Abstract
BACKGROUND:
Tobacco use is the most modifiable risk factor that increases mortality rates worldwide. The World Health Organization stated in 2015 that around six million people die each year as a result of tobacco use. Most of these deaths are diagnosed as premature. This study assessed the level of knowledge, attitude and practices of smoking cessation counseling (SCC) of primary healthcare providers (PHCPs) in Saudi Arabia.
MATERIALS AND METHODS:
A cross-sectional study conducted from June 10, 2016 to March 31, 2017 in five Primary Healthcare Centers (PHC) of the Ministry of National Guard-Health Affairs, Jeddah, Western Region (WR). The study subjects were the staff physicians, family medicine doctors and dentists. Their selection was based on convenience sampling (N = 167, n = 130).
RESULTS:
More than half of the study participants (53.2%) were middle-aged. Most were family medicine residents (25.4%) and staff physicians (24.6). Fourteen physicians were smokers, only 8 (57.1%) of whom had tried to quit. The Internet was the main source of information on SSC (21.3%), followed by postgraduate studies (19.4%). The overall level of knowledge of SCC was poor with a mean score of 35.25 ± 18.40; the overall level of attitude was good with a mean score of 76.81 ± 8.63 and the overall level of practice was average, with a mean score of 55.23 ± 21.54. There was a significant association between position (consultant) and knowledge (P < 0.001), attitude (P < 0.001) and practice (P < 0.001).
CONCLUSION:
PHCPs' have poor knowledge of counseling on the cessation of smoking and their practices are unsatisfactory despite their positive attitude to this role. This affects the delivery of SCC to the patients. Postgraduate studies, workshops and training are indeed necessary to help PHCPs' to understand the significance of the role they play in implementing SCC for patients, individuals, family and the community effectively.
Keywords: Counseling, primary health-care providers, smoking cessation
Introduction
Tobacco use is the most modifiable risk factor that increases mortality rates worldwide.[1] According to the World Health Organization (2015), around six million people die every year as a result of tobacco use. Most of these deaths are seen as premature. Moreover, around 600,000 deaths are attributable to second-hand smoke.[2] One cigarette can be detrimental to all body systems, as it contains more than five thousand harmful chemicals.[3] Furthermore, smoking is part of the causal chain for many diseases.[4,5,6]
In Saudi Arabia, the prevalence of smoking in the population was found to be 12.1%, with obvious gender discrepancy between males (23.7%) and females (1.5%).[7] Overall, the prevalence of smoking has significantly increased in the past decade making the country one of the highest ten importers of cigarettes in the world.[8] Initiation of smoking occurs mainly during adolescence, and is significantly associated with male gender, stress and family members or friends who smoke.[9]
According to the Ministry of Health, Saudi smokers spend 690 million Saudi Riyals (SR) each year on cigarettes, with an average consumption of 15 billion cigarettes annually.[7,10] In addition, the health and economic burden as a result of smoking costs the kingdom up to 5 billion SR annually.[11]
Unfortunately, smoking is a difficult habit to break, as nicotine and other biogenic amines have addictive properties. Once they enter the body's circulation, they release dopamine and other neurotransmitters which play a significant role in improving attention, working memory, pleasure and mood enhancement.[12,13] When the level of these particles decline, smokers develop withdrawal symptoms represented by a wide range of negative impacts on different cognitive functions such as irritability, anxiety, lack of concentration, and restlessness.[12,14,15]
Primary healthcare providers (PHCPs) have a golden opportunity to help reduce the rate of smoking in those who smoke, via a feasible effective method of intervention represented through counseling. They are the first line of medical contact for a significant number of smokers. Therefore, they have an excellent opportunity to build rapport with them; understand their background and social context. Furthermore, smokers trust their doctors and consider them role models.[16,17] While evidence has shown that brief advice alone can increase quitting rates up to 3%, the recommended method of counseling represented by the “5 A's” (Ask about smoking status, Advise smokers to quit, Assess willingness to quit, Assist, and Arrange follow up after date of quitting) with pharmacological therapy can triple quit rates in smokers.[18,19,20,21]
The use of the stages of change (5 A's) has been advocated to standardize and streamline smoking cessation counseling (SCC). The stages of change offer clinicians a practical framework to classify current and former smokers and predict smoking abstinence at one year. Brief office encounters with these patients are patterned on the specific counseling advice of the 5 A's. A study conducted in the US found that in an outpatient setting, more than one-third of the patients hadn't been screened for tobacco use, and only one out of four smokers had any help to stop.[22] Doctors reported that the barriers in screening their patients for smoking habits and conducting proper counseling were the lack of time, the assumption that the patients had no motivation to stop, and lack of confidence in their knowledge and skills in cessation counseling.[23,24,25] A study of the knowledge and attitude of tobacco use and cessation in dental professionals reported that around 64% of general dental practitioners said they had had no training on the cessation of smoking during their undergraduate program.[26] Similarly, when asked about their knowledge and practice, more than a half of family physicians requested training to improve their skills in SCC.[27]
There is a dearth of national studies that assessed the knowledge, attitude and practice (KAP) of SCC of PHCPs.
The aim of this study was to assess the level of KAP of SCC of PHCPs in the Ministry of National Guard Primary Healthcare Centers-Western Region (MNG-PHC-WR), Saudi Arabia.
Materials and Methods
This was a cross-sectional study conducted between June 10, 2016, and March 31, 2017, at the MNG health affairs PHCs in the WR. The study subjects were the staff physicians, Family Medicine doctors and dentists working at the MNG-PHC-WR.
We began by purposefully selecting five PHCs to get a representative sample of three major cities in the WR, as follows: Jeddah City (Iskan Jeddah PHC; Specialized Poly Clinic PHC; and Bahra PHC); Taif City (Iskan Taif PHC); and Makkah City (Sharia PHC). In the next stage of sampling, the selection of respondents was based on convenience sampling out of total 167, 130 physicians were included in the study.
The data collection tool for this study was a semi- structured self-administered questionnaire of 36 items. It was adapted from the Eldein et al's. study, and[28] permission was obtained from the original authors for its use. The questionnaire had 3 domains: the first was socio-demographic data; the second included variables related to assessment of KAP of the study population about SCC; and the third comprised self-reported barriers to SCC. Since the original copy of the questionnaire had been modified, face validity of the modified study questionnaire had to be assessed by two expert supervisors, and a pilot study was conducted on 10 randomly selected PHC physicians of the above-mentioned 5 PHCs. The calculated inter-rater reliability of the modified instrument yielded a Chonbach's a of 0.88-0.92 in the KAPs scales and subscales, which indicated high reliability.
For each knowledge question, a correct response was assigned a score of “1,” and an incorrect response a score of “0.” The total knowledge score was obtained by adding the scores for all knowledge responses (range from 0 to 12). Then, an “overall knowledge percent score” was calculated by multiplying the total knowledge score for each participant by 100 and diving by 12.
Scores from 5 to 1 were assigned for attitude statements. Responses ranged from strongly agree to strongly disagree. A “strongly agree” response was assigned a score of “5” while a “strongly disagree” response was assigned a score of “1.” A total attitude score was obtained by adding the scores for all 7 attitude scores ranging from 7 to 35. Then, an “overall attitude percent score” was calculated by multiplying the total attitude score for each participant by 100 and dividing by 35.
For practice responses, a “never” response was assigned a score of “0,” “rarely” was assigned a score of “1,” a response of “sometimes” was assigned a score of “2” and a score of “3” was assigned to “always.” Therefore, the total practice score ranged from 0 to 30. Then, an “overall practice percent score” was calculated by multiplying the total practice score for each participant by 100 and dividing by 30.
Ethical approval from the Institutional Review Board/Ethics Committee of King Abdullah International Medical Research Center (KAIMRC) was obtained and informed written consent taken from all participants in the study.
The collected data was entered into a computer using the Statistical Package for the Social Sciences (IBM Corp., Released 2012, IBM SPSS Statistics for Windows, Version 21.0, Armonk, NY: IBM Corp) for statistical analysis. Descriptive statistics were calculated (including frequencies, percentages, means and standard deviations [SDS]). To test statistical significance, differences of KAP regarding demographic data, an independent t-test or analysis of variance was conducted. A two-sided P < 0.05 was used as a level of significance.
Results
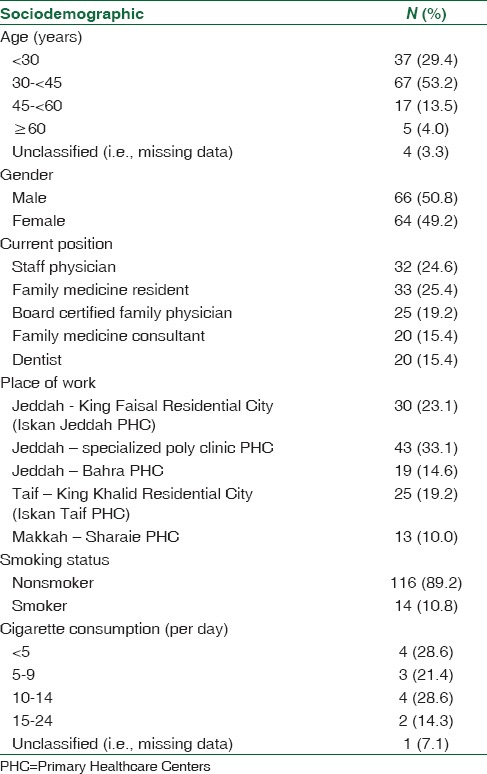
Of the 167 potential participants, 130 completed the questionnaires which represented a response rate of 77.8% of the total population of the study. They were at the mean age of 35.87 (±9.42). More than half (53.2%) of them were aged between 30 and 44 years and the distribution of males to females was almost equal, 50.8% males to 49.2% females. In terms of position, the majority were the Family Medicine residents (25.4%) and staff physicians (24.6%). Nonsmokers accounted for 89.2% while only 10.8% were smokers. Of the smokers (n = 14), the majority consumed <5 cigarettes per day (28.6%) and 10–14 cigarettes per day (28.6%). Detailed demographic data is shown in Table 1.
Table 1.
Sociodemographic characteristics of Ministry of National Guard Primary Healthcare Centers, Western Region providers (n=130)
More than half (57.1%) of those who smoked had already tried to quit smoking mainly because of health- related concerns (100%), family disapproval (62.5%), concerns about second hand smoke (12.5%), smoking bans or restrictions (12.5%) and warning on the labels (12.5%).
The participants had several sources of information for their knowledge of counseling patients on smoking cessation. The use of internet (21.3%) and postgraduate studies (19.4%) were reported as the main sources of information. The least reported sources of information were workshops (7.4%) and published research articles (7.6%).
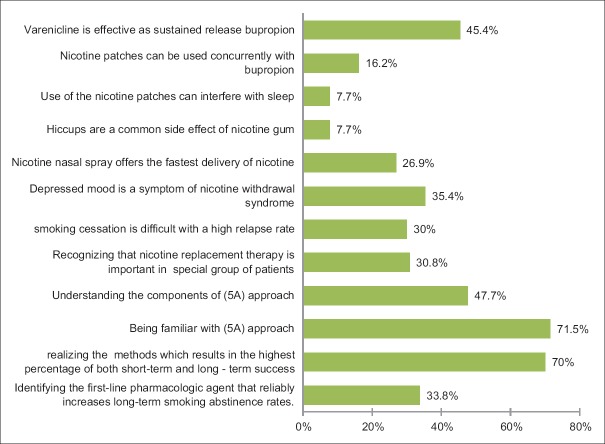
Figure 1 presented the percentages of the participants who responded correctly to the questions on SCC. “Being familiar with the 5A's approach” and “methods that result in the highest percentage of both short- and long-term success” (71.5%, and 70% respectively) were the 2 of the 12 items that were mostly answered correctly. However, when asked about what the “components of the 5A approach” were, less than half of them knew them. Such items as “hiccups are a common side effect of nicotine gum (7.7%)” and “use of the nicotine patches can interfere with sleep (7.7%)” were answered correctly by only a few.
Figure 1.
Knowledge of Ministry of National Guard-Primary Healthcare Centers-Western region providers regarding smoking cessation counseling (n= 130)
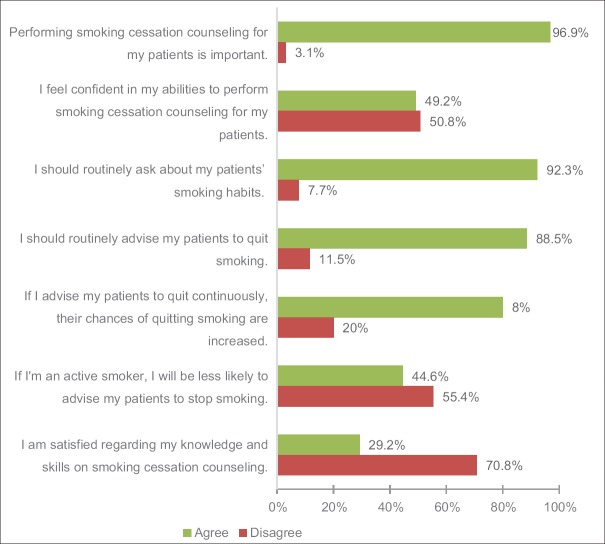
The participants' attitude towards counseling on smoking cessation is depicted in Figure 2. Most agreed that it was important to counsel the patients on the cessation of smoking (97%), by routinely asking patients about their smoking status and advising them to stop smoking (92.3% and 88.5% respectively). Conversely, more than half of the participants reported that they lacked the confidence to perform proper SCC. Moreover, around 71% of them were dissatisfied with their knowledge and skills.
Figure 2.
Attitude of Ministry of National Guard-Primary Healthcare Centers-Western region providers toward smoking cessation counseling (n = 130)
In terms of SCC practices, participants mostly performed SCC so as “to ask” and “to encourage” (47.7% and 46.9% respectively), while there were practices sometimes by participants “to document” (42.3%), “to update” (40%), “to explain” (44.6%), “to teach” (33.8) and “to discuss” (34.6%). However the following practices were rarely or never performed by participants: “to plan” (66.2%), “usage of pharmacological aids” (85.3%) and “follow up” (73.8%).
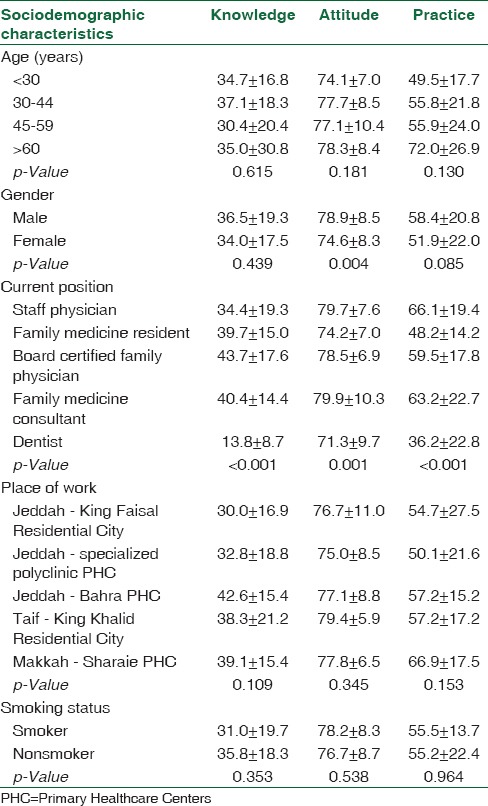
Overall, participants' percentage mean scores (mean ± SD) for SCC were 35.25 ± 18.40% for knowledge, 76.81 ± 8.63% for attitude and 55.23 ± 21.54% for practice. Table 2 presented the differences of the participants in terms of KAP based on their socio-demographic characteristics. Knowledge mean scores differed significantly amongst the participants according to their current position, with highest mean knowledge scores from Family Medicine consultants and lowest from the dentists (40.4 ± 14.4 and 13.8 ± 8.7, respectively, P < 0.001). However, there was no statistical significant difference in the participants' knowledge percentage scores by age, gender, place of work and smoking status. Participants' attitude scores were significantly higher in male than female participants (78.9 ± 8.5 and 74.6 ± 8.3, respectively, P = 0.004). Moreover, their mean scores differed significantly according to their current positions, with the highest scores from Family Medicine consultants and lowest mean scores from dentists (79.9 ± 10.3 and 71.3 ± 9.7, respectively, P = 0.001). However, participants' attitude percentage scores did not differ significantly by age groups, place of work or smoking status. Participants' practice mean percentage scores differed significantly according to their current position, the highest scores from staff physicians and lowest mean scores from dentists (66.1 ± 19.4 and 36.2 ± 22.8, respectively, P < 0.001). However, participants' practice percent scores did not differ significantly by age groups, gender, place of work or smoking status.
Table 2.
Participant’s knowledge, attitude and practice percentage scores (mean±standard deviation) according to their sociodemographic characteristics
Lastly, the barriers that hindered participants from performing SCC were the lack of training (21.8%), followed by the lack of time (20.8%), patients' reluctance to change (20%), frequent relapses and withdrawal symptoms (19.2%) and failure to follow-up (18.6).
Discussion
Despite the fact that Saudi Arabia does not grow tobacco or manufacture cigarettes, it is amongst the top ten countries that consume cigarettes and shisha the most, a feature that increases the economic and health burdens on the country.[29]
PHCPs are said to be in the first line of eradicating the habit of smoking.[30,31] However, it has been reported in studies in Germany and Saudi Arabia that about 24.0% to 31.7% of the representative population of physicians of both genders were smokers.[30] In contrast, only a few of our participants were smokers (10.8%). This very reassuring situation could be attributed to the fact that the physicians had a good level of knowledge and awareness of the adverse effects of smoking on their health.
The undergraduate medical curriculum did not have enough educational content on tobacco. Therefore, the Internet and books were most common source of information on counseling for smoking cessation.[30] In our study, other than the internet and books, postgraduate studies and undergraduate studies were found to be the other good sources of SCC information. It only goes to show that continuing education is essential in enhancing the knowledge of primary healthcare physicians', attitude and practice of effective implementation of SCC.
A study conducted in Riyadh by Jradi,[31] of PHC physicians and specialists of Family Medicine, reported that only a few physicians and specialists had used them although they were familiar with the clinical practice guidelines for SCC. Similar to our study, the majority stated that they rarely asked their patients about their smoking and encouraged them to quit. So were, prescribing medications or referring patients for further counseling. Based on these findings it is important to investigate all the barriers to the proper implementation of SCC.
Furthermore, a study in China in 2011, of Community Healthcare providers, reported that even with the positive attitude of the physicians towards SCC, the levels of knowledge and practice were inadequate.[32] This inadequacy could be improved by increasing the level of knowledge through training programs, and possible incentives for those physicians who implement these methods.
In contrast to our findings, the Al Madinah Al Munwarrah study reported that more than half of the physicians surveyed (60%) had good knowledge of SCC. They also reported that practice in some areas was adequate The physicians asked their patients about smoking, discussed the benefits of quitting with them, and encouraged them to quit by setting a target date, and arranged for follow up.[30]
Another study conducted in Riyadh in 2016 by AlAteeq et al., on PHC physicians with different specialties and educational levels, reported that around 75% of the participants had good attitudes and two-thirds had good practice. All the participants felt that giving their patients brief advice on cessation was part of their job, and the majority stated that having guidelines and special clinics for SCC motivated them to use these methods.[33] A possible explanation for that is that having specialized SCC clinics allowed them more time to discuss the different methods and techniques of stopping smoking with their patients as opposed to the restricted time in the general clinics. Furthermore, having a clear policy on the provision of SCC by the center would provide proper guidelines for practising physicians.
In our findings, consultants and Board Certified physicians had a significantly higher level of KAP than other participants. Additionally, male physicians had significantly more favorable attitude than females. Similar results were found in the Riyadh study of 2016, which reported that doctors with higher educational levels, those with more experience (>5 years) and those who were older (>40 years) had significantly better attitudes and good practices. Moreover, there was a significant association between good attitude and good practice. This association was, however, not exhibited in our study.[33]
Similarly, the Jradi study reported that there was a difference by gender in the practice of SCC. Male physicians tended to ask their patients about smoking more than female physicians did. Moreover, the rates of practice were higher with physicians who had more than ten years of experience and those who had attended a training program than others.[32]
A look at the relationship between the smoking status of the physicians and the practice of SCC, showed as in the German study of 2005 that being a smoker didn't significantly influence the role of the physician in counseling on cigarettes cessation.[23] Similar results were reported in the Al Madinah Al Munwarrah study, as well as in our current study.[30]
However, in a study conducted in Canada in 2010 on 610 General Practitioners (GPs), Meshefedjian et al. reported that smoking status of the physician influenced the role played in SCC; the rate of asking, advising and counseling patients by current smokers was lower than the rate by non-smokers and ex-smokers.[34]
Similarly, in a Syrian study conducted in 2011 of PHC providers from 7 randomly selected PHCs in Aleppo, Syria, Asfar et al. reported that smoking status of the physician influenced the KAP of SCC. Current smokers showed a significant lower level of KAP compared to non-smokers.[35]
Generally, the findings regarding the main barriers against SCC reported by almost all the studies were consistently the lack of training and time., These need to be looked into if there is to be an improvement.[23,30]
Conclusion
The level of knowledge on SCC of PHCPs' is unsatisfactory. Despite their positive attitude toward this role, their practices of SCC were inadequate. They were less satisfied with their level of knowledge and skills, which in turn had an effect on the delivery of SCC to the patients. Postgraduate studies, workshops and training are indeed necessary for the PHCPs to understand the significance of their role in the effective implementation of SCC for patients, individuals, families and the community.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, et al. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Report on the Global Tobacco Epidemic World Health Organization. 2015. [Last accessed on 2017 Aug 21]. Available from: http://www.who.int/tobacco/global_report/2015/en/
- 3.Talhout R, Schulz T, Florek E, van Benthem J, Wester P, Opperhuizen A, et al. Hazardous compounds in tobacco smoke. Int J Environ Res Public Health. 2011;8:613–28. doi: 10.3390/ijerph8020613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bjartveit K, Tverdal A. Health consequences of smoking 1-4 cigarettes per day. Tob Control. 2005;14:315–20. doi: 10.1136/tc.2005.011932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wahabi HA, Alzeidan RA, Fayed AA, Mandil A, Al-Shaikh G, Esmaeil SA, et al. Effects of secondhand smoke on the birth weight of term infants and the demographic profile of Saudi exposed women. BMC Public Health. 2013;13:341. doi: 10.1186/1471-2458-13-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Health Consequences of Smoking: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2004. [Google Scholar]
- 7.Saudi Health Interview Survey. Institute for Health Metrics and Evaluation. 2017. [Last accessed on 2017 Mar 20]. Available from: http://www.healthdata.org/sites/default/files/files/projects/KSA/smoking-ksa-findings-from-the-saudi-health-interview-survey.pdf .
- 8.World Health Organization. Guidelines for Controlling and Monitoring the Tobacco Epidemic. 1998. [Last accessed 2017 Sep 21]. Available from: http://www.apps.who.int/iris/handle/10665/42049 .
- 9.Fida HR, Abdelmoneim I. Prevalence of smoking among male secondary school students in Jeddah, Saudi Arabia. J Family Community Med. 2013;20:168–72. doi: 10.4103/2230-8229.121993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bassiony MM. Smoking in Saudi Arabia. Saudi Med J. 2009;30:876–81. [PubMed] [Google Scholar]
- 11.Al-Munif M. Report on Tobacco Control Program of Ministry of Health in Saudi Arabia. Ministry of Health Tobacco Control Program. 2009. [Last accessed on 2018 Aug 30]. Available from: http://www.sa-tcp.com/newsite/user/pdf/REPORT_ON_TCP.pdf .
- 12.Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362:2295–303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herman AI, Sofuoglu M. Cognitive effects of nicotine: Genetic moderators. Addict Biol. 2010;15:250–65. doi: 10.1111/j.1369-1600.2010.00213.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLaughlin I, Dani JA, De Biasi M. Nicotine withdrawal. Curr Top Behav Neurosci. 2015;24:99–123. doi: 10.1007/978-3-319-13482-6_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43:289–94. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- 16.Okuyemi KS, Nollen NL, Ahluwalia JS. Interventions to facilitate smoking cessation. Am Fam Physician. 2006;74:262–71. [PubMed] [Google Scholar]
- 17.Poon VH. Practice tips. Model for counseling people in relationships. Can Fam Physician. 2007;53:237–8. [PMC free article] [PubMed] [Google Scholar]
- 18.Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Treating Tobacco Use and Dependence: Clinical Practice Guideline. Rockville, MD: US Department of Health and Human Services; 2000. [Google Scholar]
- 19.U.S. Preventive Services Task Force. Counseling and interventions to prevent tobacco use and tobacco-caused disease in adults and pregnant women: U.S. Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2009;150:551–5. doi: 10.7326/0003-4819-150-8-200904210-00009. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. WHO Report on the Global Tobacco Epidemic, 2013: Enforcing Bans on Tobacco Advertising, Promotion and Sponsorship. World Health Organization. 2013 [Google Scholar]
- 21.Lancaster T, Stead L. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2004:CD000165. doi: 10.1002/14651858.CD000165.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Jamal A, Dube SR, Malarcher AM, Shaw L, Engstrom MC. Centers for Disease Control and Prevention (CDC). Tobacco use screening and counseling during physician office visits among adults – National Ambulatory Medical Care Survey and National Health Interview Survey, United States, 2005-2009. MMWR Suppl. 2012;61:38–45. [PubMed] [Google Scholar]
- 23.Ulbricht S, Meyer C, Schumann A, Rumpf HJ, Hapke U, John U, et al. Provision of smoking cessation counseling by general practitioners assisted by training and screening procedure. Patient Educ Couns. 2006;63:232–8. doi: 10.1016/j.pec.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Abdullah AS, Rahman AS, Suen CW, Wing LS, Ling LW, Mei LY, et al. Investigation of Hong Kong doctors' current knowledge, beliefs, attitudes, confidence and practices: Implications for the treatment of tobacco dependency. J Chin Med Assoc. 2006;69:461–71. doi: 10.1016/S1726-4901(09)70310-7. [DOI] [PubMed] [Google Scholar]
- 25.Vogt F, Hall S, Marteau TM. General practitioners' and family physicians' negative beliefs and attitudes towards discussing smoking cessation with patients: A systematic review. Addiction. 2005;100:1423–31. doi: 10.1111/j.1360-0443.2005.01221.x. [DOI] [PubMed] [Google Scholar]
- 26.Awan KH, Hammam MK, Warnakulasuriya S. Knowledge and attitude of tobacco use and cessation among dental professionals. Saudi Dent J. 2015;27:99–104. doi: 10.1016/j.sdentj.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eldein HN, Mansour NM, Mohamed SF. Knowledge, attitude and practice of family physicians regarding smoking cessation counseling in family practice centers, Suez Canal University, Egypt. J Family Med Prim Care. 2013;2:159–63. doi: 10.4103/2249-4863.117411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: Health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370:2044–53. doi: 10.1016/S0140-6736(07)61698-5. [DOI] [PubMed] [Google Scholar]
- 29.Al Nohair SF. Prevalence of smoking and its related behaviors and beliefs among secondary school students in Riyadh, Saudi Arabia. Int J Health Sci (Qassim) 2011;5:51–7. [PMC free article] [PubMed] [Google Scholar]
- 30.Surrati A, Alhazmi BH, Abass ZJ, Alahmary TA, Almohammadi MS. Knowledge and practice of smoking cessation among physicians in Madinah 2016. Int J Med Res Prof. 2017;3:27–33. [Google Scholar]
- 31.Jradi H. Awareness, practices, and barriers regarding smoking cessation treatment among physicians in Saudi Arabia. J Addict Dis. 2017;36:53–9. doi: 10.1080/10550887.2015.1116355. [DOI] [PubMed] [Google Scholar]
- 32.Klink K, Lin S, Elkin Z, Strigenz D, Liu S. Smoking cessation knowledge, attitudes, and practice among community health providers in China. Fam Med. 2011;43:198–200. [PubMed] [Google Scholar]
- 33.AlAteeq M, Alrashoud AM, Khair M, Salam M. Smoking cessation advice: The self-reported attitudes and practice of primary health care physicians in a military community, central Saudi Arabia. Patient Prefer Adherence. 2016;10:651–8. doi: 10.2147/PPA.S103010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meshefedjian GA, Gervais A, Tremblay M, Villeneuve D, O'Loughlin J. Physician smoking status may influence cessation counseling practices. Can J Public Health. 2010;101:290–3. doi: 10.1007/BF03405288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asfar T, Al-Ali R, Ward KD, Vander Weg MW, Maziak W. Are primary health care providers prepared to implement an anti-smoking program in Syria? Patient Educ Couns. 2011;85:201–5. doi: 10.1016/j.pec.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]