Abstract
Introduction:
This pilot study tested the efficacy of a bicycling intervention targeting inactive, low-income, overweight adults on reducing perceived barriers to bicycling, increasing physical activity, and improving health.
Methods:
A nonblinded 2-site randomized controlled trial was conducted in Milwaukee, Wisconsin, in summer 2015. Participants included members from 1 largely Latino community and a second primarily African American neighborhood. A certified bicycling instructor led a 12-week bicycling intervention. Outcome measures including biking-related attitudes, self-reported physical activity, fitness as measured by the 6-minute step test, and biometric data were collected at baseline, 12 weeks, and 20 weeks.
Results:
Thirty-eight participants completed the study. Barriers to bicycling declined significantly among intervention group participants at 12 weeks with some declines persisting to 20 weeks. Bicycling for leisure or non work transportation increased significantly more in the intervention than control group from baseline to 12 weeks but this difference attenuated by 20 weeks. Both groups increased their fitness between baseline and 12 weeks, with a trend towards greater gains in the bicycling intervention group. No significant change in biometric measurements was seen at either 12 weeks or 20 weeks.
Conclusion:
Despite the small study size, this bicycling intervention decreased perceived barriers to bicycling and increased bicycling activity in low-income minority participants. These findings support a larger-scale study to measure fitness and health changes from bicycling interventions.
BACKGROUND
Physical activity is inversely related to many medical conditions, particularly obesity, type 2 diabetes, and coronary heart disease1—the leading cause of death in the United States.2 Many factors ranging from individual to environmental and cultural contribute to widespread inactivity. Further, income disparities exist in the prevalence of physical inactivity.3 Lifestyle activities, including bicycling for active transportation, have been found to promote healthy weight and decrease the risk of adverse cardiovascular outcomes, including mortality from cardiovascular disease.4,5
Nationally, bicycling rates are increasing,6 while research suggests that lower-income and minority communities experience unique barriers to bicycling. These include lack of access to a working bicycle, bicycle theft, personal security, police harassment, safety from traffic, and cultural perceptions of bicycling as an indicator of low social status.7–10 Increasing physical activity through bicycling in low-income communities and communities of color has the potential to improve personal and public health. The previous studies of bicycling in such communities have explored barriers to bicycling or provided case study descriptions of education and encouragement programs.11,12
Identifying successful interventions to promote physical activity in inactive adults is a critical public health need. Prior research on bicycling interventions has not specifically targeted inactive, overweight or obese lower-income adults. We are unaware of any studies utilizing a controlled trial to evaluate the impact of a bicycle training and promotion intervention using biometric and survey data collection.
We theorized that a bicycle education and promotion intervention would impact the personal attitudes and barriers towards bicycling for participants, resulting in increased bicycling activity that would lead to fitness and health improvements. Our intervention was based on the Theory of Planned Behavior13 and the Transtheoretical Model.14 A separate paper (R Schneider, et al, unpublished data, June 2016) focuses on attitudes and perceived barriers to bicycling among participants while the goals of this paper are to evaluate later stages of behavioral and health change: whether or not the bicycling intervention helped participants (1) increase bicycling and general physical activity levels, and (2) improve health, as measured by fitness testing and several biometric parameters.
METHODS
Design
The study was a 2-site, nonblinded randomized controlled trial of a bicycling intervention for inactive adults in 2 lower-income neighborhoods in Milwaukee, Wisconsin. It was reviewed and approved by the Institutional Review Board of the Medical College of Wisconsin.
Participants
Eligible participants were 18 to 69 years old, spoke English and/ or Spanish, were currently physically inactive—as defined by self reporting physical activity less than 3 days per week for 20 minutes or more15—and had a body mass index (BMI) ≥ 25.0. Those not meeting inclusion criteria, were currently pregnant, planning to become pregnant during the study period, or planning to relocate were excluded. Participants were screened for safety using validated physical activity readiness questionnaires16,17 and, if necessary, physician clearance. Prior ability to ride a bicycle was not required.
The study was conducted at 2 sites. One, Sixteenth Street Community Health Centers (SSCHC), is a Federally Qualified Health Center that serves a predominantly Latino community on the south side of Milwaukee. The other, Silver Spring Neighborhood Center (SSNC), is a community center located within the Westlawn Gardens public housing development, serving a predominantly African American community on the north side of Milwaukee.
Enrollment Procedures
Participants were recruited using flyers and at community events, with assistance from community health ambassadors. Friends or family who enrolled were randomized individually. After obtaining informed consent and confirming study eligibility, participants were randomized 1:1 to the intervention or control groups, stratified by site. Random assignments were made using Research Electronic Data Capture (REDCap). It was not possible to determine group assignment prior to randomizing each individual. Neither participants nor researchers were blinded to the group assignment. Participants in the intervention group received bicycles, locks, and helmets at baseline; control group participants received gift cards at baseline. Both groups received gift cards for attending the subsequent data collections. The control group received bicycles, locks, and helmets after completing the final data collection.
Intervention
The bicycling intervention included 10 scheduled group sessions at each site over a 12-week period from June to August 2015. Intervention group participants were fitted with refurbished bicycles prior to the first session. Participants were able to keep their bicycles from that point forward and were encouraged to ride independently during and after the intervention. Sessions consisted of on-road education and group rides; bicycle safety classroom instruction occurred on rain dates. Ride lengths increased progressively from 2 to 7 miles, and pace increased from 4 miles per hour (mph) to 10 mph. Participants learned about accessing local paved bicycle trails, using bike lanes, hand signaling, and navigating traffic (eg, stops, turns). Licensed cycling instructors of the Bicycle Federation of Wisconsin administered the intervention. A bilingual instructor served the site located in the Latino community. The control group received no intervention.
A total of 52 participants were recruited for the study in the spring of 2015 between both sites. Of these, 49 were eligible to participate and were randomized, with 20 assigned to the control group and 29 to the bicycling intervention. There were 38 individuals who provided baseline data and 26 who provided follow-up data at both 12 weeks and 20 weeks. See Figure 1 for the participant flow diagram.
Figure 1.
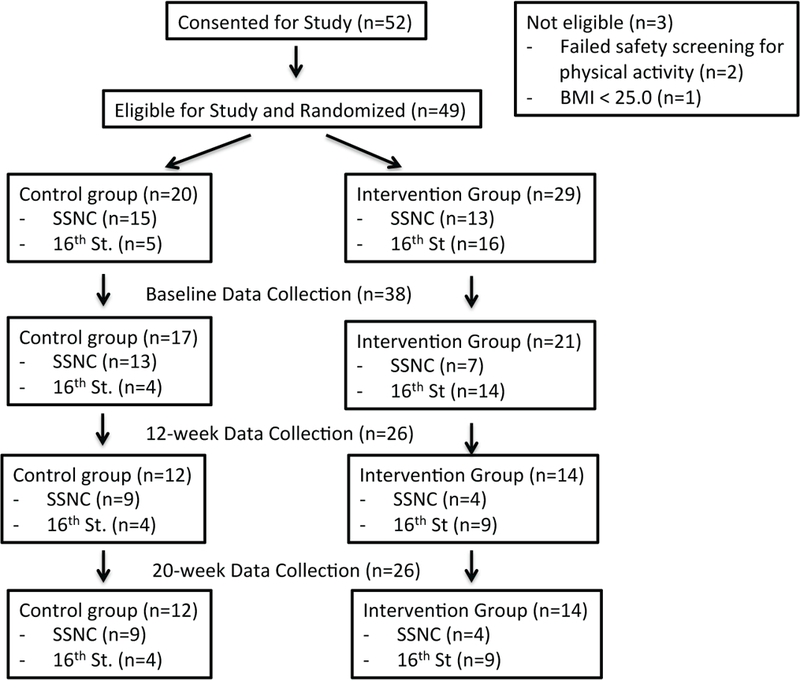
Participant Consort Diagram, as Assigned
Abbreviations: SSNC, Silver Spring Neighborhood Center; 16th St, Sixteenth Street Community Health Centers
The intervention delivered with the SSCHC group adhered closely with the intended plan. Very low participant attendance at the SSNC site resulted in only a single group ride occurring. Many attempts were made throughout the study period to engage participants and reschedule rides at this site to increase intervention participation.
Outcome Measures
Data were collected from participants at baseline, after the 12-week intervention concluded, and 20 weeks after baseline. Intervention group bicycles were outfitted with cyclometers. In addition, the cycling instructors utilized structured field notes to record observations throughout the summer. The following outcomes were collected at each of the 3 data points: (1) self-reported bicycling, perceived barriers to bicycling, and overall activity; (2) fitness; and (3) biometrics.
Self-reported bicycling, perceived barriers to bicycling and overall activity –
The International Physical Activity Questionnaire (IPAQ)18 longform, a previously validated tool, provided estimates of weekly physical activity within specific domains, including transportation and leisure. It was self-administered or interviewer-administered, at the preference of each participant. A Bicycle Attitudes Survey developed by the research team asked about bicycling activity and 19 possible barriers to bicycling. The ordinal response options for each barrier were “does not apply” (scored as 0), “not significant at all” (scored as 0), “somewhat significant” (scored as 1), “very significant” (scored as 2), and “so significant that it keeps me from riding” (scored as 3). We measured the change in perceived barriers by comparing the score at baseline with the score at 12 weeks or 20 weeks. Additional detail about this survey is available elsewhere (R Schneider, et al, unpublished data, June 2016). Both surveys were available in English and Spanish.
Fitness –
The 6-minute step test,19 a convenient and validated variation on the 6-minute walk test,20 was used as a maximal exertion fitness test. Participants were instructed to step up and down a 20-centimeter step as many times as possible in 6 minutes, while the number of steps was recorded.
Biometrics –
Baseline height and weight were collected, and weight was remeasured at 12 and 20 weeks; body mass index (BMI) was calculated; waist circumference was measured. Blood pressure was measured manually after participants sat quietly for 5 minutes; the average of 2 readings was used for each time point.
Data Analysis
Participant characteristics were summarized using descriptive statistics. Tests for baseline differences between groups were assessed using t-tests for continuous variables, chi-square Fisher exact testing for proportions and categorical variables, and exact Wilcoxon rank-sum test for ordinal variables. Two-sample paired t-tests were used to identify significant changes in bicycle activity, fitness, and biometric measures between the bicycling intervention and control groups from baseline to 12 weeks and baseline to 20 weeks (STATA 14.1, College Station, TX). IPAQ was scored per established scoring protocol, utilizing minutes/day as the outcome. Within the transportation and leisure activity domains, comparisons were made between groups from baseline to 12 and 20 weeks, respectively, using ANOVA testing (SPSS, 22.0, Chicago, IL). Data were analyzed by group using intention-to-treat analysis.
RESULTS
Participant Characteristics
The participants were predominantly female (84%) and middle-aged (mean 41.8 years, range 22–65 years). Ninety-four percent of participants at the SSCHC site were Hispanic/Latino ethnicity and 100% of participants at the SSNC site were African American. Participants at both sites had low socioeconomic status, with 53% of participants overall reporting annual incomes of less than $15,000 and 71% of participants having less than high school completion or a GED certificate. However, the bicycling intervention group had a higher income than the control group (P = 0.0021). The intervention group was also more likely to report Latino/Hispanic ethnicity than the control group (62% vs 24%, P = 0.018). There were no other significant differences between study groups by age, education, gender, employment status, health insurance status, or chronic medical conditions. At enrollment, only 14% in the intervention and 25% in the control group (P = 0.410) owned a bicycle. See Table 1 for additional participant characteristics. There were no significant differences in age, gender, study group, site, or income between participants who dropped out either prior to baseline data collection or during the intervention period.
Table 1.
Participant Characteristics
| Characteristic | Bicycling Intervention (n=21**), n (%) |
Control Group (n=17**), n (%) |
Test of Significance |
|---|---|---|---|
| Age* | 40.14 (8.50), 22–57 | 43.76 (12.13), 24–65 | 0.8565 |
| Sex | 0.778 | ||
| Male | 3 (14.3%) | 3 (17.7%) | |
| Female | 18 (85.7%) | 14 (82.4%) | |
| Preferred Language | 0.099 | ||
| English | 9 (42.9%) | 13 (76.5%) | |
| Spanish | 7 (33.3%) | 3 (17.7%) | |
| Both | 5 (23.8%) | 1 (5.9%) | |
| Highest Grade Completed | 0.3883 | ||
| < 9 | 1 (4.8%) | 2 (11.8%) | |
| 9 – 12/GED certificate | 13 (61.9%) | 11 (64.7%) | |
| > 12/GED certificate | 7(33.3%) | 4 (23.5%) | |
| Income | 0.0021 | ||
| Less than $15,000 | 5 (27.8%) | 13 (81.3%) | |
| $15,000 - $34,000 | 6 (33.3%) | 2 (12.5%) | |
| More than $34,000 | 7 (38.9%) | 1 (6.3%) | |
| Race/Ethnicity | 0.018 | ||
| Hispanic/Latino Ethnicity | 13 (61.9%) | 4 (23.5%) | |
| Non-Hispanic/Latino ethnicity, | 8 (36.1%) | 13 (76.5%) | |
| African American race | |||
| Non-Hispanic/Latino ethnicity, | 0 (0.0%) | 0 (0.0%) | |
| Other race | |||
| Employment | 0.706 | ||
| Employed | 11 (55.0%) | 7 (41.2%) | |
| Unemployed | 4 (20.0%) | 3 (17.7%) | |
| Other | 5 (25.0%) | 7 (41.2%) | |
| Health Insurance | |||
| Insured | 14 (70.0%) | 16 (94.1%) | 0.062 (type) |
| Public Insurance | 7 (35.0%) | 10 (58.8%) | |
| Private Insurance | 4 (20.0%) | 1 (5.9%) | |
| Other | 3 (15.0%) | 5 (29.4%) | |
| Not Insured | 6 (30.0%) | 1 (5.9%) | 0.102 (status) |
| Health Conditions | |||
| Diabetes | 5 (23.8%) | 3 (17.7%) | 0.643 |
| High Blood Pressure | 3 (14.3%) | 7 (41.2%) | 0.061 |
| High Cholesterol | 7 (33.3%) | 2 (11.8%) | 0.120 |
| Other | 7 (33.3% | 2 (11.8%) | 0.231 |
| Number of Health Conditions* | 1.14 (1.4), 0–5 | 0.824 (1.1), 0–3 | 0.2248 |
| Owns Bike | 3 (14.3%) | 4 (25.0%) | 0.410 |
| Knows how to Ride Bike | 20 (95.2%) | 15 (93.8%) | 0.843 |
mean (SD), range
Some participants did not report all variables, actual number reporting listed in table.
Barriers to Bicycling
Several barriers reported at baseline declined significantly more among intervention group members than control group members. At 12 weeks these barriers included not feeling healthy enough to bike (P = 0.036), being physically uncomfortable while bicycling (P = 0.012), not having a bicycle to use (P = 0.043), not having other people to bike with (P = 0.031), not knowing routes to use (P = 0.039), not feeling safe from crime (P = 0.020), not feeling safe from car traffic (P = 0.015), and adult bicycling not being socially acceptable in the respondent’s neighborhood (P = 0.049). Two of these barrier reductions remained significantly greater for the intervention group at 20 weeks: not feeling healthy enough to bike (P = 0.045) and not feeling safe from car traffic (P = 0.015). Reductions in perceived barriers to bicycling are discussed in more detail elsewhere (R Schneider, et al, unpublished data, June 2016).
Physical Activity
The analysis explored overall self-reported physical activity. However, upon initial tabulation at baseline, on average, participants reported 270.5 minutes/day of vigorous intensity activity and 467 minutes/day of moderate intensity activity. Therefore, standard IPAQ scoring procedures were followed excluding participants reporting outlying values (>960 minutes/day of activity). Six participants’ data were excluded from vigorous intensity analysis and 12 participants’ were excluded from moderate intensity analyses. Many of the outlying values were reported in the occupation and household activity sections; therefore, only transportation and leisure time activity data are presented, as those are of interest to the current study.
Responses from the IPAQ revealed a significant difference in time spent bicycling for transport between control and intervention groups (mean difference +8.8 minutes/day in intervention group [95% CI, +0.2–17.4]) at the 20-week follow-up. Additionally, there was a significant increase in time spent biking in the intervention group from baseline to 20 weeks (+8.5 min/d, 95% CI, +1.3–15.8), with no significant increase in biking time in the control group.
Further, time spent in moderate intensity leisure time physical activity was significantly different between groups at 12 weeks (mean difference +2.6 minutes/day in intervention group (95% CI, +0.8–6.0). There were no significant differences between or within groups for time spent in moderate intensity leisure time activity.
Self-reported bicycling for specific purposes also was compared between groups (Table 2). Bicycling for leisure and for non-work-related transportation both increased significantly more in the intervention than the control group (P = 0.020 and P = 0.019, respectively) from baseline to 12 weeks, while there was no significant difference between groups in bicycling to work (P = 0.751). None of these differences between groups persisted at 20 weeks.
Table 2.
Reported Bicycling Frequency, by Purpose: Intervention vs Control Group
| Travel Purpose: How often in the past 7 days did you bicycle for the following purpose 2+ times? |
Baseline Frequency (%) Intervention, Control |
Week 12 Frequency (%) Intervention, Control |
Week 20 Frequency (%) ntervention, Control |
Baseline vs Week 12 |
Baseline vs Week 20 |
||
|---|---|---|---|---|---|---|---|
| Sample Size Intervention, Control) |
Sample Size (Intervention, Control) |
||||||
| P-value* | P-value* | ||||||
| Ride to or from work | 7.1%, 0% | 7.1%, 0% | 7.7%, 0% | 14, 9 | 0.751 | 13, 8 | 0.752 |
| Ride to shop, eat, visit friends or to other activities besides work |
7.1%, 10.0% | 14.3%, 0% | 15.4%, 0% | 14, 8 | 0.020 | 13, 8 | 0.173 |
| Take a bike ride for exercise or fun without a destination |
0%, 10.0% | 42.9%, 0% | 23.1%, 0% | 14, 8 | 0.019 | 13, 8 | 0.056 |
The reported P-value evaluates the change in the number of days in the previous week that the respondent reported bicycling for a given purpose relative to the baseline survey; P-value less than 0.05 indicates that intervention group participants reported significantly greater increases in bicycling frequency than the control group participants.
Cyclometer data were available for 9 intervention group participants and reflected 23 to 72 days of data. These participants attended between 2 and 6 group rides and averaged 6.5 miles per week (range 1.0–15.0 miles per week), for a total recorded average riding distance of 38.6 miles (range 8.0–114.0 miles).
Fitness and Biometric Measures
Participants did an average of 124.3 steps on the baseline step test (95% CI, 116.0–132.6). The intervention group did an average of 128.4 (95% CI, 115.7–141.1) steps at baseline compared to 120.1 (95% CI, 108.2–132.0) in the control group; this difference was not statistically significant (P = 0.15).
Amongst baseline participants who remained in the study at 12 and 20 weeks, the group as a whole increased number of steps from 126.4 (95% CI, 117.3–135.5) to 138.5 (95% CI, 126.1–150.8) from baseline to 12 weeks (n=20, P = 0.011). BMI, waist circumference, and blood pressure did not change from baseline to 12 weeks for the group as a whole.
We compared the change in steps from baseline to 12 weeks and 20 weeks between intervention and control groups. There was a trend toward individuals in the intervention group having a greater increase in steps from baseline to 12 weeks by +13 steps (95% CI, +1.2 to +24.8) versus +11.1 steps in the control group (95% CI, −2.85 to +25.0), but this difference was not statistically significant. Both groups demonstrated some regression in fitness after the intervention period and summer months ended, with average number of steps trending back down between 12 and 20 weeks, from 136.6 to 125.1 in the control group and 145.2 to 140.4 in the intervention group; the change in steps from 12 to 20 weeks was nonsignificant (P = 0.076).
At baseline, average BMI was 36.6 (95% CI, 25.5–51.2) and waist circumference was 105.7 cm (95% CI, 72.5–136.5). Baseline average systolic blood pressure was 123.9 (95% CI, 95.5–147.0) and diastolic blood pressure was 77.5 (63.5–93.0). Baseline biometric measurements did not differ between study groups. BMI, blood pressure, and waist circumference did not change significantly between study groups throughout the study period. See Table 3 for additional biometric measurement data.
Table 3.
Biometric Testing by Study Group
| Baseline Mean (Min, Max), n |
12 Week Mean (Min, Max), n |
20 Week Mean (Min, Max), n |
Difference 12 Week vs Baseline, by Treatment Group |
Difference 20 Week vs Baseline, by Treatment Group |
|
|---|---|---|---|---|---|
| BMI | P-value, n | P-value, n | |||
| Control | 38.2 (28.0–50.0), 16 |
36.5 (23.6–50.6), 12 |
36.7 (23.1–50.4), 12 |
0.515, 24 | 0.780, 24 |
| Intervention | 35.4 (25.5–51.2), 21 |
34.8 (25.1–51.1), 14 |
34.8 (25.0–51.5), 14 |
||
|
Waist Circumference |
|||||
| Control | 110.3 (87.0–136.5), 16 | 107.0 (74.5–127.0), 12 | 108.8 (78.4–128.5), 12 | 0.069, 23 | 0.972, 24 |
| Intervention | 102.2 (72.5–136.5), 21 | 100.4 (76.0–136.0), 13 | 101.6 (74.5–134.0), 14 | ||
| Systolic BP | |||||
| Control | 127.3 (96–146), 16 | 122.2 (99–141), 12 | 128.0 (106–166), 12 | 0.547, 23 | 0.258, 24 |
| Intervention | 121.3 (99–147), 21 | 125.0 (103–141), 13 | 121.4 (107–147), 14 | ||
| Diastolic BP | |||||
| Control | 77.5 (64–93), 16 | 74.8 (63–91), 12 | 79.5 (67–94), 12 | 0.868, 23 | 0.237, 24 |
| Intervention | 77.5 (65–92), 21 | 76.0 (60–89), 13 | 76.6 (62–89), 14 | ||
| Steps | |||||
| Control | 120.1 (83–160), 15 | 136.6 (97–201), 11 | 125.1 (105–158), 10 | 0.830, 20 | 0.659, 19 |
| Intervention | 128.4 (72–159), 15 | 145.2 (113–178), 13 | 140.4 (101–200), 13 | ||
Abbreviations: BMI, body mass index; BP, blood pressure.
DISCUSSION
Our study generally supports the feasibility of conducting a bicycling intervention to improve the health of lower-income over-weight or obese adults in urban communities of color. Intervention group participants experienced greater reductions in perceived barriers to bicycling and reported bicycling more for leisure and nonwork transportation purposes than control group participants.
There was interest in our target communities to recruit participants to the study. Our gender imbalance was notable; typically, bicycling is more common for adult men than women.21 However, our recruitment tended to center around community events and health-related programming better attended by women. The implementation success of this intervention was highly discordant at the 2 sites. This led to smaller than expected sample size and dilution of the program effect, as the SSNC intervention participants each attended only 1 ride compared to the more robust intervention received by the 9 SSCHC intervention participants. Some possible factors include a more consistent ride schedule at SSCHC, a female cycling instructor (like the majority of participants), childcare availability, and different participant demographics.
However, the success of our SSCHC site intervention was notable. Participant engagement was high and bicycling skills, endurance, and comfort increased dramatically for active participants. Based on the success of our SSCHC site intervention implementation, we feel this program is feasible, with attention to the factors described above. Based on our pilot findings, we offer several recommendations for improvement and scaling for a larger study (see Table 4).
Table 4.
Recommendations for Improvement and Scaling for Larger Study
| Recruitment | • Recruit pairs or groups of friends or family to participate. • To recruit gender-balanced participant group: recruit for study at events well attended by men and women and utilize both male and female community health workers. |
| Study Design | • If using randomized controlled trial, consider crossover intervention design to increase equity for participants. Consider providing all participants a bicycle at baseline. • If feasible, follow participants further into the fall season or even the following spring or summer • Block randomize by small units (5) within each group to ensure similar number of participants start in each group. • Analyze participant data by clusters for those recruited with friends or family members |
| Intervention | • Plan to begin the intervention as early in the spring/ summer season as local weather allows, so crossover design and postintervention follow-up may be feasible. • Use a consistent schedule for group rides, and have this schedule available at the time of study recruitment. • Provide childcare for participants. • Utilize a cycling instructor who is a member of the participants’ community. |
| Data Collection | • Consider use of direct physical activity measurement using a validated mobile application, if such a tool has been developed. • Substitute an alternate tool for self-reported physical activity for IPAQ when working with low-literacy participants, such as the Rapid Assessment of Physical Activity (RAPA).26 • Consider measurement of insulin resistance in participants, as this outcome could be expected to change based on an intervention of this magnitude. |
Our pilot experience supported our general approach to data collection, particularly the use of the step test, biometric assessments, and Bicycle Attitudes Survey. Even though IPAQ is widely used, validated for use in many languages and populations, and highly accepted for physical activity measurement, there are a number of documented limitations. Specific to our population, there is a well-documented overreporting of nonleisure time moderate to vigorous physical activity (MVPA) in multicultural samples or among cultural samples with higher levels of labor-based occupations.22 Despite the availability of print and interviewer-administered IPAQ surveys in participants’ preferred language, our participants appear to have overestimated their physical activity, as evidenced by the many participants reporting outlier activity levels. Direct measurement of physical activity would be preferable, although reliable capture of bicycling can be challenging.23
This pilot study was the first of its kind to test a bicycling intervention in a community-based setting using a randomized study design. Implementing this rigorous study design within community settings posed challenges, including regular participation, comprehension of technical survey questions, and social groupings.24 However, its findings support additional research to refine bicycle program implementation and research methods in order to gain more knowledge about the potential impact of bicycling to improve the health of lower-income urban communities.
In addition to the sample size and variable intervention implementation discussed above, the study has additional limitations. We recruited and enrolled participants who were family members or friends, but randomized them individually. When pairs were randomized to the intervention, they were observed to ride together frequently between group sessions. This finding is concordant with prior studies showing social support is an important facilitator of bicycling.25 Our sample size was not adequate to consider recruiting and analyzing for this clustering effect. Another potential limitation results from the high proportion of participants without a bicycle at the beginning of the study. This instrumental barrier essentially prevented bicycling in the control group, which may have limited the usefulness of other information provided about barriers to bicycling. However, our experience was that the additional support and education provided by the intervention was necessary. Several of the intervention participants who were given access to their own bicycles either did not claim them or did not use them. Finally, our findings may not be applicable to other lower-income overweight urban populations, as we have identified that many cultural, structural, and other factors impact interest in and participation in bicycling.
Despite these limitations, this pilot study was the first of its kind to test a bicycling intervention in a community-based setting using a randomized study design. Its findings support additional research to refine bicycle program implementation and research methods in order to gain more knowledge about the potential impact of bicycling as a feasible modality to improve the health of lower-income communities.
Acknowledgements:
Thanks to Madeleine Organ for her assistance with project planning and data collection.
Funding/Support: Support was received from the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources and the National Center for Advancing Translational Sciences (grant 8UL1TR000055), the Clinical & Translational Science Institute of Southeast Wisconsin through the Advancing a Healthier Wisconsin endowment. Whitney Welch was supported by NIH/NCI training grant CA193193; Jennifer Kusch was supported by HRSA training grant T32 HP10030.
Footnotes
Financial Disclosures: None declared.
Planners/Reviewers: The planners and reviewers for this journal CME activity have no relevant financial relationships to disclose.
Contributor Information
Rebecca Bernstein, Department of Family and Community Medicine, Medical College of Wisconsin, Milwaukee, Wis.
Robert Schneider, Department of Urban Planning, UW-Milwaukee.
Whitney Welch, Department of Kinesiology, University of Wisconsin UW-Milwaukee.
Anne Dressel, College of Nursing, UW-Milwaukee.
Melissa DeNomie, Department of Family and Community Medicine, Medical College of Wisconsin, Milwaukee, Wis.
Jennifer Kusch, College of Health Sciences, Milwaukee Area Technical College.
Mirtha Sosa, Bicycle Federation of Wisconsin, Milwaukee, Wis.
REFERENCES
- 1.Handy S; for the Transportation Research Board and the Institute of Medicine Committee on Physical Activity, Health, Transportation, and Land Use. Does the built environment influence physical activity? Examining the evidence. Critical assessment of the literature on the relationships among transportation, land use, and physical activity In: Physical Activity: Transportation Research Board Special Report 2005, 282 Citeseer; 2005. http://citeseerx.ist.psu.edu/viewdoc/download;jsessionid=5DFF7816262647D671258E848018C12E?doi=10.1.1.471.2645&reP=rep1&type=pdf. Accessed June 21, 2017. [Google Scholar]
- 2.Blair SN, Brodney S. Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues. MedSciSports Exerc. 1999;31(11 Suppl):S646–S662. [DOI] [PubMed] [Google Scholar]
- 3.Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Prev Med. 2000;18(1):46–53. [DOI] [PubMed] [Google Scholar]
- 4.Sahlqvist S, Goodman A, Simmons RK, et al. The association of cycling with all cause, cardiovascular and cancer mortality: findings from the population-based EPIC- Norfolk cohort. BMJ Open. 2013;3(11). doi: 10.1136/bmjopen-2013-003797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamer M, Chida Y. Active commuting and cardiovascular risk: a meta-analytic review. Prev Med. 2008;46(1):9–13. doi: 10.1016/j.ypmed.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 6.McKenzie B Modes less traveled: commuting by bicycle and walking in the United States: 2008–2012 American Community Survey Reports, ACS-26. US Census Bureau, Washington, DC; 2014. https://www.census.gov/content/dam/Census/library/publications/2014/acs/acs-25.pdf. Accessed June 21, 2017. [Google Scholar]
- 7.Fuller D, Gauvin L, Kestens Y, Morency P, Drouin L. The potential modal shift and health benefits of implementing a public bicycle share program in Montreal, Canada. Int JBehavNutr Phys Act. 2013;10:66. doi: 10.1186/1479-5868-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCray T, Chen TD, Glass L, et al. East Austin Neighborhood: An African American Community Cycling Study Compiled for CRP 384: Transportation Access & Equity. Austin, TX: The University of Texas at Austin School of Architecture, Community and Regional Planning Program; 2011. http://www.academia.edu/7826757/Transportation_Access_and_Equity_Course_African_American_Community_Cycling_Study. Accessed June 21, 2017 [Google Scholar]
- 9.Community Cycling Center. Understanding Barriers to Bicycling Project: Final Report. Portland, OR: Community Cycling Center; 2012. http://www.communitycyclingcenter.org/wp-content/uploads/2012/07/Understanding-Barriers-Final-Report.pdf. Accessed June 22, 2017. [Google Scholar]
- 10.McCray T, Durden T, Schaubert E. Cycling in the African American Community: Safety Training Guidelines and Findings. Austin, TX: Southwest Region University Transportation Center, Texas A&M Transportation Institute; 2013. http://d2dtl5nnlpfr0r.cloudfront.net/swutc.tamu.edu/publications/technicalreports/600451-00070-1.pdf Accessed June 22, 2017. [Google Scholar]
- 11.Mason M, Welch SB, Becker A, et al. Ciclovia in Chicago: a strategy for community development to improve public health. Community Dev. 2011;42(2):221–239. [Google Scholar]
- 12.Huang HF, Raynault ET, Redmon TA, Board TR. Development of a Marketing Plan to Promote Pedestrian and Bicyclist Safety to Hispanic Audiences In: Transportation Research Board 86th Annual Meeting 2007. https://trid.trb.org/view.aspx?id=801020. Accessed August 8, 2017. [Google Scholar]
- 13.Ajzen I The theory of planned behavior. Organ BehavHum Dec. 1991;50(2):179–211. [Google Scholar]
- 14.Prochaska JO, DiClemente CC. Toward a comprehensive model of change In: Miller WR, Heather N, eds. Treating Addictive Behaviors. New York, NY: Springer; 1986:3–27. http://link.springer.com/chapter/10.1007/978-1-4613-2191-0_1. Accessed June 22, 2017. [Google Scholar]
- 15.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW 3rd, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999;281(4):327–334. [DOI] [PubMed] [Google Scholar]
- 16.Thomas S, Reading J, Shephard RJ. Revision of the physical activity readiness questionnaire (PAR-Q). Can J Sport Sci. 1992;17(4):338–345. http://psycnet.apa.org/psycinfo/1993-24047-001. Accessed June 22, 2017. [PubMed] [Google Scholar]
- 17.Warburton DE, Jamnik V, Bredin SS, Gledhill N. The 2014 Physical Activity Readiness Questionnaire for Everyone (PAR-Q+) and electronic Physical Activity Readiness Medical Examination (ePARmed-X+). Health & Fitness Journal of Canada. 2014;7(1):80–83. [Google Scholar]
- 18.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. [DOI] [PubMed] [Google Scholar]
- 19.Arcuri JF, Borghi-Silva A, Labadessa IG, Sentanin AC, Candolo C, Pires Di Lorenzo VA. Validity and reliability of the 6-minute step test in healthy individuals: a cross sectional study. Clin J Sport Med. 2016;26(1):69–75. [DOI] [PubMed] [Google Scholar]
- 20.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am JRespir Crit Care Med. 2002;166(1):111–117. [DOI] [PubMed] [Google Scholar]
- 21.Garrard J, Rose G, Lo SK. Promoting transportation cycling for women: the role of bicycle infrastructure. PrevMed. 2008;46(1):55–59. doi: 10.1016/j.ypmed.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 22.Bauman A, Ainsworth BE, Bull F, et al. Progress and pitfalls in the use of the International Physical Activity Questionnaire (IPAQ) for adult physical activity surveillance. J Phys Act Health. 2009;6 Suppl 1:S5–8. [DOI] [PubMed] [Google Scholar]
- 23.Matthews CE, Hagströmer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dressel A, Schneider R, DeNomie M, et al. Assessing health promotion interventions: limitations of traditional research methods in community-based studies. Health Promotions Practice. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Geus B, De Bourdeaudhuij I, Jannes C, Meeusen R. Psychosocial and environmental factors associated with cycling for transport among a working population. Health EducRes. 2008;23(4):697–708. doi: 10.1093/her/cym055. [DOI] [PubMed] [Google Scholar]
- 26.Topolski TD, LoGerfo J, Patrick DL, Williams B, Walwick J, Patrick MB. The Rapid Assessment of Physical Activity (RAPA) among older adults. Prev Chronic Dis. 2006;3(4):A118 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1779282/. Accessed June 22, 2017. [PMC free article] [PubMed] [Google Scholar]


