Abstract
Over the past two decades, there has been increasing attention to the importance of early intervention for psychosis. This paper describes the development of the Center for Early Detection, Assessment and Response to Risk (CEDAR), which focuses on early identification and treatment of youth at clinical high risk (CHR) for psychosis. There are relatively few models in the United States for such programs, and we present our developmental story, focusing mainly on the CEDAR Clinic, as a case study of how such a program can develop. We describe the rationale, infrastructure, and services provided at the CEDAR Clinic, and present some descriptive data from the CEDAR Clinic through 2016. A case example is provided to illustrate treatment at CEDAR. We hope that this form of cultural history of program development is informative for clinicians and policy makers as one model of how to build an early intervention service. We believe this article is timely as there is growing momentum in the United States for developing programs for intervening as early as possible for youth at CHR for psychosis.
Keywords: Clinical high risk, psychosis, clinic, early intervention, schizophrenia, ultra-high risk
Origins and Philosophy
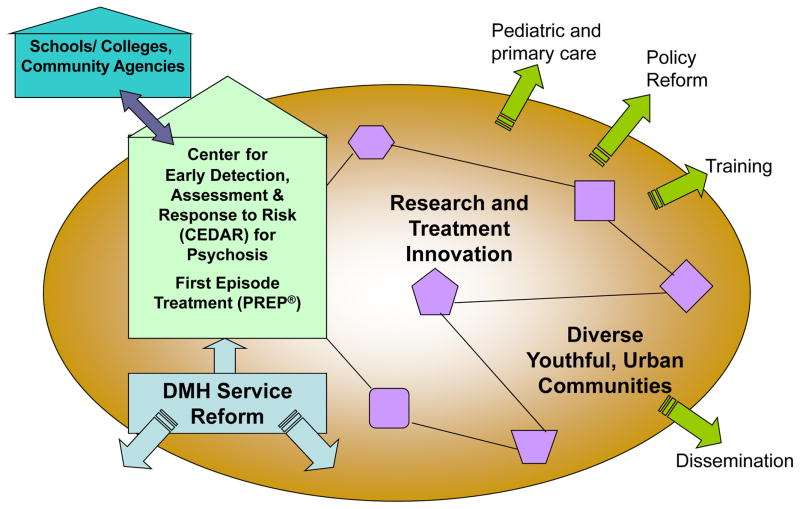
Guided by innovative thinking and clinical research emphasizing early intervention (EI), we sought to initiate a developmentally sensitive and low stigma treatment and research program for young people at clinical high risk (CHR) for psychosis in Boston in the mid-2000s. Visionary work by Patrick McGorry and Alison Yung in Australia provided a framework for the development of a specialized service.1 We had previously established a first episode psychosis (FEP) program in 2003 (Prevention and Recovery in Early Psychosis, PREP®2), thus providing a feasible model for an EI center to minimize the disability often associated with the emergence of psychosis.3 We envisioned a center with capacity for specialized treatment and clinical research, training, community outreach and education, and integrated care across risk syndromes and early psychosis (see Figure 1). Building on three initial research studies enrolling CHR youth, the “Center for Early Detection, Assessment and Response to Risk (CEDAR)” and corresponding clinic and website (www.cedarclinic.org) were launched in 2009. The clinic aimed to provide comprehensive, developmentally sensitive EI services for youth ages 14–30 at CHR and their families. In this paper we describe the rationale, development, infrastructure, services, and clients of the CEDAR Clinic through 2016. We illustrate our services with a case example.
Figure 1.
Early Psychosis Programs at MMHC
Model representing CEDAR as part of an early psychosis center with capacity for research, training, community education, outreach, and integrated care across putative prodrome and early psychosis The inside shapes represent a connected series of research studies linked to treatment. PREP® is Prevention and Recovery in Early Psychosis.
Rationale for Early Intervention
Over the past few decades, research and treatment efforts in serious mental illness have shifted towards earlier detection and treatment,4–8 motivated by the idea that intervention prior to or immediately after FEP might be expected to have the greatest impact on illness progression and outcomes.9,10 A consensus emerged that the significant developmental, neurocognitive, and social impairments, evident prior to and during FEP,11–14 were not simply a function of illness chronicity, but of abnormal neurodevelopment.15–17 The association of longer duration of untreated psychosis (DUP) with negative outcomes18 has provided particularly compelling support for EI.19,20 Moreover, earlier antipsychotic treatment was associated with better outcome in FEP.21
Accumulating evidence documenting that mental health problems begin long before FEP3,6,22,23 has driven an international effort to detect and intervene during the critical stages before FEP by responding to signs and symptoms of CHR for psychosis.24 CHR refers to a set of syndromes indicative of increased risk for psychotic illness as characterized by structured interview (e.g., Structured Interview for Psychosis Risk Syndromes; SIPS25). The SIPS identifies three CHR syndromes: 1) Attenuated Positive Symptom Syndrome (APSS): new or worsening attenuated or low-grade positive psychotic symptoms causing distress and/or impairment, 2) Genetic Risk and Deterioration Syndrome (GRDS): presumed genetic risk for psychosis (having a first degree relative with psychosis or a diagnosis of schizotypal personality disorder) coupled with a recent, serious decline in functioning, and 3) Brief Intermittent Psychotic Symptoms Syndrome (BIPSS): recent onset of brief and intermittent psychotic symptoms that do not meet criteria for a psychotic disorder. Studies of help-seeking young people meeting CHR criteria have reported average rates of transition to diagnosable psychotic disorder of around 30% within 2.5 years.26 Decline in social and role functioning is common27 and an important predictor of schizophrenia onset.28 Risk calculation is becoming more refined and individualized in the context of recent large prospective studies.24,29 However, many CHR programs include individuals with more broadly defined risk, characterized by sub-threshold negative symptoms or stable, attenuated positive symptoms.30–33
EI aims to prevent psychotic disorder onset, decrease hospitalization rates, and promote rapid recovery and better prognosis, particularly in social and role functioning.19,34–38 EI also addresses a myriad of clinical issues associated with psychosis risk (e.g., depression, anxiety, trauma symptoms, stigma, substance misuse, suicide risk, and neurocognitive deficits24,39).
Evidence for EI with Youth at CHR
Interventions with youth at CHR, including medication, individual, group, and family therapies, and integrated care,24,39 have shown promise in reducing positive symptoms and transition to psychosis.40,41 Cognitive behavioral therapy (CBT) has been most commonly studied, with overall positive findings.41,42 Family-focused treatment, aimed at educating families about symptoms and stress-vulnerability interactions and improving communication and problem-solving skills, was associated with reduced positive symptoms and improved family interactions relative to brief psychoeducation alone.43,44 Integrated care programs that provide some combination of individual, group, and family therapies, social skills training and cognitive remediation have shown reductions in short-term conversions and negative symptoms.45,46 Cognitive remediation is being tested in CHR samples to enhance cognition and functioning.47,48
Several studies have suggested that low-dose antipsychotic medications reduce symptoms and short-term risk of conversion.35,49,50 However, given the potential for harmful side effects, clinical guidelines discourage their use in individuals at CHR except in severe cases.32,51,52 Interventions involving use of supplements and/or antidepressant medications have shown some promise. Amminger et al.53 initially found that Omega-3 fatty acid supplements decrease conversion risk, although a larger trial did not replicate this finding.54 A post hoc case study of antidepressant treatment showed promise but more controlled studies are needed.55
Promising initial results have prompted healthcare systems in the United Kingdom, Europe, and Australia to make substantial commitments to specialized EI services.56 Following their lead, the United States Congress made a formal commitment to EI in 2014 by directing the Substance Abuse and Mental Health Services Administration (SAMHSA) to set aside 5% of state grant awards for EI in FEP.
CEDAR Clinic: History and Development
A Public-Academic Partnership at Massachusetts Mental Health Center (MMHC): Funding and Site Selection
In the absence of a national health care system, and consistent with most EI programs in the United States, CEDAR developed within an academic research setting. CEDAR emerged as a successful collaboration among the MMHC, Harvard Medical School (HMS) Department of Psychiatry at Beth Israel Deaconess Medical Center (BIDMC), and Massachusetts Department of Mental Health (DMH) under the auspices of the DMH Center of Excellence in Clinical Neuroscience and Psychopharmacological Research (the “Commonwealth Research Center”/CRC). Founded in 1912 by an agreement between the DMH and HMS, MMHC traditionally positioned itself at the forefront of academic research, public psychiatry, and multi-disciplinary training.57,58 It has long promoted community-based care and recovery for people with serious mental illness, thus providing a rich context for the development of CEDAR. Beginning in the mid-1990s, HMS/MMHC researchers increasingly focused on adolescence/young adulthood as a high-risk period (e.g.,59,60) through studies of familial high-risk (FHR).61 In 2001, we joined the International Prodromal Research Network (IPRN) and expanded our focus to include CHR populations. In 2003, our group joined the North American Prodrome Longitudinal Studies (NAPLS) research network organized by NIMH.62 This led to further consultation by experts in CHR assessment and specialty care, and site visits to established CHR programs (see acknowledgements). This process honed our understanding of the key elements of a CHR treatment and research program, our local vision for CEDAR, and prompted pursuit of funding and space.
In 2007, the Sidney R. Baer, Jr. Foundation funded the first of three grants (2007–2017) supporting a Prodrome Treatment and Education Program (PTEP). PTEP sought to identify and treat emerging psychosis by developing a coordinated specialty clinic, an intensive community awareness program, and clinician training. We measured outcomes to inform practice and better respond to the mental health needs of this vulnerable group of young people.
Given the DMH’s longstanding commitment to serving people with serious and persistent mental illness, we advocated for DMH interest in and financial support of EI. CEDAR’s “older sibling,” PREP®, had become a DMH-supported FEP program at MMHC in 2005 after having been seeded by the CRC and there was a strong DMH movement toward enhanced services for transition-aged youth more generally. The Baer Foundation provided funding for personnel, operational, and outreach/website start-up costs; DMH assumed many continuation costs when the original Baer Foundation grant ended in 2011.
Young people are often reluctant to seek and engage mental health services due to stigma, particularly those experiencing the confusing, earliest symptoms of psychosis. Similar to many CHR clinics, a core program philosophy was to cultivate a friendly, normalizing approach.35,63 One approach to “destigmatization” is to establish CHR clinics in a community setting disassociated from hospital-based mental health services. A leading example of this is Australia’s Headspace clinics pioneered by McGorry (https://www.orygen.org.au/).64 In 2007, DMH opened a MMHC “storefront clinic” for youth mental health services. “The SPOT” co-located three programs oriented toward “transition-aged youth” with serious mental health needs: PREP® (serving youth ages 16–30 experiencing recent FEP2), the Young Adult Team (for those ages 18–25 with long-standing youth services and DMH involvement), and the CEDAR Clinic (serving 14–30 year-olds at CHR). When the SPOT ultimately became too crowded with three growing programs, the CEDAR Clinic moved to the new MMHC building in 2011.58 Although the program lost the storefront location, the move facilitated integration with the CRC research and community outreach/education programs.
DMH has provided consistent core funding, including a .25 psychiatrist medical director, a .75 psychologist clinical director, a .50 staff psychologist, a .25 masters’ level clinician, and a .30 bachelor’s level administrative and clinical research assistant. Most staff are employed full time through research grant supplementation. Clinical services are delivered within the MMHC Outpatient Clinic.
The clinic benefits from foundation- and NIMH-funded research awarded to BIDMC faculty. Studies of stigma, cognitive enhancement, biomarkers, and family therapies provide platforms for emerging assessment and/or treatment approaches. The integration of a specialty clinic with research enhances the visibility and appeal of research and provides innovative options for referrers seeking clinical consultation and care. It also provides a rich educational environment for clinical trainees and community providers.
Outreach and Establishing a Referral Base
A significant challenge for CEDAR, as for EI initiatives worldwide, has been accurate identification and referral of appropriate individuals. Our outreach sought to facilitate the four As of EI: 1) Awareness of the early warning signs and symptoms of emerging psychosis: We targeted our education to mental health clinicians, community health clinic staff, clinical support staff in secondary and post-secondary education, pediatricians, community members with regular contact with adolescents/young adults, parents, and youth themselves. 2) Availability of CEDAR as a resource: Potential referral sources needed to know that CEDAR provides specialized expertise and clinical services and is a helpful resource for vulnerable individuals and their families. 3) Activate referrals and address concerns: We needed to challenge myths of pessimism, inevitability, and danger and provide information about the nature of EI and its potential to impact life outcomes, including altering the course of illness. We needed to address concerns that we might over-identify risk for psychosis, undervalue alternative diagnoses, or over-pathologize normal behavior. A referrer needed to trust that the individual would receive high quality, ethical and individualized care. 4) Access: We needed capacity to respond to inquiries and concerns in a timely and sensitive way and to engage individuals when they became help-seeking.
CEDAR has employed a number of outreach strategies. Clinic staff and research faculty have contacted area agencies, schools, and health and mental health practitioners via emails, letters, and phone calls to share information about CEDAR, offer free in-service trainings and consultations, and arrange individual meetings with key stakeholders and innovators in youth mental health. We launched press releases through the DMH and BIDMC and published articles in local professional and news outlets. Video, audio, and website links, podcasts and family-friendly handouts were made available via the website. Undergraduate and graduate trainees spread the word to their programs and peers. Not surprisingly, the most important element in establishing CEDAR’s reputation as a responsive, professional, and ethical service was through the care provided to each referral; the majority of referrals have come through word of mouth from people and professionals who had positive experiences. Given the high density of mental health providers and specialist services in the Boston area, it took years to break through to relevant providers and settings.
Two key elements of these efforts warrant special mention. The first is the value of having a person share his/her “lived experience” to break down stereotypes and promote hope. Several young adults in recovery shared their personal stories at community presentations. Their articulate, mature, and poignant descriptions of their experiences of psychosis and recovery had a powerful impact on audiences, prompting them to consider the many young people whose psychoses were yet unrecognized. One young woman’s story illustrated how emerging psychosis is often misdiagnosed or dismissed as other disorders (e.g., substance, conduct), and highlighted the need to consider psychosis early in all intakes.
Second, community partners were essential in growing CEDAR’s service model. We formed a “Prevention Collaborative,” comprising representatives from Boston public schools, the National Alliance on Mental Illness (NAMI), DMH, Boston Public Health Commission, Boston Children’s Hospital, adolescent medicine, pediatric and community-based health centers, local colleges, emergency services, multicultural mental health, and other groups. These stakeholders in psychosis prevention provided critical information about and connections to community partners and identified unmet needs and opportunities for outreach, screening, and publicity.
CEDAR Clinic: Services
This section describes CEDAR Clinic services and treatment approaches, and concludes with a case illustration (disguised and based on a composite of CEDAR clients).
General Culture and Approach
The culture of MMHC heavily influenced CEDAR. MMHC has a longstanding mission to conduct innovative research and develop treatments while serving the state’s most disenfranchised citizens struggling with serious mental illness and victimization, homelessness, poverty, substance abuse, legal difficulties, isolation, and/or loss of family support. MMHC clinicians provide psychotherapy and “do what it takes” to promote recovery and life goals (i.e., helping apply for housing). Clinicians work in multidisciplinary teams and meet weekly to discuss client needs and care. CEDAR’s approach was influenced by PREP®. While PREP® serves individuals (and their families) with established psychotic disorders, both clinics focus on navigating developmental challenges. Normative struggles of adolescence/young adulthood (e.g., identity formation, family relationships, emotion regulation, life goals) intersect with and reciprocally shape emerging mental health problems and pathways to treatment. Primary treatment targets for both programs’ participants may include co-occurring issues related to trauma, anxiety, mood, substance use, and/or risk to self or others.
CEDAR services emphasize a person-centered prevention and recovery orientation, a developmental perspective, inclusion of family, systems, cultural, and environmental factors, integrative care (e.g., behavioral health habits related to sleep, exercise, and nutrition and medication adherence), consideration of diagnostic uncertainty, complexity and comorbidity, and use of hopeful and non-stigmatizing language. When discussing CHR and psychosis, we emphasize an individualized approach that considers the young person’s and family’s previous exposure to the term “psychosis” and cultural beliefs. We attempt to strike a balance between motivating clients and families to take steps to minimize risk and increase protective factors, without over-stating risk or creating undue anxiety or stigma. CEDAR clinicians emphasize that most individuals who are at risk for psychosis will not develop a psychotic disorder, and that there are steps one can take to minimize risk of symptoms worsening (see http://www.cedarclinic.org/index.php/understanding-early-psychosis/what-does-qat-riskq-mean for a commonly provided description about CHR). Feedback is provided about CHR symptoms and any clinical issues relevant to help-seeking and treatment engagement. CEDAR clinicians aim to identify and challenge social and self-stigma and myths about mental illness and psychosis, and to normalize symptom experiences whenever appropriate. We note that all symptoms occur on a continuum, from mild and common difficulties to more serious, unusual, distressing, or impairing symptoms. At their most severe, these symptoms make it hard to distinguish what is real from what is not. Clinicians cultivate an attitude of hope and underscore the potential of treatment to help the youth stay engaged or re-engage in meaningful life activities and to identify and achieve personal goals. Our goal is to build resilience and protective factors while decreasing risk factors for the development of full-blown psychosis with its suffering and its destructive impact on the family and on the young person’s developing sense of self. This aim guides our recommendations as to what is best for each client at each stage of illness, treatment, and recovery.
Training
CEDAR emphasizes training the next generation of mental health practitioners. Trainees include psychiatry residents/fellows, clinical psychology practicum students, postdoctoral fellows, and undergraduate volunteers. CEDAR hosts a weekly “Treatment Seminar” which provides training in psychosocial treatments and approaches relevant to care for young people at CHR and a monthly case conference coordinated with PREP®. Foundation support has allowed CEDAR to host one to two regional, annual professional conferences related to EI in psychosis.
Referrals and Phone Consultations
CEDAR receives referrals from a range of sources. Clinicians conduct an initial phone consultation/screening to assess whether the referred individual is likely to be experiencing CHR and would benefit from a CEDAR clinical evaluation and/or research study. Initial phone contacts range from 15 minutes to several hours, and include sensitive inquiry into the young person’s difficulties. Confidential phone screenings usually involve talking with the referring clinician, family, and/or the young person to gather sufficient information, answer questions, and facilitate connection with appropriate programming. Phone screenings may involve consultation to the referring clinician regarding how to talk with the young person and family about concerns related to psychosis and to encourage them to contact CEDAR. Referrals for individuals with already established psychosis or symptoms not related to CHR/psychosis are provided with suggestions for more appropriate programming. Individuals who sound likely to be experiencing CHR symptoms are offered the choice of a CEDAR research or clinic evaluation. Many clients and families elect to participate first in a research assessment and then, if interested and recommended, seek psychiatric consultation and/or treatment through the clinic. Others choose a clinic evaluation to start and some subsequently choose to participate in a research study.
Clinical Assessment
The structure of clinic consultations and intakes varies according to the presenting issues and needs of the client and family, but involve 1–2 meetings of 2–3 hours duration with a team of clinicians typically including the medical director, a master’s or doctoral level staff clinician, a psychiatry resident, and a psychology trainee. Families participate unless the client is an adult who chooses not to include his/her family. The team begins the evaluation with the young person and family together to introduce them to the team. Then, some clinicians on the assessment team interview the client and others gather a thorough developmental history from the family. For family members who are not fluent in English, interpreter services are provided by DMH.
Whenever possible, and with consent, the evaluation also involves gathering information from the client’s family, school, other providers, and previous evaluations. Youth and family members complete self-report questionnaires to provide standardized assessment of developmental, family, and treatment histories, depression and anxiety symptoms, social relationships and satisfaction, and family attitudes towards the client. Clinicians complete a psychosocial history, with a particular focus on understanding any recent changes in functioning and symptoms. Clients are assessed for the presence of CHR syndromes using the SIPS25. CEDAR clinicians are trained on the SIPS via didactics, observation of trained clinicians, and observed interviews. They participate in ongoing consensus meetings, supervision, and reliability assessments in conjunction with research programs.
Treatment Services
Although many individuals come to CEDAR for consultation, the clinic provides treatment for a portion of these individuals (see Table 1). The clinic provides specific services depending on the client’s presenting needs, preferences, and engagement in community treatment. For clients with established outpatient providers, CEDAR offers time-limited (5–30 sessions) individual and/or family treatment focused on providing CHR-relevant psychoeducation and skill development (e.g., cognitive, acceptance, mindfulness). For others, CEDAR offers comprehensive treatment for CHR and comorbid symptoms/diagnoses, including individual psychotherapy, family therapy/support, psychiatry, cognitive remediation, and school/job support services. There is no predetermined limit on treatment duration. Treatment length ranges from a few sessions to several years (M= 18 months, SD=16.1) and is determined by the needs of the client and family, clinician availability, and the client’s and family’s access to other treatment resources in the community. Ideally, discharge from CEDAR occurs when the client’s condition has stabilized and no longer presents with a need for specialized CHR services.
Table 1.
CEDAR Clinic Treatments
| Individual psychotherapy |
|
| Psychiatry |
|
| Family psychoeducation and therapy |
|
| Cognitive enhancement/remediation |
|
| School/job coaching |
|
CEDAR Clinic Data
CEDAR collects data for all clients and families seen in the clinic for the purposes of diagnostic formulation, treatment planning, and program evaluation. CEDAR conducts follow-up assessments every six months for up to two years and at the end of treatment for those served in the clinic. CEDAR clinicians review the assessment data with the client and family to inform treatment and monitor progress. Information about referrals is also maintained. The Institutional Review Boards at BIDMC and DMH have approved the use of de-identified data for use in publications and presentations.
Clinic Referrals
Investigation of 299 referrals between 1/1/2016–12/1/2016 indicated that initial callers to the clinic were most often clinicians (45.5%). Many initial callers were family members or friends (29.1%) or self-referrals (15.1%), and a few referrals came from a PCP/pediatrician (0.3%). Out of 238 referrals with tracked outcomes, a majority were not eligible for CEDAR due to having current or past fully psychotic symptoms (28.2%), seeking services for concerns that were not related to psychosis or CHR (8.8%), or for other reasons (17.6%) such as being outside the clinic’s age range or living too far away to participate. Twenty-nine percent of individuals initially referred to CEDAR could not be reached for follow-up or refused to come. Approximately 16.4% of individuals who contacted CEDAR participated in a clinical evaluation through the clinic or research.
Clinic Assessment Data
Available data from initial CEDAR intake/consultation visits between 3/1/2009 and 12/1/2016 are presented below. Data include at least partially completed assessments for 184 clients. As of December 1, 2016, the clinic provided treatment to 94 clients; 90 engaged in consultation only.
Demographics
Table 2 shows that clients had a mean age of 19 years, were typically male (69.6%) and White (54.0%), and most often completed some high school (39.2%) or some college (32.7%). They generally came from educated families with 66.4% having a parent with a college or graduate degree.
Table 2.
Demographic characteristics of clients seen for consultation or intake
| Age (N=184) | Mean 19.0 (SD=3.7, Range 13–31) |
|---|---|
| Gender (N=184) | Male: 69.6% Female: 27.7% Transgender or Other: 2.7% |
| Race/Ethnicity (N=174)1 | Caucasian: 54.0% Black/African American: 16.7% Mixed/Multiracial: 9.8% Asian: 9.2% Hispanic/Latino: 5.7% Native Hawaiian/Pacific Islander: 1.1% American Indian/Alaskan Native: 0.6% Other: 2.9% |
| Client Education Completed (N=153) 1 | 8th Grade/Less: 7.2% Part of High School: 39.2% GED: 2.0% Graduated High School: 11.8% Some College: 32.7% Graduated 4-year College: 5.9% Advanced Degree: 1.3% |
| Parent Education Completed (N=77) 1 | Part of High School: 3.9% Graduated High School: 9.1% Some College: 24.7% Graduated 4-year College: 31.2% Advanced Degree: 31.2% |
Data is missing for some participants
Functioning
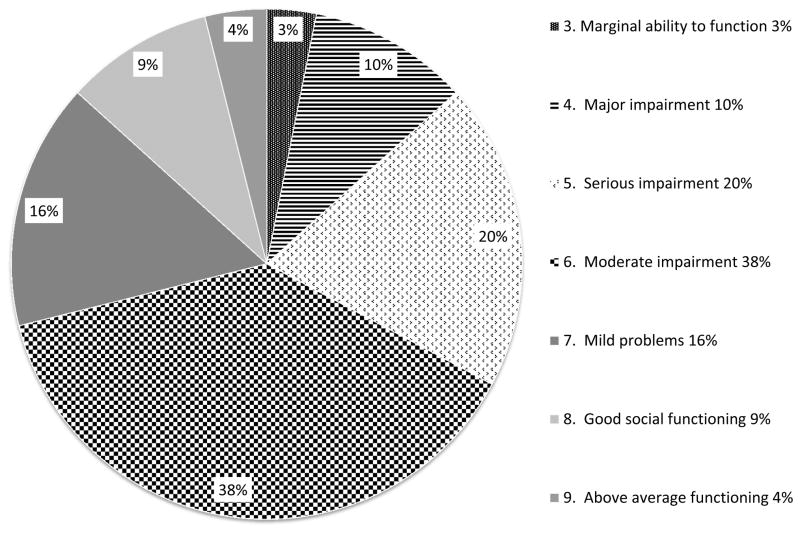
In the month prior to evaluation, the majority of clients were in school (67.8%), with 58.6% taking more than one class. Most were not working; 29.3% worked for pay. The majority of clients exhibited some impairment in social and role functioning (see Figures 2 and 3), with a large proportion exhibiting serious or worse impairment in social (32.8%) and role (45.7%) functioning on the clinician-rated Global Functioning: Social and Role scales (scales with high interrater reliability and construct validity in FEP and CHR populations65,66.
Figure 2. Social Functioning at Initial Assessment (N=128)1.
1Data is missing for some participants
Figure 3. Role Functioning at Initial Assessment (N=127)1.
1Data is missing for some participants
Clinical Characteristics
About 36.6% of individuals seen for an initial clinic consultation reported at least one prior psychiatric hospitalization (e.g., for suicidality/self-harm). The majority reported being abstinent from drugs (76.6%) and alcohol (65.4%) over the past month; 4.7% exhibited current alcohol use disorder and 9.3% exhibited other substance use disorder. The majority (60.2%) were currently taking psychiatric medications, predominantly antipsychotics (39.4%), mood stabilizers (33.9%), and/or antidepressants (33.9%). Regarding non-psychotic diagnoses, the majority of clients met criteria for mood (69.2%) and anxiety (68.8%) disorders.
The majority met CHR criteria based on the SIPS (63.7%). There were a small number of clients (5.8%) meeting broad CHR criteria 31, which includes individuals presenting with only negative symptoms or with attenuated positive symptoms that have not recently increased. A number of clients (19.9%) already met criteria for full psychosis. About 10.5% of those evaluated were found to have no symptoms of psychosis or CHR.
Composite Case Example: “Essie”
General Information
Essie was a 16 year-old Nigerian-American 10th grader referred by a school counselor who treated her when her grades declined from A’s in 9th grade to C’s and D’s. She had been leaving classes frequently, complaining of headaches and eye trouble. She eventually disclosed to her counselor that she was seeing things “that aren’t really there,” including visions of snakes. She knew the visions were not real, but they interfered with her concentration. She worried she was losing her mind.
Referral Process
The school counselor called CEDAR to determine whether Essie’s symptoms were appropriate for a referral and to discuss how to talk with Essie and her family about getting an evaluation. The counselor arranged a meeting with Essie and her parents so Essie could tell her parents about her difficulties. The counselor noted there could be a number of explanations for these symptoms, and recommended getting a consultation with a program with relevant specialized expertise. They called CEDAR from their meeting so Essie and her parents could talk directly with a clinician.
Consultation
The CEDAR intake team first met with Essie and her parents together, then invited Essie to meet alone with two clinicians while the family met with two others. It was clear that Essie had been quite accomplished. Her parents listed her many honors – obtaining a merit-based scholarship to a competitive high school and achieving state-wide recognition for her violin performances. Her mother wondered if Essie had attention deficit/hyperactivity disorder because she appeared to be having trouble paying attention in school; her father thought Essie needed to spend more time studying. Essie sank into her seat while her parents described her accomplishments and the ways she was recently falling short of her prior functioning.
When the group separated, Essie was surprised by some of the SIPS interview questions, which prompted her to describe experiences she had never told anyone. She detailed her experience of visual hallucinations, revealing that these began infrequently three years earlier, but began happening almost daily in the last six months. She also noted she occasionally heard whispers. She was bothered by the visions and whispers, but she recognized these experiences were a product of her mind. She was having difficulty getting her point across when talking, and schoolwork was taking longer to complete. She was staying up late to finish homework and then falling asleep during class. She began withdrawing from friends because spending time with them was exhausting. She was reassured to find out that other young people have these kinds of experiences. Based on the worsening of these symptoms in the past year and her maintained insight about them, she met SIPS criteria for attenuated positive symptom syndrome.
During the separate family assessment, Essie’s mother reported having a normal, full-term pregnancy and that Essie met all developmental milestones normatively. She had close and casual friends until the past year, when she began spending almost all her time alone. A maternal aunt experienced a marijuana-induced psychotic episode as a teenager.
Feedback
Following the interviews, the CEDAR team convened to discuss feedback and recommendations with Essie and her family, being careful to use the family’s words and factual, non-stigmatizing language. The team commended Essie and her family for paying attention to her symptoms, particularly given their interference with school and social functioning. The team emphasized these symptoms were treatable, and recommended that Essie and her family participate in treatment through the clinic, including psychiatry and health management, psychotherapy, family treatment, and school coaching.
Psychiatry/health management
Given the distressing nature of Essie’s visual hallucinations, the psychiatrist considered low-dose antipsychotic medication. However, she also considered the potentially negative impact of medications on Essie’s health trajectory. Given that Essie and her family would be able to make use of a range of specialized, comprehensive, psychosocial treatments at CEDAR, the psychiatrist decided to hold off on recommending medication while these other treatments were initiated. The psychiatrist emphasized the importance of good self-care, including adequate sleep and exercise.
Individual Psychotherapy
Essie began weekly individual integrated cognitive-behavioral42 and acceptance and commitment67 therapy. Her therapist worked with Essie to identify her personal values and how her symptoms were interfering. Essie identified valuing being a good student and loyal friend, and she expressed frustration about how her symptoms intruded on her ability to act on her values. The therapist helped Essie learn about her symptoms and challenged her concern that she was losing her mind. By monitoring her experiences of and responses to hallucinations, they discovered that Essie generally had catastrophizing thoughts (e.g., “everyone will know I’m crazy!”). Leaving class complaining of headaches had the negative consequences of missing class and falling further behind. They also discovered triggers for hallucinations (e.g., staying up late). Essie developed and wrote coping statements on an index card to look at when she was feeling distressed. Essie also learned and practiced mindfulness skills, including focusing on the present, making room for difficult experiences, and letting go of distressing thoughts. The therapist encouraged Essie to take behavioral steps towards her values, such as reaching out to make plans with friends.
Family Treatment
Essie and her family participated in 18 sessions of family focused treatment (FFT),43,44 which emphasizes 1) psychoeducation, 2) learning and practicing skills for improving family communication, and 3) practicing a structured problem-solving method to collaboratively reach and try out creative solutions to problems and goals. Initially, Essie’s parents had differing attitudes towards her treatment. Essie’s mother was eager for her to receive help and accommodations. Her father felt she needed to work harder to overcome difficulties and worried that accommodations would weaken her. The family clinician paid special attention to connecting with all family members, especially Essie’s father when he seemed reluctant to participate. Over time, he shared concerns about Essie’s defiance at home and the possibility that she was “getting permission” to act this way during therapy sessions. As he was reassured that Essie and the CEDAR team shared the common goal of her getting back on track with her school performance, he became more willing to try some of the team’s suggestions. The family was able to problem-solve about the tension between Nigerian and American traditions, particularly teen, cultural norms.
School/Job Coaching
Essie attended weekly school coaching to improve her school performance. Essie and her coach clarified her academic goals and obstacles to current school success. They created a schedule to ensure she got adequate sleep in order to function at her best. They also worked on reducing Essie’s school-related stress. This included dropping one elective class, arranging for Essie to receive extra time to complete homework with a note from her parents, establishing a regular time to complete homework at the library where Essie had fewer distractions, planning ahead for tests and papers, and breaking down larger assignments into smaller, more manageable steps.
Over time, Essie began to experience more successes in school. As she became more confident, she rediscovered her enjoyment of playing the violin outside of competitive venues. She began volunteering one day a week with a music teacher at an elementary school and expressed interest in pursuing a teaching career.
Discussion: Challenges and Future Directions
We have described one path for the development of a public/academic partnership aimed at providing early identification for individuals at risk for psychosis. Through a combination of federal, state, and foundation funding and resources, CEDAR has provided services to over 180 young people and families since March 2009. We conclude with a discussion of challenges and future directions for EI.
Reaching People before Onset of Full Psychosis
An ongoing challenge for CEDAR has been attracting appropriate referrals; namely, young people at risk for, but who have not yet experienced, full blown psychosis. Many CEDAR referrals have an established psychotic disorder, evident either at phone screening (28.2% of phone referrals) or in-person assessment (19.9% of initial evaluations). Thus, a large percentage of CEDAR referrals are recognized and referred “too late,” underscoring the ongoing problem of DUP. Although CEDAR staff often refer such clients to local FEP services such as PREP®, barriers to reaching FEP services include strict entry criteria (e.g., no more than 12 months of antipsychotic treatment), waiting lists, or client aversion to more clearly identified mental health services and the stigma associated with treatment in typical psychiatric settings.
An important criticism of the field of EI in psychosis has been the failure to identify or engage the vast majority of those developing psychosis3. Further, a substantial proportion of those who meet eligibility criteria for CHR have already experienced serious impairments in social and role functioning, psychiatric hospitalization, and were prescribed antipsychotic medication.3 Individuals with milder or more ambiguous signs and symptoms of psychosis risk or who are less impaired are less likely to reach out for care. Of note, 29% of individuals who contacted the clinic were “lost to follow up” before completion of phone screening, including a subset who appeared to be a good fit for an evaluation but never scheduled an appointment. Some of these individuals only re-contact CEDAR after symptoms have worsened, often months or even years following the initial phone call. Improving CEDAR’s ability to effectively engage these young people and families remains an important priority.
Demographic data indicate that those seen for intake/consultation were disproportionately from highly educated families. This is not entirely surprising given that academic, medical/research settings tend to attract more highly educated and higher socioeconomic status clients who actively seek out these settings and have the resources and job flexibility to access CEDAR during available hours. A high priority for CEDAR is to improve accessibility for young people from more racially, educationally, and socioeconomically diverse backgrounds.
Data Collection and Management in a Clinic Setting
CEDAR Clinic developed a clinical assessment battery for treatment planning and embedded it into CEDAR clinical practices. As staff resources are limited, we prioritized information needed to track clinical outcomes (e.g., SIPS and social/role functioning) and information valued by DMH (e.g., housing stability, substance abuse, work status, legal involvement). We used appropriate assessments and forms that were already being collected for clients who are participating in CEDAR research to avoid excessive burden. Despite this, clinical demands and changes in clinic staffing and trainees over time have led to changes in the assessment battery and variability in whether all aspects of the assessment have been completed.
Efficient Use of Limited Resources
Training a new generation of clinicians in early psychosis intervention is an important part of CEDAR’s educational mission, yet involves some challenges. Having trainees from multiple disciplines observe seasoned clinicians during consultations means having three to four clinicians involved in an assessment. This can be overwhelming for the client and family and involve quite a bit of clinician time. At the same time, the team approach provides additional resources for speaking with outside providers, integrating clinical information and completing documentation, and conceptualizing comprehensive clinical recommendations.
Funding
Support for CEDAR staff, infrastructure, and training comes from foundations, donors, and DMH. Although the MMHC collects insurance payment for a portion of CEDAR services, many services provided are not reimbursable (e.g., case management, services provided by trainees, team meetings). Foundation funding is generally short-term with the expectation that programs become financially self-sufficient. DMH funding, dependent on the yearly state budget, has built-in uncertainties. On one occasion, the clinic prepared to close, with funding becoming available only at the last minute. Precious staff time has been committed to identifying and applying for new funding.
Despite these challenges, CEDAR has provided high quality services to young people at CHR and their families regardless of their insurance status or ability to pay for services. The lack of dependence on a fee for service model has allowed us to model CEDAR after our existing coordinated specialty care FEP program (PREP®) and to include most of the elements of coordinated specialty care as recommended by NIMH68 for FEP. This includes a team based approach to care, assertive case management, individual psychotherapy, family education and support, and psychopharmacology. Although we offer employment and educational support, limited resources have precluded hiring a full time supported education/employment specialist who can provide services using the individualized placement and support model.
If systematic empirical data on outcomes and cost effectiveness research continues to support the value of EI,,69, 70 we expect further growth in EI services for young people at risk for mental illness and expansion of programs like CEDAR. While EI models are clinically intuitive and supported by several studies on individual therapeutic approaches to CHR, there is a need for controlled studies of multi-element specialty care models for CHR. A good example is the RAISE study, which has shown promising results for EI after the first psychotic episode71 Once available, such data may facilitate funding priorities for CHR EI programs from federal, state, and third party sources and scaling up early coordinated specialty care to change the early course of mental illness and enhance functional outcomes.
Acknowledgments
We especially thank the patients and their families for working with us to build this program over the past decade. We thank the many faculty, staff, and trainees of the Massachusetts Mental Health Center and the Beth Israel Deaconess Medical Center Department of Psychiatry, and Massachusetts Department of Mental Health personnel for their contributions to building this program. They include Rebecca Arcidiacono, Maryanne Badaracco, Benjamin Boone, Mark Cattalani, Melissa DeLeon, Donna Downing, Ken Duckworth, Mary Ellen Foti, Marcia Fowler, Jean Frazier, Ryan Guest, George Handran, David Hoffman, Joanna Imbert, Brooke Katz, Patricia Kenny, Barbara Leadholm, Peggy Lester, Huijun Li, Jennifer McKelvey, Joan Mikula, Kyle Minor, Rachel and Bob Perlmutter, Clifford Robinson, Laura Rood, Elizabeth Simpson and Rachel Steiner. We also thank our colleagues around the world working in CHR programs or research who advised us, visited us and helped build our program: Jean Addington, Barbara Cornblatt, Todd Lencz, William McFarlane, Thomas McGlashan, Patrick McGorry, Tandy Miller, Frauke Schulz-Lutter, and Barbara Walsh.
Financial Support: Supported in part by the Sidney R. Baer, Jr. Foundation (Seidman, Principal Investigator), an Anonymous Family Foundation, by the Commonwealth of Massachusetts Department of Mental Health Grant, SCDMH82101008006, “Center of Excellence in Clinical Neuroscience and Psychopharmacological Research (Seidman, Principal Investigator, 2002–2017), by NIMH Grant 1R34MH105596 (Keshavan, PI), and by NIMH Grant K23 MH102358 (Woodberry, PI).
Footnotes
Conflict of interest statement: The authors report no disclosures or conflicts of interest.
BIBLIOGRAPHY
- 1.Yung AR, McGorry PD, MacFarlane CA, Patton G. The PACE clinic: Development of a clinical service for young people at high risk of psychosis. Australian Psychiatry. 1995;3:345–9. SRC - GoogleScholar. [Google Scholar]
- 2.Caplan B, Zimmet SV, Meyer EC, et al. Prevention and recovery in early psychosis (PREP((R))): building a public-academic partnership program in Massachusetts, United States. Asian J Psychiatr. 2013;6:171–7. doi: 10.1016/j.ajp.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Woodberry KA, Seidman LJ, Bryant C, et al. Treatment precedes positive symptoms in North American adolescent and young adult clinical high risk cohort. J Clin Child Adolesc Psychol. 2016:1–10. doi: 10.1080/15374416.2016.1212361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keshavan MS, Schooler NR. First-episode studies in schizophrenia: Criteria and characterization. Schizophr Bull. 1992;18:491–513. doi: 10.1093/schbul/18.3.491. [DOI] [PubMed] [Google Scholar]
- 5.McGlashan TH. Early detection and intervention in schizophrenia: research. Schizophr Bull. 1996;22:327–45. doi: 10.1093/schbul/22.2.327. [DOI] [PubMed] [Google Scholar]
- 6.Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22:353–70. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]
- 7.Klosterkoetter J, Hellmich M, Steinmeyer EM, Schultze-Lutter F. Diagnosing schizophrenia in the initial prodromal phase. Arch Gen Psychiatry. 2001;58:158–64. doi: 10.1001/archpsyc.58.2.158. [DOI] [PubMed] [Google Scholar]
- 8.Johnstone E, Crow T, MacMillan J, Owens D, Bydder G, Steiner R. A magnetic resonance study of early schizophrenia. J Neurol Neurosurg Psychiatry. 1986;49:136–9. doi: 10.1136/jnnp.49.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Birchwood M, Macmillan F. Early intervention in schizophrenia. Aust N Z J Psychiatry. 1993;27:374–8. doi: 10.3109/00048679309075792. [DOI] [PubMed] [Google Scholar]
- 10.Howes O, Falkenberg I. Early detection and intervention in bipolar affective disorder: Targeting the development of the disorder. Curr Psychiatry Res. 2011;13:493–9. doi: 10.1007/s11920-011-0229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fusar-Poli P, Deste G, Smieskova R, et al. Cognitive functioning in prodromal psychosis: a meta-analysis. Arch Gen Psychiatry. 2012a;69:562–71. doi: 10.1001/archgenpsychiatry.2011.1592. [DOI] [PubMed] [Google Scholar]
- 12.Giuliano AJ, Li H, Mesholam-Gately RI, Sorenson SM, Woodberry KA, Seidman LJ. Neurocognition in the psychosis risk syndrome: a quantitative and qualitative review. Curr Pharm Des. 2012;18:399–415. doi: 10.2174/138161212799316019. [DOI] [PubMed] [Google Scholar]
- 13.Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ. Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology. 2009;23:315–36. doi: 10.1037/a0014708. [DOI] [PubMed] [Google Scholar]
- 14.Pantelis C, Velakoulis D, McGorry PD, et al. Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison. Lancet (London, England) 2003;361:281–8. doi: 10.1016/S0140-6736(03)12323-9. [DOI] [PubMed] [Google Scholar]
- 15.Murray RM, Lewis SW. Is schizophrenia a neurodevelopmental disorder? British medical journal (Clinical research ed) 1987;295:681–2. doi: 10.1136/bmj.295.6600.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seidman LJ. The neuropsychology of schizophrenia: a neurodevelopmental and case study approach. J Neuropsychiatry Clin Neurosci. 1990;2:301–12. doi: 10.1176/jnp.2.3.301. [DOI] [PubMed] [Google Scholar]
- 17.Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry. 1987;44:660–9. doi: 10.1001/archpsyc.1987.01800190080012. [DOI] [PubMed] [Google Scholar]
- 18.Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry. 2005;162:1785–804. doi: 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- 19.Addington J. The promise of early intervention. Early Interv Psychiatry. 2007;1:294–307. doi: 10.1111/j.1751-7893.2007.00043.x. [DOI] [PubMed] [Google Scholar]
- 20.Schimmelmann BG, Huber CG, Lambert M, Cotton S, McGorry PD, Conus P. Impact of duration of untreated psychosis on pre-treatment, baseline, and outcome characteristics in an epidemiological first-episode psychosis cohort. J Psychiatr Res. 2008;42:982–90. doi: 10.1016/j.jpsychires.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 21.Wyatt RJ. Neuroleptics and the natural course of schizophrenia. Schizophr Bull. 1991;17:325–51. doi: 10.1093/schbul/17.2.325. [DOI] [PubMed] [Google Scholar]
- 22.Liu CH, Keshavan MS, Tronick E, Seidman LJ. Perinatal risks and childhood premorbid indicators of later psychosis: Next steps for early psychosocial interventions. Schizophr Bull. 2015;41:801–16. doi: 10.1093/schbul/sbv047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hafner H, Maurer K. Early Detection and Management of Mental Disorders. John Wiley & Sons; 2005. Prodromal Symptoms and Early Detection of Schizophrenia. [Google Scholar]
- 24.Woodberry KA, Shapiro DI, Bryant C, Seidman LJ. Progress and Future Directions in Research on the Psychosis Prodrome: A Review for Clinicians. Harvard Rev Psychiatry. 2016a;24:87–103. doi: 10.1097/HRP.0000000000000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGlashan TH, Walsh BC, Woods SW. The psychosis-risk syndrome: Handbook for diagnosis and follow-up. New York, NY: Oxford University Press; 2010. [Google Scholar]
- 26.Fusar-Poli P, Bonoldi I, Yung AR, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012b;69:220–9. doi: 10.1001/archgenpsychiatry.2011.1472. [DOI] [PubMed] [Google Scholar]
- 27.Addington J, Heinssen R. Prediction and prevention of psychosis in youth at clinical high risk. Annu Rev Clin Psychol. 2012;8:269–89. doi: 10.1146/annurev-clinpsy-032511-143146. [DOI] [PubMed] [Google Scholar]
- 28.Tarbox SI, Addington J, Cadenhead KS, et al. Premorbid functional development and conversion to psychosis in clinical high-risk youths. Dev Psychopathol. 2013;25:1171–86. doi: 10.1017/S0954579413000448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cannon TD, Yu C, Addington J, et al. An Individualized Risk Calculator for Research in Prodromal Psychosis. Am J Psychiatry. 2016;173:980–8. doi: 10.1176/appi.ajp.2016.15070890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Woods SW, Miller TJ, McGlashan TH. The “prodromal” patient: both symptomatic and at-risk. CNS spectrums. 2001;6:223–32. doi: 10.1017/s1092852900008609. [DOI] [PubMed] [Google Scholar]
- 31.Keshavan MS, DeLisi LE, Seidman LJ. Early and broadly defined psychosis risk mental states. Schizophr Res. 2011 Mar;126(1–3):1–10. doi: 10.1016/j.schres.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fusar-Poli P, Borgwardt S, Bechdolf A, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–20. doi: 10.1001/jamapsychiatry.2013.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fusar-Poli P, Cappucciati M, Borgwardt S, et al. Heterogeneity of psychosis risk within individuals at clinical high risk: A meta-analytical stratification. JAMA Psychiatry. 2016;73:113–20. doi: 10.1001/jamapsychiatry.2015.2324. [DOI] [PubMed] [Google Scholar]
- 34.Compton MT, McGlashan T, McGorry P. An overview of prodromal states, the duration of untreated psychosis, and early intervention paradigms. Psychiatric Annals. 2007;37:340–8. [Google Scholar]
- 35.McGorry PD, Killackey EJ. Early intervention in psychosis: a new evidence based paradigm. Epidemiologia e psichiatria sociale. 2002;11:237–47. doi: 10.1017/s1121189x00005807. [DOI] [PubMed] [Google Scholar]
- 36.McGorry PD, Nelson B, Goldstone S, Yung AR. Clinical staging: a heuristic and practical strategy for new research and better health and social outcomes for psychotic and related mood disorders. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2010;55:486–97. doi: 10.1177/070674371005500803. [DOI] [PubMed] [Google Scholar]
- 37.Niendam TA, Bearden CE, Zinberg J, Johnson JK, O’Brien M, Cannon TD. The course of neurocognition and social functioning in individuals at ultra high risk for psychosis. Schizophr Bull. 2007;33:772–81. doi: 10.1093/schbul/sbm020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thompson E, Millman ZB, Okuzawa N, et al. Evidence-based early interventions for individuals at clinical high risk for psychosis: a review of treatment components. J Nerv Ment Dis. 2015;203:342–51. doi: 10.1097/NMD.0000000000000287. [DOI] [PubMed] [Google Scholar]
- 39.Seidman LJ, Shapiro DI, Stone WS, et al. Association of neurocognition and transition to psychosis: baseline functioning in the second phase of the North American Prodrome Longitudinal Study. JAMA Psychiatry. 2016;73:239–1248. doi: 10.1001/jamapsychiatry.2016.2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmidt SJ, Schultze-Lutter F, Schimmelmann BG, et al. EPA guidance on the early intervention in clinical high risk states of psychoses. Eur Psychiatry. 2015;30:388–404. doi: 10.1016/j.eurpsy.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 41.van der Gaag M, Smit F, Bechdolf A, et al. Preventing a first episode of psychosis: Meta-analysis of randomized controlled prevention trials of 12 month and longer-term follow-ups. Schizophr Res. 2013:1–3. doi: 10.1016/j.schres.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 42.Morrison AP, French P, Walford L, et al. Cognitive therapy for the prevention of psychosis in people at ultra-high risk: randomised controlled trial. Br J Psychiatry. 2004;185:291–7. doi: 10.1192/bjp.185.4.291. [DOI] [PubMed] [Google Scholar]
- 43.Miklowitz DJ, O’Brien MP, Schlosser DA, et al. Family-focused treatment for adolescents and young adults at high risk for psychosis: results of a randomized trial. J Am Acad Child Adolesc Psychiatry. 2014;53:848–58. doi: 10.1016/j.jaac.2014.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O’Brien MP, Miklowitz DJ, Candan KA, et al. A randomized trial of family focused therapy with populations at clinical high risk for psychosis: Effects on interactional behavior. Journal of Consulting and Clinical Psychology. 2014;82:90–101. doi: 10.1037/a0034667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bechdolf A, Wagner M, Ruhrmann S, et al. Preventing progression to first-episode psychosis in early initial prodromal states. Br J Psychiatry. 2012;200:22–9. doi: 10.1192/bjp.bp.109.066357. [DOI] [PubMed] [Google Scholar]
- 46.Nordentoft M, Thorup A, Petersen L, et al. Transition rates from schizotypal disorder to psychotic disorder for first-contact patients included in the OPUS trial. A randomized clinical trial of integrated treatment and standard treatment. Schizophr Res. 2006;83:29–40. doi: 10.1016/j.schres.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 47.Hooker C, EE C, TJ E, et al. A pilot study of cognitive training in clinical high risk for psychosis: Initial evidence of cognitive benefit. Schizophr Res. 2014;157:314–6. doi: 10.1016/j.schres.2014.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Barlati S, Peri L, Deste G, Vita A. Non-pharmacological interventions in early schizophrenia: Focus on cogntive remediation. Journal of psychopathology/giornale di psicopatologia. 2015;21:1–12. [Google Scholar]
- 49.Phillips LJ, McGorry PD, Yuen HP, et al. Medium term follow-up of a randomized controlled trial of interventions for young people at ultra high risk of psychosis. Schizophr Res. 2007;96:25–33. doi: 10.1016/j.schres.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 50.McGlashan TH, Zipursky RB, Perkins D, et al. Randomized, double-blind trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. Am J Psychiatry. 2006;163:790–9. doi: 10.1176/ajp.2006.163.5.790. [DOI] [PubMed] [Google Scholar]
- 51.McGorry PD, Nelson B, Amminger GP, et al. Intervention in individuals at ultra-high risk for psychosis: a review and future directions. J Clin Psychiatry. 2009;70:1206–12. doi: 10.4088/JCP.08r04472. [DOI] [PubMed] [Google Scholar]
- 52.Phillips LJ, Nelson B, Yuen HP, et al. Randomized controlled trial of interventions for young people at ultra-high risk of psychosis: study design and baseline characteristics. Aust N Z J Psychiatry. 2009;43:818–29. doi: 10.1080/00048670903107625. [DOI] [PubMed] [Google Scholar]
- 53.Amminger GP, Schafer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: A randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67:146–54. doi: 10.1001/archgenpsychiatry.2009.192. [DOI] [PubMed] [Google Scholar]
- 54.McGorry PD, Nelson B, Markulev C, et al. Effect of ω-3 Polyunsaturated Fatty Acids in Young People at Ultrahigh Risk for Psychotic Disorders: The NEURAPRO Randomized Clinical Trial. JAMA psychiatry. 2017;74:19–27. doi: 10.1001/jamapsychiatry.2016.2902. [DOI] [PubMed] [Google Scholar]
- 55.Cornblatt BA, Lencz T, Smith CW, et al. Can antidepressants be used to treat the schizophrenia prodrome? Results of a prospective, naturalistic treatment study of adolescents. J Clin Psychiatry. 2007;68:546–57. doi: 10.4088/jcp.v68n0410. [DOI] [PubMed] [Google Scholar]
- 56.Srihari V, Shah J, Keshavan M. Is early intervention for psychosis feasible and effective? Psychiatr Clin North Am. 2012;35:613–31. doi: 10.1016/j.psc.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tsuang MT. Images in psychiatry. The Massachusetts Mental Health Center Am J Psychiatry. 1997;154:423. doi: 10.1176/ajp.154.3.423. [DOI] [PubMed] [Google Scholar]
- 58.Salzman C, Seidman LJ, Keshavan MS. The Massachusetts Mental Health Center: going forward after 100 years. Am J Psychiatry. 2012;169:1037. doi: 10.1176/appi.ajp.2012.12030362. [DOI] [PubMed] [Google Scholar]
- 59.Kremen WS, Seidman LJ, Pepple JR, Lyons MJ, Tsuang MT, Faraone SV. Neuropsychological risk indicators for schizophrenia: A review of family studies. Schizophrenia Bulletin. 1994;20:96–108. doi: 10.1093/schbul/20.1.103. [DOI] [PubMed] [Google Scholar]
- 60.Stone W, Faraone S, Seidman L, Olson E, Tsuang M. Searching for the liability to schizophrenia: Concepts and methods underlying genetic high-risk studies of adolescents. J Child Adolesc Psychopharmacol. 2005;15:403–17. doi: 10.1089/cap.2005.15.403. [DOI] [PubMed] [Google Scholar]
- 61.Seidman LJ, Pousada-Casal A, Scala S, Meyer EC, Stone WS, Thermenos HW, Molokotos E, Agnew-Blais J, Tsuang MT, Faraone SV. Auditory vigilance and working memory in youth at familial risk for schizophrenia or affective psychosis in the Harvard Adolescent Family High Risk Study. Journal of International Neuropsychological Society. 2016;10:1026–1037. doi: 10.1017/S1355617716000242. [DOI] [PubMed] [Google Scholar]
- 62.Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Franz L, Carter T, Leiner AS, Bergner E, Thompson NJ, Compton MT. Stigma and treatment delay in first-episode psychosis: a grounded theory study. Early Interv Psychiatry. 2010;4:47–56. doi: 10.1111/j.1751-7893.2009.00155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McGorry PD, Tanti C, Stokes R, et al. headspace: Australia’s National Youth Mental Health Foundation--where young minds come first. Med J Aust. 2007;187:S68–70. doi: 10.5694/j.1326-5377.2007.tb01342.x. [DOI] [PubMed] [Google Scholar]
- 65.Cornblatt BA, Auther A, Niendam T, et al. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. 2007;33:688–702. doi: 10.1093/schbul/sbm029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Niendam TA, Bearden CE, Johnson JK, Cannon TD. Global functioning: Role scale (GF: Role) Los Angeles, CA: University of California, Los Angeles; 2006. [Google Scholar]
- 67.Hayes S, Strosahl K, Wilson K. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change. New York: Guilford Press; 2012. [Google Scholar]
- 68.Valmaggia LR, McGuire PK, Fusar-Poli P, Howes O, McCrone P. Economic impact of early detection and early intervention of psychosis. Curr Pharm Des. 2012;18:592–5. doi: 10.2174/138161212799316145. [DOI] [PubMed] [Google Scholar]
- 69.Heinssen RK, Goldstein AB, Azrin ST. Evidence-based treatments for first episode psychosis: Components of coordinated specialty care [White paper] National Institute of Mental Health; 2014. https://www.nimh.nih.gov/health/topics/schizophrenia/raise/nimh-white-paper-csc-for-fep_147096.pdf. [Google Scholar]
- 70.Ising H, Smit F, Veling W, et al. Cost-effectiveness of preventing first-episode psychosis in ultra-high-risk subjects: Multi-centre randomized controlled trial. Psychol Med. 2015;45:1435–46. doi: 10.1017/S0033291714002530. [DOI] [PubMed] [Google Scholar]
- 71.Kane JM, Robinson DG, Schooler NR, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. Am J Psychiatry. 2016;173:362–72. doi: 10.1176/appi.ajp.2015.15050632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hogarty GE, Flesher S, Ulrich R, et al. Cognitive enhancement therapy for schizophrenia: effects of a 2-year randomized trial on cognition and behavior. Arch Gen Psychiatry. 2004;61:866–76. doi: 10.1001/archpsyc.61.9.866. [DOI] [PubMed] [Google Scholar]