Lichen striatus is an uncommon, acquired and self-limiting inflammatory dermatosis that presents as small papules, which follows the Blaschko lines. It is considered as a cutaneous mosaicism and the interplay between genetic and environmental factors is postulated. The occasional appearance of lesions after trauma has been reported [1, 2]. Contrary to that, we present a case of lichen striatus in an adult woman in whom eruption disappeared after trauma. We believe it is an example of a rarely reported reverse Kőbner response and the first case of this phenomenon in lichen striatus.
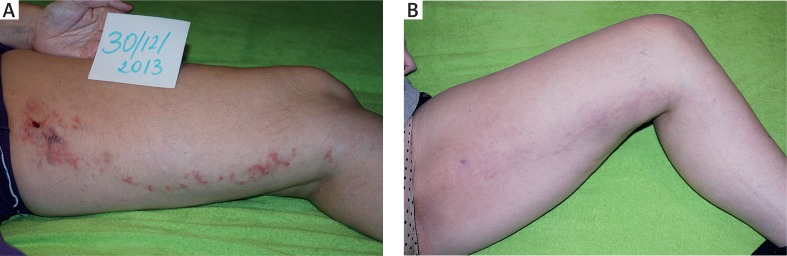
A 48-year-old Caucasian female presented with a 6-month history of linear papular eruption of her left lower extremity. The lesion appeared suddenly, initially on the thigh. Over a few weeks it had extended distally to involve the shank and the patient suffered from mild pruritus. On examination there was a linear lesion following Blaschko lines, extending from the proximal thigh to the distal shank which consisted of multiple, flat-topped, erythematous papules of a few millimeters in diameter with a scaly surface (Figure 1 A). The other areas of the skin as well as mucous membranes and nails were spared.
Figure 1.
Lichen striatus: A – the beginning clinical state with the visible biopsy area and underneath linear incisions with a scalpel, B – post-inflammatory hyperpigmentation and complete disappearance of lichen striatus 3 months after scalpel incisions
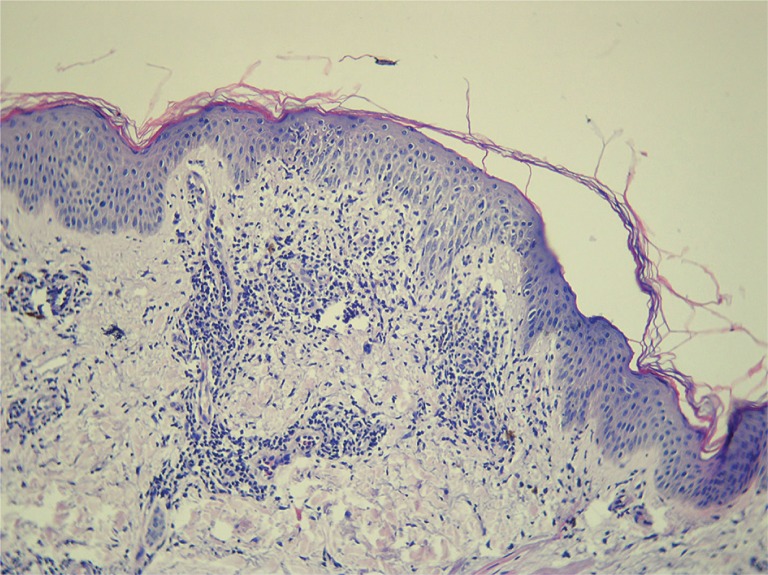
The biopsy of the lesional skin from the upper thigh was taken. Histopathology of a biopsy specimen revealed two papules: one composed of spongiotic epidermis with hydropic degeneration of the basal layer and lymphocytic exocytosis with a dense lymphocytic infiltrate in the papillary dermis containing a few melanophages (Figure 2), while the second papule composed of slightly thickened epidermis with interface changes, hyperkeratosis with focal parakeratosis and a cluster of necrotic keratinocytes in the upper layers with a mild inflammatory lymphocytic infiltrate underneath.
Figure 2.
Spongiotic epidermis with hydropic degeneration of the basal layer and lymphocytic exocytosis with a dense lymphocytic infiltrate in the papillary dermis containing a few melanophages (H + E, magnification 200×
Based on the clinical presentation and histopathological findings, a diagnosis of lichen striatus was made. The clobetasol propionate 0.05% ointment was recommended to be applied twice per day. Within 3–4 days after the biopsy the patient noticed disappearance of papules adjacent to the site of the biopsy. At the same time there was no improvement in another part of eruption. As our patient was a doctor (internist) she decided to incise a few next papules with a scalpel. After 2–3 weeks, the lesion cleared with pigmentation and within next 8–12 weeks the pigmentation disappeared completely (Figure 1 B). No recurrence during 3 years’ period of follow up was observed.
The exact etiology of lichen striatus remains unknown. It is believed to be a manifestation of cutaneous mosaicism. It is postulated that the clone of aberrant keratinocytes is attacked after contact with the triggering factor (mostly after viral infections) which affects previous tolerance [1]. The immunosuppressive effect of UV radiation was also suggested by Ciconte [3]. However cases presented by these authors may have been another example of trauma-induced lichen striatus as trauma has been reported as the triggering factor in lichen striatus as well [1, 2].
In our case the lesion disappeared after repeated trauma. Contrary to Kőbner phenomenon in which new eruptions typical of an existing dermatosis are observed at sites of injuries, such disappearance of the lesions after trauma is called reverse Kőbner response [4]. For the first time it was described in psoriatic patients [5]. According to Eyre et al., as many as 67% of patients suffering from plaque psoriasis undergoing trauma presented resolution of skin lesions. Those patients in whom reverse Kőbner response was observed had more stable disease and lower Psoriasis Area and Severity Index (PASI) than those with Kőbner phenomenon [6]. Casuistic reports on reverse Kőbner phenomenon in vitiligo [7, 8] and leukocytoclastic vasculitis were also published [9]. The skin biopsy provoked reverse Kőbner response in an interstitial variant of granuloma annulare [10].
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Shepherd V, Lun K, Strutton G. Lichen striatus in an adult following trauma. Australian J Dermatol. 2005;46:25–8. doi: 10.1111/j.1440-0960.2005.00132.x. [DOI] [PubMed] [Google Scholar]
- 2.Coto-Segura P, Costa-Romero M, Gonzalvo P, et al. Lichen striatus in an adult following trauma with central nail plate involvement and its dermoscopy features. Int J Dermatol. 2008;47:1324–5. doi: 10.1111/j.1365-4632.2008.03730.x. [DOI] [PubMed] [Google Scholar]
- 3.Ciconte A, Bekhor P. Lichen striatus following solarium exposure. Australian J Dermatol. 2007;48:99–101. doi: 10.1111/j.1440-0960.2007.00345.x. [DOI] [PubMed] [Google Scholar]
- 4.Kannangara AP, Yosipovitch G, Fleischer AB., Jr Proposed classification for Koebner, wolf isotopic, renbok, Koebner nonreaction, isotopic nonreaction and other related phenomen. Dermatol Online J. 2014;20 [PubMed] [Google Scholar]
- 5.Camargo CM, Brotas AM, Ramos-e-Silva M, et al. Isomorphic phenomenon of Koebner: facts and controversies. Clin Dermatol. 2013;31:741–9. doi: 10.1016/j.clindermatol.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 6.Eyre RW, Krueger GG. Response to injury of skin involved and uninvolved with psoriasis, and its relation to disease activity: Koebner and ‘reverse’ Koebner reactions. Br J Dermatol. 1982;106:153–9. doi: 10.1111/j.1365-2133.1982.tb00924.x. [DOI] [PubMed] [Google Scholar]
- 7.Malakar S, Dhar S. Spontaneous repigmentation of vitiligo patches distant from the autologous skin graft sites: a remote reverse Koebner’s phenomenon? Dermatology. 1998;197:274. doi: 10.1159/000018013. [DOI] [PubMed] [Google Scholar]
- 8.Laxmisha C, Kumari R, Thappa DM. Satellite repigmentation (remote reverse Koebner phenomenon) Dermatol Surg. 2006;32:596. doi: 10.1111/j.1524-4725.2006.32108.x. [DOI] [PubMed] [Google Scholar]
- 9.Yadav S, De D, Kanwar AJ. Reverse koebner phenomenon in leukocytoclastic vasculitis. Indian J Dermatol. 2011;56:598–9. doi: 10.4103/0019-5154.87169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naveen KN, Varadraj VP, Sharatchandra BA, et al. Remote reverse Koebner phenomenon in generalized granuloma annulare. Indian Dermatol Online J. 2014;5:219–21. doi: 10.4103/2229-5178.131137. [DOI] [PMC free article] [PubMed] [Google Scholar]