Abstract
Background:
Dysmenorrhoea is a common health problem among females in their reproductive years. Available information on dysmenorrhoea in university student in abah, Saudi Arabia is limited. The objective of the study was to assess the prevalence of dysmenorrhea and associated menstrual symptoms and their self-management techniques among female university students of King Khalid University (KKU).
Methods:
This cross-sectional study was conducted at College of health science in KKU, Saudi Arabia. Sample: A total of 197 students aged between 18 and 23 years. A Self-administrated questionnaire was used to collect data.
Results:
Dysmenorrhea was reported by more than two-thirds of the girls (70.6%). In the 139 girls, who reported dysmenorrhea, its related information on severity of pain, medication use, and care-seeking behavior is detailed in the table. Severe pain was reported by (35.2%) respondents. Two-third of the respondents (66%) reported using medications for pain relief and use of herbal medicine was also found to be quite prevalent (69.1%). The gastrointestinal problems were the most common symptoms experienced by the students and were significantly high among the dysmenorrheal students. Less than one in four respondents (23%) reported consulting a doctor for their dysmenorrheal while most of them consulted with friends and family.
Conclusion:
Dysmenorrhea is a very common problem among the university students. A number of symptoms were related with dysmenorrhea. Even though it is common, and may not have a pathological cause, few students seek medical advice. Increasing the awareness can help in relieving the burden of this common health problem.
Keywords: Dysmenorrhea, Saudi Arabia, students
Introduction
Menstruation is an important indicator of women's reproductive and endocrine health.[1,2,3,4] Although it is a natural phenomenon, many girls face problems of menstruation such as irregular bleeding, excessive bleeding, and painful menstruation.[5] Painful menstruation or dysmenorrhea is a common gynecologic disorder among young females. It is defined as pelvic pain directly related to menstruation and is associated with various other symptoms. Dysmenorrhea is classified into two categories: primary when pelvic examination and ovulatory function are normal and secondary when there is an identifiable gynecological pathology. Primary dysmenorrhea characteristically begins when adolescents attain their ovulatory cycles; generally, within the 1st year after menarche.[1,6] Dysmenorrhea is considered the most common symptom of all menstrual complaints and poses a greater burden of disease than any other gynecological complaint in developing countries.[7]
Although common, dysmenorrhea remains poorly understood and is rarely taken into consideration when assessing female health.[3] Pain or cramping sensations in the lower abdomen may be accompanied by headaches, dizziness, diarrhea, a bloated feeling, nausea and vomiting, backache, and leg pains.[8,9] These symptoms are reported to be the most common reasons for adolescents visiting a gynecologist.[2,10] The high prevalence of dysmenorrhea among adolescents (50%–70%),[1,2,9] especially in the 1st year of their reproductive life influences their daily activities,[8,5,10,11] and is thus a major public health problem.[12]
Although menstrual irregularity can be normal during the first few years after menarche, other menstrual signs and symptoms such as amenorrhea, excessive uterine bleeding, dysmenorrheal, and premenstrual syndrome may indicate a pathological condition which requires prompt attention and referral.[1] Difference in physiological and pathological origin of dysmenorrhea may be poorly understood and result in anxiety, fear, anger, confusion, shame, disgust, and even depression in girls during their first menstrual experiences.[8,13] Studies on the prevalence of menstrual pain have shown that many factors are related to this disorder. These factors include: age below 20, low body mass index, smoking, early menarche, prolonged or aberrant menstrual flow, pelvic infections, somatization, psychological, and genetic factors; all of these factors can influence the prevalence and the severity of dysmenorrhea.[14,15] Lifestyle modifications, for example, choosing a diet low in fat like the vegetarian diet, was found to decrease the duration and the intensity of the menstrual cramps.[16] However, to date, pharmacotherapy remains the most reliable and effective treatment for abdominal pain related to primary dysmenorrhea.[17]
With high prevalence and low awareness of menstrual disorders, investigation of this problem is deeply needed. Thus, this study was devised to assess the prevalence of dysmenorrhea and associated menstrual symptoms and their self-management techniques among female university students of King Khalid University (KKU), a large public university of Southwestern Saudi Arabia.
Subjects and Methods
This cross-sectional study was conducted at KKU, Abha, which is the capital of Aseer Province, situated at 2200 meters above sea level in Southwestern Saudi Arabia. The study sample included 197 first year students from the college of health science in the academic year 2017. Married students, students with known pelvic pathology, and those who refused to participate in this survey were excluded from the study.
The data were collected by a validated semi-structure self-administered, anonymous English questionnaire. The questionnaire was developed with reference to previous literature on the same topic conducted in Saudi Arabia and other regional countries.[18,19,20] The variables included in the questionnaire were sociodemographic data and question related to menstruation which including age at menarche, regularity of menstrual cycle, duration of cycle and flow, pain during menstruation during the last 12 months, severity of pain, symptoms experienced during menstruation, and care-seeking behavior to manage dysmenorrhea. Dysmenorrhea is defined by crampy pelvic pain beginning shortly before or at the onset of menses and lasting 1–3 days.[1]
Regular menstruation was defined as a cycle repeated once every 28–32 days with duration 5–7 days.[20] A scale of 0–10 was used to measure the severity of menstrual pain. The participants were asked to rate the degree of pain by marking on the number. The score marked on the scale were classified into mild dysmenorrhea if it is between 1 and 3 point, moderate between 4 and 7, and severe between 8 and 10 points.[2]
A pilot study was carried out among eight participants who were subsequently excluded from the study. In agreement with the participants’ feedback, further modifications were undertaken and content validity was checked by two experts in this field.
Data were collected in November and December 2017 by taking permission from the college authority based on the students’ academic schedule. Purposive sampling technique was used to select the respondents. The selected respondents were explained about the purpose of the study and were requested to complete the questionnaires. Informed verbal consent was obtained from all participants, in addition, it was stressed on the confidentiality of data and they were informed that the data would not be used for anything except for the study. Two female teachers form the college were involved in data collection. The data were collected 2 days in a week after class and the students completed the questionnaires in the presence of the teachers. The research was conducted after getting approval from the Research Ethics Committee of King Khalid University.
The data were analyzed using SPSS for Windows version 20 (IBM Corp: Armonk, NY). Descriptive statistics used to calculate mean and percentage for most the variables. A Pearson Chi-square test was used to determine the association between variables. P < 0.05 of the test measures were considered statistically significant.
Results
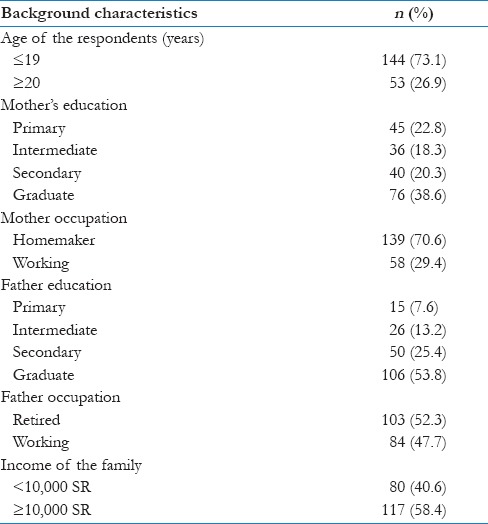
Table 1 presents the basic sociodemographic characteristics of the respondents. The age range of the study group varied between 18 and 23 years, with the mean age of 19.1 ± 0.95 years. Majority (73.1%) of them were ≤19 years and the rest of them were 20 years of age or above. Most of the study participants reported the education of their mothers as school education, namely primary (22.8%), intermediate (18.3%), and secondary (20.3%), while 38.6% mothers were reported having graduate education. More than 70% of mothers were reported being homemakers, while 30% were working mothers. On the other hand, more than half of the fathers (50.3%) were reported as graduate. The working status of fathers was reported as retired for more than half (52.3%) fathers. The monthly family income was reported as < 10,000 SR per month by 40.6% respondents and more than or equal to 10,000 SR by 58.4% respondents.
Table 1.
Background characteristics of the respondents
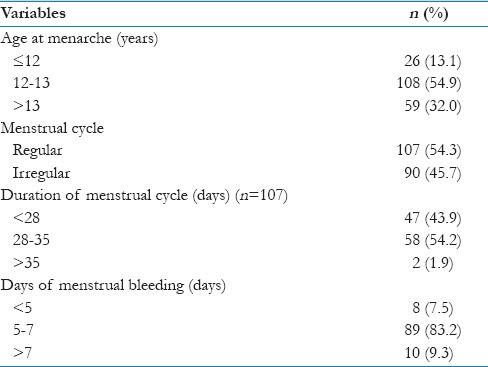
The menstruation-related information of the respondents is presented in Table 2. The age range for menarche was reported between 9 and 16 years and the mean age at menarche was found to be 12.9 ± 1.4 years. More than half of the respondents (54.9%) reported menarche between 12 and 13 years. A large proportion of the study participants reported irregular menses (45.7%). Regarding the duration of menstrual cycle, an average duration of 27.8 ± 3.8 days, with a range of 21–45 days was established. Around 44% respondents reported the duration of menstrual cycle as <28 days, while 54.2% reported between 28 and 35 days. Very few respondents (1.9%) reported a cycle of more than 35 days. Average number of bleeding days per menstrual cycle was found to be 6.3 ± 1.2 days, with a range of 2–9 days. Most of the respondents (83.2%) reported 5–7 bleeding days per period, 7.5% reported <5 days, and 9.3% reported more than 7 bleeding days per period.
Table 2.
Menstruation-related information
In Table 3, information related with dysmenorrhea is presented. Dysmenorrhea was reported by more than two-thirds of the girls (70.6%). In the 139 girls, who reported dysmenorrhea, its related information on severity of pain, medication use, and care-seeking behavior is detailed in the table. Severe pain was reported by 35.2% respondents, 46.8% reported moderate pain, while 18% reported mild pain. Two-third of the respondents (66%) reported using medications for pain relief. Nonsteroidal anti-inflammatory (NSAID) drugs like aspirin or panadol were used by 64.7% girls. Use of herbal medicine was also found to be quite prevalent (69.1%) with different herbs and home remedies such as cinnamon and anise tea.
Table 3.
Information related with dysmenorrhea
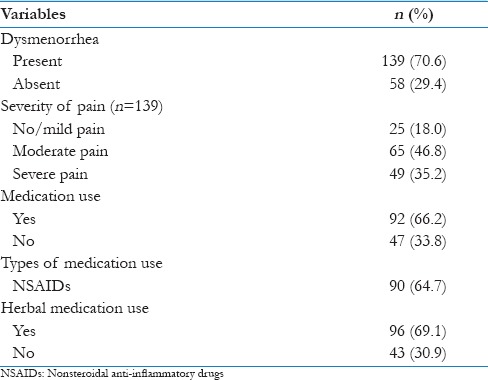
Table 4 represents the data pertaining to the symptoms experienced by the respondents during menstruation. The symptoms can be broadly classified into gastrointestinal (GI) symptoms, aches and pains, and any other symptoms. Among the GI symptoms, change in appetite was reported by more than half of the girls. Nausea (45.7%) and bloating (43.1%) were the other common symptoms. Change in bowels reported as either diarrhea, constipation, or both were reported by almost one in four participants. Vomiting was reported by 23.9% and heartburn or indigestion by 20.3% respondents. Various aches and pains were reported by the respondents. Low back pain was more commonly reported, affecting 54.3% girls, and headache was reported by 24.4%. Another symptom that affected girls during menstruation was dizziness as reported by 42.1% and tiredness by 24.4% of them.
Table 4.
Symptoms experienced by the respondents during menstruation
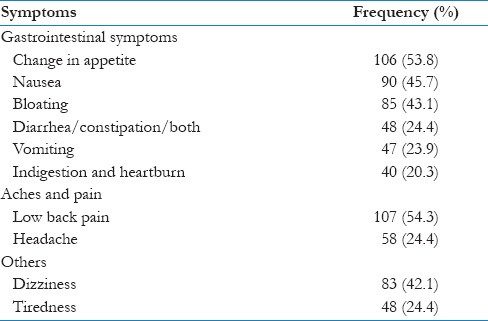
Table 5 shows the comparative analysis of the symptoms experienced during menstruation among respondents who reported dysmenorrhea, with those who reported no dysmenorrhea. Nausea was reported significantly more by respondents complaining of dysmenorrhea (81.1%) as compared to 18.9% by those not having dysmenorrhea (P = 0.003). Vomiting was reported by 89.4% of respondents having dysmenorrhea as compared to 10.6% having no dysmenorrhea, making it a significant difference between the two groups with a P = 0.001. The other significant differences were regarding feeling of indigestion that was reported by 82.5% by the girls reporting dysmenorrhea as compared to 17.5% without dysmenorrhea (P = 0.045), and change in appetite reported by 76.4% of respondents having dysmenorrhea as compared to 23.6% who did not complain of dysmenorrhea (P = 0.037). Headache was reported significantly more by respondents suffering from dysmenorrhea as compared to those without dysmenorrhea (P = 0.001). Eighty-six percent of cases of headache were reported in the dysmenorrhea group. The other symptoms such as bloating (74.1%), diarrhea (77.1%), low back pain (67.3%), tiredness (79.2%), and dizziness (72.3%) were also reported more in the group suffering from dysmenorrhea; however, these differences were not statistically significant.
Table 5.
Relationship between symptoms and dysmenorrhea
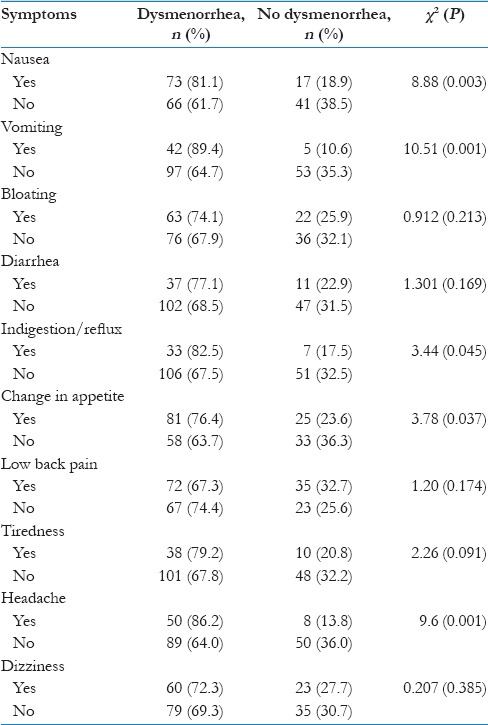
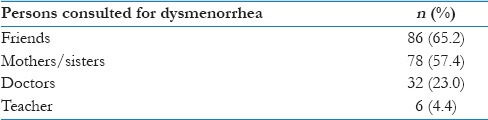
Table 6 presents information on the person consulted for dysmenorrhea. Less than one in four respondents (23%) reported consulting a doctor for their dysmenorrhea, while around 65% consulted their friends and 57.4% consulted their family members. Few respondents (4.4%) also reported consulting with their teachers about this issue of dysmenorrhea.
Table 6.
Person consulted for dysmenorrhea
Discussion
This study aimed to determine the prevalence of dysmenorrhea and its related symptoms, dysmenorrheal pain severity, and its management practices among female university students. This study established the “typical” experience of menstruation for a sample of Saudi teenage girls in terms of pain, symptoms, and help-seeking behavior.
The results of the current study showed that the prevalence of dysmenorrheal was relatively high as it was reported by more than two-thirds of the girls (70.6%), which is higher than the rate reported from a study in Saudi Arabia (60.9%).[18] However, this proportion lies within the reported values from various developing and developed countries. Published studies have shown variable rates of dysmenorrhea among university students ranging from 34% in Egypt, 70.2% in India, 85% among Hispanic female adolescents, and 93% in Australia.[2,21,22,23] The variations of prevalence rates of dysmenorrhea across the world may be due to the deficiency of a universally accepted method for defining dysmenorrheal as well as the use of different categories of target population subjects.[24]
Among those who reported dysmenorrhea, its related information on severity of pain, medication use, and help-seeking behavior was inquired. Severe pain was reported by 35.2% respondents in this study is in accordance with findings from a cross-sectional study conducted in Dammam University (Kingdom of Saudi Arabia) revealed that about 35% of university females had severe dysmenorrhea.[25] Previous studies showed that the prevalence of severe dysmenorrheal pain varies from 0.9% reported from Korea to 59.8% reported from Bangladesh.[26]
The spectrum of symptoms associated with menstrual pain ranges from various GI symptoms including nausea, abdominal cramps, aches and pains, and feeling of tiredness and dizziness.[26] In this study, the most common symptoms associated with dysmenorrhea were low back pain, dizziness, nausea, and bloating. Similar patterns of symptoms have been observed in an Indian study. They found tiredness and back pain as the most prevalent menstrual symptoms.[22] However, this is not in accordance with a regional study in Palestine, where the most common symptoms associated with dysmenorrhea were physical fatigue and emotional instability manifested as nervousness/irritability.[27] This may be due to the difference in perception of dysmenorrhea, cultural, and environmental factors.
Around two-thirds of the respondents (64.7%) in this study reported using NSAID medications for pain relief. This is an interesting finding and revealed some regional differences in medication use among girls. In some Middle Eastern countries like Palestine, approximately 58% of dysmenorrheal students with moderate/severe pain opted for medications to decrease symptoms of painful menstruation. Similar results were obtained in a study published from Iran.[28] Whereas, in an Indian study, only a small proportion of girls had sought pharmacological management (25.5%) while the majority used herbal and other nonpharmacological approaches to decrease pain.[22] In the current study, the use of herbal medicine was also found to be quite prevalent (69.1%) with different herbs and home remedies such as cinnamon and anise tea. Seeking for herbal remedies is a common feature among dysmenorrheal female students across most published studies.[2,3,4,20]
The help-seeking behavior of the respondents revealed less than one in four respondents reported consulting a doctor for their dysmenorrhea. The girls showed a preference for consulting their family members, that is, mother, sister, or friends for this issue. An important role of teachers was indicated, as about 5 in 100 participants revealed talking to their teachers about it. Previous studies have reported a reluctance of girls to consult with doctors and seek medical intervention for dysmenorrhea.[26,27] An Indian study also reported that only 14.2% had sought medical advice.[22] This suboptimal use of the medical advice has also been reported by others.[29,30] This may be because the young students may feel shy to go to doctor or they may believe that the painful periods are normal with no need to seek medical advice.
The findings of the current study derived from a small sample and in one region of Saudi Arabia limits the generalization of the results. Studies with large sample of university students are necessitated. Nevertheless, this study provided useful information about menstrual health care issues among Saudi university students thus helping physicians to plan and develop strategies for improving reproductive health among this group.
Conclusion
Based on the findings of this study, it can be concluded that dysmenorrhea is very common problem among the university students. A number of symptoms were related with dysmenorrhea. Dysmenorrheal pain and associated symptoms may affect the daily activities of the students and may lower the quality of life. This area needs further investigation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The author shows gratitude to Professor Shamsun Nahar and Dr. Aesha Farheen, assistant professor in the Department of Family and Community Medicine for helping in analysis, writing, and editing the manuscript. A special word of thanks to Dr. Amani A Othman for helping in data collection.
References
- 1.Padubidri VG, Daftar S. 16th ed. New Delhi: Reed Elsevier India Private Limited; Dysmenorrhea and pre-menstrual syndrome Shaw's Textbook of Gynecology; pp. 471–4. [Google Scholar]
- 2.Parker MA, Sneddon AE, Arbon P. The menstrual disorder of teenagers (MDOT) study: Determining typical menstrual patterns and menstrual disturbance in a large population-based study of Australian teenagers. BJOG. 2010;117:185–92. doi: 10.1111/j.1471-0528.2009.02407.x. [DOI] [PubMed] [Google Scholar]
- 3.Sharma A, Taneja DK, Sharma P, Saha R. Problems related to menstruation and their effect on daily routine of students of a medical college in Delhi, India. Asia Pac J Public Health. 2008;20:234–41. doi: 10.1177/1010539508316939. [DOI] [PubMed] [Google Scholar]
- 4.Avasarala AK, Panchangam S. Dysmenorrhoea in different settings: Are the rural and urban adolescent girls perceiving and managing the dysmenorrhoea problem differently? Indian J Community Med. 2008;33:246–9. doi: 10.4103/0970-0218.43231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumbhar SK, Reddy M, Sujana B, Reddy RK, Divya BK, Balkrishna C. Prevalence of dysmenorrhea among adolescent girls (14-19yrs) of Kadapa district and its impact on quality of life: A cross sectional study. Natl J Community Med. 2011;2:265–8. [Google Scholar]
- 6.Durain D. Primary dysmenorrhea: Assessment and management update. J Midwifery Womens Health. 2004;49:520–8. doi: 10.1016/j.jmwh.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Patel V, Tanksale V, Sahasrabhojanee M, Gupte S, Nevrekar P. The burden and determinants of dysmenorrhoea: A population-based survey of 2262 women in Goa, India. BJOG. 2006;113:453–63. doi: 10.1111/j.1471-0528.2006.00874.x. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal AK, Agarwal A. A study of dysmenorrhea during menstruation in adolescent girls. Indian J Community Med. 2010;35:159–64. doi: 10.4103/0970-0218.62586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adeyemi AS, Adekanle DA. Management of dysmenorrhoea among medical students. Int J Gynecol Obstet. 2007;7:1528–39. [Google Scholar]
- 10.Sharma M, Gupta S. Menstrual pattern and abnormalities in the high school girls of Dharan: A cross sectional study in two boarding schools. Nepal Med Coll J. 2003;5:34–6. [PubMed] [Google Scholar]
- 11.Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. 2014;36:104–13. doi: 10.1093/epirev/mxt009. [DOI] [PubMed] [Google Scholar]
- 12.Kural M, Noor NN, Pandit D, Joshi T, Patil A. Menstrual characteristics and prevalence of dysmenorrhea in college going girls. J Family Med Prim Care. 2015;4:426–31. doi: 10.4103/2249-4863.161345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan SS, Yiu KW, Yuen PM, Sahota DS, Chung TK. Menstrual problems and health-seeking behaviour in Hong Kong Chinese girls. Hong Kong Med J. 2009;15:18–23. [PubMed] [Google Scholar]
- 14.Rizk DE, Mosallam M, Alyan S, Nagelkerke N. Prevalence and impact of premenstrual syndrome in adolescent schoolgirls in the United Arab Emirates. Acta Obstet Gynecol Scand. 2006;85:589–98. doi: 10.1080/00016340600556049. [DOI] [PubMed] [Google Scholar]
- 15.Latthe P, Mignini L, Gray R, Hills R, Khan K. Factors predisposing women to chronic pelvic pain: Systematic review. BMJ. 2006;332:749–55. doi: 10.1136/bmj.38748.697465.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.French L. Dysmenorrhea. Am Fam Physician. 2005;71:285–91. [PubMed] [Google Scholar]
- 17.Lefebvre G, Pinsonneault O, Antao V, Black A, Burnett M, Feldman K, et al. Primary dysmenorrhea consensus guideline. J Obstet Gynaecol Can. 2005;27:1117–46. doi: 10.1016/s1701-2163(16)30395-4. [DOI] [PubMed] [Google Scholar]
- 18.Ibrahim NK, AlGhamdi MS, Al-Shaibani AN, AlAmri FA, Alharbi HA, Al-Jadani AK, et al. Dysmenorrhea among female medical students in King Abdulaziz University: Prevalence, predictors and outcome. Pak J Med Sci. 2015;31:1312–7. doi: 10.12669/pjms.316.8752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ismaile S, Al-Enezi S, Otaif W, Al-Mahadi A, Bingorban N, Barayaan N. Prevalence of menstrual pain among Saudi nursing students and its effect on sickness absenteeism. Health. 2016;8:198–205. [Google Scholar]
- 20.Al-AsadiJn AQ. Dysmenorrhoea and its impact on daily routine activities among secondary school students in Basra, Iraq. J Fac Med Baghdad. 2013;55:339–44. [Google Scholar]
- 21.Kamel DM, Tantawy SA, Abdelsamea GA. Experience of dysmenorrhea among a group of physical therapy students from Cairo University: An exploratory study. J Pain Res. 2017;10:1079–85. doi: 10.2147/JPR.S132544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Omidvar S, Bakouei F, Amiri FN, Begum K. Primary dysmenorrhea and menstrual symptoms in Indian female students: Prevalence, impact and management. Glob J Health Sci. 2016;8:53632. doi: 10.5539/gjhs.v8n8p135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Banikarim C, Chacko MR, Kelder SH. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch Pediatr Adolesc Med. 2000;154:1226–9. doi: 10.1001/archpedi.154.12.1226. [DOI] [PubMed] [Google Scholar]
- 24.Chia CF, Lai JH, Cheung PK, Kwong LT, Lau FP, Leung KH, et al. Dysmenorrhoea among Hong Kong university students: Prevalence, impact, and management. Hong Kong Med J. 2013;19:222–8. doi: 10.12809/hkmj133807. [DOI] [PubMed] [Google Scholar]
- 25.Al-Dabal BK, Koura MR, Al-Sowielem LS, Barayan SS. Dysmenorrhea and associated risk factors among university students in Eastern province of Saudi Arabia. World Fam Med J Inc Middle East J Fam Med. 2014;7:5. [Google Scholar]
- 26.De Sanctis V, Soliman AT, Elsedfy H, Soliman NA, Soliman R, El Kholy M, et al. Dysmenorrhea in adolescents and young adults: A review in different country. Acta Biomed. 2017;87:233–46. [PMC free article] [PubMed] [Google Scholar]
- 27.Abu Helwa HA, Mitaeb AA, Al-Hamshri S, Sweileh WM. Prevalence of dysmenorrhea and predictors of its pain intensity among Palestinian female university students. BMC Womens Health. 2018;18:18. doi: 10.1186/s12905-018-0516-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rakhshaee Z. A cross-sectional study of primary dysmenorrhea among students at a university: Prevalence, impact and of associated symptoms. Ann Res Rev Biol. 2014;4:2815. [Google Scholar]
- 29.Konapur SK, Nagaraj C. Dysmenorrhoea and premensrtual syndrome: Frequency and effect on daily activities of adolescent girls in rural areas of Bangalore. Int J Med Sci Public Health. 2014;3:1225–8. [Google Scholar]
- 30.Farotimi AA, Esike J, Nwozichi CU, Ojediran TD, Ojewole FO. Knowledge, attitude, and healthcare-seeking behavior towards dysmenorrhea among female students of a private university in Ogun State, Nigeria. J Basic Clin Reprod Sci. 2015;4:33–8. [Google Scholar]


