Abstract
Context:Ampelopsis brevipedunculata Maxim (Vitaceae) is a traditional medicinal herb used for treating liver disorders.
Objective: The hepatoprotective effects of A. brevipedunculata ethanol extract (ABE) was investigated in experimental models of fibrosis.
Materials and methods: Hepatic stellate cells (HSCs) system in vitro and thioacetamide (TAA)-induced liver fibrosis rat model in vivo were used. Sprague–Dawley rats were divided into five groups of eight each (control, TAA, TAA with ABE 10 mg/kg, ABE 100 mg/kg and silymarin 50 mg/kg groups, respectively). Fibrosis was induced except to the control group by TAA (200 mg/kg, i.p.) twice per week for 13 weeks. ABE and silymarin was administered orally six times per week from the 7th week to the 13th week.
Results: In HSC-T6 cells, ABE (0.1 mg/mL) and silymarin (0.05 mg/mL) significantly (p < 0.01) induced apoptosis (12.94 ± 5.72% and 14.9 ± 3.8%, respectively) compared with control group (7.51 ± 1.26%). The expression of fibrosis related genes (TGF-β, α-SMA and Col1A1) in HSC-T6 cells were significantly (p < 0.01) downregulated in ABE-treated groups compared with control group. In in vivo studies, ABE (10 and 100 mg/kg) treatment ameliorated the altered levels of serum biomarkers significantly (p < 0.01 and p < 0.001) in TAA-induced groups. Further, ABE (10 and 100 mg/kg) significantly (p < 0.01) attenuated the altered histopathological findings, glutathione content and the accumulation of hydroxyproline.
Conclusion: These results collectively indicate that ABE can potentially be developed as a therapeutic agent in the treatment of hepatic fibrosis.
Keywords: Extracellular matrix, glutathione, hydroxyproline, apoptosis, reactive oxygen species, silymarin
Introduction
Liver fibrosis is a chronic disease state that typically results from dysfunctional wound healing in response to tissue injury (Giannandrea & Parks 2014). Historically, liver fibrosis was thought to be a passive and irreversible process due to the collapse of the hepatic parenchyma and its substitution with a collagen-rich tissue (Schaffner & Klion 1968; Popper & Uenfriend 1970). However, clinical reports have suggested that advanced liver fibrosis is potentially reversible (Soyer et al. 1976). Liver fibrosis is the common response of the liver to drugs, toxins, virus infections, or various metabolic agents and is characterized by excessive accumulation of extracellular matrix (ECM) caused by both increased synthesis and deposition of newly formed components. Increasing or unbalancing of the ECM ultimately leads to cirrhosis and cancer (Friedman et al. 2000; Wells 2005; Liu et al. 2006). Overproduction and irregular deposition of ECM in liver tissues lead to the distortion of hepatic microstructure and liver dysfunction (Rudolph et al. 2000). Thus, the stage of fibrosis is very important in the progress of liver disease.
The key cell type of liver fibrosis is hepatic stellate cells (HSCs), formerly known as lipocytes, Ito cells or perisinusoidal cells. In the normal liver, HSCs have been described as being in a quiescent state. They represent 5–8% of the total number of liver cells, store vitamin A and maintain homeostasis of the ECM. However, HSCs undergo phenotypic changes often characterized as “myofibroblastic activation” in liver fibrogenesis (Geerts 2001). Activated stellate cells secrete the ECM scar for protection in recovery from liver damages. However, if the liver does not recover, this proceeds to liver fibrosis, liver cirrhosis and liver cancer. Therefore, it is important to induce the apoptosis of HSCs or prevent the secretion of the ECM by HSCs (Lee et al. 2014).
Ampelopsis brevipedunculata Maxim (Vitaceae) is one of the several deciduous vine plants. The leaves, stem, fruit and roots have all been used to treat liver diseases with an effect that excels at restoring liver function (Yabe et al. 1998; Wu et al. 2004). The main components of A. brevipedunculata are tannins, sterols, triterpenoids and cardiac glycosides. In a recent study, A. brevipedunculata showed a strong reducing power from the methanol extract of stems and roots in a concentration-dependent manner and inhibited the oxidation of linoleic acid (Wu et al. 2004). A. brevipedunculata extract administered orally inhibited the progression of hepatic injury induced by carbon tetrachloride (Yabe & Matsui 2000) and reduced the increased lactate dehydrogenase (LDH) release in hepatocyte injury induced by Fe (II) (Yabe et al. 1998). In addition, the water extract of A. brevipedunculata exhibited an anti-tumour activity against perchloric acid and benzo[a]pyrene (Lee & Lin 1988). However, no scientific evidence exists regarding the anti-fibrotic effects of A. brevipedunculata. Thus, in the present study, we investigated the antifibrotic effects of A. brevipedunculata extracts in an in vitro system using HSCs and an in vivo system using thioacetamide (TAA)-induced liver fibrosis rat model.
Materials and methods
Reagents and chemicals
TAA and other reagents, including silymarin, hydroxyproline, p-dimethylaminobenzaldehyde,1,1,3,3-tetraethoxypropane(TEP), chloramines-T, 5,5-dithiobis-2-nitrobenzoic acid (DTNB), reduced glutathione, glutathione (GSH) reductase, GSH peroxidase (GSH-px), and β-nicotinamide adenine dinucleotide phosphate, reduced form (β-NADPH), were purchased from Sigma (St. Louis, MO); perchloric acid was obtained from GFS Chemical Co. (Columbus, OH). All other reagents used in this study were of highest grade available commercially.
Plant material and extraction
The plant material of A. brevipedunculata was purchased in June 2016 from Jecheon Chinese Medicinal Plant Co., South Korea and was authenticated by Prof. Jong-Bo Kim, a taxonomist at Konkuk University, South Korea, based on its microscopic and macroscopic characteristics. A voucher specimen (ABE-KU2016) was kept in our department herbarium for future reference. For extraction, the dried plant material of A. brevipedunculata (80 g) was ground to a fine powder and extracted with 800 mL ethanol (95%) using Soxhlet’s extraction technique for three days. The extract was then concentrated in a vacuum under reduced pressure and lyophilized. The final yield of the lyophilized A. brevipedunculata extract (ABE) was 13.5% (w/w) and was stored at 4 °C. The lyophilized powder of ABE was dissolved in 10% dimethyl sulfoxide (DMSO) and then filtered through a 0.22 μM syringe filter and stored as stock until use for each experiment. The final concentration of DMSO used for the study was not more than 0.1%.
Cell lines and culture
An immortalized rat HSC lines (HSC-T6) were received by Prof. Chang-Gue Son (Korean Hospital of Daejeon University, Korea). HSC-T6 cell lines were cultured in DMEM supplemented with 5% FBS, 1% antibiotic-antimycotic in a humidified atmosphere of 5% CO2 at 37 °C. Quiescent HSC cells were activated after FBS supplementation.
Primary HSCs isolation and culture
HSCs were isolated from 7-week-old male SD rats by in situ pronase, collagenase perfusion, and single-step Histogenz gradient as reported previously (Knook et al. 1982; Hendriks et al. 1985). Isolated HSCs were cultured in DMEM (GIBCO, Carlsbad, CA) containing 10% FBS (GIBCO, Carlsbad, CA) and 1% antibiotic-antimycotic (GIBCO, Carlsbad, CA) maintained in a humidified atmosphere of 5% CO2 at 37 °C. Growth medium was changed on a daily basis for 7 days.
Cell viability assay
Cell viability assays were evaluated by the 3-(4,5-dimethylthiazol-2yl)-2, 5-diphenyl-2 H-tetrazolium bromide (MTT) method. In a 96-well plate, HSC-T6 (6 × 105 cells/well) were cultivated in DMEM medium supplemented as described previously. Sample material was evaluated at various concentrations (0, 0.01, 0.1, 0.5, 1.0 mg/mL) for 24 h at 37 °C in an atmosphere of 5% CO2 and 95% humidity. The cells were then incubated with 0.5 mg/mL MTT (Sigma) for 3 h, and the reaction was interrupted by addition of dimethyl sulfoxide (DMSO, JUNSEI, Japan). An ELISA reader was used to obtain the results at 540 nm. The viabilities of the control cells were used as the control values at 100%.
Cell cycle analysis
HSC-T6 cells (15 × 105 cells/well) were cultured in DMEM (GIBCO, Carlsbad, CA) containing 10% FBS (GIBCO, Carlsbad, CA) and 1% antibiotic-antimycotic (GIBCO, Carlsbad, CA) maintained in a humidified atmosphere of 5% CO2 at 37 °C. Growth medium was changed on a daily basis for 7 days. For cell cycle analysis, sample materials were evaluated at ABE 0.1 mg/mL concentration for 24 h at 37 °C in an atmosphere of 5% CO2 and 95% humidity. After treatment for 24 h, cells were washed with PBS twice, suspended in 1 mL cold PI solution (50 μg/mL PI and 100 μg/mL RNase A). Next, the cells were incubated on ice for 30 min in the dark and then analyzed with a flow cytometer.
Apoptosis analysis
Apoptosis was discriminated by Annexin V-FITC and PI (FITC Annexin V Apoptosis Detection Kit I, BD Biosciences, San Jose, CA) and detected according to manufacturer’s instructions. Data analysis was performed with CellQuest software (Beckton Dickinson), which allowed assessing of specific population only. Individualization by gates was according to size (FSC), granularity (SSC), and fluorescent (FL) parameters. Both early apoptotic (Annexin V+ and PI−) and late apoptotic (Annexin V+ and PI+) cells were included in cell death determinations.
Quantitative real-time polymerase chain reaction (qRT-PCR)
Total RNA was extracted from liver tissue samples and HSC-T6 cells using TRIzol reagent (QIAGEN, Carlsbad, CA). cDNA was synthesized from total RNA (2 μg) in a 20 μL reaction using a high-capacity cDNA reverse transcription kit (Applied Biosystems, Foster City, CA). The primers for α-SMA, collagen type 1 α 1 (ColT1A1), TGF-β1, CTGF, and β-actin were as follows. α-SMA (forward sequence, 5′-AACACGGCATCATCACCAACT-3′; reverse sequence, 5′-TTTCTCCCGGTTGGCCTTA-3′, ColT1A1 (forward sequence, 5′-CCCAGCGGTGGTTATGACTT-3′; reverse sequence, 5′-GCTGCGGATGTTCTCAATCTG-3′), TGF-β1 (forward sequence, 5′-AGGAGACGGAATACAGGGCTTT-3′; reverse sequence, 5′-AGCAGGAAGGGTCGGTTCAT-3′), β-actin (forward sequence, 5′-CTAAGGCCAACCGTGAAAAGAT-3′; reverse sequence, 5′-GACCAGAGGCATACAGGGACAA-3′). The processes of reactions were according to manufacturer’s instructions. For analysis of data, the gene expression levels were compared with those of β-actin as a reference gene.
Animals and experiment design
Forty specific-pathogen-free Sprague–Dawley (SD) male rats (six-weeks old, 190-210 g) were purchased from a commercial animal breeder (Orient Bio, Gyeonggi-do, Korea). Animals were housed in conventional cages under control conditions of temperature (23 ± 3 °C), relative humidity (50 ± 20%) and 12 h light/dark cycle. After 1 week of acclimation, the rats were divided randomly into five groups of eight animals each: Normal, TAA (TAA only), ABE 10 (TAA with 10 mg/kg ABE), ABE 100 (TAA with 100 mg/kg ABE), and positive control (TAA with 50 mg/kg Silymarin). To induce liver fibrosis, TAA (200 mg/kg) was intra-peritoneally (i.p) injected twice a week for 13 weeks to four groups except normal group (injected normal saline, i.p). ABE (10 or 100 mg/kg), Silymarin (50 mg/kg), or distilled water was given by gastric gavage six times per week from the 7th week to the 13th week. Body weight was recorded once a week. After last drug administration, animals were fasted for 18 h, and then blood was collected from cardiac puncture under CO2 anaesthesia. Livers were removed to determine absolute and relative weight. A portion of liver tissue stored at −80 °C separately were used for hydroxyproline, GSH, protein expression determination. Liver tissue fixed in Bouin’s solution was processed for histo-morphological findings. A small portion of liver tissue fixed in RNAlater solution and was stored at −80 °C for gene expression studies. All animal experiments were approved by the Committee of Laboratory Animals according to institutional guidelines of Konkuk University, Korea (IACUC No. KU15017).
Serum biochemical analysis
Blood was collected via the cardiac puncture under CO2 anaesthesia on the final day of the experiment. Serum was separated using centrifuge (3000 g, 15 min) following blood clotting. The serum levels of aspartate transaminase (AST), and alanine transaminase (ALT) were determined using a GOT-GPT assay kit (Asan Pharmaceutical, Korea).
Determination of total GSH content in liver tissues
Total GSH was determined according to the method of Ellman (Evans & Ellman 1959). Briefly, duplicate 50 μL aliquots of the samples (or GSH standard) were combined with 80 μL of a previously prepared DTNB/NADPH mixture (10 μL 4 mM DTNB and 70 μL 0.3 mM NADPH) in a 96-well plate. Finally, 20 μL (0.06 U) of GSH reductase solution was added to each well and the absorbance was measured at 405 nm after 5 min.
Determination of hydroxyproline in liver tissues
Hydroxyproline determination was performed using a slight modification of a previous method (Takayama et al. 2003). Briefly, liver tissues (150 mg) stored at −70 °C were homogenized in 1 mL of 6 N HCl and incubated overnight at 100 °C. After passage of the acid hydrolysates through filter paper (Toyo Roshi Kaisha, Tokyo, Japan), 50 μL samples or hydroxyproline standards in 6 N HCl were air-dried. The dried samples were dissolved in methanol (50 μL), and then 1.2 mL of 50% isopropanol and 200 μL of chloramine-T solution were added to each, followed by incubation at room temperature for 10 min. Ehrlich’s solution (1.3 mL) was added, and the samples were incubated at 50 °C for 90 min. The optical density of the reaction product was read at 558 nm using a spectrophotometer (Tecan, Morrisville, NC). A standard curve was constructed using serial dilutions of 0.5 mg/mL hydroxyproline solutions.
Histopathology of liver tissue
Bouin’s solution fixed liver tissues were embedded in paraffin and cut into 5 μm thick sections for histomorphological examination. After drying, liver tissue section slides were stained with haematoxylin and eosin (H&E) and Masson’s trichrome. For the semiquantitative analysis of collagen expression, the blue-stained areas in the Masson’s trichrome stained sections were measured on an image analyzer (Image J, NIH, Bethesda, MD).
Statistical analysis
All the results are expressed as the mean ± standard error of the mean (S.E.M., n = 6). Statistical significant differences between groups were analyzed using one-way analysis of variance (ANOVA) followed by Student’s t-test. The value of p < 0.05 was considered as statistically significant.
Results
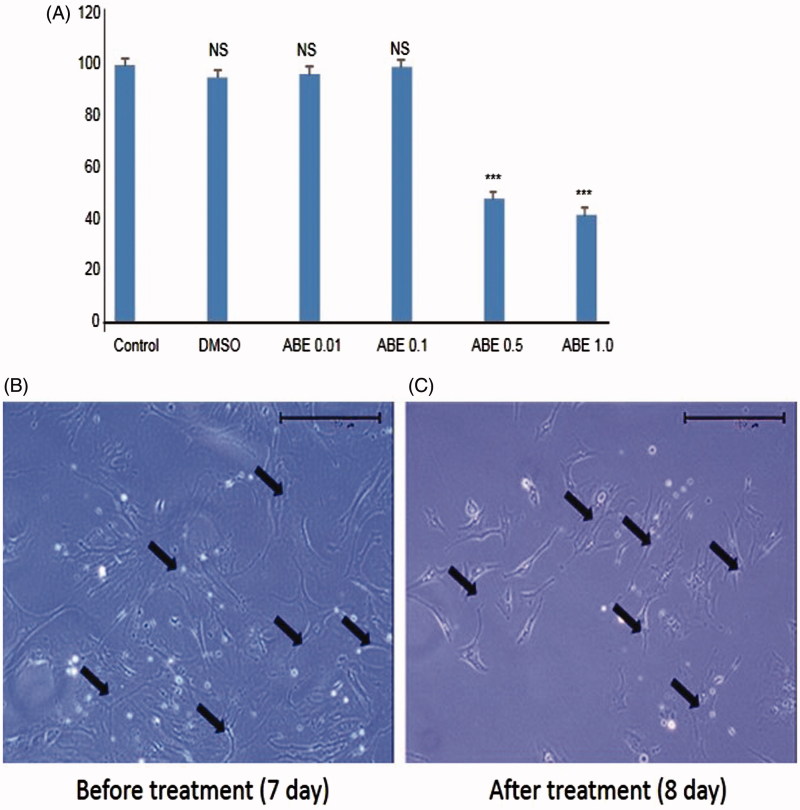
Cell viability assay and primary HSC morphology
ABE treated at indicated concentrations (0.01and 0.1 mg/mL) did not show any significant changes in the overall cell viability or produce toxicity in HSC-T6 cells. However, 0.5 and 1.0 mg/mL showed significant changes, negatively effecting the overall cell proliferation. Further the solvent, DMSO (0.1%) alone used for dissolving the ABE also did not show any toxicity in HSC-T6 cells. Therefore, all further experiments were done with ABE 0.1 mg/mL and/or 0.01 mg/mL as the concentrations were considered effective (Figure 1(A)) to study antifibrotic activity in vitro.
Figure 1.
The cell viability assay in HSC-T6 and morphological changes in primary HSCs on treatment with ABE. (A) HSC-T6 cells were incubated with ABE at indicated concentrations for 24 h and the cell viability was determined by MTT assay. (B) Primary HSCs were cultivated for 1 week and exposed to the ABE 0.1 mg/mL for 24 h. Pictures were taken after 24 h treatment with ABE. Magnification was 100X. Arrows indicate HSCs. The data are expressed as means ± SEM (n = 6), using one-way analysis of variance (ANOVA) followed by Student’s t-test. ***p < 0.001, compared with control group. NS: Not significant compared with control group.
As shown in Figure 1(B), untreated activated HSCs showed normal morphology (7th day). In the presence of ABE 0.1 mg/mL for 24 h (8th day), cultured primary HSCs showed shrinking collagen fibre morphology (Figure 1(C)). Treatment with ABE decreased the number of viable HSCs. Further, decreased stretched fibres were observed after 24 h when compared to the untreated activated HSCs. This clearly indicates that ABE influenced the morphology of the cultured activated HSCs.
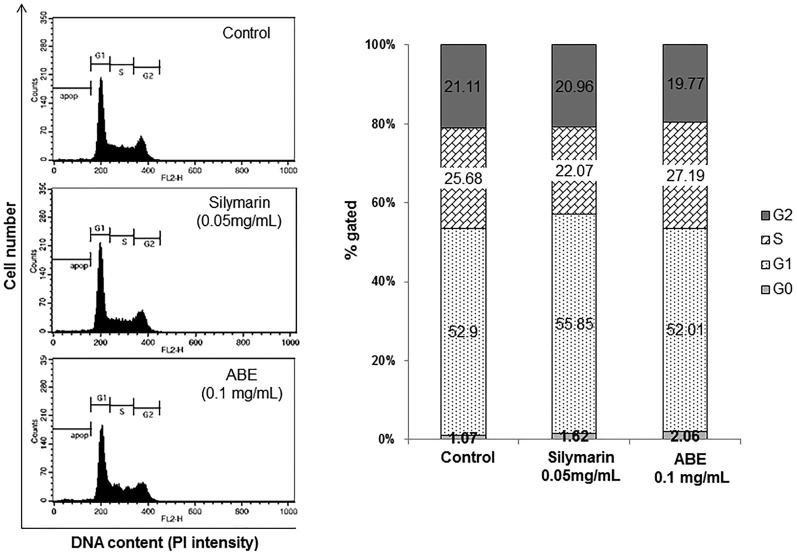
Cell cycle analysis
Flow cytometric analysis of ABE 0.1 mg/mL treated HSC-T6 cells showed marked effect with 2.06% of the cells compared to the non-treated cells showing a distribution of 1.07% of the cells in the sub-G1 phase. Silymarin also exerted effects with 1.62% of the cells in the sub-G1 phase. These results show that ABE treatment has mild effects including the induction of cell death in HSC-T6 cells (Figure 2).
Figure 2.
Effect of ABE on the cell cycle in HSC-T6 cells. DNA contents in different phases of the cell cycle were measured using propidium iodide by flow cytometry. The cell cycle distribution and the percentage of the cell cycle distribution were represented by graphs (A) and histogram (B), respectively.
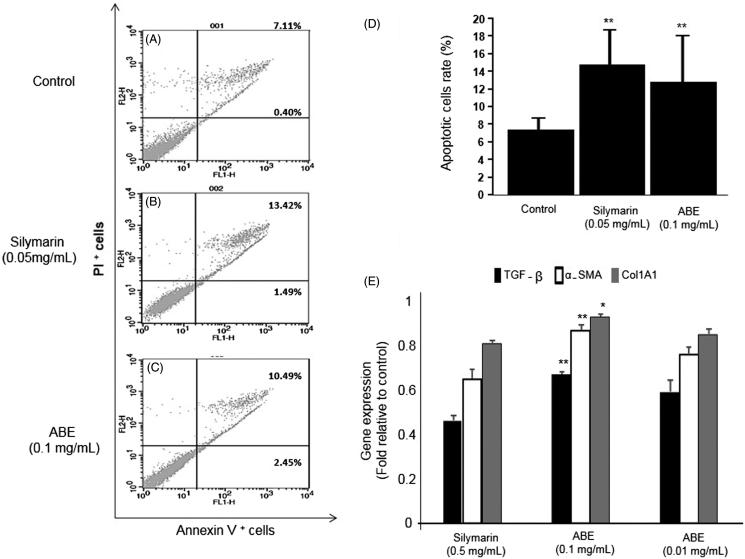
Apoptosis analysis
In order to verify the apoptosis effect in HSCs, apoptosis of HSC-T6 cells was distinguished by Annexin V-FITC and PI staining. HSC-T6 cells were treated with silymarin 0.05 mg/mL and ABE 0.1 mg/mL (ABE 100) for 24 h. As indicated by the Annexin V-FITC/PI assay, ABE and silymarin markedly increased apoptosis when compared with control group in HSC-T6 cells (Figure 3(A–C)). The percentage of cells undergoing apoptotic cell death increased from 7.51 ± 1.26 to 14.9 ± 3.8 in silymarin group and 12.94 ± 5.72% in ABE-treated group, respectively, for 24 h. Compared with the Annexin V positive cells in control group, ABE and silymarin had about two times more Annexin V positive cells (Figure 3(D)). These results show that ABE significantly (p < 0.01) induced apoptosis in HSC-T6 cells.
Figure 3.
Effect of ABE on apoptosis and fibrosis expression in HSC-T6 cells. (A) Control cells. Flow cytometric data indicate apoptosis in HSC-T6 cells after incubation with Silymarin (B), ABE 0.1 mg/mL (C) for 24 h. (D) Data showed the apoptotic (Annexin V+ and PI−) and late apoptotic (Annexin V+ and PI+) cells. (E) Fibrosis related gene expression. The data are represented as mean ± SEM (n = 6) using one-way analysis of variance (ANOVA) followed by Student’s t-test. *p < 0.05, **p < 0.01 and ***p < 0.001, as compared with control group.
Fibrosis related gene expression in HSCs
Gene expression associated with fibrosis was analyzed to verify the fibrosis suppression effect in HSC-T6 cells. TGF-β, which induces fibrosis and activates HSCs, was significantly down-regulated in both the ABE 0.1 mg/mL and ABE 0.01 mg/mL treatment groups when compared with control treated group. Further, α-SMA and Col1A1, which induce ECM accumulation, were also down-regulated significantly in ABE-treated groups when compared with that of the control treated group. However the positive control silymarin exhibited superior effect in regulating the fibrosis suppression effects when compared with ABE-treated groups (Figure 3(E)).
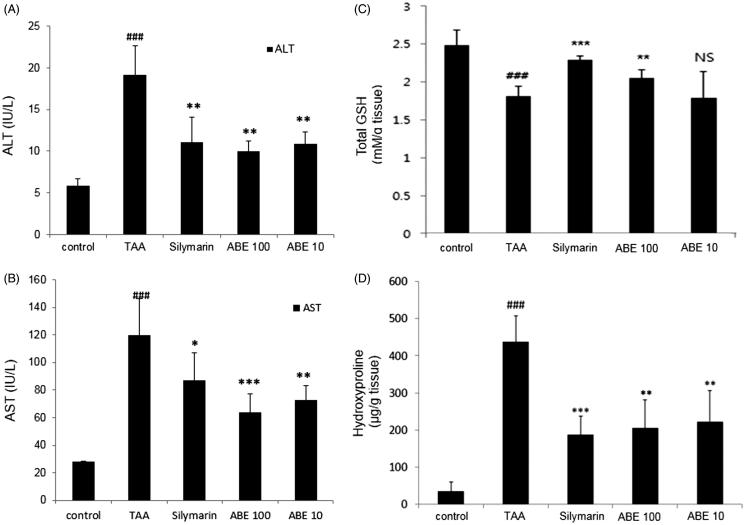
Serum biochemical analysis
TAA treatment significantly elevated the serum AST and ALT levels when compared with control group. The elevated levels of AST and ALT were significantly attenuated by ABE 100 and ABE 10 treatment when compared with TAA treated group. Although not significant, similar results were observed with silymarin treatment when compared with ABE-treated groups (Figure 4(A,B).
Figure 4.
Effect of ABE on AST/ALT levels, total glutathione (GSH) content and hydroxyproline levels in TAA-induced liver fibrosis rats. (A) HSC-T6 cells were incubated with ABE 0.1 and 0.01 mg/mL for 24 h. Fibrosis-related genes expression in HSC-T6 cells were determined by real-time PCR. The results are expressed as normalized fold values relative to the control. Levels of AST (A) and ALT (B) in serum were measured using spectrophotometry. (C) Total GSH contents in liver tissue were measured using spectrophotometry. (D) Hydroxyproline levels from TAA-induced liver tissue of rats. TAA: Thioacetamide-induced liver fibrosis rats, Silymarin: Positive control rats, ABE 100: ABE 100 mg/kg treated rats, ABE 10: ABE 10 mg/kg treated rats. The data are expressed as means ± SEM (n = 6) using one-way analysis of variance (ANOVA) followed by Student’s t-test. ###p < 0.001 as compared with control group, *p < 0.05, **p < 0.01, ***p < 0.001 as compared with TAA group.
Determination of the total glutathione (GSH) content in liver tissues
It was well known that TAA cause liver injury through reactive oxygen species (ROS) damage which is associated with antioxidant enzymes. Therefore, the total GSH content were measured in the liver tissue. TAA treatment significantly decreased (p < 0.001) the total GSH content in the liver tissue compared with control group. ABE 100 treatment significantly (p < 0.01) increased the GSH content. However, the restored level of the GSH content was not statistically significant between the TAA and ABE 10 group (Figure 4(C)). The positive control silymarin also significantly (p < 0.001) attenuated the TAA-induced decrease in GSH levels.
Determination of hydroxyproline in liver tissues
The hydroxyproline content in liver tissue was significantly increased in the TAA group compared to the normal group (p < 0.01). ABE treatment at both concentrations significantly reduced hydroxyproline levels compared with TAA group (Figure 4(D)). The silymarin treatment also showed a positive effect in reducing hydroxyproline.
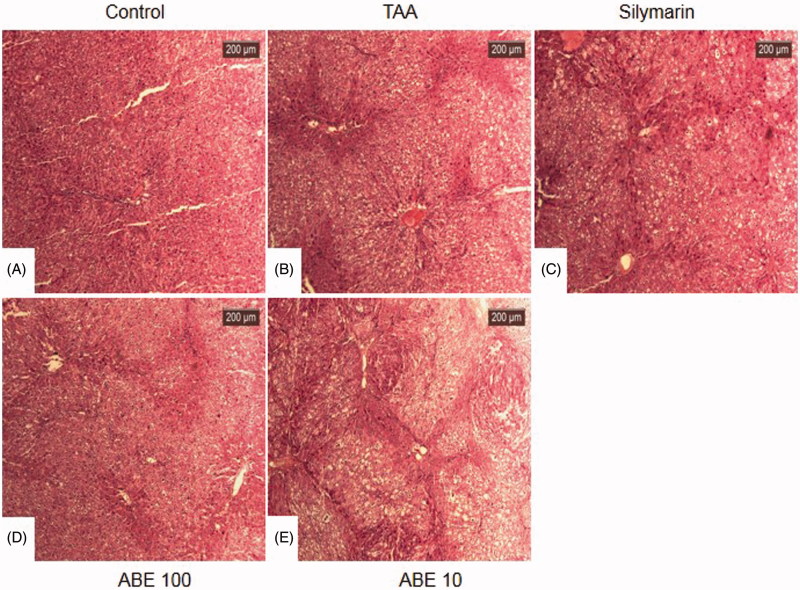
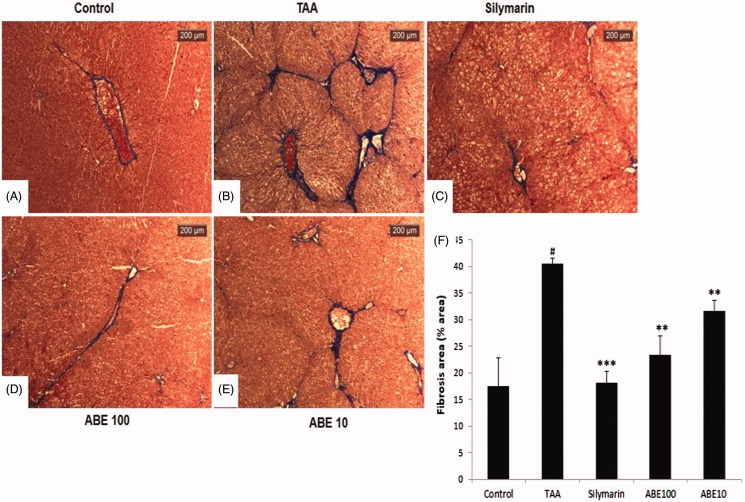
Histopathology of liver tissues
In the liver sections, control group showed normal morphology (Figure 5(A)). TAA treatment induced a shrunken, solidified and abnormally patterned liver due to the formation of numerous regenerative nodules (Figure 5(B)). The histological observation revealed severe pathological alterations by TAA treatment. However, ABE 100 and silymarin treatment dramatically attenuated these changes (Figure 5(C,D)). No obvious difference was observed between the ABE 10 and TAA treatments (Figure 5(E)). Masson’s trichrome showed severe collagen accumulation (part of the blue staining) in the TAA group while the ABE 100 treated group remarkably protected against collagen accumulation (Figure 6(A–E)). Percentage area of fibrosis revealed significant damage in TAA-treated group compared with control group. However, ABE at both concentrations ameliorated these changes significantly. Silymarin also exhibited significant attenuating affect when compared with TAA-treated group (Figure 6(F)).
Figure 5.
Haematoxylin and eosin stain of liver tissues. At the end of the experiment, all of the animals were sacrificed and livers were fixed in Bouin’s solution. After staining with haematoxylin and eosin, liver sections were taken under light microscopy. Control: naive rats (A), TAA: TAA-induced liver fibrosis rats (B), Silymarin: Positive control rats (C), ABE 100: ABE 100 mg/kg treated rats (D), ABE 10: ABE 10 mg/kg treated rats (E), Scale bar =200 μM.
Figure 6.
Masson’s trichrome stain of liver tissues. This stain was performed like H&E stain. Control: naive rats (A), TAA: TAA-induced liver fibrosis rats (B), Silymarin: Positive control rats (C), ABE 100: ABE 100 mg/kg treated rats (D), ABE 10: ABE 10 mg/kg treated rats (E), Fibrosis are plot (F). Scale bar =200 μM. Quantification was done using ImageJ. Values are represented as mean ± SEM (n = 6) using one-way analysis of variance (ANOVA) followed by Student’s t-test. #p < 0.05 as compared with control group, **p < 0.01, ***p < 0.001 as compared with TAA group. TAA: Thioacetamide-induced liver fibrosis rats, Silymarin: Positive control rats, ABE 100: ABE 100 mg/kg treated rats, ABE 10: ABE 10 mg/kg treated rats.
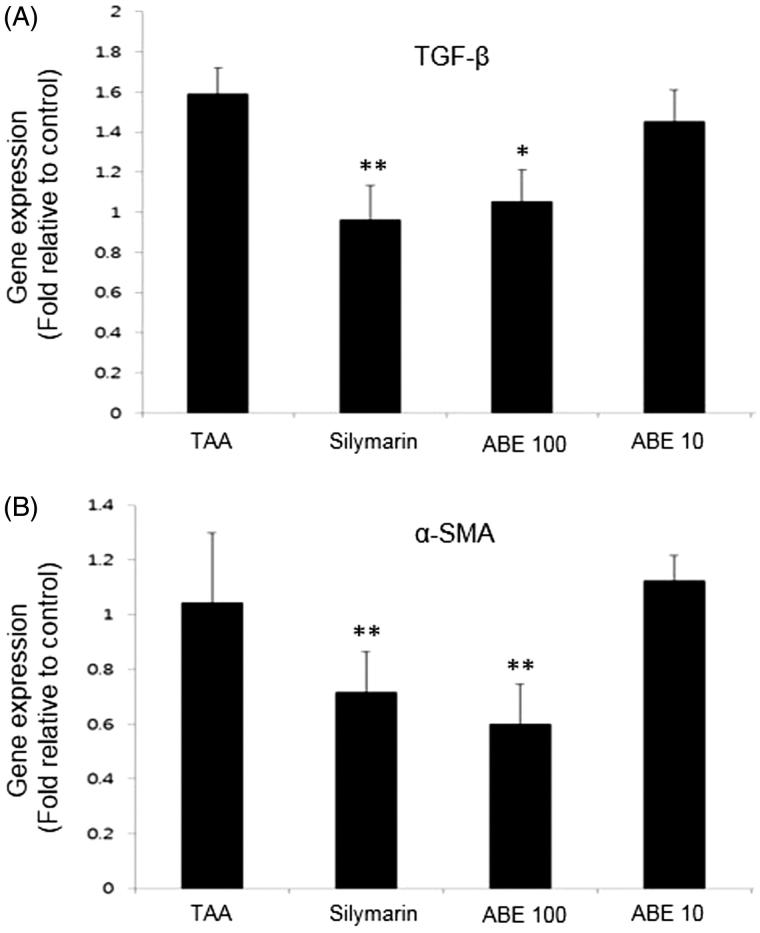
Fibrosis related gene expression in the liver tissues
Expression of fibrosis associated genes in liver tissue was analyzed to investigate the hepatoprotective mechanism with RT- PCR. TAA treatment up-regulated the gene expression of α-SMA and TGF-β, while ABE 100 and positive control silymarin treated groups down-regulated the gene expression of α-SMA and TGF-β (Figure 7(A,B)). However, ABE 10 treated group did not show any effect. Further, silymarin treated group exhibited superior effect than ABE-treated group in down regulating TGF-β expression, which was in agreement with in vitro data (Figure 7).
Figure 7.
Fibrosis-related gene expression analysis in the liver tissues. Fibrosis related gene expressions of liver tissue were determined by real-time PCR. (A) TGF-β, (B) α-SMA. The results are expressed as normalized fold values relative to the control. Values are represented as mean ± SEM (n = 6) using one-way analysis of variance (ANOVA) followed by Student’s t-test. *p < 0.05, **p < 0.01, ***p < 0.001 as compared to TAA group. TAA: Thioacetamide-induced liver fibrosis rats, Silymarin: Positive control rats, ABE 100: ABE 100 mg/kg treated rats, ABE 10: ABE 10 mg/kg treated rats.
Discussion
Activation of HSCs is known to be responsible for hepatic fibrosis (Parola et al. 2008). Hepatic damage has become a serious health problem due to the utilization of several prescription drugs and exposure to various toxins. Natural products, especially herbs with immense medicinal history of exhibiting beneficial effects against liver diseases are considered an alternative therapeutic approach (Khanna et al. 2007). In the present study, the ethanol extract of A. brevipedunculata was examined as a promising therapy for treating hepatofibrosis in cellular and experimental rat model.
In in vitro studies, ABE at 0.1 mg/mL concentration inhibited that HSC activation and the associated fibrogenic events. It is well documented that suppression of activation or fibrogenesis and induction of apoptosis, in HSCs have been proposed as therapeutic strategies against liver fibrosis. When round-shape quiescent HSCs undergo activation by liver damage, the production of ECM is increased, and their shape changes resembling myofibroblasts (Kisseleva & Brenner 2007). Activated HSCs are characterized by a high rate of proliferation and increased production of ECM which is collagen scar around cells. Lipid droplets within the cells are a storage site for vitamin A and they are the main extracellular matrix-producing cell type within the liver. Thus, morphological changes in the lipid droplets that decrease stretching fibres mean the inhibition of activated HSCs. These characteristics of HSCs were used to identify the antifibrotic effect of ABE. In this study, ABE treated at 0.1 mg/mL significantly inhibited the activation and altered the morphology of HSCs.
Since HSCs play a critical role in the pathogenesis of hepatic fibrosis, induction of HSC apoptosis has become potentially important for the prevention or treatment of hepatic fibrosis (Elsharkawy et al. 2005; Henderson & Iredale 2007). Enhanced HSC apoptosis may reduce the formation of procollagen and increase extracellular matrix degradation, aiding the recovery from hepatic fibrosis. Further, ABE (0.1 mg/mL) down regulated the gene expression of TGF-β, α-SMA, a marker of HSC activation and Col1A1in HSCs in vitro.
It is well known that TAA is a potent hepatotoxic agent and frequently used to develop a hepatofibrosis model in experimental animals. In the present study, TAA (200 mg/kg, i.p.) was injected twice a week for 13 weeks to produce hepatic damage. ALT and AST are aminotransferase enzymes present in hepatocytes. They are measured as the main markers in liver function tests (LFT). These enzymes are secreted into the blood when the liver is damaged. Therefore, they are used as markers of liver function when liver cells are damaged (Kim et al. 2010). In the present study, ABE 100 and ABE 10 groups significantly reduced the level of these enzymes compared to the increase induced by TAA. The inhibitory effect of ABE on these serum markers might also involve in the reduction of inflammatory events, a highly beneficial property of a therapy for hepatic injury and fibrosis. In addition, TAA-induced damaged morphology was returned to normal in the ABE-treated groups, as shown by the H&E staining. Moreover, the fibrosis area was recovered in the ABE-treated groups as indicated by Masson’s trichrome staining. Further, hydroxyproline one of the key factors in stabilizing collagens (Krane 2008; Palfi & Perczel 2008), and its instability or abnormal activity may cause cancer (Guszczyn & Sobolewski 2004; Sunila & Kuttan 2006; Guruvayoorappan & Kuttan 2008). Therefore, identifying hydroxyproline in proteins may provide useful information for biomedical research and drug development (Xu et al. 2014). In the present study, TAA-induced and significant increase in the hydroxyproline levels and ABE at both concentrations significantly ameliorated this increase in rat liver tissues. Glutathione (GSH) plays an important role in cellular detoxification, because it effectively scavenges free radicals and other ROS. In the present study, the total GSH levels were decreased in TAA-induced rats, however, treatment with ABE 100 attenuated the decreased GSH levels significantly (p < 0.01).
TGF-β1 has a central role in fibrogenesis which is a particularly well-studied cytokine and widely regarded as a pro-fibrogenic agent in liver injury, particularly after chronic liver injury (Liu et al. 2006). α-SMA is an actin isoform and a specific marker for smooth muscle cell differentiation. Therefore, α-SMA expression has been used to identify activated HSCs that show a myofibroblastic phenotype (Carpino et al. 2005). TAA-induced increased levels of TGF-β and α-SMA expression was significantly reduced in ABE 100 group.
Silymarin the positive control used in this study is well regarded as a potent agent for its antioxidant and protective effects on the liver (Saller et al. 2001; Wu et al. 2009). In agreement, in the present study, silymarin exhibited hepatoprotective effects both in vitro (0.5 mg/mL) and in vivo (50 mg/mL), however, the effects were inferior when compared with ABE 0.1 mg/mL treated group in vitro and ABE 100 mg/kg in vivo.
Ampelopsis brevipedunculata contains several active constituents including tannins, sterols, triterpenoids and cardiac glycosides (Rashed et al. 2015). Some of these compounds were reported to possess strong antioxidant and hepatoprotective effects (Kundakovic et al. 2008; Rashed et al. 2015). The compounds present in the ABE might act synergistically in delivering potent antihepatofibrotic effects. Isolation of active constituents present in ABE and exploring the detailed mechanism is quite necessary.
Conclusion
In conclusion, ABE showed hepatoprotective effects evidenced by the increased apoptosis and inhibited ECM accumulation in HSC-T6 cells. Furthermore, the results show that ABE possess hepatic protective effect and antifibrotic effect in a TAA-induced chronic liver fibrosis model. The results of this study suggest that ABE can be an effective treatment against oxidative-stress-induced liver fibrosis.
Acknowledgements
This work was supported by Konkuk University in the year 2016.
Disclosure statement
The authors report no declarations of interest.
References
- Carpino G, Morini S, Ginanni CS, Franchitto A, Merli M, Siciliano M, Gentili F, Onetti MA, Berloco P, Rossi M, et al. . 2005. Alpha-SMA expression in hepatic stellate cells and quantitative analysis of hepatic fibrosis in cirrhosis and in recurrent chronic hepatitis after liver transplantation. Dig Liver Dis. 37:349–356. [DOI] [PubMed] [Google Scholar]
- Elsharkawy AM, Oakley F, Mann DA.. 2005. The role and regulation of hepatic stellate cell apoptosis in reversal of liver fibrosis. Apoptosis. 10:927–939. [DOI] [PubMed] [Google Scholar]
- Evans JC, Ellman GL.. 1959. The ionization of cysteine. Biochim Biophys Acta. 33:574–576. [DOI] [PubMed] [Google Scholar]
- Friedman SL, Maher JJ, Bissell DM.. 2000. Mechanisms and therapy of hepatic fibrosis: report of the AASLD single topic basic research conference. Hepatology. 32:1403–1408. [DOI] [PubMed] [Google Scholar]
- Geerts A.2001. History, heterogeneity, developmental biology, and functions of quiescent hepatic stellate cells. Semin Liver Dis. 21:311–335. [DOI] [PubMed] [Google Scholar]
- Giannandrea M, Parks WC.. 2014. Diverse functions of matrix metalloproteinases during fibrosis. Dis Model Mech. 7:193–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guruvayoorappan C, Kuttan G.. 2008. Anti-metastatic effect of Biophytum sensitivum is exerted through its cytokine and immunomodulatory activity and its regulatory effect on the activation and nuclear translocation of transcription factors in B16F-10 melanoma cells. J Exp Ther Oncol. 7:49–63. [PubMed] [Google Scholar]
- Guszczyn T, Sobolewski K.. 2004. Deregulation of collagen metabolism in human stomach cancer. Pathobiology. 71:308–313. [DOI] [PubMed] [Google Scholar]
- Henderson NC, Iredale JP.. 2007. Liver fibrosis: cellular mechanisms of progression and resolution. Clin Sci (Lond). 112:265–280. [DOI] [PubMed] [Google Scholar]
- Hendriks HF, Verhoofstad WA, Brouwer A, de Leeuw AM, Knook DL.. 1985. Perisinusoidal fat-storing cells are the main vitamin A storage sites in rat liver. Exp Cell Res. 160:138–149. [DOI] [PubMed] [Google Scholar]
- Khanna D, Sethi G, Ahn KS, Pandey MK, Kunnumakkara AB, Sung B, Aggarwal A, Aggarwal BB.. 2007. Natural products as a gold mine for arthritis treatment. Curr Opin Pharmacol. 7:344–351. [DOI] [PubMed] [Google Scholar]
- Kim HW, Ha TH, Cho MR, Cho SI.. 2010. Effects of herbal remedy for diabetes mellitus-01 (HRDM-01) on liver and serum lipid level in diabetic rats. Kor J Herbology. 25:117–121. [Google Scholar]
- Kisseleva T, Brenner DA.. 2007. Role of hepatic stellate cells in fibrogenesis and the reversal of fibrosis. J Gastroenterol Hepatol. 22:S73–S78. [DOI] [PubMed] [Google Scholar]
- Knook DL, Seffelaar AM, de Leeuw AM.. 1982. Fat-storing cells of the rat liver. Their isolation and purification. Exp Cell Res. 139:468–471. [DOI] [PubMed] [Google Scholar]
- Krane SM.2008. The importance of proline residues in the structure, stability and susceptibility to proteolytic degradation of collagens. Amino Acids. 35:703–710. [DOI] [PubMed] [Google Scholar]
- Kundakovic T, Stanojkovic T, Milenkovic M, Grubin J, Juranic Z, Stevanovic B, Kovacevic N.. 2008. Cytotoxic, antioxidant, and antimicrobial activities of Ampelopsis brevipedunculata and Parthenocissus tricuspidata (Vitaceae). Arch Biol Sci. 60:641–647. [Google Scholar]
- Lee H, Lin JY.. 1988. Antimutagenic activity of extracts from anticancer drugs in Chinese medicine. Mutat Res. 204:229–234. [DOI] [PubMed] [Google Scholar]
- Lee JJ, Yang SY, Kim DH, Hur SJ, Lee JD, Yum MJ, Song MD.. 2014. Liver fibrosis protective effect of Hovenia dulcis fruit. Curr Topics Nutra Res. 12:43–50. [Google Scholar]
- Liu X, Hu H, Yin JQ.. 2006. Therapeutic strategies against TGF-beta signaling pathway in hepatic fibrosis. Liver Int. 26:8–22. [DOI] [PubMed] [Google Scholar]
- Palfi VK, Perczel A.. 2008. How stable is a collagen triple helix? An ab initio study on various collagen and beta-sheet forming sequences. J Comput Chem. 29:1374–1386. [DOI] [PubMed] [Google Scholar]
- Parola M, Marra F, Pinzani M.. 2008. Myofibroblast - like cells and liver fibrogenesis: emerging concepts in a rapidly moving scenario. Mol Aspects Med. 29:58–66. [DOI] [PubMed] [Google Scholar]
- Popper H, Uenfriend S.. 1970. Hepatic fibrosis. Correlation of biochemical and morphologic investigations. Am J Med. 49:707–721. [DOI] [PubMed] [Google Scholar]
- Rashed K, Said A, Feitosa C, Sucupira ACC.. 2015. Evaluation of anti-alzheimer activity of Ampelopsis brevipedunculata and the isolated compounds. Res J Phytochem. 9:16–24. [Google Scholar]
- Rudolph KL, Chang S, Millard M, Schreiber-Agus N, DePinho RA.. 2000. Inhibition of experimental liver cirrhosis in mice by telomerase gene delivery. Science. 287:1253–1258. [DOI] [PubMed] [Google Scholar]
- Saller R, Meier R, Brignoli R.. 2001. The use of silymarin in the treatment of liver diseases. Drugs. 61:2035–2063. [DOI] [PubMed] [Google Scholar]
- Schaffner F, Klion FM.. 1968. Chronic hepatitis. Annu Rev Med. 19:25–38. [DOI] [PubMed] [Google Scholar]
- Soyer MT, Ceballos R, Aldrete JS.. 1976. Reversibility of severe hepatic damage caused by jejunoileal bypass after re-establishment of normal intestinal continuity. Surgery. 79:601–604. [PubMed] [Google Scholar]
- Sunila ES, Kuttan G.. 2006. A preliminary study on antimetastatic activity of Thuja occidentalis L. in mice model. Immunopharmacol Immunotoxicol. 28:269–280. [DOI] [PubMed] [Google Scholar]
- Takayama T, Fujita K, Suzuki K, Sakaguchi M, Fujie M, Nagai E, Watanabe S, Ichiyama A, Ogawa Y.. 2003. Control of oxalate formation from l-hydroxyproline in liver mitochondria. J Am Soc Nephrol. 14:939–946. [DOI] [PubMed] [Google Scholar]
- Wells RG.2005. The role of matrix stiffness in hepatic stellate cell activation and liver fibrosis. J Clin Gastroenterol. 39:S158–S161. [DOI] [PubMed] [Google Scholar]
- Wu JW, Lin LC, Tsai TH.. 2009. Drug-drug interactions of silymarin on the perspective of pharmacokinetics. J Ethnopharmacol. 121:185–193. [DOI] [PubMed] [Google Scholar]
- Wu MJ, Yen JH, Wang L, Weng CY.. 2004. Antioxidant activity of Porcelain berry (Ampelopsis brevipedunculata (Maxim.) Trautv.). Am J Chin Med. 32:681–693. [DOI] [PubMed] [Google Scholar]
- Xu Y, Wen X, Shao XJ, Deng NY, Chou KC.. 2014. iHyd-PseAAC: predicting hydroxyproline and hydroxylysine in proteins by incorporating dipeptide position-specific propensity into pseudo amino acid composition. Int J Mol Sci. 15:7594–7610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yabe N, Matsui H.. 2000. Ampelopsis brevipedunculata (Vitaceae) extract inhibits a progression of carbon tetrachloride-induced hepatic injury in the mice. Phytomedicine. 7:493–498. [DOI] [PubMed] [Google Scholar]
- Yabe N, Tanaka K, Matsui H.. 1998. An ethanol-extract of Ampelopsis brevipedunculata (Vitaceae) berries decreases ferrous iron-stimulated hepatocyte injury in culture. J Ethnopharmacol. 59:147–159. [DOI] [PubMed] [Google Scholar]