Abstract
Introduction:
Anemia is common in Chronic Kidney Disease (CKD) and diabetes is a major leading risk factor for it. In Diabetic Kidney Disease (DKD), it worsens more, which further increases cardiovascular morbidity and mortality. Despite of adequate iron stores anemia persist, which may be due to impaired iron release from body stores that is unable to meet the demand for erythropoiesis (also called reticuloendothelial cell iron blockade). High parathyroid hormone (PTH) along with vitamin D, may be attributable for anemia.
Methods:
A cross-sectional study of 150 advanced (Stage 4 & 5) pre dialyzed DKD patients (GFR <30ml/min/1.73 m2), aged 40-70 years were included over a period of 1 year. Any other concomitant illness/ drugs leading to anemia were excluded. Serum samples were collected and urea, creatinine, hemoglobin, iron profile, vitamin D, iPTH, uric acid, calcium, phosphorous and albumin levels were measured. A data base was constructed on Microsoft Excel 2007 and statistical analyses were performed using the SPSS software version 20.0 (IBM, NY, USA).
Results:
Stage 5 DKD had more pronounced anemia compared to stage 4 DKD (P < 0.001). Hemoglobin (Hb) was inversely correlated with iPTH (r = -0.74, P < 0.001) and was associated with vitamin D deficiency (r = 0.51, P < 0.001) but not with serum ferritin. DKD patients with low eGFR (r = -0.6, P < 0.001), vitamin D (r = -0.43, P < 0.001) and serum calcium (r = -0.37, P < 0.001) had higher iPTH. Secondary hyperparathyroidism (beta=-0.005; P < 0.001) and Vitamin D (beta=0.053; P < 0.01) were strong predictor for Hb while parameters of iron profile was not statistically significant.
Conclusion:
An efficient control of PTH hypersecretion is therefore required to achieve a better management of anemia as well as mineral metabolism in DKD patients.
Keywords: Anemia, diabetes kidney disease, iron profile, intact parathyroid hormone, Vitamin D
Introduction
Anemia commonly contributes to the poor quality of life (QOL) in patients with chronic kidney disease (CKD).[1] It is commonly prevalent in CKD patients and difficult to manage.[2] More than 50% of CKD patients have diabetes. Anemia is most common in diabetic kidney disease (DKD) patients due to multifactorial causes, and hence, it should be evaluated independently of CKD stage to identify any reversible process contributing to the anemia.[3,4] Serum parameters of iron profile are important determinants for anemia and guide further management in CKD patients.[5,6] However, secondary hyperparathyroidism (SHPTH) such as anemia develops early in the course of CKD and worsen as the disease progress and have a deleterious effect.[3,7] Disorder of CKD-associated mineral bone disorder might be one of the underrecognized causes of anemia, and it needs to be corrected. Hence, a cross-sectional study was undertaken in Indian context, to access the association of Vitamin D and SHPTH with hemoglobin (Hb) level in nondialyzed advanced DKD patients.
Materials and Methods
A cross-sectional study of 150 advanced (Stage 4 and 5) predialyzed DKD patients (glomerular filtration rate [GFR] <30 ml/min/1.73 m2), aged 40–70 years were included over 1 year. Patients taking nonsteroidal anti-inflammatory drugs and those having external blood loss, malignancy, malaria, septicemia, tuberculosis, autosomal dominant polycystic kidney disease or concomitant, any other chronic illness such as rheumatoid arthritis and systemic lupus erythematosus, and Vitamin B12/folic acid deficient patients were excluded from this study. There was no history of blood transfusion or intravenous iron therapy in the past 3 months, and the patients were not on erythropoietin (EPO) therapy or Vitamin D supplementation. This study was approved by the ethical committee of the University, and informed consent was obtained from patients, and it confirms to the provision of Declaration of Helsinki (as revised in Tokyo 2004). Patients were categorized according to the stages of CKD by calculating the GFR by modification of diet in renal disease equation (Kidney Disease: Improving Global Outcomes guidelines). Predialysis venous blood samples were taken. Blood chemistry was carried out with Mindray BC-5380 autoanalyzer and Roche Cobas C-311 biochemical analyzer. Vitamin D and intact parathyroid hormone (iPTH) were assessed by chemiluminescent immunoassay technology by Roche Cobas e-411 Immunoanalyzer. Fasting iron profile was assessed by Roche Cobas C-311 biochemical analyzer. To increase the sensitivity and specificity of this study, we have calculated iPTH by the third generation immunometric assay. A database was constructed on Microsoft Excel 2007, and statistical analyses were performed using the SPSS software version 20.0 (IBM, NY, USA).
Results
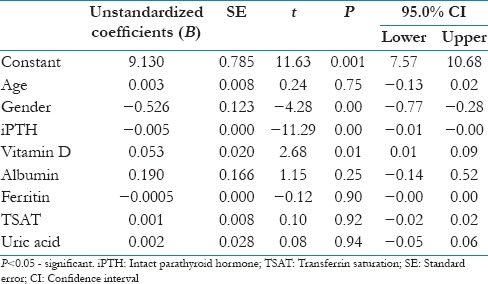
Age of the patients ranged from 40 to 70 years with a mean age of 50.01 ± 8.20 years. About 53.3% were male (n = 83), whereas 44.7% were female (n = 67). A total of 50 (33.3%) cases were Stage 4 DKD while remaining 100 (66.7%) were Stage 5 DKD. About 75% of the above patients were also hypertensive. Half of the above patients had uncontrolled blood sugar, and in 52 (34.6%) patients, blood sugar was within normal limit without any glucose lowering drug. Proteinuria was present in all patients by dipstick method. Biochemical parameters of above patients are shown in Table 1, which showed low mean Hb with SHPTH with Vitamin D deficiency, hypocalcemia, and hyperphosphatemia as well as hyperuricemia. Serum ferritin and transferrin saturation (TSAT) were sufficient. Significantly lower level of Hb, Vitamin D, and higher iPTH were found in patients of Stage 5 DKD than Stage 4 DKD [Table 2]. Univariate analysis showed Hb was strongly correlated with iPTH (r = −0.74, P < 0.001) and serum Vitamin D (r = 0.51, P < 0.001) but not with serum ferritin. iPTH was inversely correlated with Vitamin D (r = −0.43, P < 0.001) and serum calcium (r = −0.37, P < 0.001). Multivariate linear regression analysis showed iPTH (β = −0.005; P < 0.001) and Vitamin D (β =0.053; P = 0.01) were strong predictor for Hb, whereas parameters of iron profile was not statistically significant [Table 3].
Table 1.
Biochemical characteristics of diabetic kidney disease patients
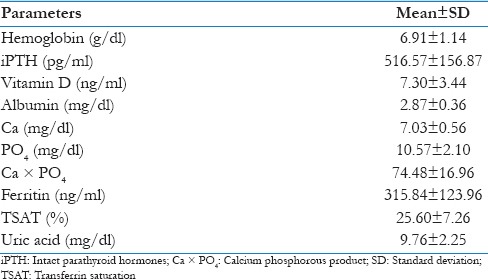
Table 2.
Biochemical parameters according to stage of diabetic kidney disease
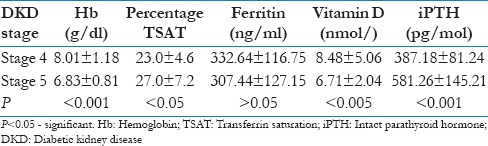
Table 3.
Multiple regression analysis with serum hemoglobin level as dependent variable in patients
Discussion
Patients with DKD and anemia have poorer outcomes and an impaired QOL; anemia is a significant contributor to both. The presence of diabetes and progression of CKD are associated with increased incidence of anemia.[8]
In our study, despite adequate TSAT and serum ferritin, patients had low Hb. Patients in Stage 5 compared to Stage 4 DKD had significant low level of Hb along with significant low level of Vitamin D and high level of iPTH which is consistent with other studies.[9,10] However, with significantly high TSAT (Stage 5 vs. Stage 4), Hb was low which may be due to impaired iron release from body stores that is unable to meet the demand for erythropoiesis (also called reticuloendothelial cell iron blockade).[11] High PTH may be one of the attributable causes along with low Vitamin D.
In our study, patients with low Hb level were found to have high iPTH which is consistent with other studies.[12,13,14] The high levels of circulating PTH have multiple biological effects, including an unfavorable influence on anemia of CKD patients. There may be inhibition of early erythroid progenitors, endogenous EPO synthesis, and red blood cell (RBC) survival and loss as well as due to indirect, negative effect of PTH on bone marrow cellularity; there is fibrosis which may lead to decreased EPO and increased resistance to EPO.[15] In CKD patients, the surgical and pharmacological suppression of PTH release leads to improvement in anemia. In the prerecombinant human EPO (r-HuEpo) era, these centered on a direct toxic effect of PTH on proliferation of red cell precursors in the marrow and antagonism of the effect of endogenous or exogenous EPO.[16,17,18] In the r-HuEpo-treated patients, a clear relationship has been demonstrated between the degree of trabecular fibrosis and r-HuEpo dose. Moreover, the high-PTH level could also shift bone cells toward adipocytes. It is suggested that excessive amounts of PTH interfere with normal erythropoiesis by downregulating the EPO receptors on erythroid progenitor cells in the bone marrow. Therefore, physiologic concentrations of EPO can no longer sustain normal red cell counts with ensuing normocytic normochromic anemia. In primary hyperparathyroidism, this effect is observed with very high concentrations of PTH. In SHPTH, during chronic renal failure, this effect is more pronounced because EPO synthesis is impaired.[19]
A significant association and positive correlation are found between serum Vitamin D and Hb level.[20,21] EPO cells express calcitriol receptors, which induces proliferation and maturation of erythroid progenitor cells. Therefore, deficiency of calcitriol, a cause of hyperparathyroidism may impair erythropoiesis. The administration of Vitamin D and analogs has been associated with an improvement of anemia and/or a reduction in EPO requirements. The positive effects of Vitamin D on both anemia and EPO requirements, during CKD, could be related to its suppressive effects on PTH.[10]
Vitamin D was inversely correlated with iPTH and is consistent with other various studies. When estimated GFR drops below 30 ml/min/1.73 m2 (CKD Stage 4), the 1α-hydroxylase activity becomes impaired. This, in turn, will cause a significant decrease in intestinal calcium absorption leading to a reduction in circulating serum calcium.[22] It is postulated that calcitriol deficiency, direct effect of PTH on EPO release, RBC production, and loss of erythrocytes, reduce erythropoiesis.[23] Downregulation of the parathyroid, Vitamin D, and calcium-sensing receptors are the critical steps that lead to abnormalities in mineral metabolism – high phosphate, low calcium, and Vitamin D deficiency. These imbalances result in parathyroid hyperplasia leading to SHPTH, low serum calcium, elevated phosphorus, and high calcium-phosphorus product.[12] As a result of these, the relative risk of mortality and anemia increases.
The medical management of SHPTH in patients with CKD principally involves dietary changes, the use of the combination of phosphate binders, active Vitamin D analogs, and/or calcimimetics (which increase the sensitivity of the calcium-sensing receptors to calcium) with the treatment of underlying conditions including hypertension, cardiac ailments, and diabetes. This will lead to improvement in anemia as well as cardiovascular mortality.[24]
Conclusion
An efficient control of PTH hypersecretion is, therefore, required to achieve a better management of anemia as well as mineral metabolism in DKD patients. Recent studies are also looking for additional inflammatory markers for hyporesponsiveness of anemia in DKD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mehdi U, Toto RD. Anemia, diabetes, and chronic kidney disease. Diabetes Care. 2009;32:1320–6. doi: 10.2337/dc08-0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nurko S. Anemia in chronic kidney disease: Causes, diagnosis, treatment. Cleve Clin J Med. 2006;73:289–97. doi: 10.3949/ccjm.73.3.289. [DOI] [PubMed] [Google Scholar]
- 3.O’Mara NB. Anemia in patients with chronic kidney disease. Diabetes Spectr. 2008;21:12–9. [Google Scholar]
- 4.Nakhoul G, Simon JF. Anemia of chronic kidney disease: Treat it, but not too aggressively. Cleve Clin J Med. 2016;83:613–24. doi: 10.3949/ccjm.83a.15065. [DOI] [PubMed] [Google Scholar]
- 5.National Kidney Foundation. KDIGO clinical practice guidelines for anemia in chronic kidney disease. Kidney Int Suppl. 2012;2:279–335. [Google Scholar]
- 6.Iimori S, Naito S, Noda Y, Nishida H, Kihira H, Yui N, et al. Anaemia management and mortality risk in newly visiting patients with chronic kidney disease in Japan: The CKD-ROUTE study. Nephrology (Carlton) 2015;20:601–8. doi: 10.1111/nep.12493. [DOI] [PubMed] [Google Scholar]
- 7.Joy MS, Karagiannis PC, Peyerl FW. Outcomes of secondary hyperparathyroidism in chronic kidney disease and the direct costs of treatment. J Manag Care Pharm. 2007;13:397–411. doi: 10.18553/jmcp.2007.13.5.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bajaj S, Makkar BM, Abichandani VK, Talwalkar PG, Saboo B, Srikanta SS, et al. Management of anemia in patients with diabetic kidney disease: A consensus statement. Indian J Endocrinol Metab. 2016;20:268–81. doi: 10.4103/2230-8210.176348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lau BC, Ong KY, Yap CW, Vathsala A, How P. Predictors of anemia in a multi-ethnic chronic kidney disease population: A case-control study. Springerplus. 2015;4:233. doi: 10.1186/s40064-015-1001-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Icardi A, Paoletti E, De Nicola L, Mazzaferro S, Russo R, Cozzolino M, et al. Renal anaemia and EPO hyporesponsiveness associated with vitamin D deficiency: The potential role of inflammation. Nephrol Dial Transplant. 2013;28:1672–9. doi: 10.1093/ndt/gft021. [DOI] [PubMed] [Google Scholar]
- 11.Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. 2012;23:1631–4. doi: 10.1681/ASN.2011111078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chutia H, Ruram AA, Bhattacharyya H, Boruah P, Nath C. Association of secondary hyperparathyroidism with hemoglobin level in patients with chronic kidney disease. J Lab Physicians. 2013;5:51–4. doi: 10.4103/0974-2727.115935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baradaran A, Nasri H. Intensification of anaemia by secondary hyperparathyroidism in hemodialysis patients. Med J Islam Acad Sci. 2001;14:161–6. [Google Scholar]
- 14.Memon I, Norris KC, Bomback AS, Peralta C, Li S, Chen SC, et al. The association between parathyroid hormone levels and hemoglobin in diabetic and nondiabetic participants in the National Kidney Foundation's Kidney Early Evaluation Program. Cardiorenal Med. 2013;3:120–7. doi: 10.1159/000351229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drüeke TB, Eckardt KU. Role of secondary hyperparathyroidism in erythropoietin resistance of chronic renal failure patients. Nephrol Dial Transplant. 2002;17(Suppl 5):28–31. doi: 10.1093/ndt/17.suppl_5.28. [DOI] [PubMed] [Google Scholar]
- 16.Gallieni M, Corsi C, Brancaccio D. Hyperparathyroidism and anemia in renal failure. Am J Nephrol. 2000;20:89–96. doi: 10.1159/000013563. [DOI] [PubMed] [Google Scholar]
- 17.Cunningham J, Locatelli F, Rodriguez M. Secondary hyperparathyroidism: Pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol. 2011;6:913–21. doi: 10.2215/CJN.06040710. [DOI] [PubMed] [Google Scholar]
- 18.Sliem H, Tawfik G, Moustafa F, Zaki H. Relationship of associated secondary hyperparathyroidism to serum fibroblast growth factor-23 in end stage renal disease: A case-control study. Indian J Endocrinol Metab. 2011;15:105–9. doi: 10.4103/2230-8210.81939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nasri H. Intensification of anemia by secondary hyperthyroidism in hemodialysis patients. Iran J Med Sci. 2003;28:195–7. [Google Scholar]
- 20.Gutierrez O. Philadelphia, Pennsylvania: 2008. Nov 4-9, Vitamin D Deficiency and Anemia in Chronic Kidney Disease (CKD). Program and Abstracts of the Renal Week 2008: American Society of Nephrology (ASN) Annual Meeting, F-FC325. [Google Scholar]
- 21.Kim YL, Kim H, Kwon YE, Ryu DR, Lee MJ, Park KS, et al. Association between vitamin D deficiency and anemia in patients with end-stage renal disease: A Cross-sectional study. Yonsei Med J. 2016;57:1159–64. doi: 10.3349/ymj.2016.57.5.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rozita M, Noorul Afidza M, Ruslinda M, Cader R, Halim AG, Kong CT, et al. Serum vitamin D levels in patients with chronic kidney disease. EXCLI J. 2013;12:511–20. [PMC free article] [PubMed] [Google Scholar]
- 23.Wu SG, Jeng FR, Wei SY, Su CZ, Chung TC, Chang WJ, et al. Red blood cell osmotic fragility in chronically hemodialyzed patients. Nephron. 1998;78:28–32. doi: 10.1159/000044878. [DOI] [PubMed] [Google Scholar]
- 24.Mousavi SS, Shahbazian H, Tamadon MR. Association of secondary hyperparathyroidism with anemia in patients with end-stage renal disease; A review on current knowledge. J Parathyroid Dis. 2016;4:48–53. [Google Scholar]


