Abstract
Context: Curcumin has long been used as a condiment and a traditional medicine worldwide.
Objective: The current study investigates the possible protective effect of curcumin on heart function in myocardium ischemia-reperfusion (MIR) rats.
Materials and methods: We fed Sprague–Dawley (SD) rats (10 in each group) either curcumin (10, 20 or 30 mg/kg/d) or saline. Twenty days later, the rats were subjected to myocardial injuries by ligating the left anterior descending coronary artery (60 min), and subsequently, the heart (3 h) reperfused by releasing the ligation. Then, lipid profile, lipid peroxidation products, antioxidant enzymes and gene expression were assessed in myocardium tissue.
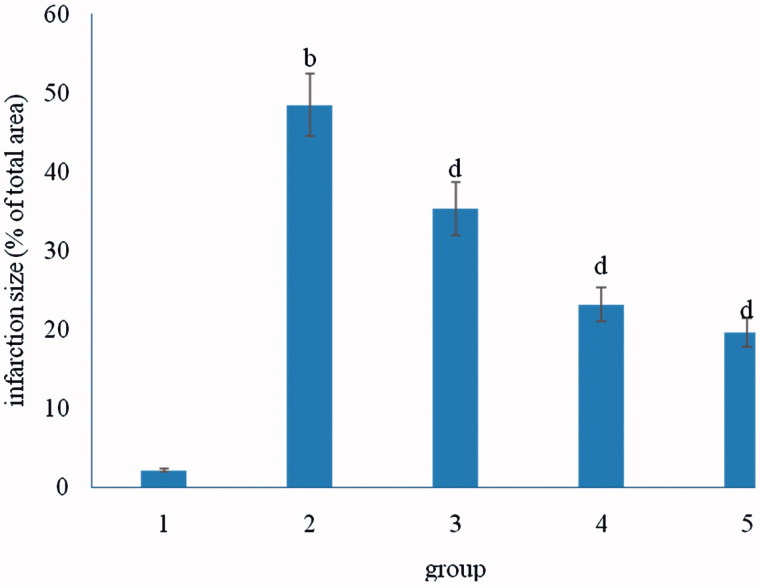
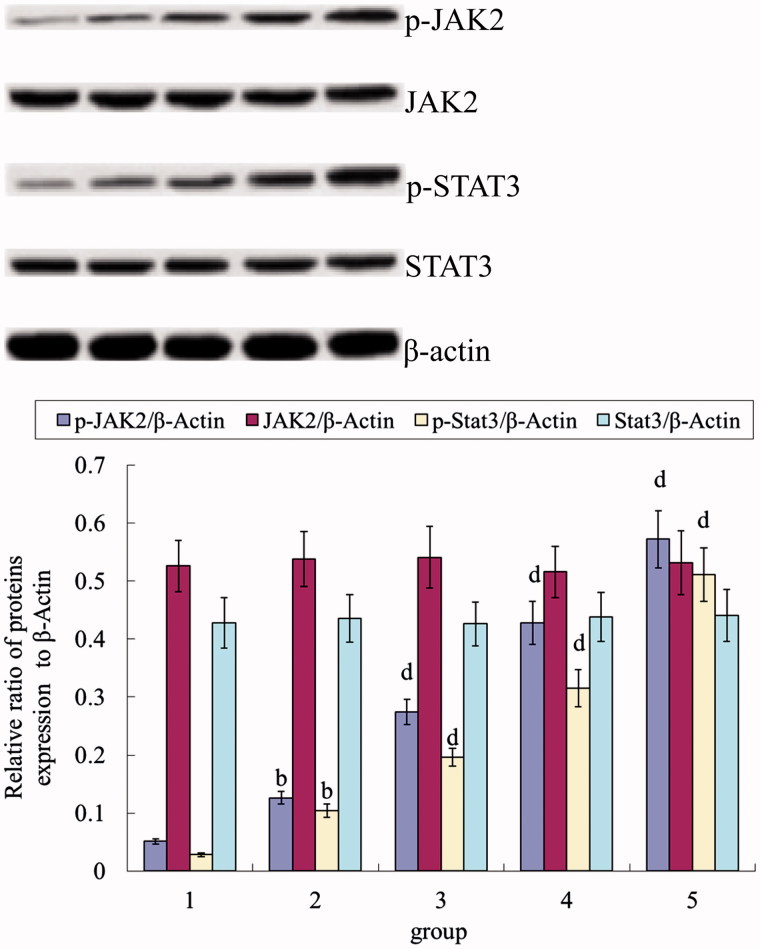
Results: Only the rats that were supplemented with curcumin (10, 20 or 30 mg/kg/d) showed significant (p < 0.05) reductions in oxidative stress (3-fold), infarct size (2.5-fold), which was smaller than that of the control group. The percentage of infarct size in MIR rats with curcumin at 10, 20 or 30 mg/kg/d decreased (from 49.1% to 18.3%) compared to ischemia-reperfusion (I/R). The enhanced phosphorylation of STAT3 was further strengthened by curcumin (10, 20 or 30 mg/kg/d) in a dose-dependent manner.
Discussion and conclusion: Curcumin intake might reduce the risk of coronary heart disease by stimulating JAK2/STAT3 signal pathway, decreasing oxidative damage and inhibiting myocardium apoptosis.
Keywords: Blood lipid, immunity, antioxidant, signal pathway
Introduction
Curcumin [1,7-bis(4-hydroxy-3-methoxyphenyl)-1,6-heptadiene-3,5-dione] is a naturally occurring compound extracted from the roots of Curcuma longa L. (Zingiberaceae). Curcumin exhibits multiple pharmacological activities including antioxidant, anticarcinogenic and anti-inflammatory in different models of rodents. In an in vivo study, curcumin improves outcomes and attenuates focal cerebral ischemic injury by decreasing the expression of apoptotic genes in rats (Zhao et al. 2010). In addition, curcumin improves motor function by inhibiting apoptosis and neuronal loss after spinal cord injury in rats. Several investigators have provided evidence suggesting protective effects of curcumin against diverse cardiovascular pathological states leading towards heart failure (Morimoto et al. 2008; Ahuja et al. 2011; Kumphune et al. 2015).
Cardiac ischemia is one of the most important diseases in developed countries. Cell injury during ischemia and posterior reperfusion may be mediated by oxidative stress and calcium overload, leading to necrosis and/or apoptosis and impairment of cardiac function. The pathogenesis of injury in myocardial ischemia has many mechanisms. The anatomic changes and the distinctions of biochemical markers for ischemic myocardial cell injury and death have been well characterized. The cardiac dysfunction is generated in myocardial ischemia, and the loss of energy substrates in myocardial ischemia leads to the generation of reactive oxygen species (ROS) (Levraut et al. 2003); the high levels of ROS are detrimental (Kloner et al. 1989) and can induce a variety of cardiomyocyte abnormalities (Mahmoud & El Bassossy 2014).
Several studies have demonstrated that the Janus kinase 2 (JAK2)/STAT3 signalling pathway is significant in mediating an inflammatory response (Kim et al. 2002; Cho et al. 2013; Guo et al. 2014). STAT3 is positioned downstream of JAK2 and can be activated via the phosphorylation of serine (Ser) 727 and tyrosine (Tyr) 705. Once activated, STAT3 is translocated into the nucleus to regulate target genes.
Our present study assesses whether pre-treatment with curcumin produces cardioprotective effects in the rats model of acute myocardial ischemia.
Materials and methods
Materials
Curcumin (98%) was purchased from Puruifa Company (Chendu, China).
We purchased primary antibodies anti-JAK2, anti-P-JAK2, anti-STAT3 and anti-P-STAT3 from Santa Cruz Biotechnology (Santa Cruz, CA). Anti-Bcl2 and anti-Bax were from Cell Signaling Technology (Beverly, MA).
Animals and grouping
Fifty male Sprague–Dawley (SD) rats (200–250 g, 8-weeks-old) were purchased from the Animal Experiment Center of Shanghai Jiao Tong University, China. The animals were maintained in a temperature-controlled room at 20–23 °C, with a relative humidity of 40–50% and a 12 h light/dark cycle and allowed free access to food and water. All animal care and experimental procedures were in accordance with the guidelines of the NIH (National Institutes of Health) and approved by the Institutional Animal Care and Use Committee at Shanghai Jiao Tong University.
Rats were anesthetized by intraperitoneal injection of ketamine hydrochloride (90 mg/kg) and xylazine hydrochloride (10 mg/kg), and ventilated with room air using a rodent ventilator with the body temperature maintained between 36 °C and 37 °C using a heating pad. Rats were divided into five groups: (1) sham control group; (2) ischemic reperfusion (IR) group; (3) IR + curcumin (10 mg/kg/d) group; (4) IR + curcumin (20 mg/kg/d) group and (5) IR + curcumin (30 mg/kg/d) group. In sham and IR control groups, rats (10 rats in each group) were given saline by oral gavage for 15 d before IR operation. In curcumin treatment groups, rats were administered with curcumin (10, 20 or 30 mg/kg/d) by oral gavage for 20 d before IR operation.
Cardiac ischemia-reperfusion (myocardial infarction)
Rats were subjected to a 60-min coronary artery occlusion followed by 3 h of reperfusion. The snare encircling the coronary artery was used for occlusion by pulling up on the suture and clamping it with a plastic tube. Coronary artery reperfusion was restored by releasing the clamp. The sham groups were not exposed to ischemia-reperfusion, but to a time-matched normal perfusion. Echocardiography was performed as previously described, with a Hewlett-Packard echocardiography system SONOS 2000 with a 3.5/2.7 MHz transducer, and recorded.
For left ventricular (LV) pressure recordings, a water-filled small latex balloon by polythene cannula was inserted through left atrium into the left ventricle and connected to the pressure transducer (model 1050BP; Biopac System, Goleta, CA) for the LV systolic and diastolic pressure measurements. The LV developed pressure (LVDP) was the difference between systolic and diastolic pressures. The LV end-diastolic pressure (LVEDP) was adjusted to 10 mmHg at the beginning of the experiment and the LV pressures were differentiated to estimate the maximum rate of pressure development (+dP/dtmax) and the maximum rate of LV pressure decay (−dP/dtmax) with Acknowledge 3.71 software for Windows (Biopac System).
Antioxidant enzymes analysis
Analysis of tissue malondialdehyde (MDA) level as an indicator of lipid peroxidation was performed by the spectrophotometry method. This method was used to obtain a spectrophotometric measurement of the colour produced during the reaction to thiobarbituric acid with MDA at 535 nm. The MDA level is expressed as nmol/g-tissue protein.
SOD (Superoxide dismutases) activity was determined by its ability to increase the riboflavin-sensitized photooxidation of o-dianisidine (Mylorie et al. 1986). GSH-Px (glutathione peroxidase) activity was measured using the method of Lawrence and Burk (1976).
The activity of catalase (CAT) was measured. The principle of this method is that dichromate in acetic acid is reduced to chromic acid, when heated in the presence of H2O2, with the formation of perchloric acid as an unstable intermediate; the chromic acetate thus produced is measured at 570 nm.
Glutathione reductase (GR) which utilizes NADPH to convert oxidized glutathione to the reduced glutathione was assayed.
Evaluation of myocardial infarction and injury
After 60 min of myocardial ischemia and 180 min of reperfusion, hearts were immediately removed, cleaned of blood with physiological saline via the aorta, injected with 1% TTC (triphenyltetrazolium chloride) until they became red, and snap frozen in liquid nitrogen for 20 min. Subsequently, the hearts were cut into cross-sectional pieces and fixed in 10% formaldehyde for 12 h. The TTC-stained sections were photographed. The percentage of infarct size is determined by weight.
Estimation of myocardial injury markers
The prepared serum samples were used for the determination of cardiac marker enzymes creatinine kinase-MB (CK-MB), lactate dehydrogenase (LDH), Ca2+-ATPase and Na+-K+-ATPase using commercially available standard kits (Shanghai Haoran Bioengineering Inc., Shanghai, China) by RT-9600 Semi-automatic Biochemical Analyzer. All measurements were performed according to the kits manufacturers’ instructions.
Western blot analysis
The heart tissue was chopped into pieces and homogenized in ice-cold RIPA (Radio Immunoprecipitation Assay) buffer (0.1% phenylmethylsulfonyl fluoride), containing protease inhibitor (complete Cocktail tablets, Roche Applied Science, Mannheim, Germany). The supernatant was collected after centrifugation at 12,000 rpm for 20 min. The protein concentration was determined by using the BCA (bicinchoninic acid) protein assay kit. Protein extracts were loaded and separated by an SDS (sodium dodecyl sulfate)-polyacrylamide gel electrophoresis, and the resolved proteins were transferred onto PVDF (polyvinyl difluoride) membranes. The membranes were blocked with 5% skim milk in Tris buffer saline and incubated at 4 °C overnight with separate primary antibodies, anti-Caspase-3 (1:1000), anti-Bax (1:1000), anti-Bcl-2 (1:1000), anti-JAK2 (1:500), anti-p-JAK2 (1:500), anti-STAT3 (1:1000), anti-p-STAT3 (1:1000) and anti-β-actin (1:1000). After washing three times with Tris-buffered saline-Tween-20, the membranes were incubated with secondary antibody (1:12,000) for 1.5 h at room temperature. The bands were visualized by using enhanced chemiluminescence detection reagents (Dizhao, Nanjing, China) and a gel imaging system. Densitometric analysis of Western blot bands was densitometrically analyzed by Image J software (National Institutes of Health, Bethesda, MD).
Statistical analysis
Data were expressed as mean ± SD and were analyzed using one-way ANOVA followed by the Bonferroni multiple comparison methods. Results with p < 0.05 were considered to be statistically significant. All statistical analyses were performed using the SPSS version 20.0 (Chicago, IL).
Results
Curcumin improved post-ischemic heart systolic and diastolic functions. As shown in Table 1, myocardium ischemia-reperfusion (MIR) rats showed a significant increase in LVDP, LVEDP, +dp/dtmax and − dp/dtmin values compared to sham group. Treatment of MIR rats with curcumin at 10, 20 or 30 mg/kg/d increased the LVDP, LVEDP, +dp/dtmax and − dp/dtmin values. These results suggest that structure restoration in the ischemic heart (Table 1) was translated into cardiac function improvements. Thus, curcumin could improve cardiac contractibility, attenuate hypercontraction and reduce diastolic pressure, which is believed to be a major reason for increased O2 demand.
Table 1.
Effect of curcumin on myocardium LVDP, LVEDP, +dp/dtmax and − dp/dtmin values.
| Group | LVDP (mmHg) | LVEDP (mmHg) | +dp/dtmax (mmHg/s) | −dp/dtmin (mmHg/s) |
|---|---|---|---|---|
| 1 | 98.36 ± 8.57 | 1727.43 ± 15.37 | 1802.35 ± 157.23 | 1326.05 ± 100.35 |
| 2 | 61.52 ± 5.92b | 1043.26 ± 98.56b | 1236.26 ± 118.36b | 862.59 ± 56.03b |
| 3 | 74.25 ± 6.94d | 1291.05 ± 113.03d | 1369.25 ± 105.73d | 969.32 ± 87.49d |
| 4 | 81.93 ± 8.33d | 1481.33 ± 122.49d | 1527.05 ± 144.29d | 1149.01 ± 94.26d |
| 5 | 92.49 ± 8.47d | 1622.13 ± 170.34d | 1783.26 ± 152.05d | 1315.26 ± 128.39d |
bp < 0.01, compared with group 1; dp < 0.01, compared with group 2.
The myocardium antioxidant enzymes (Tables 2 and 3) demonstrated insignificant changes following the treatment of MIR rats with 10, 20 or 30 mg/kg/d of curcumin. Compared with sham group, MIR rats demonstrated a significant increase in MDA content, while that of antioxidant enzyme activities (SOD, CAT, GPx and GR) was significantly decreased. Treatment of MIR rats with curcumin at 10, 20 or 30 mg/kg/d enhanced the antioxidant enzymes activities. Treatment with curcumin at 30 mg/kg b.wt. showed better amelioration.
Table 2.
Effect of curcumin on myocardium MDA levels.
| Group | MDA |
|---|---|
| 1 | 1.34 ± 0.12 |
| 2 | 5.39 ± 0.44b |
| 3 | 3.72 ± 0.41d |
| 4 | 2.42 ± 0.18d |
| 5 | 1.05 ± 0.11d |
bp < 0.01, compared with group 1; dp < 0.01, compared with group 2.
Table 3.
Effect of curcumin on myocardium SOD, CAT, GPx and GR activities.
| Group | SOD | CAT | GPx | GR |
|---|---|---|---|---|
| 1 | 153.85 ± 13.67 | 47.23 ± 3.79 | 67.39 ± 5.55 | 51.42 ± 4.93 |
| 2 | 48.38 ± 5.03b | 13.69 ± 1.72b | 23.29 ± 2.03b | 15.83 ± 1.33b |
| 3 | 94.14 ± 8.88d | 22.15 ± 2.61d | 44.37 ± 3.84d | 39.25 ± 3.55d |
| 4 | 132.5 ± 11.39d | 38.93 ± 3.06d | 52.92 ± 4.93d | 44.28 ± 4.15d |
| 5 | 144.57 ± 15.62d | 41.62 ± 3.77d | 61.36 ± 5.52d | 53.07 ± 4.91d |
bp < 0.01, compared with group 1; dp < 0.01, compared with group 2.
Compared with sham group, MIR rats demonstrated a significant increase in LDH and CK activities, while those of Ca2+-ATPase and Na+-K+-ATPase were significantly decreased (Table 4). Treatment of MIR rats with curcumin at 10, 20 or 30 mg/kg/d reduced the elevated LDH and CK activities. On the other hand, curcumin administration increased Ca2+-ATPase and Na+-K+-ATPase activities.
Table 4.
Effect of curcumin on myocardium LDH, CK-MB, Ca2+-ATPase and Na+-K+-ATPase activities.
| Group | LDH (U/mg protein) | CK (U/mg protein) | Ca2+-ATPase (μmol·mg protein−1·h−1) | Na+-K+-ATPase (μmol·mg protein−1·h−1) |
|---|---|---|---|---|
| 1 | 1.48 ± 0.13 | 2.29 ± 0.25 | 1.65 ± 0.14 | 3.28 ± 0.25 |
| 2 | 6.28 ± 0.49b | 7.49 ± 0.61b | 0.59 ± 0.05b | 1.27 ± 0.14b |
| 3 | 4.02 ± 0.35d | 5.27 ± 0.48d | 0.87 ± 0.07c | 2.06 ± 0.19d |
| 4 | 3.16 ± 0.28d | 4.11 ± 0.37d | 1.21 ± 0.11d | 2.66 ± 0.23d |
| 5 | 2.69 ± 0.23d | 3.52 ± 0.31d | 1.41 ± 0.13d | 2.95 ± 0.25d |
bp < 0.01, compared with group 1; cp < 0.05, dp < 0.01, compared with group 2.
The percentage of infarct size in MIR rats with curcumin at 10, 20 or 30 mg/kg/d decreased by 5.81% and 13.06% compared to IR (Figure 1).
Figure 1.
Effect of curcumin on myocardium infarction size. bp < 0.01, compared with group 1; dp < 0.01, compared with group 2.
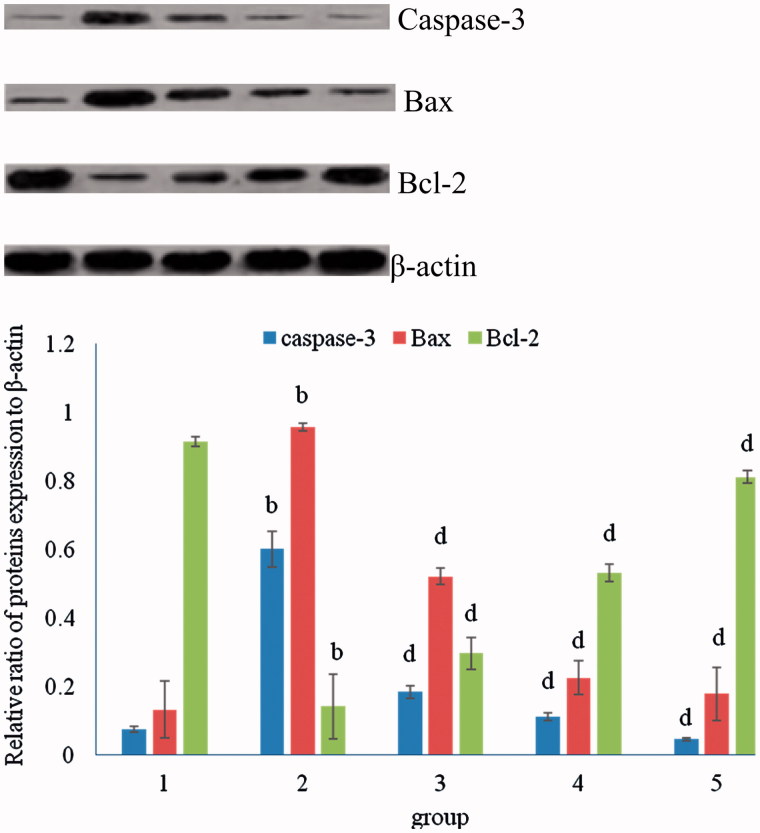
MIR significantly increased the myocardial expression of Bax, and Caspases-3 proteins and decreased the Bcl2 expression when compared to sham control rats. Curcumin pretreatment (10, 20 or 30 mg/kg/d) effectively reduced the myocardial expression of Bax and Caspase-3, and increased the Bcl2 level (Figure 2).
Figure 2.
Effect of curcumin on myocardium Caspase-3, Bax and Bcl-2 protein expression. bp < 0.01, compared with group 1; dp < 0.01, compared with group 2.
As shown in Figure 3, the phosphorylations of JAK2 and STAT3 were increased obviously after MIR compared to sham control group. In addition, the enhanced phosphorylation of STAT3 but not STAT1 was further strengthened by curcumin (10, 20 or 30 mg/kg/d) in a dose-dependent manner. By contrast, total JAK2 and STAT3 proteins expression did not obviously vary between groups.
Figure 3.
Effect of curcumin on myocardium JAK2, p-JAK2, STAT3 and p-STAT3 protein expression. bp < 0.01, compared with group 1; dp < 0.01, compared with group 2.
Discussion
Curcumin improved post-ischemic heart systolic and diastolic functions. Treatment of MIR rats with curcumin at 10, 20 or 30 mg kg−1 d−1 increased the LVDP, LVEDP, +dp/dtmax and − dp/dtmin values. These results suggest that curcumin could improve cardiac contractibility, attenuate hypercontraction and reduce diastolic pressure, which is believed to be a major reason for increased O2 demand.
Oxidative stress is a well-recognized factor of ischemia-reperfusion injury. It induces damage of lipids and proteins, and consequently might cause changes in the activity of transport systems (Murin et al. 2001). Strategies that target oxidative stress have been developed for the treatment of MI (Hu et al. 2015). Accordingly, we evaluated oxidative stress in rats treated with curcumin. Results revealed that different concentrations of curcumin attenuated MI-induced oxidative stress, as characterized by reduced ROS. These changes were dose-dependent and were the most pronounced in 30 mg/kg curcumin group.
Results indicated 10, 20 and 30 mg/kg curcumin following MI could inhibit myocyte apoptosis significantly. Therefore, this might be one of the mechanisms underlying the cardioprotective effects of curcumin. This could be ascribed to the protective effects against oxidative stress reported in the current study.
As important indicators of myocardial damage, the serum levels of LDH, CK-MB, Ca2+-ATPase and Na+-K+-ATPase, which are enzymes that are released from myocardial cells after ischemic injury, were monitored in all of the groups. The results further characterized and confirmed the cardioprotective effects of curcumin on cardiac myocytes in vivo, i.e. the decrease of the myocardium enzymes LDH, CK-MB and increase of myocardium Ca2+-ATPase and Na+-K+-ATPase, which are typical biomarkers of myocardial cell injury or death.
Caspase-3 is a key terminal molecular regulated apoptosis in cellular apoptosis pathways. Bcl-2 is essential to the process of apoptosis because it suppresses the initiation of the cell death process; moreover, Bax gene is the first identified pro-apoptotic member of the Bcl-2 protein family (Cory et al. 2003). In this study, the expression changes of Bcl-2 and Bax induced by curcumin treatment showed a signalling mechanism of antiapoptotic effect of curcumin. In this study, we showed that curcumin intake attenuates myocardial injury by inhibiting intrinsic apoptotic cascades in MIR rats. Curcumin pretreatment reduced Bcl-2/Bax ratio, inhibited procaspase-3 activation to cleaved caspase-3, and blocked DNA nick generation, all of which are steps involved in the intrinsic apoptotic cascades (Webster 2012; Oerlemans et al. 2013).
In the study, we focused on the potential role of JAK2–STAT3 pathway in curcumin-induced protection. This is because inactivation of STAT3 or deletion of STAT3 appears to be a key event in the diminution of cardioprotection in response to various physiological stresses including I/R (Boengler et al. 2008a; Barry et al. 2009; Bolli et al. 2011). Moreover, it has been shown that mice with a cardiomyocyte-restricted deletion of STAT3 develop spontaneous heart failure in response to stress (Jacoby et al. 2003; Hilfiker-Kleiner et al. 2004; Boengler et al. 2008b).
Taken together, the current findings demonstrate that curcumin exerts antioxidative and antiapoptotic effects on MI, which lead to the improved myocardial function and attenuated heart damage. Our results show that curcumin induced phosphorylation of JAK2 and STAT3, with upregulation of the myocardium Bcl-2/Bax expression and inactivation of caspase-3. These studies provide novel mechanistic insights into curcumin-induced cardioprotection, which may help in expanding the therapeutic utility of this drug in limiting myocardial infarction and apoptosis following I/R injury, in addition to its current use in drug-eluting stents to reduce coronary restenosis.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Ahuja S, Kohli S, Krishnan S, et al. 2011. Curcumin: a potential therapeutic polyphenol, prevents noradrenaline-induced hypertrophy in rat cardiac myocytes. J Pharm Pharmacol. 63:1604–1612. [DOI] [PubMed] [Google Scholar]
- Barry SP, Townsend PA, McCormick J, Knight RA, Scarabelli TM, Latchman DS, et al. 2009. STAT3 deletion sensitizes cells to oxidative stress . Biochem Biophys Res Commun. 385:324–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boengler K, Buechert A, Heinen Y, Roeskes C, Hilfiker-Kleiner D, Heusch G, et al. 2008b. Cardioprotection by ischemic postconditioning is lost in aged and STAT3-deficient mice. Circ Res. 102:131–135. [DOI] [PubMed] [Google Scholar]
- Boengler K, Hilfiker-Kleiner D, Drexler H, Heusch G, Schulz R.. 2008a. The myocardial JAK/STAT pathway: from protection to failure . Pharmacol Ther. 120:172–185. [DOI] [PubMed] [Google Scholar]
- Bolli R, Stein AB, Guo Y, Wang OL, Rokosh G, Dawn B, et al. 2011. A murine model of inducible, cardiac-specific deletion of STAT3: its use to determine the role of STAT3 in the upregulation of cardioprotective proteins by ischemic preconditioning. J Mol Cell Cardiol. 50:589–597. [DOI] [PubMed] [Google Scholar]
- Cho SO, Lim JW, Kim H.. 2013. Red ginseng extract inhibits the expression of MCP-1 and iNOS in Helicobacter pylori-infected gastric epithelial cells by suppressing the activation of NADPH oxidase and Jak2/Stat3. J Ethnopharmacol. 150:761–764. [DOI] [PubMed] [Google Scholar]
- Cory S, Huang DC, Adams JM.. 2003. The Bcl-2 family: roles in cell survival and oncogenesis. Oncogene 22:8590–8607. [DOI] [PubMed] [Google Scholar]
- Guo D, Li JR, Wang Y, Lei LS, Yu CL, Chen NN.. 2014. Cyclovirobuxinum D suppresses lipopolysaccharide-induced inflammatory responses in murine macrophages in vitro by blocking JAK-STAT signaling pathway. Acta Pharmacol Sin. 35:770–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilfiker-Kleiner D, Hilfiker A, Fuchs M, Kaminski K, Schaefer A, Schieffer B, et al. 2004. Signal transducer and activator of transcription 3 is required for myocardial capillary growth, control of interstitial matrix deposition, and heart protection from ischemic injury. Circ Res. 95:187–195. [DOI] [PubMed] [Google Scholar]
- Hu H, Zhai C, Qian G, Gu A, Liu J, Ying F, Xu W, Jin D, Wang H, Hu H, et al. 2015. Protective effects of tanshinone IIA on myocardial ischemia reperfusion injury by reducing oxidative stress, HMGB1 expression, and inflammatory reaction. Pharm Biol. 53:1752–1758. [DOI] [PubMed] [Google Scholar]
- Jacoby JJ, Kalinowski A, Liu MG, Zhang SS, Gao Q, Chai GX, et al. 2003. Cardiomyocyte-restricted knockout of STAT3 results in higher sensitivity to inflammation, cardiac fibrosis, and heart failure with advanced age . Proc Natl Acad Sci USA. 100:12929–12934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim OS, Park EJ, Joe EH, Jou I.. 2002. JAK-STAT signaling mediates gangliosides-induced inflammatory responses in brain microglial cells. J Biol Chem. 277:40594–40601. [DOI] [PubMed] [Google Scholar]
- Kloner RA, Przyklenk K, Whittaker P.. 1989. Deleterious effects of oxygen radicals in ischemia/reperfusion. Resolved and unresolved issues. Circulation 80:1115–1127. [DOI] [PubMed] [Google Scholar]
- Kumphune S, Surinkaew S, Chattipakorn SC, Chattipakorn N.. 2015. Inhibition of p38 MAPK activation protects cardiac mitochondria from ischemia/reperfusion injury. Pharm Biol. 53:1831–1841. [DOI] [PubMed] [Google Scholar]
- Lawrence RA, Burk RF.. 1976. Glutathione peroxidase activity in selenium deficient rat liver. Biochem Biophys Res Commun. 71:952–958. [DOI] [PubMed] [Google Scholar]
- Levraut J, Iwase H, Shao ZH, et al. 2003. Cell death during ischemia: relationship to mitochondrial depolarization and ROS generation. Am J Physiol Heart Circ Physiol. 284:H549–H558. [DOI] [PubMed] [Google Scholar]
- Mahmoud MF, El Bassossy HM.. 2014. Curcumin attenuates fructose-induced vascular dysfunction of isolated rat thoracic aorta rings. Pharm Biol. 52:972–977. [DOI] [PubMed] [Google Scholar]
- Morimoto T, Sunagawa Y, Kawamura T, et al. 2008. The dietary compound curcumin inhibits p300 histone acetyltransferase activity and prevents heart failure in rats. J Clin Invest. 118:868–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murin R, Drgova A, Kaplán P, et al. 2001. Ischemia/reperfusion-induced oxidative stress causes structural changes of brain membrane proteins and lipids. Gen Physiol Biophys. 20:431–438. [PubMed] [Google Scholar]
- Mylorie AA, Collins H, Umbles C, et al. 1986. Erythrocyte superoxide dismutase activity and other parameters of copper status in rats ingesting lead acetate . Toxicol Appl Pharmacol. 82:512–520. [DOI] [PubMed] [Google Scholar]
- Oerlemans MI, Koudstaal S, Chamuleau SA, et al. 2013. Targeting cell death in the reperfused heart: pharmacological approaches for cardioprotection. Int J Cardiol. 165:410–422. [DOI] [PubMed] [Google Scholar]
- Webster KA.2012. Mitochondrial membrane permeabilization and cell death during myocardial infarction: roles of calcium and reactive oxygen species. Future Cardiol. 8:863–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, Yu S, Zheng W, Feng G, Luo G, Wang L, Zhao Y.. 2010. Curcumin improves outcomes and attenuates focal cerebral ischemic injury via antiapoptotic mechanisms in rats. Neurochem Res. 35:374–379. [DOI] [PubMed] [Google Scholar]