Abstract
In this review, we have attempted to share our 10 years’ clinical experience with aripiprazole use and switching from other antipsychotics to aripiprazole. There are various reasons for switching, including a partial or complete lack of efficacy, adverse side effects, and partial or noncompliance with medication. Aripiprazole has some unique receptor-binding qualities that provides some advantages over other antipsychotics in certain clinical situations. We have covered potential clinical scenarios for aripiprazole use as a single agent and switching from other agents in inpatient and outpatient settings. Patients switched from other antipsychotics to aripiprazole have been shown to benefit from significant improvements in clinical response and tolerability. This review examines the strategies for switching patients from antipsychotic drugs to aripiprazole.
Keywords: aripiprazole, depression, first episode, obsessive–compulsive disorder, schizophrenia, switching
Introduction
Aripiprazole is an atypical antipsychotic drug with a high affinity for dopamine D2 and D3 receptors, and serotonin 5-HT1A, 5-HT2 and 5-HT2B receptors.1 Due to aripiprazole’s partial agonist activity at D2 receptors, it has lower propensity for extrapyramidal symptoms.2 Having a unique mechanism, aripiprazole has not only a lower liability for inducing hyperprolactinemia, but also has the ability to normalize elevated prolactin levels induced by previous antipsychotics. Aripiprazole, acting as a partial agonist at D2 and 5-HT1A receptors, is reported to be effective on anxiety, depressive symptoms, cognitive symptoms and negative symptoms. 5-HT2 receptors antagonism has positive effects on negative and cognitive symptoms. Aripiprazole has not only favorable impact on cognition due to increase in dopamine release in the prefrontal cortex and hippocampus but also unlikely to cause cognitive dysfunction due to its low affinity on acetylcholine muscarinic receptors.3 Aripiprazole does not cause a high level of sedation, which is attributed to its mild antagonist effect on the histamine H1 receptors.4
The acute and long-term efficacy of aripiprazole for treatment of schizophrenia and schizoaffective disorder has been demonstrated with long-term studies.5–13 On the other hand, a Cochrane review that benchmarked aripiprazole with other atypical antipsychotics has shown that aripiprazole has similar efficacy, compared with clozapine, quetiapine, risperidone, ziprasidone and olanzapine; aripiprazole leads to improved quality of life, compared with clozapine and quetiapine; aripiprazole is associated with lower incidence of extrapyramidal symptoms (EPS); aripiprazole-associated weight gain is lower, compared with olanzapine, but higher than ziprasidone; and aripiprazole is associated with a higher incidence of early discontinuation of treatment, compared with olanzapine.14
The efficacy of aripiprazole for treatment of bipolar disorder has been documented in different studies.15–22 Treatment guidelines have indicated that the efficacy of aripiprazole for continuation treatment of acute mania and bipolar disorders is of ‘high level’, and aripiprazole has a ‘good’ risk-benefit ratio. In addition, treatment algorithms have suggested ‘aripiprazole as a single agent’ or ‘aripiprazole combined with lithium or divalproex’ as a first choice of treatment.23,24 In a recent review, ‘aripiprazole as a single agent’ or ‘augmentation with aripiprazole’ has been suggested as the first choice for treatment of acute mania, and maintenance treatment of manic or mixed episodes.25 The same review has also reported that aripiprazole is associated with lower medical costs compared with olanzapine, quetiapine, risperidone, and ziprasidone.25
Aripiprazole has been reported to be an effective augmenter where there is poor response to antidepressants in depressive disorders.26–30 In a study which compares aripiprazole with other second-generation antipsychotics in depression, patients who used aripiprazole had a better ‘health-related quality of life’.31 Another study has compared ‘supplemental treatment for aripiprazole’, ‘antidepressant combination’ and ‘changing antidepressant’ strategies in patients with major depressive disorder who were nonresponsive to antidepressant; supplemental treatment for aripiprazole has been reported as more effective compared with the other strategies.32
A multidisciplinary panel entitled ‘Switching from other antipsychotics to aripiprazole and aripiprazole use’ was convened in Turkey to provide practical guidance for prescribing aripiprazole. This report describes the consensus recommendations agreed during the meeting and reflects the 10-year experience of aripiprazole use in Turkey. A comprehensive literature search was conducted to support these recommendations. There are similar initiatives in other countries, and some of these documents were reviewed during preparation of this report.33,34
Switching to aripiprazole from other antipsychotic drugs
Switching between antipsychotics in the treatment of schizophrenia and bipolar disorder is a common practice among psychiatrists. Most common reasons for considering an alternative are insufficient efficacy and persistent side effects.35 Naturalistic observation studies have suggested that compliance to treatment is poor with antipsychotics in general,36 which is mainly due to treatment-related adverse events and treatment dissatisfaction among patients.37 The widespread use of second-generation (atypical) anti-psychotics led to a decrease in EPS; however, various side effects including metabolic issues (mainly weight gain), hyperprolactinemia and prolonged QTc have been consistently reported.30,38–41
In general, metabolic syndrome represents the major disadvantage of the second-generation antipsychotics. Aripiprazole has the most favorable profile among this category with respect to metabolic side effects.42,43 In a meta-analysis based on the data collected from 784 patients with schizophrenia or schizoaffective disorder from different countries and ethnicities, significant weight loss has been reported following the transition to aripiprazole from another antipsychotic.44 Aripiprazole does not cause hyperprolactinemia; in fact, addition of aripiprazole to other antipsychotics leads to a decrease in elevated prolactin levels.4 Aripiprazole is considered a safe antipsychotic from a cardiovascular standpoint, having the lowest risk of prolonged QTc and coronary heart disease.5,45–47 Among all antipsychotics, aripiprazole is associated with lower frequency of sexual side effects.48,49 Given its positive effects on cognitive symptoms and negative symptoms, aripiprazole can be preferred for patients who experience such side effects.50–53 Aripiprazole has been reported to cause less sedation and somnolence, compared with other antipsychotics.54,55 Due to lower level of anticholinergic effects, it is expected that side effects such as xerostomia and constipation are seen at a lower frequency.56 The advantages of aripiprazole include effectiveness in depressive symptoms in schizophrenia, positive effects on quality of life, and preference by patients.6,52 Aripiprazole has been reported as effective for treatment of depressive disorders, alcohol-use disorder associated with bipolar disorder and schizoaffective disorder; in another study, aripiprazole treatment has been reported to reduce the severity in alcohol-use disorder.57–59 It has also been reported that aripiprazole treatment leads to a significant reduction of obsessive–compulsive symptoms in schizophrenia, and in obsessive–compulsive disorder (OCD) when added to selective serotonin reuptake inhibitor (SSRI) treatment.60,61
The main side effects of switching and proposed alternatives are shown in Table 1. As shown in Table 1, aripiprazole is recommended as the next choice for the switch when several side effects are seen.
Table 1.
Side effects that can lead to antipsychotic switching; antipsychotics that can cause side effects and alternative antipsychotics.
| Reasons for switching | Possible causes | Alternative antipsychotics |
|---|---|---|
| Metabolic side effects (weight gain/dyslipidemia/altered glucose tolerance) | Olanzapine, quetiapine | Aripiprazole, amisulpride, ziprasidone, haloperidol |
| Hyperprolactinemia | Amisulpride, risperidone, paliperidone | Aripiprazole, quetiapine |
| EPS | Haloperidol, risperidone, amisulpride | Aripiprazole, olanzapine, quetiapine |
| Tardive dyskinesia | Haloperidol, risperidone | Clozapine, aripiprazole, olanzapine, quetiapine |
| Insufficient efficacy/dissatisfaction | Quetiapine, haloperidol | Aripiprazole |
| Postural hypotension | Chlorpromazine, quetiapine | Aripiprazole, amisulpride, haloperidol |
| Prolonged QTc | Ziprasidone, sulpiride | Aripiprazole |
| Sedation | Quetiapine, olanzapine, first-generation antipsychotics | Aripiprazole, paliperidone |
| Sexual side effects | Amisulpride, risperidone, paliperidone | Aripiprazole, quetiapine |
| Negative/depressive symptoms | First-generation antipsychotics, risperidone | Aripiprazole, amisulpride, paliperidone |
| Cognitive function | First-generation antipsychotics, olanzapine, quetiapine | Aripiprazole, paliperidone, amisulpride |
| Comorbid obsessive–compulsive symptoms | Olanzapine, risperidone | Aripiprazole, amisulpride, haloperidol |
Evaluation before switching to aripiprazole
Before switching to aripiprazole, patients with schizophrenia, schizoaffective disorder or bipolar disorder should be evaluated in detail, as would be done in the case of switching to any other antipsychotic. Past psychiatric history, medical history and psychotropic-use history, most recent psychiatric functioning and psychiatric review of symptoms (positive, negative, depressive and cognitive symptoms, social and occupational functionality, quality of life) should be considered; the reason for switching to aripiprazole and expectations should be outlined. It is recommended that the decision for switching be made in a collaborative effort by the patient and the clinician (if needed, together with the carer).62 Weight, waist circumference, fasting blood glucose level, glycated hemoglobin level, lipid profile, and prolactin level should be measured prior to switch. Assessment of extrapyramidal symptoms, nutritional status, diet, and physical activity is necessary. Electro-cardiogram is indicated for patients with a history of hypertension or cardiovascular disease, or patients receiving inpatient treatment.62
It is important to inform patients about common issues associated with transition, including withdrawal symptoms, drug–drug interactions, and possible relapse in psychiatric symptoms should be discussed. During the switching period, it is important to monitor patients closely, with frequent outpatient visits.
Starting aripiprazole treatment and patients likely to benefit from switching to aripiprazole
According to a multidisciplinary panel on use of aripiprazole for treatment of schizophrenia, patients: who are newly diagnosed or have not received any treatment; who are unable to tolerate the current antipsychotic; who developed metabolic side effects; whose symptoms did not remit; who experienced acute exacerbation while on the current antipsychotic or who discontinued current antipsychotic due to poor efficacy or tolerance, are likely to benefit from aripiprazole treatment.33 There have been other reports of successful transition to aripiprazole in patients with shorter disease duration and antipsychotic use, patients with less symptom severity, and patients who do not have a history of recurrent relapse63–65 (Table 2).
Table 2.
Patients who are likely to benefit from switching to aripiprazole.
| Newly diagnosed patients or patients who have not received antipsychotic treatment before |
| Patients who are unable to tolerate the antipsychotic medication they use |
| Patients who experience problems (e.g. metabolic) with current antipsychotic |
| Patients whose symptoms cannot be maintained with current antipsychotic |
| Patients who discontinue antipsychotic treatment (due to insufficient symptom control or tolerability problems) |
| Patients who switched from another second-generation antipsychotic to aripiprazole |
Method of switching to aripiprazole
Some studies have suggested that a rapid switch to aripiprazole is acceptable66–69; yet, at least one study has reported that a rapid switch can be hazardous.70 There are also other reports that propose switching to aripiprazole should be gradual.33,34
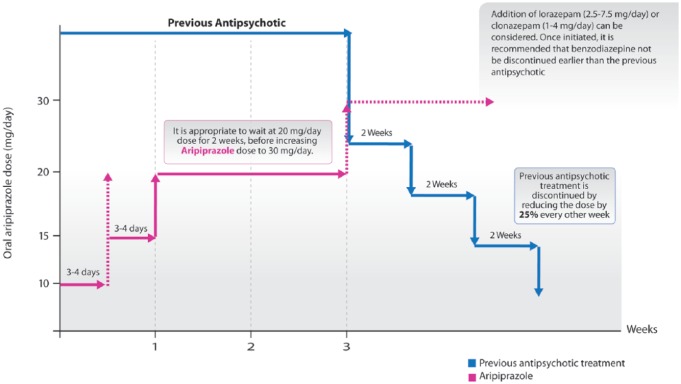
Switching to aripiprazole in patients with stable schizophrenia in outpatient setting
Switching to aripiprazole for treatment of patients with stable schizophrenia is summarized in Figure 1. These patients generally experience side effects from existing treatment, or respond poorly to the existing treatment. In addition to the existing treatment, it is appropriate to initiate aripiprazole treatment with 2.5–5 mg/day, increase the dose to 5–10 mg/day at the end of first week, and then to 10–15 mg/day at the end of second week. Once the target dose of 10–15 mg/day is reached, aripiprazole and previous antipsychotics should be used together for at least 2 weeks. Afterwards, previous antipsychotic treatment should be discontinued by reducing the dose by 25% with minimum 2-week intervals (e.g. for a given dose of 20 mg/day, 15►10►5; for a given dose of 4 mg/day, 3►2►1 and stop). In some cases, it may be necessary to titrate the aripiprazole dose up to 30 mg. In such cases, the dose should be first increased to 15–20 mg, and should be maintained for at least 2 weeks. If necessary, the dose can be increased to 30 mg. In view of the current literature, aripiprazole treatment can vary within 10–30 mg/day dose range for maintenance treatment of schizophrenia.71–73
Figure 1.
Switching to aripiprazole in case of outpatients with stable schizophrenia.
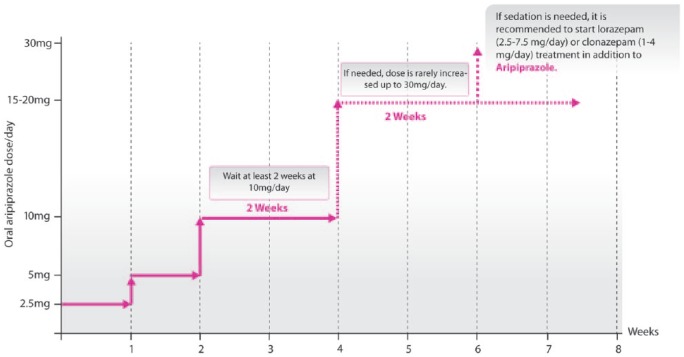
Switching to aripiprazole in patients with history of recurrent psychotic relapse in the outpatient setting
Switching to aripiprazole for treatment of outpatients with recurrent psychotic exacerbation is summarized in Figure 2. For this patient group, it is appropriate to start aripiprazole treatment at a dose of 10 mg/day. If possible problems are predicted, it is possible to start treatment with a dose of 5 mg/day. It is recommended to increase the dose by 5–10 mg with 1-week intervals and reach 20–30 mg/day. Once a 20 mg/day dose is reached, it is appropriate to wait for 2 weeks before increasing the dose to 30 mg/day. At 2 weeks after reaching the desired aripiprazole dose, the previous antipsychotic treatment can be discontinued by reducing the dose by 25% every 2 weeks. If the reason for stopping previous antipsychotic treatment is inefficacy, tapering it down by weekly dose reduction is recommended.
Figure 2.
Switching to aripiprazole for treatment of outpatients with recurrent psychotic exacerbation.
Switching to aripiprazole in the inpatient setting
The switching to aripiprazole for inpatients with schizophrenia is summarized in Figure 3. In this patient group, the treatment should be started with a dose of 10 mg/day. Afterwards, the dose can be increased to 20–30 mg/day, with 5–10 mg increases every 3–4 days. In the inpatient setting, it is recommended to stay at 20 mg for at least 2 weeks. Clinicians should also consider augmentation with lorazepam (2.5–7.5 mg/day) or clonazepam (1–2 mg/day) during the switch to aripiprazole. Once the desired aripiprazole dose is reached, previous antipsychotic can be tapered off by reducing the dose by 25% no faster than every 2 weeks, unless the reason for the switch is solely due to the inefficacy of the previous antipsychotic, in which case, weekly tapering is reasonable. It is generally recommended to discontinue benzodiazepine treatment, if added, after the discontinuation of the previous antipsychotic, but it can be done earlier.
Figure 3.
Switching to aripiprazole in the inpatient setting.
Management of adverse symptoms during the switch
When switching from other antipsychotics to aripiprazole, withdrawal from the previous antipsychotic medication or initiation of aripiprazole may lead to undesired symptoms. In such cases, benzodiazepines, beta blockers, antihistamines and anticholinergics can be successfully used to suppress the undesired symptoms.34,74–76 The adverse symptoms during switch and recommendations for managing the symptoms are summarized in Table 3.
Table 3.
Possible adverse effects during switch from other antipsychotics to aripiprazole and their management.
| Symptom | Approach/additional drug |
|---|---|
| Akathisia | Decrease aripiprazole dose, slow down dose reduction of the previous antipsychotic; add benzodiazepine and possibly a beta-blocker and possibly anticholinergics |
| Mania, psychosis | Slow down dose reduction of the previous antipsychotic or
reverse switch; increase aripiprazole dose Add benzodiazepine and possibly valproate (for bipolar disorder) |
| Agitation | Slow down dose reduction of the previous antipsychotic or
reverse switch; increase aripiprazole dose Add benzodiazepine and possibly valproate (for bipolar disorder) |
| Anxiety | Slow down dose reduction of the previous antipsychotic or
reverse switch; increase aripiprazole dose Add benzodiazepine |
| Insomnia | Slow down dose reduction of the previous
antipsychotic Add benzodiazepine and possibly an antihistaminic and possibly a hypnotic |
| Nausea/vomiting | Slow down dose reduction of the previous antipsychotic, reduce
aripiprazole dose temporarily (2–3 days), split total daily dose
in two Add antihistaminic and possibly an antiemetic |
| Hiccups | Slow down reduction of the previous antipsychotic; reduce aripiprazole dose (half dose) and wait for 2 weeks and increase the dose again; if hiccups occur again, stop aripiprazole |
Use of aripiprazole in first episode psychosis
The use of aripiprazole for first-episode psychosis is summarized in Figure 4. Generally, patients experiencing first attacks are more sensitive to antipsychotic effect and side effects. Therefore, lower doses are recommended for this patient group.77 Initiating aripiprazole treatment is recommended at 2.5 mg/day. The dose can be increased to 5 mg/day by the end of the first week, and to 10 mg/day by the end of second week. Staying at 10 mg/day is recommended for at least 2 weeks, and if needed, the dose can be further increased to 15–20 mg/day. In severe cases, the dose can be increased to 30 mg/day. Before increasing the dose to 30 mg/day, staying at the 15–20 mg/day dose is recommended for at least 2 weeks.
Figure 4.
Use of aripiprazole for treatment of first-episode psychosis.
If the patient requires sedation, addition of lorazepam (2.5–7.5 mg/day or clonazepam (1–2 mg/day) should be considered.
Use of aripiprazole in bipolar mania
The use of aripiprazole in bipolar mania is summarized in Figure 5. For treatment of acute mania, initiation of aripiprazole is recommended at 10 mg/day. The dose can be increased by 5–10 mg every 3–4 days, up to 20–30 mg/day and we recommend staying at 20 mg/day for at least 2 weeks before considering further titration. Addition of lorazepam (2.5–7.5 mg/day) or clonazepam (1–2 mg/day) can be considered, which should be tapered down slowly following stabilization. To prevent recurrent manic episodes, it is recommended keeping aripiprazole treatment at 15–30 mg/day.78
Figure 5.
The use of aripiprazole for treatment of acute bipolar episodes.
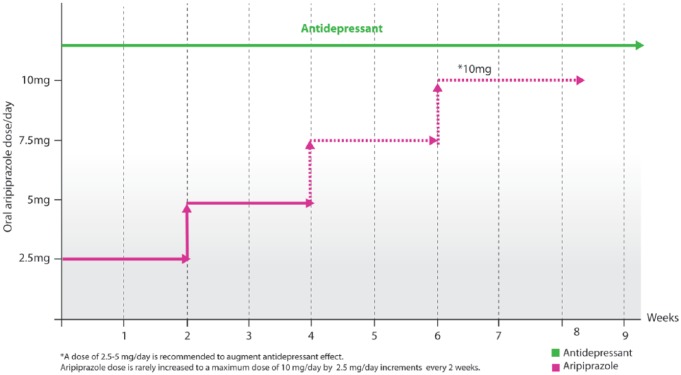
The use aripiprazole in patients with depression in the setting of inadequate response to antidepressants
The use of aripiprazole for treatment of depression is summarized in Figure 6. If response to antidepressant treatment is inadequate, addition of an atypical antipsychotic (e.g. aripiprazole, quetiapine or olanzapine) is considered the most common and effective augmentation strategy.30 For augmentation purposes, using aripiprazole within a dose range of 2.5–10 mg/day is recommended. In this patient group, it is reasonable to start aripiprazole at 2.5 mg/day (in addition to antidepressant treatment); if needed, the dose can be increased to a maximum level of 10 mg/day, by increasing 2.5 mg every 2 weeks.
Figure 6.
Addition of aripiprazole in the setting of poor response to antidepressants.
The use of aripiprazole in patients with antipsychotic-induced hyperprolactinemia
The use of aripiprazole for treatment of antipsychotic-induced hyperprolactinemia is summarized in Figure 7. Hyperprolactinemia is a major adverse effect of second-generation antipsychotics, which can lead to amenorrhea and galactorrhea in women, and gynecomastia in men. Moreover, it can also cause sexual side effects and osteoporosis in both men and women.79 In the setting of hyperprolactinemia associated with antipsychotic administration, switching to aripiprazole should be considered, particularly when the response to the existing antipsychotic is limited. When the existing regimen is sufficiently controlling the symptoms, addition of aripiprazole to the existing treatment can also be considered. In such cases, it is reasonable to add low-dose aripiprazole (e.g. 2.5 mg/day) to the current regimen, and if needed, it can be titrated up to 10 mg/day.80 On the other hand, in the setting of hyperprolactinemia associated with benzamide-derivative antipsychotics (sulpiride and amisulpride), addition of aripiprazole has no demonstrated effect on prolactin levels.81
Figure 7.
The use of aripiprazole in the setting of hyperprolactinemia associated with antipsychotics.
The use of aripiprazole in the setting of treatment-resistant obsessive–compulsive disorder
The use of aripiprazole for OCD is summarized in Figure 8. Antipsychotic augmentation of the serotonin reuptake inhibitor (SRI) or clomipramine use in patients with treatment-resistant OCD is a recommended option according to the NICE treatment guidelines.82 Additionally, a systematic review and meta-analysis on augmentation treatment of SRI-re-sistant OCD with antipsychotics have suggested that aripiprazole is an effective agent for augmentation.61 In this patient group, in addition to SRI or clomipramine, initiating aripiprazole treatment at 2.5 mg/day is recommended, and then titrating up to 10 mg/day with 2.5 mg increases every 2 weeks. For this patient group, increasing the dose up to a maximum of 20 mg/day is recommended. If a dose > 10 mg/day is considered, staying at least 4 weeks at 10 mg/day is recommended and 15 mg/day subsequently, before titrating further.
Figure 8.
The use of aripiprazole in the setting of treatment resistant obsessive–compulsive disorder.
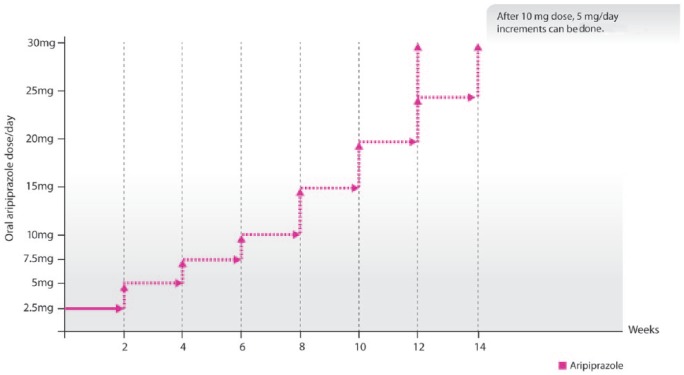
The use of aripiprazole for tic disorders
The use of aripiprazole for treatment of tic disorders is summarized in Figure 9. Aripiprazole is suggested as a treatment option for tic disorders by the Canada treatment guidelines.83 Aripiprazole has been reported as effective for comorbid conditions in tic disorders, including OCD, depression, anxiety, and attention-deficit hyperactivity disorder.84 Another study has reported that 82 of 100 patients with Tourette syndrome responded to aripiprazole treatment.85
Figure 9.
The use of aripiprazole for treatment of tic disorders.
For tic disorders, initiating aripiprazole treatment at 2.5 mg/day is recommended, which should be increased to 10 mg by 2.5 mg increments every 2 weeks. Where further titration is appropriate, 5 mg per day increase every 2 weeks for a target dose of 30 mg/day can be considered. It is also acceptable to make a rapid increase from 20 mg/day to 30 mg/day, where clinically justified. When a sufficient response is achieved at a dose within the 2.5–30 mg range, the dose should not be increased further.
Summary and conclusion
In this review, we have attempted to share our 10-year clinical experience with aripiprazole use and switching from other antipsychotics to aripiprazole. Aripiprazole has some unique receptor binding qualities which provides some advantages over other antipsychotics in certain clinical situations. We have covered potential clinical scenarios for aripiprazole use as a single agent and switching from other agents in inpatient and outpatient settings. Our goal is to create an aid for clinicians on most appropriate use of aripiprazole in different clinical situations.
Key points
(1) The management of switching from atypical antipsychotics to aripiprazole is critical because of the pharmacological properties.
(2) The duration of the steady state is 2 weeks. Waiting for 2 weeks to decide about increasing the dose is recommended.
(3) OCD and tic disorders are the most common psychiatric diseases that psychiatrists prefer in their prescriptions.
Acknowledgments
Contributors to the Turkish aripiprazole consensus group meeting and report:
Prof. Mesut Cetin
Prof. Murat Atmaca
Prof. Haluk Savas
Dr Canan Tinaz
Dr Ulas Camsari
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The consensus group meeting for the development of this publication was organized and funded by Nobel Pharmaceuticals. This publication is based on the discussions from the consensus group meeting, with all authors contributing to all drafts of the article. The opinions expressed in this article are the independent consensus views of the authors and have not been influenced by third-party sponsorship.
Prof. Dilbaz has received speaker honoraria, been invited member of advisory boards and participated in clinical trials on behalf of several pharmaceutical companies including Nobel, Abdi İbrahim, Janssen Cilag, Lundbeck, Generica, Santa Pharma and Pfizer.
Prof. Veznedaroglu has received speaker honoraria, been invited member of advisory boards and participated in clinical trials on behalf of several pharmaceutical companies including, Abdi İbrahim Otsuka, Bilim İlaç, Bristol-Myers Squibb, GlaxoSmithKline, Janssen Cilag, Lilly, Nobel, Sanofi-Synthelabo, Sanovel.
Prof. Uzun has received speaker honoraria, been invited as a member of advisory boards and participated in clinical trials on behalf of several pharmaceutical companies including Janssen Cilag and Nobel.
Prof. Isik has received speaker honoraria from Nobel and Lundbeck and been invited as a member of advisory boards of Nobel and Lundbeck.
ORCID iD: Nesrin Dilbaz  https://orcid.org/0000-0003-0724-3489
https://orcid.org/0000-0003-0724-3489
Contributor Information
Baybars Veznedaroglu, Psychiatry, Ege University, Izmir, Turkey.
Nesrin Dilbaz, Nesrin Dilbaz Psychiatry, NP Brain Hospital, Uskudar University, Ahmet Tevfik Ileri cad. No: 18, Umraniye, Istanbul 34768, Turkey.
Ozcan Uzun, Psychiatry, Gulhane Training and Research Hospital, Ankara, Turkey.
Erdal Isik, Psychiatry, Gazi University, Ankara, Turkey.
References
- 1. Leysen JE, Janssen PM, Schotte A, et al. Interaction of antipsychotic drugs with neurotransmitter receptor sites in vitro and in vivo in relation to pharmacological and clinical effects: role of 5HT 2 receptors. Psychopharmacology 1993; 112: S40–S54. [DOI] [PubMed] [Google Scholar]
- 2. Marder SR, McQuade RD, Stock E, et al. Aripiprazole in the treatment of schizophrenia: safety and tolerability in short-term, placebo-controlled trials. Schizophr Res 2003; 61: 123–136. [DOI] [PubMed] [Google Scholar]
- 3. Lieberman JA. Dopamine partial agonists. CNS Drugs 2004; 18: 251–267. [DOI] [PubMed] [Google Scholar]
- 4. De Berardis D, Fornaro M, Serroni N, et al. Treatment of antipsychotic-induced hyperprolactinemia: an update on the role of the dopaminergic receptors D2 partial agonist aripiprazole. Recent Pat Endocr Metab Immune Drug Discov 2014; 8: 30–37. [DOI] [PubMed] [Google Scholar]
- 5. Kane JM, Carson WH, Saha AR, et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 2002; 63: 133–156. [DOI] [PubMed] [Google Scholar]
- 6. Kasper S, Lerman MN, McQuade RD, et al. Efficacy and safety of aripiprazole vs. haloperidol for long-term maintenance treatment following acute relapse of schizophrenia. Int J Neuropsychopharmacol 2003; 6: 325–337. [DOI] [PubMed] [Google Scholar]
- 7. Pigott TA, Carson WH, Saha AR, et al. Aripiprazole for the prevention of relapse in stabilized patients with chronic schizophrenia: a placebo-controlled 26-week study. J Clin Psychiatry 2003; 64: 1048–1056. [DOI] [PubMed] [Google Scholar]
- 8. Potkin SG, Saha AR, Kujawa MJ, et al. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry 2003; 60: 681–690. [DOI] [PubMed] [Google Scholar]
- 9. Chrzanowski WK, Marcus RN, Torbeyns A, et al. Effectiveness of long-term aripiprazole therapy in patients with acutely relapsing or chronic, stable schizophrenia: a 52-week, open-label comparison with olanzapine. Psychopharmacology 2006; 189: 259–266. [DOI] [PubMed] [Google Scholar]
- 10. Kane JM, Crandall DT, Marcus RN, et al. Symptomatic remission in schizophrenia patients treated with aripiprazole or haloperidol for up to 52 weeks. Schizophr Res 2007; 95: 143–150. [DOI] [PubMed] [Google Scholar]
- 11. Janicak PG, Glick ID, Marder SR, et al. The acute efficacy of aripiprazole across the symptom spectrum of schizophrenia: a pooled post hoc analysis from 5 short-term studies. J Clin Psychiatry 2009; 70: 25–35. [DOI] [PubMed] [Google Scholar]
- 12. Glick ID, Mankoski R, Eudicone JM, et al. The efficacy, safety, and tolerability of aripiprazole for the treatment of schizoaffective disorder: results from a pooled analysis of a sub-population of subjects from two randomized, double-blind, placebo-controlled, pivotal trials. J Affect Disord 2009; 115: 18–26. [DOI] [PubMed] [Google Scholar]
- 13. Kwon JS, Jang JH, Kang DH, et al. Long-term efficacy and safety of aripiprazole in patients with schizophrenia, schizophreniform disorder, or schizoaffective disorder: 26-week prospective study. Psychiatry Clin Neurosc 2009; 63: 73–81. [DOI] [PubMed] [Google Scholar]
- 14. Khanna P, Suo T, Komossa K, et al. Aripiprazole versus other atypical antipsychotics for schizophrenia. Cochrane Database Syst Rev 2014; 1: CD006569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry 2003; 160: 1651–1658. [DOI] [PubMed] [Google Scholar]
- 16. Keck Jr PE, Calabrese JR, McQuade RD, et al. A randomized, double-blind, placebo-controlled 26-week trial of aripiprazole in recently manic patients with bipolar I disorder. J Clin Psychiatry 2006; 67: 626–637. [DOI] [PubMed] [Google Scholar]
- 17. Keck JP, Calabrese JR, McIntyre RS, et al. Aripiprazole monotherapy for maintenance therapy in bipolar I disorder: a 100-week, double-blind study versus placebo. J Clin Psychiatry 2007; 68: 1480–1491. [DOI] [PubMed] [Google Scholar]
- 18. Keck P, Orsulak P, Cutler A, et al. Aripiprazole monotherapy in the treatment of acute bipolar I mania: a randomized, double-blind, placebo-and lithium-controlled study. J Affect Disord 2009; 112: 36–49. [DOI] [PubMed] [Google Scholar]
- 19. Sachs G, Sanchez R, Marcus R, et al. Aripiprazole in the treatment of acute manic or mixed episodes in patients with bipolar I disorder: a 3-week placebo-controlled study. J Psychopharmacol 2006; 20: 536–546. [DOI] [PubMed] [Google Scholar]
- 20. Muzina D, Momah C, Eudicone J, et al. Aripiprazole monotherapy in patients with rapid-cycling bipolar I disorder: an analysis from a long-term, double-blind, placebo-controlled study. Int J Clin Pract 2008; 62: 679–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Young AH, Oren DA, Lowy A, et al. Aripiprazole monotherapy in acute mania: 12-week randomised placebo-and haloperidol-controlled study. Br J Psychiatry 2009; 194: 40–48. [DOI] [PubMed] [Google Scholar]
- 22. El-Mallakh RS, Marcus R, Baudelet C, et al. A 40-week double-blind aripiprazole versus lithium follow-up of a 12-week acute phase study (total 52 weeks) in bipolar I disorder. J Affect Disord 2012; 136: 258–266. [DOI] [PubMed] [Google Scholar]
- 23. Grunze H, Vieta E, Goodwin GM, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2009 on the treatment of acute mania. World J Biol Psychiatry 2009; 10: 85–116. [DOI] [PubMed] [Google Scholar]
- 24. Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2013. Bipolar Disord 2013; 15: 1–44. [DOI] [PubMed] [Google Scholar]
- 25. Canada Canadian Agency for Drugs and Technologies in Health. Aripiprazole for patients with bipolar disorder: a review of the clinical effectiveness, cost-effectiveness and guidelines. Ottawa, ON: Canada Canadian Agency for Drugs and Technologies in Health, 2016, contract no.: RC00780–000. [PubMed] [Google Scholar]
- 26. Nelson JC, Pikalov A, Berman RM. Augmentation treatment in major depressive disorder: focus on aripiprazole. Neuropsychiatr Dis Treat 2008; 4: 937–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nelson JC, Thase ME, Bellocchio EE, et al. Efficacy of adjunctive aripiprazole in patients with major depressive disorder who showed minimal response to initial antidepressant therapy. Int Clin Psychopharmacol 2012; 27: 125–133. [DOI] [PubMed] [Google Scholar]
- 28. Nelson JC, Rahman Z, Laubmeier KK, et al. Efficacy of adjunctive aripiprazole in patients with major depressive disorder whose symptoms worsened with antidepressant monotherapy. CNS Spectr 2014; 19: 528–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Casey D, Laubmeier K, Eudicone J, et al. Response and remission rates with adjunctive aripiprazole in patients with major depressive disorder who exhibit minimal or no improvement on antidepressant monotherapy. Int J Clin Pract 2014; 68: 1301–1308. [DOI] [PubMed] [Google Scholar]
- 30. McIntyre RS, Filteau M-J, Martin L, et al. Treatment-resistant depression: definitions, review of the evidence, and algorithmic approach. J Affect Disord 2014; 156: 1–7. [DOI] [PubMed] [Google Scholar]
- 31. Kalsekar I, Wagner J-S, DiBonaventura M, et al. Comparison of health-related quality of life among patients using atypical antipsychotics for treatment of depression: results from the National Health and Wellness Survey. Health Qual Life Outcomes 2012; 10: 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Han C, Wang S-M, Seo H-J, et al. Aripiprazole augmentation, antidepressant combination or switching therapy in patients with major depressive disorder who are partial or non-responsive to current antidepressants: a multi-center, naturalistic study. J Psychiatr Res 2014; 49: 75–82. [DOI] [PubMed] [Google Scholar]
- 33. Sullivan G, Bienroth M, Jones M, et al. Practical prescribing with aripiprazole in schizophrenia: consensus recommendations of a UK multidisciplinary panel. Curr Med Res Opin 2007; 23: 1733–1744. [DOI] [PubMed] [Google Scholar]
- 34. Fagiolini A, Brugnoli R, Di Sciascio G, et al. Switching antipsychotic medication to aripiprazole: position paper by a panel of Italian psychiatrists. Expert Opin Pharmacother 2015; 16: 727–737. [DOI] [PubMed] [Google Scholar]
- 35. Kane JM. Treatment of schizophrenia. Schizophrenia Bullet 1987; 13: 133–156. [DOI] [PubMed] [Google Scholar]
- 36. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New Engl J Med 2005; 353: 1209–1223. [DOI] [PubMed] [Google Scholar]
- 37. Chue P. The relationship between patient satisfaction and treatment outcomes in schizophrenia. J Psychopharmacol 2006; 20(Suppl 6): 38–56. [DOI] [PubMed] [Google Scholar]
- 38. Cha DS, McIntyre RS. Treatment-emergent adverse events associated with atypical antipsychotics. Expert Opin Pharmacother 2012; 13: 1587–1598. [DOI] [PubMed] [Google Scholar]
- 39. Turrone P, Kapur S, Seeman M, Flint AJ. Elevation of prolactin levels by atypical antipsychotics. Year Am J Psychiatry 2003; 159: 133–135. [DOI] [PubMed] [Google Scholar]
- 40. Newcomer JW. Antipsychotic medications: metabolic and cardiovascular risk. J Clin Psychiatry 2007; 68(Suppl 4): 8–13. [PubMed] [Google Scholar]
- 41. Correll CU. Balancing efficacy and safety in treatment with antipsychotics. CNS Spectr 2007; 12: 12–20. [DOI] [PubMed] [Google Scholar]
- 42. Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry 2007; 68(Suppl 1): 20–27. [PubMed] [Google Scholar]
- 43. Citrome L, Kalsekar I, Baker RA, et al. A review of real-world data on the effects of aripiprazole on weight and metabolic outcomes in adults. Curr Med Res Opin 2014; 30: 1629–1641. [DOI] [PubMed] [Google Scholar]
- 44. Barak Y, Aizenberg D. Switching to aripiprazole as a strategy for weight reduction: a meta-analysis in patients suffering from schizophrenia. J Obes 2011; 1: 13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. El-Sayeh H, Morganti C. Aripiprazole for schizophrenia. Cochrane Database Syst Rev 2004; 2: CD004578. [DOI] [PubMed] [Google Scholar]
- 46. Polcwiartek C, Sneider B, Graff C, et al. The cardiac safety of aripiprazole treatment in patients at high risk for torsade: a systematic review with a meta-analytic approach. Psychopharmacology 2015; 232: 3297–3308. [DOI] [PubMed] [Google Scholar]
- 47. Stroup TS, Byerly MJ, Nasrallah HA, et al. Effects of switching from olanzapine, quetiapine, and risperidone to aripiprazole on 10-year coronary heart disease risk and metabolic syndrome status: results from a randomized controlled trial. Schizophr Res 2013; 146: 190–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Serretti A, Chiesa A. A meta-analysis of sexual dysfunction in psychiatric patients taking antipsychotics. Int Clin Psychopharmacol 2011; 26: 130–140. [DOI] [PubMed] [Google Scholar]
- 49. De Boer MK, Castelein S, Wiersma D, et al. The facts about sexual (dys)function in schizophrenia: an overview of clinically relevant findings. Schizophr Bull 2015; 41: 674–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kern RS, Green MF, Cornblatt BA, et al. The neurocognitive effects of aripiprazole: an open-label comparison with olanzapine. Psychopharmacology 2006; 187: 312–320. [DOI] [PubMed] [Google Scholar]
- 51. Hori H, Yoshimura R, Katsuki A, et al. The cognitive profile of aripiprazole differs from that of other atypical antipsychotics in schizophrenia patients. J Psychiatr Res 2012; 46: 757–761. [DOI] [PubMed] [Google Scholar]
- 52. Kerwin R, Millet B, Herman E, et al. A multicentre, randomized, naturalistic, open-label study between aripiprazole and standard of care in the management of community-treated schizophrenic patients Schizophrenia Trial of Aripiprazole:(STAR) study. Eur Psychiatry 2007; 22: 433–443. [DOI] [PubMed] [Google Scholar]
- 53. Stip E, Tourjman V. Aripiprazole in schizophrenia and schizoaffective disorder: a review. Clin Ther 2010; 32: S3–S20. [DOI] [PubMed] [Google Scholar]
- 54. Komossa K, Rummel-Kluge C, Schmid F, et al. Aripiprazole versus other atypical antipsychotics for schizophrenia. Cochrane Database Syst Rev 2009; 4: CD006569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Jones M, Nicholl D, Trakas K. Efficacy and tolerability of paliperidone ER and other oral atypical antipsychotics in schizophrenia. Int J Clin Pharmacol Ther 2010; 48: 383–399. [DOI] [PubMed] [Google Scholar]
- 56. DeLeon A, Patel NC, Crismon ML. Aripiprazole: a comprehensive review of its pharmacology, clinical efficacy, and tolerability. Clin Ther 2004; 26: 649–666. [DOI] [PubMed] [Google Scholar]
- 57. Han DH, Kim SM, Choi JE, et al. Adjunctive aripiprazole therapy with escitalopram in patients with co-morbid major depressive disorder and alcohol dependence: clinical and neuroimaging evidence. J Psychopharmacol 2013; 27: 282–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Brown ES, Jeffress J, Liggin JD, et al. Switching outpatients with bipolar or schizoaffective disorders and substance abuse from their current antipsychotic to aripiprazole. J Clin Psychiatry 2005; 66: 756–760. [DOI] [PubMed] [Google Scholar]
- 59. Myrick H, Li X, Randall PK, et al. The effect of aripiprazole on cue-induced brain activation and drinking parameters in alcoholics. J Clin Psychopharmacol 2010; 30: 365–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Schirmbeck F, Rausch F, Englisch S, et al. Differential effects of antipsychotic agents on obsessive–compulsive symptoms in schizophrenia: a longitudinal study. J Psychopharmacol 2013; 27: 349–357. [DOI] [PubMed] [Google Scholar]
- 61. Veale D, Miles S, Smallcombe N, et al. Atypical antipsychotic augmentation in SSRI treatment refractory obsessive-compulsive disorder: a systematic review and meta-analysis. BMC Psychiatry 2014; 14: 317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kuipers E, Yesufu-Udechuku A, Taylor C, et al. Excellence NIfC. Management of Psychosis and schizophrenia in adults: summary of updated NICE guidance. Br Med J (online). 2014; 348: 1–4. [DOI] [PubMed] [Google Scholar]
- 63. Lin HC, Chong MY, Lee Y, et al. Switching of antipsychotics to aripiprazole in the treatment of schizophrenia. Chang Gung Med J 2009; 32: 409–416. [PubMed] [Google Scholar]
- 64. Takase M, Kanahara N, Oda Y, et al. Dopamine supersensitivity psychosis and dopamine partial agonist: a retrospective survey of failure of switching to aripiprazole in schizophrenia. J Psychopharmacol 2015; 29: 383–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Takaesu Y, Kishimoto T, Murakoshi A, et al. Factors associated with discontinuation of aripiprazole treatment after switching from other antipsychotics in patients with chronic schizophrenia: a prospective observational study. Psychiatry Res 2016; 236: 71–74. [DOI] [PubMed] [Google Scholar]
- 66. Casey DE, Carson WH, Saha AR, et al. Switching patients to aripiprazole from other antipsychotic agents: a multicenter randomized study. Psychopharmacology 2003; 166: 391–399. [DOI] [PubMed] [Google Scholar]
- 67. Takeuchi H, Suzuki T, Uchida H, et al. A randomized, open-label comparison of 2 switching strategies to aripiprazole treatment in patients with schizophrenia: add-on, wait, and tapering of previous antipsychotics versus add-on and simultaneous tapering. J Clin Psychopharmacol 2008; 28: 540–543. [DOI] [PubMed] [Google Scholar]
- 68. Ryckmans V, Kahn J, Modell S, et al. Switching to aripiprazole in outpatients with schizophrenia experiencing insufficient efficacy and/or safety/tolerability issues with risperidone: a randomized, multicentre, open-label study. Pharmacopsychiatry 2009; 42: 114–121. [DOI] [PubMed] [Google Scholar]
- 69. Hwang T-J, Lo W-M, Chan H-Y, et al. Fast versus slow strategy of switching patients with schizophrenia to aripiprazole from other antipsychotics. J Clin Psychopharmacol 2015; 35: 635–644. [DOI] [PubMed] [Google Scholar]
- 70. Pae C-U, Serretti A, Chiesa A, et al. Immediate versus gradual suspension of previous treatments during switch to aripiprazole: results of a randomized, open label study. Eur Neuropsychopharmacol 2009; 19: 562–570. [DOI] [PubMed] [Google Scholar]
- 71. Mace S, Taylor D. Aripiprazole. CNS Drugs 2009; 23: 773–780. [DOI] [PubMed] [Google Scholar]
- 72. Leucht S, Samara M, Heres S, et al. Dose equivalents for second-generation antipsychotics: the minimum effective dose method. Schizophr Bull 2014; 40: 314–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Charpeaud T, Samalin L, Llorca P. Efficacy of aripiprazole for the treatment of schizophrenia: what dose is required? L’Encephale 2014; 40: 62–73. [DOI] [PubMed] [Google Scholar]
- 74. Correll C. From receptor pharmacology to improved outcomes: individualising the selection, dosing, and switching of antipsychotics. Eur Psychiatry 2010; 25: S12–S21. [DOI] [PubMed] [Google Scholar]
- 75. Hori H, Nakamura J. Hiccups associated with switching from olanzapine to aripiprazole in a patient with paranoid schizophrenia. Clin Neuropharmacol 2014; 37: 88–89. [DOI] [PubMed] [Google Scholar]
- 76. Kutuk MO, Tufan AE, Guler G, et al. Persistent hiccups due to aripiprazole in an adolescent with obsessive compulsive disorder responding to dose reduction and rechallenge. Oxf Med Case Reports 2016; 2016: 66–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lehman AF, Lieberman JA, Dixon LB, et al. Practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry 2004; 161(Suppl 2): 1–56. [PubMed] [Google Scholar]
- 78. Fagiolini A, Nitti M, Forgione RN, et al. Aripiprazole for the treatment of bipolar disorder: a review of current evidence. Exp Opin Pharmacother 2011; 12: 473–488. [DOI] [PubMed] [Google Scholar]
- 79. Bostwick JR, Guthrie SK, Ellingrod VL. Antipsychotic-induced hyperprolactinemia. Pharmacotherapy 2009; 29: 64–73. [DOI] [PubMed] [Google Scholar]
- 80. Li X, Tang Y, Wang C. Adjunctive aripiprazole versus placebo for antipsychotic-induced hyperprolactinemia: meta-analysis of randomized controlled trials. PLoS One 2013; 8: e70179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Chen C-K, Huang Y-S, Ree S-C, et al. Differential add-on effects of aripiprazole in resolving hyperprolactinemia induced by risperidone in comparison to benzamide antipsychotics. Prog Neuropsychopharmacol Biol Psychiatry 2010; 34: 1495–1499. [DOI] [PubMed] [Google Scholar]
- 82. National Collaborating Centre for Mental Health. Obsessive-compulsive disorder: core interventions in the treatment of obsessive-compulsive disorder and body dysmorphic disorder. Leicester, UK: British Psychological Society, 2006. [PubMed] [Google Scholar]
- 83. Pringsheim T, Doja A, Gorman D, et al. Canadian guidelines for the evidence-based treatment of tic disorders: pharmacotherapy. Can J Psychiatry 2012; 57: 133–143. [DOI] [PubMed] [Google Scholar]
- 84. Gerasch S, Kanaan AS, Jakubovski E, et al. Aripiprazole improves associated comorbid Conditions in addition to Tics in adult patients with Gilles de la Tourette syndrome. Front Neurosci 2016; 10: 416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Wenzel C, Kleimann A, Bokemeyer S, et al. Aripiprazole for the treatment of Tourette syndrome: a case series of 100 patients. J Clin Psychopharmacol 2012; 32: 548–550. [DOI] [PubMed] [Google Scholar]