orientation question.
In 2014, 5130 of 43 719 (12.5%) of heterosexual adults and 373 of 1876 (23.0%) of sexual minority adults in the 9 states in the sample experienced mental distress. Baseline levels of mental distress were similar among sexual minority adults in same-sex denial states (156 of 815; 21.9%) and control states (217 of 1061; 23.5%) and did not significantly differ (adjusted odds ratio [aOR], 0.96; 95% CI, 0.43 to 2.16; P = .92). In the 2012 to 2014 dataset, trends in mental distress were not statistically significantly different in states that implemented laws permitting denial of services to same-sex couples compared with control states (aOR, 1.02; 95% CI, 0.96 to 1.09; eTable 4 and the eFigure in the Supplement).
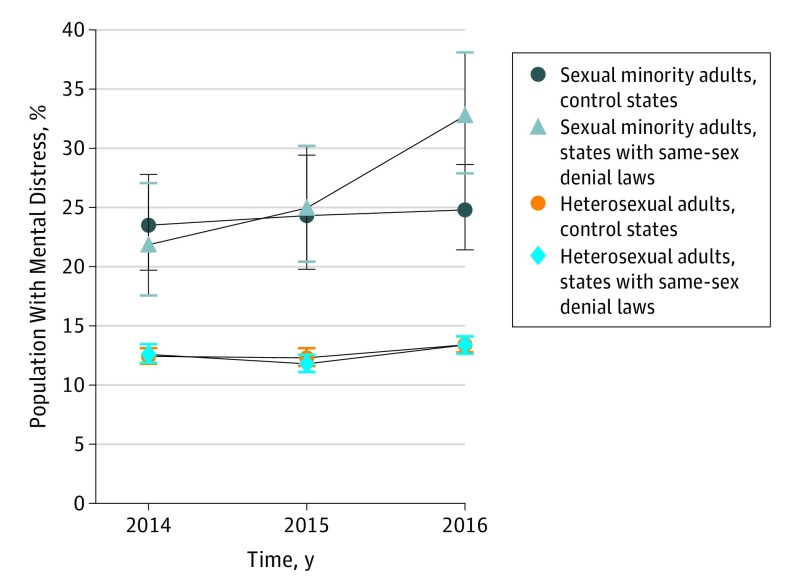
The proportion of sexual minority adults reporting mental distress increased by 10.9 percentage points, from 156 of 815 (21.9%) in 2014 to 203 of 739 (32.8%) in 2016, in the 3 states that implemented laws permitting denial of services to same-sex couples. In contrast, the proportion of sexual minority adults reporting mental distress increased by 1.3 percentage points, from 217 of 1061 (23.5%) in 2014 to 259 of 1187 (24.8%) in 2016, in the 6 control states (Figure). In the main difference-in-difference-in-differences analysis, the proportion of sexual minority adults reporting mental distress increased by 10.13% (95% CI, 1.76 to 18.50 percentage points; permutation adjusted P value = .046; Table 2; eTable 5 in the Supplement) in states that passed laws permitting denial of services to same-sex couples compared with heterosexual adults in the same state and sexual minority adults in the 6 control states. This is equivalent to a 46% relative increase in the proportion of sexual minority adults reporting mental distress. The proportion of heterosexual adults experiencing mental distress increased by 0.8 percentage points, from 2038 of 18 675 (12.6%) in 2014 to 2147 of 17 258 (13.4%) in 2016, in the 3 states that passed laws permitting denial of services to same-sex couples and increased 1.0 percentage points, from 3029 of 25 044 (12.4%) in 2014 to 3063 of 23 438 (13.4%) in 2016, in the 6 control states. Laws permitting denial of services to same-sex couples were not associated with statistically significant changes in the proportion of heterosexual adults experiencing mental distress (−0.36 percentage points; 95% CI, −1.73 to 1.01 percentage points).
Figure. Changes in the Percentage of Adults Experiencing Mental Distress in Same-Sex Denial and Control States by Sexual Orientation.
Table 2. Change in Population Experiencing Mental Distress After Implementation of Laws Permitting Denial of Services to Same-Sex Couples.
| Population (N = 109 089) | Mental Distress in Same-Sex Denial States, No. (%) | Mental Distress in Control States | Difference-in-Difference Estimatesa | |||||
|---|---|---|---|---|---|---|---|---|
| 2014 | 2016 | Change | 2014 | 2016 | Change | Change in Mental Distress, Percentage Points | 95% CI, Percentage Points | |
| Heterosexual adults (n = 104 433)b | 2038/ 18 675 (12.6) |
2147/ 17 258 (13.4) |
0.8 | 3029/ 25 044 (12.4) |
3063/ 23 438 (13.4) |
1.0 | −0.36 | −1.73 to 1.01 |
| Sexual minority adults (n = 4656)b | 156/ 815 (21.9) |
203/ 739 (32.8) |
10.9 | 217/ 1061 (23.5) |
259/ 1187 (24.8) |
1.3 | 10.13c | 1.76 to 18.50 |
Difference-in-difference estimates of changes on mental distress associated with laws permitting the denial of services to same-sex couples.
Group sizes reflect the full sample size in the main analysis, including 2015 data for control states.
P = .046.
The results of sensitivity analyses were consistent with the main results when we ran a logistic regression analysis (aOR, 1.88; 95% CI, 1.13 to 3.13; eTable 6 in the Supplement), when we included adults over age 65 years (8.70 percentage points; 95% CI, 1.18 to 16.22 percentage points; eTable 7 in the Supplement), when we excluded adults who were unsure of their sexual orientation (9.75 percentage point; 95% CI, 0.42 to 19.19 percentage points; eTable 8 in the Supplement), and when we included same-sex marriage (10.14 percentage points; 95% CI, 1.77 to 18.51 percentage points; eTable 9 in the Supplement). Same-sex denial laws were associated with 2.47 additional unhealthy days in the past 30 days (95% CI, 0.49 to 4.46 days; eTable 10 in the Supplement) among sexual minority adults.
Discussion
Our finding that laws permitting denial of services to same-sex couples were associated with a 46% increase in the proportion of sexual minority adults experiencing mental distress suggests that these laws might harm sexual minority mental health. The findings may have relevance to ongoing national discussions at a time when 12 states have laws permitting denial of services to sexual minorities, when the US Supreme Court is considering the constitutionality of a Colorado law preventing the denial of services to same-sex couples,17 and when the US Department of Health and Human Services might permit health care professionals to deny services to sexual and gender minorities.38
Prior evidence indicates that state same-sex marriage laws were associated with improvements in mental health for sexual minority adolescents14 and adults15 and that constitutional amendments banning same-sex marriage were associated with increases in psychiatric morbidity among sexual minorities.39 Our findings contribute important additional information by extending this literature to laws permitting denial of services to same-sex couples. Together, these results suggest that multiple types of laws affecting sexual minority rights are associated with sexual minority mental health.
There are a number of potential mechanisms by which state laws that permit denial of services based on sexual orientation might affect mental health outcomes among sexual minorities. First, directly experiencing a refused marriage license or adoption might harm mental health. The effects of marriage or adoption refusal could also affect the mental health of sexual minority individuals in the same social networks as those who experience refusal. Second, state laws that permit discrimination against sexual minorities might affect whether others perceive and treat sexual minorities as equal citizens and whether sexual minorities perceive themselves as equal citizens. Third, media coverage of state laws permitting denial of services to same-sex couples and attendant discourse may also affect the salience of these laws and their impact on sexual minority mental health.40 That increases in mental distress occurred within 7 to 18 months after the implementation of these laws suggests that changes in mental distress might have been because of mechanisms with an immediate impact, such as media coverage and the awareness of unequal rights, rather than slower mechanisms, such as direct exposure to service denial. It will be important for future research to further investigate these and other mechanisms.
The validity of the difference-in-differences approach is contingent on no other state-level changes impacting mental distress during the same time period. We have evidence that it is unlikely there were other factors that led to changes in mental distress in the full population, because we observed no significant changes in the mental health of heterosexual adults living in same-sex denial states. We also found that our results were robust to the inclusion of state same-sex marriage laws.
The magnitude of the 10.13–percentage point increase (a 46% relative increase) in mental distress associated with laws permitting denial of services to same-sex couples is on the larger end of the spectrum compared with other laws and policies that affect population mental health. In comparison, expansion of health insurance in Massachusetts was associated with a 1.5–percentage point decline in mental distress.41 Undocumented immigrants who became eligible for the Deferred Action for Childhood Arrivals program providing temporary work permits and preventing deportation in 2012 had a 48% reduction in the odds of reporting psychological distress after program implementation compared with immigrants who were not eligible for the program.42 Women who benefited from the expansion of the earned income tax credit antipoverty program in 1990 were 8.3% less likely to report being depressed compared with low-income women who did not meet eligibility criteria.43
A key strength of the study was that we took a difference-in-differences analytical approach that included state fixed effects, which controlled for all time-invariant state characteristics, including any policy differences that did not change during the study period. With the difference-in-differences approach, we focused on changes in mental distress in each state between 2014 and 2016 rather than on absolute differences in mental distress between states, which could have many causes.
Limitations
A limitation was that we could only conduct the analysis in states and years with data on sexual orientation; thus, we could not evaluate baseline trends in mental distress specifically among sexual minority adults prior to 2014 (though baseline trends did not differ in the full sample) or include all 5 states with laws permitting denial of services to same-sex couples. Though our study includes a diverse range of states, the findings might not be generalizable to states that did not collect data on sexual orientation. Including the CDC sexual orientation and gender identity module as part of the core BRFSS survey distributed to all states would improve the ability of researchers to study the causes and extent of health disparities affecting sexual and gender minorities. We also could not control for unmeasured state characteristics that may have changed during the study period, such as social support for sexual minorities. Finally, future research should examine the generalizability of our results to other measures of mental health, including diagnostic assessments of psychiatric morbidity.
Conclusions
Our findings indicate that laws permitting the denial of services to sexual minorities, which exist in 12 states and are under consideration by the US Supreme Court, are associated with a 46% increase in the proportion of sexual minority adults experiencing mental distress. Lawmakers and courts considering laws permitting denial of services to sexual minorities should consider the association between these laws and increases in the proportion of sexual minority adults experiencing mental distress.
eAppendix 1. BRFSS data source citations and disclaimers
eAppendix 2. Selection of control states
eTable 1. Population characteristics in Utah and control states
eTable 2. Population characteristics in Michigan and potential control states
eTable 3. Population characteristics in North Carolina and control states
eTable 4. Logistic regression analysis of prior trends in mental distress among all adults in states that passed laws permitting denial of services to same-sex couples and control states, 2012-2014
eTable 5. Change in percent of population experiencing mental distress after implementation of laws permitting denial of services to same-sex couples
eTable 6. Logistic regression analysis of state laws permitting denial of services to same-sex couples and mental distress
eTable 7. Change in percent of population experiencing mental distress after implementation of laws permitting denial of services to same-sex couples including those aged 65 and older
eTable 8. Change in percent of population experiencing mental distress after implementation of laws permitting denial of services to same-sex couples excluding those unsure of their sexual orientation
eTable 9. Change in percent of population experiencing mental distress after implementation of laws permitting denial of services to same-sex couples including same-sex marriage laws
eTable 10. Change in mentally unhealthy days after implementation of laws permitting denial of services to same-sex couples
eFigure. Changes in mental distress over time in states that did and did not pass laws permitting denial of services to same-sex couples, 2012-2014
References
- 1.Gonzales G, Henning-Smith C. Health disparities by sexual orientation: results and implications from the behavioral risk factor surveillance system. J Community Health. 2017;42(6):1163-1172. [DOI] [PubMed] [Google Scholar]
- 2.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802-813. [DOI] [PubMed] [Google Scholar]
- 3.Kiecolt-Glaser JK, Glaser R. Depression and immune function: central pathways to morbidity and mortality. J Psychosom Res. 2002;53(4):873-876. [DOI] [PubMed] [Google Scholar]
- 4.Chang H-J, Lin H-C, Lee H-C, Lin C-C, Pfeiffer S. Risk of mortality among depressed younger patients: a five-year follow-up study. J Affect Disord. 2009;113(3):255-262. [DOI] [PubMed] [Google Scholar]
- 5.Blazer DG, Hybels CF, Pieper CF. The association of depression and mortality in elderly persons: a case for multiple, independent pathways. J Gerontol A Biol Sci Med Sci. 2001;56(8):M505-M509. [DOI] [PubMed] [Google Scholar]
- 6.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;Spec No:80-94. [PubMed] [Google Scholar]
- 7.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813-821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363-385. [Google Scholar]
- 9.Duncan DT, Hatzenbuehler ML, Johnson RM. Neighborhood-level LGBT hate crimes and current illicit drug use among sexual minority youth. Drug Alcohol Depend. 2014;135:65-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hatzenbuehler ML, Birkett M, Van Wagenen A, Meyer IH. Protective school climates and reduced risk for suicide ideation in sexual minority youths. Am J Public Health. 2014;104(2):279-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123(1):346-352. [DOI] [PubMed] [Google Scholar]
- 12.Berlan ED, Corliss HL, Field AE, Goodman E, Austin SB. Sexual orientation and bullying among adolescents in the growing up today study. J Adolesc Health. 2010;46(4):366-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newcomb ME, Mustanski B. Internalized homophobia and internalizing mental health problems: a meta-analytic review. Clin Psychol Rev. 2010;30(8):1019-1029. [DOI] [PubMed] [Google Scholar]
- 14.Raifman J, Moscoe E, Austin SB, McConnell M. Difference-in-differences analysis of the association between state same-sex marriage policies and adolescent suicide attempts. JAMA Pediatr. 2017;171(4):350-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatzenbuehler ML, O’Cleirigh C, Grasso C, Mayer K, Safren S, Bradford J. Effect of same-sex marriage laws on health care use and expenditures in sexual minority men: a quasi-natural experiment. Am J Public Health. 2012;102(2):285-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hatzenbuehler ML. Structural stigma and the health of lesbian, gay, and bisexual populations. Curr Dir Psychol Sci. 2014;23:127-132. [Google Scholar]
- 17.Supreme Court of the United States Masterpiece Cakeshop v. Colorado Civil Rights Commission (Undecided); oral arguments. https://www.supremecourt.gov/qp/16-00111qp.pdf. Published December 5, 2017. Accessed March 9, 2018.
- 18.American Civil Liberties Union Anti-LGBT religious exemption legislation across the country. https://www.aclu.org/other/past-anti-lgbt-religious-exemption-legislation-across-country?redirect=anti-lgbt-religious-refusals-legislation-across-country.Accessed March 14, 2018.
- 19.Centers for Disease Control and Prevention The BRFSS data user guide 2013. https://www.cdc.gov/brfss/data_documentation/pdf/userguidejune2013.pdf. Published August 15, 2013. Accessed March 9, 2018.
- 20.Adams SJ, Christensen L Utah Senate Bill 297: protections for religious expression and beliefs about marriage, family, or sexuality. https://le.utah.gov/~2015/bills/static/SB0297.html. Published 2015. Accessed March 14, 2018.
- 21.LaFontaine A, Crawford K, McBroom E, et al. Enrolled House Bill 4188: an act to amend 1973 PA 116. http://www.legislature.mi.gov/documents/2015-2016/publicact/pdf/2015-PA-0053.pdf.Published 2015. Accessed March 14, 2018.
- 22.Berger P, Barefoot JC, Brock AC, et al. North Carolina Senate bill 2: an act to allow magistrates, assistant registers of deeds, and deputy registers of deeds to recuse themselves from performing duties related to marriage ceremonies due to sincerely held religious objection. https://www.ncleg.net/Sessions/2015/Bills/Senate/PDF/S2v4.pdf. Published 2015. Accessed March 14, 2018.
- 23.Bishop S, Howard S North Carolina House Bill 2: an act to provide for single-sex multiple occupancy bathroom and changing facilities in schools and public agencies and to create statewide consistency in regulation of employment and public accommodations. https://www.ncleg.net/gascripts/BillLookUp/BillLookUp.pl?Session=2015E2&BillID=h2. Published 2016. Accessed March 14, 2018.
- 24.Kruse D, Schneider S, Steele B Indiana Senate Bill 101: religious freedom restoration. https://iga.in.gov/legislative/2015/bills/senate/101. Published 2015. Accessed March 14, 2018.
- 25.Young M, Crider M Indiana Senate Bill 50: antidiscrimination safeguards. https://iga.in.gov/legislative/2015/bills/senate/50#digest-heading. Published 2015. Accessed March 14, 2018.
- 26.Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s healthy days measures—population tracking of perceived physical and mental health over time. Health Qual Life Outcomes. 2003;1:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health. 2003;57(5):339-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Toet J, Raat H, van Ameijden EJ. Validation of the Dutch version of the CDC core healthy days measures in a community sample. Qual Life Res. 2006;15(1):179-184. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1-3):163-173. [DOI] [PubMed] [Google Scholar]
- 30.Newschaffer CJ. Validation of Behavioral Risk Factor Surveillance System (BRFSS) HRQOL measures in a statewide sample. Atlanta, GA: Centers for Disease Control and Prevention; 1998. [Google Scholar]
- 31.Slabaugh SL, Shah M, Zack M, et al. Leveraging health-related quality of life in population health management: the case for healthy days. Popul Health Manag. 2017;20(1):13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reeves WC, Strine TW, Pratt LA, et al. ; Centers for Disease Control and Prevention (CDC) . Mental illness surveillance among adults in the United States. MMWR Suppl. 2011;60(3):1-29. [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC) Self-reported frequent mental distress among adults—United States, 1993-1996. MMWR Morb Mortal Wkly Rep. 1998;47(16):326-331. [PubMed] [Google Scholar]
- 34.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401-2402. [DOI] [PubMed] [Google Scholar]
- 35.Wooldridge J. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press, 2010. [Google Scholar]
- 36.Greene W. The behaviour of the maximum likelihood estimator of limited dependent variable models in the presence of fixed effects. Econom J. 2004;7:98-119. [Google Scholar]
- 37.Rokicki S, Cohen J, Fink G, Salomon JA, Landrum MB. Inference with difference-in-differences with a small number of groups: a review, simulation study, and empirical application using SHARE data. Med Care. 2018;56(1):97-105. [DOI] [PubMed] [Google Scholar]
- 38.Office of the Federal Register Protecting Statutory Conscience Rights in Health Care; Delegation of Authority. https://www.federalregister.gov/documents/2018/01/26/2018-01226/protecting-statutory-conscience-rights-in-health-care-delegations-of-authority. Published January 26, 2018. Accessed March 14, 2018.
- 39.Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: a prospective study. Am J Public Health. 2010;100(3):452-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chomsky D, Barclay S. The mass media, public opinion, and lesbian and gay rights. Annu Rev Law Soc Sci. 2010;6:387-403. [Google Scholar]
- 41.Van Der Wees PJ, Zaslavsky AM, Ayanian JZ. Improvements in health status after Massachusetts health care reform. Milbank Q. 2013;91(4):663-689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Venkataramani AS, Shah SJ, O’Brien R, Kawachi I, Tsai AC. Health consequences of the US Deferred Action for Childhood Arrivals (DACA) immigration programme: a quasi-experimental study. Lancet Public Health. 2017;2(4):e175-e181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boyd-Swan C, Herbst CM, Ifcher J, Zarghamee H. The earned income tax credit, mental health, and happiness. J Econ Behav Organ. 2016;126:18-38. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. BRFSS data source citations and disclaimers
eAppendix 2. Selection of control states
eTable 1. Population characteristics in Utah and control states
eTable 2. Population characteristics in Michigan and potential control states
eTable 3. Population characteristics in North Carolina and control states
eTable 4. Logistic regression analysis of prior trends in mental distress among all adults in states that passed laws permitting denial of services to same-sex couples and control states, 2012-2014
eTable 5. Change in percent of population experiencing mental distress after implementation of laws permitting denial of services to same-sex couples
eTable 6. Logistic regression analysis of state laws permitting denial of services to same-sex couples and mental distress
eTable 7. Change in percent of population experiencing mental distress after implementation of laws permitting denial of services to same-sex couples including those aged 65 and older
eTable 8. Change in percent of population experiencing mental distress after implementation of laws permitting denial of services to same-sex couples excluding those unsure of their sexual orientation
eTable 9. Change in percent of population experiencing mental distress after implementation of laws permitting denial of services to same-sex couples including same-sex marriage laws
eTable 10. Change in mentally unhealthy days after implementation of laws permitting denial of services to same-sex couples
eFigure. Changes in mental distress over time in states that did and did not pass laws permitting denial of services to same-sex couples, 2012-2014