Abstract
Men on the Move–Nashville was a quasi-experimental, 10-week pilot physical activity intervention. A total of 40 overweight or obese African American men ages 30 to 70 (mean age = 47) enrolled in the intervention. Participants attended 8 weekly, 90-minute small group sessions with a certified personal trainer. Each session consisted of discussions aimed to educate and motivate men to be more physically active, and an exercise component aimed to increase endurance, strength, and flexibility. Throughout each week, men used wearable activity trackers to promote self-monitoring and received informational and motivational SMS text messages. Of the 40 enrolled men, 85% completed the intervention, and 80% attended four or more small group sessions. Additionally, 70% of participants successfully used the activity tracker, but only 30% of men utilized their gym memberships. Participants benefited from both the small group discussions and activities through increasing social connection and guidance from their trainer and group members. These African American men reported being motivated to engage in physical activity through each of these technologies. Men reported that the activity trackers provided an important extension to their social network of physically active people. The intervention resulted in significant increases in men’s self-reported levels of light, moderate, vigorous, and sports-related physical activities, and high-density lipoprotein cholesterol levels, and significant decreases in weight and body fat percentage with small, moderate and large effects shown. Including technology and didactic components in small group-based interventions holds promise in motivating African American men to increase their physical activity.
Keywords: African American men, physical activity, obesity, self-determination theory, motivational interviewing, health communications, men’s health
Introduction
Physical activity is a key health promotion strategy across the life course, yet, relative to younger men, middle-aged and older aged African American men’s physical activity rates tend to be lower (King et al., 2008). This is particularly problematic because individuals who are physically inactive are at a higher risk for developing chronic diseases, especially as they age (Appel et al., 2011; Joyner & Nose, 2009; Thorpe et al., 2013). Compared with White men and women and African American women, African American men are more likely to experience higher rates and earlier onset of chronic conditions associated with the leading causes of death in the United States (Howlader et al., 2010; Keenan & Shaw, 2011; Warner & Hayward, 2006).
Despite the need to increase physical activity in this population, all physical activity and weight loss interventions targeted to African Americans recruited considerably more women than men (Newton, Griffith, Kearney, & Bennett, 2014; Whitt-Glover et al., 2014; Whitt-Glover & Kumanyika, 2009). In addition, reviews of physical activity in men found few studies reporting data for African American men (George et al., 2012; Kassavou, Turner, & French, 2013; Wong, Gilson, van Uffelen, & Brown, 2012). In a review of African American men’s response to interventions aiming to promote weight loss, increase healthy eating, or increase physical activity, there were only six community-based studies that reported data separately for African American men (Newton et al., 2014). Of these six studies, four were exclusively geared toward African American men, and two of these four focused on physical activity (Hooker, Harmon, Burroughs, Rheaume, & Wilcox, 2011; Treadwell et al., 2010) and reported moderate, but significant changes in physical activity.
Since this review, the findings from one community-based physical activity intervention have been published—Men on the Move (Griffith, Allen, Johnson-Lawrence, & Langford, 2014). In Men on the Move, participants met in weekly sessions at an agreed on time to engage in physical activity led by a personal trainer. While the pilot produced modest yet significant increases in African American men’s perceived health status, self-efficacy to sustain physical activity and intensity of physical activity, the increase in physical activity seemed to be primarily due to the activity they engaged in during the weekly session. In another model, Hooker et al. (2011) held didactic sessions to educate and motivate men to engage in physical activity, but it did not build in time for men to exercise. To date, no study with African American men has structured sessions to include both a physical activity training component and didactic educational and motivational activities.
In these recent studies, African American men noted how important social support, social connectedness, and motivation are to becoming and remaining physically active (Griffith et al., 2014; Griffith, Gunter, & Allen, 2011; Hooker et al., 2011; Treadwell et al., 2010). These findings are consistent with qualitative work conducted by Griffith, King, and Allen (2013) who reported that African American men highly valued the role of male peers in helping them remain motivated to engage in physical activity; however, only Hooker and colleagues (2011) explicitly built social support into formal sessions of their program. While Hooker used team building activities (e.g., creating team names, facilitating group identity) and promoted healthy competition between teams, none of these previous studies utilized technology to motivate men to be more active or to promote self-monitoring of physical activity, social connectivity, and social support.
The emergence of recent technology such as text messaging, accelerometers, and other wearable activity trackers has provided new tools that can be utilized to increase healthy behaviors, specifically physical activity (Mohr, Burns, Schueller, Clarke, & Klinkman, 2010). SMS text messaging is a widely used mode of communication and has been used to disseminate information and increase preventive health behaviors (Fjeldsoe, Marshall, & Miller, 2009; Kannisto, Koivunen, & Välimäki, 2014). In addition, accelerometers and other wearable activity trackers help individuals monitor their activity and have been effective within certain physical activity interventions (Butryn, Arigo, Raggio, Colasanti, & Forman, 2016; Gerber, Stolley, Thompson, Sharp, & Fitzgibbon, 2009). Butryn et al. (2014) tested a pilot intervention that promoted self-monitoring and social connectivity by giving a physical activity tracker to middle-aged women at risk for cardiovascular diseases. Moderate to vigorous physical activity significantly increased across their 6-month program. These positive findings raise the question of the generalizability of these tools to promote physical activity among African American men. To date, while some studies have included wearable devices as part of the evaluation (Hooker et al., 2011), no community-based physical activity intervention for African American men has included SMS text messaging or wearable activity trackers as a component of the intervention (Kirwan, Duncah, Vandelanotte, & Mummery, 2012; Newton et al., 2014).
This article describes Men on the Move–Nashville: a 10-week physical activity pilot intervention for middle to older age African American men. This study aimed to (a) assess the feasibility and acceptability of didactic, small group workout sessions, SMS text messages, and a wearable physical activity tracker and (b) increase physical activity and improve health outcomes.
Method
Setting
Nashville is the second largest metropolitan statistical area in Tennessee, and 27.7% of the city’s population is African American (U.S. Census Bureau, 2010). African Americans in Nashville have increased risk of morbidity from diseases such as heart disease, diabetes, and several forms of cancer (Davidson County Health Department, 2014), and African American men have lower life expectancy compared with their non-Hispanic, White counterparts (Davidson County Health Department, 2014; Hull, Reece, Atchison, & Husaini, 2009; Peng, Li, & Bauer, 2013).
Recruitment
Men on the Move–Nashville was reviewed and approved by the Vanderbilt Institutional Review Board. Snowball sampling was implemented to recruit participants via word of mouth, distributing fliers, and sending e-mails to staff and partner organization social networks, and a database of people who expressed interest in participating in studies conducted by the Institute for Research on Men’s Health at Vanderbilt.
Eligibility Criteria
Men were eligible to participate if they met all of the following criteria: (a) primarily identified as African American or Black, (b) were 30 to 70 years old, (c) had a body mass index (BMI) of 25 or greater, (d) weighed less than 400 pounds, and (e) did not have or regularly use a gym membership (defined as <8 days of gym membership use in past 30 days). Given, people with gym memberships use their gym facility on average two times per week, or eight times per month, this was set as the criteria for regular use of gym membership (International Health, Racquet & Sportsclub Association and Industry Insights, Inc., 2012). Eligible men were given the Physical Activity Readiness Questionnaire, a screening tool used to determine the possible risk of exercising for an individual (American College of Sports Medicine, Tharrett, & Peterson, 1997). Those who answered “yes” to any question on the Physical Activity Readiness Questionnaire were required to obtain a physician’s approval to participate in the study.
Participants
Forty African American men were enrolled in this study (see Table 1). The mean age for participants was 46.9 years (SD = 9.8), but ages ranged from 31 to 67 years. Most men were either married or in a relationship (75%); 55% of men had household incomes of $50,000 or more, and 50% of the men indicated it was somewhat or very difficult to pay bills. Table 2 highlights baseline health and physical activity characteristics of participants. Over 67% of men were obese (BMI ≥ 30), and 60% had a waist circumference of 40 inches or more. Fewer than half (47.5%) of men indicated that they were confident that they could set aside 30 minutes of physical activity at least three times a week. Only 45% of men self-reported they were engaging in regular physical activity.
Table 1.
Baseline Demographic Characteristics of all Men on the Move–Nashville Participants (n = 40).
| n (%) | |
|---|---|
| Age (years), mean (SD) | 46.9 (9.8) |
| African American men | 40 (100.0) |
| Married/in a relationship | 30 (75.0) |
| Average household size (N people) | 3.3 people |
| Income | |
| Less than $25,000 | 6 (15.0) |
| $25,000-$49,999 | 10 (25.0) |
| $50,000 and more | 22 (55.0) |
| Somewhat/very difficult to pay bills | 20 (50.0) |
Table 2.
Baseline Characteristics of all Men on the Move–Nashville Participants (n = 40).
| Mean (SD) | |
|---|---|
| Physiological characteristics | |
| Weight (lbs.) | 242.1 (57.8) |
| BMI | 34.5 (7.8) |
| Waist circumference | 41.3 (5.9) |
| Body fat percentage | 31.2 (6.7) |
| Glucose | 110.7 (33.7) |
| Total cholesterol | 189.5 (32.6) |
| HDL level | 41.3 (11.0) |
| Self-reported physical activity | |
| Total minutes physical activity/week | |
| All physical activity | 678.38 (470.12) |
| Moderate-to-vigorous physical activity | 391.13 (280.12) |
| Vigorous physical activity | 97.50 (106.17) |
| Sports | 342.00 (333.66) |
| Caloric expenditure/week (Kcal/week) | |
| All physical activity | 4358.82 (3090.38) |
| Moderate-to-vigorous physical activity | 3062.02 (2259.98) |
| Vigorous physical activity | 1133.66 (1277.76) |
| Sports | 2565.12 (2547.31) |
| Health, n (%) | |
| Obese (BMI ≥ 30), (%) | 27 (67.5) |
| Unhealthy waist size (>40 in.), (%) | 24 (60.0) |
| Self-rated health as poor or fair | 19 (47.5) |
| Met recommended level of weekly physical activity (2.5 hour moderate/1.25 hour vigorous) | 33 (82.5) |
| Attitudes about physical activity, n (%) | |
| Very confident could set aside time for physical activity (at least 30 minutes, three times a week) | 19 (47.5) |
| Physical activity readiness, n (%) | |
| Currently engage in regular physical activity | 18 (45.0) |
| Regularly active for the past 6 months | 14 (35.0) |
Note. BMI = body mass index; HDL = high-density lipoprotein.
Conceptual and Theoretical Foundations
The intervention model was anchored in the Social Ecological Framework of health behavior (McLeroy, Bibeau, Steckler, & Glanz, 1988) to highlight environmental constraints (e.g., resources and opportunities to engage in physical activity) that men face (Hill, 2006). Elements of Social Cognitive Theory were also included to identify the importance of providing opportunities for goal setting, self-monitoring, social support, and skills training and mastery to increase self-efficacy to change and maintain health behavior (Bandura, 2004). Additionally, this study aimed to enhance Autonomous Motivation, a key element of Self-determination Theory, that highlights the need for men to identify their own sources of motivation, not ones performed due to external or internal pressure or coercion (e.g., pleasing others, fear of disease, avoiding guilt or shame; Fortier, Williams, Sweet, & Patrick, 2009). Finally, social support was included to facilitate and grow men’s active social networks that could help them combat time pressures, unhealthy social norms, and other interpersonal barriers to physical activity (Anderson, Winett, & Wojcik, 2007; Israel & McLeroy, 1985).
Intervention Components
Men on the Move–Nashville involved four key components: (a) weekly small group sessions that included group discussion and physical activity, (b) providing men with a Fitbit® Flex™ (wearable activity tracker), (c) sending participants SMS text messages three times a week, and (d) increasing access to outside physical fitness centers. These intervention components were selected based on qualitative and other pilot research designed by and with African American men (Griffith et al., 2011; Griffith et al., 2013; Griffith et al., 2014; Griffith, Gunter, & Allen, 2012). While these components are perhaps common to interventions with other men, this intervention is culturally sensitive in that it incorporates attention to deep, culturally relevant sources of social support and motivation discussed in the small group sessions (Resnicow, Baranowski, Ahluwalia, & Braithwaite, 1999). Participants could receive up to $140 in incentives for completing physiological screenings and health questionnaires at the beginning and end of the study and participating in small group sessions during the intervention.
Small Group Sessions
Participants were assigned to one of four small groups of 8 to 10 men based on when they indicated they could meet consistently once a week for 90 minutes. Small group sessions were held at a personal training facility that was centrally located. All trainers that led the small group sessions were African American men. Prior to beginning the program, each trainer completed an orientation with study staff to understand the expectations of the program and their roles as small group leaders and trainers in the program.
At the beginning of the program, each group was tasked with coming up with a team name and were given t-shirts with their team name to initiate socialization among group members and competition between groups. Weekly sessions lasted for 90 minutes and included (a) a 45-minute small group discussion on specific topics relevant to creating and maintaining an active and healthy lifestyle (e.g., finding sources of motivation, addressing barriers to physical activity, identifying, and maintaining healthy social supports) and (b) a 45-minute workout session led by the group’s personal trainer. The small group component was designed to foster self-efficacy, autonomous motivation, and enjoyment (Fortier et al., 2009). People lose motivation to maintain an active lifestyle in part because they simply no longer enjoy it, are not confident in their ability to successfully engage in new activities, or they do not see how it benefits things that are most important to them. Consequently, these sessions were designed to integrate skills building (and therefore self-efficacy) and connect being active to personal values, spirituality, and goal setting in order to facilitate autonomous motivation and enjoyment of physical activity.
The small group intervention also was selected because it can serve as an important source of vicarious learning and social support. In the previous pilot study, African American men enjoyed the camaraderie and support they received from their small group, and they benefitted from seeing that others were struggling with and overcoming similar barriers to physical activity they faced (Griffith et al., 2014). The men reported that they learned from and supported one another with strategies to overcome barriers to physical activity. During the workout portion of the small group sessions in the current pilot, personal trainers taught and engaged participants in physical activities the men could easily do on their own outside their weekly sessions.
The discussion component of the small group sessions was facilitated by the certified personal trainer and guided by worksheets designed by the principal investigator and research team. The worksheets aimed to help men identify key sources of motivation to engage in physical activity and lead a healthier lifestyle. Following the discussion, worksheets were collected by the trainer and submitted weekly to study staff.
The structure and questions of the small group worksheets were modified from a group-based motivational interviewing intervention for women with HIV (Holstad, DiIorio, Kelley, Resnicow, & Sharma, 2011) and included an adapted form of the values linkage execrise (Cornish, McKissic, Dean, & Griffith, 2017). For Session 1, participants were shown a list of 26 characteristics based on Resnicow et al. (2008) findings on the important aspects of African Americans’ identities and potential sources of autonomous motivation. Some characteristics included being a good parent, good spouse, good provider, strong, competent, spiritual, good Christian, successful, and responsible (Resnicow et al., 2008). Participants were first prompted to “Circle 2-3 values or goals that are important you.” Men were asked, “How might being as healthy as you can be help you to achieve these goals?” The last question was “Health can affect your relationships with others, your work and other areas of your life. What are some areas of your life that could be better if you are healthier?”
During Session 3, men revisited the same list of values and goals, and they were asked again to choose two to three core values or life goals that were important to them. This time, participants were asked to answer the following question, “Being more active can help you at home, at work, with friends, with stress or just to feel better. What are some ways you hope being more physically active can help you?” (Cornish et al., 2015).
These are two examples of how the intervention content was designed to be culturally sensitive to African American men (Resnicow et al., 1999). This intervention sought to identify deep structural values, goals, and beliefs that could help men connect their ethnic and gendered goals and values with the goals of promoting health and increasing physical activity. While the previous use of the values clarification exercise was designed for African Americans regardless of gender, these and other worksheet exercises conducted as part of the intervention connected their larger goals and values with health and physical activity in ways that could reflect how ethnic and cultural values are gendered. This is consistent with research by Griffith, Brinkley-Rubinstein, Thorpe, Bruce, & Metzl, 2015) that explores how African American men’s notions of social roles and cultural values were related to how they thought about notions of both manhood and health.
Fitbit Activity Tracker
Each participant received a Fitbit Flex to self-monitor their activity levels throughout the intervention. The Fitbit Flex is a device worn around the wrist that tracks activity levels, including steps, light, moderate and vigorous activity, calories burned, and hours slept and times awoken. Participants were asked to set up their Fitbit online account to regularly sync their device. They were also encouraged to explore the additional social support features available through Fitbit. The activity tracker is connected to a web-platform accessible via mobile devices and computers. Daily activity is automatically synced to this web-platform where men monitor their goals, levels of physical activity, and sleep patterns. Data from the Fitbit Flex were not used in the analyses because data collection from men who wore the activity tracker was inconsistent.
SMS Text Messaging
Scheduled messages were sent to each group of men through an online SMS text messaging system, MobileCommons, based on the day and time of their small group sessions. Study staff sent three different SMS text messages per week to participants throughout the intervention. The content of the messages fell into one of three categories: reminders, informational, or motivational. Reminder messages were sent 24 hours before the designated small group time as a way to prompt men to remember their workout session was near. Informational messages were sent 48 hours after each weekly session and provided a fact they could use as it related to the topic discussed in the session that week. Motivational texts were sent 96 hours (4 days) after each weekly session, and these messages were sources of encouragement for the men to continue being physically active throughout the week. Each participant received the same message content throughout the week to assess general acceptability of receiving text messages.
Fitness Center Membership
In the previous pilot study and in consultation with African American men who participated in cancer awareness activities designed for African American men, participants noted that a barrier to physical activity is the cost, specifically costs to purchase a gym membership (Griffith et al., 2014; Langford, Griffith, Beasley, & Braxton, 2014). In order to reduce this barrier and increase men’s opportunities to engage in physical activity outside of small group sessions, each participant was given a 3-month gym membership to local community fitness centers. The free membership gave participants access to fitness facilities, gyms, a pool, and aquatic classes at six regional community centers in the area. The centers operated from 6:00 a.m. to 8:30 p.m. during the week with shorter hours on the weekend.
Midpoint Check-In
A short midpoint assessment was conducted at the beginning of the small group session in the fifth week to help men gauge their progress halfway through the program and to motivate them to continue engaging in physical activity. Study staff assessed men’s waist circumference, weight, and body fat percentage. Each man who was present at the Week 5 session completed the International Physical Activity Questionnaire (Craig et al., 2003) to measure physical activity level throughout the week. This measure was used at the midway point because it was considerably briefer than the Community Healthy Activities Model Program for Seniors (CHAMPS). Because different physiological data measuring equipment were used during the midpoint compared with the baseline and final assessments, data from this midpoint were not used in the evaluation of program outcome measures.
Process and Outcome Evaluation Measures
Baseline (Week 1) and final (Week 10) evaluations included a self-report survey and a physiological assessment. Each assessment tool is described below.
Self-Report Survey
The health survey included questions on demographic information, overall health status, consumption of healthy food and physical activity using the modified CHAMPS physical activity questionnaire for African Americans (Resnicow et al., 2003). Physical activity categories (moderate-to-vigorous, vigorous, sports, and all physical activity) were defined and calculations were conducted based on prior studies (Ainsworth et al., 1993; Stewart et al., 2001). Additionally, the baseline survey tapped into psychosocial factors related to health and physical activity, and incorporated questions on self-efficacy to engage in physical activity (Resnicow et al., 2002), motivation (baseline only; Ryan, Frederick, Lepes, Rubio, & Sheldon, 1997), perceived social norms around physical activity (e.g., for men, women, African American men; Mahalik, Burns, & Syzdek, 2007), and social support (from the Program for Research on Black Americans’ National Survey of American Life).
Physiological Assessment
Nurses from a university-based health center conducted two physiological assessments at the baseline and final sessions. All anthropometric measurements were conducted using the health center’s established protocols and equipment to ensure the data collection process was consistent and accurate. This screening assessed each man’s height, weight, BMI, waist circumference, body fat percentage, and blood pressure. Nurses drew a small amount of blood to measure nonfasting glucose level, total cholesterol, and high-density lipoprotein (HDL).
Postprogram Feedback
Men who completed the final assessment were offered an opportunity to provide written or verbal, open-ended feedback on the program. Verbal responses were audio-recorded and transcribed. Additionally, two postprogram focus groups were conducted with study participants to obtain more detailed, qualitative insight on men’s experiences and satisfaction with the program components.
Data Analysis
The primary outcomes of interest were recruitment, enrollment, and completion rates based on pilot study guidelines outlined in Thabane et al. (2010). Variance in small group attendance, and overall use of Fitbit Flex and gym memberships were computed as well. Secondary outcomes included changes in physical activity and physiological measures and were assessed using paired t tests for participants with both baseline and final assessment data. A separate set of paired t tests was conducted for participants who attended at least 50% of the small group sessions, which was considered an adequate dose of the intervention. Simple linear regressions were conducted to examine if and to what extent small group attendance influenced changes in physical activity and physiological outcomes. Statistical significance was set at p < .05. IBM SPSS Statistics 22 was used for all quantitative analyses.
A thematic analysis was used to identify, organize, and analyze participants’ feedback from the final assessment and focus group discussions regarding their experience and satisfaction with program components (Aronson, 1994; Braun & Clarke, 2006). This analytic approach was similar to previous research conducted (Griffith et al., 2011; Griffith et al., 2013).
Results
Recruitment, Enrollment, and Completion Rates
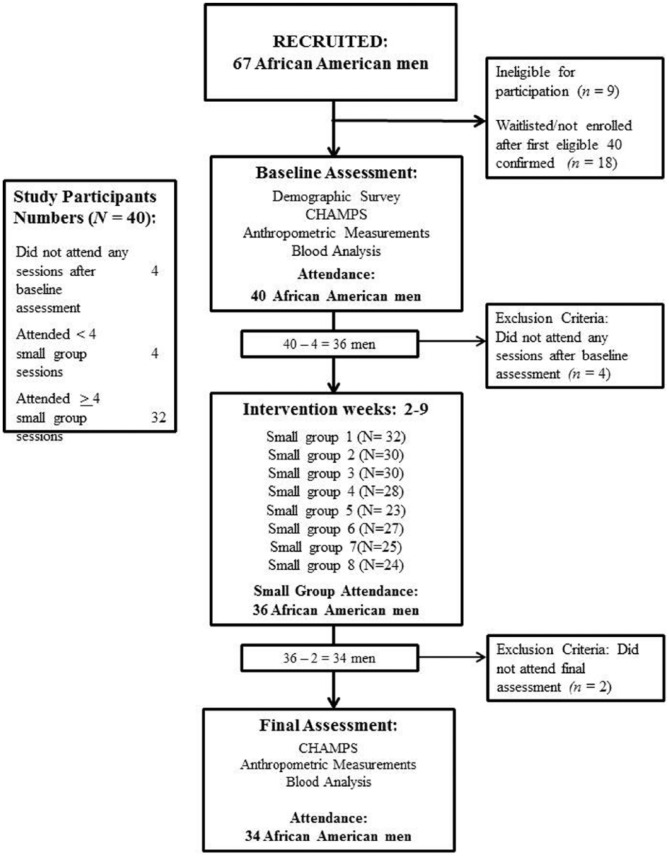
Figure 1 is the consort form documenting participant flow through this intervention. During the recruitment period (June 18-July 29, 2014), 67 men expressed interest in this study. Among the recruited sample, 9 men (13%) were ineligible to participate because they were not in the specified age range or they regularly used a gym membership. The first 40 eligible men consented to participate and were enrolled in the study. Of the 40 men enrolled, 4 participants did not attend any sessions after the baseline assessment, and 2 additional participants did not attend the final assessment. In total, 34 participants (85%) completed the study. Eighty percent of enrolled men participated in at least half of the small group sessions, and attendance across all eight small group sessions ranged from 58% to 80% (Mean = 68 ± 8%).
Figure 1.
Diagram of participant flow through Men on the Move−Nashville pilot intervention.
Note. CHAMPS = Community Healthy Activities Model Program for Seniors.
Intervention Acceptability
Overall, participants felt they benefited from Men on the Move–Nashville in multiple ways. They shared how each component helped increase their motivation to engage in physical activity and offered suggestions as well.
Small Group Sessions
The men enjoyed the camaraderie and support they received from their small group. For example, one participant noted, “[Men on the Move–Nashville] helped establish friendships and brotherhood, so I think this has been a fantastic opportunity to make friends to have people that you’re accountable to.” Men reported that they learned from and supported one another with strategies to overcome barriers to physical activity.
One of the real good things for me with the group I was in . . . because we talked about it, all the guys knew my pains. Everything I’ve gone through. They were pushing me. They would wait for me. When we had to run the blocks, a couple of them would wait on me. They would encourage me. “Man, I’m not doing this.” But they would push me. And I made it every time. That was a great thing; guys you don’t know were pushing me like that. That was a great thing for me. I really enjoyed that.
A few men also mentioned they wanted to see more group goal setting and competition within and between groups. One participant recommended, “Just because it’s guys, having a group goal would even work. ‘Hey, collectively before we meet again. I need you guys to do this.’ [Have] the trainer set expectations for the group.” In addition, men suggested “if they [the trainers] gave a workout goal sheet for the week, ‘Okay you worked out on Saturday. Over the next six days after this, you should do these things at the minimum.’” Another said, “I like the t-shirts, I like the groups, but I would like to have seen more competition.”
Fitbit Use
Throughout the program, men were encouraged to wear their activity tracker to help them monitor their physical activity progress. Some men either lost this device or experienced technological challenges operating and syncing their Fitbit Flex to their mobile device or computer. As a result, only 28 of the 40 men (70%) consistently wore their working device. An independent t test was conducted to compare ages of men who used their activity tracker with men who did not. Table 3 highlights these findings. There was a significant difference in age of Fitbit users compared with Fitbit nonusers, t(1) = 2.10; p < .05. Participants who successfully set up and used their activity tracker were on average 7 years younger than those who did not use their activity tracker. To that end, men shared both barriers and benefits to using the Fitbit.
Table 3.
Mean Age by Fitbit User Status of Men on the Move Participants (n = 40).
| n | Mean age (years) | SD | t | p | |
|---|---|---|---|---|---|
| Fitbit usage | 2.10 | .043 | |||
| Fitbit non-user | 12 | 51.7 | 9.820 | ||
| Fitbit user | 28 | 44.9 | 9.162 |
Some men noted they had technical difficulties with setup, “The Fitbit tracker I’ve got [has] pros and cons. I’ve had to reset it and send it in. It was great when it was working. If they can get the kinks out, that would be great.” Anecdotally, some men shared throughout the program that their Fitbit Flex would fall off, and they suggested having activity trackers that included watch-like clasps to help prevent Fitbit loss.
Several men shared how they were able to use the device to connect with their group and other individuals in their sphere of influence. One said, “I knew nothing about Fitbit before this. Once I started using it, it rocked my world. I was connected with people and networking through it. Being motivated and motivating other people. To me, it was a selling point.”
Participants also offered suggestions for incorporating this activity tracker with other intervention components. In particular, some wanted the Fitbit to be integrated into the small group sessions. One participant recommended,
Bring the Fitbit® into the actual work-out. We did it amongst ourselves during the week. “Hey, you gotta get more steps than that.” or “Hey, I beat you this week.” And we were competing within our group. But the trainer was not a part of that. It was not a part of the structure, but it easily could be with this [Fitbit®] device.
SMS Text Messaging
Participant feedback also included discussions around the SMS text messages. A few were initially leery about receiving text messages, but the overwhelming majority responded favorably to receiving SMS text messages. One participant shared, “Initially, I was skeptical. I thought it was corny. I said naw, I’m not interested in that, but it was a part of the program so I’ll do it.” Another noted that the messages were timely and the content was appropriate. Regarding the appropriateness of messages, one participant said:
It felt eerie. I’m saying it in a good way, because of how appropriate the messages were. Specifically, there was one time where I was debating if I should change my walking route. And I got a text message about not being afraid to try new things, and to change it up.
Men saw these messages as key reminders and sources of motivation to stay active during the week.
Gym Memberships
While men liked the idea of having a gym membership, many who provided comments about this component felt the regional centers were not conveniently located and had limited hours. In addition, men noted that they would have been more likely to utilize the gym facilities with a workout partner. For example, one man stated,
I could have made time, but I would have if I had someone near me that said, hey I’m going. I could have made time, but like I said, I was by myself, so I was like, I’ll just run around my complex at home. . . . So connecting with all the groups, finding out who lives near you. I could have linked up with some of you [men in the focus group] as soon as my group ended; I just didn’t know anyone that lived near me.
As a result, only 30% of participants utilized their fitness facility 3-month membership to the regional centers; the number of visits ranged from 1 to 13 times.
Physical Activity Changes
Table 4 reports values for self-reported physical activity measures at baseline and final sessions. In Table 5, the same physical activity measures are shown only for men who participated in four or more (at least 50%) of the small group sessions. Significant (p < .05) increases in total minutes of physical activity for every physical activity category (i.e., all physical activity, moderate to vigorous, vigorous, and sports) were identified. Similarly, caloric expenditure per week improved significantly (p < .05). There were moderate Cohen’s effect sizes across all physical activity categories for all participants who completed the baseline and final assessment values (d = −.467 to −.780). Similar, but slightly larger Cohen’s effect sizes for changes in caloric expenditure and weekly minutes in all physical activity categories were identified for participants who completed four or small group sessions (d = −.508 to −.874).
Table 4.
Change in CHAMPS Physical Activity Measures (Baseline to Final Assessments) for Men on the Move–Nashville Participants (n = 34).
| Outcome measure | Baseline assessment |
Final assessment |
t | p | Effect size (d) | r |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||||
| Total minutes of physical activity/week | ||||||
| All physical activity | 640.15 (419.04) | 981.62 (598.15) | 3.04 | .005 | .671 | .210 |
| Moderate-to-vigorous physical activity | 367.50 (248.90) | 616.76 (421.94) | 3.39 | .002 | .743 | .267 |
| Vigorous physical activity | 87.35 (99.60) | 159.26 (173.13) | 2.88 | .007 | .527 | .540* |
| Sports | 330.00 (327.34) | 632.65 (448.90) | 3.80 | .001 | .780 | .318 |
| Caloric expenditure/week (Kcal/week) | ||||||
| All physical activity | 4243.63 (3001.86) | 6637.76 (4240.72) | 3.25 | .003 | .661 | .334 |
| Moderate-to-vigorous physical activity | 2968.23 (2178.37) | 4908.29 (3707.98) | 3.22 | .003 | .659 | .379* |
| Vigorous physical activity | 1072.49 (1258.25) | 1849.48 (2071.64) | 2.84 | .008 | .467 | .638* |
| Sports | 2538.06 (2564.20) | 4507.02 (3385.61) | 3.59 | .001 | .662 | .451* |
Note. CHAMPS = Community Healthy Activities Model Program for Seniors. Paired t tests, effect sizes (Cohen’s d), and correlations (r) limited to participants with baseline and final assessment data for each outcome.
p < .05.
Table 5.
Change in CHAMPS Physical Activity Measures (Baseline to Final Assessments) for Men on the Move–Nashville Participants who Attended at Least 50% of Small Group Sessions.
| Outcome measure (n = 31) | Baseline assessment |
Final assessment |
t | p | Effect size (d) | r |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||||
| Total minutes of physical activity/week | ||||||
| All physical activity | 642.58 (426.03) | 1032.58 (597.40) | 3.28 | .003 | .762 | .199 |
| Moderate-to-vigorous physical activity | 370.65 (249.90) | 655.16 (419.63) | 3.70 | .001 | .850 | .261 |
| Vigorous physical activity | 89.03 (103.12) | 169.35 (177.74) | 2.98 | .006 | .572 | .538* |
| Sports | 325.16 (331.26) | 667.26 (451.50) | 4.12 | <.001 | .874 | .332 |
| Caloric expenditure/week (Kcal/week) | ||||||
| All physical activity | 4113.70 (2752.52) | 6887.67 (4275.64) | 3.65 | .001 | .789 | .336 |
| Moderate-to-vigorous physical activity | 2870.95 (1975.32) | 5126.33 (3770.13) | 3.65 | .001 | .785 | .419* |
| Vigorous physical activity | 1071.85 (1297.38) | 1943.91 (2138.98) | 2.96 | .006 | .508 | .642* |
| Sports | 2373.58 (2345.59) | 4655.32 (3449.75) | 4.12 | <.001 | .787 | .488* |
Note. CHAMPS = Community Healthy Activities Model Program for Seniors. Paired t tests, effect sizes (Cohen’s d), and correlations (r) limited to participants with baseline and final assessment data for each outcome.
p < .05.
Physiological Changes
Table 6 presents baseline and final assessment data for physiological outcomes including weight, BMI, and glucose levels. Significant weight loss from the baseline to final assessment was observed (t(33) = 2.86, p < .05, d = .052); participants lost an average of 2.93 pounds. Additionally, body fat percentage decreased by an average of 1.2% from the baseline to final assessment (t(33) = 2.63, p < .05, d = .175). HDL cholesterol levels improved from 41.25 mg/dl to 43.74 mg/dl(t(33) = 3.31, p < .001, d = .338). Small, but statistically insignificant decreases in BMI, waist circumference and glucose levels at week 10 were identified, which given the sample size, is noteworthy.
Table 6.
Change in Physiological Measures (Baseline to Final Assessments) for Men on the Move–Nashville Participants (n = 34).
| Outcome measure | Baseline assessment |
Final assessment |
t | p | Effect size (d) | r |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||||
| Weight (lbs.) | 242.15 (57.19) | 239.22 (55.89) | 2.86 | .007 | .052 | .995* |
| BMI | 34.58 (7.89) | 34.49 (8.43) | 0.23 | .818 | .011 | .963* |
| Waist circumference | 41.12 (5.78) | 40.97 (6.64) | 0.29 | .776 | .024 | .893* |
| Body fat percentage | 31.52 (7.03) | 30.31 (6.72) | 2.63 | .013 | .175 | .927* |
| Glucose | 112.53 (35.72) | 106.47 (35.31) | 1.30 | .202 | .171 | .708* |
| Total cholesterol | 192.97 (30.54) | 189.97 (28.27) | 0.88 | .386 | .102 | .774* |
| HDL level | 40.26 (9.77) | 43.74 (10.76) | 3.31 | .002 | .338 | .827* |
Note. BMI = body mass index; HDL = high-density lipoprotein. Paired t tests, effect sizes (Cohen’s d), and correlations (r) limited to participants with baseline and final assessment data for each outcome.
p < .05.
Table 7 reports mean changes just for men who attended at least 50% of the small group sessions. Similar to the results in Table 6, there were significant decreases in weight (t(30) = 2.20, p < .05, d = .047) and body fat percentage(t(30) = 2.31, p < .05, d = .198). Marked improvement in HDL cholesterol levels were also observed in this subsample (t(30) = 5.07, p < .001, d = .415).
Table 7.
Change in Physiological Measures (Baseline to Final Assessments) for Men on the Move–Nashville Participants Who Attended at Least 50% of Small Group Sessions (n = 31).
| Outcome measure | Baseline assessment |
Final assessment |
t | p | Effect size (d) | r |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||||
| Weight (lbs.) | 239.23 (49.73) | 236.94 (49.03) | 2.20 | .036 | .047 | .993* |
| BMI | 34.02 (6.11) | 34.07 (7.07) | −0.10 | .922 | −.006 | −.947* |
| Waist circumference | 41.03 (5.20) | 40.65 (5.99) | 0.72 | .478 | .069 | .866* |
| Body fat percentage | 31.32 (6.13) | 30.16 (5.58) | 2.31 | .028 | .198 | .894* |
| Glucose | 113.23 (36.09) | 106.90 (36.95) | 1.32 | .196 | .173 | .734* |
| Total cholesterol | 193.26 (31.78) | 191.94 (28.01) | 0.39 | .700 | .044 | .807* |
| HDL level | 39.84 (10.09) | 44.19 (10.88) | 5.07 | <.001 | .415 | .899* |
Note. BMI = body mass index; HDL = high-density lipoprotein. Paired t tests, effect sizes (Cohen’s d), and correlations (r) limited to participants with baseline and final assessment data for each outcome.
p < .05.
Effect of Small Group Attendance
Simple linear regressions were conducted to assess the influence of small group attendance on changes in physical activity, weight, body fat percentage, and HDL cholesterol. Table 8 reports the significant regression model for changes in HDL cholesterol on, F(1, 32) = 4.18; p = .049, where small group attendance accounted for 11.6% of the variability in the change in HDL cholesterol. Participants’ predicted change in HDL cholesterol is equal to −3.902 + 1.18(number of small groups attended). There were nonsignificant effects of small group attendance on changes in weekly minutes of physical activity, caloric expenditure of physical activity, weight, and body fat percentage.
Table 8.
Effect of Small Group Attendance on Change in HDL Cholesterol.
| Independent variable | Slope |
|---|---|
| No. of small groups attended | 1.18* |
| Constant | −3.902 |
| R 2 | .116 |
| N | 34 |
Note. HDL = high-density lipoprotein.
p < .05.
Discussion
Men on the Move–Nashville was a pilot physical activity intervention for overweight and obese African American men ages 30 to 70. The goal of this study was to assess the feasibility and acceptability of this technology-enhanced small group intervention. Eighty-five percent of men completed the program, and 80% attended at least half of the small group sessions. This study is one of few, if not the only published, interventions targeting African American men that included both a physical activity training component and a didactic component in the small group sessions. This study also was novel in that it was the first to our knowledge to test SMS text messaging and wearable, self-monitoring physical activity trackers with this population, and one of few that have used anthropometric data to assess changes in health outcomes. Additionally, this pilot intervention included gym memberships to increase physical activity outside small group sessions, which was a specific limitation in the previous Men on the Move program (Griffith et al., 2014).
Participants were provided with gym memberships in this pilot study to facilitate engaging in physical activity outside of their small group session. While men appreciated having the gym memberships, consistent with previous research (Griffith et al., 2013), they noted that they were more interested in building a support system of men who they could workout with at the gym facilities. At baseline, 25% of men indicated they owned a gym membership before starting the program. Thus, some men may have utilized other gyms instead of the community center facilities in this study. Regardless, while men appreciated receiving the memberships, based on attendance data from the facilities, the memberships went largely unused. Some men noted that the distance and time it would take to get to these exercise facilities were barriers to utilization. Consistent with previous studies (Griffith et al., 2014; Hooker et al., 2011), these findings suggest that facilitating financial access to exercise facilities may be important. However, these findings also highlight the importance of making sure that these exercise locations are geographically accessible. Future studies should explore the best ways to increase accessibility of places for men to be physically active.
One way physical activity interventions have sought to facilitate social support to promote physical activity is by including small groups in behavioral interventions with men (George et al., 2012). Similar to previous studies that have used small groups to promote physical activity in African American men (Griffith et al., 2014; Hooker et al., 2011; Treadwell et al., 2010), men in this study discussed how important it was for them to participate in the small group sessions. Men reported that the sessions helped build camaraderie with other group members and identify strategies to help them overcome time and other unique barriers to physical activity.
While small groups have been a key component of previous physical activity interventions with men, very few group-based physical activity interventions included both the didactic and workout component together; most interventions only include one of these components in their small group sessions (George et al., 2012; Kassavou et al., 2013; Newton et al., 2014). The findings from this study suggest that the strategy of including both the physical activity training and didactic components together is promising. The two part sessions appeared to be advantageous to establish social connections from the beginning as men fostered relationships through sharing experiences with physical activity during discussions. Men used this knowledge to encourage and motivate other group members. Men enjoyed having structured opportunities to discuss goals, barriers, and facilitators and engage in physical activity with the same men in their group. Having these discussions appeared to help facilitate connections, build trust, and increase socialization for the group; the didactic portion seemed to make it easier for men to build such networks. It is also possible that the men enjoyed the activity and, as opposed to models that just include the didactic portion, found tangible benefit to participate in the sessions for the activity alone. Future research should explore how these components can be maximized to promote physical activity and health among African American men.
In this intervention, caloric expenditure and total average weekly minutes in all categories of physical activity significantly increased. Since the average self-reported weekly minutes of physical activity at final assessment was more than the minutes spent in the small group session, it can be inferred that men were active both during and outside of their small group session. This was a limitation of the previous version of Men on the Move, whose findings suggested that the increase in physical activity was primarily due to their participation in the small group session (Griffith et al., 2014). More research is needed to assess the independent and added value of including the didactic and exercise components within the small group session.
In addition to the increase in reported physical activity, significant improvements in weight, body fat percentage, and HDL cholesterol level were observed for men who completed baseline and final assessments and for the subset of men who attended four or more small group sessions. The small to moderate effect sizes in these physical activity and physiological changes after 8 weeks of small group sessions provide solid evidence that a main study with elements from this pilot study is warranted. The slightly larger effect sizes for physical activity changes among men who completed four or more of the small group sessions suggest that there may be greater benefit in attending at least half of small group sessions.
Of the few physical activity interventions that specifically targeted African American men (Treadwell, et al., 2010; Griffith et al, 2014, Hooker, et al., 2011) or that targeted men of other racial or ethnic groups (George, et al., 2012), this is the first to our knowledge that used SMS text messaging and physical activity trackers to enhance the effectiveness of a physical activity intervention. In addition to being used as objective outcome evaluation tools, these devices help facilitate self-monitoring and social connectedness (Kirwan et al., 2012). Future studies should continue to utilize these tools and explore how they can mediate the effectiveness of physical activity and weight loss interventions.
Findings from this study suggest that African American men are open to receiving SMS text messaging and using a wearable physical activity tracker. Participants responded positively to receiving SMS text messages. They thought the timing and frequency of receiving three messages per week was adequate and appropriate. Despite some mechanical and technological challenges, most consistently wore the activity tracker. Unsurprisingly, however, men at the older end of the age range experienced more difficulty operating wearable device than men who were younger. In addition, one of the underutilized features of the self-monitoring Fitbit devices was the social connectivity platform to facilitate social support and accountability as well as healthy competition among individuals and groups. Integrating this feature and the activity tracker into the small group sessions may further help men reach their goals and increase their motivation to exercise outside of the small group setting. More studies should explore how best to maximize these technological features.
Limitations
Although this study provides promising results to the benefits of a technology-enhanced physical activity program, there were limitations in the study design, measures used, and usability of technological components that should be addressed in a fully powered randomized controlled trial. First, this was a nonrandomized study with no control group; thus, the findings from this study may not be generalizable to other groups. Because this intervention lasted only 10 weeks, it was not designed to see large physiological changes nor was it designed to assess the maintenance of behavior change over time. Despite the brevity of this intervention, positive changes in physiological outcomes were still identified, which is consistent with the notion that even small changes in physical activity can begin to make a difference in health (National Heart, Lung, and Blood Institute, 2011). This study used a self-report measure as the primary method of assessing physical activity changes; future studies should aim to include an objective measure of physical activity to reduce the risk of bias (Newton et al., 2014). Several men were not able to fully use the Fitbit device because they either lost it or had difficulties operating and syncing their device. More training should be incorporated to help men, particularly those who might not be comfortable with technology, better understand how to fully work such activity trackers. There are now additional versions of the Fitbit and other activity trackers that include watch-like clasps; these types of wearable devices should be utilized in the future to minimize chances of loss. While the small group didactic discussions focused on motivation, changes in motivation were not explicitly tested. Finally, future studies should be designed to tease apart the independent and additive effects of the intervention components to determine which aspects of the intervention are most important.
Conclusions
The findings from this study suggest that middle- and older-aged African American men can respond to and remain interested in the Men on the Move intervention strategy. Furthermore, these findings offer evidence that this is a promising approach to increase physical activity among this population. It is critical to continue to develop and test interventions for populations such as middle- and older-aged African American men given their high rates of premature mortality from chronic diseases are associated with physical inactivity and sedentary lifestyles. It also is important to continue to explore how best to employ gender-specific strategies to improve the health of men of color since they tend to be underrepresented in studies targeting men or populations of color to reduce health disparities. Future research should consider moving beyond these strategies that are targeted to this demographic group to strategies that are tailored to people’s individual needs, preferences, and patterns.
Acknowledgments
We would like to thank Men on the Move–Nashville participants and trainers.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This article was supported in part by grants from the Vanderbilt Ingram Cancer Center (5-P30-CA68485-17), the Aetna Foundation, Inc. (15-0046), NIDDK (7 R21 DK095257-02), NCATS (2UL1TR000445-08), and Vanderbilt University Institute for Research on Men’s Health.
References
- Ainsworth B. E., Haskell W. L., Leon A. S., Jacobs D. R., Jr., Montoye H. J., Sallis J. F., Paffenbarger R. S., Jr. (1993). Compendium of physical activities: Classification of energy costs of human physical activities. Medicine and Science in Sports and Exercise, 25, 71-80. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine, Tharrett S. J., Peterson J. A. (1997). ACSM’s health/fitness facility standards and guidelines (2nd ed.). Champaign, IL: Human Kinetics. [Google Scholar]
- Anderson E. S., Winett R. A., Wojcik J. R. (2007). Self-regulation, self-efficacy, outcome expectations, and social support: Social cognitive theory and nutrition behavior. Annals of Behavioral Medicine, 34, 304-312. [DOI] [PubMed] [Google Scholar]
- Appel L. J., Clark J. M., Yeh H.-C., Wang N.-Y., Coughlin J. W., Daumit G., . . . Brancati F. L. (2011). Comparative effectiveness of weight-loss interventions in clinical practice. New England Journal of Medicine, 365, 1959-1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronson J. (1994). A pragmatic view of thematic analysis. Qualitative Report, 2(1), 1-3. Retrieved from http://nsuworks.nova.edu/tqr/vol2/iss1/3 [Google Scholar]
- Bandura A. (2004). Health promotion by social cognitive means. Health Education & Behavior, 31, 143-164. [DOI] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77-101. [Google Scholar]
- Butryn M. L., Arigo D., Raggio G. A., Colasanti M., Forman E. M. (2016). Enhancing physical activity promotion in midlife women with technology-based self-monitoring and social connectivity: A pilot study. Journal of Health Psychology, 21(8), 1548-1555. [DOI] [PubMed] [Google Scholar]
- Cornish E. K., McKissic S., Dean D. A. L., Griffith D. M. (2017). Lessons learned about motivation from a pilot physical activity intervention for African American men. Health Promotion Practice, 18(1), 102-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig C. L., Marshall A. L., Sjostrom M., Bauman A. E., Booth M. L., Ainsworth B. E., . . . Oja P. (2003). International physical activity questionnaire: 12-Country reliability and validity. Medicine and Science in Sports and Exercise, 35, 1381-1395. doi: 10.1249/01.mss.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- Davidson County Health Department. (2014). Healthy Nashville: 2014. Retrieved from http://www.healthynashville.org/modules.php?op=modload&name=NS-Indicator&file=index&group=category&breakout=all
- Fjeldsoe B. S., Marshall A. L., Miller Y. D. (2009). Behavior change interventions delivered by mobile telephone short-message service. American Journal of Preventive Medicine, 36, 165-173. [DOI] [PubMed] [Google Scholar]
- Fortier M. S., Williams G. C., Sweet S. N., Patrick H. (2009). Self-determination theory: Process models for health behavior change. Emerging Theories in Health Promotion Practice and Research: Strategies for Improving Public Health, 2, 157-183. [Google Scholar]
- George E., Kolt G., Duncan M., Caperchione C., Mummery W. K., Vandelanotte C., . . . Noakes M. (2012). A review of the effectiveness of physical activity interventions for adult males. Sports Medicine, 42, 281-300. [DOI] [PubMed] [Google Scholar]
- Gerber B. S., Stolley M. R., Thompson A. L., Sharp L. K., Fitzgibbon M. L. (2009). Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: A feasibility study. Health Informatics, 15, 17-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D. M., Allen J. O., Johnson-Lawrence V., Langford A. (2014). Men on the move: A pilot program to increase physical activity among African American men. Health Education & Behavior, 41, 164-172. doi: 10.1177/1090198113496788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D. M., Brinkley-Rubinstein L., Thorpe R. J., Jr., Bruce M. A., Metzl J. M. (2015). The interdependence of African American men’s definitions of manhood and health. Family & Community Health, 38, 284-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D. M., Gunter K., Allen J. O. (2011). Male gender role strain as a barrier to African American men’s physical activity. Health Education & Behavior, 38, 482-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D. M., Gunter K., Allen J. O. (2012). A systematic approach to developing contextual, culturally, and gender sensitive interventions for African American men: The example of Men 4 Health. In Elk R., Landrine H. (Eds.), Cancer disparities: Causes and evidence-based solutions (pp. 193-210). New York, NY: Springer. [Google Scholar]
- Griffith D. M., King A. F., Allen J. O. (2013). Male peer influence on African American men’s motivation for physical activity: Men’s and women’s perspectives. American Journal of Men’s Health, 7, 169-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill J. O. (2006). Understanding and addressing the epidemic of obesity: An energy balance perspective. Endocrine Reviews, 27, 750-761. [DOI] [PubMed] [Google Scholar]
- Holstad M., DiIorio C., Kelley M., Resnicow K., Sharma S. (2011). Group motivational interviewing to promote adherence to antiretroviral medications and risk reduction behaviors in HIV infected women. AIDS and Behavior, 15, 885-896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooker S. P., Harmon B., Burroughs E. L., Rheaume C. E., Wilcox S. (2011). Exploring the feasibility of a physical activity intervention for midlife African American men. Health Education Research, 26, 732-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlader N. A., Noone A. M., Krapcho M., Neyman N., Aminou R., Waldron W., . . . Edwards B. K. (Eds.). (2010). SEER Cancer Statistics Review, 1975-2008 (Surveillance, Epidemiology, and End Results Program). Retrieved from http://seer.cancer.gov/csr/1975_2008/
- Hull P. C., Reece M. C., Atchison C., Husaini B. A. (2009). Psychosocial and cultural carriers to prostate cancer screening: Racial comparisons. Nashville: Tennessee State University. [Google Scholar]
- International Health, Racquet & Sportsclub Association and Industry Insights, Inc. (2012). IHRSA profiles of success: The annual industry data survey of the health and fitness club industry. Boston, MA: Author. [Google Scholar]
- Israel B. A., McLeroy K. R. (1985). Social networks and social support: Implications for health education: Introduction. Health Education Quarterly, 12, 1-4. [DOI] [PubMed] [Google Scholar]
- Joyner M. J., Nose H. (2009). Physiological regulation linked with physical activity and health. Journal of Physiology, 587, 5525-5526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kannisto K., Koivunen M., Välimäki M. (2014). Use of mobile phone text message reminders in health care services: A narrative literature review. Journal of Medical Internet Research, 16, e222. doi: 10.2196/jmir.3442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassavou A., Turner A., French D. P. (2013). Do interventions to promote walking in groups increase physical activity? A meta-analysis. International Journal of Behavioral Nutrition and Physical Activity, 10(1), 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan N. L., Shaw K. M. (2011). Coronary heart disease and stroke deaths: United States, 2006. Morbidity and Mortality Weekly Report, 60, 62-66. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/su6001a13.htm [PubMed] [Google Scholar]
- King A. B., Ahn D. K., Oliveira B. M., Atienza A. A., Castro C. M., Gardner C. D. (2008). Promoting physical activity through hand-held computer technology. American Journal of Preventive Medicine, 2, 138-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirwan M., Duncan M. J., Vandelanotte C., Mummery W. K. (2012). Using smartphone technology to monitor physical activity in the 10,000 steps program: A matched case-control trial. Journal of Medical Internet Research, 14, e55. doi: 10.2196/jmir.1950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langford A. T., Griffith D. M., Beasley D. D., Braxton E. I.-D. (2014). A cancer center’s approach to engaging African American men about cancer: The men’s fellowship breakfast, Southeastern Michigan, 2008–2014. Preventing Chronic Disease, 11, 140187. doi: 10.5888/pcd11.140187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahalik J. R., Burns S. M., Syzdek M. (2007). Masculinity and perceived normative health behaviors as predictors of men’s health behaviors. Social Science & Medicine, 64, 2201-2209. [DOI] [PubMed] [Google Scholar]
- McLeroy K. R., Bibeau D., Steckler A., Glanz K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15, 351-377. [DOI] [PubMed] [Google Scholar]
- Mohr D. C., Burns M. N., Schueller S. M., Clarke G., Klinkman M. (2010). Behavioral intervention technologies: Evidence review and recommendations for future research. General Hospital Psychiatry, 35, 332-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Heart, Lung, and Institute Blood. (2011). Recommendations for physical activity. Bethesda, MD: Author. [Google Scholar]
- Newton R. L., Jr., Griffith D. M., Kearney W., Bennett G. G. (2014). A systematic review of physical activity, dietary, and weight loss interventions involving African American men. Obesity Reviews, 15(Suppl. S4), 93-106. [DOI] [PubMed] [Google Scholar]
- Peng F., Li Y., Bauer A. M. (2013). Life expectancy in Tennessee: 2009-2011. Retrieved from https://www.tn.gov/assets/entities/health/attachments/Life_Expectancy_in_Tennessee_2009_to_2011.pdf
- Resnicow K., Baranowski T., Ahluwalia J. S., Braithwaite R. L. (1999). Cultural sensitivity in public health: Defined and demystified. Ethnicity & Disease, 9(1), 10-21. [PubMed] [Google Scholar]
- Resnicow K., Davis R., Zhang G., Konkel J., Strecher V., Shaikh A., . . . Wiese C. (2008). Tailoring a Fruit and Vegetable Intervention on Novel Motivational Constructs: Results of a Randomized Study. Annals of Behavioral Medicine, 35(2), 159-169. [DOI] [PubMed] [Google Scholar]
- Resnicow K., Jackson A., Braithwaite R., DiIorio C., Blisset D., Rahotep S., Periasamy S. (2002). Healthy body/healthy spirit: A church-based nutrition and physical activity intervention. Health Education Research, 17, 562-573. [DOI] [PubMed] [Google Scholar]
- Resnicow K., McCarty F., Blissett D., Wang T., Heitzler C., Lee R. E. (2003). Validity of a modified CHAMPS physical activity questionnaire among African-Americans. Medicine and Science in Sports and Exercise, 35, 1537-1545. [DOI] [PubMed] [Google Scholar]
- Ryan R. M., Frederick C. M., Lepes D., Rubio N., Sheldon K. M. (1997). Intrinsic motivation and exercise adherence. International Journal of Sport Psychology, 28, 335-354. [Google Scholar]
- Stewart A. L., Mills K. M., King A. C., Haskell W. L., Gillis D., Ritter P. L. (2001). CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Medicine and Science in Sports and Exercise, 33, 1126-1141. [DOI] [PubMed] [Google Scholar]
- Thabane L., Mal J., Chu R., Cheng J., Ismaila A., Rios L. P., . . . Goldsmith C. H. (2010). A tutorial on pilot studies: The what, why and how. BMC Medical Research Methodology, 10(1). Retrieved from https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe R. J., Jr., Wilson-Frederick S., Bowie J. V., Coa K., Clay O., LaVeist T. A., Whitfield K. E. (2013). Health behaviors and all-cause mortality in African American men. American Journal of Men’s Health, 7(4 Suppl.), 8s-18s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treadwell H., Holden K., Hubbard R., Harper F., Wright F., Ferrer M., . . . Kim E. K. (2010). Addressing obesity and diabetes among African American men: Examination of a community-based model of prevention. Journal of the National Medical Association, 102, 794-802. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2010). American Community Survey 2005-2009 estimates. Washington, DC: Author. [Google Scholar]
- Warner D. F., Hayward M. D. (2006). Early-life origins of the race gap in men’s mortality. Journal of Health & Social Behavior, 47, 209-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitt-Glover M. C., Keith N. R., Ceaser T. G., Virgil K., Ledford L., Hasson R. E. (2014). A systematic review of physical activity interventions among African American adults: Evidence from 2009 to 2013. Obesity Reviews, 15, 125-145. [DOI] [PubMed] [Google Scholar]
- Whitt-Glover M. C., Kumanyika S. K. (2009). Systematic review of interventions to increase physical activity and physical fitness in African-Americans. American Journal of Health Promotion, 23, S33-S56. [DOI] [PubMed] [Google Scholar]
- Wong J. Y. L., Gilson N. D., van Uffelen J. G. Z., Brown W. J. (2012). The effects of workplace physical activity interventions in men: A systematic review. American Journal of Men’s Health, 6, 303-313. [DOI] [PubMed] [Google Scholar]