Abstract
Several studies have used the Edinburgh Postnatal Depression Scale (EPDS), developed to screen new mothers, also for new fathers. This study aimed to further contribute to this knowledge by comparing assessment of possible depression in fathers and associated demographic factors by the EPDS and the Gotland Male Depression Scale (GMDS), developed for “male” depression screening. The study compared EPDS score ≥10 and ≥12, corresponding to minor and major depression, respectively, in relation to GMDS score ≥13. At 3–6 months after child birth, a questionnaire was sent to 8,011 fathers of whom 3,656 (46%) responded. The detection of possibly depressed fathers by EPDS was 8.1% at score ≥12, comparable to the 8.6% detected by the GMDS. At score ≥10, the proportion detected by EPDS increased to 13.3%. Associations with possible risk factors were analyzed for fathers detected by one or both scales. A low income was associated with depression in all groups. Fathers detected by EPDS alone were at higher risk if they had three or more children, or lower education. Fathers detected by EPDS alone at score ≥10, or by both scales at EPDS score ≥12, more often were born in a foreign country. Seemingly, the EPDS and the GMDS are associated with different demographic risk factors. The EPDS score appears critical since 5% of possibly depressed fathers are excluded at EPDS cutoff 12. These results suggest that neither scale alone is sufficient for depression screening in new fathers, and that the decision of EPDS cutoff is crucial.
Keywords: depression, father, Edinburgh Postnatal Depression Scale (EPDS), Gotland Male Depression Scale (GMDS), risk factors
The period after the birth of a child may be demanding and overwhelming for parents. This can in turn lead to parental depression, which may negatively affect the child as well as the other parent (Goodman, 2004; Ramchandani, Stein, Evans, O’Connor, & ALSPAC study team, 2005; Ramchandani et al., 2008a; Ramchandani et al., 2008b; Ramchandani et al., 2011; Paulson & Bazemore, 2010). According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V; APA, 2013), perinatal depression is the concept for describing parental depression in relation to pregnancy and new parenthood, replacing older terms like antenatal and postnatal depression.
A review by Paulson and Bazemore (2010) stated an overall prevalence of 10.4% of depression among fathers and 23.8% among mothers during the first year after birth, although with a substantial variation between studies, for example, regarding EPDS score corresponding to both minor (>6) and major depression (>12). Similarly, a Swedish study by Bergström (2013) reported that 10.3% of first-time fathers had depression as indicated by EPDS score 11 or higher. Fathers have an increased risk of depression if their partners also suffer from these symptoms, as conveyed in a review by Goodman (2004) based on studies with, for example, EPDS scores corresponding to minor (10) or major (12/13) depression. A study of couples using EPDS score 9/10 reached the same conclusion (Matthey, Barnett, Kavanagh, & Howie, 2001). According to the review by Paulson and Bazemore (2010), the correlation between paternal and maternal postnatal depression is moderate as demonstrated by r = .31 (95% CI [0.23, 0.38]). Based on this knowledge, depression screening could be recommended for both parents.
A review by Edward, Castle, Mills, Davis, and Casey (2010) informs that except for maternal depression, some other risk factors for paternal depression are earlier episodes of depression, financial/life stressors, and lack of social support. Bergström (2013) demonstrated that low educational level and low income (crude odds ratios; OR), and also poor partner relationship quality and financial worry (OR adjusted for sociodemographic factors) implied a higher risk for depression. Furthermore, young paternal age was a risk factor for depression after adjustment for both sociodemographic and psychological factors (Bergström, 2013). Studies on the consequences for the child of paternal depression have used EPDS score 12 or higher, including only major depression (Ramchandani et al., 2005; Ramchandani et al., 2008a; Ramchandani et al., 2008b), but also EPDS score 10 or higher, including minor depression (Ramchandani et al., 2011).
The lower prevalence of perinatal depression in men compared to women could be due to several factors, for example, that screening instruments like the Edinburgh Postnatal Depression Scale (EPDS) are developed for mothers (Cox, Holden, & Sagovsky, 1987). The validation of EPDS by Cox et al. (1987) stated that an EPDS score of 12 or more indicates major depression, but that a score of 9 or more could be used for clinical routine screening in order to not miss out cases. Furthermore, fathers may express their depressive symptoms differently (Martin, Neighbors, & Griffith, 2013). Some literature suggests that men feel less able to cry and manifest vulnerability due to masculinity norms, and instead express externalizing depressive symptoms like anger and irritability, in contrast to the internalizing symptoms more common among women (Rutz, von Knorring, Pihlgren, Rihmer, & Wålinder, 1995; Zierau, Bille, Rutz, & Bech, 2002; Magovcevic & Addis, 2008; Martin et al., 2013). As a consequence, men with depression may be incapable of showing weakness or of asking for help (Rutz et al., 1995).
In a Danish study on new fathers (Madsen & Juhl, 2007), the EPDS was compared with the Gotland Male Depression Scale (GMDS), developed to detect typical “male” depressive symptoms (Zierau et al., 2002). The study by Madsen and Juhl (2007) indicated depression in 2.1% of the fathers detected by both the EPDS and the GMDS, in 3.1% detected by the EPDS alone, and in 1.3% detected by the GMDS alone, at a score of 10 or higher for the EPDS and 13 or higher for the GMDS. This suggests that some fathers with perinatal depression remain undetected if using only one scale.
How Swedish new fathers respond to the EPDS is of special interest considering that Swedish new mothers are routinely offered EPDS screening. It would be both appealing and practical if the EPDS could also be used for fathers. The possible negative consequences of untreated depression for the children, the fathers and their partners, emphasize the need for screening and support at indication.
Several studies have validated the EPDS for fathers with different results regarding optimal score for possible depression (Massoudi, Hwang, & Wickberg, 2013; Matthey et al., 2001). Matthey et al. (2001) evaluated that score 9/10 or more was optimal for detection of minor and/or major depression. Massoudi et al. (2013) recommend EPDS for detection of major depression at score 12 or more. Another aspect to consider when using the “female” EPDS on fathers is to compare it with a “male” instrument such as the GMDS (Madsen & Juhl, 2007), based on the idea that men and women might express different depressive symptoms. Considering these findings, it would be of interest to study (a) how a population of new Swedish, urban fathers responded to the EPDS at score ≥10 and ≥12, respectively, compared to the GMDS and (b) whether certain sociodemographic risk factors are associated with possible depression detected by the EPDS, the GMDS, or the both scales combined.
Method
Study Design
A cross-sectional design was used to study the prevalence of possible depression and its association with certain sociodemographic factors in a population of fathers with children 3 to 6 months old. The term possible depression intends that this condition is indicated by EPDS and/or GMDS scores, although the diagnosis has not been confirmed by a clinical interview. This period was considered relevant due to the increased prevalence of depressive symptoms reported in both mothers and fathers during this time (Paulson & Bazemore, 2010).
Study Population and Data Collection Procedure
The study population consisted of men who had become fathers during November–December 2010 and May–June 2011. Their names and addresses were provided through the Swedish Tax Agency’s population registry. In total, 8,011 fathers were sent a questionnaire that could be completed either on the web or in written form when their children were 3 to 4 months old, with two reminders up to 6 months. Of these, 3,656 fathers (46%) answered and 4,251 (54%) did not.
All fathers were sent a personally addressed letter containing information about the study, together with the questionnaire, a pre-stamped envelope for postal response, and web log in information. Fifty-six percent (N = 2,047) of the responding fathers answered the questionnaire in postal form and 44% (N = 1,609) answered via the web.
Response Rate by Area Income
Respondents and nonrespondents were divided into three groups according to their residential address postal code based on median income per year for each area (reported per household for men 18–64 years old, according to the Stockholm County Council Area Database, 2011). The area median income groups were categorized (a) more than 31,983 Euros, (b) between 26,653–31,983 Euros, and (c) below 26,653 Euros. The middle-income interval covered the overall median income in Stockholm county of approximately 28,678 Euros. In the highest income group, 50% (N = 1,700) responded, in the middle-income group 45% (N = 1,537) and in the lowest group 33% (N = 419). Thus, the response rate was lower in areas with generally lower incomes. This difference was significant according to Pearson’s χ2 test (χ2 = 32.71, p = .001).
Measures
Fathers were identified as possibly depressed if reaching a certain score (further specified below) at screening by the EPDS and the GMDS. The EPDS was originally developed by Cox et al. (1987) and contains 10 items with four response options each rated 0–3. Thus the range is 0–30 points, where higher scores indicate more depressive symptoms. The EPDS asks if, during the last seven days, the respondent had been able to laugh/see the funny side of things, looked forward to things with enjoyment, blamed oneself unnecessarily when things went wrong, been anxious or worried for no good reason, felt scared or panicky for no good reason, felt that things had been “getting on top” [of the respondent], had been so unhappy that it has been difficult to sleep, had felt sad or miserable, had been so unhappy that [the respondent] has been crying, and if the thought of harming oneself had occurred to the respondent. The EPDS has been validated for fathers by Matthey et al. (2001), who demonstrated that score 9/10 or more was optimal for detection of minor and/or major depression, with a sensitivity of 71.4%, a specificity of 93.8%, and a positive predictive value of 29.4%. The EPDS has also been validated for Swedish fathers with a resulting sensitivity of 100%, a specificity of 87.4% and a positive predictive value of 20.0% when only including major depression (Massoudi et al., 2013). The reliability for EPDS was 0.81 according to Cronbach’s α in both the validation of EPDS for fathers by Matthey et al. (2001) and the one by Massoudi et al. (2013), and in the present study 0.83.
The Gotland Male Depression Scale (GMDS) was developed and validated for men by Zierau et al. (2002) and has 13 items with four response options, also rated 0–3. The possible range for the GMDS is 0–39. A total score of 13–26 indicates possible depression and scores of 27 or above clearly indicates depression. The GMDS asks about stress, aggressiveness/outward-reactivity/difficulties keeping self-control, feeling of being burned out and empty, constant inexplicable tiredness, irritability/restlessness/frustration, difficulty making everyday decisions, sleep problems, morning disquiet/anxiety/uneasiness, overconsumption of alcohol or pills/hyperactivity/over- or undereating, tendency in the biological family of abuse/depression/dejection/suicide attempts/proneness to behavior involving danger, being unrecognizable/hard to deal with as perceived by oneself and/or others, expressions of hopelessness, and self-pity during the last month. The reliability for GMDS was 0.86 according to Cronbach’s α in the study by Zierau et al. (2002), and in the present study 0.88.
Two different scores were used for the EPDS due to the different outcomes of validation studies, either a score of 10 and more (Matthey et al., 2001) or a score of 12 and more (Massoudi et al., 2013). Since the main focus of the study was on the EPDS, only the score of 13 or more was used for the GMDS, which indicates possible major depression according to Ziearau et al. (2002). A score above 26 clearly indicates major depression according to Zierau et al. (2002). Regardless of GMDS score, fathers scoring 10 or more on the EPDS thus may be considered as having possible minor or major depression (Matthey et al., 2001), while fathers scoring 12 or more on the EPDS, may be considered as having possible major depression (Massoudi et al., 2013).
In addition to the EPDS and GMDS items, the survey also contained questions covering possible risk factors related to the sociodemographic variables: marital status, income, education, occupation, country of birth, paternal age, and number of children. The major rationale behind the choice of sociodemographic factors was that they are relatively approachable in the design of interventions (Whitehead & Dahlgren, 2006). If the prevalence of depression is associated with certain sociodemographic background factors, these factors may give a clue to which fathers may be in most need of depression screening and prevention/intervention efforts. Table 1 describes the categories of the included sociodemographic variables and their distribution for fathers with and without possible depression.
Table 1.
Sociodemographic Data of the Participants.
|
EPDSa ≥10 and/or GMDSb ≥13
|
EPDSa ≥12 and/or GMDSb ≥13
|
|||
|---|---|---|---|---|
| Fathers with possible depression according to the EPDSa/ GMDSb | Fathers without depression according to the EPDSa/ GMDSb | Fathers with possible depression according to the EPDSa/ GMDSb | Fathers without depression according to the EPDSa/ GMDSb | |
|
Age, mean, years (SD)
Min–max |
35.4 (6.1) 18–63 |
35.4 (5.9) 19–74 |
35.4 (6.3) 18–63 |
35.3 (5.9) 19–74 |
| Marital status [N (%)] | ||||
| Married | 335 (58.6) | 1,719 (56.0) | 249 (56.6) | 1,805 (56.4) |
| Co-habitant | 225 (39.3) | 1,323 (43.1) | 184 (41.8) | 1,364 (42.6) |
| Living apart | 8 (1.4) | 16 (.5) | 5 (1.1) | 19 (.6) |
| Single | 4 (.7) | 6 (.2) | 2 (.5) | 8 (.2) |
| Widower | – | 3 (.1) | – | 3 (.1) |
| Other | – | 3 (.1) | – | 3 (.1) |
| Income, Euros/month [N (%)] | ||||
| <3,205 | 260 (45.4) | 774 (25.4) | 203 (46.6) | 831 (25.9) |
| 3,205–4,273 | 140 (24.4) | 758 (24.8) | 109 (25.0) | 789 (24.6) |
| 4,274–5,342 | 86 (15.0) | 726 (23.8) | 63 (14.4) | 749 (23.4) |
| >5,343 | 84 (14.7) | 792 (26.0) | 62 (14.2) | 814 (25.4) |
| Occupation [N (%)] | ||||
| Employment | 443 (78.1) | 2,606 (85.4) | 349 (80.0) | 2,700 (84.2) |
| Self-employed | 52 (9.2) | 312 (10.2) | 35 (8.0) | 329 (10.3) |
| Parental allowance | 9 (1.6) | 22 (.7) | 8 (1.8) | 23 (.7) |
| Unemployment fund | 10 (1.8) | 22 (.7) | 8 (1.8) | 24 (.7) |
| Sickness benefit | 10 (1.8) | 3 (.1) | 10 (2.3) | 3 (.1) |
| Study allowance | 15 (2.6) | 48 (1.6) | 13 (3.0) | 50 (1.6) |
| Other | 17 (3.0) | 38 (1.2) | 12 (2.8) | 43 (1.3) |
| Education [N (%)] | ||||
| Public school | 43 (7.5) | 131 (4.3) | 37 (8.5) | 137 (4.3) |
| High school 2 years | 35 (6.1) | 176 (5.7) | 27 (6.2) | 184 (5.7) |
| High school 3 or 4 years | 154 (26.9) | 711 (23.2) | 124 (28.4) | 741 (23.1) |
| Basic education adults | 54 (9.4) | 168 (5.5) | 36 (8.3) | 186 (5.8) |
| University | 263 (45.9) | 1,766 (57.6) | 196 (45.0) | 1,833 (57.2) |
| Other | 24 (4.2) | 114 (3.7) | 20 (4.6) | 118 (3.7) |
| Country of birth [N (%)] | ||||
| Sweden | 386 (67.4) | 2,465 (80.8) | 300 (68.8) | 2,551 (79.6) |
| Others | 182 (31.8) | 584 (19.2) | 137 (31.4) | 629 (19.6) |
| Number of children, mean (SD), min–max | 1.9 (.9) 1–6 |
1.7 (.9) 0–10 |
1.9 (.9) 1–5 |
1.7 (.9) 1–10 |
Note. Percentage/SD within parentheses. aEPDS = Edinburgh Postnatal Depression Scale; bGMDS = Gotland Male Depression Scale.
Ethical Considerations
The study was approved by the Regional Ethics Committee at the Karolinska Institutet (Registration No. 2010/2001-31/4). The information letter clarified that participation was voluntary and could be interrupted at any time and that confidentiality was guaranteed. Fathers with possible depression were offered support from a psychologist (LL) and at indication further referred to a psychiatric specialist.
Statistical Analysis
Statistical analyses were performed by SPSS (IBM SPSS Statistics 20). In the descriptive data (Table 1), fathers who did not answer certain EPDS or GMDS items were also included, if their total score reached ≥10 or ≥12 respectively, or more for the EPDS, and/or ≥13 or more for the GMDS. χ2 tests were used to compare outcome of EPDS versus GMDS, area prevalence, and area income.
Multinomial logistic regression was used to analyze the relationship between possible depression and sociodemographic factors and also included fathers with incomplete answers if they scored 10/12 or more on the EPDS and/or 13 or more on the GMDS. All variables were entered into the model in one step, and p = .05 chosen as significance level. Effect sizes were calculated with Odds Ratios (OR) where a value of 1.5 or less was considered as a small effect size, a value of 2 or less as a medium effect size and a value of 3 or more as a large effect size (Sullivan & Feinn, 2012).
Results
Prevalence of Possible Depression Assessed by the EPDS and the GMDS
Figure 1a demonstrates the prevalence of fathers with possible depression detected by the EPDS alone, the GMDS alone or by the both scales combined. At score 10 or more, EPDS alone detected 7.1% (N = 258) of fathers with possible depression, and the GMDS alone 2.4% (N = 88), while the combined EPDS and GMDS detected 6.2% (N = 227). At score 12 or more, the EPDS alone detected 3.3% (N = 121) and the GMDS alone detected 3.9% (N = 141) of fathers with possible depression, while the EPDS and the GMDS combined detected 4.8% (N = 174).
Figure 1a.
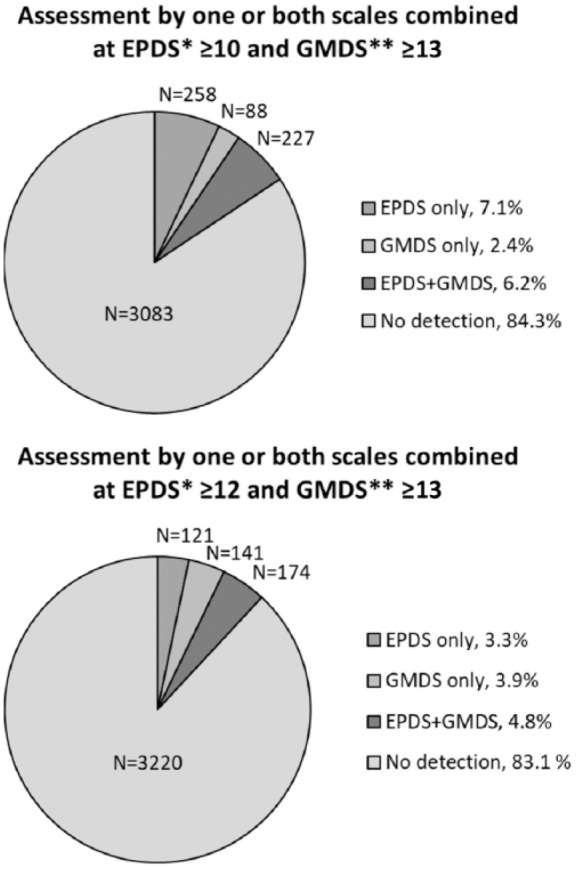
Prevalence of possible depression assessed by EPDS at cutoff ≥10 or ≥12, respectively, and GMDS at cutoff ≥13. Percentage within parentheses. *EPDS = Edinburgh Postnatal Depression Scale;**GMDS = Gotland Male Depression Scale.
Another way to present the prevalence is as in Figure 1b, without regard to the overlapping detection by EPDS and GMDS. From this perspective EPDS at score 10 or more detected 13.3% (N = 485) and EPDS at score 12 or more detected 8.1% (N = 295) of fathers with possible depression, while GMDS at score 13 or more detected 8.6% (N = 315). Thus, the fathers scoring 10 or 11 on the EPDS constituted a quite large group of potentially depressed fathers (5.2%) that are not detected if score 12 or higher is used for the EPDS.
Figure 1b.
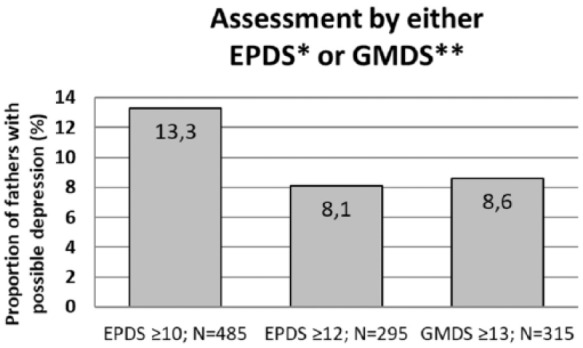
Prevalence of possible depression assessed by each scale, EPDS and GMDS, respectively, regardless of overlapping detection. EDPS has been assessed at cutoff ≥10 or ≥12 and GMDS at cutoff ≥13. Percentages. *EPDS = Edinburgh Postnatal Depression Scale;**GMDS = Gotland Male Depression Scale.
Internal Reliability of EPDS and GMDS and Their Intercorrelation
Cronbach’s α was used to measure the internal reliability within the screening instruments EPDS (0.83) and GMDS (0.88). The intercorrelation between the EPDS and GMDS was assessed by Pearson’s test (0.76, p <.001).
Possible Depression in Relation to Sociodemographic Variables
Analyses based on odds ratios of how possible depression was associated with sociodemographic factors were conducted separately for fathers detected by the EPDS alone, by the GMDS alone, or by the combined EPDS and GMDS. Table 2 demonstrates OR in each detection group following analysis at EPDS ≥10 and EPDS ≥12, respectively, and/or GMDS ≥13.
Table 2.
Association Between Possible depression and Sociodemographic Factors, for Fathers Scoring 10/12 or More on the EPDS and/or 13 or More on the GMDS (multiple regression).
| Depressive symptoms outcome |
EPDSa alone
(at EPDS ≥10) (N = 258) |
EPDSa alone
(at EPDS ≥12) (N = 121) |
GMDSb alone
(at EPDS ≥10) (N = 88) |
GMDSb alone
(at EPDS ≥12) (N = 141) |
Both EPDSa + GMDSb
(at EPDS ≥10) (N = 227) |
Both EPDSa + GMDSb (at EPDS ≥12)
(N = 174)
|
|---|---|---|---|---|---|---|
| Exp B (95% CI) | Exp B (95% CI) | Exp B (95% CI) | Exp B (95% CI) | Exp B (95% CI) | Exp B (95% CI) | |
| Marital status | ||||||
| Single/living apart/widower | 2.4 [0.8, 5.4] | 0.6 [0.1, 4.4] | 4.2 [1.3, 12.8]* | 3.1 [1.1, 8.4]* | 1.0 [0.2, 4.2] | 0.5 [0.1, 3.8] |
| Married or cohabitant | Reference | Reference | Reference | Reference | Reference | Reference |
| Income/month | ||||||
| <3,205 Euros | 2.7 [1.8, 4.3]*** | 2.7 [1.4, 5.0]** | 2.7 [1.3, 5.9]* | 2.5 [1.4, 4.6]** | 2.9 [1.8, 4.7]*** | 3.2 [1.8, 5.6]*** |
| 3,205–4,273 Euros | 1.2 [0.6, 1.9] | 0.8 [0.4, 1.6] | 2.2 [1.0, 4.6]* | 2.0 [1.1, 3.5]* | 2.1 [1.3, 3.4]*** | 2.3 [1.3, 4.0]** |
| 4,274–5,342 Euros | 1.2 [0.7, 1.9] | 1.1 [0.6, 2.2] | 1.0 [0.4, 2.4] | 1.0 [0.6 2.0] | 1.1 [0.6, 1.8] | 1.1 [0.6, 2.0] |
| >5,343 Euros | Reference | Reference | Reference | Reference | Reference | Reference |
| Education | ||||||
| Other education | 0.8 [0.4, 1.7] | 1.2 [0.5, 3.3] | 0.3 [0.0, 2.5] | 0.2 [0.0, 1.4] | 1.1 [0.5, 2.2] | 1.4 [0.7, 2.8] |
| Public school | 1.0 [0.5, 1.8] | 1.5 [0.7, 3.3] | 2.1 [0.9, 4.7] | 1.4 [0.7, 2.9] | 0.9 [0.5, 1.7] | 1.0 [0.5, 2.0] |
| High school 2 years | 0.7 [0.4, 1.4] | 0.7 [0.3, 2.0] | 1.4 [0.5, 3.4] | 0.8 [0.4, 1.9] | 1.0 [0.5, 1.7] | 1.2 [0.6, 2.2] |
| High school 3–4 years | 1.3 [0.9, 1.8] | 1.9 [1.2, 3.1]** | 1.1 [0.6, 1.9] | 1.1 [0.7, 1.7] | 1.1 [0.8, 1.6] | 1.0 [0.7, 1.5] |
| Basic education adults | 1.7 [1.1, 2.8]* | 1.8 [0.9, 3.6] | 1.8 [0.8, 3.9] | 1.0 [0.5, 2.0] | 0.8 [0.4, 1.5] | 1.0 [0.5, 1.9] |
| University | Reference | Reference | Reference | Reference | Reference | Reference |
| Country of birth | ||||||
| Born outside Sweden | 1.6 [1.2, 2.2]** | 1.5 [0.9, 2.3] | 0.9 [0.5, 1.6] | 0.8 [0.5, 1.3] | 1.4 [1.0, 1.9] | 1.6 [1.1, 2.3]* |
| Born in Sweden | Reference | Reference | Reference | Reference | Reference | Reference |
| Paternal age, years | ||||||
| 18–31 | 0.8 [0.6, 1.3] | 0.8 [0.4, 1.3] | 1.7 [0.8, 3.4] | 1.2 [0.7, 2.0] | 0.8 [0.6, 1.3] | 0.9 [0.6, 1.5] |
| 32–35 | 0.9 [0.6, 1.3] | 0.8 [0.5, 1.4] | 1.3 [0.7, 2.7] | 1.1 [0.7, 1.9] | 0.9 [0.6, 1.4] | 1.0 [0.6, 1.5] |
| 36–38 | 1.1 [0.8, 1.7] | 0.8 [0.5, 1.5] | 1.5 [0.7, 3.0] | 1.2 [0.7, 2.1] | 1.1 [0.7, 1.6] | 1.0 [0.6, 1.7] |
| 39 or older | Reference | Reference | Reference | Reference | Reference | Reference |
| Number of children | ||||||
| One child | 0.6 [0.4, 0.8]** | 0.6 [0.3, 0.9]* | 0.9 [0.4, 1.7] | 0.8 [0.5, 1.5] | 0.8 [0.5, 1.2] | 0.7 [0.4, 1.2] |
| Two children | 1.0 [0.7, 1.4] | 0.9 [0.5, 1.5] | 1.2 [0.6, 2.4] | 1.2 [0.7, 2.1] | 1.2 [0.8, 1.9] | 1.1 [0.7, 1.8] |
| Three or more children | Reference | Reference | Reference | Reference | Reference | Reference |
Note. aEPDS = Edinburgh Postnatal Depression Scale; bGMDS = Gotland Male Depression Scale.
p < .05. **p <.01. ***p < .001.
In all groups, there was a significant association between possible depression and low income (OR 2.6–3.2), indicating a moderate or large effect size. The fathers detected by EPDS alone (at both score ≥10 or ≥12) had this association in the lowest income category, while the GMDS and the EPDS + GMDS detected fathers had it for the two lowest income categories (Table 2).
Fathers detected by EPDS alone at score ≥10 had an increased risk of possible depression (OR = 1.8) if their highest education was basic education for adults, while fathers detected by EPDS alone at score ≥12 had an increased risk (OR = 1.9) if their highest education was high school 3–4 years (Table 2). The findings regarding education implied small effects.
Fathers born outside Sweden had a significant association with possible depression in the group detected by EPDS alone at score ≥10, and in the group detected by EPDS + GMDS at EPDS score ≥12, corresponding to a small effect (OR 1.6 in both cases).
Fathers in the group detected by GMDS only had a higher risk (OR = 3.1–4.2) for depression if they had another marital status than married or co-habitants, a finding applicable at both cutoffs for EPDS. No associations were seen regarding paternal age. In the EPDS group, at both score ≥10 and ≥12, fathers with three or more children appeared at increased risk for possible depression since having only one child was associated with a significantly lower risk (OR 0.6 in both cases).
Area-Related Risk for Depressive Symptoms
To investigate whether areas with lower incomes might constitute a possible risk factor for paternal perinatal depression, three income area categories were compared regarding the outcome of EPDS and GMDS assessment among the responders. This comparison was performed at EPDS score ≥10 and ≥12, respectively, corresponding to Tables 3a and 3b. Pearson’s χ2 test identified that there was a significant association between the prevalence of possible depression and area income level (χ2 = 39.93 based on EPDS score ≥10 and χ2 = 26.92 based on EPDS score ≥12, p <.001 in both cases). This analysis indicated that the proportion of fathers with possible depression was higher among the respondents in areas with generally lower incomes (medium effect size, OR = 1.67 and 1.69, at EPDS ≥10 and ≥12, respectively).
Table 3.
Prevalence of Depressive Symptoms Among Responders in Relation to Area-Related Median Income, EPDS ≥ 10 and GMDS ≥ 13.
| Area type by income
category (median year income, Euros/year) |
|||
|---|---|---|---|
| Higher | Medium | Lower | All areas |
| More than 31,983 Euros |
26,653– 31,983 Euros |
Below 26,653 Euros |
|
| Number of fathers with possible depression, N (%) | |||
| 203 (11.9) | 274 (17.8) | 96 (22.9) | 573 (15.7) |
Note. χ2 = 39.93, p < .001. OR = 1.67. Fathers detected with EPDS ≥ 10 and/or GMDS ≥ 13. Percentage within parentheses. aEPDS = Edinburgh Postnatal Depression Scale; bGMDS = Gotland Male Depression Scale.
Table 4.
Prevalence of Depressive Symptoms Among Responders in Relation to Area-Related Median Income, EPDS ≥ 12 and GMDS ≥ 13.
| Area type by income
category (median year income, Euros/year) |
|||
|---|---|---|---|
| Higher | Medium | Lower | All areas |
| More than 31,983 Euros |
26,653– 31,983 Euros |
Below 26,653 Euros |
|
| Number of fathers with possible depression, N (%) | |||
| 158 (9.3) | 204 (13.3) | 74 (17.7) | 436 (11.9) |
Note. χ2 = 26.92, p < .001. OR = 1.69. Fathers detected with EPDS ≥ 12 and/or GMDS ≥ 13. Percentage within parentheses. aEPDS = Edinburgh Postnatal Depression Scale; bGMDS = Gotland Male Depression Scale.
Discussion
An important finding of the present study was that many of the fathers with possible depression were detected only by one of the two instruments used, either EPDS or GMDS. This indicates that the EPDS and the GMDS probably capture different aspects of depression and that neither scale is optimal for detection of paternal perinatal depression. In addition, the risk factors associated with possible depression varied between the categories of fathers detected by EPDS, GMDS, or both scales combined, further supporting that they measure different depressive aspects.
Low income was a sociodemographic factor associated with possible depression in all of the detection groups (EPDS alone, GMDS alone, or both scales). Therefore, low income is a probable risk factor for perinatal depression, which has also been reported elsewhere (Bergstrom, 2013; Eastwood, Phung, & Barnett, 2011; Rosenthal, Learned, Liu, & Weitzman, 2013), as generally for men with depression (Everson, Maty, Lynch, & Kaplan, 2002). The association between a lower income and possible depression was also observed at area level, when comparing general area median income and the corresponding area prevalence of possible depression. Low income and depression may mutually affect each other and have a reciprocal causal relationship (Williams & Cheadle, 2016). The financial hardship could lead to distress and depression, but impaired mental health may also interfere with provision and career opportunities (Williams & Cheadle, 2016.)
Certain educational levels were, among fathers detected by EPDS alone, possible risk factors for depression. At EPDS ≥ 12, fathers with high school 3–4 years as their highest education had an increased risk for depression. This probably reflects that a higher proportion, 28.4%, of high-scoring fathers belonged to this educational category compared to 23.1% of the low-scoring fathers. It is worth to mention that both these figures are higher than the corresponding 19.7% in Stockholm county with 3–4 years high school education, thus implying that the responding fathers of this study generally were slightly more educated than the actual population. At EPDS ≥ 10, instead, basic education for adults increased the risk for depression. Individuals that undergo basic education for adults normally do so to complete unfinished or unsuccessful schooling. It could thus be speculated that fathers that reported this education category might have experienced school problems earlier in life. A vast literature has pointed at a correlation between mental ill health (including depression) and lower school grades (Schulte-Korne, 2016). In addition, poor school performance has been demonstrated as a mediator of the association between unfavorable childhood conditions and psychiatric care utilization in young adulthood (Björkenstam et al., 2016). The increased risk for depression associated with basic education for adults may also be related to an early debut of depression and thus an increased risk for recurrent depressions in a lifetime perspective (Paulson & Bazemore, 2010). A joint outcome at both EPDS ≥ 10 and EPDS ≥ 12, was that university, the highest education level, was associated with the lowest risk for possible depression.
To have been born in a foreign country seemed to be a possible risk factor for paternal depression in certain detection groups. In line with this result, a foreign country of birth has also been demonstrated a risk factor for depression in new mothers (Eastwood et al., 2011; Almeida, Costa-Santos, Caldas, Dias, & Ayres-de-Campos, 2016; Fellmeth, Fazel, & Plugge, 2017). Parents that have been born in another country might be more prone to depression due to the psychological impact by forced migration or traumatic experiences like torture and loss of family members (Almeida et al., 2016; Fellmeth et al., 2017). Even when the reasons for migration are less dramatic, like striving for better life opportunities, migrants run increased risk for impaired mental health due to, for example, isolation, loss of social support, language difficulties, unemployment, and other problems related to the new environment (Almeida et al., 2016; Fellmeth et al., 2017).
In the group of fathers detected by the EPDS alone, having only one child implied a lower risk of depression and could be considered as a protective factor compared to fathers with three or more children. This result is not surprising since the burden of caretaking could be expected to increase with the number of children. Accordingly, multiparous mothers have a higher risk of postnatal depressive symptoms (Lanier & Jonson-Reid, 2014).
Within the group that was detected with the GMDS alone, there was a higher risk for depression for fathers that were singles, living apart, or widowers. This result is somewhat difficult to explain, but further supports the impression that the EPDS and the GMDS measure different aspects of depression and thereby may be associated with different risk factors. The two screening instruments measure different time frames and, to the most part, ask different questions. Both these factors could have influenced the results. The EPDS asks the respondent to answer the items based on the experienced mental health during the last week, while the GMDS items on the other hand asks about this condition during the last month. Thus, the GMDS encompasses a four times longer period, and might to a higher degree catch depressions of longer duration than the EPDS. Depressive symptoms of longer duration could in turn be expected to have a stronger association with problems in the relationship, which may at least partially explain why fathers who did not live with a partner to a higher degree screened positively on the GMDS alone. Another possibility is that the GMDS items, asking about aggressiveness, outward-reactivity, difficulties keeping self-control, or irritability, to a higher degree than the EPDS items catch a depressive condition that is more destructive for relations.
A strength of the study is that both responders and nonresponders could be categorized and grouped based on the general income level of their residences. This categorization indicated that areas with lower incomes had a greater proportion of fathers with possible depression, thus supporting the finding of low income as a risk factor for depression.
A limitation of the present study is that the percentage of nonresponders was greater than 50%; however, this result is similar to other surveys (Bladon, 2010; Czajka & Beyler, 2016) that report a general downward trend in response rates. Possible explanations for this trend include a survey “tiredness” or the idea that surveys “drown” in a society with an increasing information flow. The high proportion of nonresponders implies an uncertainty about the prevalence in the total population. Since the response rate was lower in areas with a lower average income, it is not unlikely that the prevalence of depression was even higher in these areas. Still, other factors that were not considered in this study could have contributed to an overestimation of the prevalence. A further limitation is that the GMDS contains multiple question items (e.g., tendency in the biological family of abuse/depression/dejection/suicide attempts/proneness to behavior involving danger), that may be interpreted differently by respondents, which in turn could aggravate the interpretation of the results.
Conclusions
The findings of the present study confirm the results by Madsen and Juhl (2007) that the EPDS and the GMDS are partially overlapping in detecting depression, also in Swedish new fathers. The dissonance is further indicated by different risk factors associated within the detection groups. Thus, the use of both scales would likely reduce the risk of missing new fathers with depression.
If aiming to prevent depression, it is justified to use a lower EPDS score, 10 or even lower, in order to decrease the risk for missing cases and to include also minor depression, which could otherwise evolve into major depression (Cox et al., 1987). The use of an EPDS score including minor depression is also motivated by the observations of an increased risk for inter-parental conflict, and to some extent also higher levels of difficulties in infant temperament, at assessment of paternal depression with EPDS score ≥10 (Ramchandani et al., 2011).
Low income was a possible risk factor for all groups. This finding raises the question whether fathers or families suffering from economic hardship might need further diagnostic assessment for depression in order to receive adequate treatment or other support. The finding of a higher prevalence of possible depression in low-income areas pointed in the same direction. To be born in a foreign country and to have many children were other possible risk factors constituting possible target criteria for aimed support.
There is an ongoing discussion in the literature to separate between parental distress and parental depression, although there are indications that also parental distress can negatively affect the child (Eastwood et al., 2011; Ramchandani et al., 2011). From a preventive perspective, it would be more careful to screen parents for all types of mental illness, both for the reason that little is known about the pathogenetic pathways between distress and depression, and because it is generally easier to treat mental illness at earlier stages. The findings of this and other studies (Massoudi et al., 2013; Matthey et al., 2001) suggest further research to develop screening of new fathers with both EPDS and GMDS, or a questionnaire based on the combined scales, in order to increase the detection of distress and depression.
Acknowledgments
Without the fathers that participated in the study no results would have been obtained, so the authors are sincerely thankful to the responders. Hopefully the findings will be useful. The authors deeply regret that Fia Simon, who contributed to the study, is no longer with us. Finally, the authors express their gratitude to the Stockholm County Council that provided the funding.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by the Public Health Grant (HSNF-0978) from the Stockholm County Council.
References
- Almeida L. M., Costa-Santos C., Caldas J. P., Dias S., Ayres-de-Campos D. (2016). The impact of migration on women’s mental health in the postpartum period. Revista Saude Publica, 50(35), 1–13. doi: 10.1590/S1518-8787.2016050005617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- APA (American Psychological Association). (2013). Diagnostic and statistical manual of mental disorders (DSM-V). Washington, DC: American Psychological Association. [Google Scholar]
- Bergstrom M. (2013). Depressive symptoms in new first-time fathers: Associations with age, sociodemographic characteristics, and antenatal psychological well-being. Birth: Issues in Perinatal Care, 40(1), 32–38. doi: 10.1111/Birt.12026 [DOI] [PubMed] [Google Scholar]
- Björkenstam E., Dalman C., Vinnerljung B., Weitoft G. R., Walder D. J., Burström B. (2016). Childhood household dysfunction, school performance and psychiatric care utilisation in young adults: A register study of 96 399 individuals in Stockholm County. Journal of Epidemiology and Community Health, 70(5), 473–480. Retrieved from 10.1136/jech-2015-206329 [DOI] [PubMed] [Google Scholar]
- Bladon T. L. (2010). The downward trend of survey response rates: Implications and considerations for evaluators. The Canadian Journal of Program Evaluation, 24(2), 131–156. [Google Scholar]
- Cox J. L., Holden J. M., Sagovsky R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150(6), 782–786. [DOI] [PubMed] [Google Scholar]
- Czajka J. L., Beyler A. (2016). Declining response rates in federal surveys: Trends and Implications (Final report volume I). Washington, DC: Mathematica Policy Research. [Google Scholar]
- Eastwood J. G., Phung H., Barnett B. (2011). Postnatal depression and socio-demographic risk: Factors associated with Edinburgh Depression Scale scores in a metropolitan area of New South Wales, Australia. Australian and New Zealand Journal of Psychiatry, 45(12), 1040–1046. doi: 10.3109/00048674.2011.619160 [DOI] [PubMed] [Google Scholar]
- Edward K.-L., Castle D., Mills C., Davis L., Casey J. (2015). An integrative review of paternal depression. American Journal of Men’s Health, 9(1) 26–34. doi: 10.1177/1557988314526614 [DOI] [PubMed] [Google Scholar]
- Everson S. A., Maty S. C., Lynch J. W., Kaplan G. A. (2002). Epidemiologic evidence for the relation between socioeconomic status and depression, obesity and diabetes. Journal of Pychosomatic Research, 53(4), 891–895. [DOI] [PubMed] [Google Scholar]
- Fellmeth G., Fazel M., Plugge E. (2017). Migration and perinatal mental health in women from low- and middle-income countries: a systematic review and meta-analysis. The British International Journal of Obstetrics and Gynaecology, 124(5), 742–752. doi: 10.1111/1471-0528.14184 [DOI] [PubMed] [Google Scholar]
- Goodman J. H. (2004). Paternal postpartum depression, its relationship to maternal postpartum depression, and implications for family health. Journal of Advanced Nursing, 45(1), 26–35. [DOI] [PubMed] [Google Scholar]
- Lanier P., Jonson-Reid M. (2014). Comparing primiparous and multiparous mothers in a nurse home visiting prevention program. Birth: Issues in Perinatal Care, 41(4), 344–352. doi: 10.1111/birt.12120 [DOI] [PubMed] [Google Scholar]
- Madsen S. A., Juhl T. (2007). Paternal depression in the postnatal period assessed with traditional and male depression scales. Journal of Men’s Health and Gender, 4(1), 26–31. [Google Scholar]
- Magovcevic M., Addis M. E. (2008). The Masculine Depression Scale: Development and psychometric evaluation. Psychology of Men & Masculinity, 9(3), 117–132. [Google Scholar]
- Martin L. A., Neighbors H. W., Griffith D. M. (2013). The experience of symptoms of depression in men vs women: Analysis of the national comorbidity survey replication. JAMA Psychiatry, 70(10), 1100–1106. doi: 10.1001/jamapsychiatry.2013.1985 [DOI] [PubMed] [Google Scholar]
- Massoudi P., Hwang C. P., Wickberg B. (2013). How well does the Edinburgh Postnatal Depression Scale identify depression and anxiety in fathers? A validation study in a population based Swedish sample. Journal of Affective Disorders, 149(1–3), 67–74. doi: 10.1016/j.jad.2013.01.005 [DOI] [PubMed] [Google Scholar]
- Matthey S., Barnett B., Kavanagh D. J., Howie P. (2001). Validation of the Edinburgh Postnatal Depression Scale for men, and comparison of item endorsement with their partners. Journal of Affective Disorders, 64(2–3), 175–184. [DOI] [PubMed] [Google Scholar]
- Paulson J. F., Bazemore S. D. (2010). Prenatal and postpartum depression in fathers and its association with maternal depression: A meta-analysis. Journal of American Medical Association, 303(19), 1961–1969. doi: 10.1001/jama.2010.605 [DOI] [PubMed] [Google Scholar]
- Ramchandani P., Stein A., Evans J., O’Connor T. G, & ALSPAC study team. (2005). Paternal depression in the postnatal period and child development: a prospective population study. Lancet, 365(9478), 2201–2205. doi: 10.1016/S0140-6736(05)66778-5 [DOI] [PubMed] [Google Scholar]
- Ramchandani P. G., O’Connor T. G., Evans J., Heron J., Murray L., Stein A. (2008. a). The effects of pre- and postnatal depression in fathers: A natural experiment comparing the effects of exposure to depression on offspring. Journal of Child Psychology and Psychiatry, 49(10), 1069–1078. doi: 10.1111/j.1469-7610.2008.02000.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchandani P. G., Stein A., O’Connor T. G., Heron J., Murray L., Evans J. (2008. b). Depression in men in the postnatal period and later child psychopathology: A population cohort study. Journal of the American Academy of Child and Adolescent Psychiatry, 47(4), 390–398. doi: 10.1097/CHI.0b013e31816429c2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchandani P. G., Psychogiou L., Vlachos H., Iles J., Sethna V., Netsi E., Lodder A. (2011). Paternal depression: An examination of its links with father, child and family functioning in the postnatal period. Depression and Anxiety, 28(6), 471–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal D. G., Learned N., Liu Y. H., Weitzman M. (2013). Characteristics of fathers with depressive symptoms. Maternal and Child Health Journal, 17(1), 119–128. doi: 10.1007/s10995-012-0955-5 [DOI] [PubMed] [Google Scholar]
- Rutz W., von Knorring L., Pihlgren H., Rihmer Z., Wålinder J. (1995). Prevention of male suicides: Lessons from Gotland study. The Lancet, 345(8948), 524. [DOI] [PubMed] [Google Scholar]
- Schulte-Korne G. (2016). Mental health problems in a school setting in children and adolescents. Deutsches Arzteblatt International, 113(11), 183–190. doi: 10.3238/arztebl.2016.0183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan G. M., Feinn R. (2012). Using effect size-or why the p value is not enough. The Journal of Graduate Medical Education, 4(3), 279–282. doi: 10.4300/JGME-D-12-00156.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead M., Dahlgren G. (2006). Concepts and principles for tackling social inequities in health: Levelling up part 1. Copenhagen: WHO Regional Office for Europe. [Google Scholar]
- Williams D. T., Cheadle J. E. (2016). Economic hardship, parents’ depression, and relationship distress among couples with young children. Society and Mental Health, 6(2), 73–89. doi: 10.1177/2156869315616258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zierau F., Bille A., Rutz W., Bech P. (2002). The Gotland Male Depression Scale: A validity study in patients with alcohol use disorder. Nordic Journal of Psychiatry, 56(4), 265–271. doi: 10.1080/08039480260242750 [DOI] [PubMed] [Google Scholar]


