Abstract
Men who have sex with men (MSM) may prioritize interpersonal and structural factors, such as LGBTQ-related inequalities, housing instability, financial insecurity, and relationship seeking, over HIV prevention. The aim of this study was to assess how MSM prioritize HIV relative to other factors and the association between HIV prioritization, HIV testing and sexual risk behavior, and perceived risk. Data were collected from a national online survey of MSM in the United States assessing HIV knowledge and prioritization. Participants ranked HIV prevention relative to LGBTQ-related concerns and life issues (e.g., housing, job, relationship). Adjusted regression models were conducted to assess the association of HIV prioritization with HIV testing and condomless anal sex (CAS) and to evaluate associations between perceived risk and HIV risk behavior. Among 516 participants, HIV prevention was ranked significantly higher among MSM reporting recent CAS (p = .04) and HIV testing within the past (p = .02); HIV prevention was prioritized higher relative to life issues among MSM reporting last HIV test more than 1 year ago (p = .02). Perceived HIV risk was significantly associated with higher HIV prioritization relative to LGBTQ concerns (p = .001) and life issues (p = .001). Higher HIV perceived risk was associated with lower odds of any CAS (p < .001) and higher odds of having an HIV test in the past year (p < .001). In this online study, HIV prioritization was identified as differentially associated with HIV testing, sexual risk behavior, and perceived HIV risk. HIV prevention programs should integrate strategies to address social and structural inequalities based on priority needs of MSM.
Keywords: gay health issues, gender issues and sexual orientation, public health, health-care issues, HIV/AIDS, physiological and endocrine disorders, quantitative research, research
Overall rates of new HIV diagnoses have been declining over the last decade in the United States, but incident diagnoses among men who have sex with men (MSM) have remained relatively unchanged, primarily driven by increases among young and racial/ethnic minority men (Hall et al., 2017; Centers for Disease Control and Prevention [CDC], 2015). Of the nearly 40,000 new HIV diagnoses in the United States, over two-thirds are among MSM (CDC, 2015). Data from multiple studies indicate that inconsistent condom use during anal sex may be increasing among MSM, including condomless anal sex (CAS) with HIV serodiscordant or unknown status partners (CDC, 2013; Paz-Bailey et al., 2016; Smith, Herbst, Zhang, & Rose, 2015). Despite efforts to increase routine HIV testing among MSM (Linley et al., 2016), 34% of MSM living with HIV do not know their status (CDC, 2016a), and annual routine HIV testing remains below CDC recommendations among all MSM and even lower among young MSM in particular (Branson et al., 2006; CDC, 2013; Scott, Fuqua, & Raymond, 2014; Stein et al., 2017).
Perception of HIV risk has been identified as one factor associated with sexual and HIV testing behavior among MSM. Underestimation of HIV risk has been reported as a significant predictor of both CAS and underutilization of HIV testing (Golub & Gamarel, 2013; Stephenson, White, Darbes, Hoff, & Sullivan, 2015; White & Stephenson, 2016). HIV risk perception, particularly among young MSM, may be declining, partly due to “treatment optimism,” the awareness that antiretroviral treatments are highly effective in reducing HIV viremia (Huebner, Rebchook, & Kegeles, 2004), along with the introduction of pre-exposure prophylaxis (PrEP), the use of antiretroviral medications among HIV to lower risk of HIV infection (Chen, 2013; Kalichman et al., 2017). Studies have identified increases in condomless sex and higher rates of sexually transmitted infection among PrEP users, suggesting a potential association between prevention optimism and risk compensation related to PrEP (Holt & Murphy, 2017; Traeger et al., 2018). In a recent study of sexually active MSM, one-third reported zero perceived risk of HIV, including nearly a quarter of men not in stable monogamous partnerships, and over half reported high confidence in remaining HIV uninfected (Stephenson et al., 2015). Other studies have reported similar perceived HIV risk among MSM reporting CAS, multiple partners, and low rates of HIV testing (Klein & Tilley, 2012; MacKellar et al., 2007; Mayer et al., 2012).
While HIV prevention remains a top public health focus (Fisher et al., 2017; “Winnable Battles,” 2016), MSM may not identify HIV prevention as a high priority compared to competing concerns. Sexual minority populations face unique LGBTQ-related interpersonal and structural challenges, such as discrimination, stigma, harassment, bullying, and violence (“Hate violence against lesbian,” 2009; Herek, 2009; Jeffries et al., 2017; Kosciw, Greytak, Bartkiewicz, Boesen, & Palmer, 2012). Several surveys of sexual minority priorities, including gay and bisexual men, have reported HIV prevention and care ranked below other concerns, including workplace equality, anti-LGBTQ discrimination, LGBTQ bullying and harassment, transgender rights, and marriage equality (“10th Annual LGBT Community Survey – 2016,” 2016; Cahill & Bryan, 2006; Egan, Edelman, & Sherrill, 2008; Hamel et al., 2014). MSM are disproportionately impacted by poverty, housing instability and job insecurity, and other structural inequalities (Badgett, Durso, & Schneebaum, 2013; Corliss, Goodenow, Nichols, & Austin, 2011; Movement Advancement Project, 2014). These competing priorities, coupled with lower perceived HIV risk, may influence sexual risk and HIV testing behavior. Understanding how MSM perceive HIV risk and prioritize HIV prevention relative to other concerns in their lives is important for designing targeted prevention strategies, including how HIV prevention models can best address the complexity of priorities. Thus, the aim of the present study is to assess how HIV prevention is prioritized compared to other life issues and the relationship of perceived HIV risk and sexual risk and testing behavior among an online sample of MSM in the United States.
Methods
Study Population
The Prioritizing U survey was conducted in August and September 2015 to collect cross-sectional self-reported data on HIV knowledge, prevention, and priorities among MSM in the United States. The survey and data collection methods have been previously described (Sharma, Sullivan, & Stephenson, 2017). Study participants were recruited through convenience sampling methods using online banner advertisements posted on social media sites targeting user profiles matching the study eligibility criteria. Men were eligible for the survey if they reported being 18 years of age or older, identified as male, resided in the United States, and reported sex with a man in the past 6 months. Men who clicked on the internet link were directed to an introductory page and given a brief screening questionnaire. Participants who completed the consent page and were eligible to participate completed a self-administered, confidential online survey. In total, 2,241 men were screened eligible and completed the survey. The study was approved by the University of Michigan Institutional Review Board. No monetary incentives were provided to participants.
The survey included questions on demographics (e.g., age, race, geographic location, education, and employment), sexual behavior with male and female partners in the past 3 months, HIV testing history and HIV infection status, and concern about contracting HIV collected on a scale of 0 (representing the least amount of concern) to 10 (representing the greatest amount of concern). In addition, participants were asked 11 questions about how they prioritized HIV relative to other issues (Table 1), including the importance of remaining HIV negative in comparison to life issues (paying mortgage/rent, affording food, having a good job, finding a romantic partner) and importance of preventing HIV in comparison to addressing specific concerns faced by the LGBTQ community (ending LGBTQ employment/workplace discrimination, reducing LGBTQ homelessness, improving trans-related health care, enhancing rights of undocumented LGBTQ immigrants, improving LGBTQ imprisonment/detention standards, reducing violence against transgender people, helping to stop bullying of LGBTQ youth). Response options for these questions were presented on a scale of 0 to 10, with 0 representing HIV as the least amount of importance and 10 representing HIV as the greatest amount of importance.
Table 1.
Priority Questionnaire Items and Corresponding Factor Loadings From the Rotated Factor Pattern Matrix and Factor Structure Matrix.
| Factor pattern | Factor structure | |||
|---|---|---|---|---|
| 1 | 2 | 1 | 2 | Questionnaire item |
| Factor 1: LGBTQ concerns | How important is preventing HIV in comparison to… | |||
| 75 | 8 | 78 | 44 | ending LGBTQ employment/workplace discrimination for the LGBTQ community? |
| 79 | 9 | 83 | 46 | reducing LGBTQ homelessness for the LGBTQ community? |
| 88 | −3 | 87 | 39 | improving trans-related health care for the LGBTQ community? |
| 76 | 1 | 77 | 37 | enhancing the rights of undocumented LGBTQ immigrants for the LGBTQ community? |
| 84 | −4 | 83 | 36 | improving LGBTQ imprisonment and detention standards for the LGBTQ community? |
| 83 | −1 | 83 | 39 | reducing violence against trans people for the LGBTQ community? |
| 75 | 7 | 78 | 42 | helping to stop the bullying of LGBTQ youth for the LGBTQ community? |
| Factor 2: Life issues | How important is remaining HIV negative in comparison with… | |||
| 0 | 91 | 43 | 91 | being able to pay your rent/mortgage? |
| 0 | 89 | 42 | 88 | being able to afford food? |
| 2 | 84 | 42 | 85 | having a good job? |
| 8 | 60 | 37 | 64 | find a romantic/sexual partner? |
Statistical Analysis
For this analysis, participants who self-reported their HIV status as negative or unknown, had at least one male partner in the past 3 months, and answered HIV prioritization questions were included. The analysis excluded 80 participants that did not provide their actual age (the screening questionnaire only confirmed age ≥18 years old). Participants were identified as HIV negative if they self-reported a negative HIV status and had tested for HIV in the past 3 years, and of unknown HIV status if they self-reported not knowing their HIV status or not having an HIV test in the past 3 years. CAS was defined as any insertive or receptive anal sex with a male partner in the previous 3 months, and a primary male partner was defined as a person the respondent was committed to above all others, such as a boyfriend, partner, spouse, husband, or significant other. Perceived risk was defined by the survey question asking participants to rank their concern about contracting HIV, with a higher ranking indicating a higher perceived risk. To assess differences in HIV prioritization and perceptions by age, three categories of age groups were defined (18–29, 30–49, and 50 years or older).
Participants’ characteristics were compared using descriptive statistics, including chi-square (χ2) for categorical variables and t-tests for continuous variables. Medians with interquartile ranges (IQR) and means ± standard deviations were calculated for HIV perceived risk and each of the 11 HIV prioritization questions, and differences in perceived risk and prioritization by age group were assessed using the Kruskal–Wallis one-way analysis of variance. Exploratory factor analysis was performed to reduce the 11 HIV prioritization questions using squared multiple correlations as prior communality estimates. The maximum likelihood method was used to extract factors, followed by a promax rotation to account for correlation between factors. A scree test followed by a test for the proportion of common variance indicated that two meaningful factors be retained for rotation. In interpreting the rotated factor pattern, an item was said to load on a given factor if the factor loading was 0.40 or greater for that factor and less than 0.40 for the other factor. Applying these criteria, seven items were found to load on the first factor, which was subsequently labeled “LGBTQ concerns,” and four items were loaded on the second factor, labeled “Life issues” (Table 1). Optimally-weighted linear composites for each factor as standardized estimates of factor scores were used for subsequent analyses. Multiple logistic regression models stratified by age category and adjusted for race were used to assess associations between the two factors (life issues and LGBTQ concerns) and four outcomes: any CAS in the past 3 months, CAS with a non-primary male partner and/or multiple male partners in the past 3 months, not having an HIV test in the past year, and unknown HIV status.
Correlation between HIV perceived risk and HIV prioritization was assessed using Spearman’s rank-order correlation and associations between perceived risk and prioritization were compared using multiple linear regressions, adjusted for age and race. Finally, multiple logistic regression models were used, adjusted for age, race, LGBTQ concerns, and life issues to evaluate associations between perceived risk and three behavioral outcomes: any CAS in the past 3 months, CAS with a non-primary male partner and/or multiple male partners in the past 3 months, and not having an HIV test in the past year. All statistical analyses were conducted using SAS v.9.3 (Cary, N.C.).
Results
Of 2,241 eligible participants, 2,012 (93.1%) reported being HIV negative or unknown status, of which 970 (48.2%) reported having at least one male anal sex partner in the previous 3 months. Among those, 516 (53.2%) responded to the HIV priority questions and were retained for this analysis. Most participants were White (410/516, 79.5%), college-educated (300/516, 58.1%), and employed full-time (389/516, 75.4%; Table 2). The median age was 47 years (interquartile range, IQR, 28–54 years), with over a quarter (146/516, 28.3%) between 18 and 29 years old. Less than 2% (10/516) reported current PrEP use for HIV prevention.
Table 2.
Characteristics of Study Population by Age Group.
| N (%) | ||||
|---|---|---|---|---|
| 18–29 | 30–49 | 50+ | Total | |
| Race | ||||
| Black/African American | 5 (3.4) | 5 (3.6) | 2 (0.9) | 12 (2.3) |
| Hispanic/Latino | 25 (17.1) | 30 (21.7) | 11 (4.7) | 66 (12.8) |
| White | 102 (69.9) | 95 (68.8) | 213 (91.8) | 410 (79.5) |
| Other/multiple | 14 (9.6) | 8 (5.8) | 6 (2.6) | 28 (5.4) |
| Geographic region | ||||
| Midwest | 39 (26.7) | 31 (22.5) | 59 (25.4) | 129 (25.0) |
| Northeast | 29 (19.9) | 20 (14.5) | 41 (17.7) | 90 (17.4) |
| South | 46 (31.5) | 51 (37.0) | 92 (39.7) | 189 (36.6) |
| West | 30 (20.6) | 32 (23.2) | 38 (16.4) | 100 (19.4) |
| Education | ||||
| Less than high school or diploma/equivalent | 16 (11.0) | 11 (8.0) | 12 (5.2) | 39 (7.6) |
| Some college or technical degree | 64 (43.8) | 34 (24.6) | 79 (34.1) | 177 (34.3) |
| College degree or postgraduate | 66 (45.2) | 93 (67.4) | 141 (60.8) | 300 (58.1) |
| Employment | ||||
| Full-time work | 86 (58.9) | 123 (89.3) | 180 (77.6) | 389 (75.4) |
| Part-time work | 37 (25.3) | 5 (3.6) | 16 (6.9) | 58 (11.2) |
| Unemployed/disability/other | 22 (15.1) | 10 (97.3) | 36 (15.5) | 68 (13.2) |
| Number of anal sex partners, past 3 months | ||||
| 1 | 84 (57.5) | 74 (53.6) | 142 (61.2) | 300 (58.1) |
| 2–4 | 46 (31.5) | 38 (27.5) | 64 (27.6) | 148 (28.7) |
| 5+ | 16 (11.0) | 26 (18.8) | 26 (11.2) | 68 (13.2) |
| Anal sex without condom, past 3 months | ||||
| Yes | 99 (67.8) | 105 (76.1) | 167 (72.0) | 371 (71.9) |
| No | 36 (24.7) | 25 (18.1) | 56 (24.1) | 117 (22.7) |
| More recent HIV test | ||||
| Within past year | 91 (62.3) | 80 (58.0) | 117 (50.4) | 288 (55.8) |
| >1 year ago | 26 (17.8) | 49 (35.5) | 100 (43.1) | 175 (33.9) |
| Never/Not sure when last tested | 29 (19.9) | 9 (6.5) | 15 (6.5) | 53 (10.3) |
| HIV status | ||||
| Negative | 110 (75.3) | 103 (74.6) | 174 (75.0) | 387 (75.0) |
| Don’t know/never tested | 36 (24.7) | 35 (25.4) | 58 (25.0) | 129 (25.0) |
| Total | 146 | 138 | 232 | 516 |
Less than half of participants reported sex with more than one male partner in the previous 3 months (216/516, 41.9%), with an overall average of three male sex partners in the previous 3 months (range 1–30). Most (323/516, 62.6%) reported a primary male partner, of which 99/323 (30.7%) reported anal sex with more than one male partner in the past 3 months. Nearly three-quarters (371/516, 71.9%) of all participants reported anal sex without a condom in the previous 3 months; CAS was slightly higher among men reporting more than one male sex partner in the same time period (144/216, 75%) and was significantly higher among participants reporting only one male partner and having a primary partner (193/224, 86.2%, χ2 = 26.6, p < .001). Most (463/516, 89.7%) reported ever having been tested for HIV, although over a third of those (175/463, 37.8%) reported that their last test was more than 1 year ago, and 129/516 (25%) did not know their HIV status or had never HIV tested. Participants reporting CAS with a non-primary male partner and/or multiple male sex partners in the past 3 months were significantly more likely to have been tested in the past year (χ2 = 32.0, p < .001). No significant differences in sexual risk behavior or HIV testing were identified by age category, although younger participants (age 18–29 years) reported less CAS (67.8% vs. 73.5% for participants 30 years or older, n.s.) and a higher proportion of HIV testing in the past year (62.3% vs. 53.2% for participants 30 years or older, n.s.).
HIV Prioritization
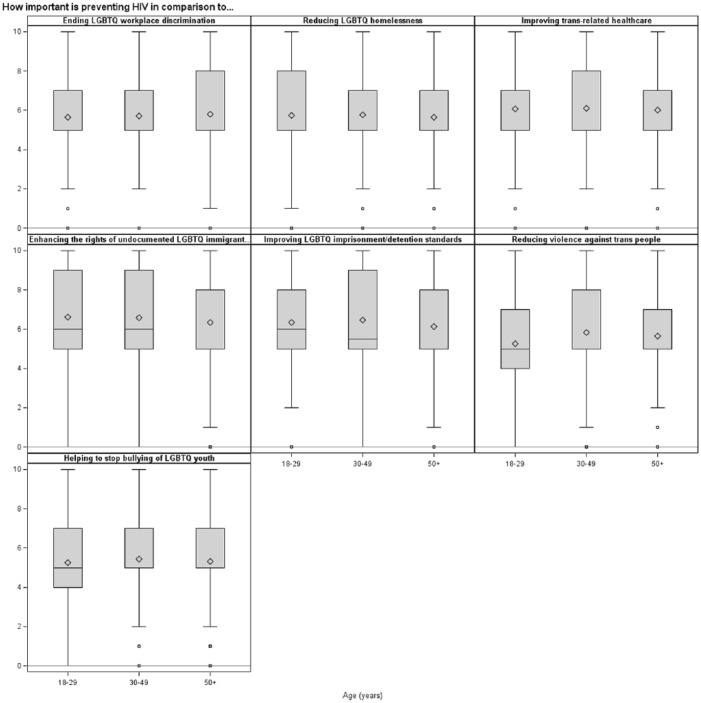
Preventing HIV and remaining HIV negative were prioritized consistently across age categories (Figure 1a and b). Overall, the median rank for HIV prioritization compared to each LGBTQ concern and life issue was approximately 5 (out of a range of 0–10), with the exception of finding a romantic/sexual partner, where remaining HIV negative was ranked higher (median 7, IQR 5–10). The two factors, LGBTQ concerns and life issues, identified through the factor analysis reduction of the 11 prioritization questions did not significantly differ by age and education, but participants reporting Hispanic ethnicity were significantly more likely to report higher HIV prioritization over LGBTQ concerns (β = 0.22, 95% CI [0.06, 0.59], p = .02) and life issues (β = 0.36, 95% CI [0.06, 0.58], p = .02) compared to non-Hispanic white participants. Among all participants, higher HIV prioritization relative to LGBTQ concerns was significantly associated with a decreased odds of any CAS in the past 3 months (adjOR 0.77, 95% [CI 0.59, 0.99], p = .04) but not associated with odds of CAS with non-primary and/or multiple male sex partners (Table 3). Higher HIV prioritization relative to LGBTQ concerns was associated with increased odds of having an HIV test in the past year (adjOR 1.32, 95% CI [1.04, 1.64], p = .02), although HIV prioritization relative to life issues was significantly associated with decreased odds of having an HIV test in the past year (adjOR 0.77, 95% CI [0.61, 0.96], p = .02). HIV prioritization was not associated with participants knowing their HIV status (negative versus unknown) or CAS with a non-primary male partner and/or multiple male sex partners in the past 3 months. In comparisons by age category, the only significant differences identified were among participants age 50 years or older: Higher HIV prioritization over LGBTQ concerns was associated with lower CAS (adjOR 0.62, 95% CI [0.41, 0.93], p = .02), and HIV prioritization over life issues was associated with lower odds of HIV testing in the past year (adjOR 0.63, 95% CI [0.61, 0.96], p = .01). Finally, HIV prioritization was not associated with CAS or HIV testing among younger participants.
Figure 1.
HIV prioritization relative to LGBTQ concerns and life issues.
Box plot distribution by age group (a) importance in preventing HIV in comparison to LGBTQ concerns and (b) importance in remaining HIV negative in comparison to life issues. Mean values denoted by diamonds and median values denoted by bars. Box includes 25th to 75th quartiles and whiskers represent range of values.
Table 3.
Recent Condomless Anal Intercourse, HIV Testing, and HIV Status by LGBTQ Concerns and Life Issues.
| HIV Prioritization Relative to LGBTQ Concerns, adjOR (95% CI)a | HIV Prioritization Relative to Life Issues, adjOR (95% CI)a | |||||||
|---|---|---|---|---|---|---|---|---|
| 18–29 years, N = 146 |
30–49 years, N = 138 |
50+ years, N = 232 |
All ages, N = 516 |
18–29 years, N = 146 |
30–49 years, N = 138 |
50+ years, N = 232 |
All ages, N = 516 |
|
| Any condomless anal intercourse, past 3 months | 0.87 [0.54, 1.39] | 0.88 [0.48, 1.62] | 0.62 [0.41, 0.93] | 0.77 [0.59, 0.99] | 0.93 [0.57, 1.51] | 0.78 [0.41, 1.47] | 1.19 [0.80, 1.77] | 1.02 [0.78, 1.33] |
| Condomless anal intercourse with non-primary and/or multiple male partners, past 3 months | 1.13 [0.74, 1.74] | 0.93 [0.58, 1.47] | 1.02 [0.71, 1.46] | 0.99 [0.78, 1.24] | 0.94 [0.61, 1.46] | 0.94 [0.57, 1.56] | 0.83 [0.59, 1.16] | 0.91 [0.72, 1.15] |
| Last HIV test >1 year ago | 0.90 [0.59, 1.37] | 0.61 [0.37, 0.99] | 0.82 [0.57, 1.16] | 0.76 [0.61, 0.96] | 1.01 [0.65, 1.56] | 1.20 [0.72, 1.99] | 1.59 [1.14, 2.24] | 1.30 [1.04, 1.64] |
| Unknown HIV status | 1.13 [0.65, 1.95] | 0.84 [0.35, 2.00] | 1.13 [0.57, 2.21] | 0.96 [0.66, 1.38] | 0.75 [0.43, 1.32] | 1.22 [0.46, 3.21] | 1.38 [0.70, 1.09] | 1.09 [0.74, 1.58] |
Note. aAdjusted for age and race.
Bolded results p < .05.
Perceived Risk of HIV
The median rank of perceived HIV risk was 7 on a scale of 0–10 (IQR 3–8). The Kruskal–Wallis test reported a significant difference in perceived HIV risk by age group (χ2 (2) = 6.77, p = .03), with highest perceived risk in the youngest age group 18–29 years (median = 7, IQR = 5–8) compared to age group 30–49 years (median = 7, IQR = 3–8) and 50 years or older (median = 6, IQR = 2–8). Perceived risk was significantly correlated with both LGBTQ concerns (ρ = 0.16, p < .001) and life issues (ρ = 0.17, p < .001). In multiple regression models, adjusted for race, an increase in perceived risk was significantly associated with an increasing HIV prioritization over both LGBTQ concerns (β = 0.05, 95% CI [0.02, 0.08], p = .001) and life issues (β = 0.06, 95% CI [0.03, 0.09], p < .001). In younger participants, aged 18–29 years, perceived risk was associated with higher HIV priority relative to life issues (β = 0.06, 95% CI [0.02, 0.10], p = .03) but not associated with higher HIV priority relative to LGBTQ concerns. The reverse was true for older participants, where perceived risk was not associated with increasing HIV priority compared to life issues but was significantly associated with increasing HIV priority over LGBTQ concerns (30–49-year-olds: β = 0.10, 95% CI [0.04, 0.15], p = .001; 50+-year-olds: β = 0.06, 95% CI [0.02, 0.10], p = .005). In multiple logistic regression models, adjusted for age, race, HIV status, life issues, and LGBTQ concerns, perceived HIV risk was significantly associated with lower odds of CAS in the past 3 months (adjOR 0.82, 95% CI [0.75, 0.89], p < .001; Table 4) but a higher odds of CAS with a non-primary male partner and/or multiple male sex partners in the past 3 months (adjOR 1.12, 95% CI [1.05, 1.20], p < .001). The odds of having an HIV test in the past year significantly increased with higher perceived HIV risk (adjOR 1.16, 95% [1.08, 1.24], p < .001). These findings were consistent across all age groups.
Table 4.
Perceived HIV Risk by Condomless Anal Intercourse and HIV Testing.
| Perceived HIV Risk, adjOR (95% CI)a | ||||
|---|---|---|---|---|
| 18–29 years | 30–49 years | 50+ years | All ages | |
| Any condomless anal intercourse, past 3 months | 0.81 [0.68, 0.97] | 0.81 [0.67, 0.98] | 0.84 [0.74, 0.94] | 0.82 [0.75, 0.89] |
| Condomless anal intercourse with non-primary and/or multiple male partners, past 3 months | 1.18 [1.02, 1.37] | 1.09 [0.96, 1.25] | 1.14 [1.03, 1.26] | 1.12 [1.05, 1.20] |
| Last HIV test >1 year ago | 0.87 [0.74, 1.03] | 0.91 [0.80, 1.03] | 0.84 [0.76, 0.92] | 0.86 [0.81, 0.92] |
Note. aAdjusted for LGBTQ concerns, life issues, age, race, and HIV status (negative or unknown).
Bolded results p < .05.
Discussion
In this online survey of U.S. MSM, HIV prevention was generally not found to be prioritized over other factors, such as LGBTQ concerns and life issues. Among all prioritization questions in the survey, most MSM did not report remaining HIV negative or HIV prevention at the top or the bottom of the scales, suggesting a generally similar relevance to LGBT-specific concerns and other life issues. Participants in the study who ranked HIV prevention as a higher priority relative to LGBTQ issues were less likely to have engaged in recent CAS and were more likely to have had a recent HIV test. Higher HIV prevention prioritization may reflect MSM that receive regular HIV testing and do not engage in higher risk sexual behavior, and yet are highly concerned about preventing HIV in their communities in addition to concern over their own HIV risk. Participants who ranked HIV prevention a higher priority relative to life issues were less likely to have had a recent HIV test, and no significant association was found for participants reporting higher sexual risk behavior. This finding suggests the possibility that participants that prioritized HIV prevention over life issues may be at lower risk and do not test as frequently, or MSM with more frequent HIV testing were less likely to be negatively impacted by life issues, such as economic security and housing stability.
MSM in this study were significantly more likely to prioritize HIV prevention over LGBTQ concerns and life issues if they perceived themselves to be at higher risk for HIV infection. HIV prevention is one of a number of concerns experienced by MSM. Many MSM are confronted by daily realities of discrimination, homophobia, social isolation, and potential violence, identified as high priority issues in sexual minority communities (“10th Annual LGBT Community Survey – 2016,” 2016; Cahill & Bryan, 2006). Negative interpersonal and contextual experiences of MSM have been identified in other studies to be associated with increased HIV acquisition risk (Frye et al., 2015; Jeffries, Marks, Lauby, Murrill, & Millett, 2013; Mansergh et al., 2015), and structuralized stigma may also create barriers to increasing utilization of HIV prevention services (Oldenburg et al., 2015). Structural inequalities that disproportionately impact sexual minority populations, including poverty, homelessness, and inadequate employment, have also been found to be directly linked to sexual risk behavior (Forsyth & Valdiserri, 2015; Mena, Crosby, & Geter, 2016; Nelson et al., 2016; Whittle et al., 2015). The syndemic impact of structural inequality, marginalization, and violence experienced by MSM has been identified as a potential cause for the continued high risk for HIV acquisition among MSM, particularly young and racial/ethnic minority MSM (Mustanski et al., 2017; Wilson et al., 2014). The findings from the present study suggest that MSM may have concerns beyond HIV prevention that may be associated with HIV risk and also may prevent seeking out HIV prevention services.
Several studies have concluded a need to incorporate methods for addressing interpersonal and structural factors in HIV prevention strategies, as well as through policies aimed at increasing protections for sexual minority populations (Nelson et al., 2016; Oldenburg et al., 2015; Whittle et al., 2015). The National Institute of Minority Health and Health Disparities has identified developing tailored interventions for diverse populations that incorporate relevant sexual minority content and experiences as priority research needs in HIV prevention (Rhodes & Wong, 2016). Individual- and community-level HIV prevention efforts need to do more to integrate the interpersonal and structural factors that contribute to increased HIV risk. With the exception of HIV and sexually transmitted infection research, there is an inadequate number of studies addressing priority issues of sexual minorities (Boehmer, 2002). There is a need to identify the health and social priorities of MSM in the development of comprehensive prevention programs that incorporate the interpersonal (i.e., discrimination) and structural issues (i.e., housing) associated with HIV risk.
Participants reporting high-risk sexual behavior (e.g., CAS with a non-primary male partner and/or multiple male sex partners) were more likely to perceive a higher HIV risk and to have been tested for HIV within the past year. MSM with a higher perceived risk may prioritize HIV prevention, as demonstrated in this study, and, thus, may be more likely to seek prevention services and testing. Perceived risk may not directly translate into decreased sexual risk behavior, just as getting HIV tested does not necessarily translate into behavior change if the test result is negative. Studies have found mixed associations between perceived HIV risk and actual risk behavior (Adams, Stuewig, Tangney, & Kashdan, 2014; Downing, 2014; Goedel, Halkitis, & Duncan, 2016; Klein & Tilley, 2012; Lacefield, Negy, Schrader, & Kuhlman, 2015; MacKellar et al., 2007), possibly a result of differences in study populations or the result of complex factors associated with behavior. The results from this study identify that perceived risk was associated with an increase in CAS with a non-primary partner or multiple partners that is consistent with previous studies that indicate perceived risk may be defined by type and serostatus of sexual partners (Kesler et al., 2016; MacKellar et al., 2005; Stephenson et al., 2015).
The increase in biobehavioral interventions for HIV prevention, including PrEP, has been cited as an explanation for changes in perceived HIV risk reflected in sexual behavior (Tully, Cojocaru, & Bauch, 2015; Zimmerman & Kirschbaum, 2017). Kalichman et al. (2017) found a trend of increasing sexual risk behavior since the introduction of antiretrovirals as an HIV prevention strategy, and the CDC noted a sharp increase in sexually transmitted infections after the introduction of PrEP (Prevention, 2016b). A recent systematic review identified increases in sexually transmitted infections and condomless sex in studies of PrEP users (Traeger et al., 2018). Other studies suggest that sexual risk behavior is associated with perceived partner status, and the relationship between perceived and actual risk may also be closely mediated by individual factors, such as serosorting and HIV knowledge (Cox, Beauchemin, & Allard, 2004; Sharma et al., 2017). In a previous analysis using data from this survey, Sullivan and Stephenson found that MSM perceiving a lower local community HIV prevalence were more likely to engage in higher risk sexual behavior and less likely to have a recent HIV test (Sullivan & Stephenson, 2017). Perception of HIV risk, and whether or not that contributes to actual risk, varies by population and may be the result of HIV prevention and testing campaigns and interventions that may not adequately target higher risk populations (Albarracin et al., 2005; Drumhiller et al., 2017). Strategies to improve HIV prevention messaging should be considered for increasing knowledge and appropriate perception of individual HIV risk.
Limitations are noted for this study. First, the study population consisted of a convenience sample of online participants that were primarily White, older, and more likely to have a college education. Thus, the data were significantly underrepresented by the highest HIV risk population: younger and racial/ethnic minority MSM. However, HIV prevention prioritization and risk perceptions were compared by age group and substantially meaningful differences were not identified. Study recruitment was conducted through online banner advertisements which potentially limited sampling of populations not active on social media. Second, due to small sample sizes, no assessment of differences by race/ethnicity were possible that would have been particularly useful given that sexual risk behavior, life experiences, and perceptions of HIV risk may substantially differ by race/ethnicity. Finally, although we attempted to formulate an exhaustive list of questions assessing HIV prioritization relative to potential issues faced by the LGBTQ community, we acknowledge that this question set might not be complete.
HIV prevention does not exist in a vacuum in the lives of MSM, and the interpersonal and structural experiences of MSM should be considered as part of a holistic strategy for HIV prevention. The current HIV trends among U.S. MSM are likely the result of an ongoing syndemic of social discrimination, behavioral disinhibition, and economic disenfranchisement, and future research needs to focus on the development of prevention programs that tackle social and structural inequalities as pathways to shaping and changing HIV risk. Additional research is needed to better understand the role of perceived HIV risk in sexual behavior and how perceptions and behavior are shaped by comprehensive HIV prevention messaging across diverse populations of MSM.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Erin M. Kahle  https://orcid.org/0000-0001-6060-9852
https://orcid.org/0000-0001-6060-9852
Akshay Sharma  https://orcid.org/0000-0001-7864-5464
https://orcid.org/0000-0001-7864-5464
References
- 10th Annual LGBT Community Survey - 2016. (2016). Retrieved from Washington, DC: http://thedccenter.org/wp-content/uploads/2017/04/2016LGBTQCommunitySUrvey.pdf [Google Scholar]
- Adams L. M., Stuewig J. B., Tangney J. P., Kashdan T. B. (2014). Perceived susceptibility to AIDS predicts subsequent HIV risk: A longitudinal evaluation of jail inmates. Journal of Behavioral Medicine, 37(3), 511–523. doi: 10.1007/s10865-013-9507-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracin D., Gillette J. C., Earl A. N., Glasman L. R., Durantini M. R., Ho M. H. (2005). A test of major assumptions about behavior change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychology Bulletin, 131(6), 856–897. doi: 10.1037/0033-2909.131.6.856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badgett M. V. L., Durso L. E., Schneebaum A. (2013). New patterns of poverty in the lesbian, gay, and bisexual community. Los Angeles, CA: The Williams Institute; Retrieved from https://williamsinstitute.law.ucla.edu/wp-content/uploads/LGB-Poverty-Update-Jun-2013.pdf [Google Scholar]
- Boehmer U. (2002). Twenty years of public health research: Inclusion of lesbian, gay, bisexual, and transgender populations. American Journal of Public Health, 92(7), 1125–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branson B. M., Handsfield H. H., Lampe M. A., Janssen R. S., Taylor A. W., Lyss S. B., … Prevention. (2006). Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. Morbidity and Mortality Weekly Report Recommendations and Reports, 55(RR-14), 1–17; quiz CE11-14. [PubMed] [Google Scholar]
- Cahill S., Bryan K. B. (2006). Policy priorities for the LGBT community: Pride survey 2006. Retrieved from http://www.thetaskforce.org/static_html/downloads/reports/reports/2006PrideSurvey.pdf
- Centers for Disease Control & Prevention. (2013). HIV testing and risk behaviors among gay, bisexual, and other men who have sex with men - United States. Morbidity and Mortality Weekly Report, 62(47), 958–962. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2015). HIV surveillance report, 2015. Retrieved from http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- Centers for Disease Control and Prevention. (2016. a). CDC fact sheet: HIV testing in the United States. Retrieved from https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/hiv-testing-us-508.pdf
- Centers for Disease Control and Prevention. (2016. b). Sexually transmitted disease surveillance 2015. Retrieved from https://www.cdc.gov/std/stats15/STD-Surveillance-2015-print.pdf
- Chen Y. (2013). Treatment-related optimistic beliefs and risk of HIV transmission: A review of recent findings (2009–2012) in an era of treatment as prevention. Current HIV/AIDS Report, 10(1), 79–88. doi: 10.1007/s11904-012-0144-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corliss H. L., Goodenow C. S., Nichols L., Austin S. B. (2011). High burden of homelessness among sexual-minority adolescents: Findings from a representative Massachusetts high school sample. American Journal of Public Health, 101(9), 1683–1689. doi: 10.2105/AJPH.2011.300155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox J., Beauchemin J., Allard R. (2004). HIV status of sexual partners is more important than antiretroviral treatment related perceptions for risk taking by HIV positive MSM in Montreal, Canada. Sexually Transmitted Infections, 80(6), 518–523. doi: 10.1136/sti.2004.011288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downing M. J. (2014). Perceived likelihood of HIV and sexually transmitted infection acquisition among men who have sex with men. Journal of the Association of Nurses in AIDS Care, 25(1), 98–102. doi: 10.1016/j.jana.2013.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drumhiller K., Murray A., Gaul Z., Aholou T. M., Sutton M. Y., Nanin J. (2017). “We deserve better!”: Perceptions of HIV testing campaigns among Black and Latino MSM in New York City. Archives of Sexual Behavior, 47(1), 289–297. doi: 10.1007/s10508-017-0950-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan P. J., Edelman M. S., Sherrill K. (2008). Findings from the Hunter College poll of lesbians, gays, and bisexuals: New discoveries about identity, political attitudes, and civic engagement. New York, NY: Hunter College, City University of New York. [Google Scholar]
- Fisher H. H., Essuon A., Hoyte T., Shapatava E., Shelley G., Rios A., … Sapiano T. (2017). The changing landscape of HIV prevention in the United States: Health department experiences and local adaptations in response to the national HIV/AIDS strategy and high-impact prevention approach. Journal of Public Health Management and Practice, 24(3), 225–234. doi: 10.1097/PHH.0000000000000575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsyth A. D., Valdiserri R. O. (2015). A state-level analysis of social and structural factors and HIV outcomes among men who have sex with men in the United States. AIDS Education and Prevention, 27(6), 493–504. doi: 10.1521/aeap.2015.27.6.493 [DOI] [PubMed] [Google Scholar]
- Frye V., Nandi V., Egan J., Cerda M., Greene E., Van Tieu H., … Koblin B. A. (2015). Sexual orientation- and race-based discrimination and sexual HIV risk behavior among urban MSM. AIDS and Behavior, 19(2), 257–269. doi: 10.1007/s10461-014-0937-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goedel W. C., Halkitis P. N., Duncan D. T. (2016). Behavior- and partner-based HIV risk perception and sexual risk behaviors in Men who have Sex with Men (MSM) who use geosocial-networking smartphone applications in New York City. Journal of Urban Health, 93(2), 400–406. doi: 10.1007/s11524-016-0043-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub S. A., Gamarel K. E. (2013). The impact of anticipated HIV stigma on delays in HIV testing behaviors: Findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care and STDS, 27(11), 621–627. doi: 10.1089/apc.2013.0245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall H. I., Song R., Tang T., An Q., Prejean J., Dietz P., … Mermin J. (2017). HIV trends in the United States: Diagnoses and estimated incidence. Journal of Medical Internet Research Public Health and Surveillance, 3(1), e8. doi: 10.2196/publichealth.7051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamel L., Firth J., Hoff T., Kates J., Levine S., Dawson L. (2014). HIV/AIDS in the lives of gay and bisexual men in the United States. Retrieved from http://files.kff.org/attachment/survey-hivaids-in-the-lives-of-gay-and-bisexual-men-in-the-united-states
- Hate violence against lesbian, gay, bisexual, and transgender people in the United States: 2008. (2009). Retrieved from New York: https://avp.org/wp-content/uploads/2017/04/2008_NCAVP_HV_Report.pdf [Google Scholar]
- Herek G. M. (2009). Hate crimes and stigma-related experiences among sexual minority adults in the United States: Prevalence estimates from a national probability sample. Journal of Interpersonal Violence, 24(1), 54–74. doi: 10.1177/0886260508316477 [DOI] [PubMed] [Google Scholar]
- Holt M., Murphy D. A. (2017). Individual versus community-level risk compensation following preexposure prophylaxis of HIV. American Journal of Public Health, 107(10), 1568–1571. doi: 10.2105/AJPH.2017.303930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebner D. M., Rebchook G. M., Kegeles S. M. (2004). A longitudinal study of the association between treatment optimism and sexual risk behavior in young adult gay and bisexual men. JAIDS Journal of Acquired Immune Deficiency Syndromes, 37(4), 1514–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffries W. L., Gelaude D. J., Torrone E. A., Gasiorowicz M., Oster A. M., Spikes P. S., … Bertolli J. (2017). Unhealthy environments, unhealthy consequences: Experienced homonegativity and HIV infection risk among young men who have sex with men. Global Public Health, 12(1), 116–129. doi: 10.1080/17441692.2015.1062120 [DOI] [PubMed] [Google Scholar]
- Jeffries W. L., Marks G., Lauby J., Murrill C. S., Millett G. A. (2013). Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among Black men who have sex with men. AIDS and Behavior, 17(4), 1442–1453. doi: 10.1007/s10461-012-0189-y [DOI] [PubMed] [Google Scholar]
- Kalichman S. C., Price D., Eaton L. A., Burnham K., Sullivan M., Finneran S., … Allen A. (2017). Diminishing perceived threat of AIDS and increasing sexual risks of HIV among men who have sex with men, 1997–2015. Archives of Sexual Behavior, 46(4), 895–902. doi: 10.1007/s10508-016-0934-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesler M. A., Kaul R., Liu J., Loutfy M., Gesink D., Myers T., Remis R. S. (2016). Actual sexual risk and perceived risk of HIV acquisition among HIV-negative men who have sex with men in Toronto, Canada. BMC Public Health, 16, 254. doi: 10.1186/s12889-016-2859-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein H., Tilley D. L. (2012). Perceptions of HIV risk among internet-using, HIV-negative barebacking men. American Journal of Men’s Health, 6(4), 280–293. doi: 10.1177/1557988311434825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosciw J. G., Greytak E. A., Bartkiewicz M. J., Boesen M. J., Palmer N. A. (2012). The 2011 national school climate survey: The experiences of lesbian, gay, bisexual and transgender youth in our nation’s schools. Retrieved from https://www.glsen.org/sites/default/files/2011%20National%20School%20Climate%20Survey%20Full%20Report.pdf
- Lacefield K., Negy C., Schrader R. M., Kuhlman C. (2015). Comparing psychosocial correlates of condomless anal sex in HIV-diagnosed and HIV-nondiagnosed men who have sex with men: A series of meta-analyses of studies from 1993–2013. LGBT Health, 2(3), 200–220. doi: 10.1089/lgbt.2014.0069 [DOI] [PubMed] [Google Scholar]
- Linley L., An Q., Song R., Valverde E., Oster A. M., Qian X., Hernandez A. L. (2016). HIV testing experience before HIV diagnosis among men who have sex with men - 21 jurisdictions, United States, 2007–2013. Morbidity and Mortality Weekly Report, 65(37), 999–1003. doi: 10.15585/mmwr.mm6537a3 [DOI] [PubMed] [Google Scholar]
- MacKellar D. A., Valleroy L. A., Secura G. M., Behel S., Bingham T., Celentano D. D., … Young Men’s Survey Study, Group. (2005). Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: Opportunities for advancing HIV prevention in the third decade of HIV/AIDS. Journal of Acquired Immune Deficiency Syndrome, 38(5), 603–614. [DOI] [PubMed] [Google Scholar]
- MacKellar D. A., Valleroy L. A., Secura G. M., Behel S., Bingham T., Celentano D. D., … Young Men’s Survey Study, Group. (2007). Perceptions of lifetime risk and actual risk for acquiring HIV among young men who have sex with men. AIDS and Behavior, 11(2), 263–270. doi: 10.1007/s10461-006-9136-0 [DOI] [PubMed] [Google Scholar]
- Mansergh G., Spikes P., Flores S. A., Koblin B. A., McKirnan D., Hudson S. M., … Project, M. I. X. Study Group. (2015). Internalised homophobia is differentially associated with sexual risk behaviour by race/ethnicity and HIV serostatus among substance-using men who have sex with men in the United States. Sexually Transmitted Infections, 91(5), 324–328. doi: 10.1136/sextrans-2014-051827 [DOI] [PubMed] [Google Scholar]
- Mayer K. H., Ducharme R., Zaller N. D., Chan P. A., Case P., Abbott D., … Cavanaugh T. (2012). Unprotected sex, underestimated risk, undiagnosed HIV and sexually transmitted diseases among men who have sex with men accessing testing services in a New England bathhouse. JAIDS Journal of Acquired Immune Deficiency Syndromes, 59(2), 194–198. doi: 10.1097/QAI.0b013e31823bbecf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mena L., Crosby R. A., Geter A. (2016). A novel measure of poverty and its association with elevated sexual risk behavior among young Black MSM. International Journal of STDs and AIDS, 28(6), 602–607. doi: 10.1177/0956462416659420 [DOI] [PubMed] [Google Scholar]
- Movement Advancement Project. (2014). Paying an unfair price: The financial penalty for being LGBT in America. Retrieved from http://www.lgbtmap.org/file/paying-an-unfair-price-full-report.pdf
- Mustanski B., Phillips G., Ryan D. T., Swann G., Kuhns L., Garofalo R. (2017). Prospective effects of a syndemic on HIV and STI incidence and risk behaviors in a cohort of young men who have sex with men. AIDS and Behavior, 21(3), 845–857. doi: 10.1007/s10461-016-1607-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson L. E., Wilton L., Moineddin R., Zhang N., Siddiqi A., Sa T., … Team, Hptn Study. (2016). Economic, legal, and social hardships associated with HIV risk among Black men who have sex with men in Six US Cities. Journal of Urban Health, 93(1), 170–188. doi: 10.1007/s11524-015-0020-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg C. E., Perez-Brumer A. G., Hatzenbuehler M. L., Krakower D., Novak D. S., Mimiaga M. J., Mayer K. H. (2015). State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. AIDS, 29(7), 837–845. doi: 10.1097/QAD.0000000000000622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz-Bailey G., Mendoza M. C., Finlayson T., Wejnert C., Le B., Rose C., … Group, Nhbs Study. (2016). Trends in condom use among MSM in the United States: The role of antiretroviral therapy and seroadaptive strategies. AIDS, 30(12), 1985–1990. doi: 10.1097/QAD.0000000000001139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes S. D., Wong F. Y. (2016). HIV prevention among diverse young MSM: Research needs, priorities, and opportunities. AIDS Education and Prevention, 28(3), 191–201. doi: 10.1521/aeap.2016.28.3.191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott H. M., Fuqua V., Raymond H. F. (2014). Utilization of HIV prevention services across racial/ethnic groups among men who have sex with men in San Francisco, California, 2008. AIDS and Behavior, 18(Suppl 3), 316–323. doi: 10.1007/s10461-013-0526-9 [DOI] [PubMed] [Google Scholar]
- Sharma A., Sullivan S. P., Stephenson R. B. (2017). Detailed knowledge about HIV epidemiology and transmission dynamics and their associations with preventive and risk behaviors among gay, bisexual, and other men who have sex with men in the United States. Journal of Medical Internet Research Public Health and Surveillance, 3(1), e11. doi: 10.2196/publichealth [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith D. K., Herbst J. H., Zhang X., Rose C. E. (2015). Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. Journal of Acquired Immune Deficiency Syndrome, 68(3), 337–344. doi: 10.1097/QAI.0000000000000461 [DOI] [PubMed] [Google Scholar]
- Stein R., Xu S., Marano M., Williams W., Cheng Q., Eke A., … Wang G. (2017). HIV testing, linkage to HIV medical care, and interviews for partner services among women - 61 health department jurisdictions, United States, Puerto Rico, and the U.S. Virgin Islands, 2015. Morbidity and Mortality Weekly Report, 66(41), 1100–1104. doi: 10.15585/mmwr.mm6641a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R., White D., Darbes L., Hoff C., Sullivan P. (2015). HIV testing behaviors and perceptions of risk of HIV infection among MSM with main partners. AIDS and Behavior, 19(3), 553–560. doi: 10.1007/s10461-014-0862-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan S., Stephenson R. (2017). Perceived HIV prevalence accuracy and sexual risk behavior among gay, bisexual, and other men who have sex with men in the United States. AIDS and Behavior. Advance online publication. doi: 10.1007/s10461-017-1789-3 [DOI] [PubMed] [Google Scholar]
- Traeger M. W., Schroeder S. E., Wright E. J., Hellard M. E., Cornelisse V. J., Doyle J. S., Stoove M. A. (2018). Effects of pre-exposure prophylaxis for the prevention of HIV infection on sexual risk behavior in men who have sex with men: A systematic review and meta-analysis. Clinical Infectious Disease. Advance online publication. doi: 10.1093/cid/ciy182 [DOI] [PubMed] [Google Scholar]
- Tully S., Cojocaru M., Bauch C. T. (2015). Sexual behavior, risk perception, and HIV transmission can respond to HIV antiviral drugs and vaccines through multiple pathways. Scientific Reports, 5, 15411. doi: 10.1038/srep15411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White D., Stephenson R. (2016). Correlates of perceived HIV prevalence and associations with HIV testing behavior among men who have sex with men in the United States. American Journal of Men’s Health, 10(2), 90–99. doi: 10.1177/1557988314556672 [DOI] [PubMed] [Google Scholar]
- Whittle H. J., Palar K., Napoles T., Hufstedler L. L., Ching I., Hecht F. M., Weiser S. D., … (2015). Experiences with food insecurity and risky sex among low-income people living with HIV/AIDS in a resource-rich setting. Journal of the International AIDS Society, 18, 20293. doi: 10.7448/IAS.18.1.20293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson P. A., Nanin J., Amesty S., Wallace S., Cherenack E. M., Fullilove R. (2014). Using syndemic theory to understand vulnerability to HIV infection among Black and Latino men in New York City. J Urban Health, 91(5), 983–998. doi: 10.1007/s11524-014-9895-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winnable Battles, Final Report. (2016). Retrieved from Atlanta, GA: https://www.cdc.gov/winnablebattles/report/docs/winnable-battles-final-report.pdf [Google Scholar]
- Zimmerman R. S., Kirschbaum A. L. (2017). News of biomedical advances in HIV: Relationship to treatment optimism and expected risk behavior in US MSM. AIDS and Behavior, 22(2), 367–378. doi: 10.1007/s10461-017-1744-3 [DOI] [PubMed] [Google Scholar]