Abstract
Background.
There is a great deal of tools for treatment of occipital neuralgia but currently we are lacking a complete consensus among practitioners regarding the optimal approach to this debilitating condition. Occipital nerve block (ONB) is known as one of the management options but there is lack of scientific literature exploring its effectiveness.
Materials and methods.
The prospective study was undertaken between March 2014 and February 2018 at the State Vilnius University Hospital. Forty-four patients aged from 28 to 84 years (age mean = 56.30 ± 14.71) of which 79.55% were female (n = 35) were diagnosed with occipital neuralgia (ON) and treated with a local anaesthetic and corticosteroids combination injection into the greater or greater plus lesser occipital nerve (n = 29 and n = 15, respectively) and followed up after 6 months. Analysis of the outcomes of those patients was done by comparing the Visual Analog Scale (VAS) and Barrow Neurological Institute Pain Intensity Score (BNIPIS) prior to treatment, 24 hours after the block, and at a follow-up 6 months later. Analgesic medication consumption before and after 6 months was recorded. A comparison of procedure efficacy in lidocaine and bupivacaine groups was made. Evaluation of block potency for acute and chronic pain categories was conducted as well. The success criteria were defined as patient satisfaction with own condition for at least 6 months, not requiring another block in order to stay comfortable.
Results.
Of 44 patients, 42 (95.45%) who underwent the occipital nerve block procedure showed satisfactory results for at least 6 months. Mean headache VAS scores decreased from 7.23 ± 0.93 (pre-treatment) to 1.95 ± 1.59 (24 hours after, p < 0.0001) and increased to 2.21 ± 1.73 at the follow-up after 6 months, showing no statistically significant difference between post-interventional and six-month VAS scores (p = 0.07). In all patients the necessity of medication to control pain decreased to 16.67% (n = 7) during the the check-up after 6 months. There was no statistically significant difference in the effectiveness of ONB with regard to the local anaesthetic used or the pain group targeted. Similar results were obtained comparing patients who underwent more than one ONB.
Conclusions.
Occipital nerve block with a local anaesthetic and corticosteroids provides a safe, simple, and effective treatment method for the patient with medically-refractory occipital neuralgia.
Keywords: occipital neuralgia, greater occipital nerve, lesser occipital nerve, occipital nerve block, headache
Abstract
PAKAUŠINĖS NEURALGIJOS GYDYMO EFEKTYVUMAS TAIKANT NERVŲ BLOKADĄ: PROSPEKTYVINĖ 44 PACIENTŲ ANALIZĖ
Santrauka
Įvadas. Šiuo metu yra nemažai potencialių pakaušinės neuralgijos gydymo būdų, tačiau trūksta susitarimo tarp gydytojų dėl optimalaus šios ligos gydymo plano. Pakaušinių nervų blokada yra vienas iš galimų pasirinkimų, tačiau mokslinėje literatūroje trūksta tyrimų, kurie analizuotų šio metodo efektyvumą.
Tyrimo medžiaga ir metodai. Prospektyvinis tyrimas vyko nuo 2014 metų kovo iki 2018 metų vasario mėnesio Respublikinėje Vilniaus universitetinėje ligoninėje. 44 pacientams, kurių amžius nuo 28 iki 84 metų (amžiaus vidurkis = 56,30 ± 14,71), iš jų 79,55 % – moterys (n = 35), diagnozuota medikamentiniam gydymui atspari pakaušinė neuralgija. Jie buvo gydomi lokalių anestetikų ir kortikosteroidų injekcijos kombinacija į didįjį arba didįjį ir mažąjį pakaušinius nervus (atitinkamai n = 29 ir n = 15). Pacientų būklė vertinta prieš procedūrą ir praėjus 24 val. ir 6 mėn. po jos, taikant skausmo vizualinę analogų (VAS) ir Barrow neurologinio instituto skausmo intensyvumo skales. Taip pat dokumentuotas analgetikų vartojimas prieš gydymą ir praėjus 6 mėnesiams. Palyginti skirtingų vaistų grupių analgetikų – lidokaino ir bupivakaino – gydymo rezultatai. Be to, pacientai buvo suskirstyti į ūmaus ir lėtinio skausmo stebėjimo grupes, VAS rodikliai palyginti abiejose grupėse prieš intervenciją, 24 valandos po jos ir po 6 mėnesių. Teigiamas gydymo rezultatas traktuotas kaip paties paciento pasitenkinimas savo būkle bent šešis mėnesius be pakartotinės injekcijos.
Rezultatai. Iš 44 pacientų teigiamą poveikį bent 6 mėn. pajautė 42 tiriamieji (95,45 %). Vidutinis galvos skausmo VAS sumažėjo nuo 7,23 ± 0,93 iki 1,95 ± 1,59 (24 val. po intervencijos, p < 0,0001) ir padidėjo iki 2,21 ± 1,73 patikrinus pacientus po pusės metų, tačiau nėra statistiškai reikšmingo skirtumo lyginant pointervencinį 24 val. ir 6 mėn. stebėjimo VAS vidurkį (p = 0,07). Prieš injekciją visi pacientai vartojo analgetikus, tačiau per 6 mėn. sekimą jų reikėjo 16,67 % tiriamųjų (n = 7). Nepavyko gauti statistiškai reikšmingo skirtumo palyginus VAS vidurkį tarp lidokaino ir bupivakaino bei ūmaus ir lėtinio skausmo pacientų stebėjimo grupių. Panašūs rezultatai gauti vertinant pacientus, kuriems blokada taikyta pakartotinai.
Išvados. Pakaušinio nervo blokada naudojant lokalaus anestetiko ir kortikosteroidų mišinį yra paprastas, efektyvus ir saugus konservatyviam gydymo būdui atsparios pakaušinės neuralgijos gydymo metodas.
Raktažodžiai: pakaušinė neuralgija, didysis pakaušinis nervas, mažasis pakaušinis nervas, pakaušinio nervo blokada, galvos skausmas
INTRODUCTION
According to the International Headache Society, occipital neuralgia (ON) is defined as unilateral or bilateral paroxysmal, shooting, or stabbing pain in the posterior part of the scalp, following the distribution of the greater occipital nerve (GON) and/or the lesser occipital nerve (LON). The pain is often accompanied by dysaesthesia or tenderness over the corresponding dermatomes (1).
GON is merely a medial branch of dorsal ramus of C2 spinal nerve exiting between lamina of C1 and C2, bending around the inferior oblique muscle, and coursing deep to semispinalis capitis and trapezius muscles, finally emerging subcutaneously just medial to the occipital artery and lateral to the external occipital protuberance. From there the innervation area extends through the vertex, roughly as far as the coronal suture (2). LON is part of the cervical plexus and is mainly formed of C2 fibres: it pierces deep fascia at Erb’s point and travels subcutaneously towards the retroauricular area along the posterior border of the sternocleidomastoid muscle innervating its epifascial course, and posterosuperiorly to the ear (3).
ON occurs when GON/LON is irritated in virtually any place along the course and this mostly happens due to cervical spondylosis or a chronic contraction of neck muscles but neurogenic causes such as multiple sclerosis or C2 myelitis are possible as well (4–7). Consequently, constant activation of pain pathways due to a certain trigger causes long-term potentiation in the trigeminocervical nucleus, making those neurons hypersensitive to even a minor stimulus and, in extreme cases, leading to allodynia. This process is called central sensitization and is thought to be the main pathophysiological mechanism implicated in ON (8–10).
A wide range of treatment options for ON are available, but currently there is no consensus among practitioners as to which method is superior to another since most of the therapies lack randomized controlled studies and the approach is usually based on present case studies or clinical experience. Nonetheless, the initial focus should be placed on conservative measures, including rest, hot or cold compresses, postural adjustment, and physical therapy with the aim to reduce neuralgic and muscular pain (11). Since in most cases conservative options might not provide the desired relief, first-line pharmacological approach includes tricyclic antidepressants, serotonin reuptake inhibitors, and anticonvulsants, while NSAIDs and paracetamol fare worse in treatment of neuropathic pain, especially in more advanced ON cases (11–13). Pulsed radiofrequency treatment and Botulinum toxin A injections also show their potential for ON management (14, 15). Furthermore, surgical options such as occipital nerve stimulation or neurolysis are used for treatment-resistant ON, but these are invasive and irreversible procedures with their own risks such as infection and/or lead migration (16–18). The treatment should be applied in a step-by-step fashion and more invasive techniques are considered only if conservative treatment options fail to prove satisfactory.
Occipital nerve block (ONB) using a local anaesthetic combined with corticosteroids is a relatively simple and safe procedure providing an effective treatment option for ON with a low risk of side effects. Generally positive results are documented in scientific literature (19–21) regarding the efficacy of the ONB technique, but considerable variability exists in response rates, pain reduction, and relief durations from study to study. For this reasons we decided to share our own experience of managing ON with a blocking method and to compare our findings with the ones present in current literature.
MATERIALS AND METHODS
The prospective analysis of 44 occipital neuralgia patients treated with ONB was done over the period of nearly four years from March 2014 to February 2018 at the State Vilnius University Hospital. All injections were done by a single physician using the same method. The decision on the target nerve was made according to the patients’ complaints and clinical signs, such as pain and dysaesthesia in the distribution area. The injection site for GON block was 2 cm lateral and 2 cm inferior to the external occipital protuberance, while LON block was performed at 5 cm lateral and 1 cm inferior to the same bony landmark (Fig. 1). The injection solution involved a combination of local anaesthetic (lidocaine or bupivacaine) and 4 mg of dexamethasone for all patients.
Fig. 1.
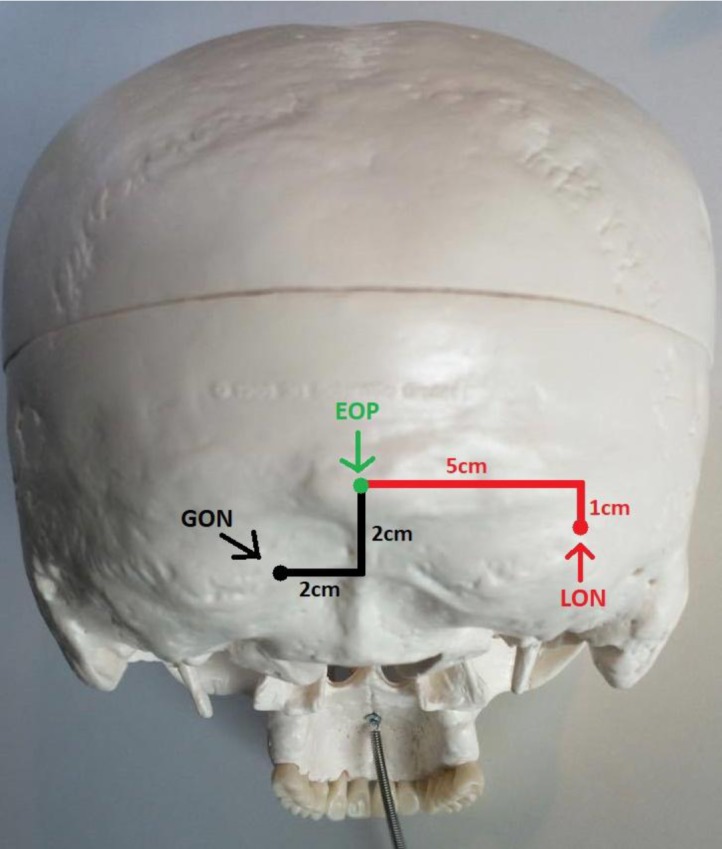
Anatomical representation of greater and lesser occipital nerves block points according to the position of the external occipital protuberance. GON: the greater occipital nerve, LON: the lesser occipital nerve, EOP: the external occipital protuberance
Prior to the block, we recorded the Visual Analog Scale (VAS), Barrow Neurological Institute Pain Intensity Score (BNIPIS, Table 1), and whether the patients used any analgesic medication. Twenty-four hours after the procedure, we re-evaluated VAS of the patients. At the follow-up after 6 months we again recorded VAS, BNIPIS, and the necessity for analgesic medication. Then a comparison of pre-interventional VAS, that of 24 hours after the injection, and of 6 months after the injection was done by paired t-test.
Table 1.
Barrow Neurological Institute Pain Intensity Score (BNIPIS)
| Score | Pain description |
|---|---|
| I | Patient is pain free and does not require medication |
| II | Patient experiences occasional mild pain but no medication is required |
| III | Patient experiences moderate pain but it is adequately controlled with medication |
| IV | Patient experiences moderate pain but it is not adequately controlled with medication |
| V | Patient experiences severe pain and medication does not provide any relief |
Also, we assigned patients to two distinct groups based on the time from onset of the disease: patients experiencing pain for <6 months fell into the acute pain category, while those experiencing pain for >6 months were already considered as a chronic pain group. We assessed whether there was any difference between the VAS score of the two groups before the procedure, 24 hours after the ONB, and, finally, at the follow-up after 6 months by applying the Mann-Whitney U test to evaluate the effectiveness of ONB for pain management in acute and chronic setting.
Similarly, to assess the difference in the potency of lidocaine and bupivacaine as substrates for ONB, we used the Mann-Whitney U test, comparing VAS of two local anaesthetics recorded 24 hours after injection and at the follow-up after 6 months.
Another group of interest were patients who had two or more blocks. There were nine people out of 44 (20.45%) who underwent a second ONB procedure and the time between two procedures was recorded in days. Similarly, VAS values before treatment, 24 hours and 6 months after treatment were compared. In addition, distributions of BNIPIS frequencies were measured.
Finally, there were two patients who received three and five injections, respectively. Both of them were analyzed as separate cases and potentially contributing factors of why those patients needed more frequent blocks were evaluated.
STATISTICAL ANALYSIS
The data was analyzed using the R Project for Statistical Computing, R commander (Version 3.4.1) for Windows. Student’s t-test was used for normally distributed and equal variance quantitative variables for a mean comparison between two groups. For non-normally distributed metric variables comparison, we used the Mann-Whitney U test and the Wilcoxon signed rank test for independent and paired samples, respectively. A statistically significant p value was considered as p < 0.05 in two-sided analysis. The results we obtained are shown as mean ± SD, unless stated differently.
RESULTS
The study consisted of 44 patients aged from 28 to 84 (age mean – 56.30 ± 14.71), of which 79.55% were female (n = 35) who received at least one ONB. In total, we made 29 greater occipital nerve blocks (GONB) and 15 patients required a block of both, greater and lesser occipital nerves. In 72.73% of cases (n = 32), the blockage side was unilateral, while 27.27% (n = 12) required bilateral anaesthetic injections of either both of the nerves or the greater occipital nerve alone. The contingency table (Table 2) illustrates frequency distributions between the target nerve(s) and blockage side(s). At least 6 months of condition improvement was achieved in 95.45% of patients (n = 42), while other two required another ONB before the follow-up after 6 months. In 75% of cases (n = 33), the anaesthetizing agent used was 2% 5 ml of lidocaine, while the rest of 25% (n = 11) of injections were made with 0.5% 5ml of bupivacaine; regardless of the anaesthetic, all of the solutions contained 4 mg of dexamethasone. Patient distribution by pain onset groups was 40.91% for acute and 59.09% for chronic categories, respectively.
Table 2.
Frequency distribution of blocked nerves and sides
| Block side | Total | |||
|---|---|---|---|---|
| Bilateral | Unilateral | |||
| Nerve block | GON and LON | 4 | 11 | 15 |
| GON only | 8 | 21 | 29 | |
| Total | 12 | 32 | 44 | |
Paired t-test was performed to compare VAS scores before ONB, 24 hours after, and at the follow-up after 6 months. Statistically significant mean VAS score difference was recorded during the comparison of pre-interventional and 24 hour post-interventional data, while there was no statistically significant difference between VAS scores at the follow-ups after 24 hours and then after 6 months (Table 3). The frequency table for BNIPIS scale before injection and at the follow-up half a year later is shown in Table 4. Before the treatment, all patients required analgesic medication, but only for 19.04% (n = 8) pain could be controlled adequately. At the follow-up after 6 months, 83.33% (n = 35) of patients did not use any medication for pain, while the rest of them required analgesics in order to stay comfortable.
Table 3.
Comparison of mean VAS scores before the treatment and at check-ups after 24 hours and after 6 months.
| Before the treatment | 24 hours after the treatment | 6 months after the treatment | |
|---|---|---|---|
| VAS score (VAS; SD) | 7.23 ± 0.93 | 1.95 ± 1.59 | 2.21 ± 1.73 |
| Paired t-test (p-value; 95% CI) | p < 0.0001; p = 0.07; | ||
| (4.69–5.58) (–0.49; 0.17) | |||
SD: standard deviation, 95% CI: 95% confidence interval
Table 4.
Comparison of frequency distribution of BNIPIS scores before the treatment and at the follow-up after 6 months
| BNIPIS category | Frequency before the injection | Frequency at the follow-up after 6 months |
|---|---|---|
| I | – | 11 |
| II | – | 24 |
| III | 8 | 7 |
| IV | 15 | - |
| V | 19 | - |
Furthermore, the Mann-Whitney U test was used to assess the difference in potency of two local anaesthetics. There was no statistically significant difference in VAS scores between lidocaine and bupivacaine groups during 24 hours (p = 0.37) and 6 months (p = 0.16) evaluations. The same test was performed to compare the effectiveness of ONB in acute and chronic pain setting and there was no statistically significant difference in median VAS values between groups before ONB (p = 0.86), 24 hours after (p = 0.18), and at the follow-up after 6 months (p = 0.17).
In total, nine patients received at least two ONBs. The mean of 270.1 ± 150.9 days (range 32–465) between the first and the second injections was recorded. The average time from the first injection until the worsening of the condition after the block was 191.2 ± 97.20 days (range 21–315). The Wilcoxon signed rank test was performed to compare VAS scores before the second ONB (median ± IQR = 7 ± 0.25) and 24 hours after (median ± IQR = 2.5 ± 1.5) the procedure, showing statistically significant (p = 0.01) improvement based on the VAS report. The same test was used to compare VAS scores of one day after the block with those at the follow-up after 6 months (median ± IQR = 3 ± 1.5) indicating no statistically significant difference (p = 0.15) between the two measurements. Distributions of frequency of BNIPIS categories included seven patients in category IV and two in category V, whereas after 6 months the distribution was two in category I and seven in category II.
Finally, a manual analysis of two patients who failed to respond to our initial ONB attempts was made. A 55-year-old male required three injections over the period of two months to finally achieve six months of satisfactory result. Similarly, a 34-year-old woman required five injections over the period of 14 months to meet our success criteria. Both patients were in the acute stage of their disease, suffering from ON for about two months before the start of treatment with VAS of 8 and BNIPIS of 5. All of the injections were made using lidocaine but the last ones: for both patients the most recent injection was made with bupivacaine and both of them met our 6-months satisfaction aim after the switch of local anaesthetic.
DISCUSSION
The study we performed implies that the ONB procedure is an effective choice of treatment for patients with ON, reducing mean VAS scores, improving BNIPIS categories and, in general, decreasing medication necessity in order to stay comfortable for at least six months in 95.45% cases. The statistical significance was achieved comparing VAS scores prior to the injection and 24 hours after, providing evidence that ONB is a fast and effective treatment method, while on the other hand VAS scores between 24 hours post-injection and the follow-up after 6 months failed to appear statistically significant suggesting that the effect of treatment is long-lasting and clinically successful six months after the injection.
In addition to decreased pain scores, analgesic medication requirement for coping with pain decreased from 100% to 16.67%, implying another positive clinical benefit that reduces possible side effects of the drugs and might help to control increasing morbidity of analgesics tolerance and medication-overuse headache.
We failed to get any statistically significant differences in VAS scores while comparing the groups according to the usage of lidocaine or bupivacaine as a substrate for injection and, similarly, there was not enough evidence to conclude that the efficacy of ON treatment using block technique depends on whether the patient was in the acute or chronic setting of the disease. These findings suggest that effectiveness of ONB might not depend on local anaesthetic used or the duration of ON prior to treatment.
The data obtained from patients who underwent repeated ONB procedures also imply that multiple injections might be as effective as the first and actually changing the local anaesthetic might be beneficial if original attempts did not provide a sufficient clinical effect.
All preventive measures against adverse events were employed but there still was one minor complication: the patient felt dizziness and nausea after the block, but during the next 15 minutes all the side effects faded away and the patient showed good treatment results.
Comparing our results with currently present in the literature we see a similar tendency and success rate among other practitioners. Tobin’s retrospective analysis of 35 ON patients treated with ONB showed mean decrease of 84% in pain severity that lasted for 8.9 ± 8.8 weeks on average with success rate being 78%. The author concluded that the results were worse due to 36% of patients also suffering from medication-overuse headache and the success rate in those patients was three times lower, implying a decreased effectiveness of ONB for such patients. Another point is that the local anaesthetic used was only bupivacaine and the dose was more than two times smaller (22). In general, the study design and the results are similar except for the fact that our benefit lasted significantly longer. Therefore we hypothesize that a higher dose might prolong the effect but currently we are lacking a comparative study analysing the impact of local anaesthetics dosage on ON.
Even though we are lacking randomized double-blinded comparative study for ON using ONB method, there is well-documented evidence on the efficacy of the ONB as potential management tool for cervicogenic and cluster headaches (23, 24). Similarly, new reports about clinical application of local anaesthetic injections for migraine-type headaches are emerging and implying satisfactory outcomes (25, 26). This positive effect of ONB applicability in a wide range of headache disorders is exceeding the half-life of local anaesthetics and is attributed to the changes in nociceptive pathways in the brain. The current understanding is that injections induce diffuse noxious stimulus inhibitory control across the trigeminocervical complex, preventing further spread of nociceptive sensation towards the primary sensory areas in the cortex (8).
The effectiveness and long-lasting improvement we achieved with ONB procedure in ON patients show similar results in terms of pain relief and duration of improvement in comparison to more invasive and irreversible neurotomy techniques such as pulsed radiofrequency and neurolysis (15, 17).
The main limitations of our study include a relatively small sample size, female predominance, and all of the patients coming from similar socioeconomic and demographic background. The study design was not comparative and due to that we cannot entirely rule out the placebo effect. Likewise, when comparing different local anaesthetics, the group treated with bupivacaine consisted of only 11 patients, and even though there was no statistically significant difference between the two groups, more accurate evaluation is necessary. Finally, there were only nine patients who underwent another ONB procedure and even though results were consistent, the small group size is a major limitation in drawing definitive conclusion regarding repetitive effectiveness of the ONB procedures.
CONCLUSIONS
Despite the limitations, it is hard to deny the effectiveness of ONB as a treatment choice for ON. It is a safe, technically simple, and effective method that carries a minimal risk of side effects and can be applied for patients that do not achieve desired pain relief using conventional pain management methods. In the future, a well-designed randomized double-blinded comparative study is necessary to further evaluate the effectiveness of ONB in a more systematic and controlled fashion in order to establish better treatment recommendations for patients suffering from ON.
Raimondas Juškys, Gytis Šustickas
References
- The International classification of headache disorders, 3rd edition (beta version) Cephalalgia. 2013; 33(9): 629–808. [DOI] [PubMed] [Google Scholar]
- Güvençer M, Akyer P, Sayhan S, Tetik S.. The importance of the greater occipital nerve in the occipital and the suboccipital region for nerve blockade and surgical approaches – an anatomic study on cadavers. Clin Neurol Neurosurg. 2011; 113(4): 289–94. [DOI] [PubMed] [Google Scholar]
- Lee M, Brown M, Chepla K, Okada H, Gatherwright J, Totonchi A, et al. . An anatomical study of the lesser occipital nerve and its potential compression points: implications for surgical treatment of migraine headaches. Plast Reconstr Surg. 2013; 132(6): 1551–6. [DOI] [PubMed] [Google Scholar]
- Cohen SP, Plunkett AR, Wilkinson I, Nguyen C, Kurihara C, Flagg A, 2nd, et al. . Headaches during war: analysis of presentation, treatment, and factors associated with outcome. Cephalalgia. 2012; 32(2): 94–108. [DOI] [PubMed] [Google Scholar]
- Magnusson T, Ragnarsson T, Bjornsson A.. Occipital nerve release in patients with whiplash trauma and occipital neuralgia. Headache. 1996; 36(1): 32–6. [DOI] [PubMed] [Google Scholar]
- Boes CJ. . C2 myelitis presenting with neuralgiform occipital pain. Neurology. 2005; 64(6): 1093–4. [DOI] [PubMed] [Google Scholar]
- De Santi L, Monti L, Menci E, Bellini M, Annunziata P.. Clinical-radiologic heterogeneity of occipital neuralgiform pain as multiple sclerosis relapse. Headache. 2009; 49(2): 304–7. [DOI] [PubMed] [Google Scholar]
- Woolf CJ. . Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011; 152(3 Suppl): S2–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel EaM S. Principles of neural science. 5th ed. New York: McGraw-Hill Medical; 2014. p. 530–56. [Google Scholar]
- Latremoliere A, Woolf CJ. . Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009; 10(9): 895–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanelderen P, Lataster A, Levy R, Mekhail N, van Kleef M, Van Zundert J.. 8. Occipital neuralgia. Pain Pract. 2010; 10(2): 137–44. [DOI] [PubMed] [Google Scholar]
- Trescot AM. . Headache management in an interventional pain practice. Pain physician. 2000; 3(2): 197–200. [PubMed] [Google Scholar]
- Finnerup NB, Sindrup SH, Jensen TS. . The evidence for pharmacological treatment of neuropathic pain. Pain. 2010; 150(3): 573–81. [DOI] [PubMed] [Google Scholar]
- Oh HM, Chung ME. . Botulinum Toxin for Neuropathic Pain: A Review of the Literature. Toxins. 2015; 7(8): 3127–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanelderen P, Rouwette T, De Vooght P, Puylaert M, Heylen R, Vissers K, et al. . Pulsed radiofrequency for the treatment of occipital neuralgia: a prospective study with 6 months of follow-up. Reg Anesth Pain Med. 2010; 35(2): 148–51. [DOI] [PubMed] [Google Scholar]
- Mammis A, Agarwal N, Mogilner AY. . Occipital nerve stimulation. In: Schramm J, editor. Advances and technical standards in neurosurgery: volume 42 Cham: Springer International Publishing; 2015. p. 23–32. [DOI] [PubMed] [Google Scholar]
- Ducic I, Hartmann EC, Larson EE. . Indications and outcomes for surgical treatment of patients with chronic migraine headaches caused by occipital neuralgia. Plast Reconstr Surg. 2009; 123(5): 1453–61. [DOI] [PubMed] [Google Scholar]
- Gille O, Lavignolle B, Vital JM. . Surgical treatment of greater occipital neuralgia by neurolysis of the greater occipital nerve and sectioning of the inferior oblique muscle. Spine. 2004; 29(7): 828–32. [DOI] [PubMed] [Google Scholar]
- Anthony M. Headache and the greater occipital nerve. Clin Neurol Neurosurg. 1992; 94(4): 297–301. [DOI] [PubMed] [Google Scholar]
- Goicochea MT, Romero C, Leston JA. . Occipital neuralgia with cervical myelitis. Cephalalgia. 2008; 28(5): 567–8. [DOI] [PubMed] [Google Scholar]
- Jurgens TP, Muller P, Seedorf H, Regelsberger J, May A.. Occipital nerve block is effective in craniofacial neuralgias but not in idiopathic persistent facial pain. J Headache Pain. 2012; 13(3): 199–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin JA, Flitman SS. . Occipital nerve blocks: effect of symptomatic medication: overuse and headache type on failure rate. Headache. 2009; 49(10): 1479–85. [DOI] [PubMed] [Google Scholar]
- Naja ZM, El-Rajab M, Al-Tannir MA, Ziade FM, Tawfik OM. . Repetitive occipital nerve blockade for cervicogenic headache: expanded case report of 47 adults. Pain Pract. 2006; 6(4): 278–84. [DOI] [PubMed] [Google Scholar]
- Ambrosini A, Vandenheede M, Rossi P, Aloj F, Sauli E, Pierelli F, et al. . Suboccipital injection with a mixture of rapid- and long-acting steroids in cluster headache: a double-blind placebo-controlled study. Pain. 2005; 118(1–2): 92–6. [DOI] [PubMed] [Google Scholar]
- İNan N, İNan LE, CoŞKun Ö, TunÇ T, İLhan M.. Effectiveness of greater occipital nerve blocks in migraine prophylaxis. Nöro Psikiyatri Arşivi. 2016; 53(1): 45–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin J, Flitman S.. Occipital nerve blocks: when and what to inject? Headache. 2009; 49(10): 1521–33. [DOI] [PubMed] [Google Scholar]


