Abstract
Background
Prolonged neck flexion during smartphone use is known as a factor of neck pain and alteration of neck muscle activity. Studies on the effects of shoulder taping on neck discomfort and neck muscle responses while texting on a smartphone are still lacking. The aim of this study was to examine the effects of shoulder taping on neck discomfort using a numerical rating scale, and neck muscle activity and fatigue using a surface electromyography during a texting task on a touchscreen smartphone.
Methods
Twenty-five healthy adolescents used the dominant hand to perform a 30-minute texting task using a touchscreen smartphone at two separate times under one of the following two conditions: taping across the upper trapezius muscle and no taping. Neck discomfort, normalized root mean square, and normalized median frequency slopes for upper trapezius, cervical erector spinae, and sternocleidomastoid muscles were recorded.
Results
The results revealed that shoulder taping provided significantly lower neck discomfort than no taping (p < 0.001). However, shoulder taping did not significantly alter normalized root mean square and normalized median frequency slope values of all muscles when compared with no taping controls.
Conclusion
Shoulder taping reduces neck discomfort but does not affect neck muscle activity and fatigue while texting on a touchscreen smartphone.
Keywords: Muscle activity, Muscle fatigue, Neck discomfort, Shoulder taping, Smartphone
1. Introduction
A touchscreen smartphone is now an essential handheld communication device in humans' daily life and work. For 2016, it has been forecasted that the number of touchscreen smartphone users worldwide will reach 2.08 billion [1]. Thais are among the highest smartphone users in the Association of Southeast Asian Nations (ASEAN), and the number is estimated to reach 20 million in 2016 and it continues to grow [2]. Touchscreen smartphones offer advanced 3G and 4G features and capability such as voice communication, social networking, and text messaging [3]. Rainie [4] reported that most US users do text messaging and e-mailing on smartphones. Smartphone owners spend an average of 2.7 hours daily on their phone [5]. Use of a smartphone for prolonged periods possibly increases the risk of orthopedic problems such as neck and shoulder pain [6], [7], [8].
Texting on smartphone devices involves looking down at the device and touching the touchscreen display, which may contribute to sustained awkward head posture, repetitive movements, and workplace stress [9], [10], [11]. Forward head flexion posture produces excessive external flexion force, resulting in a larger load on neck extensors and adjacent connective tissues of the neck [12]. Increased activities of neck muscles, particularly cervical erector spinae (CES) and upper trapezius (UT), while texting on a smartphone has been reported previously [10], [11], [13], [14]. These muscles represent the major muscles for counterbalancing external forces and stabilizing neck and shoulder regions [15]. Prolonged contraction of these neck muscles in such a posture has been proposed as a cause of increased neck muscle fatigue [10], [16]. A high level of neck muscle fatigue caused by sustained smartphone use for a long time may increase pain eventually [17], [18]. A recent study conducted by Yang et al [19] revealed the association between musculoskeletal discomfort and the duration of smartphone ancillary function use.
Numerous interventions such as electromyographic (EMG) and mechanomyographic biofeedback have been suggested to improve neck muscle activity for the prevention of neck–shoulder complaints during texting tasks [20]. The application of taping across the UT muscle with tension in the tape or shoulder taping, which is performed perpendicular to the UT fibers, is another possible intervention [18], [21], [22], [23]. Although the mechanisms underlying shoulder taping are still ambiguous, the taping is thought to increase mechanical stability of neck and shoulder regions and offload adjacent soft tissues [21], [23]. A few studies have examined the effects of shoulder adhesive taping on neuromuscular responses [18], [21], but these findings are controversial. Takasaki and colleagues [18] investigated the effects of tensioned taping across the UT muscle on UT activity during 15-minute typing task, and they found that tensioned taping reduced UT activity, while another study failed to find any effects of shoulder taping on UT activity [21].
To date, research into the effects of shoulder taping on neck muscle activity and fatigue as well as neck discomfort during prolonged texting on a smartphone is still lacking. As there is an increasing extensive use of touchscreen smartphones by adolescents, it will be of considerable benefit to examine neck muscle responses in that population. Therefore, the purpose of this study was to investigate the shoulder taping effects during texting task using a smartphone on neck discomfort, and neck activity and fatigue in healthy adolescents. It was hypothesized that participants receiving shoulder taping may present lower neck discomfort (H1), lower neck muscle activity (H2), and lower neck muscle fatigue (H3) than those with no taping.
2. Materials and methods
2.1. Study design
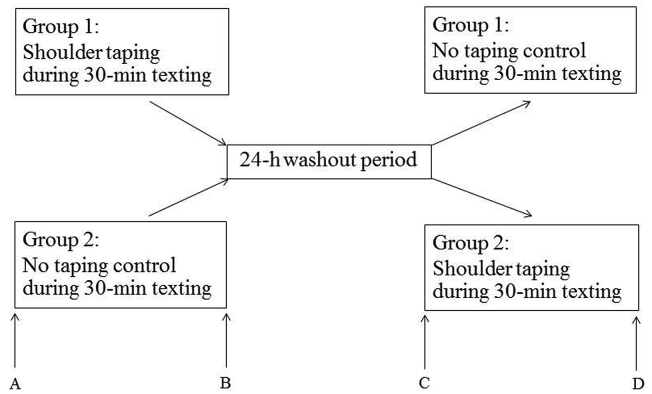
This study was an assessor-blinded randomized crossover trial with two conditions (shoulder taping and no taping controls) conducted in the Physical Therapy Laboratory at Mae Fah Luang University. Each participant participated in two sessions separated by at least 24 hours to wash out the contamination effect on the outcome measures of the previous session, according to the method described by Jones et al [24]. The order of condition was randomized across participants using a simple randomization method (Fig. 1).
Fig. 1.
Protocol of the study. Assessments were performed at the start and end of each intervention period. The letters A, B, C, and D represent assessment time points.
2.2. Participants
Twenty-five healthy Thai adolescents (19 women and 6 men) were recruited via advertising in Chiang Rai city, Thailand, from October 2015 to March 2016. Participants had a mean age of 20.8 ± 1.5 years, mean experience in smartphone use of 4.4 ± 1.5 years, and mean daily use of smartphones of 8.4 ± 6.2 hours. Participants preferred to use the dominant hand in one-handed texting in the initial examination (19 right-handed and 6 left-handed). A medical doctor who was unaware of the study protocol screened the participants using medical history, clinical examination, and radiography. None of the participants reported musculoskeletal disorders such as disc herniation, scoliosis, cervical spondylolisthesis, rheumatoid arthritis, neck and shoulder muscle strain, ligament sprain or other connective tissue diseases of the neck–shoulder region, neurological deficits (numbness, or loss of sensation or muscle weakness in the neck and upper limbs), or recent neck, shoulder, and/or upper limb surgery. In addition, participants with a history of allergic reactions to rigid tape were excluded. Eligible participants signed an informed consent form before the start of the study. The study was approved by the Ethics Committee for Human Research at Mae Fah Luang University, Thailand (REH-59056), which was in accordance with the Declaration of Helsinki.
2.3. Experimental procedures
2.3.1. Randomization
Participants chose a card with the order of the two conditions from a sealed opaque envelope, which was used for the purpose of concealed allocation. The randomization procedure was managed by the researcher (K.O.) who was unaware of the condition procedure. The assessor (S.T.) was blinded to the two conditions. This was achieved by covering the shoulder during each data collection period. In addition, the EMG data were coded by a researcher (Y.H.) to maintain blinding of the assessor for the purpose of analysis.
2.3.2. Intervention protocols
The participants who participated in both shoulder taping and nontaping conditions had the texting task using the smartphone. For the shoulder taping condition, the researcher (P.A.) who was a physiotherapist and experienced in manual therapy applied the taping on the shoulder of the dominant arm without disturbing the surface electrode attachment, as suggested by Takasaki et al [18]. A 2-inch-wide rigid tape (Neoplast Inc., Pathum Thani, Thailand) was attached from midclavicle across the muscle bundle of the UT to the level of the seventh rib posteriorly. The tension force of taping was 2 kg, measured by a spring scale [18]. For the nontaping condition, the participants did not receive taping on the shoulder.
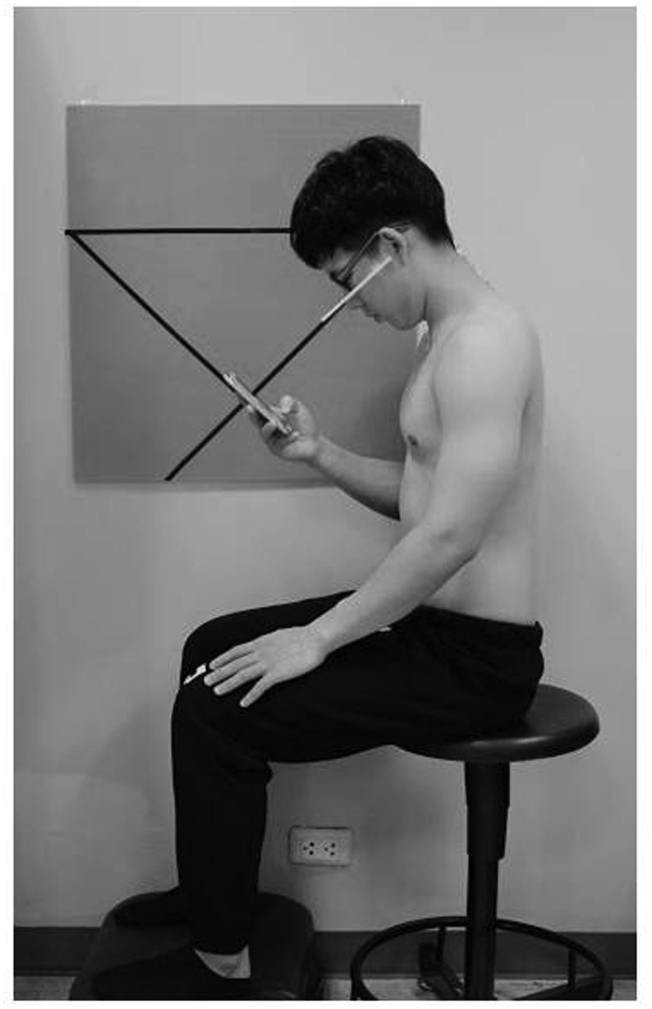
The texting task was performed using the iPhone 5S smartphone (Apple Inc., California, USA), which was technically invented to have the following features: 112 g of weight and a 4-inch touchscreen with QWERTY keyboard format. The participants were instructed distinctly for texting procedures until they performed the procedures correctly before the real intervention was started, and the device was also steady set for texting prior to the start of the experiment. Prior to the start of texting, participants were rested in a supine lying position for 10 minutes. For the position of tasking, they were made to sit on a height-adjustable stool coupled with neck flexion of 45°, trunk erection, hip and knee flexion of 90°, and feet resting on the floor. Their arms were kept close to the trunk, dominant elbow was bended, and the smartphone was held with the dominant hand while the nondominant hand was placed on the thigh. The distance between the eyes and the smartphone was approximately 30 cm. In the tasking procedures, participants were asked to communicate with a research assistant by texting the answers of 100 yes/no binary questions via Line chatting program (Line Cooperation, Tokyo, Japan). During the task, participants were always investigated for correct neck flexion of 45° by attaching evaluating tubes at the left side of their face linked to their nose, as illustrated in Fig. 2.
Fig. 2.
Texting on a touchscreen smartphone in a seated position.
2.3.3. Outcome measures
All outcome measures were collected through 30-minute texting task. To minimize the diurnal variation of muscle activity and fatigue, all measurements were performed at the same time of the day.
The primary outcome measure was neck discomfort, which referred to the symptom of discomfort between the neck and the shoulder of the dominant arm. Neck discomfort was reported by the participants via texting on the touchscreen smartphone. Neck discomfort was measured using an 11-point (0–10) numerical rating scale (NRS), where 0 represents no discomfort and 10 represents the worst discomfort [25].
The secondary outcome measures included normalized root mean square (NRMS) for muscle activity measurement and normalized median frequency slope (NMFslope) for muscle fatigue measurement measured by a surface electromyography. The EMG setting of a Biopac MP 35 surface EMG system (Biopac, Goleta, CA, USA) was followed a protocol stated previously [25]. The skin over the areas of the UT muscle to be taped, CES, and sternocleidomastoid (SCM) muscles was cleaned with alcohol, and hair was removed when necessary in order to reduce skin impedance to <5 kΩ. Marking on transparency sheets with a chemical pencil was used to ensure correct repositioning of the electrodes on Day 2. For the UT muscle, electrodes were attached at approximately 20% medial to the midpoint between the C7 spinous process and the tip of acromion process [26]. For the CES muscle, the electrodes were attached at the level of the C4 spinous process, on the most bulky part of the CES muscle during resisted neck extension [27]. For the SCM muscle, the electrodes were attached at the midpoint of SCM length from the mastoid process to the suprasternal notch [28]. Three ground electrodes were placed over the C7 spinous process, C4 spinous process, and the acromion process for the UT, CES, and SCM muscles, respectively. Surface electrodes and amplifiers were connected via snap leads for signal transferring.
For the normalization of root mean square (RMS), the maximum voluntary isometric contraction (MVIC) of the UT, CES, and SCM muscles of the dominant arm was measured using the manual muscle test, as described by previous researches [29], [30]. Each MVIC test of each muscle was performed for 5 seconds three times, and the average of the three readings of the middle 3rd seconds was used for normalization. A 30-second rest period between MVIC trials was provided to prevent muscle fatigue [30]. The RMS of those muscles at the starting and end point of texting task was calculated and expressed as the percentage of the MVIC. The normalized RMS (NRMS) represents muscle activity.
For normalization of median frequency slope (MFslope), a fast Fourier transform was applied with 1-second data epochs (including 1,000 data points) used to calculate the signal spectrum [31]. All MF data were normalized by initial MF values at rest. The MF values were plotted over 30 minutes, and linear regression analysis was applied to the normalized MF observations (1,800) during 30-minute texting task in order to determine the MFslope. The NMFslope was referred to the MFslope divided by the initial MF value and presented as percent per second. A steeper NMFslope represents more muscle fatigue. A decrease in NMFslope during an isometric contraction is an indicator of myoelectric muscle fatigue [32]. The possible influences of distance between the EMG electrodes on the MFslope can be diminished by the method of MF normalization [33].
2.3.4. Statistical analysis
SPSS version 16.0 for Windows (SPSS Inc., Chicago, IL, USA) was employed for all statistical analyses. Shapiro–Wilk's test reported that the data of NRS rating neck discomfort and NRMS of all muscles met the normality assumption for parametric tests. Levine's test revealed that those outcome measures met the assumption of constant variance. The data were continuously analyzed using a two-way analysis of variance, with group and time as the independent variables. If a significant group × time interaction effect was presented, pairwise comparisons were employed to evaluate differences between the groups for each time.
An independent t test was then used to compare the data of NMFslope between groups. An independent t test was also employed to compare all data of outcome measures at the initial period between groups. The level of statistical significance was set at an alpha level of 0.05.
Prior to data collection, the within-assessor reliability of the EMG MVIC measurements of the UT, CES, and SCM muscles was assessed on 10 participants by testing each participant three times with 30-second rest between the measurements. The intraclass correlation coefficient [ICC(1,1)] was calculated, and good to excellent reliability of the UT [ICC(1,1) = 0.91], CES [ICC(1,1) = 0.94], and SCM [ICC(1,1) = 0.82] muscles was found.
3. Results
The independent t test showed no significant differences of NRS, NRMS, and NMFslope between groups at baseline (p > 0.05; Fig. 1, Fig. 2, Fig. 3, Fig. 4).
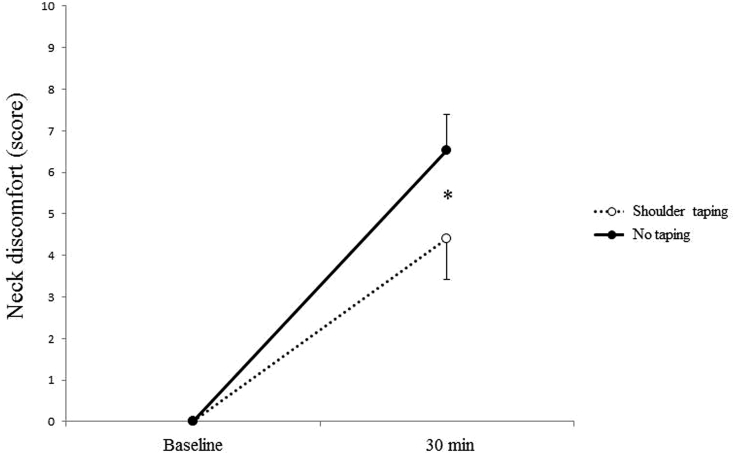
Fig. 3.
Means and standard deviation of neck discomfort measured by a numerical rating scale for shoulder taping (dash line) and no taping (solid line) conditions while texting on a touchscreen smartphone (n = 25). * p < 0.001.
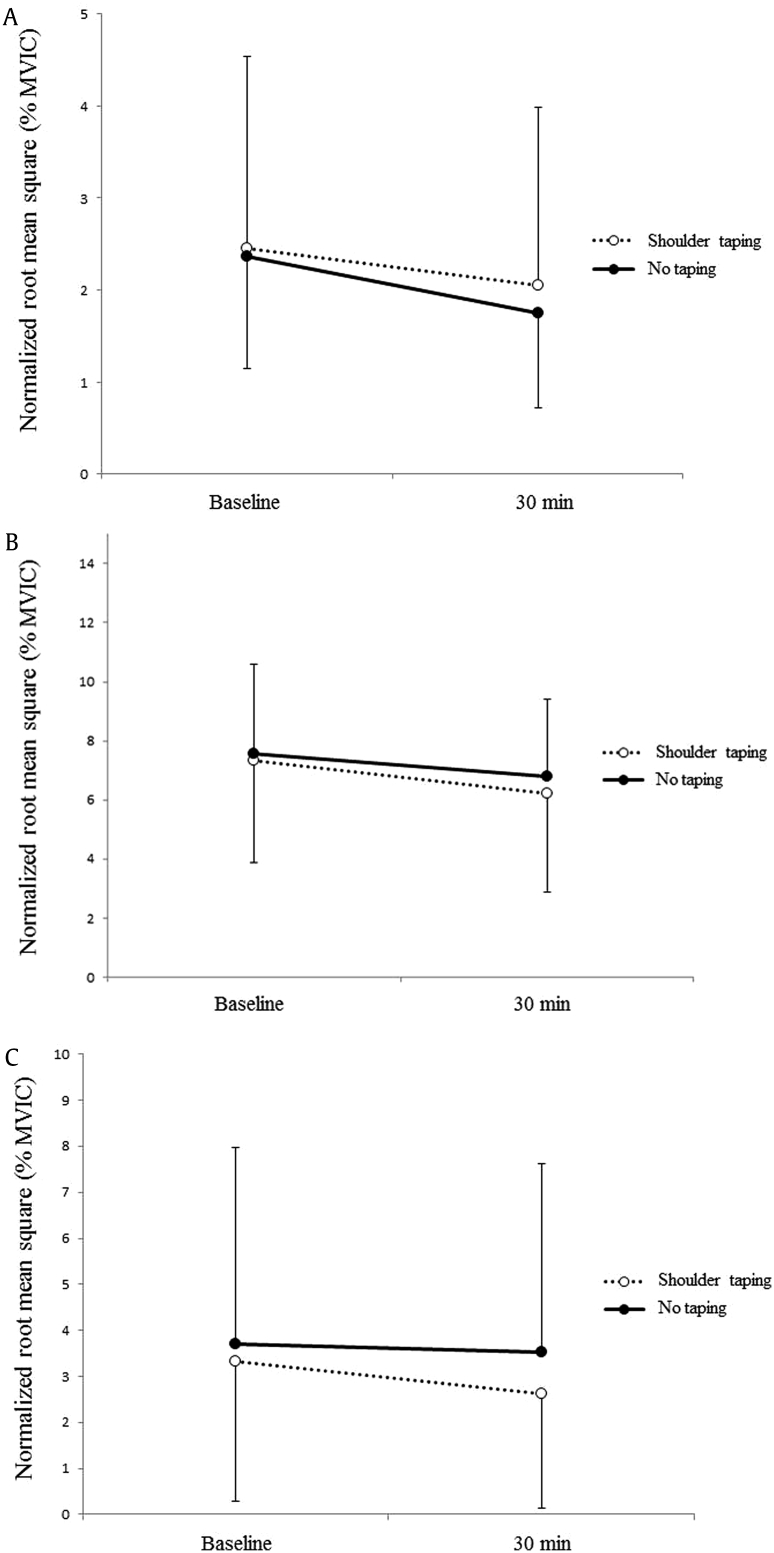
Fig. 4.
Means and standard deviation of normalized root mean square of (A) upper trapezius, (B) cervical erector spinae, and (C) sternocleidomastoid, measured by surface electromyography for shoulder taping (dash line) and no taping (solid line) conditions while texting on a touchscreen smartphone (n = 25). MVIC, maximum voluntary isometric contraction.
Results from two-way analysis of variance showed a statistically significant group × time interaction effect on the NRS rating neck discomfort [F(1,96) = 22.06, p < 0.001]. Pairwise comparisons demonstrated shoulder taping to produce significantly lower neck discomfort than no taping [mean difference = 2.12 ± 0.45, 95% confidence interval (95% CI) = 1.21–3.03, p < 0.001 at 30 minutes of intervention period; Fig. 3]. Significant group × time interaction effect on NRMS of the UT [F(1,96) = 0.11, p = 0.74], CES [F(1,96) = 0.07, p = 0.79], and SCM [F(1,96) = 0.14, p = 0.71; Figs. 4A–C] muscles was not seen.
The independent t test revealed no significant difference on NMFslope of the UT [t(48) = –0.75, p = 0.46], CES [t(48) = –0.46, p = 0.65], and SCM [t(48) = –0.34, p = 0.73] muscles between the conditions. The mean differences in NMFslope were as follows: –0.32 ± 0.43, 95% CI = –1.17 to 0.54, p = 0.46 for the UT muscle; –0.16 ± 0.35, 95% CI = –0.86 to 0.54, p = 0.65 for the CES muscle; and –0.10 ± 0.29, 95% CI = –0.69 to 0.49, p = 0.73 for the SCM muscle.
4. Discussion
The purpose of the present study was to investigate the effects of shoulder taping on neck discomfort, and muscle activity and fatigue of the UT, CES, and SCM muscles while texting on a touchscreen smartphone for 30 minutes. The findings of this study showed that nonelastic shoulder taping across the UT muscle of the dominant arm resulted in lower NRS ratings for neck discomfort than that of the no taping condition. This finding supported H1. Results failed to demonstrate the differences between two conditions on NRMS and NMFslope responses of the UT, CES, and SCM muscles at 30-minute texting period. These results were not consistent with H2 and H3, respectively. On the basis of these findings, it appears that shoulder taping provides more comfortable sensation on the neck than no taping. However, shoulder taping does not alter activity and fatigue of all muscles when compared with the no taping condition.
In the present study, while texting on a touchscreen smartphone, 45° of neck flexion was maintained, which may have caused more mechanical disadvantage of neck extensors compared with the erect neck–head posture [12]. Previous studies suggested that forward flexed posture of the neck during texting on smartphone devices is a more vulnerable factor than the neck upright neutral posture [9], [10], [11]. The flexed posture may produce excessive external flexion force, and alter length–tension relationships and moment arm lengths of the muscles, resulting in a larger load on neck extensors and adjacent connective tissues of the neck [12]. The neck muscles may have to increase their activities to stabilize the neck in such a task and become fatigued after prolonged contraction [10], [11], [13], [14]. The results of this study revealed no significant difference in RMS activity in the UT muscle based on the application of shoulder taping. There was no change in CES and SCM muscle activities because the taping may not have influenced the adjacent muscles around the taping site. It is consistent with the study of Cools and colleagues [21] in terms of no significant change on UT activity. Although nonelastic taping during static posture may provide mechanical support to the adjacent joints near the taping site, it may provide only nonsignificant subtle change in muscle activity beneath the taping location [34]. In contrast to the present findings, Takasaki and colleagues [18] who examined the effect of nonelastic taping across the UT muscle on UT muscle activity during a 15-minute typing task on a computer reported that UT taping technique reduced EMG activity of the UT muscle when compared with the no taping condition. Although the technique of tape application in the present study was similar to that in the study of Takasaki and colleagues [18], the difference in the findings may be attributed to the dissimilar methodology, especially the task condition (a typing task on a computer in a previous study versus a texting task on a touchscreen smartphone in the present study) and the duration of task (15 minutes in the previous study and 30 minutes in the present study), making comparison difficult. Previous studies claimed that longer time of the smartphone task possibly reduces more neck muscle activities and increases their fatigue than the shorter time [7], [18].
Taping across muscle belly is thought to decrease muscle activity via the proposed sensory and mechanical mechanisms. While applying taping, cutaneous intravenous nociceptors would be stimulated and their impulses would result in an underlying muscle inhibition response via local inhibitory interneuron in the spinal cord [35]. From a mechanical aspect, it is speculated that taping applied in such a fashion causes muscle lengthening, decreased actin and myosin overlap, and decreased cross-bridge ability to generate muscle force [36]. However, the findings of the present study do not support the proposed mechanisms. All participants who received shoulder taping reported moderate tension on the skin over the shoulder area but not intense pain. Moreover, they also felt more stable at their shoulder during taping. Previous study claimed that little or moderate tension on the skin during applying taping may not sufficiently stimulate type intravenous nociceptors or modify the length of muscle [21]. However, the influence of taping across the muscle belly on sensory modification and alteration of muscle length should be systematically investigated.
Results revealed that NMFslope for the UT, CES, and SCM muscles were not different between shoulder taping and no taping conditions. Generally, muscle fatigue results from a task that requires sustained muscle contraction in static posture or repeated movements, and a steeper NMFslope of the muscle indicates more muscle fatigue [16], [25]. Previous studies proposed a relationship between alterations of muscle activity and muscle fatigue [36], [37]. Hence, nonsignificant differences of UT, CES, and SCM activities between shoulder taping and no taping conditions may result in unchanged fatigue of those muscles.
Shoulder taping provided a result of lower neck discomfort compared with no taping. Although the actual mechanisms to explain the neck discomfort relieving effect of shoulder taping are still unclear, it may be speculated that tension of the tape may play a role in decreasing discomfort. Our participants who received shoulder taping reported only moderate tension on the skin, which may facilitate cutaneous mechanoreceptors and diminish the nociceptive impulses via pain inhibitory mechanism of the gate control theory to reduce participants' discomfort [38], [39].
There were a number of strengths of this study. First, this study was of a randomized crossover controlled trial with blinded assessment to eliminate measurement bias. This study design is commonly used in clinical trials to reduce confounding factors such as age and sex [40]. This study also provided an adequate washout period of baseline outcome measures such as neck discomfort (a 0 score for baseline values of both groups). In our knowledge, this is the first study to show the effect of shoulder taping on neck muscle activity and fatigue, and neck discomfort during prolonged texting on a touchscreen smartphone. There are, however, some limitations in this study. First, this study did not measure the responses of upper limb or trunk EMG activity and fatigue during the texting task; therefore, further studies should be conducted to explore this effect. Second, we investigated the EMG responses and discomfort during texting on a smartphone and cannot generalize the results to other activities; additional research is needed on activities such as watching videos, searching the Internet, or playing games on a smartphone. Third, adolescents were recruited in this study and may not be representative of other populations. Future studies should explore the effects of shoulder taping in individuals of other age groups such as children, working people, or the elderly. Fourth, we acknowledge that the findings of this study cannot describe the effects of shoulder taping in other symptomatic persons such as patients with neck pain. Finally, as the study did not have a randomized controlled trial (RCT) which is the goal standard of the true experimental study, future studies using RCTs are required to strengthen the evidence, and long-term effect of shoulder taping should be further investigated in order to fulfill the knowledge in this field.
In conclusion, the findings of this study revealed that shoulder taping can reduce neck discomfort, but did not change EMG activities and fatigue of neck muscles in healthy adolescents while texting on a touchscreen smartphone. These can be used as evidence for the therapist to take into account before applying shoulder taping to smartphone users. Future studies should examine the effect of shoulder taping on people with neck pain, and should compare this intervention with other methods such as EMG biofeedback in terms of reducing work-related neck discomfort and muscle responses.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Acknowledgments
The authors would like to thank all the participants for their best cooperation. In addition, the authors are grateful to Dr Mitra Cassely for proofreading.
References
- 1.Statista. Number of Smartphone Users Worldwide from 2014 to 2019 [Internet]. 2016a [cited 2016 Jun 17]. Available from: http://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/.
- 2.Statista. Number of Smartphone Users in Thailand from 2013 to 2019 [Internet]. 2016b [cited 2016 Jun 17]. Available from: http://www.statista.com/statistics/467191/forecast-of-smartphone-users-in-thailand/.
- 3.Bian M., Leung L. Linking loneliness, shyness, smartphone addiction symptoms, and patterns of smartphone use to social capital. Soc Sci Comput Rev. 2014;33:61–79. [Google Scholar]
- 4.Rainie L. Vol. 5. 2010. (Internet, broadband, and cell phone statistics). Pew Internet & American Life Project. [Google Scholar]
- 5.Fogg B., Hreha J. Proceeding of Persuasive. 2010. Behavior wizard: a method for matching target behaviors with solutions; pp. 117–131. [Google Scholar]
- 6.Berolo S., Wells R.P., Amick B.C. Musculoskeletal symptoms among mobile hand-held device users and their relationship to device use: a preliminary study in a Canadian university population. Appl Ergon. 2011;42:371–378. doi: 10.1016/j.apergo.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Kim G.Y., Auh C.S., Jeon H.W., Lee C.R. Effects of the use of smartphones on pain and muscle fatigue in the upper extremity. J Phys Ther Sci. 2012;24:1255–1258. [Google Scholar]
- 8.Korpinen L., Pääkkönen R., Gobba F. Self-reported neck symptoms and use of personal computers, laptops and cell phones among Finns aged 18–65. Ergonomics. 2013;56:1134–1146. doi: 10.1080/00140139.2013.802018. [DOI] [PubMed] [Google Scholar]
- 9.Gold J.E., Driban J.B., Yingling V.R., Komaroff E. Characterization of posture and comfort in laptop users in non-desk settings. Appl Ergon. 2012;43:392–399. doi: 10.1016/j.apergo.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 10.Lee S., Kang H., Shin G. Head flexion angle while using a smartphone. Ergonomics. 2015;58:220–226. doi: 10.1080/00140139.2014.967311. [DOI] [PubMed] [Google Scholar]
- 11.Xie Y., Szeto G.P.Y., Dai J., Madeleine P. A comparison of muscle activity in using touchscreen smartphone among young people with and without chronic neck-shoulder pain. Ergonomics. 2016;59:61–72. doi: 10.1080/00140139.2015.1056237. [DOI] [PubMed] [Google Scholar]
- 12.Bonney R.A., Corlett E.N. Head posture and loading of the cervical spine. Appl Ergon. 2002;33:415–417. doi: 10.1016/s0003-6870(02)00036-4. [DOI] [PubMed] [Google Scholar]
- 13.Kietrys D.M., Gerg M.J., Dropkin J., Gold J.E. Mobile input device type, texting style, and screen size influence upper extremity and trapezius muscle activity, and cervical posture while texting. Appl Ergon. 2015;50:98–104. doi: 10.1016/j.apergo.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Ning X., Huang Y., Hu B., Nimbarte A.D. Neck kinematics and muscle activity during mobile device operations. Int J Ind Ergon. 2015;48:10–15. [Google Scholar]
- 15.Zhang F.R., He L.H., Wu S.S., Li J.Y., Ye K.P., Wang S. Quantify workload and muscle functional activation patterns in neck-shoulder muscles of female sewing machine operators using surface electromyogram. Chin Med J. 2011;124:3731–3737. [PubMed] [Google Scholar]
- 16.Kim H.J., Kim J.S. The relationship between smartphone use and subjective musculoskeletal symptoms and university students. J Phys Ther Sci. 2015;27:575–579. doi: 10.1589/jpts.27.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szeto G.P., Straker L.M., O'Sullivan P.B. Examining the low, high and range measures of muscle activity amplitudes in symptomatic and asymptomatic computer users performing typing and mousing tasks. Eur J Appl Physiol. 2009;106:243–251. doi: 10.1007/s00421-009-1019-4. [DOI] [PubMed] [Google Scholar]
- 18.Takasaki H., Delbridge B.M., Johnston V. Taping across the upper trapezius muscle reduces activity during a standardized typing task—an assessor-blinded randomized cross-over study. J Electromyogr Kinesiol. 2015;25:115–120. doi: 10.1016/j.jelekin.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Yang S.Y., Chen M.D., Huang Y.C., Lin C.Y., Chang C.H. Association between smartphone use and musculoskeletal discomfort in adolescent students. J Commun Health. 2017;42:423–430. doi: 10.1007/s10900-016-0271-x. [DOI] [PubMed] [Google Scholar]
- 20.Madeleine P., Vedsted P., Blangsted A.K., SjØgaard G., SjØgaard K. Effects of electromyographic and mechanomyographic biofeedback on upper trapezius muscle activity during standardized computer work. Ergonomics. 2006;49:921–933. doi: 10.1080/00140130600665828. [DOI] [PubMed] [Google Scholar]
- 21.Cools A.M., Witvrouw E.E., Danneels L.A., Cambier D.C. Does taping influence electromyographic muscle activity in the scapular rotators in healthy shoulders? Man Ther. 2002;7:154–162. doi: 10.1054/math.2002.0464. [DOI] [PubMed] [Google Scholar]
- 22.Morin G.E., Tiberio D., Austin G. The effect of upper trapezius taping on electromyographic activity in the upper and middle trapezius region. J Sport Rehabil. 1997;6:309–318. [Google Scholar]
- 23.Morrissey D. Proprioceptive shoulder taping. J Bodyw Mov Ther. 2000;4:189–194. [Google Scholar]
- 24.Jones D., Round J., de Haan A. Churchill Livingstone; London (UK): 2004. Skeletal muscle from molecules to movement. [Google Scholar]
- 25.Areeudomwong P., Puntumetakul R., Kaber D.B., Wanpen S., Leelayuwat N., Chatchawan U. Effects of handicraft sitting postures on lower trunk muscle fatigue. Ergonomics. 2012;55:693–703. doi: 10.1080/00140139.2012.658086. [DOI] [PubMed] [Google Scholar]
- 26.Samani A., Holtermann A., Søgaard K., Madeleine P. Effects of eccentric exercise on trapezius electromyography during computer work with active and passive pauses. Clin Biomech. 2009;24:619–625. doi: 10.1016/j.clinbiomech.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 27.Gosselin G., Rassoulian H., Brown I. Effects of neck extensor muscles fatigue on balance. Clin Biomech. 2004;19:473–479. doi: 10.1016/j.clinbiomech.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 28.Pallegama R.W., Ranasinghe A.W., Weerasinghe V.S., Sitheeque M.A. Influence of masticatory muscle pain on electromyographic activities of cervical muscles in patients with myogenous temporomandibular disorders. J Oral Rehabil. 2004;31:423–429. doi: 10.1111/j.1365-2842.2004.01266.x. [DOI] [PubMed] [Google Scholar]
- 29.Ekstrom R.A., Soderberg G.L., Donatelli R.A. Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. J Electromyogr Kinesiol. 2005;15:418–428. doi: 10.1016/j.jelekin.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 30.Yoon T.L., Kim K.S., Cynn H.S. Slow expiration reduces sternocleidomastoid activity and increases transversus abdominis and internal oblique muscle activity during abdominal curl-up. J Electromyogr Kinesiol. 2014;24:228–232. doi: 10.1016/j.jelekin.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Stulen F.B., De Luca C.J. Frequency parameters of the myoelectric signal as a measure of muscle conduction velocity. IEEE Trans Biomed Eng. 1981;28:515–523. doi: 10.1109/TBME.1981.324738. [DOI] [PubMed] [Google Scholar]
- 32.Farina D., Gazzoni M., Merletti R. Assessment of low back muscle fatigue by surface EMG signal analysis: methodological aspects. J Electromyogr Kinesiol. 2003;13:319–332. doi: 10.1016/s1050-6411(03)00040-3. [DOI] [PubMed] [Google Scholar]
- 33.Greig A.M., Bennell K.L., Briggs A.M., Hodges P.W. Postural taping decreases thoracic kyphosis but does not influence trunk muscle electromyographic activity or balance in women with osteoporosis. Man Ther. 2008;13:249–257. doi: 10.1016/j.math.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 34.Tobin S., Robinson G. The effect of McConnell's vastus lateralis inhibition taping technique on vastus lateralis and vastus medialis oblique activity. Physiotherapy. 2000;86:173–183. [Google Scholar]
- 35.Maganaris C.N. Force–length characteristics of in vivo human skeletal muscle. Acta Physiol Scand. 2001;172:279–285. doi: 10.1046/j.1365-201x.2001.00799.x. [DOI] [PubMed] [Google Scholar]
- 36.Dolan P., Adams M.A. Repetitive lifting tasks fatigue the back muscles and increase the bending moment acting on the lumbar spine. J Biomech. 1998;31:713–721. doi: 10.1016/s0021-9290(98)00086-4. [DOI] [PubMed] [Google Scholar]
- 37.Sparto P.J., Parnianpour M., Reinsel T.E., Simon S. The effect of fatigue on multijoint kinematics and load sharing during a repetitive lifting test. Spine. 1997;22:2647–2654. doi: 10.1097/00007632-199711150-00013. [DOI] [PubMed] [Google Scholar]
- 38.Kneeshaw D. Shoulder taping in the clinical setting. J Bodyw Move Ther. 2002;6:2–8. [Google Scholar]
- 39.Williams S., Whatman C., Hume P.A., Sheerin K. Kinesio taping in treatment and prevention of sports injuries. Sports Med. 2012;42:153–164. doi: 10.2165/11594960-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 40.Wellek S., Blettner M. On the proper use of the crossover design in clinical trials. Dtsch Arztebl Int. 2012;109:276–281. doi: 10.3238/arztebl.2012.0276. [DOI] [PMC free article] [PubMed] [Google Scholar]