Abstract
Background
Improving a patient’s experience with their care through an online interface for communication (an eHealth patient portal) has been shown to be beneficial in some studies of chronic disease populations. However, little is known about the effectiveness of an eHealth portal for delivery of care to home dialysis patients.
Objectives
Primary: To determine whether an eHealth portal is effective at improving a patient’s experience with their home dialysis care. Secondary: (1) To determine whether an eHealth portal improves health-related quality of life for home dialysis patients, (2) to assess patient satisfaction with an eHealth portal and perceived impact on aspects of their home dialysis therapy and health, (3) to determine the acceptability of the eHealth portal software, and (4) to determine the change in telephone usage for communication after patient adoption of an eHealth portal.
Design
Single-arm pilot trial with recruitment over a 4-month period.
Setting
The multidisciplinary home dialysis clinic in Halifax Nova Scotia Canada.
Patients
Adults (>18 years) receiving either home hemodialysis or peritoneal dialysis.
Measurements
Consumer quality index (CQI), health-related quality of life using the EuroQol Five Dimensions Questionnaire (EQ-5D), acceptability of the eHealth portal software (using the Acceptability E-scale), and satisfaction/perceived impact (using a modified questionnaire).
Methods
A web-based application (McKesson, Canada, RelayHealth®) allowed patients and health care workers to communicate through a secure, password-protected online portal that permitted visualization of the messaging history by patient and provider. Patients and the home dialysis health care team had the ability to send messages related to patient care at any time including proposed changes to medication, instructions after a clinic visit, times of new appointments, upcoming investigations, or questions about care. Patient experience with home dialysis care using the CQI, health-related quality of life using the EQ-5D, acceptability of the eHealth portal software, and satisfaction/perceived impact were assessed at baseline, 6, and 12 months of follow-up (where applicable). Total minutes of telephone communication was assessed prior to and after adoption of the portal.
Results
Of the 41 patients who consented to join the portal, 27 (66%) created an online account. At baseline, patients had a positive experience for the care and communication provided by their nephrologist (CQI: 3.63, 95% confidence interval [CI]: 3.50-3.76) and this did not change significantly over the study period. Similar results were observed for the care provided by other nephrology health care team members. Health-related quality of life using the EQ-5D score was 0.80 (interquartile range [IQR]: 0.71-0.83) at baseline and this also did not significantly change over the study period. Patients were satisfied with the eHealth portal (mean Likert scale score of 6.5 ± 0.6 in overall satisfaction, scale ranging from 1 completely dissatisfied to 10 completely satisfied), but only a minority (N = 12) completed a satisfaction questionnaire. Median monthly phone usage decreased from 12.5 to 10 minutes (P = .02) after adoption of the portal.
Limitations
The study is limited by the small sample size, high rate of patient dropout, and limited response rate.
Conclusions
In this study of home dialysis patients, we identified that an eHealth communication did not lead to significant improvements in patient experience with home dialysis care.
Trial Registration
ClinicalTrials.gov number NCT02128347
Keywords: consumer quality index, eHealth, telehealth, hemodialysis, peritoneal dialysis, information and communication technology, health-related quality of life, shared decision making, web-based portal
Abrégé
Contexte
Le recours à un outil de communication en ligne (un portail santé destiné aux patients) pour améliorer l’expérience des patients en regard de leurs soins s’est avéré bénéfique dans quelques études sur des populations de patients atteints de maladies chroniques. Cependant, on en sait peu sur l’efficacité d’un tel portail pour la prestation de soins aux patients dialysés à domicile.
Objectifs
Principal — Déterminer si un portail de santé en ligne se montre efficace pour améliorer l’expérience des patients en matière de soins de dialyse à domicile.
Secondaires — a. Déterminer si ce portail améliore la qualité de vie liée à la santé des patients dialysés à domicile; b. évaluer la satisfaction des patients à l’égard de l’outil en ligne et connaître son incidence sur certains aspects de leur santé générale et de leurs traitements; c. avoir une idée du niveau d’acceptation du logiciel du portail; d. évaluer les changements dans l’usage du téléphone comme outil de communication, une fois le portail en ligne adopté par le patient.
Type d’étude
Un essai pilote à un seul bras pour lequel le recrutement s’est étalé sur une période de quatre mois.
Cadre
La clinique multidisciplinaire de dialyse à domicile d’Halifax (Nouvelle-Écosse) au Canada.
Sujets
Des patients adultes recevant des traitements de dialyse à domicile (hémodialyse ou dialyse péritonéale).
Mesures
La qualité de l’expérience des patients à l’égard de leurs soins a été évaluée avec le Consumer Quality Index ou CQI (norme néerlandaise mesurant l’expérience des patients à l’égard des soins de santé). On a mesuré le score de qualité de vie liée à la santé à l’aide du questionnaire EQ-5D (EuroQol Five Dimensions Questionnaire); et l’acceptation du logiciel du portail de santé par l’entremise de l’AES (Acceptability E-scale). Enfin, la satisfaction des patients et l’incidence perçue sur la santé et les traitements ont été évaluées à l’aide d’un questionnaire modifié.
Méthodologie
Une application sur le Web (McKesson, Canada, RelayHealth®) a permis aux patients et aux professionnels de la santé de communiquer par le biais d’un portail en ligne sécurisé et protégé par un mot de passe. L’historique des messages envoyés par le patient et le fournisseur de soins était visible sur le portail. Les patients et les membres de l’équipe de soins avaient en tout temps la possibilité d’envoyer des messages liés aux soins du patient. Les messages concernaient notamment des changements proposés dans la médication, des instructions à la suite d’une visite en clinique, les dates et heures de rendez-vous, les enquêtes à venir ou des questions générales relatives aux soins. L’expérience du patient en regard de la dialyse à domicile, évaluée par le CQI; la qualité de vie liée à la santé, évaluée par le questionnaire EQ-5D; l’acceptation du logiciel, de même que la satisfaction générale et l’incidence perçue sur la santé et les traitements ont été mesurées au début de l’étude et après six mois et douze mois de suivi (lorsque possible). La durée des communications téléphoniques a été évaluée avant et après l’adoption du portail.
Résultats
Des 41 patients ayant accepté de joindre le portail, 27 (66 %) ont créé un compte en ligne. Au début de l’étude, les patients disaient avoir une expérience positive en regard des soins offerts et de la communication avec leur néphrologue (CQI : 3,63; IC 95 % : 3,50-3,76) et cette perception est demeurée sensiblement la même tout au long de l’étude. Des résultats similaires ont été observés pour les soins offerts par les autres membres de l’équipe de soins en néphrologie. Le score de la qualité de vie relative à la santé, mesuré par le questionnaire EQ-5D, était de 0,80 (ÉIQ : 0,71-0,83) au début de l’étude et n’a pas varié de façon significative au cours de la période de l’étude. De manière générale, les répondants se sont dits satisfaits du portail de santé en ligne, avec un score moyen de 6,5 ±0,6 sur l’échelle de Likert pour la satisfaction générale (échelle allant de 1, pour « pas du tout satisfait », à 10, pour « entièrement satisfait »). Par contre, seule une minorité de patients (n=12) a rempli le questionnaire évaluant la satisfaction. L’utilisation mensuelle médiane du téléphone pour les communications avait diminué à la suite de l’adoption du portail, passant de 12,5 minutes initialement, à 10 minutes après l’adoption.
Limites
Les constatations de cette étude sont limitées par le très faible échantillon de sujets, par le faible taux de réponse aux questionnaires et par le taux élevé d’abandon des patients.
Conclusion
Dans cette étude, menée auprès de patients dialysés à domicile, nous avons constaté que le recours à un outil de communication en ligne n’a pas amélioré de façon significative l’expérience des patients en matière de soins de dialyse à domicile.
What was known before
Improving patient experience with their home dialysis care has potential to improve health-related quality of life in these patients. Development of novel communication systems to better support home dialysis care may improve health outcomes.
What this adds
This study provided valuable information on the use of online communication portals for patients who are on either peritoneal dialysis or home hemodialysis. To our knowledge, this is one of the first studies in dialysis patients focusing on online communication strategies. We identified that an eHealth communication did not lead to significant improvements in patient experience with home dialysis care but has the potential to improve patient outcomes.
Introduction
Home dialysis, including peritoneal dialysis and home hemodialysis, has a number of potential benefits compared with in-center hemodialysis including lower health care costs and improved quality of life for patients.1-3 However, overall quality of life remains low compared with the general population.4,5 To address impairments in health-related quality of life (HRQOL), some recent efforts to improve patients’ experience with home dialysis care have been proposed and studied, particularly in the areas of shared decision making and handling of patient requests.6-8 Regarding patients’ experience with their care, peritoneal dialysis patients have identified that attentiveness to their concerns and clarity of recommendations are important aspects of communication that have traditionally been lacking.8 Improving patient experience with their home dialysis care has potential to improve quality of life in these patients.6
Acknowledging that there is potential for improvement in communication for home dialysis patients, the development of novel communication systems to better support home dialysis care while reducing the potential burden of telephone communication is crucial. The use of eHealth online portals that support online communication between patients and health care workers is increasing. An interface that allows patients to discuss treatment plans and address clinical problems while reducing the need for telephone communication has been evaluated in some studies.9-11 Such a system may improve patients’ experience with their care, reduce health service utilization, and potentially improve health outcomes.9-11 Thus far, the use of an eHealth online portal to facilitate communication and improve patients’ experience with their care has not been evaluated in home dialysis. The primary purpose of this study, in a sample of home dialysis patients, was to determine whether an eHealth portal improved patient experience with home dialysis care. Our secondary objectives were (1) to determine whether an eHealth patient portal improved HRQOL for home dialysis patients, (2) to assess patients’ satisfaction with an eHealth portal and perceived impact on aspects of their home dialysis therapy and health, (3) to determine the acceptability of the eHealth portal software, and (4) to determine the change in telephone usage for communication after patient adoption of an eHealth portal. We hypothesized that the eHealth portal would improve patient experience with care and HRQOL and that patients would be satisfied with the portal. We also hypothesized that telephone usage would decrease after patient adoption of the eHealth portal.
Methods
Study Design and Participants
The study was approved by the Nova Scotia Health Research Ethics Board, registered as a clinical trial (ClinicalTrials.gov no.: NCT02128347) and was conducted among home dialysis (peritoneal and home hemodialysis patients) affiliated with the Nova Scotia Health Authority (NSHA) Central Zone Renal Program. Overall, the NSHA Central Zone Renal Program provided care to approximately 450 prevalent dialysis patients (in-center and home dialysis) and 80 home dialysis patients during 2014-2015.
The multidisciplinary home dialysis clinic is staffed with nephrologists, nurses, pharmacists, dieticians, and social workers caring for peritoneal dialysis and home hemodialysis patients.
We conducted a single-arm pilot trial among patients receiving either home hemodialysis or peritoneal dialysis. Patients were recruited over a 4-month period (October 2014-January 2015). This time frame was chosen to ensure all patients primarily followed by our dialysis program would have one scheduled clinic visit within this time frame to allow an opportunity to be introduced to the study. Patients were enrolled if they had been receiving dialysis for 3 or more months prior to the start of the study. Patients were excluded from study participation if they did not provide consent or did not have access to a computer with an Internet connection. Participants were followed for 1 year and instructed to use the portal for the entire year. Assessments were performed at baseline, at 6 months, and at 12 months. Participant demographics, laboratory data, clinical data, need for assistance, phone usage, distance traveled to the home dialysis unit, and dialysis vintage were collected at baseline.
Standard of Care
The current standard at our center is that patients receiving home dialysis use telephone communication for urgent and nonurgent home dialysis issues. Patients have access to telephone nursing support (for emergency and routine care) between 7:30 a.m. and 3:30 p.m. After-hours on-call nursing support is provided for emergency issues. During working hours, patient queries are discussed over the phone with an on-call dialysis nurse and documented in the patient chart. Any medical issues are discussed with the on-call physician. Physician-directed changes to care are verbally communicated to patients over the phone by home dialysis nurses. Dates and times for appointments or investigations are also verbally communicated. All telephone calls with patients in the home unit are tracked with a start and end time to capture telephone usage. Therefore, this information is routinely collected as standard of care for home dialysis patients.
Intervention
Patients evaluated through the clinic were given the option of accepting an electronic invitation to join an online eHealth patient portal (McKesson Canada, RelayHealth®). This web-based application allows patients and health care workers to communicate through a secure, password-protected online portal and permits visualization of the messaging history by patient and provider. Specialty nurses underwent training for the portal. After joining the portal, patients and the home dialysis health care team, which included nurses, a home dialysis physician, and dieticians, had the ability to send messages related to patient care at any time. Messages could be sent between the health care team and patient including proposed changes to medication, instructions after a clinic visit, times of new appointments, upcoming investigations, or questions about care. Messages were electronically stored within the portal and printed and placed in the patient hospital chart to comply with hospital legal standards. The patient and health care team could also directly view electronic patient records. Both patients and the health care team were made aware of new messages through email prompt. Patients were informed not to send messages pertaining to medical emergencies (which were reserved for telephone communication as per the regular standard of care) and were made aware that messages sent after hours or on weekend days would not be addressed until the following business day.
Outcome Measures
The primary outcome of this study was change in patient experience with home dialysis care at 12 months after initiating the eHealth portal using the consumer quality index (CQI). This is a Dutch-based questionnaire by van der Veer et al6 that is comprised of a set of items and answering categories that measure a patient’s experience with home dialysis care combined with an assessment of the priority of each item. The questionnaire was translated to English using validated methodology.12 CQI assessments were performed at baseline, 6 months, and 12 months. The CQI is calculated by multiplying the proportion of respondents who rated an item as being “always” in the patient experience questionnaire, which assessed the item’s priority. The proportion of respondents who reported a suboptimal experience for that aspect of care (ie, by answering “never” or “sometimes”) was used to identify areas of improvement. The top 10 items that had the highest priority at baseline were compared at 12 months to determine whether CQI improved. Domains of interest included nephrologists’ care and communication, nurses’ care and communication, and dieticians’ care and communication. Each item was measured using a 4-point Likert response scale with 1 = not important, 2 = of some importance, 3 = important, and 4 = extremely important.
Secondary outcomes included the following:
HRQOL was measured using the EuroQol Five Dimensions Questionnaire (EQ-5D) which has been previously used to assess HRQOL in patients on chronic dialysis.13 We reported EQ-5D data using population preference-weighted health index score based on the descriptive responses as well as patient’s self-reported assessment of health status through visual analogue scale (EQ-VAS).14 The EQ-5D is an index score between 0 and 1.0 where 5 dimensions of health are assessed based on patient self-report: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The EQ-5D was given to patients at baseline, 6 months, and at 12 months. The EQ-VAS is a value between 0 and 100 where 100 is perfect health. Patients self-reported these values at baseline, 6 months, and at 12 months.
Acceptability of the eHealth portal software was assessed using the validated Acceptability E-Scale.15 This was an 8-item questionnaire that asked about patients’ perception of the communication portal platform including their average time spent on the online portal system. For 6 of the 8 items, a 5-point Likert scale was used with 1 = very unhelpful/dissatisfied, 3 = neutral response, and 5 = very acceptable/satisfied. The last 2 items of the scale were a quantitative measure of time spent on the portal.
A separate 15-item questionnaire was used to measure overall patient satisfaction and the impact of the RelayHealth® portal in addressing aspects of a patients’ health and dialysis therapy. This questionnaire was modeled after a similar questionnaire used in a recent study of home dialysis patients.16 These were assessed at 6 months and 12 months.
Total phone usage was compared for the time before joining the portal (up to a maximum of 6 months) and after adoption of the portal (for the 6 months).
A diagram showing the timeline of questionnaires are shown in Supplementary File 1. Importantly, all 3 tools measured different aspects of care to allow a more complete overview of the effectiveness of the portal. The CQI focused on patient experience as an established indicator of quality of care and aimed to address whether communication and care provided by nephrologists, nurses, and dieticians was improved after implementation of the eHealth portal. The Acceptability E Scale addressed the RelayHealth® technology itself, to ensure any lack of benefit was not the result of the design/operation of the electronic platform. Finally, the satisfaction questionnaire addressed overall satisfaction and perceived impact of the portal on multiple factors including their health, stress, mood, and management of their dialysis or kidney disease. All questionnaires used for this study were filled in person and can be found in Supplemental File 1. A timeline for assessment of study participants at baseline, 6 months, and 12 months is shown in Figure A of Supplemental File 2.
Baseline Characteristics
Patient demographics collected at baseline included age, sex, body mass index (BMI), current smoker, history of hypertension, diabetes, coronary artery disease, congestive heart failure, cerebrovascular disease, peripheral vascular disease, previous failed kidney transplant, and/or history of cancer. Patient use of information and communication technologies (ICTs) was also assessed using a modified questionnaire.17
Data Analysis
The primary purpose of this pilot study was to determine patient experience with home dialysis care after adoption of an eHealth portal and to gather important secondary outcomes that would better inform the design of a randomized controlled trial; therefore, a convenience sample of all home dialysis patients prospectively assessed over a 4-month period was chosen. Baseline characteristics of the study cohort were assessed using means and standard deviations for continuous normally distributed data, medians and interquartile range (IQR) for nonnormally distributed data, and proportions for categorical data. Comparative statistics using paired t tests for normally distributed data and Wilcoxon signed-rank tests were used to assess changes in CQI and QOL among the patients who joined the portal. A P value <.05 was considered statistically significant. Changes were reported for each individual item of CQI, QOL as measured by the EQ-5D, acceptability, and satisfaction over the study time period. Median monthly phone usage in minutes was compared pre-post intervention using the Wilcoxon signed-rank test. Comparative analysis of baseline demographics and QOL was performed post hoc as a sizeable number of patients consented to participate in the study but did not join the portal. All statistical analyses were performed using STATA 13.1 statistics package.18
Results
Study Participants and Baseline Characteristics
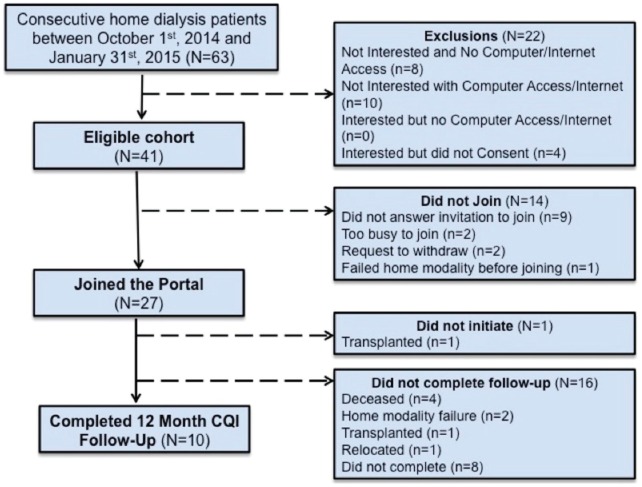
There were 63 patients who were approached for the study, of whom 41 patients provided consent. Of these patients, 27 (66%) created an online account and joined the portal. At 6 months, 16 patients had completed follow-up, and at 12 months, 10 patients had completed follow-up for our primary outcome (Figure 1). Participant characteristics are shown in Table 1 (Demographics of participants who consented but did not join the portal are available in Supplementary File 2, Table A).
Figure 1.
Flow diagram of patient approached to participate in the study.
Note. CQI = consumer quality index.
Table 1.
Demographics of Patients Who Joined the Online Portal.
| Variable | Study group, n = 27 |
|---|---|
| Mean age, y | 57.1 ± 1.9 |
| Female, n (%) | 13 (48) |
| Mean body mass index, m/kg2 | 32.8 ± 2.2 |
| Hypertension, n (%) | 23 (85) |
| Coronary artery disease, n (%) | 6 (22) |
| Cerebrovascular disease, n (%) | 1 (4) |
| Peripheral vascular disease, n (%) | 4 (15) |
| Diabetes, n (%) | 12 (44) |
| Failed kidney transplant, n (%) | 6 (22) |
| Home hemodialysis, n (%) | 10 (37) |
| Congestive heart failure, n (%) | 3 (11) |
| Smoker, n (%) | 4 (15) |
| Median distance to home dialysis unit (km) | 81 (IQR: 13-131) |
| Median time to home dialysis unit (min) | 70 (IQR: 22-110) |
Note. IQR = interquartile range.
Twenty-one (51%) of patients reported their technology use in the 6 months prior to joining the study (Supplementary File 2, Table B and C). More than half (52.4%) used text messaging or short message service (SMS). The majority of patients used email (62%) with 28.6% having used email both on desktop computers and on handheld devices. Most patients (85%) who responded to the ICT questionnaire indicated that they had interacted with health care staff via telephone in the 2 months prior to enrollment. Over 90% of patients interacted with health care professionals less than 3 times per month.
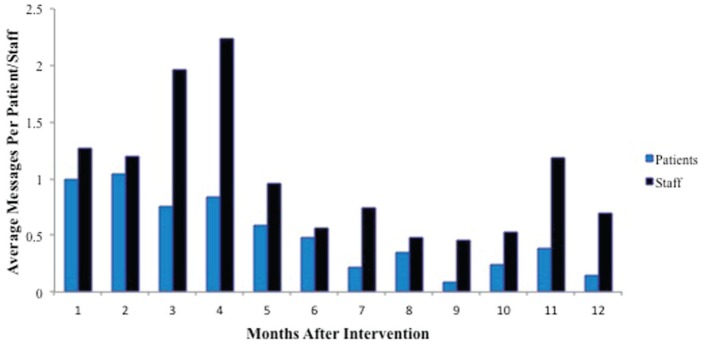
Utilization of the eHealth Portal
Staff and patient messaging frequency (messages/month) is shown in Figure 2. Staff and health care providers consistently used the portal more often than patients (Figure 2). Most messages that were sent pertained to health-related concerns (25%), followed by medication-related questions (17%) and questions about test results (10%) (Figure 3). No messages were sent for emergency issues that required re-direction to telephone or that resulted in patient harm due to delay.
Figure 2.
Histogram showing frequency of messaging by patients and staff over the study period.
Figure 3.
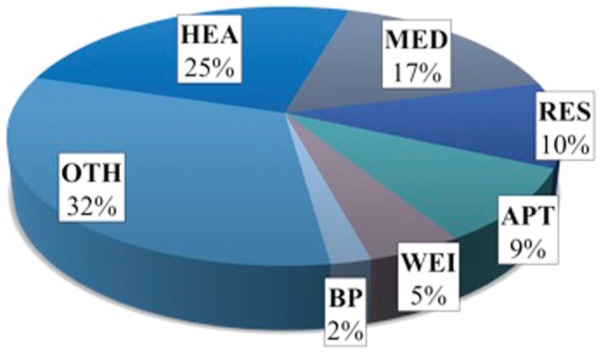
Proportion of types of messages sent by patients.
Note. No messages were sent for access/nonaccess infections, supplies, or emergencies. HEA = health; med = medication; RES = test result; OTH = other; APT = appointment; WEI = weight adjustment, BP = blood pressure.
Change in Patient Experience With Home Dialysis Care
At baseline, 31 of 41 patients (76%) filled out the CQI questionnaire in 3 health care domains (nephrologists, nurses, and dieticians). Mean CQI for the sample is shown in Supplementary File 2, Table D. Table 2 shows the mean CQI scores at baseline, 6 months, and 12 months of follow-up. In the nephrologists’ care and communication domain, overall CQI did not significantly differ at the end of the study in comparison with baseline (P = .33). This remained true for nursing and dietician domains. Sample size was limited in the social work domain with about half of the respondents indicating social work was not applicable to them at each interval of assessment.
Table 2.
Consumer Quality Index in 3 Domains of Care (Nephrology, Nursing, and Dieticians) for Patients Who Used the Online Portal System (Where 1 = Never, 2 = Sometimes, 3 = Usually, and 4 = Always).
| Score at baseline, n = 25 | Score at 6 months, n = 16 | Score at 12 months, n = 10 | |
|---|---|---|---|
| Nephrologists’ care and communication | 3.63 (3.50, 3.76) | 3.55 (3.39, 3.70)a | 3.41 (2.97, 3.84)a |
| Nephrologist explained things clearly | 3.60 (3.39, 3.81) | 3.63 (3.36, 3.89) | 3.50 (3.12, 3.88) |
| Nephrologist provided information to enable shared decision making | 3.28 (2.98, 3.58) | 3.31 (2.94, 3.69) | 3.20 (2.54, 3.86) |
| Nephrologist listened attentively | 3.52 (3.31, 3.73) | 3.50 (3.22, 3.78) | 3.40 (2.90, 3.90) |
| Nephrologist took concerns seriously | 3.56 (3.35, 3.77) | 3.50 (3.22, 3.78) | 3.60 (3.23, 3.97) |
| Nephrologist was respectful | 3.84 (3.64, 4.00) | 3.94 (3.80, 4.00) | 3.80 (3.49, 4.00) |
| Nephrologist spent enough time with patient | 3.42 (3.17, 3.66) | 3.56 (3.29, 3.84) | 3.30 (2.82, 3.78) |
| Nephrologist involves patient in decision making | 3.32 (3.04, 3.60) | 3.38 (2.99, 3.76) | 3.20 (2.64, 3.76) |
| Nephrologist asks about medication use | 3.71 (3.48, 3.94) | 3.69 (3.37, 4.00) | 3.60 (3.10, 4.00) |
| Nephrologist spends enough time on physical complaints | 3.35 (3.08, 3.62) | 3.40 (3.05, 3.75) | 2.88 (2.05, 3.70) |
| Nurses’ care and communication | 3.60 (3.40, 3.80) | 3.69 (3.41, 3.96)a | 3.55 (3.23, 3.86)a |
| Nurses explained things clearly | 3.64 (3.41, 3.87) | 3.69 (3.43, 3.94) | 3.56 (3.23, 3.90) |
| Being taken seriously by nurses | 3.56 (3.32, 3.80) | 3.69 (3.37, 4.00) | 3.62 (3.36, 3.89) |
| Dieticians’ care and communication | 3.59 (3.38, 3.80) | 3.79 (3.60, 3.98)a | 3.80 (3.54, 4.00)a |
| Dietician explaining things clearly | 3.72 (3.50, 3.94) | 3.93 (3.79, 4.00) | 3.90 (3.67, 4.00) |
| Providing information on recommended diet | 3.32 (3.01, 3.63) | 3.73 (3.48, 3.99) | 3.56 (2.99, 4.00) |
| Taken seriously by dietician | 3.72 (3.50, 3.94) | 3.92 (3.73, 4.00) | 3.90 (3.67, 4.00) |
No significant difference compared with baseline.
Change in HRQOL
There were no statistically significant differences in baseline HRQOL scores for those who participated in the portal and those who did not. At baseline, 24 patients had completed EQ-VAS and ED-5Q with 16 patients completing them at 12 months. HRQOL scores at baseline, 6 months, and 12 months are shown in Table 3.
Table 3.
EQ-5D and EQ-VAS at Baseline, 6 Months, and 12 Months.
| Online portal group | |
|---|---|
| EQ-VAS Baseline n = 24 |
70 (IQR: 55-80) |
| EQ-VAS 6 months n = 17 |
60 (IQR: 50-80) |
| EQ-VAS 12 months n = 16 |
70 (IQR: 60-80) |
| ED-5Q Baseline n = 24 |
0.81 (IQR: 0.71-0.85) |
| ED-5Q 6 months n = 16 |
0.78 (IQR: 0.59-0.83) |
| ED-5Q 12 months n = 16 |
0.80 (IQR: 0.45-0.85) |
Note. EQ-5D = EuroQol Five Dimensions Questionnaire; EQ-VAS = EuroQol-visual analogue scale; IQR = interquartile range.
Acceptability of the eHealth Portal Software
Perception of acceptability of the communication portal among participants is shown in Table 4. Response rate at 6 months was low for 11 participants (41%). Respondents found the online portal easy to use with a median response of 4 (IQR: 4-5). Overall satisfaction with the online portal was also high with a median response of 4 (IQR: 4-5). Average time spent sending messages on the portal was 4.8 ± 2.0 minutes per day at 6 months. Average time spent checking messages on the portal was 3.1 ± 1.1 minutes per day at 6 months. At 12 months, 5 (19%) of the online participants responded to the Acceptability E-scale. Those who responded continued to find the portal easy to use and were very satisfied with portal (median response of 5 IQR: 5-5).
Table 4.
Acceptability E-Scale at 6 Months for Patients Who Used the Online Portal System (Where 1 = Very Difficult/Unhelpful/ Unenjoyable and 5 = Very Easy/Helpful) (n = 11).
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| How easy was this communication portal for you to use? | — | — | 2 (18.2%) | 4 (36.4%) | 5 (45.5%) |
| How understandable were the responses you received to your portal messages? | — | — | — | 6 (54.6%) | 5 (45.5%) |
| How much did you enjoy using this communication portal? | 1 (9.1%) | — | 2 (18.2%) | 2 (18.2%) | 6 (22.2%) |
| How helpful was this communication portal in describing your symptoms and quality of life? | — | 1 (9.1%) | 3 (27.3%) | 4 (36.4%) | 3 (27.3%) |
| Was the amount of time it took to complete messages using this communication portal acceptable? | — | — | 2 (18.2%) | 4 (36.4%) | 5 (45.5%) |
| How would you rate your overall satisfaction with this communication portal? | — | — | 2 (18.2%) | 4 (36.4%) | 5 (45.5%) |
Satisfaction With Care After Adoption of the eHealth Portal
Satisfaction questionnaires were given at 6 months with 12 (44%) participants completing them. Of these patients, most were satisfied with a mean score of 6.5 ± 0.6 in overall satisfaction. The portal was not perceived by participants to have any negative impact on their care (Table 5). The majority of patients believed that the online portal had a positive impact on access to a kidney specialist (6.6 ± 0.6).
Table 5.
Satisfaction Questionnaire at 6 Months (Visual Analogue Scale Where 1 = Very Negative Impact, 5 = No Impact, and 10 = Very Positive Impact (n = 12).
| Impact of the portal on | M | SE |
|---|---|---|
| Overall Satisfaction | 6.5 | 0.6 |
| Chance of needing readmission to the hospital | 5.6 | 0.4 |
| Overall Health | 5.5 | 0.4 |
| Understanding of medications and dosing | 6.1 | 0.5 |
| Technical aspects of dialysis | 6 | 0.6 |
| Getting appointments with specialist doctors | 6 | 0.6 |
| Getting access to kidney specialist | 6.6 | 0.6 |
| Minimizing time spent managing your medical conditions | 5.9 | 0.5 |
| Personal privacy | 6.2 | 0.5 |
| Time spent traveling to get dialysis related-care | 5.4 | 0.4 |
| Stress related to performing home dialysis | 6.3 | 0.6 |
| Personal independence | 6.4 | 0.6 |
| Personal finances | 5.4 | 0.4 |
| Mood | 6.2 | 0.6 |
Change in Telephone Usage
Phone usage before and after joining the online portal was available for 23 (85.2%) participants. Median monthly phone usage prior to the online portal was 12.5 minutes per month (IQR: 4.2-26.7 minutes) and median monthly phone usage after 6 months was 10 minutes per month (IQR: 0-15 minutes), which was a statistically significant difference, P = .02.
Discussion
Principal Results
In this study, we found that communication using an online eHealth portal did not lead to an improvement in patient experience with care or HRQOL. Patients used the eHealth portal as designed using online messages for nonemergent health-related concerns. Among the small sample of patients who completed acceptability and satisfaction questionnaires, patients found the portal easy to use and were satisfied with the portal. The portal was found to have a neutral or mildly positive impact on patient management of several domains of their dialysis care (including reductions in stress, improved understanding of medications, increased personal independence, and access to a kidney specialist). Finally, there was a small but statistically significant reduction in patient telephone usage after adoption of the eHealth portal.
The use of online messaging to improve care between patients and health care providers in other areas of medicine has been increasing19 and online portals for patients to help manage their disease has been met with enthusiasm.20 ICT has been shown to improve self-management and satisfaction of care in various settings, with evidence of improved health outcomes in chronic disease populations.21-23 More recently, ICT has spread to the dialysis population with the advent of online self-management support tools and advances in telemedicine technologies.24-26
Although ICT has been shown to be beneficial in previous studies, we did not identify an improvement in patient experience with home dialysis care or HRQOL for patients who joined the RelayHealth® eHealth portal. This may be due to a number of factors. Although 65% of patients consented to participating in the study, only 66% of those who consented subsequently joined the portal. Furthermore, average monthly per-patient messaging frequency did not exceed 1/month. This suggests that the portal was not frequently used and, thus, may not have had a large impact on patient experience with care or HRQOL. What are the reasons for limited use? For the purposes of this study, prevalent and not incident patients were used for the target population. Patients newly initiating home dialysis are at high risk of experiencing gaps in care and interventions to improve communication are potentially best used at these vulnerable times.27 Due to the importance of needing a baseline patient experience with home dialysis care to assess improvement after initiating the portal, our study was structured to only include prevalent patients who were established on home dialysis. Many of these patients may have been well connected to the health care team and less likely to use or benefit from a change in communication. In support of this notion was the observation that 90% of ICT respondents interacted with the home dialysis team less than 3 times/month. Another contrasting reason for nonuse may be the complexity of care surrounding home dialysis. Asynchronous messaging is best reserved for less-urgent concerns and it is possible that patients perceived many of their health issues as ones that were better reserved for telephone communication. Although the number of minutes of telephone communication was significantly lower for patients after adoption of the portal, the magnitude of the difference was small (median of 12.5 vs 10 minutes for baseline vs follow-up). This suggests that patients continued to use telephone communication even after adopting the portal, and this would be expected if most of their calls were for urgent issues. Another explanation for the lack of benefit is that similar to a previous study of dialysis patients in the Netherlands,6 most of our patients had a positive experience with the care being provided at baseline. This suggests that there was little room to improve patient experience with care to a higher level. With respect to HRQOL, we elected to use a simple measure with little questionnaire burden, namely, the EQ-5D. However, it is possible that the eHealth portal did not have enough of an impact to affect generic HRQOL. It would appear that our sample had a high self-reported HRQOL at baseline and therefore we may not have been able to see a significant change. Compared with other studies, the baseline HRQOL with our measures are similar.28-30 Inclusion of kidney-specific HRQOL measures such as the Kidney Disease Quality of Life (KDQOL) may have led to different results. Home dialysis patient quality of life has historically been low,31 as was demonstrated in our study. Improving quality of life in home dialysis patients may require more than one tool, rather a multifactorial intervention before benefit is observed.32 Finally, one could surmise that our largely older population may have had less benefit from online communication compared with a younger population that is more likely to have and adopt technology. However, this was not evident in our study; those who did participate in the study were frequent users of technology including email and text/SMS messaging services. However, it is possible that use of ICT and subsequent patient experience would have been improved if a predominantly younger population were used. In addition, staff and health care providers use of the portal exceeded patient use throughout the study. This could potentially be explained through the loss to follow-up where staff were still contacting patients but the participants in the study stopped using the portal.
Although there was no significant improvement in our primary outcome or HRQOL, the portal was perceived by patients to have a mild positive impact on overall satisfaction and getting access to a kidney specialist (Likert scale of ⩾6.5, with 5 being neutral). Although this may suggest that online communication using an eHealth portal is beneficial for some patients, the results must be interpreted with caution as only 12 patients (44%) completed a satisfaction questionnaire. It is possible that perceived satisfaction may have been even lower if a larger sample of participants completed questionnaires at the end of follow-up.
Despite growing interest in ICT among dialysis patients and providers, the results of this study would suggest that an eHealth portal does not have a considerable positive impact on care and communication with home dialysis patients. Although we acknowledge that larger trials need be considered to truly determine whether there is benefit, the results of this study would suggest that RCTs of eHealth communication portals among home dialysis patients may be difficult to design for a number of reasons. Finding appropriate measures that accurately capture all aspects of home dialysis care without being too cumbersome are crucial. Although we attempted to use multiple surveys to ascertain the effect of an eHealth portal, some of the individual items of each survey (ie, item “nephrologist listens attentively” of the CQI) may not have applied to our study. An additional factor to consider in this patient population in particular is the high rate of attrition in dialysis patients; these patients often become acutely ill and have a high mortality compared with other patient groups. Knowing this, appropriate methodology to allow proper evaluation of data gleaned from these intervention studies needs to be carefully considered in future studies.
This study provided valuable information on the use of our online communication portal in patients who are on either peritoneal or home dialysis. To our knowledge, this is one of the first studies in dialysis patients focusing on online communication strategies. Our study sample was a reasonable representation of peritoneal dialysis patients and the intervention itself was practical and easy to implement as the majority of patients were already using ICT in their personal lives. The eHealth patient portal did not present our patients with any health education for self-care. However, this is one avenue for future patient portals and personalized health information targeted to the specific patient. There remains a paucity of literature of smartphone-based applications for CKD patients but one study provides strong rationale for a potential benefit.33
Limitations
Our study is limited by the small sample size and high rate of patient dropout. Many patients were lost to follow-up due to worsening health (by virtue of being on dialysis) or treatment failure. The limited sample size prevents us from making firm conclusions about the benefits or lack thereof with regard to the portal. Even among participants who were not lost to follow-up, there was the perception of a questionnaire burden evidenced by a limited response rate. Although each questionnaire itself was not burdensome, the combination of all questionnaires may have been too difficult and cumbersome for patients to complete. We did not have qualitative data on staff experiences or the time spent by staff in using the portal. Therefore, this analysis only takes into account the patient perspective. We are unable to comment on the patient population that consented to join the study but did not join the online portal outside of baseline characteristics. It would have been beneficial to determine why this group did not join the portal. This study was a single-arm trial and was not designed as a randomized control trial. Therefore, any observed change could have been the result of changes in care delivery that would have similarly applied to patients who did and did not join the portal. Although a randomized controlled trial would have been ideal, the limited sample size and response rate would have resulted in an even smaller sample size for evaluation of the portal. We were unable to describe differences in other metrics of health care utilization such as hospitalization rates, but this will be the target for future publication.
Conclusion
In this study of home dialysis patients, use of an online portal did not improve patient experience with home dialysis care or HRQOL. A larger, multicenter trial is needed to more rigorously evaluate the utility and feasibility of online communication portals for home dialysis patients.
Supplemental Material
Supplemental material, SupplementaryFile1_(1) for Effectiveness of a Web-Based eHealth Portal for Delivery of Care to Home Dialysis Patients: A Single-Arm Pilot Study by James Kiberd, Usman Khan, Cynthia Stockman, Arun Radhakrishnan, Matthew Phillips, Bryce A. Kiberd, Kenneth A. West, Steven Soroka, Christopher Chan and Karthik K. Tennankore in Canadian Journal of Kidney Health and Disease
Supplemental Material
Supplemental material, SupplementaryFile2_Version2 for Effectiveness of a Web-Based eHealth Portal for Delivery of Care to Home Dialysis Patients: A Single-Arm Pilot Study by James Kiberd, Usman Khan, Cynthia Stockman, Arun Radhakrishnan, Matthew Phillips, Bryce A. Kiberd, Kenneth A. West, Steven Soroka, Christopher Chan and Karthik K. Tennankore in Canadian Journal of Kidney Health and Disease
Acknowledgments
The authors thank McKesson Canada for their support and web-based application.
Footnotes
Ethics Approval and Consent to Participate: Nova Scotia Health Authority Research Ethics Board. Ethics Approval No.: #1016493.
Consent for Publication: Consent for publication was acquired by the lead authors for each tool.
Availability of Data and Materials: Materials available on request from the PI.
Author Contributions: Tennankore devised the idea. All authors were involved in the design of study. Khan and Tennankore collected data for the study. Kiberd and Tennankore contributed to the analysis. Kiberd wrote the first draft of the article. All authors reviewed the final version of the article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The results of this study were supported by a Nova Scotia Health Authority “Translating Research Into Care Grant.”
ORCID iD: James Kiberd  https://orcid.org/0000-0002-8048-779X
https://orcid.org/0000-0002-8048-779X
Supplemental Material: Supplemental material is available for this article online.
References
- 1. Lee H, Manns B, Taub K, et al. Cost analysis of ongoing care of patients with end-stage renal disease: the impact of dialysis modality and dialysis access. Am J Kidney Dis. 2002;40(3):611-622. [DOI] [PubMed] [Google Scholar]
- 2. Culleton B, Walsh M, Quinn R, Donnelly S, Friedrich M, Kumar A. Effect of frequent nocturnal hemodialysis vs conventional hemodialysis. J Am Med Assoc. 2007;298(11):1291-1299. [DOI] [PubMed] [Google Scholar]
- 3. Kutner NG, Zhang R, Barnhart H, Collins AJ. Health status and quality of life reported by incident patients after 1 year on haemodialysis or peritoneal dialysis. Nephrol Dial Transplant. 2005;20(10):2159-2167. [DOI] [PubMed] [Google Scholar]
- 4. Cameron JI, Whiteside C, Katz J, Devins GM. Differences in quality of life across renal replacement therapies: a meta-analytic comparison. Am J Kidney Dis. 2000;35(4):629-637. [DOI] [PubMed] [Google Scholar]
- 5. Merkus MP, Jager KJ, Dekker FW, Boeschoten EW, Stevens P, Krediet RT. Quality of life in patients on chronic dialysis: self-assessment 3 months after the start of treatment. The Necosad Study Group. Am J Kidney Dis. 1997;29(4):584-592. [DOI] [PubMed] [Google Scholar]
- 6. Van Der Veer SN, Jager KJ, Visserman E, et al. Development and validation of the Consumer Quality index instrument to measure the experience and priority of chronic dialysis patients. Nephrol Dial Transplant. 2012;27(8):3284-3291. [DOI] [PubMed] [Google Scholar]
- 7. Rubin HR, Fink NE, Plantinga LC, Sadler JH, Kliger AS, Powe NR. Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. JAMA. 2004;291(6):697-703. [DOI] [PubMed] [Google Scholar]
- 8. Wuerth DB, Finkelstein SH, Kliger AS, Finkelstein FO. Patient assessment of quality of care in a chronic peritoneal dialysis facility. Am J Kidney Dis. 2000;35(4):638-643. [DOI] [PubMed] [Google Scholar]
- 9. Zhou YY, Garrido T, Chin HL, Wiesenthal AM, Liang LL. Patient access to an electronic health record with secure messaging: impact on primary care utilization. Am J Manag Care. 2007;13(7):418-424. [PubMed] [Google Scholar]
- 10. Liederman EM, Lee JC, Baquero VH, Seites PG. Patient-physician web messaging: the impact on message volume and satisfaction. J Gen Intern Med. 2005;20(1):52-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Reed M, Huang J, Brand R, et al. Implementation of an outpatient electronic health record and emergency department visits, hospitalizations, and office visits among patients with diabetes. JAMA. 2013;310(10):1060-1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fransen MP, Van Schaik TM, Twickler TB, Essink-Bot ML. Applicability of internationally available health literacy measures in the Netherlands. J Health Commun. 2011;16:134-149. [DOI] [PubMed] [Google Scholar]
- 13. Wasserfallen JB, Halabi G, Saudan P, Perneger T, Feldman HI, Martin PY, Wauters JP. Quality of life on chronic dialysis: comparison between haemodialysis and peritoneal dialysis. Nephrol Dial Transpl. 2004;19(6):1594-1599. [DOI] [PubMed] [Google Scholar]
- 14. Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. 2005;43(3):203-220. [DOI] [PubMed] [Google Scholar]
- 15. Tariman JD, Berry DL, Halpenny B, Wolpin S, Schepp K. Validation and testing of the Acceptability E-scale for Web- based patient-reported outcomes in cancer care. Appl Nurs Res. 2012;24(1):53-58. doi: 10.1016/j.apnr.2009.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schachter ME, Bargman JM, Copland M, et al. Rationale for a home dialysis virtual ward: design and implementation. BMC Nephrol. 2014;15(33):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Radhakrishnan AK. The Use of Information and Communication Technologies for Knowledge Translation in a Mentoring Network of Physicians to Optimize Roles in the management of Chronic Pain [dissertation]. University of Toronto, Ontario, Canada; 2013. [Google Scholar]
- 18. StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- 19. Free C, Phillips G, Watson L, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med. 2013;10(1):e1001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zarcadoolas C, Vaughon WL, Czaja SJ, Levy J, Rockoff ML. Consumers’ perceptions of patient-accessible electronic medical records. J Med Internet Res. 2013;15(8):e168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lamprinos I, Demski H, Mantwill S, Kabak Y, Hildebrand C, Ploessnig M. Modular ICT-based patient empowerment framework for self-management of diabetes: design perspectives and validation results. Int J Med Inform. 2016;91:31-43. [DOI] [PubMed] [Google Scholar]
- 22. Petullo B, Noble B, Dungan KM. Effect of electronic messaging on glucose control and hospital admissions among patients with diabetes. Diabetes Technol Ther. 2016;18(9):555-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shimada SL, Allison JJ, Rosen AK, Feng H, Houston T. Sustained use of patient portal features and improvements in diabetes physiological measures. J Med Internet Res. 2016;18(7):e179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Whitten P, Buis L. Use of telemedicine for haemodialysis: perceptions of patients and health-care providers, and clinical effects. J Telemed Telecare. 2008;14(2):75-78. [DOI] [PubMed] [Google Scholar]
- 25. Krishna VN, Managadi K, Smith M, Wallace E. Telehealth in the delivery of home dialysis care: catching up with technology. Adv Chronic Kidney Dis. 2017;24(1):12-16. doi: 10.1053/j.ackd.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 26. Hayashi A, Yamaguchi S, Waki K, et al. Testing the feasibility and usability of a novel smartphone-based self-management support system for dialysis patients: a pilot study. JMIR Res Protoc. 2017;6(4):e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Raphael MJ, Nadeau-Fredette A-C, Tennankore KK, Chan CT. A virtual ward for home hemodialysis patients—a pilot trial. Can J Kidney Heal Dis. 2015;2:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Van Bulck L, Claes K, Dierickx K, et al. Patient and treatment characteristics associated with patient activation in patients undergoing hemodialysis: a cross-sectional study. BMC Nephrology. 2018;19:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Khatib ST, Hemadneh MK, Hasan SA, Khazneh E, Zyoud SH. Quality of life in hemodialysis diabetic patients: a multicenter cross-sectional study from Palestine. BMC Nephrology. 2018;19:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Liem YS, Bosch JL, Hunink MGM. Preference-based quality of life of patients on renal replacement therapy: a systematic review and meta-analysis. Value Health. 2008;11(4):733-741. [DOI] [PubMed] [Google Scholar]
- 31. Wu AW, Fink NE, Marsh-Manzi JVR, et al. Changes in quality of life during hemodialysis and peritoneal dialysis treatment: generic and disease specific measures. 2004;15:743-753. doi: 10.1097/01.ASN.0000113315.81448.CA. [DOI] [PubMed] [Google Scholar]
- 32. Mitema D, Jaar BG. How can we improve the quality of life of dialysis patients? Semin Dial. 2016;29:93-102. doi: 10.1111/sdi.12467. [DOI] [PubMed] [Google Scholar]
- 33. Ong SW, Jassal SV, Miller JA, et al. Integrating a smartphone-based self-management system into usual care of advanced CKD. Clin J Am Soc Nephrol. 2016;11(6):1054-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, SupplementaryFile1_(1) for Effectiveness of a Web-Based eHealth Portal for Delivery of Care to Home Dialysis Patients: A Single-Arm Pilot Study by James Kiberd, Usman Khan, Cynthia Stockman, Arun Radhakrishnan, Matthew Phillips, Bryce A. Kiberd, Kenneth A. West, Steven Soroka, Christopher Chan and Karthik K. Tennankore in Canadian Journal of Kidney Health and Disease
Supplemental material, SupplementaryFile2_Version2 for Effectiveness of a Web-Based eHealth Portal for Delivery of Care to Home Dialysis Patients: A Single-Arm Pilot Study by James Kiberd, Usman Khan, Cynthia Stockman, Arun Radhakrishnan, Matthew Phillips, Bryce A. Kiberd, Kenneth A. West, Steven Soroka, Christopher Chan and Karthik K. Tennankore in Canadian Journal of Kidney Health and Disease