To the Editor
The use of rose bengal photodynamic antimicrobial therapy (PDAT) for the treatment of infectious keratitis in humans was introduced by Amescua et al. in 2017 with a successful clinical case.1 Our research team has demonstrated the in vitro antimicrobial efficacy of rose bengal PDAT against multiple species of bacteria and fungi.2, 3 Recently, we had the opportunity to review clinical photographs, anterior segment optical coherence tomography (AS-OCT) and histopathology of a case previously reported in 2017 in Cornea.1
In short, the case detailed a 56-year-old female patient with history of penetrating keratoplasty due to keratoconus, who presented with corneal infection secondary to Fusarium keratoplasticum, unresponsive to standard medical treatment. It is of note that this patient never underwent riboflavin crosslinking to treat her keratoconus. The patient underwent two 0.1% rose bengal PDAT sessions for a total radiant exposure of 2.7 J/cm2 without complications. Complete clinical resolution was evident five weeks after the first treatment.1 She underwent optical corneal transplant 16 months after rose bengal PDAT and on the last follow up, the corneal graft remained clear and the patient has a BCVA of 20/30.
Prior to rose bengal PDAT, there was no evidence of a demarcation line observed on slit-lamp examination. However, at the 1-, 3-, 8- and 16-month follow-ups, a demarcation line in the anterior stroma was identified (Figure 1). At Day 19 post rose bengal PDAT, the AS-OCT showed corneal swelling (976 +/− 21 μm) but no demarcation line. However, after 8 months there was a clear demarcation line and the corneal thickness was 578 +/− 5.5 μm. The demarcation line persisted at 16 months post-treatment with a stable corneal thickness of 592 +/−8.3 μm. The demarcation line was evident under slit-lamp examination and estimated at a depth of 220 μm using Image J software on slit-lamp photographs and at 212 μm using the AS-OCT digital caliper. No demarcation line was seen on the contralateral healthy eye at any exam days (Figure 2).
Figure 1.
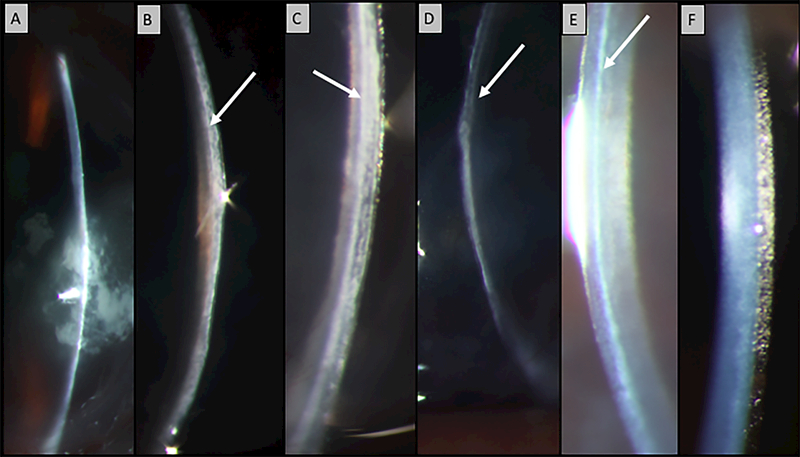
Narrow slit beam photographs. A: Pre-treatment shows a central corneal ulcer but no demarcation line on the clear corneal zone. B-E: Shows a demarcation line (arrow) in the anterior corneal stroma post rose bengal PDAT (B: Month 1, C: Month 3, D: Month 8, E: Month 16). F: Contralateral healthy eye shows no demarcation line.
Figure 2.
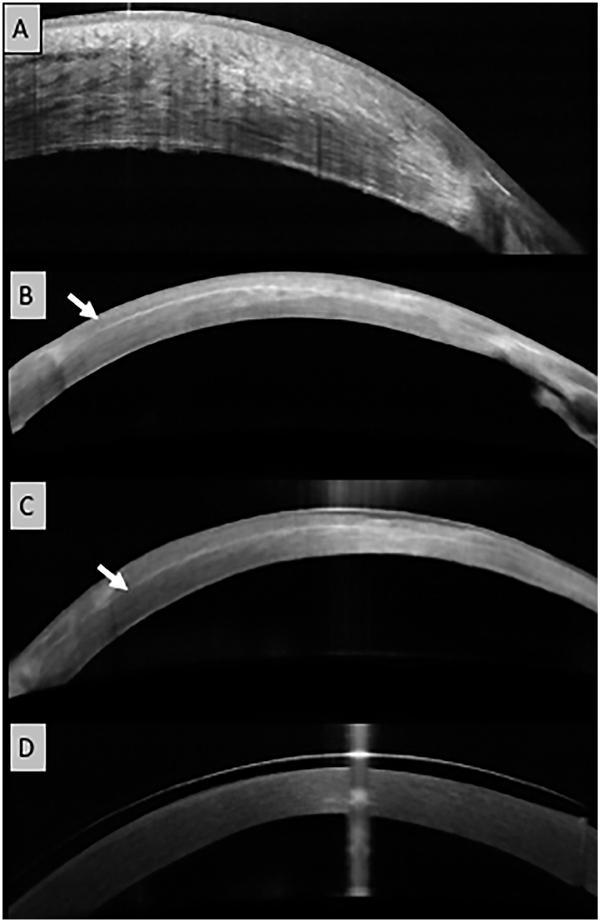
Anterior Segment OCT findings. A. Image taken 19 days after rose bengal PDAT shows an increased central corneal thickness but no demarcation line. B-C, showing a demarcation line (arrow) at anterior corneal stroma after rose bengal PDAT with a regular corneal surface (B: Month 8, C: Month 16). D: Contralateral healthy eye shows no demarcation line.
Hematoxylin and eosin (H&E) and Periodic acid–Schiff (PAS) stained slides revealed a demarcation within the anterior stroma that was present centrally at a depth of ~220 μm, with fibrosis present in the anterior third of corneal stroma. There was no corneal epithelial defect, vascularization was present at the deep margin of the aforementioned fibrosis, and the keratocytes appeared unremarkable throughout the posterior stroma. Alpha smooth muscle stain (Novocastra Laboratories Inc., Burlingame, California, USA) for myofibroblast was negative within the stroma and highlighted intrastromal vascularization (Figure 3).
Figure 3.
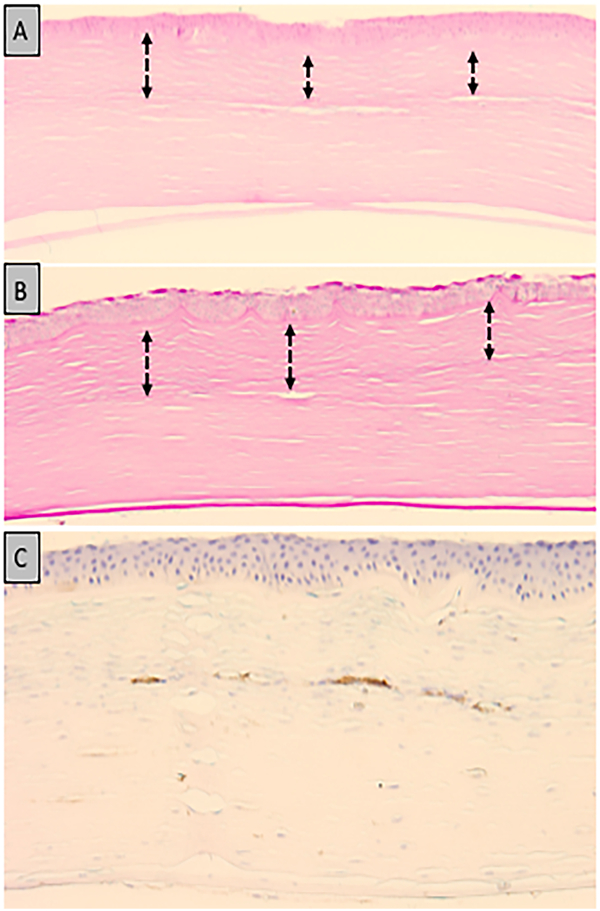
Photomicrograph of human cornea 16 months after rose bengal PDAT for Fusarium keratitis. Anterior stromal scarring (double arrow) with disorganization of the collagen bundles present to a depth of 220 μm. (A: Hematoxylin and eosin; original magnification × 200) (B: Periodic acid–Schiff ; original magnification × 200) C: Negative alpha-smooth muscle actin staining within the stromal cells and focal positivity within blood vessels.
Although other groups have examined in vitro and in vivo corneal changes that occur after rose bengal CXL, to the best of our knowledge, no studies have reported human corneal changes after rose bengal PDAT. Contrary to our findings, Gallego-Muñoz et al. did not observe a demarcation line in ex vivo rabbit corneas post-rose bengal CXL.4 Cherfan et al. reported a penetration depth of rose bengal approximately 100 μm into the corneal stroma and a stromal stiffening of 3.8x in ex vivo rabbit corneas when 150 J/cm2 of green light was applied.5 Zhu et al. found that after one day of rose bengal CXL treatment in rabbits, there was a decrease in keratocytes up to 125 μm in the anterior stroma, with complete regeneration after 28 days.6
The limited diffusion of rose bengal in the cornea reported in the literature cannot be assumed in a corneal infection setting where collagenase destroys the uniformity of the collagen bundles, potentially allowing rose bengal to penetrate deeper into the stroma, and thus, treat deeper corneal infections.
In this study, the anterior stromal changes in a human cornea after rose bengal PDAT for infectious keratitis were detected with slit lamp and AS-OCT in vivo. We were also able to compare the histopathology findings with in vivo imaging techniques, which provided a more comprehensive understanding of the tissue changes occurring after rose bengal PDAT. Furthermore, the corneal stromal demarcation line observed could indicate the location of tissue changes that occur after rose bengal PDAT. Understanding the depth of rose bengal PDAT effect would allow for better treatment guidance for progressive infectious keratitis.
Acknowledgments
Financial disclosures: This research was supported by the Edward D. and Janet K. Robson Foundation (Tulsa, OK, USA), the Florida Lions Eye Bank and the Beauty of Sight Foundation (Miami, FL, USA), Drs. K. R. Olsen and M. E. Hildebrandt, Drs. Raksha Urs and Aaron Hurtado, NIH Center Grant P30EY14801, Research to Prevent Blindness, the Pan-American Association of Ophthalmology (PAAO) and Retina Research Foundation (J. D. Martinez) and the Henri and Flore Lesieur Foundation (Chicago, IL, USA) (J.-M. Parel).
Footnotes
conflicts of interest: The authors have no conflict of interest.
References
- 1.Amescua G, Arboleda A, Nikpoor N, et al. Rose Bengal Photodynamic Antimicrobial Therapy: A Novel Treatment for Resistant Fusarium Keratitis. Cornea. 2017;36:1141–1144. doi: 10.1097/ICO.0000000000001265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arboleda A, Miller D, Cabot F, et al. Assessment of rose bengal versus riboflavin photodynamic therapy for inhibition of fungal keratitis isolates. Am J Ophthalmol. 2014;158:64–70. doi: 10.1016/j.ajo.2014.04.007. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halili F, Arboleda A, Durkee H, et al. Rose Bengal- and Riboflavin-Mediated Photodynamic Therapy to Inhibit Methicillin-Resistant Staphylococcus aureus Keratitis Isolates. Am J Ophthalmol. 2016;166:194–202. doi: 10.1016/j.ajo.2016.03.014. [DOI] [PubMed] [Google Scholar]
- 4.Gallego-Munoz P, Ibares-Frias L, Lorenzo E, et al. Corneal Wound Repair After Rose Bengal and Green Light Crosslinking: Clinical and Histologic Study. Invest Ophthalmol Vis Sci. 2017;58:3471–3480. doi: 10.1167/iovs.16-21365. [DOI] [PubMed] [Google Scholar]
- 5.Cherfan D, Verter EE, Melki S, et al. Collagen cross-linking using rose bengal and green light to increase corneal stiffness. Invest Ophthalmol Vis Sci. 2013;54:3426–33. doi: 10.1167/iovs.12-11509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu H, Alt C, Webb RH, Melki S, Kochevar IE. Corneal Crosslinking With Rose Bengal and Green Light: Efficacy and Safety Evaluation. Cornea. 2016;35:1234–41. doi: 10.1097/ICO.0000000000000916. [DOI] [PubMed] [Google Scholar]


