Abstract
Background
Refinement of parameters defining prostate cancer (PC) prognosis are urgently needed to identify patients with indolent versus aggressive disease. The Canadian Prostate Cancer Biomaker Network (CPCBN) consists of researchers from four Canadian provinces to create a validation cohort to address issues dealing with PC diagnosis and management.
Methods
A total of 1512 radical prostatectomy (RP) specimens from five different biorepositories affiliated with teaching hospitals were selected to constitute the cohort. Tumoral and adjacent benign tissues were arrayed on tissue microarrays (TMAs). A patient clinical database was developed and includes data on diagnosis, treatment and clinical outcome.
Results
Mean age at diagnosis of patients in the cohort was 61 years. Of these patients, 31% had a low grade (≤6) Gleason score (GS), 55% had GS 7 (40% of 3 + 4 and 15% of 4 + 3) and 14% had high GS (≥8) PC. The median follow-up of the cohort was 113 months. A total of 34% had a biochemical relapse, 4% developed bone metastasis and 3% of patients died from PC while 9% died of other causes. Pathological review of the TMAs confirmed the presence of tumor and benign tissue cores for > 94% of patients. Immunohistochemistry and FISH analyses, performed on a small set of specimens, showed high quality results and no biorepository-specific bias.
Conclusions
The CPCBN RP cohort is representative of real world PC disease observed in the Canadian population. The frequency of biochemical relapse and bone metastasis as events allows for a precise assessment of the prognostic value of biomarkers. This resource is available, in a step-wise manner, for researchers who intend to validate prognostic biomarkers in PC. Combining multiple biomarkers with clinical and pathologic parameters that are predictive of outcome will aid in clinical decision-making for patients treated for PC.
Electronic supplementary material
The online version of this article (10.1186/s12894-018-0392-x) contains supplementary material, which is available to authorized users.
Keywords: Prostate cancer, Tissue microarray, Biomarker validation, Immunohistochemistry, Patient prognosis
Background
The inability to clearly distinguish indolent versus aggressive disease is a major challenge for physicians caring for patients with prostate cancer (PC) [1]. Patients are stratified into groups ranging from very low to very high risk based on prostate-specific antigen (PSA) levels at time of diagnosis, tumor Gleason score (GS) in biopsies, and tumor stage at clinical presentation [2–4]. However, the biology of PC reflects a multifocal and multiclonal nature of tumors that is far more complex than initial predictions from current clinical parameters [5–7].
Foremost, the prognostic ability of new biomarkers should determine the risk for lethal PC and track disease progression in order for the therapy to be modified [2]. Several emerging biomarker candidates have been described; none so far have been fully validated or robust enough to be added to clinical parameters used in practice. Tissue microarrays (TMAs) represent a high-throughput platform to apply protein- and nucleotide-based assays enabling biomarker testing within a single tumor core [3] of hundreds of patient samples simultaneously [8]. Current strategies aspire to multiplex approaches combining current clinical parameters with a comprehensive panel of biomarkers to improve diagnostic accuracy of disease status and resolve the heterogeneity that confounds risk stratification in PC [2].
The Canadian Prostate Cancer Biomarker Network (CPCBN) represents a community of clinicians and researchers that is committed to improving the clinical management of PC. The CPCBN initiative is a validation rather than discovery platform and invites biomarker proposals from all researchers with preliminary evidence demonstrating their utility in PC management. An application to access the TMA platform is available on the CPCBN website, along with details on the CPCBN program and affiliated partners http://www.tfri.ca/en/research/translational-research/cpcbn.aspx). A compilation of potential biomarkers has already been reviewed and studies are underway using the radical prostatectomy (RP) cohort. Data for well-known PC biomarkers such as ERG, PTEN, Ki67 and AR will be available to researchers upon request. This platform serves as an invaluable resource for the entire PC research community, accelerating breakthroughs in PC research, and supporting the establishment of nomograms to predict patient progression.
In this study, we report a TMA-based validation process which includes assembly of a retrospective multi-center RP cohort to build TMAs that will evaluate both biomarkers and their utility in identifying patients at high risk for biochemical recurrence (BCR) and the development of metastases or PC-specific mortality. To ensure homogeneity across sites, we used the Canadian Tumor Repository Network (CTRNet, www.ctrnet.ca) standards for quality assurance and developed standard operating procedures (SOPs). We also report on the quality control of this RP TMA series with quality assessments and controls, focusing on the TMA suitability for immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH) techniques.
Methods
Patient cohort and participating centers
RP specimens were selected from five different biobanks affiliated with academic health care centers across Canada: Centre hospitalier de l’Université de Montréal (CHUM), CHU de Québec-Université Laval (CHUdeQ-UL), McGill University Health Centre (MUHC), Vancouver Prostate Centre (VPC), and University Health Network (UHN). The selected specimens were biobanked between 1990 and 2011. All patients signed an informed consent to participate within one of the above listed biobanks and agreed to the use of their specimens and data for research purposes. Inclusion criteria included: RP specimens archived as formalin-fixed paraffin-embedded (FFPE) blocks, treatment (hormone or chemotherapy) naïve patients with a minimum follow-up of 24 months. Patients with severe comorbidity were naturally excluded as they are not candidates for RP surgery. Each center received ethical approval from their Institutional Review Board (IRB) for biobanking activity and for their contributions to the CPCBN. CTRNet standards were followed for quality assurance and ensured appropriate handling of human tissue.
Clinical data management
Clinical data for each patient were collated into an Advanced Tissue Management (ATiM) database developed by the CTRNet and customized for the CPCBN. Complete clinical data provided the month and year of diagnosis and surgery, age, pretreatment PSA level, pathologic stage, Gleason grade, margin status, date of BCR, PSA progression, development of metastasis, and treatments received following RP when applicable. BCR endpoints were based on serum PSA measurement in three different conditions: PSA levels of 0.2 ng/mL and rising, a PSA level followed by salvage/adjuvant treatment and finally, when initial post-operative PSA levels were greater than 0.2 ng/mL and rising following surgery (failed RP). Appearance of bone metastasis and PC mortality were considered ultimate endpoints.
TMA construction
TMA construction was performed at each site: CHUM, UHN, and VPC used the TMArrayer (Pathology Devices, Inc., Westminster, MD, USA), while the CHUdeQ-UL and MUHC used the manual tissue arrayer, MTA-1 (Beecher Instruments, WI, USA). A pathologist selected the FFPE block, and the area of interest (tumor or adjacent benign) was circled directly onto the hematoxylin and eosin (H&E) stained slide. Cores of 0.6 mm were extracted from the corresponding FFPE block and arrayed on a receiver paraffin block. A SOP was developed and guided the construction of the different TMA series.
TMA design
To build the quality control TMA (QC-TMA), a TMA block was circulated across four sites where three tumor cores from 10 PC specimens were arrayed to evaluate the feasibility of the multi-center resource. Due to specific institution requirements, one site arrayed their specimens on a separate TMA, resulting in two QC-TMA blocks. However, sections were combined onto the same glass slide for subsequent analyses. The optimization TMA (OPT-TMA) was constructed at the CHUM and included banked tissues from 15 RP, 5 breast cancer and 5 ovarian cancer cases along with mouse xenograft tissues derived from human PC cell lines 22RV1, LNCaP, DU145 and PC3. The Test-TMA series was composed of 250 RP specimens selected from four biobanks: CHUM, MUHC, CHUdeQ-UL (50 RP specimens each), and VPC (100 RP specimens). Each TMA block contained three cores of tumor and two cores of adjacent benign tissues from 50 RP cases. The Validation-TMA series contain prostate tissues from 1262 specimens across five centers. Three to four cores of tumor and one to two cores of adjacent benign tissues were arrayed on receiver blocks. Validation-TMAs also contained 50 RP cases per block with a few exceptions. On each TMA block composing the test or the validation series, two cores of the 4 PC cell line-derived xenografts used for the OPT-TMA were also included. After a first pathology review, cores were repunched as necessary and resulted in a total of seven TMA blocks for the Test-TMA and 31 TMA blocks for the Validation-TMA series.
IHC staining and analysis
Tissue quality was assessed with the following markers: PSMA, PSA, p63, P504s, P501s, Ki67, AR, CK18, and HMW-CK. Details about antibody sources, dilutions, antigen retrieval and incubation conditions are described in Additional file 1. QC-TMA slides were stained at the coordinating center (CHUM) using the BenchMark XT automated stainer (Ventana Medical System Inc.). TMA slides were scanned and assessed visually for analysis (OlyVIA, Olympus, ON, Canada). Two independent observers blindly scored the percentage of stained cells for all markers except for PSA and CK18 where the intensity of staining was also evaluated.
FISH analysis
The PTEN FISH probe consisting in a four-color probe combination detecting PTEN, WAPAL, FAS and CEP 10, was obtained from CymoGenDx/Biocare Medical (Concord, CA) and was used as previously described [9]. The pathologist selected areas of TMA sections stained with DAPI, which were analyzed against immediately adjacent sections stained with H&E. PTEN copy number was determined by counting signals of all four markers in 50–100 distinct and intact interphase nuclei per tumor core using SemRock filters selected for excitation/emission spectra of each probe. Cores that showed visible deletions were scored by reviewing 50 cells per core. Hemizygous (single copy) PTEN deletion denoted cores with 50% of nuclei exhibiting clonal loss of PTEN whereas homozygous PTEN deletion was assigned to cores with loss of both PTEN loci in 30% of nuclei.
Central pathology review
Central pathology review assessed RP specimens of the QC-TMA, Test-TMA and Validation-TMA series. Scoring criteria included GS, the amount of glandular tissue present, and specificity of the core nature in terms of adjacent benign, cancer, prostatic intraepithelial neoplasia (PIN), intraductal carcinoma (IDC), atypical small acinar proliferation (ASAP), stroma, muscle or inflammation [10]. Upon review, cores were qualified as informative if the specific tissue of interest (adjacent benign or cancer) was present in at least 5 to 10% of the core area. Additional cores were requested for replacement if less than two cores for either tumor or adjacent benign tissues did not meet established criteria. Replacement cores were reviewed and added to a new or existing array, and if tissue samples were depleted, additional cores or patients were included to complete the full cohort.
Statistical analyses
Hierarchical clustering analysis of markers assessed in the QC-TMA was performed with Genespring software (Agilent Genomics, CA, USA) using Pearson correlation as a similarity measure and an average linkage-clustering algorithm. Survival analyses (Cox regression and Kaplan-Meier curves) were performed using the IBM SPSS Statistics (Version 23) software.
Results
Feasibility of the multi-center TMA-based resource
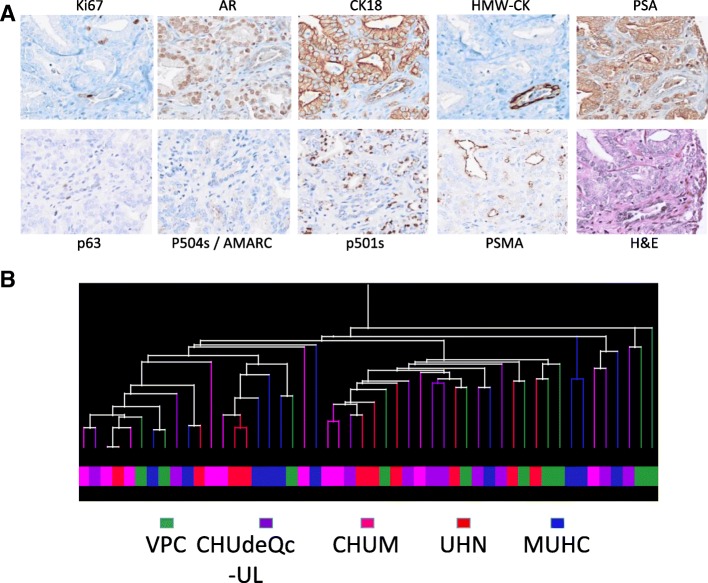
A quality control TMA (QC-TMA) was constructed (Fig. 1, left column) using three cores from 10 PC specimens with GS 7 from each of the five biorepositories. The 150 cores composing this array were evaluated for tissue integrity, antigenicity, and performance in protein and nucleic acid-based assays. These cores were tumors of expected Gleason grade (in at least 2/3 cores) in 94% (47/50) of samples. Tissue integrity and antigenicity was determined by evaluation of the expression of nine different markers with nuclear and/or cytoplasmic localization (Ki67, AR, CK18) in addition to markers that distinguish tumor vs. benign glands (HMW-CK, p63, and P504S/AMACR) or proteins usually expressed by prostate cells (PSA, P501S and PSMA) (Fig. 2a). Hierarchal clustering using a Pearson centered distance metric was based on the detection of these nine markers. Hierarchal clustering demonstrated that there was no site-specific bias (Fig. 2b).
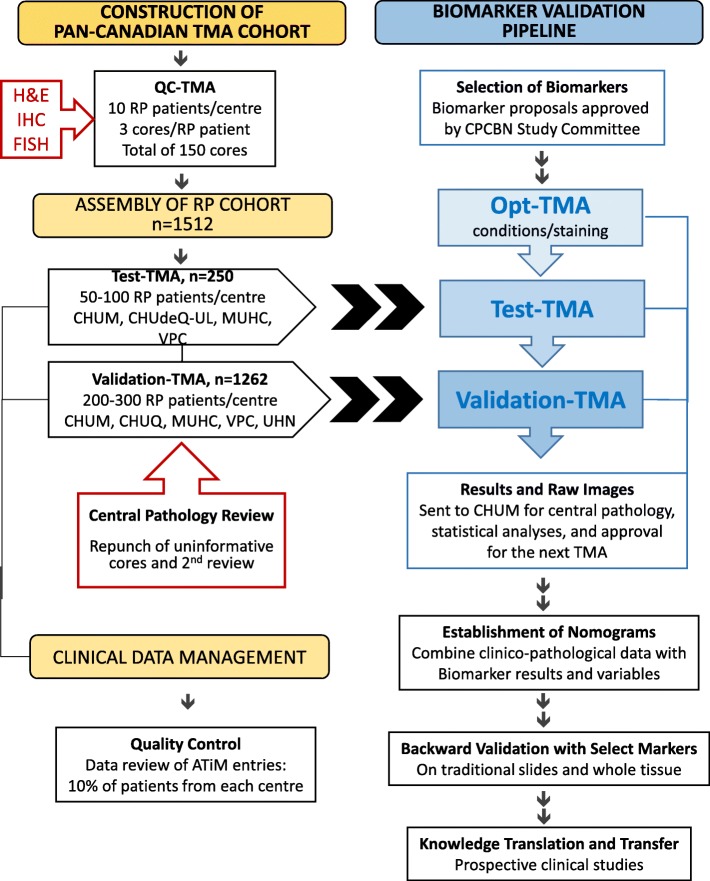
Fig. 1.
Design of the CPCBN Validation Tissue Microarray Platform for Prostate Cancer Biomarkers
Fig. 2.
Immunohistochemistry and hierarchal clustering analysis of biobanked specimens arrayed in the QC-TMA, representing 50 radical prostatectomy cases from five different centres (total of 150 cores). a IHC evaluation with nine protein tissue markers. b Hierarchal clustering based on IHC detection of the nine different markers in samples of different center origin, corresponding to the colour legend below
Analysis of FISH data using the four-probe FISH assay, showed that PTEN deletions were hemizygous or homozygous at 15.5% each, whereas the majority of cores displayed no PTEN deletions (69%) (Fig. 3a-d). The FISH results reflected the quality of the cores, reported as very good, intermediate or poor (Fig. 3e). Approximately 13% of cores were considered of poor quality because the core was either absent due to mechanical processing/sectioning, over-digested, or else, yielded a poor signal (Additional file 2). These results highlighted the need for potential modifications for TMA FISH protocols to optimize digestion and reduce background signal. Nonetheless, PTEN status was assessed for 87% of the cores. Overall, the QC-TMA demonstrated the feasibility of coordinating a large multi-institutional cohort with specimens of acceptable quality on which protein and DNA markers could be assessed.
Fig. 3.
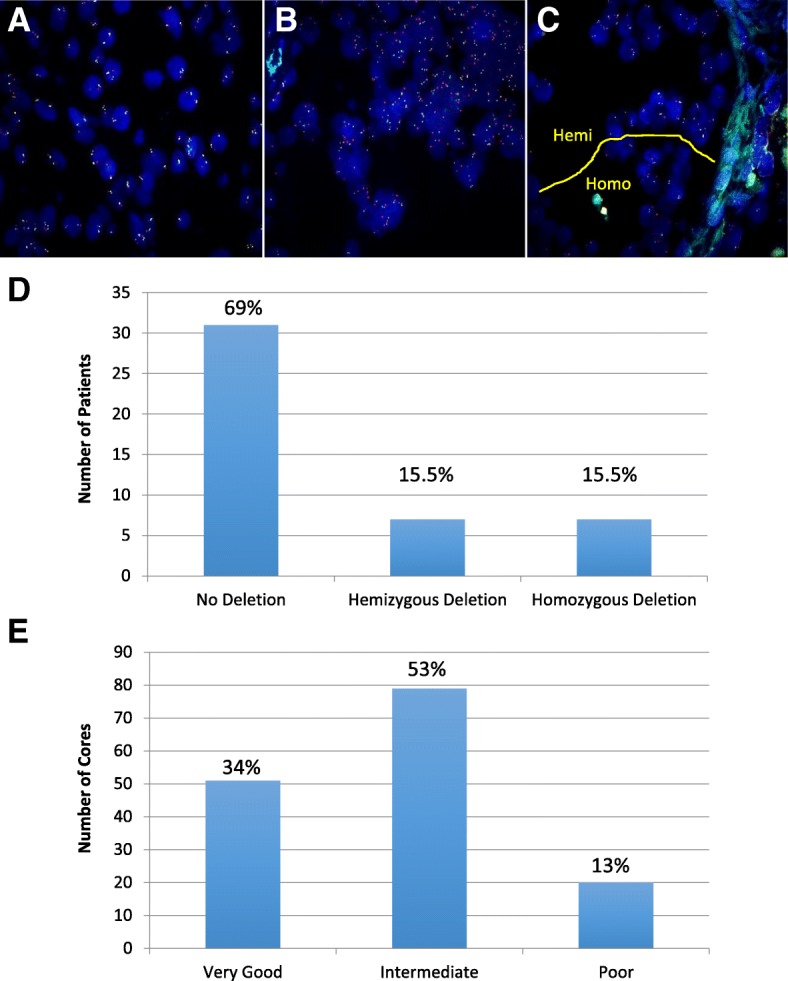
Fluorescence in-situ hybridization of the QC-TMA, with DNA probes detecting PTEN (orange), WAPAL (green), FAS (aqua), and CEP 10 (red). a Cells representing no PTEN deletion. b Cells showing homozygous PTEN deletion with relative hemizygous loss of WAPAL and FAS signal. c Cells in the same gland showing homozygous (Homo) and hemizygous (Hemi) PTEN deletions. d PTEN deletion status among the 50 patients in the QC-TMA. e Overall quality assessment of 150 cores for FISH analysis. Intermediate quality was assigned to 53% of cores that had a detectable PTEN deletion status but also had high background to signal ratios or had areas that were over-digested. Very good quality was observed for 34% of cores that produced strong signal over low background and even digestion throughout (Additional file 2)
Design and strategy of a biomarker validation process
Under the pipeline scheme (Fig. 1, right column), a study committee comprised of pathologists, clinicians and researchers selects promising markers for access to TMA resources and clinical data according to specific criteria (Table 1). This is followed by sequential evaluation through the TMA series starting with the OPT-TMA, which confirms reproducibility and reliability of staining conditions and reagents on different tissues. Upon successful completion of this step, the Test-TMA (n = 250), which evaluates the biomarker strength within a small subset representing the RP cohort, is released to the investigator. Finally, after evaluation of the performance of the biomarker, the large Validation-TMA, which contains the remaining cases of the entire RP cohort (n = 1262) is released. Both the OPT-TMA and Test-TMA represent checkpoints that determine whether biomarkers can advance along the pipeline. In the end, raw data and images are compiled and transferred to the coordinating center (CHUM) for repository and central pathology review, and secured for future nomogram development. This nomogram, once validated, could be used in a clinical setting to discriminate patients that would need a more aggressive treatment compared to those with a favorable prognosis.
Table 1.
Biomarker selection criteria and considerations
| Interest of the biomarker based on extensive preliminary data | |
| Relevance to CPCBN objectives and clinical impact for prostate cancer | |
| Cohort size used to determine biomarker status | |
| Assay performed on paraffin-embedded tissue or TMA | |
| Staining quality and requirements that include the following: • Reliable staining against controls and background levels using an automated stainer • Antibody specificity validated by western blot or IHC/immunofluorescence with appropriate controls • Preferences towards monoclonal antibody use • Preferences towards digital image analysis | |
| Specific role in prostate cancer prognosis and supporting statistical data (BCR, development of metastasis, p value) | |
| Sufficient resources for biomarker analysis (proposed laboratory, supportive infrastructure, funding, and partners) |
Test and validation TMA evaluation
Each center selected 300 RP cases to build the Test and Validation TMAs. A central pathologist reviewed each TMA block to ensure the high quality of the resource (Table 2). Core assessments for sufficient material and accurate tissue representation (cancer or adjacent benign) determined which patient samples required additional cores. At least 2 cores of tumor tissues were arrayed from a total of 1429 patients (95%) whereas 1047 patients (69%) had 3 cores or more (Table 3). For the benign adjacent tissue, at least 1 core was obtained for 1496 patients (99%) and 2 cores for 1212 patients (80%) (Table 3).
Table 2.
Central pathology review of all tissue cores contributing to the Test- and Validation-TMA series
| Sites | |||||
|---|---|---|---|---|---|
| CHUM | CHUdeQ-UL | MUHC | UHN | VPC | |
| EXPECTED BENIGN CORES | 623 | 545 | 627 | 773 | 691 |
| Reviewed as Benign | 597 | 436 | 485 | 673 | 511 |
| Reviewed as Cancer | 0 | 19 | 67 | 25 | 88 |
| Reviewed as Uninformativea | 26 | 90 | 75 | 75 | 92 |
| EXPECTED TUMOR CORES | 954 | 1269 | 953 | 1042 | 1135 |
| Reviewed as Cancer | 845 | 944 | 707 | 825 | 825 |
| Reviewed as Benign | 52 | 133 | 109 | 109 | 192 |
| Reviewed as Uninformativea | 57 | 192 | 137 | 108 | 118 |
aProstatic intraepithelial neoplasia, intraductal carcinoma, atypical small acinar proliferation, < 5% tumor cells, stroma only, muscle or inflammation
Table 3.
Number and nature of cores included in the Test- and Validation-TMA series after central pathology review
| Sites | Number of Patients | Number of Tumor Cores per Patient | Number of Benign Adjacent Cores per Patient | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | > 4 | 0 | 1 | 2 | 3 | > 4 | ||
| CHUM | 304 | 2 | 6 | 55 | 236 | 5 | 1 | 16 | 241 | 37 | 9 |
| CHUdeQ-UL | 301 | 1 | 9 | 65 | 98 | 128 | 4 | 130 | 104 | 36 | 27 |
| MUHC | 304 | 6 | 26 | 93 | 167 | 12 | 5 | 50 | 208 | 37 | 4 |
| UHN | 303 | 9 | 10 | 111 | 119 | 54 | 1 | 37 | 177 | 28 | 60 |
| VPC | 300 | 5 | 9 | 58 | 165 | 63 | 5 | 51 | 162 | 49 | 33 |
| Total | 1512 | 23 | 60 | 382 | 785 | 262 | 16 | 284 | 892 | 187 | 133 |
Clinical data management
A central ATiM database was created and customized for the CPCBN repository in which clinical data were entered and yearly updated using a standardized process. The database was subjected to quality control measures to assess the degree of entry error or missing information across all centers (Fig. 1, left panel). An audit was performed on entries for 10% of patients contributed by each site. Based on this exercise, 6 out of 6309 data entries resulted in an error rate of 0.09%, which was taken into account for standardization of data and future database updates (data not shown).
Demographic of the CPCBN cohort
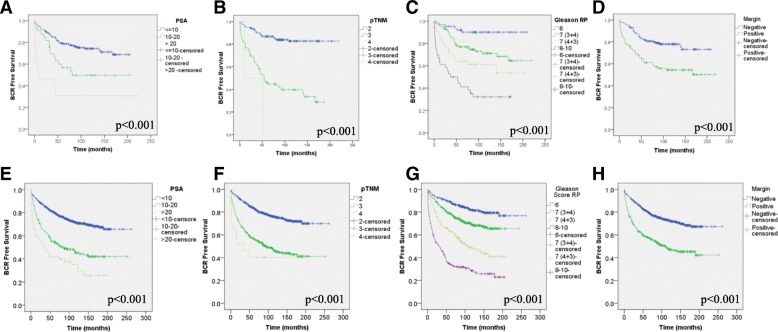
The median patient follow-up of patients was approximately 9.8 years, and a sufficient number of patients presented with endpoint elements such as BCR (34%), development of bone metastasis (4.3%) and death from PC (2.6%) to perform statistical analyses. Details on the clinico-pathological data of cohorts of patients whose prostate tissues were included in the Test-TMA as well as the Validation-TMA are presented in Table 4. In order to determine if the CPCBN cohort was representative of a general PC cohort, Cox regression analyses and Kaplan-Meier curves coupled with log-rank tests were performed using clinical parameters known to be associated with patient prognosis. As expected, PSA serum levels prior to surgery, pathological TNM, Gleason grade and margin status showed an association with BCR in both Test and Validation cohorts (Table 5 and Fig. 4). All clinical parameters except for margin status were also associated with the development of bone metastasis (Table 5 and Additional file 3: A-H) and death (Table 5 and Additional file 3: I-L).
Table 4.
Clinico-pathological features of prostate cancer patients treated by radical prostatectomy
| TMA series | Test | Validation | |||
|---|---|---|---|---|---|
| Number of patients | 250 | 1262 | |||
| Mean age at diagnosis | 61 | 61 | |||
| Median follow-up (months) | 113 | 120 | |||
| N | % | N | % | ||
| Gleason score at RP | ≤3 + 3 | 64 | 25.6 | 392 | 31.1 |
| 3 + 4 | 104 | 41.6 | 499 | 39.5 | |
| 4 + 3 | 42 | 16.8 | 188 | 14.9 | |
| ≥4 + 4 | 36 | 14.4 | 175 | 13.9 | |
| NA | 4 | 1.6 | 8 | 0.6 | |
| pTNM | 2 | 171 | 68.4 | 788 | 62.4 |
| 3 | 77 | 30.8 | 453 | 35.9 | |
| 4 | 2 | 0.8 | 21 | 1.7 | |
| Margin status | Negative | 156 | 62.4 | 837 | 66.3 |
| Positive | 91 | 36.4 | 418 | 33.1 | |
| NA | 3 | 1.2 | 7 | 0.6 | |
| Biochemical relapse | No | 173 | 69.2 | 828 | 65.6 |
| Yes | 77 | 30.8 | 434 | 34.4 | |
| Type of biochemical relapse | Rising PSA | 54 | 21.6 | 264 | 20.9 |
| Failed RP | 16 | 6.4 | 85 | 6.7 | |
| Treatment | 7 | 2.8 | 85 | 6.7 | |
| Bone metastasis | No | 239 | 95.6 | 1208 | 95.7 |
| Yes | 11 | 4.4 | 54 | 4.3 | |
| Castrate resistant | No | 237 | 94.8 | 1201 | 95.2 |
| Yes | 13 | 5.2 | 61 | 4.8 | |
| Mortality | PC specific | 4 | 1.6 | 36 | 2.9 |
| Other cause(s) | 17 | 6.8 | 119 | 9.4 | |
| Overall | 21 | 8.4 | 155 | 12.3 | |
TMA tissue microarray, RP radical prostatectomy, pTNM pathological staging, NA not available, Rising PSA serum level of prostate-specific antigen (PSA) of 0.2 ng/mL and rising, Failed RP PSA level after surgery > 0.2 ng/mL, PC prostate cancer
Table 5.
Cox regression analyses of clinico-pathological parameters on the Test- and Validation-TMA cohorts
| Endpoint | Clinical parameter | Test-TMA cohort | Validation-TMA cohort | ||||||
|---|---|---|---|---|---|---|---|---|---|
| P | Exp(B) | 95.0% CI | P | Exp(B) | 95.0% CI | ||||
| Lower | Upper | Lower | Upper | ||||||
| BCR | Serum PSA level | < 0.001 | 1.064 | 1.042 | 1.086 | < 0.001 | 1.031 | 1.026 | 1.036 |
| Gleason score at RP (6, 3 + 4, 4 + 3, > 8) | < 0.001 | 2.035 | 1.631 | 2.54 | < 0.001 | 1.946 | 1.778 | 2.13 | |
| pTNM | < 0.001 | 4.673 | 3.133 | 6.97 | < 0.001 | 2.599 | 2.202 | 3.067 | |
| Margin status | < 0.001 | 2.392 | 1.517 | 3.77 | < 0.001 | 2.362 | 1.955 | 2.852 | |
| Bone metastasis | Serum PSA level | 0.051 | 1.047 | 1 | 1.096 | 0.047 | 1.018 | 1 | 1.036 |
| Gleason score at RP (6, 3 + 4, 4 + 3, > 8) | 0.001 | 3.159 | 1.6 | 6.237 | < 0.001 | 3.333 | 2.476 | 4.487 | |
| pTNM | < 0.001 | 8.396 | 3.043 | 23.162 | < 0.001 | 3.882 | 2.422 | 6.22 | |
| Margin status | 0.125 | 2.624 | 0.765 | 9.008 | 0.988 | 0.996 | 0.569 | 1.743 | |
| PC specific death | Serum PSA level | – | – | – | – | 0.046 | 1.02 | 1 | 1.039 |
| Gleason score at RP (6, 3 + 4, 4 + 3, > 8) | 0.001 | 3.159 | 1.6 | 6.237 | < 0.001 | 3.333 | 2.476 | 4.487 | |
| pTNM | – | – | – | – | < 0.001 | 3.263 | 1.843 | 5.78 | |
| Margin status | – | – | – | – | 0.117 | 1.689 | 0.877 | 0.3252 | |
TMA tissue microarray, 95% CI 95% confidence interval, BCR biochemical recurrence, PSA prostate-specific antigen, RP radical prostatectomy, pTNM pathological staging, PC prostate cancer. Bold indicate significance
Fig. 4.
Kaplan-Meier plots showing relationship of clinical parameters with biochemical relapse (BCR). Both cohort of patients, Test (a-d) and Validation (e-h), were assessed independently. Clinical parameter evaluated were PSA level prior to surgery (a, e), pTNM (b, f), Gleason grade (c, g) and margin status (d, h). Statistical significance was set at p < 0.05
Discussion
The mandate of the CPCBN is to identify the best set of molecular markers that will complement current parameters for clinical decision-making in PC. The underlying incentive behind this pursuit is to minimize adverse health complications that result from overtreatment of clinically-indolent PC. Current diagnostics are unable to resolve the range of heterogeneity and individualized risk of patients. Although active surveillance is now an option, still too many newly diagnosed patients with early-stage tumors are aggressively treated to safeguard them against the potential fraction of tumors that progress or cause lethal disease. Despite several reports of proposed biomarkers with prognostic impact, most have been reported in the context of small cohorts, same-institution studies, or lack follow-up patient data, introducing a level of bias that limits their validation for broad clinical use [3, 5, 11, 12]. The CPCBN addresses the outstanding need for validating existing biomarkers with a TMA-based platform to validate tissue markers. With large cohorts of adequate power, standardized protocols, and extensive clinical information centralized into one database, the CPCBN validation platform provides a resource to refine a panel of markers that can be readily integrated into clinical practice.
The first phase of this initiative involved the construction of the QC-TMA, which demonstrated the quality and feasibility of a multi-center TMA resource. The results of this exercise provided a logistical assurance in building large-scale cohorts from five participating biobanks, without site-specific bias. More noteworthy was the overall informative quality of cores that were evaluated by IHC and FISH techniques already used in clinical pathology practice and diagnostic labs. With H&E staining and reference markers of tissue integrity and malignancy, we were able to assess that 94% of samples provided at least two informative cores of high quality. FISH results also demonstrated a distribution of PTEN deletions among tumor cores that were aligned with previous reports in the literature [13]. With a homogeneous patient cohort, we were able to accumulate a large sample size (n = 1512) based on power calculations that would bestow statistical significance on biomarker performance. Division of the RP cohort into a Test-TMA (n = 250) and Validation-TMA (n = 1262) enhances the selection process and power of the platform, centered upon a rigorous checkpoint scheme in which biomarker status is assessed at several stages with a “Go or No-Go” decision tree. With the addition of an OPT-TMA to ensure the efficacy of conditions and staining protocols with prospective candidates, the sequence of testing from OPT-TMA to Test-TMA to Validation-TMA guards against wasting efforts with weak biomarkers, and preserving the Validation-TMA for the most robust candidates.
CTRNet policies and SOPs, patient information is updated each year on the ATiM database. In addition updates regarding the progress status of biomarkers and associated TMAs that are assigned to each project are also entered into the database. The centralized database can also coordinate several projects for meta-analysis and help to develop nomograms that will combine current parameters with biomarker analyses and integrate age, co-morbidity, clinico-pathological staging to ultimately define an accurate profile indicating individual risk for each PC patients. The application of emerging nomograms including biomarkers could be useful in the decision-making process with correlative evidence-based science to guide patient care.
Conclusions
In conclusion, the CPCBN RP TMA has been constructed, controlled for quality and is available, in a step-wise manner, for researchers who intend to validate prognostic biomarkers in prostate cancer (for more information see http://www.tfri.ca/en/research/translational-research/cpcbn/cpcbn_access.aspx). As the first completed TMA series of the CPCBN-TMA platform, this RP cohort will serve as a prototype model that will facilitate the assembly of future retrospective and prospective cohorts for biomarker validation. Altogether the CPCBN-TMA platform will serve as an invaluable resource for the entire PC research community, accelerating breakthroughs in PC research, and supporting the establishment of nomograms to predict progression.
Additional files
Antibodies and conditions for automated immunohistochemistry staining. This table contained the antibodies and conditions for immunohistochemistry staining. (DOCX 13 kb)
Core scores of QC-TMA based on FISH analysis of PTEN deletion status. This table contains information regarding the core quality for FISH scoring. (DOCX 12 kb)
Kaplan-Meier plots showing relationship of clinical parameters with patient outcome. Both cohort of patients, Test (A-D) and Validation (E-L), were assessed independently for the endpoints of bone metastasis (A-H) and prostate cancer-specific mortality (I-L). Clinical parameter evaluated were PSA level prior to surgery (A, E), pTNM (B, F), Gleason grade (C, G) and margin status (D, H). Statistical significance was set at p < 0.05. (PPTX 302 kb)
Acknowledgements
Authors are grateful to patients who generously agreed to participate in this research by providing specimens and data to the CPCBN affiliated repositories (for a full list and for biomarker proposal form see http://www.tfri.ca/en/research/translational-research/cpcbn/cpcbn). We are also grateful to Véronique Barrès (CRCHUM), Nathalie Delvoye (CRCHUM), Jennifer Good (Kingston University), Dr. Eleonora Scarlata (MUHC-RI), Dr. Lucie Hamel (MUHC-RI), Hélène Hovington (CHUdeQ-UL), Céline Veilleux (CHUdeQ-UL), Alireza Moeen (VPC), and Karen Chadwick (UHN) for their technical support. We thank the molecular pathology core facility of the CRCHUM for performing the sections, IHC and slide scanning. We thank Jacqueline Chung for editing this manuscript. The CPCBN was funded by the Terry Fox Research Institute and the Canadian Partnership against cancer. This networks are managed and supervised by the CRCHUM. The authors declare that they have no competing interests.
Funding
This research was part of a pan-Canadian initiative named the Canadian Prostate Biomarker Network and funded by the Terry Fox Research Institute (TFRI) and the Canadian Partnership Against Cancer (CPAC). The funding body did not had any role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript in this section.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request and following the evaluation of the request by the CPCBN Study Committee.
Abbreviations
- ASAP
Atypical small acinar proliferation
- ATiM
Advanced Tissue Management
- BCR
Biochemical relapse
- CHUdeQ-UL
Centre hospitalier universitaire de Québec-Université Laval CHUdeQ-UL
- CHUM
Centre hospitalier de l’Université de Montréal
- CPCBN
Canadian prostate cancer biomarker network
- CTRNet
Canadian Tumor Repository Network
- FFPE
Formalin-fixed paraffin-embedded
- FISH
Fluorescence in situ hybridization
- GS
Gleason score
- H&E
Hematoxylin and eosin
- IDC
Intraductal carcinoma
- IHC
Immunohistochemistry
- IRB
Institutional Review Board
- MUHC
McGill University Health Centre
- OPT-TMA
Optimization TMA
- PC
Prostate cancer
- PIN
Prostatic intraepithelial neoplasia
- PSA
Prostate-specific antigen
- QC-TMA
Quality control TMA
- RP
Radical prostatectomy
- SOPs
Standard operating procedures
- TMA
Tissue microarray
- UHN
University Health Network
- VPC
Vancouver Prostate Centre
Authors’ contributions
Participation in the conception and initial design: VO, AA, AB, RGB, SC, LF, NEF, MG, PK, LK, LL, JBL, TvdK, ML, DT, AMMM, FS, Participation in the acquisition: VO, AA, AB, FB, SC, LF, LL, NEF, MG, TvdK, JAS, ML, DT, AMMM, FS. Participation in the analysis and interpretation: VO, AA, AB, FB, RGB, SC, DD, LF, LL, NEF, MG, PK, LK, JBL, TvdK, JAS, ML, DT, AMMM, F. Participation in the drafting and/or revision of the manuscript: VO, AA, AB, FB, RGB, SC, DD, LF, NEF, MG, PK, LK, LL, JBL, TvdK, JAS, ML, DT, AMMM, FS. All authors have read and approved the manuscript.
Ethics approval and consent to participate
Research ethics approval was obtained from each of the participating sites: the Centre de recherche du Centre hospitalier de l’Université de Montréal (CRCHUM), CHU de Québec-Université Laval (CHUdeQ-UL), McGill University Health Centre (MUHC), Vancouver Prostate Centre (VPC), and University Health Network (UHN). All patients signed an informed consent to participate within one of the biobanks and agreed to the use of their specimens and data for research purposes.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Véronique Ouellet, Email: veronique.ouellet.chum@ssss.gouv.qc.ca.
Armen Aprikian, Email: armen.aprikian@muhc.mcgill.ca.
Alain Bergeron, Email: Alain.Bergeron@crchudequebec.ulaval.ca.
Fadi Brimo, Email: Fadi.brimo@mcgill.ca.
Robert G. Bristow, Email: robert.bristow@manchester.ac.uk
Simone Chevalier, Email: simone.chevalier@mcgill.ca.
Darrel Drachenberg, Email: drach13@mymts.net.
Ladan Fazli, Email: lfazli@prostatecentre.com.
Neil E. Fleshner, Email: Neil.Fleshner@uhn.on.ca
Martin Gleave, Email: m.gleave@ubc.ca.
Pierre Karakiewicz, Email: pierrekarakiewicz@gmail.com.
Laurence Klotz, Email: laurence.klotz@sunnybrook.ca.
Louis Lacombe, Email: Louis.Lacombe@crchudequebec.ulaval.ca.
Jean-Baptiste Lattouf, Email: jean-baptiste.lattouf.chum@ssss.gouv.qc.ca.
Theodorus van der Kwast, Email: Theodorus.vanderKwast@uhn.ca.
Jeremy A. Squire, Email: jsquireinsp@gmail.com
Mathieu Latour, Email: mathieu.latour.chum@ssss.gouv.qc.ca.
Dominique Trudel, Email: dominique.trudel.chum@ssss.gouv.qc.ca.
Anne-Marie Mes-Masson, Email: anne-marie.mes-masson@umontreal.ca.
Fred Saad, Phone: 514 890-8000, Email: fredsaad@videotron.ca.
References
- 1.Frank SB, Miranti CK. Disruption of prostate epithelial differentiation pathways and prostate cancer development. Front Oncol. 2013;3:273. doi: 10.3389/fonc.2013.00273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Auprich M, Bjartell A, Chun FK, de la Taille A, Freedland SJ, Haese A, et al. Contemporary role of prostate cancer antigen 3 in the management of prostate cancer. Eur Urol. 2011;60(5):1045–1054. doi: 10.1016/j.eururo.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Huber F, Montani M, Sulser T, Jaggi R, Wild P, Moch H, et al. Comprehensive validation of published immunohistochemical prognostic biomarkers of prostate cancer -what has gone wrong? A blueprint for the way forward in biomarker studies. Br J Cancer. 2015;112(1):140–148. doi: 10.1038/bjc.2014.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohler JL, Kantoff PW, Armstrong AJ, Bahnson RR, Cohen M, D'Amico AV, et al. Prostate cancer, version 2.2014. J Natl Compr Canc Netw. 2014;12(5):686–718. doi: 10.6004/jnccn.2014.0072. [DOI] [PubMed] [Google Scholar]
- 5.Prensner JR, Rubin MA, Wei JT, Chinnaiyan AM. Beyond PSA: the next generation of prostate cancer biomarkers. Sci Transl Med. 2012;4(127):127rv3. doi: 10.1126/scitranslmed.3003180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fraser M, Berlin A, Ouellet V, Saad F, Bristow RG. Prostate Cancer genomics as a driver of personalized medicine-Chapter 14. In: Dellaire G, Berman JN, Arceci RJ, editors. Cancer genomics: Academic Press; 2014.
- 7.Boutros PC, Fraser M, Harding NJ, de Borja R, Trudel D, Lalonde E, et al. Spatial genomic heterogeneity within localized, multifocal prostate cancer. Nat Genet. 2015;47(7):736–745. doi: 10.1038/ng.3315. [DOI] [PubMed] [Google Scholar]
- 8.Kristiansen G. Diagnostic and prognostic molecular biomarkers for prostate cancer. Histopathology. 2012;60(1):125–141. doi: 10.1111/j.1365-2559.2011.04083.x. [DOI] [PubMed] [Google Scholar]
- 9.Yoshimoto M, Ludkovski O, Good J, Pereira C, Gooding RJ, McGowan-Jordan J, et al. Use of multicolor fluorescence in situ hybridization to detect deletions in clinical tissue sections. Lab Invest. 2018;98(6):839. doi: 10.1038/s41374-018-0037-4. [DOI] [PubMed] [Google Scholar]
- 10.Leyh-Bannurah SR, Trudel D, Latour M, Zaffuto E, Grosset AA, Tam C, et al. A multi-institutional validation of Gleason score derived from tissue microarray cores. Pathol Oncol Res. 2018. [DOI] [PubMed]
- 11.Hawley S, Fazli L, McKenney JK, Simko J, Troyer D, Nicolas M, et al. A model for the design and construction of a resource for the validation of prognostic prostate cancer biomarkers: the canary prostate Cancer tissue microarray. Adv Anat Pathol. 2013;20(1):39–44. doi: 10.1097/PAP.0b013e31827b665b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Narayan VM, Konety BR, Warlick C. Novel biomarkers for prostate cancer: an evidence-based review for use in clinical practice. Int J Urol. 2017;24(5):352–360. doi: 10.1111/iju.13326. [DOI] [PubMed] [Google Scholar]
- 13.Troyer DA, Jamaspishvili T, Wei W, Feng Z, Good J, Hawley S, et al. A multicenter study shows PTEN deletion is strongly associated with seminal vesicle involvement and extracapsular extension in localized prostate cancer. Prostate. 2015;75(11):1206–1215. doi: 10.1002/pros.23003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Antibodies and conditions for automated immunohistochemistry staining. This table contained the antibodies and conditions for immunohistochemistry staining. (DOCX 13 kb)
Core scores of QC-TMA based on FISH analysis of PTEN deletion status. This table contains information regarding the core quality for FISH scoring. (DOCX 12 kb)
Kaplan-Meier plots showing relationship of clinical parameters with patient outcome. Both cohort of patients, Test (A-D) and Validation (E-L), were assessed independently for the endpoints of bone metastasis (A-H) and prostate cancer-specific mortality (I-L). Clinical parameter evaluated were PSA level prior to surgery (A, E), pTNM (B, F), Gleason grade (C, G) and margin status (D, H). Statistical significance was set at p < 0.05. (PPTX 302 kb)
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request and following the evaluation of the request by the CPCBN Study Committee.