Abstract
Background and Objectives:
This study examined the relationship between distress tolerance and psychosocial changes among individuals participating in Mindfulness-Based Stress Reduction (MBSR). The objective of the analysis was to discern whether individuals with lower distress tolerance measured before MBSR showed larger reductions in perceived stress following MBSR.
Design and Methods:
Data were collected from a sample of convenience (n = 372) using a quasi-experimental design. Participants completed self-report measures immediately prior to course enrollment and following course completion.
Results:
Perceived stress, distress tolerance, and mood states showed favorable changes from pre- to post-MBSR in the current study. Baseline distress tolerance significantly moderated reductions on perceived stress, supporting the primary hypothesis that individuals with lower baseline distress tolerance evidenced a greater decline in perceived stress following MBSR. For a one-unit increase on the self-reported baseline Distress Tolerance Scale, reported perceived stress scores decreased by 2.5 units (p < .0001).
Conclusions:
The finding that individuals with lower baseline distress tolerance evidenced a greater decline in perceived stress may offer hints about who is most likely to benefit from MBSR and other mindfulness-based treatments. Identifying moderators of treatment outcomes may yield important benefits in matching individuals to treatments that are most likely to work for them.
Keywords: Distress tolerance, moderation, mindfulness-based stress reduction, MBSR
Introduction
Mindfulness has been defined as a psychological state of deliberate attention to the present moment, with an attitude of non-judgment (Kabat-Zinn, 1990). A non-judgmental attitude includes open curiosity and acceptance of one’s experience, including aversive and emotionally challenging experiences (Bishop et al., 2004). A substantial and growing body of research demonstrates that mindfulness training confers positive benefits for individuals suffering from a variety of medical and psychiatric conditions (Grossman, Niemann, Schmidt, & Walach, 2004), as well as for healthy individuals seeking a greater capacity to regulate day-to-day stress and anxiety (Academic Mindfulness Interest Group, 2006; Grossman et al., 2004). Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1982, 1990) is among the most commonly studied structured mindfulness-training programs. Empirical evidence has shown that MBSR is effective in ameliorating stress related to physical or psychosomatic illness in medical patients and is helpful in treating anxiety and mood disorders in clinical populations (Baer, 2003; Grossman et al., 2004, Hofmann, Sawyer, Witt, & Oh, 2010). While MBSR appears to be a largely beneficial training program, it is likely that not all participants benefit from the program. Surprisingly, little attention has been paid to examining individual differences that may moderate MBSR effectiveness, which could provide important information about whether certain individuals may be more or less responsive to mindfulness training.
The ability to tolerate distress is one individual difference that may moderate the effectiveness of mindfulness-based interventions. Distress tolerance has been defined as an individual’s capacity to experience and withstand challenging negative psychological states (Simons & Gaher, 2005). Individuals with low distress tolerance are thought to perceive emotional discomfort as unacceptable and to strive to find ways to attenuate any undesirable emotional or psychological experiences (Bliesner, 2010; Simons & Gaher, 2005). Moreover, individuals’ with low distress tolerance who strive and fail to attenuate their undesirable experiences are likely to further exacerbate their distress. Thus, if individuals with low distress tolerance can develop a non-judgmental acceptance of aversive or challenging physical and emotional experiences, their perception of stress may diminish. Not surprisingly, mindfulness training, including MBSR, has been hypothesized to be particularly helpful for individuals with low distress tolerance (Coffey & Hartman, 2008; Siegel, Germer, & Olendzki, 2008) due to a focus on fostering this quality in mindfulness programs (Bishop, 2002; Eifert & Heffner, 2003).
In fact, in a clinical sample of patients with a history of alcohol or drug (AOD) use, mindfulness-based relapse prevention (MBRP, Bowen et al., 2009) was superior to treatment as usual (TAU) and individuals with lower distress tolerance who received MBRP exhibited a greater reduction in AOD use days than those with low distress tolerance who received TAU (Hsu, Collins, & Marlatt, 2013). This finding suggests that distress tolerance is a particularly relevant treatment consideration and that mindfulness training may be well-suited to increase distress tolerance, at least among individuals struggling with problematic AOD use. However, extant empirical research is limited regarding the role that mindfulness training plays among those with low distress tolerance. Further elucidating the putative moderating role of distress tolerance on treatment outcome may help to identify those individuals who derive the greatest benefit from mindfulness-based approaches. Such information would contribute to the advancement of personalized medicine by facilitating a match between individual patients and treatments that are most likely to be effective for them. Thus, the primary purpose of the current study was to test the hypothesis that distress tolerance would moderate the effect of MBSR.
The study had two aims. First, we sought to replicate findings from other studies demonstrating that MBSR confers beneficial results. We hypothesized that perceived stress, distress tolerance, and mood states would improve from pre- to post-MBSR. Second, we hypothesized that baseline distress tolerance would moderate pre- to post-MBSR changes in perceived stress such that individuals with lower DTS scores at baseline would evidence greater reductions in perceived stress after MBSR. To our knowledge, no studies have examined self-reported distress tolerance prior to and following MBSR or the potentially moderating role of distress tolerance on stress reduction.
Material and method
Participants
Data were collected from a sample of convenience using a quasi-experimental design. Participants in this study were 372 individuals who completed an 8-week MBSR course between Fall 2005 and Winter 2012. Two hundred and fifty-nine participants completed all post-MBSR assessment measures while 113 failed to complete these measures, resulting in a 70% response rate. All participants were self-referred or referred by a clinician, physician, or friend. MBSR groups were, on average, comprised of 15 members (SD = 7.8) and ranged in size from 12 to 26. All participants expressing an interest in group enrollment completed a brief structured telephone screening questionnaire which is standard procedure for this MBSR setting. The purpose of the telephone screening was to assess appropriateness for group enrollment (i.e. participant’s potential to be disruptive to group procedures and/or make other participants feel unsafe) by evaluating, via participants’ self-reported response to yes/no questions, the presence of psychotic symptoms, suicidal ideation, homicidal ideation, and the participants’ willingness to participate in the group. Individuals were excluded from the group if they met any of the following criteria: (1) endorsed having psychotic symptoms, (2) endorsed suicidal ideation, (3) endorsed homicidal ideation, (4) indicated a clinical level of psychopathology and sought to use MBSR as a primary treatment, (5) indicated an overt unwillingness to complete the weekly homework assignments, and (6) indicated that they could only attend six or fewer MBSR groups. All participants who were excluded from group enrollment were provided with appropriate referrals. Thus, this sample is likely comprised of relatively healthy individuals looking to learn better ways to manage stress.
Data acquisition for this project was primarily for program improvement and evaluation. Individuals in MBSR groups assented to the completion of self-report measures prior to and following group participation, but did not provide written informed consent. De-identified data analysis for this project was determined by the Institutional Review Board of the University of Pennsylvania’s Perelman School of Medicine to be approved for publication. Limited demographic data were available for a broader array of individuals who participated in MBSR between Fall 2001 and Winter 2012. Based on these general data, group enrollees were primarily married (59%) with the mean age of group of enrollees being 48.9 (SD = 12.2). We anticipate a similar demographic make up for participants in the current study.
Procedures
MBSR.
MBSR groups were offered through a university hospital stress-management program modeled after the work of Jon Kabat-Zinn’s MBSR program (see Kabat-Zinn, 1994 for a detailed description of MBSR). MBSR classes were provided through a university-based stress-management program and were located in a variety of conference rooms and meeting rooms located across the Philadelphia metropolitan area. MBSR participants were taught to focus and regulate attention, to adopt a non-judgmental attitude, and to maintain awareness of present moment immediate experience. MBSR was delivered in 8 weekly, 150-minute, group sessions, and a 7-hour day-long, mostly silent, and meditation retreat. During MBSR sessions, individuals participated in didactic learning about mindfulness, received instruction and guidance in practicing mindfulness meditation, engaged in question and answer dialogues, and discussed their experiences with home-practice assignments (Kabat-Zinn, 1990). Group participation also entailed receiving and completing daily homework assignments that included listening to recorded guided meditations and engaging in activities aimed at fostering greater mindfulness in daily activities. Additional information about the MBSR session structure is presented in supplemental materials table.
Groups were led by facilitators with extensive training in MBSR. Prior to leading MBSR groups, all facilitators received extensive training in teaching mindfulness meditation and yoga, and all had received additional professional training to teach the structured MBSR curriculum. All facilitators had a minimum of a college degree, a minimum of 10 years of personal mindfulness practice, and at least 3 years of additional training in the delivery of MBSR. The professional background of facilitators included masters and doctoral level psychotherapists (n = 4), medically licensed physicians (n = 4), doctoral level professors and educators (n = 2), with some of the teachers also holding certi-fications as yoga instructors (n = 3).
Between 3 and 12 MBSR groups were run concurrently. All group facilitators administered the same content in the same week to ensure the consistency of information delivery between groups. MBSR program fidelity was maintained through weekly group supervision meetings where all facilitators met to discuss the content and delivery of information for a designated week. While MBSR is not a rigid protocol driven program, the course does designate specific topics and exercises be covered each week (Kabat-Zinn, 1990). Group facilitators introduced specific themes each week, lead pre-determined exercises, and administered handouts and homework assignments, which included listening to audio-recorded, guided meditations.
Assessment.
Pre- and post-treatment self-report measures were voluntarily completed by participants at the beginning of their first session and upon completion of their final (eighth) session of MBSR. Prior to the start of and after full completion of the MBSR program, group facilitators informed participants that, in order to evaluate the successful delivery of MBSR, they would be asked to evaluate their self-reported experience of stress. Participants were informed that their enrollment into MBSR was not contingent upon their completion of these pre–post self-report measures and that they had the option to not complete them. The overwhelming majority of participants completed all pre- and post-MBSR assessment measures. All self-report assessment materials were distributed and collected by a secretarial assistant prior to the close of the first and last sessions.
Measures
The Distress Tolerance Scale (DTS; Simons & Gaher, 2005) is a 15-item self-report measure designed to assess the extent to which one believes he or she can experience and withstand distressing emotional states. Respondents indicate the degrees of tolerance and acceptance of distressing emotions using a 5-point Likert-scale ranging from 1 (strongly agree) to 6 (strongly disagree), with higher scores suggesting higher tolerance for psychological distress. The DTS has evidenced good internal consistency, with Cronbach alpha coefficients reported between 0.72 and 0.82 (Simons & Gaher, 2005). Internal consistency in the current sample was good (Cronbach α = 0.93). During development of the scale (Simons & Gaher, 2005) four first-order factor subscales of the DTS were identified, including(1) Tolerance, (2) Appraisal, (3) Absorption, and (4) Regulation. However, follow-up examinations have used only a single higher order distress tolerance score from the four related sub-factors (Buckner, Keough, & Schmidt, 2007; Zvolensky et al., 2009). To inform the most appropriate strategy for scoring the DTS, we conducted an exploratory factor analysis (see “preliminary analyses”). The factor analysis yielded two factors “Aggregate” (combination of Tolerance, Absorption, and Appraisal items) and “Regulation”. In addition to the DTS total score, these two factors were used in final analyses.
The Perceived Stress Scale (PSS; Cohen, 1994) is a 10-item measure designed to assess the current perception of life stress and the degree to which one appraises situations as stressful. Respondents complete the measure by indicating the severity of each item using a 5-point scale (0 = never; 4 = very often), with higher scores reflecting greater overall perceived stress. The PSS is among the most widely used measures of perceived stress, associates with greater vulnerability to stressful life events, and has strong internal consistency with Cronbach α’s ranging from 0.84 to 0.86 (Cohen, Kamarch, & Mermelstein, 1983). Internal consistency was good in the present sample, (Cronbach α = 0.88).
The Profile of Mood States-Short Form (POMS-SF; McNair, Lorr, & Droppleman, 1992) is a commonly used self-report measure of affective states. It is comprised of six subscales: Anger, Confusion, Depression, Fatigue, Tension, and Vigor. Using a Likert-scale (0 = not at all, 4 = extremely), respondents indicate the extent to which they have experienced specific mood states in the past week. The POMSSF has evidenced good internal consistency (Tension: α = 0.86–0.88; Depression: α = 0.81–0.83; Anger: α = 0.87–0.89; Fatigue: α = 0.89–0.91; Confusion: α = 0.75–0.79; and Vigor: α = 0.89–0.90; Andrykowski et al., 1990; Baker et al., 1994). For the present study, Cronbach’s alpha measure of internal consistency were in the acceptable to good range for all POMS-SF subscales (Tension: α = 0.84; Depression: α = 0.84; Anger: α = 0.88; Fatigue: α = 0.91; Confusion: α = 0.70; and Vigor: α = 0.89).
Data analytic strategy
Our data analytic approach had three parts: (1) preliminary analyses to inform the scoring of the DTS,(2) tests of pre–post change in PSS, DTS, and POMS-SF, and (3) tests of distress tolerance as a moderator of pre–post change in PSS. Analyses were performed using the SAS version 9.3 statistical software package (SAS Institute, 2010, Car, NC).
Preliminary Analyses: Factor analysis of the DTS. Prior to hypothesis testing, exploratory factor analysis using principal axis factoring was conducted on baseline DTS in PASW 17. Varimax rotation was applied on the factors. Factors were selected if corresponding eigenvalues were greater than 1 and internal consistency was examined using Cronbach’s α. The rotated raw scores of the chosen factors were then examined as moderators of change in PSS in a generalized estimating equation (GEE) model run in SASv9.3.
Tests of pre–post change. Hypothesized pre–post differences on the DTS, PSS, and POMS were examined using two-tailed paired t-tests on available data.
Tests of distress tolerance as a moderator of pre–post change. To examine the moderating effect of baseline DTS on the pre–post change in PSS, a GEE model was applied with an exchangeable correlation matrix structure. The model included baseline DTS as a continuous predictor, time dummy coded with 0 for pre-measurement and 1 for post-measurement, and the interaction between the two. The significance of the interaction was determined by the Type 3 Score test. We interpreted a significant interaction as the change in PSS scores over time is dependent on the DTS baseline score; a significant interaction would indicate a dependency between the rate of change in PSS scores over time and the DTS baseline score.
Results
Preliminary analyses: factor analysis of the DTS
An examination of the Kaiser–Meyer–Olkin measure of sampling adequacy suggested that the sample was factorable (KMO = 0.938). Based on inspection of eigenvalues and the scree plot, two factors emerged from the baseline DTS. The eigenvalues for the first four factors were 7.47, 1.19,0.87, and 0.77. The two-factor solution accounted for 57.7% of the total variance and 52.3% of the common variance. Table 1 displays the factor score coefficients, loadings, and communalities after varimax rotation. Factor 1 is an aggregate of the Tolerance, Absorption, and Appraisal subscales of the DTS; all items loaded highly on factor 1 (>0.45) except Regulation items 8, 13, and 14. Internal consistency was high for these 12 items (α = 0.92). Factor 2 is mainly the Regulation subscale, with Items 8, 13 and 14 loading highly on Factor 2 (α = 0.79).
Table 1.
Factor score coefficients, loadings, and communities after varimax rotation.
| Score coefficients | Loadings | |||||
|---|---|---|---|---|---|---|
| Distress Tolerance Scale Item | Scale | Aggregate | Regulation | Aggregate | Regulation | Communality |
| 1. Feeling distressed or update is unbearable to me | Tolerance | 0.09 | 0.01 | 0.63 | 0.37 | 0.53 |
| 2. When 1 feel distressed or upset, all 1 can think about is how bad 1 feel | Absorption | 0.15 | −0.05 | 0.72 | 0.18 | 0.54 |
| 3. 1 can’t handle feeling distressed or upset | Tolerance | 0.22 | −0.07 | 0.76 | 0.31 | 0.68 |
| 4. My feelings of distress are so intense that they completely take over | Absorption | 0.26 | −0.15 | 0.79 | 0.21 | 0.66 |
| 5. There’s nothing worse than feeling distressed or upset | Tolerance | 0.02 | 0.06 | 0.49 | 0.45 | 0.43 |
| 6.1 can tolerate being distressed or upset as well as most people | Appraisal | 0.08 | −0.02 | 0.55 | 0.24 | 0.36 |
| 7. My feelings of distress or being upset are not acceptable | Appraisal | 0.07 | 0.02 | 0.54 | 0.28 | 0.37 |
| 8. I’ll do anything to avoid feeling distressed or upset | Regulation | −0.13 | 0.32 | 0.19 | 0.77 | 0.63 |
| 9. Other people seem to be able to tolerate feeling distressed or upset better than 1 can | Appraisal | 0.10 | −0.04 | 0.61 | 0.23 | 0.42 |
| 10. Being distressed or upset is always a major ordeal for me | Appraisal | 0.14 | 0.04 | 0.69 | 0.41 | 0.64 |
| 11.1 am ashamed of myself when I feel distressed or upset | Appraisal | 0.06 | 0.01 | 0.51 | 0.33 | 0.37 |
| 12. My feelings of distress or being upset scare me | Appraisal | 0.09 | −0.01 | 0.59 | 0.32 | 0.46 |
| 13. I’ll do anything to stop feeling distressed or upset | Regulation | −0.25 | 0.68 | 0.31 | 0.85 | 0.81 |
| 14. When I feel distressed or upset, I must do something about it immediately | Regulation | 0.01 | 0.07 | 0.38 | 0.48 | 0.37 |
| 15. When I feel distressed or upset I cannot help but concentrate on how bad the distress actually feels | Absorption | 0.15 | −0.04 | 0.70 | 0.31 | 0.58 |
Tests of pre–post change
Results were consistent with a-priori hypotheses that participants who completed MBSR would evidence improvements in distress tolerance, mood states, and perceived stress. Significant pre- to post-MBSR changes were observed on all measures, with increases on the DTS and decreases on the PSS and all sub-components of the POMS-SF (see Table 2). Effect sizes were calculated using the formula: d = mean (change score)/SD (change score) (Rosenthal, 1991) as this formula has been found to relate the correlation between time points (Cohen, 1988). Effect sizes were observed to be large for perceived stress (d = −1.12), and medium to large for distress tolerance (d = 0.62), POMS-Vigor (d = 0.68), POMS-Tension (d = −0.73), POMS-Fatigue (d = −0.72), POMS-Depression (d = −0.62), POMS-Anger (d = −0.59), and POMS-Confusion (d = −0.55).
Table 2.
Paired comparisons of pre- and post-measurements.
| Pre | Post | Difference (Post-Pre) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | N | Mean | SD | Mean | SD | Mean | SD | 95% Cl | t | df | Cohen’s d | p-Value | |
| DTS | 268 | 3.3 | 0.9 | 3.8 | 0.6 | 0.5 | 0.8 | 0.4 | 0.6 | 10.2 | 267 | 0.62 | <.0001 |
| Absorption | 269 | 3.1 | 1.2 | 3.7 | 0.9 | 0.7 | 1.1 | 0.5 | 0.8 | 10.0 | 268 | 0.61 | <.0001 |
| Appraisal | 269 | 3.3 | 1.0 | 3.5 | 0.7 | 0.2 | 0.9 | 0.0 | 0.3 | 2.7 | 268 | 0.16 | .0000 |
| Regulation | 268 | 3.4 | 1.1 | 3.8 | 0.9 | 0.5 | 1.0 | 0.4 | 0.6 | 8.1 | 267 | 0.49 | <.0001 |
| Tolerance | 269 | 3.5 | 1.0 | 4.1 | 0.8 | 0.6 | 0.9 | 0.5 | 0.7 | 11.4 | 268 | 0.70 | <.0001 |
| PSS | 258 | 20.3 | 7.0 | 13.6 | 5.4 | −6.7 | 6.0 | −7.4 | −6.0 | −18.0 | 257 | −1.12 | <.0001 |
| POMS | |||||||||||||
| Anger | 263 | 5.1 | 3.8 | 3.0 | 2.6 | −2.1 | 3.5 | −2.5 | −1.6 | −9.5 | 262 | −0.59 | <.0001 |
| Confusion | 260 | 5.6 | 3.2 | 4.0 | 2.4 | −1.7 | 3.0 | −2.0 | −1.3 | −8.9 | 259 | −0.55 | <.0001 |
| Depression | 267 | 5.6 | 4.2 | 3.3 | 3.2 | −2.3 | 3.8 | −2.8 | −1.9 | −10.1 | 266 | −0.62 | <.0001 |
| Fatigue | 261 | 8.3 | 4.9 | 4.9 | 3.9 | −3.3 | 4.6 | −3.9 | −2.8 | −11.7 | 260 | −0.72 | <.0001 |
| Tension | 267 | 7.4 | 4.0 | 4.7 | 2.9 | −2.7 | 3.8 | −3.2 | −2.3 | −11.9 | 266 | −0.73 | <.0001 |
| Vigor | 259 | 8.0 | 3.8 | 10.6 | 4.0 | 2.6 | 3.8 | 2.1 | 3.1 | 11.0 | 258 | 0.68 | <.0001 |
Notes: DTS = Distress Tolerance Scale (Simons & Gaher, 2005); PSS = Perceived Stress Scale (Cohen, 1994); POMS-SF = Profile of Mood States-Short Form (McNair, Lorr, & Droppleman, 1992).
Testing moderation
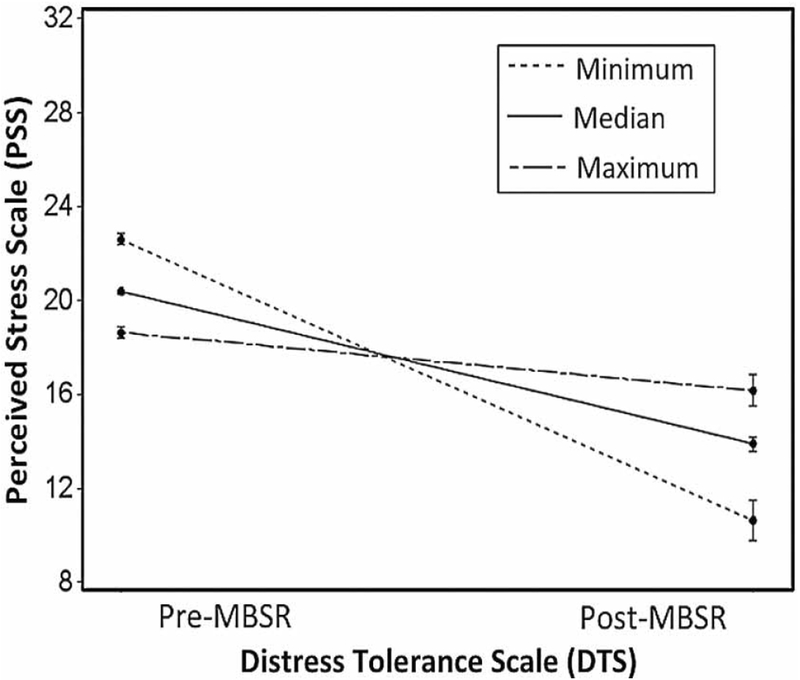
There was a significant interaction between baseline DTS total score and change in PSS from pre-MBSR to post-MBSR measurement, indicating that higher baseline DTS scores were associated with smaller changes in PSS scores. Specifically, for every one-unit increase in DTS, the PSS score decreased by 2.5 (SE = 0.37, 95%CI[1.78,3.25], χ2(1) = 33.2, p < .0001). Controlling for baseline PSS scores in the model did not significantly change the results (see Figure 1).
Figure 1.
Perceived stress reduction moderated by distress tolerance.
In order to determine whether DTS sub-factors differentially effected moderation analysis, the two factors that emerged from our psychometric testing of the DTS were also assessed to evaluate the moderating effects of distress tolerance. There was a significant interaction between the Aggregate factor (Tolerance, Absorption, and Appraisal) and change in PSS, with smaller change in PSS associated with higher factor scores. For every one-unit increase in the Aggregate factor score, the PSS score decreased by 2.4 (SE = 0.36, 95%CI[1.63, 3.11], χ2(1) = 30.7, p < .0001). There was a signifi-cant main effect of the Regulation factor score (β = −3.97, SE = 0.33, 95%CI[−4.61, −3.33], χ2(1) = 78.1, p < .0001), indicating that high Regulation factor scores were associated with lower PSS scores in general.
Discussion
Results of the current study are consistent with the growing literature that supports the use of MBSR to improve individuals’ abilities to manage stress such that distress tolerance, perceived stress, and mood states evidenced pre- to post-MBSR improvements. Results of this study support our primary hypothesis that baseline distress tolerance would moderate improvements in perceived stress. Individuals with lower distress tolerance experienced greater reductions in perceived stress. This finding lends support to prior speculations about the relation between mindfulness training and distress tolerance and may help to identify individuals who might experience greater benefit from participation in MBSR. The identification of individuals that would derive greater benefit from a particular treatment permits patient-treatment matching. Although the sample evaluated was not from a psychiatric population, taken in conjunction with the findings of Hsu et al. (2013), our data suggest that the benefits of mindfulness training are linked with distress tolerance such that those who have lower distress tolerance may find that mindfulness training is particularly beneficial.
Interestingly, examination of the DTS revealed two factors, one aggregate factor comprised of the Absorption, Appraisal, and Tolerance subscales and a second comprised of the DTS-Regulation sub-scale. Moderation analysis on both subscales revealed that only the aggregate DTS factor was significant. Participants low in DTS-Regulation did not show significant moderating effects, suggesting that the key components of distress tolerance, according to Simons and Gaher’s (2005) model, are Absorption, Appraisal, and Tolerance. Although the DTS-Regulation factor improved from pre- to post-MBSR, this construct did not have a significant moderating effect on perceived stress. It has been proposed that the regulation component of the DTS reflects an individual’s intentions to alleviate distress through regulatory acts (e.g. “When I feel distressed or upset I must do something about it immediately”; Simons & Gaher, 2005). The fact that DTS-Regulation was not a moderator may reflect the importance of mindfulness in helping individuals to appraise stress as being acceptable (Appraisal), volitionally direct attention away from stress in the moment (Absorption), and perceive that they can better tolerate stress when it occurs (Tolerance).
Certain considerations should be kept in mind when interpreting the findings. While we observed change to occur from pre- to post-MBSR, our lack of a control group precludes causal inference. Follow-up data subsequent to the completion of MBSR was not collected, precluding the examination of whether improvements in PSS, DTS, and POMS were sustained following completion of MBSR (e.g. 6 months post-MBSR). Data collection was for quality assurance and improvement and systematic data acquisition of demographic variables took second priority to clinical emphasis. Thus, demographic variables are not adequately available for further analysis of how age, sex, education, race, and marital status may moderate changes in perceived stress. Data were also not collected on between-session home practice of formal mindfulness exercises (e.g. body scan; sitting meditation), which has been shown to be an important correlate of improvement following MBSR (Carmody & Baer, 2008). While outside the scope of this study, the lack of clinical interviews and psychological assessments measures precludes the possibility of assessing how psychiatric diagnoses modulates the relationship between distress tolerance and MBSR. Participants enrolled in and paid for the course of their own volition and may therefore represent a biased population that was invested in learning stress reduction techniques and had the financial means to do so. Additionally, although MBSR practitioners received extensive training prior to facilitating groups, we have no objective measures of facilitator adherence to MBSR principles or protocols. The lack of a systematic and objective measure of MBSR program fidelity constitutes an additional limitation.
Despite these considerations, the findings are consistent with the notion that mindfulness training is particularly beneficial for individuals with low distress tolerance. To our knowledge, this is the first study that examined the moderating role of distress tolerance on MBSR outcome. Future research should expand the treatment focus to larger, more heterogeneous populations and do so using a randomized controlled trial designs. Future studies should also examine the moderating effects of distress tolerance on other treatments and whether providing a specific mindfulness-training component prior to treatment confers greater response to behavioral interventions for psychiatric disorders. For example, MBSR may be a good prelude to more difficult exposure-based interventions such as Prolonged Exposure (Rapgay et al., 2014), as MBSR provides preliminary training that cultivates one’s awareness of avoidance tendencies and fosters a greater capacity to approach and tolerate avoided aversive emotional states.
Acknowledgements
This paper was prepared with partial support of the VISN 4 Mental Illness Research, Education, and Clinical Center, Philadelphia Veterans Affairs Medical Center, Philadelphia, PA. The paper does not necessarily represent the position or opinions of the Department of Veterans Affairs, and those opinions expressed are the sole responsibility of the authors. The authors would like to acknowledge and thank Elliott Sturgis Berkowitz for his help in the data organization necessary for the production of this manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplemental data
Supplemental data for this article can be accessed at 10.1080/10615806.2015.1085513
References
- Academic Mindfulness Interest Group. (2006). Mindfulness-based psychotherapies: A review of conceptual foundations, empirical evidence and practical considerations. Australian and New Zealand Journal of Psychiatry, 40(4), 285–294. doi: 10.1111/j.1440-1614.2006.01794.x [DOI] [PubMed] [Google Scholar]
- Andrykowski MA, Altmaier EM, Barnett RL, Otis ML, Gingrich R, & Henslee-Downey PJ (1990). The quality of life in adult survivors of allogeneic bone marrow transplantation: Correlates and comparison with matched renal transplant recipients. Transplantation, 50(3), 399–405. [DOI] [PubMed] [Google Scholar]
- Baer R (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology:Science and Practice, 10(2), 125–143. doi: 10.1093/clipsy/bpg015 [DOI] [Google Scholar]
- Baker F, Wingard JR, Curbow B, Zabora J, Jodrey D, Fogarty L, & Legro M (1994). Quality of life of bone marrow transplant long-term survivors. Bone Marrow Transplantation, 13(5), 589–596. [PubMed] [Google Scholar]
- Bishop SR (2002). What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine, 64(1),71–83. PMID: . [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson LE, Anderson ND, Carmody J, Devins G (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241. doi: 10.1093/clipsy/bph077 [DOI] [Google Scholar]
- Bliesner AE (2010). Mindfulness and distress tolerance: A review of the literature. (Unpublished master’s thesis). Pacific University, Forest Grove, Oregon. [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu SH, Grow J, Marlatt A (2009). Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Substance Abuse, 30(4), 295–305. doi: 10.1080/08897070903250084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Keough ME, & Schmidt NB (2007). Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addictive Behaviors, 32(9), 1957–1963. doi: 10.1016/j.addbeh.2006.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmody J, & Baer RA (2008). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine, 31(1), 23–33. [DOI] [PubMed] [Google Scholar]
- Coffey KA, & Hartman M (2008). Mechanisms of action in the inverse relationship between mindfulness and psychological distress. Complementary Health Practice Review, 13(2), 79–91. doi: 10.1177/1533210108316307 [DOI] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. New York, NY: Routledge Academic. [Google Scholar]
- Cohen S (1994). Perceived Stress Scale. Mind Garden. Retrieved from http://www.mindgarden.com
- Cohen S, Kamarch T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. doi: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Eifert GH, & Heffner M (2003). The effects of acceptance versus control contexts on avoidance of panic-related symptoms. Journal of Behavior Therapy and Experimental Psychiatry, 34(3), 293–312. doi: 10.1016/j.jbtep.2003.11.001 [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, & Walach H (2004). Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research, 57(1), 35–43. doi: 10.1016/S0022-3999(03)00573-7 [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, & Oh D (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. doi: 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu SH, Collins SE, & Marlatt AG (2013). Examining psychometric properties of distress tolerance and its moderation of mindfulness-based relapse prevention effects on alcohol and other drug use outcomes. Addictive Behaviors, 38, 1852–1858. doi: 10.1016/j.addbeh.2012.11.002 [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. doi: 10.1016/0163-8343(82)90026-3 [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Dell Publishing, 295. [Google Scholar]
- Kabat-Zinn J (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York: Hyperion. [Google Scholar]
- McNair DM, Lorr M, & Droppleman LF (1992). EdITS manual for the Profile of Mood States, revised 1992. San Diego, CA, EdITS/Educational and Industrial Testing Service. [Google Scholar]
- Rapgay L, Ross JL, Petersen O, Izquierdo C, Harms M, Hawa S, Couper G (2014). A proposed protocol integrating classical mindfulness with prolonged exposure therapy to treat posttraumatic stress disorder. Mindfulness, 5(6), 742–755. [Google Scholar]
- Rosenthal R (1991). Meta-analytic procedures for social research (Rev. ed.). Newbury Park, CA: Sage. [Google Scholar]
- SAS Institute Inc. (2010). SAS/GRAPH ® 9.2 reference (2nd ed.). Cary, NC: Author. [Google Scholar]
- Siegel RD, Germer CK, & Olendzki A (2008). Mindfulness: What is it? Where did it come from? In Didonna F (Ed.),Clinical handbook of mindfulness (pp. 17–36). New York, NY: Springer. [Google Scholar]
- Simons JS, & Gaher RM (2005). The distress tolerance scale: Development and validation of a self-report measure.Motivation and Emotion, 29(2), 83–102. doi: 10.1007/s11031-005-7955-3 [DOI] [Google Scholar]
- Zvolensky MJ, Marshall EC, Johnson K, Hogan J, Bernstein A, & Bonn-Miller MO (2009). Relations between anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations to coping and conformity marijuana use motives among young adult marijuana users. Experimental and Clinical Psychopharmacology, 17(1), 31. doi: 10.1037/a0014961 [DOI] [PMC free article] [PubMed] [Google Scholar]