Abstract
Context: Tea (Camellia sinensis (L.) Kuntze [Theaceae]) is used to induce urination and inducing nervous excitation. Green and black teas have multifarious physiological functions. The different effects of green and black tea aqueous extracts (GTEs and BTEs) on hyperuricemia are not definitely reported.
Objective: The different effects of GTEs and BTEs on lowering serum uric acid (UA) in hyperuricemic mice were determined.
Materials and methods: Kunming mice were divided into nine groups (n = 6/each group). GTEs and BTEs at the doses of 0.5, 1 and 2 g/kg were orally administrated to mice for seven days, respectively. Hepatic xanthine oxidase (XOD) and adenosine deaminase (ADA) activities as mechanisms of actions were assessed.
Results: Research indicated that the LD50 of tea extract is greater than 2 g/kg in mice. UA levels were suppressed significantly with dose-dependent treatment of 0.5, 1 and 2 g/kg BTEs (up to 25.5%, 28.7% and 29.8%, respectively); the serum UA levels were decreased by GTEs but not significant. The activities of XOD and ADA in high dose (2 g/kg) groups of both GTEs and BTEs were notably lower than those of the model group.
Discussion and conclusions: The results suggested that both GTEs and BTEs have hypouricaemic and renal protective effects on hyperuricemic mice and the latter one was better. Our study sheds light on the research and development of anti-hyperuricemic functional foods and drugs from tea.
Keywords: Hyperuricemia, hepatoprotective, xanthine oxidase
Introduction
Hyperuricemia, resulting from elevated urate concentrations in the blood, is a pathological condition which may result from the increase in purine metabolism and/or impairment of renal clearance of uric acid (UA) (Merriman and Dalbeth 2011). As the primary risk factor of gout, hyperuricemia has been shown in clinical reports to be also associated with chronic nephritis, renal dysfunction and metabolic syndromes (Lin et al. 2000; Iseki et al. 2001, 2004; Ishizaka et al. 2005; Dawson et al. 2007). Allopurinol (AP) is the most common clinically used xanthine oxidase (XOD) inhibitor prescribed for the treatment of gout. However, its usage is limited by hypersensitivity problems (Hammer et al. 2001), Stevens–Johnson syndrome (Fritsch and Sidoroff 2000), renal toxicity (Horiuchi et al. 2000) and even fatal liver necrosis (Pereira et al. 1998). Many natural products possess protective effect against hyperuricemia, such as mangiferin (Niu et al. 2012), cassia oil (Zhao et al. 2006), Smilax china L. (Liliaceae) (Chen et al. 2011) and Smilax riparia (Liliaceae) (Wu et al. 2015), which showed obvious effects on reducing serum UA.
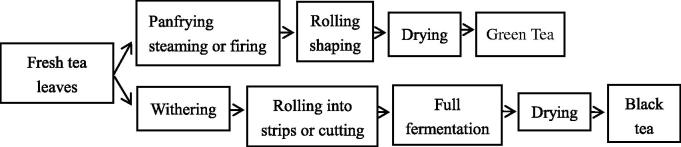
Tea (Camellia sinensis (L.) Kuntze [Theaceae]) is the most popular flavoured and healthy beverage beyond water in the world (Jiang et al. 2015). Accounting for about 78% of the worldwide tea production is black tea (Sang et al. 2011). The health benefits of tea and tea extracts have been well documented, especially with respect to chemopreventive effects on cancers, cardiovascular diseases and inflammation (Widlansky et al. 2005; Stangl et al. 2006; Yang et al. 2006). Green tea and black tea are different types of tea. To clearly understand the differences of green tea and black tea, the manufacturing processes of them are profiled in Figure 1 (Zhang et al. 2013). Green tea has a strong antioxidant property by acting through multiple mechanisms, including antilipid peroxidation, free-radical scavenging, metal sequestration, and inhibition of several enzymes including XOD (Fraga et al. 2010); the hypouricaemic effect of green tea polyphenols in hyperuricemic mice was demonstrated (Chen et al. 2015). Black tea has shown diverse health benefits such as protection against cardiovascular diseases, neuro-degeneration, cancers and pathogenic bacteria (Higdon and Frei 2003; Del Rio et al. 2013). The principal catechins in green tea are catechin (C), epicatechin (EC), epigallocatechin (EGC), epicatechin gallate (ECG) and epigallocatechin gallate (EGCG). Black tea is rich in various antioxidant polyphenols, such as catechins, theaflavins, thearubigins and other nutrients including amino acids and bioactive carbohydrates (Higdon and Frei 2003; Li et al. 2013).
Figure 1.
Main manufacture process of green tea and black tea.
In this work, we compared the serum UA lowering effects of green and black tea from aqueous extracts in hyperuricemic mice.
Materials and methods
Reagents and drugs
All chemicals and reagents were of analytical reagent grade. Assay kits of UA, blood urea nitrogen (BUN), serum creatinine (Cr), XOD and adenosine deaminase (ADA) were purchased from Nanjing Jiancheng Biotech (Nanjing, China). Allopurinol was obtained from Shanghai Sine Wanxiang Pharmaceutical Co., Ltd (Shanghai, China). Potassium oxonate (PO) was purchased from Nanjing Duly Biotech Co., Ltd (Nanjing, China). Yeast extract was the products of Beijing Aobox Biotechnology Co., Ltd Beijing(, China). Green tea was purchased from market in Hefei province. Black tea was purchased from Qimen Xiang Tea Industry Co., Ltd (Qimen, China).
Preparation of green tea extracts (GTEs) and black tea extracts (BTEs)
Green tea and black tea leaves (50 g, respectively) were brewed twice, each time with 500 mL boiling distilled water for 30 min. The two filtrates were collected, respectively, evaporated in vacuum rotary evaporator, and then the two samples were stored at −20 °C after freeze-drying.
Analysis of GTEs and BTEs by high-performance liquid chromatographic (HPLC)
High-performance liquid chromatography (HPLC) analysis was performed on Wufeng LC-100 series HPLC system, using a Luna 5 μ C18 (2) 100 A column (250 × 4.60 mm, 5μ) (Phenomenex, Torrance, CA). Column temperature was kept at 30 °C. Analysis of GTEs by HPLC was as follows: the gradient elution was composed of mobile phase A (water containing 0.15% acetic acid) and mobile phase B (acetonitrile). The gradient of mobile phase A was: 0–5 min, kept at 92%; 5–35 min, from 92% to 75%; 35–36 min, from 75% to 0%; 36–41 min, kept at 0% for 5 min; 41–42 min, from 0% to 92% and then kept at 92% for 8 min. Analysis of BTEs by HPLC was as follows: the gradient elution was composed of mobile phase A (water containing 0.17% acetic acid) and mobile phase B (acetonitrile). The gradient of mobile phase A was: 0–4 min, 92%; 4–32 min, from 92% to 70%; 32–45 min, from 70% to 41.8%; 45–50 min, from 41.8% to 0%; 50–51 min, from 0% to 92% and then kept at 92% for 9 min. The flow rate was 1 mL/min and the detection was performed at 278 nm. Weighing 2.5 mg tea extracts (GTE and BTE) were dissolved in 1 mL 70% aqueous methanol. Each sample (20 μL) was injected into the column after filtration through a 0.22 μm filter disk.
Animals
Male Kunming mice (25 ± 2.0 g) used in the study were purchased from Shanghai SLAC Laboratory Animal Co. Ltd. (Shanghai, China), six mice in each group were housed in a plastic cage. All mice were housed under the following conditions: temperature 22 ± 2 °C, humidity 50 ± 10% and constant 12 h light/dark cycle and were acclimatized for one week with free access to water and food before the experiments. The protocol was approved by the Laboratory Animal Center of SLAC, Shanghai, China (Permit Number: 2012-0002). All surgery was performed under chloral hydrate anaesthesia, and all efforts were made to minimize suffering. All animals were humanly treated in accordance with the Guide for the Care and Use of Laboratory Animals (Ministry of Science and Technology of the People’s Republic of China) and the animal protocols were reviewed and approved by the ethics committee of Anhui Agricultural University.
Mouse model of hyperuricemia and drug administration
The mice were randomly divided into nine groups and the experimental design was performed as follows: (1) normal control group mice were intragastrically administrated with 0.5 mL of saline for consecutive seven days; (2) model group mice were intragastrically treated with 0.5 mL of saline for continuous six days and treated with p.o. (250 mg/kg) and yeast extract (7.5 g/kg) dissolved in distilled-water on the 7th day (Hassan and Samah 2015); (3) AP group mice were intragastrically treated with 5 mg/kg AP everyday but on the 7th day AP was treated 1 h after modelling; (4)–(9) mice were intragastrically treated with 0.5, 1 and 2 g/kg GTEs and BTEs respectively for six days. At the 7th day, tea extracts were administered 1 h after modelling; food, but not water, was withdrawn from the animals 12 h prior to drug administration. All drugs given were based on body weight measured immediately prior to each dose. No adverse events were observed in the animals during the seven-day experimental period.
Blood and liver sample collection
Mice were sacrificed under anaesthesia (intraperitoneal, ip) 1 h after the last drugs administration and peripheral blood from the ophthalmic vein was collected into an Eppendorf tube. The blood was allowed to clot for approximately 1 h at room temperature and centrifuged at 3000 rpm for 10 min to obtain serum. The serum samples were stored at −20 °C till assayed. UA was detected using phosphotungstic acid method (Carroll et al. 1971). BUN and Cr were detected according to kits. Livers were excised and rinsed in ice-cold saline; pieces of hepatic tissue were stored at −80 °C. Before determination, the tissue was homogenized in 9 volumes of saline. The homogenate was then centrifuged at 3000×g for 10 min. The lipid layer was carefully removed and the final supernatant was used for XOD and ADA activities assay.
Statistical analysis
All results were presented as the mean ± standard error (S.E.M.). All data were analysed using Graph Pad Prism 5 (Graph Pad Software, San Diego, CA) and one-way analysis of variance (ANOVA). Values of p < 0.05 were considered statistically significant.
Results
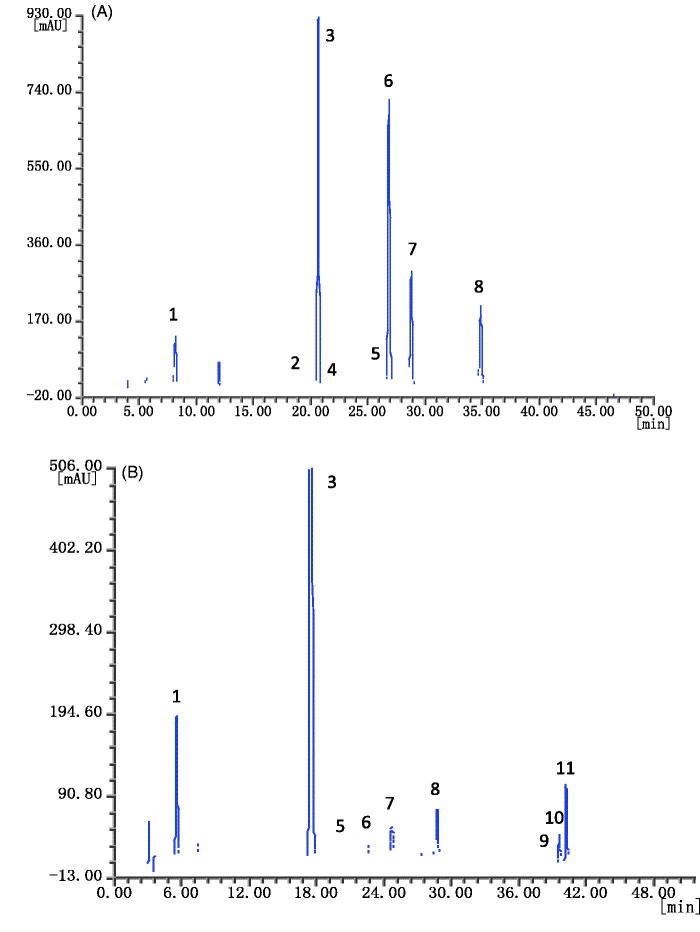
HPLC-fingerprint of GTE and BTE
HPLC of GTE and BTE is shown in Figure 2 (A and B, respectively).
Figure 2.
HPLC of GTE (A) and BTE (B). Detection was performed at 278 nm. Peaks identification: 1: gallic acid (GA); 2: epigallocatechin (EGC); 3: caffeine; 4: catechin (C); 5: epicatechin (EC); 6: epigallocatechin gallate (EGCG); 7: gallocatechin gallate (GCG); 8: epicatechin gallate (ECG); 9: theaflavin (TF); 10: theaflavin-3-gallate (TF-3-G); 11: theaflavin-3′-gallate (TF-3′-G).
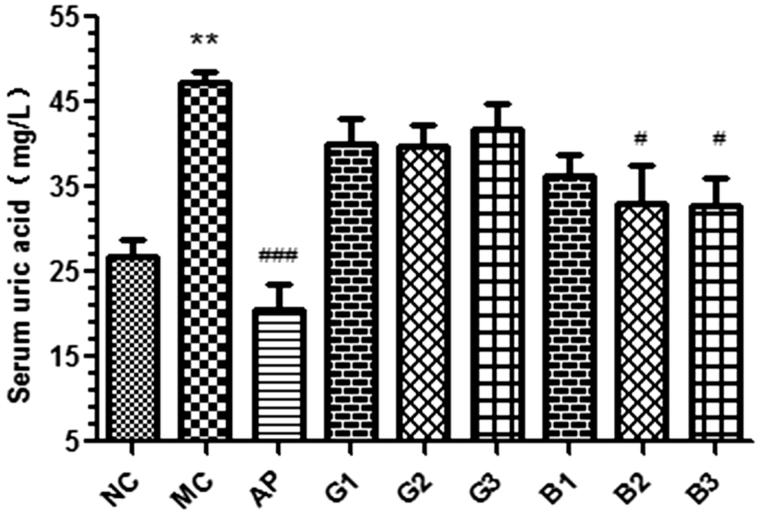
Effects of GTEs and BTEs on serum UA levels in hyperuricemic mice
As shown in Figure 3, the level of serum UA in model group was significantly increased to 47 mg/L (p < 0.01) after PO and yeast extract administration, which indicated that hyperuricemic model was established successfully in mice. Compared with model group, the serum UA levels were decreased by GTEs but not significant; BTEs at the dose of 1 and 2 g/kg decreased to 33 and 32 mg/mL (all p < 0.05), though inferior to AP (20 mg/L, p < 0.001). It means that the GTEs and BTEs all have anti-hyperuricemic effects, and the BTEs are more effective.
Figure 3.
Effects of GTEs and BTEs on serum UA in hyperuricemic mice. N = 6 per group. NC: normal control; MC: model group; AP: allopurinol (5 mg/kg); G1, G2 and G3 mean 0.5, 1 and 2 g/kg GTEs; B1, B2 and B3 mean 0.5, 1 and 2 g/kg BTEs; **p < 0.01, compared with NC group; #p < 0.05, ###p < 0.001, compared with MC group.
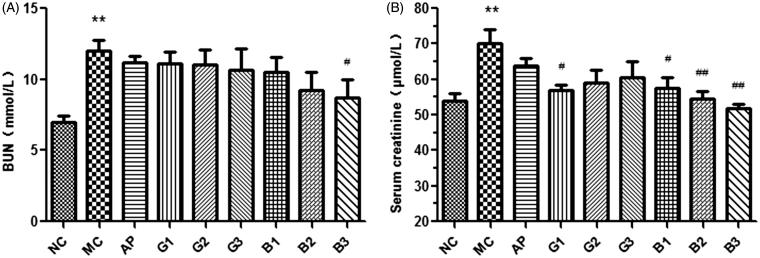
Effects of GTEs and BTEs on serum BUN and Cr levels in hyperuricemic mice
As shown in Figure 4(A), the model group had a higher BUN level (11.875 mmol/L, p < 0.01) compared with normal control group (6.875 mmol/L). After treatment with AP, the BUN level was decreased. Compared with model group, the serum BUN levels were decreased slightly by GTEs, but there were no difference. BTEs significantly reduced BUN levels in a dose-dependent manner and the BUN levels was decreased significantly at the dose of 2 g/kg (8.435 mmol/L, p < 0.05). Compared with AP group, the obvious reduction also signified less renal injury by tea-given BTEs groups.
Figure 4.
Effects of GTEs (A) and BTEs (B) on serum BUN and Cr in hyperuricemic mice. N = 6 per group. NC: normal control; MC: model group; AP: allopurinol (5 mg/kg); G1, G2 and G3 mean 0.5, 1 and 2 g/kg GTEs; B1, B2 and B3 mean 0.5, 1 and 2 g/kg BTEs; **p < 0.01, compared with the control group; #p < 0.05, ##p < 0.01, compared with the model group.
As shown in Figure 4(B), the serum Cr values in model group showed significant difference (70 μmol/L, p < 0.01) compared with control group (54 μmol/L). Tea-treated groups showed lower serum Cr levels and the serum Cr levels of BTEs’ groups decreased significantly (57.5, 54.5 and 50 μmol/L; p < 0.05, p < 0.01 and p < 0.01, respectively); compared with BTEs’ groups, GTEs showed higher Cr levels, but lower than that of AP (63 μmol/L). It was indicated that AP induced serious renal injury.
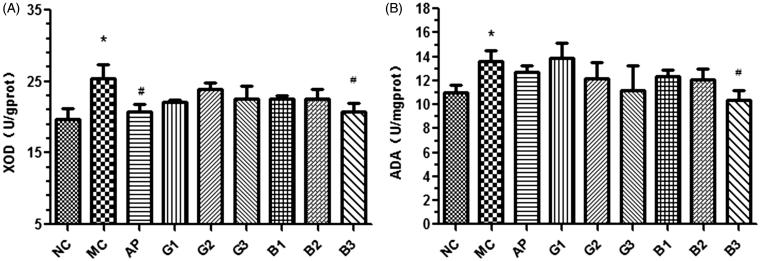
Effects of GTEs and BTEs on hepatic XOD and ADA activities in hyperuricemic mice
As shown in Figure 5(A), after treatment with PO and yeast extract, there was a significant increase of the hepatic XOD values compared to the normal control group (25 U/gprot, p < 0.05); AP as a positive control at the dose of 5 mg/kg suppressed significantly (p < 0.05) hepatic XOD activity in hyperuricemic mice. Three different doses of GTEs performed slightly suppression on XOD activities. The enzyme activity in livers of mice from high dose group (2 g/kg) of BTEs was significantly different compared to the model group (25 U/gprot, p < 0.05), while low dose groups (0.5 g/kg) and middle dose groups (1 g/kg) presented slight effect on XOD.
Figure 5.
Effects of GTEs (A) and BTEs (B) on hepatic XOD and ADA in hyperuricemic mice. N = 6 per group. NC: normal control; MC: model group; AP: allopurinol (5 mg/kg); G1, G2 and G3 mean 0.5, 1 and 2 g/kg GTEs; B1, B2 and B3 mean 0.5, 1 and 2 g/kg BTEs; *p < 0.05, compared with the control group; #p < 0.05, compared with the model group.
As shown in Figure 5(B), the levels of ADA of model group in liver tissue increased significantly (13.5 U/mgprot, p < 0.05) compared to the normal control group; in the group treated with AP, the hepatic ADA activity was slightly decreased, but not significantly; compared with model group, there were dose-dependent manners in GTEs and BTEs; The group which was treated with highest dose of BTE (2 g/kg) presented significantly suppressing effect on ADA (10 U/mgprot, p < 0.05), and both low dose groups (0.5 g/kg) and middle dose groups (1 g/kg) of GTEs and BTEs showed slight effects on ADA compared to model group.
Discussion
The result of our study demonstrated that the hypouricaemic effects of GTEs and BTEs in hyperuricemic mice induced by PO and yeast extract. They showed significant hypouricaemic activities and displayed different dose-dependence. Comparing the hypouricaemic effects of two kinds of tea extracts, BTEs showed better effects on lowering serum UA levels than GTEs, especially presenting a significant dose-dependent manner.
Renal damage can be associated with increases of serum BUN and Cr, indicating urea and Cr clearance reduction (Hoffmann et al. 2010). The BUN levels of model groups were significantly higher than that of normal control group, which means modelling drugs may cause renal damage. Compared with model group and AP group, the BUN levels were all decreased at the dose of 0.5, 1 and 2 g/kg GTEs and BTEs groups, which means good kidney protection; at the dose of 2 g/kg BTEs group, it was suppressed significantly. As an important factor for renal function evaluation, Cr level can abnormally rise, resulting from Cr excretion disorder due to kidney damage. Treatment of the mice with 0.5 g/kg GTEs and BTEs in three different doses (0.5, 1 and 2 g/kg) for seven consecutive days, the serum Cr levels of both showed significant decrease, which indicated that GTEs and BTEs could reverse the mice kidney damage caused by hyperuricemia in a way.
In purine metabolism, xanthine and hypoxanthine are oxidized into UA by XOD, which is highly expressed in liver (Lee 1973; Borges et al. 2002). To further explore the involved mechanisms, we evaluated the effects of GTEs and BTEs on the hepatic XOD activities. As shown in Figure 5(A), all of the tea extracts suppressed effect on XOD, and at the dose of 2 g/kg in BTE groups showed significantly inhibiting activity compared with model group. It is indicated that the hypouricaemic effect of black tea is based on suppressing XOD activity.
ADA is one of the enzymes playing an important role in purine metabolism. The study indicated that the increase of the ADA activity can increase the generation of xanthine and hypoxanthine in the body and cause cytotoxicity (Bellé et al. 2011). Moreover, its decreased activity could improve the anti-inflammatory effect of the body (Kaminsky and Kosenko 2010). As shown in Figure 5(B), compared to model group, at the dose of 1 and 2 g/kg GTEs’ groups and three different dose groups of BTEs all can restrain the activity of hepatic ADA to some certain extent in hyperuricemic mice, which suggested that the two kinds of tea extracts in certain dose can not only reduce the body generation of xanthine and hypoxanthine through inhibiting the activity of ADA, thereby reducing generated UA in the body, but also help to improve the body's anti-inflammatory ability.
In recent years, hyperuricemia is in a focus of attention because of its rapid growth of morbidity and trend in young people all around the world. AP as a positive drug has been estimated that approximately 2% of patients treated with AP develop adverse reactions (Vazquez-Mellado et al. 2001). Since tea is a popular beverage around the world, it is safe and has little side effects and low toxicity unlike AP, benzbromarone (Chaichian et al. 2014), etc. Gout is a kind of disease resulting from disordering metabolism of purine biosynthesis, which featured as increase of UA biosynthesis and reduction of excretion. We found that GTE and BTE could decrease UA levels. It can be speculated that these reduction are related with other compositions in green tea and black tea. The active ingredient with hypouricaemic effect of GTE is tea polyphenol (Chen et al. 2015) and active constituents of BTE may be catechins and theaflavins. Future studies are needed to evaluate the specific active-constituents of hypouricaemic effects in tea extracts and the expression of related urate transporter genes and proteins.
Conclusions
The present study has demonstrated that both GTEs and BTEs could significantly reduce serum UA levels in hyperuricemic mice induced by PO joint with yeast extract, and the hypouricaemic activity of the BTEs’ group is better than that of the GTEs. At the same time, compared with AP group, both of the GTEs and BTEs groups showed lower serum BUN and Cr levels, which signified tea extracts had renal protective effect on hyperuricemic mice; In addition to low dose of GTEs, other tea-given groups displayed inhibiting effects on hepatic XOD and ADA in hyperuricemic mice. This finding indicated that GTEs and BTEs may possess the potent hypouricaemic effect on hyperuricemic mice through suppressing ADA and XOD activities. Due to the different machining process, these two kinds of tea showed different degrees of hypouricaemic effects.
Funding Statement
The study was supported by grants from the Project of Education Department of Anhui [KJ2017A128], the earmarked fund for China Agriculture Research System (CARS-19), Anhui Major Demonstration Project for Leading Talent Team on Tea Chemistry and Health, and Anhui Provincial Science and Technology Major Project [15czz03116].
Disclosure statement
The authors declare no conflict of interest.
References
- Bellé LP, Bitencourt PER, Abdalla FH, Guerra RB, Funchal C, Moretto MB.. 2011. An in vitro comparison of a new vinyl chalcogenide and sodium selenate on adenosine deaminase activity of human leukocytes. Chem Biol Interact. 189:141–145. [DOI] [PubMed] [Google Scholar]
- Borges F, Fernandes E, Roleira F.. 2002. Progress towards the discovery of xanthine oxidase inhibitors. CMC. 9:195–217. [DOI] [PubMed] [Google Scholar]
- Carroll JJ, Coburn H, Douglass R, Babson AL.. 1971. A simplified alkaline phosphotungstate assay for uric acid in serum. Clin Chem. 17:158–160. [PubMed] [Google Scholar]
- Chaichian Y, Chohan S, Becker MA.. 2014. Long-term management of gout: nonpharmacologic and pharmacologic therapies. Rheum Dis Clin N Am. 40:357–374. [DOI] [PubMed] [Google Scholar]
- Chen G, Tan ML, Li KK, Leung PC, Ko CH.. 2015. Green tea polyphenols decreases uric acid level through xanthine oxidase and renal urate transporters in hyperuricemic mice. J Ethnopharmacol. 175:14–20. [DOI] [PubMed] [Google Scholar]
- Chen LY, Yin HF, Lan Z, Ma SW, Zhang CF, Yang ZL, Li P, Lin BQ.. 2011. Anti-hyperuricemic and nephroprotective effects of Smilax china L. J Ethnopharmacol. 135:399–405. [DOI] [PubMed] [Google Scholar]
- Dawson J, Quinn T, Walters M.. 2007. Uric acid reduction: a new paradigm in the management of cardiovascular risk? Curr Med Chem. 14:1879–1886. [DOI] [PubMed] [Google Scholar]
- Del Rio D, Rodriguez-Mateos A, Spencer JPE, Tognolini M, Borges G, Crozier A.. 2013. Dietary (poly) phenolics in human health: structures, bioavailability, and evidence of protective effects against chronic diseases. Antioxid Redox Signal. 18:1818–1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraga CG, Galleano M, Verstraeten SV, Oteiza PI.. 2010. Basic biochemical mechanisms behind the health benefits of polyphenols. Mol Aspects Med. 31:435–445. [DOI] [PubMed] [Google Scholar]
- Fritsch PO, Sidoroff A.. 2000. Drug-induced Stevens–Johnson syndrome/toxic epidermal necrolysis. Am J Clin Dermatol. 1:349–360. [DOI] [PubMed] [Google Scholar]
- Hammer B, Link A, Wagner A, Bohm M.. 2001. Hypersensitivity syndrome during therapy with allopurinol in asymptomatic hyperuricemia with a fatal outcome. Dtsch Med Wochenschr. 126:1331–1334. [DOI] [PubMed] [Google Scholar]
- Hassan FA, Samah AA.. 2015. Effects of crude clavonoids from ginger (Zingiber officinale), on serum uric acid levels, biomarkers of oxidative stress and xanthine oxidase activity in oxonate-induced hyperuricemic rats. Int J Adv Res. 3:1033–1039. [Google Scholar]
- Higdon JV, Frei B.. 2003. Tea catechins and polyphenols: health effects, metabolism, and antioxidant functions. Crit Rev Food Sci Nutr. 43:89–143. [DOI] [PubMed] [Google Scholar]
- Hoffmann D, Fuchs TC, Henzler T, Matheis KA, Herget T, Dekant W, Hewitt P, Mally A.. 2010. Evaluation of a urinary kidney biomarker panel in rat models of acute and subchronic nephrotoxicity. Toxicology. 277:49–58. [DOI] [PubMed] [Google Scholar]
- Horiuchi H, Ota M, Nishimura S, Kaneko H, Kasahara Y, Ohta T, Komoriya K.. 2000. Allopurinol induces renal toxicity by impairing pyrimidine metabolism in mice. Life Sci. 66:2051–2070. [DOI] [PubMed] [Google Scholar]
- Iseki K, Ikemiya Y, Inoue T, Iseki C, Kinjo K, Takishita S.. 2004. Significance of hyperuricemia as a risk factor for developing ESRD in a screened cohort. Am J Kidney Dis. 44:642–650. [PubMed] [Google Scholar]
- Iseki K, Oshiro S, Tozawa M, Iseki C, Ikemiya Y, Takishita S.. 2001. Significance of hyperuricemia on the early detection of renal failure in a cohort of screened subjects. Hypertens Res. 24:691–697. [DOI] [PubMed] [Google Scholar]
- Ishizaka N, Ishizaka Y, Toda E, Nagai R, Yamakado M.. 2005. Association between serum uric acid, metabolic syndrome, and carotid atherosclerosis in Japanese individuals. Arterioscler Thromb Vasc Biol. 25:1038–1044. [DOI] [PubMed] [Google Scholar]
- Jiang HY, Engelhardt UH, Thrane C, Maiwald B, Stark J.. 2015. Determination of flavonol glycosides in green tea, oolong tea and black tea by UHPLC compared to HPLC. Food Chem. 183:30–35. [DOI] [PubMed] [Google Scholar]
- Kaminsky Y, Kosenko E.. 2010. AMP deaminase and adenosine deaminase activities in liver and brain regions in acute ammonia intoxication and subacute toxic Hepatitis. Brain Res. 1311:175–181. [DOI] [PubMed] [Google Scholar]
- Lee PC. 1973. Developmental changes of adenosine deaminase, xanthine oxidase, and uricase in mouse tissues. Dev Biol. 31:227–233. [DOI] [PubMed] [Google Scholar]
- Li S, Lo CY, Pan MH, Lai CS, Ho CT.. 2013. Black tea: chemical analysis and stability. Food Funct. 4:10–18. [DOI] [PubMed] [Google Scholar]
- Lin KC, Lin HY, Chou P.. 2000. The interaction between uric acid level and other risk factors on the development of gout among asymptomatic hyperuricemic men in a prospective study. J Rheumatol. 27:1501–1505. [PubMed] [Google Scholar]
- Merriman TR, Dalbeth N.. 2011. The genetic basis of hyperuricaemia and gout. Joint Bone Spine. 78:35–40. [DOI] [PubMed] [Google Scholar]
- Niu YF, Lu W, Gao LH, Lin H, Liu X, Li L.. 2012. Reducing effect of mangiferin on serum uric acid levels in mice. Pharm Biol. 50:1177–1182. [DOI] [PubMed] [Google Scholar]
- Pereira S, Almeida J, Silva AO, Quintas M, Candeias O, Freitas F.. 1998. Fatal liver necrosis due to allopurinol. Acta Med Port. 11:1141–1144. [PubMed] [Google Scholar]
- Sang SM, Lambertb JD, Ho CT, Yang CS.. 2011. The chemistry and biotransformation of tea constituents. Pharmacol Res. 64:87–99. [DOI] [PubMed] [Google Scholar]
- Stangl V, Lorenz M, Stangl K.. 2006. The role of tea and tea flavonoids in cardiovascular health. Mol Nutr Food Res. 50:218–228. [DOI] [PubMed] [Google Scholar]
- Vazquez-Mellado J, Morales EM, Pacheco-Tena C, Burgos-Vargas R.. 2001. Relation between adverse events associated with allopurinol and renal function in patients with gout. Ann Rheum Dis. 60:981–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widlansky ME, Duffy SJ, Hamburg NM, Gokce N, Warden BA, Wiseman S, Keaney JF Jr, Balz Frei B, Vita JA.. 2005. Effects of black tea consumption on plasma catechins and markers of oxidative stress and inflammation in patients with coronary artery disease. Free Radic Biol Med. 38:499–506. [DOI] [PubMed] [Google Scholar]
- Wu XH, Wang CZ, Wang SQ, Mi C, He Y, Zhang J, Zhang YW, Anderson S, Yuan CS.. 2015. Anti-hyperuricemia effects of allopurinol are improved by Smilax riparia, a traditional Chinese herbal medicine. J Ethnopharmacol. 162:362–368. [DOI] [PubMed] [Google Scholar]
- Yang CS, Lambert JD, Hou Z, Ju J, Lu G, Hao X.. 2006. Molecular targets for the cancer preventive activity of tea polyphenols. Mol Carcinog. 45:431–435. [DOI] [PubMed] [Google Scholar]
- Zhang L, Zhang ZZ, Zhou YB, Ling TJ, Wan XC.. 2013. Chinese dark teas: postfermentation, chemistry and biological activities. Food Res Int. 53:600–607. [Google Scholar]
- Zhao X, Zhu JX, Mo SF, Pan Y, Kong LD.. 2006. Effects of Cassia oil on serum and hepatic uric acid levels in oxonate-induced mice and xanthine dehydrogenase and xanthine oxidase activities in mouse liver. J Ethnopharmacol. 103:357–365. [DOI] [PubMed] [Google Scholar]